Abstract
Malaria poses significant public health challenges and huge disease and economic burdens across the world, notably in low-income countries. Although great strides have been achieved, the COVID-19 pandemic hinders the progress towards global elimination of malaria. This study utilizes data from the global burden of disease study 2021 data sources to assess trends in incidence and mortality of, and disability-adjusted life years (DALYs) lost due to malaria before and after the global COVID-19 pandemic, and projects the incidence of malaria in 2030 at international, regional and national levels. The age-standardized incidence of malaria declined from 3789.28 per 100,000 populations in 2010 to 3332.96 per 100,000 population in 2019, followed by a rapid increase to 3485.27 per 100,000 populations in 2021. The estimated annual percentage change was 2.26% (95% confidence interval: 1.84–2.68%) from 2019 to 2021, suggesting a significant acceleration in the increasing rate compared to previous years. The numbers of DALYs lost and death due to malaria also increased in 2021. Children under 5 years of age and regions with low socio-demographic index were disproportionately affected with the highest burden of malaria associated with the COVID-19 pandemic. The pandemic is projected to lead to an additional 472.59 malaria cases per 100,000 populations by 2030. The global COVID-19 pandemic has posed substantial challenges to the global malaria elimination program as revealed by increasing incidence, death and DALYs lost across the world.
Similar content being viewed by others
Introduction
Malaria, a vector-borne disease caused by infection with the genus Plasmodium and transmitted by female anopheline mosquitoes, remains a significant global public health challenge, particularly in tropical and subtropical regions where environmental conditions facilitate its transmission1,2. Decades of efforts have resulted in great strides in the global malaria elimination programme3; however, there has been a resurgence in the global burden due to malaria, and 263 million cases were estimated to have malaria across the world in 2023, with 597 000 deaths reported4. In many African and Southeastern Asian countries, malaria remains highly prevalent5. For example, more than 3.24 million people were affected by malaria in Ethiopia in 20236.
Insecticide-treated bed nets and indoor residual spraying are crucial components of malaria control strategies, which have been proven to be effective to prevent malaria transmission in many settings7. However, these efforts had been hindered by the coronavirus disease 2019 (COVID-19) pandemic after 20208. COVID-19, caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2)9, has brought a profound socioeconomic impact on various aspects of society, including the global malaria elimination programme5,6. Control initiatives such as bed net distribution, mass drug administration (MDA), surveillance activities, diagnosis and treatment services were disrupted or halted during the pandemic, creating gaps in preventive measures, case identification and treatment coverage12. This disruption potentially contributed to the resurgence of malaria in affected regions6. It was estimated that at least two-thirds of the excess deaths due to malaria (47,000 out of 69,000 deaths) reported in 2020 compared to 2019 figures were associated with the COVID-19 pandemic13.
Updating our understanding of the empirical evidence regarding the impact of the global COVID-19 pandemic on malaria is crucial for intensified control efforts and public health support. In this study, we conducted a systematic evaluation of the global burden of malaria using the global burden of disease (GBD) dataset. Our objective was to assess the global, regional, and national burdens of malaria before and after the COVID-19 pandemic, aiming to contribute to a deeper understanding of the indirect consequences of the COVID-19 pandemic on malaria, which may provide insights into formulation of the global malaria elimination strategy during the post-COVID-19 era.
Methods
Data sources
This study utilized data from the GBD study, which is coordinated by the Institute for Health Metrics and Evaluation (IHME) at the University of Washington. Specifically, we employed the GBD 2021 dataset, which provides comprehensive burden estimates for 371 diseases and injuries, as well as 87 risk factors and their combinations14. These estimates cover 21 regions globally, encompassing 204 countries and territories14. The GBD 2021 study methodology, along with its enhancements compared to previous versions, has been extensively detailed in prior publications7,8,9,10,11.
Data extraction
This article provided a comprehensive analysis of the disease burden of malaria spanning the period from 2010 to 2021, with a specific focus on the 10-year period from 2010 to 2019 before and 2 years after the onset of the COVID-19 pandemic (2020 and 2021). The study utilized data presented as rates per 100,000 person-years, ensuring comparability through age-standardized rate (ASR) and uncertainty interval (UI) using the GBD world population standard. Standardized methodologies are employed to estimate key epidemiological metrics such as prevalence, incidence, mortality, and disability-adjusted life years (DALYs). In addition, the UI of the incidence, mortality of and DALYs lost due to malaria were estimated.
The study presented results stratified by gender, age, and the socio-demographic index (SDI), which categorized 204 countries and territories into five distinct regions based on their socio-economic development and health status. Age was categorized into five groups: <5 years, 5–14 years, 15 to 49 years, 50 to 69 years, and 70 + years.
Statistical analysis
The estimated annual percentage change (EAPC) was calculated for the quantification of annual changes in disease burden, providing insights into the direction and magnitude of trends. The EAPC allows indicators, ASR trends were interpreted as follows: a decrease if both the EAPC and the upper limit of its 95% confidence interval (CI) were 0 and below and an increase if both were above 0, while stability if neither condition was met. To forecast the burden of malaria in 2030, we used a linear log age-time-cohort model for projections of linear trends. The statistical software programs used for modeling were R version 4.3.3. The prediction model was created using the NORDPRED package in R software12.
Results
Incidence
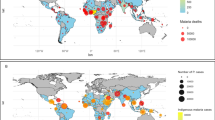
In 2010, an estimated 0.26 billion (95% UI: 0.22 to 0.31 billion) incident cases of malaria were recorded globally. This number decreased to 0.24 billion (95% UI: 0.19 to 0.30 billion) by 2019; however, it rose again to 0.25 billion (95% UI: 0.20 to 0.32 billion) in 2021. The ASR of malaria incidence declined from 3,789.28 (95% UI: 3242.61 to 4534.81) per 100,000 populations in 2010 to 3332.96 (95%UI 2666.75 to 4225.54) per 100,000 populations in 2019, with an EAPC of −1.44% (95% CI −2.09 to −0.79%). Nevertheless, the ASR of malaria incidence was 3485.27 (95% UI 2804.46 to 4435.69) per 100,000 populations in 2021, with an EAPC of 2.26% (95% CI 1.84–2.68%) from 2019 to 2021, suggesting a shift from a downward trend to an upward trend relative to the period 2010 to 2019 (Table 1; Fig. 1A). As shown in (Fig. 1A), the trends for both genders decreased gradually from 2010 to 2019, and maintained stable for several years thereafter. After that, another sharp rise was seen again after 2019. The overall ASR of malaria incidence was slightly higher among females than males across the study period, and the highest incidence of malaria was observed among children under 5 years of age, followed by at ages of 5 to 14 years. Increasing incidence was noticed after 2019 among children under 5 years (Fig. 1B). ASR of malaria incidence was highest in low SDI regions, while the fastest increase rate was seen in middle SDI regions (Fig. 1C). The top 10 countries with incidence of over 20% (over 20,000 per 100,000 populations) included Liberia, Benin, Burkina Faso, Solomon Islands, Sierra Leone, Guinea, Central African Republic, Mozambique, Nigeria and Democratic Republic of the Congo in 2021 (Table 2), where the increasing rate remained stable after the COVID-19 pandemic. Notably, Nicaragua is the country with the highest rate of change in malaria incidence: increased incidence from 27.86 per 100,000 populations in 2010 to 459.40 per 100,000 populations in 2019, followed by a sharp increase to 2340.84 per 100,000 populations in 2021, with an annual increasing rate of over 125% after the COVID-19 pandemic (Supplementary Table 1).
The ASR of malaria from 2010 to 2021. (A) Incidence grouped by gender; (B) Incidence grouped by age groups; (C) Incidence grouped by SDI regions; (D) Deaths grouped by gender; (E) Deaths grouped by age groups; (F) Deaths grouped by SDI regions; (G) DALYs lost due to malaria grouped by gender; (H) DALYs lost due to malaria grouped by age groups; (I) DALYs lost due to malaria grouped by SDI regions. ASR Age-standardized rate, DALYs disability-adjusted life years, SDI socio-demographic index.
Death
In 2010, 866,834 deaths occurred due to malaria, which decreased to 667,861 in 2019; however, the deaths rebounded to 748,131 in 2021. The overall ASR of malaria mortality was 13.00 (95% UI 7.05 to 21.16) per 100,000 populations in 2010, decreased to 9.30 (95% UI 3.73 to18.07) per 100,000 populations in 2019, and rose to 10.51 (95% UI 3.81 to 21.45) per 100,000 populations in 2021 (Table 1). There was no significant difference in malaria mortality across genders (Fig. 1D). Deaths due to malaria were extremely high among younger populations and were lowest at ages of 15 to 59 years (Table 1; Fig. 1E). The ASR of malaria mortality was negatively associated with SDI levels, showing that low SDI regions had the highest ASR (Fig. 1F). Countries with a malaria mortality rate of more than 1% (> 100 per 100,000 populations) included Burkina Faso, Sierra Leone, Niger, Liberia, Benin, Cote d’Ivoire, Cameroon, Mozambique, and Nigeria in 2021 (Table 2). Notably, Uganda experienced a 50% decline in the malaria mortality from 2010 to 2019 (from 89.91 to 45.00 per 100,000 populations), but it returned to previous levels after the COVID-19 pandemic (93.01 per 100,000 populations).
DALYs
The numbers of DALYs lost due to malaria have showed a downward trend before the COVID-19 pandemic and an upward trend after the COVID-19 pandemic, with 66.43 million in 2010, 49.72 million in 2019, and 55.17 million in 2021. DALYs lost due to malaria had experienced a significant decline from 2010 to 2019, followed by a sharp increase after the COVID-19 pandemic (Fig. 1G). Most DALYs lost due to malaria was found among populations under 5 years of age (Fig. 1H) and those from low SDI countries (Table 1; Fig. 1I). The top ten countries with the heaviest burden of DALYs lost due to malaria included Sierra Leone, Burkina Faso, Niger, Benin, Liberia, Cote d’Ivoire, Nigeria, Uganda, Burundi, and Cameroon. Among these countries, Uganda experienced a doubled DALYs lost due to malaria in 2021 [6008.63 per 100,000 populations, 95% UI (2044.84 to 11,064.79) per 100,000 populations] comparing to 2996.12 (95% UI 1102 to 5597.64) per 100,000 populations in 2019 (Table 2).
Projection of malaria burden in 2030
To illustrate the impact of the COVID-19 pandemic on the malaria burden in the coming decade, we initially utilized data from 1990 to 2019 to forecast future trends in malaria incidence. The malaria burden was projected to continue its decline after 2019, with an estimated incidence rate of 2806.07 cases per 100,000 populations by 2030 (Fig. 2A and Supplementary Table 2). We then extended our analysis to include data from the pandemic era (1990–2021) to reassess the disease burden up to 2030. The findings indicated an additional 472.59 cases per 100,000 populations, resulting in a total of 3278.65 cases per 100,000 populations in 2030 (Fig. 2A). A similar increase in deaths and DALYs lost due to malaria was noted, suggesting that the projected malaria burden in 2030 surpassed the estimates made in 2019 (Fig. 2B, C).
The ASR of malaria and its prediction to 2030. (A) The prediction of incidence; (B) The prediction of deaths; (C) The prediction of DALYs lost due to malaria. The green line represents predictions based on data up to 2019, while the red line represents predictions based on data up to 2021. ASR age-standardized rate, EAPC estimated annual percentage change.
Discussion
This study revealed that, despite significant progress in the global malaria elimination programme, the burden of malaria experienced a resurgence after the COVID-19 pandemic. The rebound is particularly pronounced in low SDI regions and among children under 5 years of age.
The global progress towards malaria elimination has been substantial over the last decade, driven by effective interventional strategies such as distribution and use of insecticide-treated nets, indoor residual spraying, and targeted drug interventions for vulnerable groups, such as children under 5 years and pregnant women13. The COVID-19 pandemic has had significant and multifaceted impacts on malaria elimination efforts globally14, which has been predicted by multiple studies15,16. It was estimated that malaria-related deaths could increase by up to 36% globally over the next five years because of the COVID-19 pandemic15. The resurgence of malaria, particularly noticeable in low SDI regions and among children under 5 years old, may be attributed to a confluence of factors exacerbated by the COVID-19 pandemic. These areas, characterized by weaker healthcare infrastructures and limited access to essential health services, were already facing significant challenges in malaria control before the pandemic. The main reasons for malaria rebound of after the COVID-19 pandemic include disruption of routine immunizations and preventive measures that leads to a decline in herd immunity and increased transmission, reduced family investments into preventive measures and timely medical care-seeking due to pandemic-induced economic downturns, and reshaping of resources towards COVID-19 response, leaving fewer resources for malaria elimination programmes.
One of the primary impacts resulting from the COVID-19 pandemic is the disruptions to health systems and malaria control programmes11. Preventive measures implemented to reduce COVID-19 transmission after the pandemic, such as lockdowns and travel restrictions, although seem effective to reduce the transmission of many infectious diseases, did not directly impact the life cycle of malaria parasites. Nevertheless, disruptions in supply chains and access to healthcare services also affected the availability of resources critical for malaria elimination15. Scenario analysis indicated that frequent implementation and withdrawal of infection prevention strategies may lead to unstable malaria exposure patterns, potentially increasing the risk of severe diseases17. Another cause was allocation of limited resources after the pandemic. As suggested by the WHO in April 2020, medical and other resources should be shifted towards containment of the COVID-19 pandemic to fight this unprecedented global health crisis18, and this may lead to the temporary cessation of case detection, community surveys, and mass treatment of many infectious diseases, including malaria.
Our findings showed that children under 5 years remained disproportionately affected by malaria during the pandemic, but the situation was exacerbated due to disruptions in routine health services and preventive measures. The interruption of critical health services, such as antenatal care, immunization programmes, and regular distribution of long-lasting insecticidal nets19, together with restricted access to diagnostics and treatment, led to a surge in malaria cases and deaths among this vulnerable population. Given the success of school-based mass drug administration programs20, such as seasonal malaria chemoprophylaxis, in reducing malaria incidence among children, it is crucial to explore the feasibility and potential impact of integrating these targeted interventions into broader malaria elimination strategies. Thus, while young children have always been major victims of malaria, the pandemic intensifies their vulnerability through service disruptions and necessitates targeted investments to restore and enhance malaria control interventions1. There had been no available malaria vaccines recommended by WHO to battle this big killer until late 202121. This absence contributed to maintaining high malaria incidence globally, as highlighted in recent studies22.
Despite these challenges, the COVID-19 pandemic presents opportunities to enhance malaria elimination efforts in the post-pandemic era. The WHO recommends a “reactive” approach for the control of malaria—implemented soon after a confirmed case is identified—and a “focal” strategy—targeting higher-risk individuals residing near the case to control malaria transmission23. Lessons gained from containment of the COVID-19 pandemic, notably advanced contact tracing methodologies and reorganization of healthcare infrastructures for rapid emergency responses, share valuable experiences that may be adapted to intensify malaria elimination efforts. Specifically, implementation of digital contact tracing platforms, which has been proven to be effective for rapid tracking and isolation of COVID-19 cases, may potentially be employed to monitor and manage populations at a risk of malaria, thereby breaking transmission cycles24,25. Moreover, the prospective widespread deployment of malaria vaccines, informed by rapid advancements in COVID-19 vaccine research and development, holds significant promise for reducing childhood mortality rates attributed to malaria in the future26. During the COVID-19 pandemic, there was a significant mobilization of resources towards combating the virus, demonstrating the strong global coordination and information sharing if a disease is recognized as a global threat2. However, this study highlights that such a singular focus on COVID-19 may have inadvertently harmed other health priorities, such as malaria elimination. It is crucial to strike a balance between addressing emerging global health threats and maintaining essential health services for ongoing diseases like malaria.
The strength of this study lies in its utilization of the updated GBD data 2021 to provide a detailed estimate of the burden due to malaria before and after COVID-19 pandemic. While the effects of the pandemic on malaria have been a subject of extensive study by organizations such as the World Health Organization, our findings provide a unique perspective by focusing on pre- and post-COVID-19 pandemic. Gao and colleagues27 also examined the disease burden of malaria following the COVID-19 pandemic; however, their analysis was limited in Africa and used the data up to 2020, which did not comprehensively assessed the global, regional or national burdens of malaria. A primary limitation of our study is the potential underreporting of cases throughout the pandemic period. Restrictions on movement, diminished access to healthcare services, and prioritization of diagnostic resources for COVID-19 testing have collectively hampered routine malaria diagnosis and surveillance efforts, potentially resulting in underestimations and delays in case identification. Should these factors indeed contribute to underreported data, the actual disease burden could be more severe than estimated. Another constraint is the temporal scope of the available data, which spans merely two years post-pandemic, as the GBD dataset has been updated only up to 2021. Conclusive assessments of long-term health consequences of this unprecedented event rely on continued data collection and analysis over time.
Conclusions
In summary, the results of the present study demonstrate that the burden of malaria has escalated sharply since 2019, disproportionately affecting younger populations and low-income countries. The COVID-19 pandemic has posed substantial challenges to the global malaria elimination programme, exacerbating the complex interplay between poverty and disease burden and worsening conditions for vulnerable populations globally.
Data availability
Publicly available datasets were analyzed in this study. The raw data are available from GBD data 2021 (https://vizhub.healthdata.org/gbd-results/).
References
Duffy, P. E., Gorres, J. P., Healy, S. A. & Fried, M. Malaria vaccines: a new era of prevention and control. Nat. Rev. Microbiol. https://doi.org/10.1038/s41579-024-01065-7 (2024).
Monroe, A., Williams, N. A., Ogoma, S., Karema, C. & Okumu, F. Reflections on the 2021 world malaria report and the future of malaria control. Malar. J. 21, 154. https://doi.org/10.1186/s12936-022-04178-7 (2022).
Feachem, R. G. A. et al. Malaria eradication within a generation: ambitious, achievable, and necessary. Lancet 394, 1056–1112. https://doi.org/10.1016/s0140-6736(19)31139-0 (2019).
World Health Organization. World malaria report 2024. (accessed 11 December 2024); https://www.who.int/teams/global-malaria-programme
Lassi, Z. S., Naseem, R., Salam, R. A., Siddiqui, F. & Das, J. K. The impact of the COVID-19 pandemic on immunization campaigns and programs: A systematic review. Int. J. Environ. Res. Public Health 18 https://doi.org/10.3390/ijerph18030988 (2021).
Dalton, M. et al. Impact of COVID-19 on routine childhood immunisations in low- and middle-income countries: A scoping review. PLoS Glob. Public. Health 3, e0002268. https://doi.org/10.1371/journal.pgph.0002268 (2023).
Global incidence. prevalence, years lived with disability (YLDs), disability-adjusted life-years (DALYs), and healthy life expectancy (HALE) for 371 diseases and injuries in 204 countries and territories and 811 subnational locations, 1990–2021: a systematic analysis for the global burden of disease study 2021. Lancet (Lond. Engl.) https://doi.org/10.1016/s0140-6736(24)00757-8 (2024).
Global burden of. 288 Causes of death and life expectancy decomposition in 204 countries and territories and 811 subnational locations, 1990–2021: a systematic analysis for the global burden of disease study 2021. Lancet (Lond. Engl.) https://doi.org/10.1016/s0140-6736(24)00367-2 (2024).
Global fertility in 204 countries and territories. 1950–2021, with forecasts to 2100: a comprehensive demographic analysis for the global burden of disease study 2021. Lancet (Lond. Engl.) https://doi.org/10.1016/s0140-6736(24)00550-6 (2024).
Global age-sex. -specific mortality, life expectancy, and population estimates in 204 countries and territories and 811 subnational locations, 1950–2021, and the impact of the COVID-19 pandemic: a comprehensive demographic analysis for the global burden of disease study 2021. Lancet (Lond. Engl.) https://doi.org/10.1016/s0140-6736(24)00476-8 (2024).
Burden of disease scenarios for 204 countries and territories. 2022–2050: a forecasting analysis for the global burden of disease study 2021. Lancet (Lond. Engl.) 403, 2204–2256. https://doi.org/10.1016/s0140-6736(24)00685-8 (2024).
Møller, B. et al. Prediction of cancer incidence in the nordic countries: empirical comparison of different approaches. Stat. Med. 22, 2751–2766. https://doi.org/10.1002/sim.1481 (2003).
Monroe, A. et al. Improving malaria control by Understanding human behaviour. Bull. World Health Organ. 99, 837–839. https://doi.org/10.2471/blt.20.285369 (2021).
Heuschen, A. K. et al. Public health-relevant consequences of the COVID-19 pandemic on malaria in sub-Saharan Africa: a scoping review. Malar. J. 20, 339. https://doi.org/10.1186/s12936-021-03872-2 (2021).
Hogan, A. B. et al. Potential impact of the COVID-19 pandemic on HIV, tuberculosis, and malaria in low-income and middle-income countries: a modelling study. Lancet Glob. Health 8, e1132–e1141. https://doi.org/10.1016/s2214-109x(20)30288-6 (2020).
Prabhu, S. R. et al. Malaria epidemiology and COVID-19 pandemic: are they interrelated? Omics: J. Integr. Biol. 26, 179–188. https://doi.org/10.1089/omi.2021.0227 (2022).
De Salazar, P. M. et al. Severe outcomes of malaria in children under time-varying exposure. Nat. Commun. 15, 4069. https://doi.org/10.1038/s41467-024-48191-7 (2024).
Organization, W. H. Considerations for Implementing Mass Treatment, Active case-finding and population-based Surveys for Neglected Tropical Diseases in the Context of the COVID-19 Pandemic: Interim Guidance (World Health Organization, 2020).
Markwalter, C. F. et al. Plasmodium falciparum infection in humans and mosquitoes influence natural anopheline biting behavior and transmission. Nat. Commun. 15, 4626. https://doi.org/10.1038/s41467-024-49080-9 (2024).
Bundy, D. A. P. et al. A positive consequence of the COVID-19 pandemic: how the counterfactual experience of school closures is accelerating a multisectoral response to the treatment of neglected tropical diseases. Philos. Trans. R. Soc. Lond. B Biol. Sci. 378, 20220282. https://doi.org/10.1098/rstb.2022.0282 (2023).
World Health Organization. New malaria vaccines: A breakthrough in the fight against malaria. WHO News, 53 (2021).
Organization, W. H. World malaria report 2022. Geneva: World Health Organ. (2022).
Organization, W. H. WHO guidelines for malaria. (2023).
Toor, J. et al. Predicted impact of COVID-19 on neglected tropical disease programs and the opportunity for innovation. Clin. Infect. Dis. 72, 1463–1466. https://doi.org/10.1093/cid/ciaa933 (2021).
Zarandi, M. B. et al. Pandemic COVID-19 and endemic neglected tropical diseases: friends or foes? Zoonoses 3, 20230024 (2023).
World Health Organization. Malaria vaccines: A global disparity in the fight against malaria. Glob. Health 8(2), 15–20 (2022).
Gao, L. et al. Impact of the COVID-19 pandemic on malaria control in Africa: A preliminary snalysis. Trop. Med. Infect. Dis. 8. https://doi.org/10.3390/tropicalmed8010067 (2023).
Acknowledgements
The authors thank the Institute for Health Metrics and Evaluation for providing the data for this study.
Funding
This study was supported by National Natural Science Foundation of China (No. 82300652).
Author information
Authors and Affiliations
Contributions
JFH, WW and SL conceived and designed the study. JFH, YKH, YLW, LP and MFW collected and analyzed data. JFH and YKH prepared the first version of the manuscript. YLW, LP, MFW, WW and SL provided critical comments on the revision of the manuscript. WW and SL revised and finalized the manuscript. All authors approved the submission of the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Huang, J., Hu, Y., Wu, Y. et al. Global burden of malaria before and after the COVID-19 pandemic based on the global burden of disease study 2021. Sci Rep 15, 9113 (2025). https://doi.org/10.1038/s41598-025-93487-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-93487-3
Keywords
This article is cited by
-
Synthesis of qualitative evidence on community experiences and perceptions of Plasmodium knowlesi malaria and factors influencing prevention and healthcare-seeking behaviours in Malaysia
Malaria Journal (2026)
-
A five-year (2020–2024) malaria surveillance data analysis of Mattu Karl Specialized Comprehensive Hospital, Oromia region, Southwest Ethiopia
Malaria Journal (2026)
-
Impact of the COVID-19 pandemic on malaria transmission in the state of Pará, Brazil
Malaria Journal (2025)