Abstract
Objectives: Rhabdomyolysis is characterized by muscle breakdown and the release of myocyte contents into the bloodstream, which can lead to severe complications. Elevated troponin levels, typically a marker of heart muscle injury, have been observed in rhabdomyolysis, but their clinical significance in this context remains unclear. This study aimed to evaluate the association between elevated troponin levels and mortality in patients with rhabdomyolysis, specifically those with normal kidney function and left ventricular function. Methods: This single-centre, retrospective study was conducted at a tertiary university medical centre from 2010 to 2022. The study included 252 patients diagnosed with rhabdomyolysis, defined by a creatine phosphokinase (CPK) level at least five times the upper normal limit. Patients were stratified into troponin-positive and troponin-negative groups. Only patients with an estimated glomerular filtration rate (eGFR) above 90 ml/min and normal left ventricular function were included. The primary outcome was 90-day survival, with secondary outcomes including 30-day survival and in-hospital mortality. Results: Patients with elevated troponin levels had significantly higher 90-day mortality rates, longer hospital stays, and were older with more comorbidities compared to the troponin-negative group. These patients had worse outcomes despite lower CPK levels in the troponin-positive group. The receiver operating characteristic (ROC) analysis showed a limited predictive value for CPK levels for troponin positivity. Conclusions: Elevated troponin levels in rhabdomyolysis, particularly in older patients, are associated with increased mortality, independent of kidney and left ventricular function. This suggests the need for heightened monitoring and potentially more aggressive management of these patients.
Similar content being viewed by others
Introduction
Rhabdomyolysis is characterised by the breakdown of muscle tissue, which releases myocyte contents, including myoglobin, an oxygen-storage protein, into the bloodstream. Trauma, muscle overexertion, medications and toxins, genetic conditions, infection, and inflammation may cause it1. Symptoms include muscle pain, weakness, and dark urine; there can be severe complications such as kidney failure and cardiac arrhythmias. The diagnosis is typically based on findings of elevated blood levels of creatine phosphokinase (CPK) and myoglobin and elevated urine myoglobin levels, which can lead to acute kidney injury and an electrolyte imbalance2.
Troponin is a protein expressed by muscle tissue, mainly cardiac and skeletal, that plays a crucial role in muscle contraction. Blood levels of specific cardiac subtypes troponin I (cTnI) and troponin T (cTnT) are highly sensitive and specific markers for heart muscle damage or injury, such as myocardial infarction (MI)3,4. Both cTnI and cTnT have unique amino acid sequences compared to skeletal muscle troponins, enabling the development of highly specific immunoassays for their detection. While both are highly specific to cardiac muscle, there are differences in their clinical application. Unlike cTnI, which has multiple proprietary assays leading to variability in reported values, cTnT is exclusively measured using a standardized assay from a single manufacturer (Roche), ensuring consistency in reference ranges and measurement5.
Cardiac troponin T (cTnT) is a highly sensitive and specific biomarker for myocardial injury, primarily used in diagnosing acute myocardial infarction6. However, elevated cTnT levels can occur in various conditions beyond acute coronary syndromes, including both cardiovascular and non-cardiovascular diseases7. Interestingly, elevated cTnT levels have been observed in patients with neuromuscular disorders, such as Pompe disease and amyotrophic lateral sclerosis (ALS), without evidence of acute myocardial injury8,9. In these cases, the elevated cTnT is likely associated with skeletal muscle damage rather than cardiac injury. This finding highlights the importance of cautious interpretation of cTnT levels in patients with neuromuscular disorders to avoid unnecessary cardiac interventions9.
Several studies have shown that rhabdomyolysis may also be associated with elevated troponin levels in various mechanisms, including subendocardial injury, toxic injury, and a response to hemodynamic compromise. However, the exact mechanism remains unknown10,11,12. Those studies are 20 years old, with several methodological issues, not addressing other causes that can elevate troponin levels, such as myocardial injury history or kidney failure13.
The most recent studies included mainly case reports of elevated troponin levels among patients with infectious etiology or due to heat stroke14,15.
The present study aimed to determine if elevated troponin levels are associated with lower survival in patients with rhabdomyolysis and normal kidney and left ventricular function.
Methods
Study design settings
This single-centre, retrospective study was conducted in the emergency department of a tertiary university medical centre from 2010 to 2022. The study cohort included all patients diagnosed with rhabdomyolysis, defined by a creatine phosphokinase (CPK) level at least 5 times the upper normal limit. The patients were stratified into two groups based on their troponin levels: one group with positive troponin results and the other with negative troponin results.
Inclusion criteria:
-
Patients diagnosed with rhabdomyolysis, defined as a creatine phosphokinase (CPK) level ≥ 5 times the upper normal limit.
-
Patients with an estimated glomerular filtration rate (eGFR) ≥ 90 ml/min, indicative of normal kidney function.
-
Patients with confirmed good left ventricular (LV) function (LVEF ≥ 55%) based on transthoracic echocardiography for troponin-positive cases or when clinically indicated for troponin-negative cases.
-
Patients admitted between 2010 and 2022 at the study centre.
Exclusion criteria:
-
Patients with an eGFR < 90 ml/min, indicative of chronic kidney disease or acute kidney injury.
-
Patients with documented reduced LV function (LVEF < 55%) on transthoracic echocardiography.
-
Patients with other known causes of elevated troponin, such as sepsis, acute coronary syndromes, myocarditis, or pulmonary embolism or chronic elevation of troponin.
-
Patients with incomplete medical records, missing data regarding key variables, or unavailable CPK or troponin measurements at admission.
-
Patients under the age of 18 years.
Transthoracic echocardiography (TTE)
TTE was performed routinely for patients with elevated troponin levels at the time of admission to assess left ventricular (LV) function. Good LV function was defined as a left ventricular ejection fraction (LVEF) ≥ 55% for these patients, calculated using the modified biplane Simpson’s method. Patients with normal troponin levels did not routinely undergo TTE; echocardiography was performed only when clinically indicated based on their symptoms or medical history.
Estimated glomerular filtration rate (eGFR)
eGFR was calculated using the Cockcroft-Gault equation, which accounts for a patient’s age, weight, sex, and serum creatinine levels to estimate kidney function.
The eGFR cutoff of ≥ 90 mL/min was selected to ensure that troponin elevation was not influenced by impaired renal clearance, as chronic kidney disease is an independent cause of troponin elevation.
Troponin assay
Cardiac troponin T (cTnT) was measured exclusively in our laboratory using a high-sensitivity immunoassay. This assay is known for its high sensitivity and specificity in detecting myocardial injury, with minimal cross-reactivity with non-cardiac tissue. The lower limit of detection for cTnT was 13 ng/L, with a 99th percentile cutoff value of 14 ng/L, as recommended by international guidelines. The use of cTnT allowed for consistent and reliable differentiation between cardiac and non-cardiac causes of elevated troponin levels.
Throughout the study period (2010–2022), no significant changes in assay protocols or thresholds for positivity occurred, ensuring consistency in troponin measurement and interpretation.
Measurements and data collection
The following data were collected:1 demographics and medical history (i.e., age, gender, background diseases, and smoking status)2, Laboratory data (levels of CPK, troponin, creatinine, urea, white blood cell count, platelet count, and haemoglobin and albumin levels)3, Charlson Comorbidity Index (CCI).
Data were collected from the electronic patient records, including Chameleon™ (Elad Group, Israel).
Outcome measures
The primary outcome measure was 90-day survival after admission. Secondary outcomes were 30-day survival and in-hospital mortality.
Ethics and administrative approval
Ethical approval for this study was obtained from the Institutional Review Board of Rabin Medical Centre (RMC-0436-22). The Beilinson Helsinki Review Board waived the requirement for informed consent due to the study’s retrospective nature. We confirm that all experiments were performed in accordance with relevant guidelines and regulations.
Statistical analysis
Descriptive statistics were used to summarise the data. The distribution of variables was visually assessed using histograms and QQ plots. Normally distributed numerical variables were presented as means ± standard deviation (SD); non-normally distributed variables were presented as medians [25th to 75th percentiles]. Categorical variables were presented as frequency and percentages (%).
Receiver operating characteristic (ROC) analysis was performed to investigate the value of CPK in predicting troponin-positive patients with rhabdomyolysis, and the area under the curve (AUC) was calculated. The relationship between CPK and troponin values was visualised using a scatter plot. The odds ratio (OR) and confidence interval (CI) were computed to measure the association between troponin level and mortality.
Logistic regression was initially performed to assess the association between troponin levels and mortality, both independently and after adjusting for age and the Charlson Comorbidity Index (CCI). However, alternative methods were employed due to the occurrence of perfect separation, which prevented the logistic regression models from converging.
A Random Forest classifier was used to evaluate the relative importance of troponin levels, age, and CCI in predicting mortality.
Data was generated with SPSS, version 25.0. A p-value of < 0.05 was considered significant.
Results
The cohort included 252 patients with rhabdomyolysis, of which 152 had positive and 100 had negative troponin levels. Among those with negative troponin levels, the proportion of men was significantly higher than that of women (85% vs. 60%, P < 0.001). The troponin-positive group had higher rates of diabetes mellitus (27.6% vs. 7% vs. P < 0.0001) and cerebrovascular attacks (19.7% vs. 3% P < 0.0001) compared to the troponin-negative group. The troponin-negative group had fewer cases of past MI compared to the troponin-positive group (4% vs. 16%, P < 0.01) (Table 1). Additionally, the troponin-positive group had a significantly higher mean age (68.94 ± 18.73 vs. 38.66 ± 16.19 years, P < 0.001) and a higher mean Charlson Comorbidity Index (CCI) score (3.94 ± 2.31 vs. 0.77 ± 1.43, P < 0.001) than the troponin-negative group. Excessive exercise for rhabdomyolysis etiology was more common in the troponin negative than the roponin positive group (58(58%) vs. 49(32%), p < 0.001). Table 1.
On analysis of laboratory values, the positive-troponin group had higher mean levels of urea (52.72 ± 34.33 vs. 26.37 ± 10.89, P < 0.0001) and white blood cell (9.18 ± 2.58 vs. 7.54 ± 2.81 P < 0.0001) and lower mean albumin (3.57 ± 0.5 vs. 4.18 ± 0.39 P < 0.0001) and haemoglobin (12.15 ± 1.65 vs. 13.81 ± 1.43 P < 0.0001)—Table 2.
Initial and maximal median CPK levels were significantly higher in the troponin-negative group [6346 (3017–15420) vs. 3623 (1635–7267) P < 0.001 and 6628 (3143–15758) vs. 4411 (1932–9692) P < 0.01 respectively].
The primary outcome, the 90-day mortality rate, was significantly higher in the positive-troponin group (5.28% vs. 0, p = 0.001) (primary outcome). Secondary outcomes, including in-hospital mortality and 30-day mortality rate, were higher among the positive troponin group (3.29% vs. 0, P < 0.001 and 3.95% vs. 0 p < 0.001, respectively). The median hospital duration was significantly extended among the positive troponin group with 43,4,5 vs. 64,5,6,7,8,9,10, P < 0.001. Table 3.
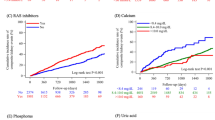
On ROC analysis using CPK of 7787 mg/dl as the cutoff, CPK had a specificity of 66% and sensitivity of 75% for predicting patients with troponin-positive rhabdomyolysis; the AUC was 0.63. (Fig. 1). Calculating the log of the first CPK value in predicting the log of the first troponin value yielded no direct correlation (r = 0.04, p = 0.78; Fig. 2).
Receiver operating characteristic (ROC) curve of CPK levels predicting troponin-positive rhabdomyolysis patients. The ROC analysis evaluated the effectiveness of Creatine Phosphokinase (CPK) levels in predicting troponin positivity among rhabdomyolysis patients. With a CPK cutoff value of 7,787 mg/dL, the test achieved a sensitivity of 75% and a specificity of 66%. The area under the curve (AUC) was calculated to be 0.63, indicating a modest predictive capability.
Scatter plot illustrating the relationship between log-transformed initial CPK and troponin levels. A scatter plot was constructed to visualise the correlation between the logarithmically transformed initial CPK values and initial troponin levels in the cohort. The analysis revealed no significant correlation between these two variables, with a correlation coefficient (r) of 0.04 and a p-value of 0.78, suggesting that CPK levels are not a reliable predictor of troponin levels in this context.
The OR for mortality at 90 days was also calculated for each parameter, including log-transformed troponin, log-transformed CPK, age, and gender. For log-transformed troponin, while the confidence interval crossed 1, the first positive troponin value at admission showed a trend toward an association with higher mortality (OR 1.78, CI 0.92–3.4) (Fig. 3).A Random Forest classifier was utilised to evaluate the relative contributions of log-transformed troponin levels, age, and the Charlson Comorbidity Index (CCI) in predicting mortality. The model achieved perfect classification accuracy (100%) on the test set, demonstrating the strong predictive relationships between these variables and mortality.
Odds ratios (OR) for 90-day mortality based on various clinical parameters. A forest plot was generated to display the odds ratios for 90-day mortality associated with different clinical parameters among the study participants. Notably, an elevated troponin level at admission was associated with higher odds of mortality (OR 1.78); however, the 95% confidence interval (CI 0.92–3.4) crossed 1, indicating this finding was not statistically significant. Other parameters were also analysed, but none were significantly associated with 90-day mortality.
Feature importance analysis revealed that log-transformed troponin levels emerged as a critical predictor of mortality, with an importance score of 0.345. The CCI, representing the cumulative burden of comorbidities, held the highest importance score (0.368), slightly exceeding that of troponin levels. Age contributed to the model with a relative importance score of 0.287.
Discussion
The present study highlights the prognostic significance of elevated troponin levels in patients with rhabdomyolysis. Elevated troponin levels were strongly associated with higher mortality, reflecting the critical role of myocardial injury as a determinant of outcomes in this cohort. While the analysis of raw troponin levels demonstrated a statistically significant association with mortality, the log-transformed troponin levels showed only a trend toward significance (OR 1.78, CI 0.92–3.4). This discrepancy underscores the importance of considering both raw and transformed data in statistical modelling to capture clinically relevant patterns and address variability. The confidence interval crossing 1 in the log-transformed analysis highlights the limitation of our sample size, which may have reduced the power to detect a significant association. Nevertheless, the consistent trend observed in both raw and log-transformed analyses reinforces the clinical relevance of troponin as a marker of poor prognosis.
Confounding factors, such as advanced age and a greater prevalence of comorbidities in the troponin-positive group, likely influenced these findings. Adjusted analyses for these variables were attempted, but the issue of perfect separation in logistic regression precluded conclusive results. Alternative methods, including Random Forest models, confirmed the prognostic value of troponin alongside age and the Charlson Comorbidity Index (CCI). However, while insightful, these methods lack the inferential clarity of traditional regression techniques.
While patients with troponin elevation had significantly higher comorbidity burdens, feature importance analysis demonstrated that troponin levels remained a strong independent predictor of mortality. This suggests that troponin is more than just a bystander marker and may reflect underlying myocardial stress or Type 2 myocardial infarction, contributing directly to worse outcomes.
To minimise selection bias, only patients with an eGFR of over 90 ml/min and good left ventricular function were included. Notably, patients with elevated troponin levels were older and had more comorbidities despite having lower CPK levels, while patients with higher CPK levels tended to be younger and troponin-negative.
The precise mechanism accounting for the elevation of the serum cTnI in diseases other than acute coronary syndromes remains to be elucidated. Still, several potential mechanisms exist when reviewing the literature: A proposed mechanism involves subendocardial injury, which is caused by increased wall stress, which occurs in patients with hypertension or left ventricular hypertrophy16,17.
Another potential mechanism involves toxic injury to the heart, which is observed in critically ill patients in response to endogenous substances released during sepsis18. Lastly, a proposed mechanism that was described involved trauma, which could be cardioversion, implantable cardioverter defibrillator discharges or heart infections19,20 .
The findings of this study demonstrate the prognostic significance of elevated troponin levels in patients with rhabdomyolysis who have normal kidney and cardiac function. By refining the study population to exclude confounding factors such as impaired renal function or left ventricular dysfunction, this research builds upon and diverges from prior investigations, which often lacked similar controls. Punukollu et al.21 examined the prevalence and clinical implications of elevated serum cardiac troponin I in patients with rhabdomyolysis, including those with varied renal and cardiac health. Our study, by contrast, focused on individuals with normal kidney function (eGFR ≥ 90 ml/min) and preserved left ventricular function (LVEF ≥ 55%), eliminating key confounders to isolate troponin elevation as an independent prognostic factor. Similarly, Viallon et al.22 investigated elderly patients (≥ 70 years) with rhabdomyolysis, excluding those with acute coronary syndrome or pulmonary embolism. Their prospective study grouped patients by troponin I levels (≥ 0.15 ng/mL vs. < 0.15 ng/mL) and found a non-significant trend towards higher six-month mortality in troponin-positive patients (23% vs. 8%, p = 0.07). While both studies share an emphasis on specific subgroups, our inclusion of a broader age range and stricter renal and cardiac function criteria offers a more nuanced assessment of troponin’s role as a prognostic marker.
The patient population in our study differs markedly from prior research in terms of age, comorbidities, and troponin positivity. Punukollu et al.’s cohort had a mean age of 57.8 years, whereas our troponin-positive group averaged 68.9 years, reflecting greater systemic stress and comorbidity burdens, such as higher rates of diabetes mellitus (27.6% vs. 10%) and cerebrovascular accidents (19.7% vs. not reported). Viallon et al.’s study focused exclusively on older adults (mean age 81 years), further narrowing the cohort to a distinct, high-risk demographic.
Both studies acknowledge the multifactorial etiology of troponin elevation in rhabdomyolysis. Punukollu et al. proposed mechanisms such as subendocardial injury due to increased wall stress, toxic injury in critically ill patients, and hemodynamic compromise. Viallon et al. noted a lack of correlation between troponin and CPK levels and suggested possible mechanisms, including hypoperfusion and oxidative stress, without evident ischemia. Our findings align with these hypotheses but extend the discussion by proposing Type 2 myocardial infarction (MI) as a plausible mechanism.
The clinical outcomes across studies highlight both similarities and divergences. Punukollu et al. found elevated troponin levels associated with higher ICU admission rates and longer hospital stays but reported no significant mortality differences. Viallon et al. observed a trend toward increased six-month mortality in troponin-positive elderly patients, although the difference was not statistically significant (23% vs. 8%, p = 0.07). Our study, however, demonstrated a significantly higher 90-day mortality rate in troponin-positive patients (5.28% vs. 0%, p < 0.001). Additionally, our troponin-positive group experienced extended hospital stays (6 vs. 4 days, p < 0.001), emphasising troponin’s utility as a prognostic biomarker and its potential influence on care strategies.
CPK levels poorly correlated with troponin levels in our cohort, with 66% specificity and 75% sensitivity for a CPK of 7787 mg/dlThe lack of correlation between CPK and troponin levels in rhabdomyolysis reflects their distinct biological origins and mechanisms. CPK is a marker of skeletal muscle damage, while troponin specifically indicates myocardial injury. Previous studies23,24,25 have shown that troponin elevation in rhabdomyolysis is often driven by systemic or cardiac stress, such as subendocardial injury caused by hemodynamic instability, toxic effects from critical illness, or myocardial oxygen imbalance (Type 2 MI). Additionally, differences in the timing of sample collection may contribute to the observed inverse relationship, as CPK and troponin levels follow different kinetics: CPK peaks later and declines more slowly, while troponin levels may rise and normalise earlier in the disease course. This highlights the importance of considering temporal factors when interpreting these biomarkers26.
The inverse relationship between these biomarkers may also stem from differing aetiologies of rhabdomyolysis. Troponin-positive patients are often older with more comorbidities, reflecting cardiac stress, whereas younger, healthier patients may exhibit higher CPK levels due to primary skeletal muscle injury and potentially greater overall muscle mass. For instance, previous studies have reported weak or no correlation between CPK and troponin levels (r = -0.08), further supporting the notion that these biomarkers reflect independent pathophysiological processes21,27.
These findings emphasise the need to interpret CPK and troponin levels independently in rhabdomyolysis, as troponin elevation may signify systemic stress or cardiac injury rather than the severity of skeletal muscle damage. Considering both timing and the underlying aetiology of rhabdomyolysis is essential for a comprehensive understanding of these biomarkers. Excessive exercise as a cause of rhabdomyolysis was more common in the negative troponin group. However, we assume that this is related to the higher prevalence of excessive exercise in younger age groups, which have a higher incidence of negative troponin, rather than to the etiology itself.
Consistent with prior literature, our findings show that higher troponin levels were predominantly observed in older patients within our cohort. A prospective descriptive study of patients over 70 with rhabdomyolysis similarly compared clinical, laboratory, and treatment variables based on troponin levels (> 0.15 vs. 0–0.15 ng/mL) and found that elevated troponin was associated with higher mortality at six months. Importantly, this study excluded patients with acute coronary syndrome and pulmonary embolism and found no correlation between serum cTnI and creatine kinase levels22. Consistent with these results, our study also found no correlation between CPK and troponin levels, and we observed significantly higher mortality in patients with elevated serum troponin.
Literature suggests that elevated troponin levels in rhabdomyolysis are often attributed to acute kidney injury28,29,30 or co-existent myocarditis or coronary ischemia31,32,33,34.
Our study—which excluded patients with abnormal kidney function or left ventricular dysfunction—supports an alternative hypothesis. We propose that elevated troponin in rhabdomyolysis may indicate Type 2 MI, characterised by an imbalance between myocardial oxygen supply and demand without plaque rupture35,36,37.
This mechanism aligns with other stress-related conditions, such as sepsis or respiratory failure, irrespective of CPK levels.
Strengths
This study has several key strengths. First, it focuses on a well-defined cohort of patients with normal kidney and left ventricular function, minimising potential confounding from these common variables. By excluding patients with abnormal renal or cardiac function, the study provides a clearer assessment of the relationship between troponin levels and mortality in rhabdomyolysis. Second, the use of multiple analytical approaches, including Random Forest models, allowed for a comprehensive evaluation of predictors such as troponin levels, the Charlson Comorbidity Index (CCI), and age, highlighting the clinical importance of these variables. Finally, the study contributes to a growing body of evidence by proposing a novel hypothesis regarding Type 2 MI as a potential mechanism for troponin elevation in rhabdomyolysis.
Limitations
This retrospective study is inherently subject to selection and information biases. The reliance on electronic medical records may have resulted in incomplete data capture. Conducted at a single tertiary medical centre, the findings may not be generalisable to broader populations. Furthermore, including only patients who underwent echocardiography at admission may have led to selection bias, potentially overrepresenting specific subgroups. While we restricted the study to patients with normal kidney and left ventricular function to minimise confounding, unmeasured variables such as comorbidities, medications, or in-hospital interventions may have influenced outcomes.
The study’s observational nature also precludes causal inferences. Elevated troponin levels in rhabdomyolysis may be a marker of severity or an independent risk factor, but the directionality remains unclear. Additionally, the small sample size limited the ability to conduct robust multivariable modelling and contributed to perfect separation, which constrained the use of logistic regression. Alternative methods, such as Random Forest models, provided insights into the relative contributions of troponin, CCI, and age but lacked the inferential clarity of traditional regression methods. Despite these limitations, the consistent trends observed reinforce the clinical importance of troponin as a predictor of mortality in rhabdomyolysis.
While our findings highlight an association between troponin elevation and increased mortality in rhabdomyolysis, the precise causes of death were often multifactorial. Many patients had significant comorbidities, including cardiovascular disease and sepsis, which could have contributed to mortality independent of rhabdomyolysis. Future studies with more detailed cause-of-death assessments are warranted to further elucidate these relationships.
This study underscores the need for larger, prospective studies to validate these findings, refine predictive models, and explore the underlying mechanisms driving troponin elevation in rhabdomyolysis.
Conclusions
Troponin elevation is a complication of rhabdomyolysis, especially in older patients. It is associated with an increased risk of mortality, regardless of LV and kidney function. These results underscore the importance of monitoring troponin levels in patients with rhabdomyolysis as part of their risk stratification. Elevated troponin levels should prompt clinicians to consider more intensive monitoring and possibly more aggressive management strategies to mitigate the higher mortality risk associated with this biomarker in rhabdomyolysis patients. Further research is needed to elucidate the exact mechanisms by which elevated troponin levels contribute to increased mortality and to develop targeted interventions for this high-risk patient population.
Data availability
The datasets used and or analysed during the current study available from the corresponding author on reasonable request.
References
Sauret, J. M., Marinides, G. & Wang, G. K. Rhabdomyolysis. Am. Fam. Phys. 65(5), 907–913 (2002).
Long, B., Koyfman, A. & Gottlieb, M. An evidence-based narrative review of the emergency department evaluation and management of rhabdomyolysis. Am. J. Emerg. Med. 37 (3), 518–523 (2019).
Muthu, V., Kozman, H., Liu, K., Smulyan, H. & Villarreal, D. Cardiac troponins: bench to bedside interpretation in cardiac disease. Am. J. Med. Sci. 347 (4), 331–337 (2014).
Apple, F. S. et al. Single High-Sensitivity Point-of-Care Whole-Blood cardiac troponin I measurement to rule out acute myocardial infarction at low risk. Circulation 146 (25), 1918–1929 (2022).
Cardiac Troponin. What’s the difference between T and I? (Division of LGM, 2015).
Mair, J. et al. How is cardiac troponin released from injured myocardium? Eur. Heart Journal: Acute Cardiovasc. Care. 7 (6), 553–560 (2018).
De Gennaro, L. et al. Increased troponin levels in nonischemic cardiac conditions and noncardiac diseases. J. Interven Cardiol. 21 (2), 129–139 (2008).
Castro-Gomez, S. et al. Teaching an old dog new tricks: serum troponin T as a biomarker in amyotrophic lateral sclerosis. Brain Commun. 3 (4), fcab274 (2021).
Wens, S. C. A. et al. Elevated plasma cardiac troponin T levels caused by skeletal muscle damage in Pompe disease. Circ. Cardiovasc. Genet. 9(1), 6–13 (2016).
Petejova, N. & Martinek, A. Acute kidney injury due to rhabdomyolysis and renal replacement therapy: a critical review. Crit. Care. 18 (3), 1–8 (2014).
Hausfater, P. et al. Elevation of cardiac troponin I during non-exertional heat-related illnesses in the context of a heatwave. Crit. Care. 14, 1–9 (2010).
Hall, T. S. et al. Cardiac troponin I for prediction of clinical outcomes and cardiac function through 3-month follow-up after primary percutaneous coronary intervention for ST-segment elevation myocardial infarction. Am. Heart J. 169 (2), 257–265 (2015). e1.
Chauin, A. The main causes and mechanisms of increase in cardiac troponin concentrations Other Than acute myocardial infarction (Part 1): physical exertion, inflammatory heart disease, pulmonary embolism, renal failure, sepsis. Vasc. Health Risk Manag. 601–617 (2021).
Rausa, J., Shetty, I. & Loomba, R. S. Troponin elevation in the setting of exercise-induced rhabdomyolysis in an athletic teenager. Cardiol. Young. 29 (12), 1552–1555 (2019).
Ali, L. et al. Acute myocardial injury and rhabdomyolysis in COVID-19 patients: incidence and mortality. Cureus 13 (10), e18899 (2021).
Sreekumar, A., Sahu, A. K., Aggarwal, P., Nayer, J. & Narang, R. Assessment of troponin I levels as a predictor of mortality in acute decompensated heart failure. Cureus [Internet]. https://www.cureus.com/articles/205162-assessment-of-troponin-i-levels-as-a-predictor-of-mortality-in-acute-decompensated-heart-failure. Accessed 3 Jan 2025.
Hernández-domínguez, L. Cardiac troponin I in patients with chronic kidney disease stage 3 to 5 in conditions other than acute coronary syndrome. Clin. Lab. [Internet]. (2014). http://www.clin-lab-publications.com/article/1388. Accessed 3 Jan 2025.
Spies, C. et al. Serum cardiac troponin T as a prognostic marker in early sepsis. Chest 113 (4), 1055–1063 (1998).
Zheng, P. et al. Cardiac troponin as a prognosticator of mortality in patients with sepsis: A systematic review and meta-analysis. Immun. Inflam Disease. 11 (9), e1014 (2023).
Cemin, R., Rauhe, W., Marini, M., Pescoller, F. & Pitscheider, W. Serum troponin I level after external electrical direct current synchronized cardioversion in patients with normal or reduced ejection fraction: no evidence of myocytes injury. Clin. Cardiol. 28 (10), 467–470 (2005).
Punukollu, G. et al. Elevated serum cardiac troponin I in rhabdomyolysis. Int. J. Cardiol. 96 (1), 35–40 (2004).
Viallon, A. et al. Troponin I values during rhabdomyolysis in elderly patients admitted to the emergency department. Presse Med. 35 (11 Pt 1), 1632–1638 (2006).
Wu, C. et al. Causes of troponin elevation and associated mortality in young patients. Am. J. Med. 131 (3), 284–292e1 (2018).
Long, B., Long, D. A., Tannenbaum, L. & Koyfman, A. An emergency medicine approach to troponin elevation due to causes other than occlusion myocardial infarction. Am. J. Emerg. Med. 38 (5), 998–1006 (2020).
Egholm, G. & Pareek, M. Drug-Induced rhabdomyolysis with elevated cardiac troponin T. Case Rep. Med. 2015, 1–3 (2015).
Almarzooqi, F. et al. Resolved myositis, normal creatine kinase, and peaking cardiac troponin T. J. Appl. Lab. Med. 9 (4), 848–853 (2024).
Li, S. F., Zapata, J. & Tillem, E. The prevalence of false-positive cardiac troponin I in ED patients with rhabdomyolysis. Am. J. Emerg. Med. 23 (7), 860–863 (2005).
Bosch, X., Poch, E. & Grau, J. M. Rhabdomyolysis and acute kidney injury. N. Engl. J. Med. 361 (1), 62–72 (2009).
Młynarska, E., Krzemińska, J., Wronka, M., Franczyk, B. & Rysz, J. Rhabdomyolysis-induced AKI (RIAKI) including the role of COVID-19. Int. J. Mol. Sci. 23 (15), 8215 (2022).
Vangstad, M., Bjornaas, M. A. & Jacobsen, D. Rhabdomyolysis: a 10-year retrospective study of patients treated in a medical department. Eur. J. Emerg. Med. 26 (3), 199–204 (2019).
Finsterer, J. & Stöllberger, C. Where does troponin I derive from in rhabdomyolysis? Am. J. Emerg. Med. 4 (24), 509–510 (2006).
Min, M. K. et al. Russula subnigricans poisoning causes severe rhabdomyolysis that could be misdiagnosed as non-ST segment elevation myocardial infarction. Wilderness Environ. Med. 33 (3), 324–328 (2022).
Ayan, M. et al. Multiple admissions to the coronary care unit due to falsely elevated cardiac troponin. In Baylor University Medical Center Proceedings. 197–199 (Taylor & Francis, 2018).
Nguyen, J., Thachil, R., Vyas, N. & Marino, T. Falsely elevated Troponin: rare occurrence or future problem. J. Community Hosp. Intern. Med. Perspect. 6 (6), 32952 (2016).
Smilowitz, N. R. et al. Provoking conditions, management and outcomes of type 2 myocardial infarction and myocardial necrosis. Int. J. Cardiol. 218, 196–201 (2016).
Šerpytis, R. et al. Type 2 myocardial infarction and Long-Term mortality risk factors: A retrospective cohort study. Adv. Therapy. 40 (5), 2471–2480 (2023).
Cryer, L., Shannon, S. B., Van Amsterdam, M. & Leff, B. Costs for ‘hospital at home’patients were 19% lower, with equal or better outcomes compared to similar inpatients. Health Aff. 31 (6), 1237–1243 (2012).
Author information
Authors and Affiliations
Contributions
SS and SM wrote the manuscriptEY and EN statistics.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Naamany, E., Medeot, S., Edel, Y. et al. Elevated troponin levels in rhabdomyolysis as a predictor of mortality in patients with normal kidney and cardiac function. Sci Rep 15, 9575 (2025). https://doi.org/10.1038/s41598-025-94405-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-94405-3