Abstract
Colorectal cancer is one of the most common malignant tumors, and its drug resistance poses a huge challenge and a serious threat to people’s health. In previous studies, we have found that the combination of paclitaxel and BEZ235 has synergistic anti-colon cancer effects, particularly in drug-resistant colorectal cancer, demonstrating excellent anti-tumor effects. Therefore, this study aims to investigate the preparation of the nanoemulsification of paclitaxel and BEZ235 (NEs-PTX-BEZ235) and to explore the potential key parameters for its clinical translation. This study aims to provide a new therapeutic strategy for colorectal cancer, especially for drug-resistant colorectal cancer. The nanomaterials were prepared by low energy self-emulsification method, and analyzed by Malvern laser particle size analyzer. Cell drug uptake was observed under fluorescence microscope. CCK8, Western blot and flow cytometry were used to compare the anti-cancer effects and mechanisms of different experimental groups on ordinary and drug-resistant colon cancer cells. Human colon cancer primary cells were extracted to verify the anti-tumor effect of drugs. Finally, we found that NEs-PTX-BEZ235 significantly killed colon cancer cells, especially drug-resistant cells, and performed better than Nab-PTX. It may play a synergistic role in reducing drug resistance, inhibiting tumor stemness and inducing apoptosis of colon cancer cells by inhibiting drug resistance proteins.
Similar content being viewed by others
Introduction
PI3K/Akt/mTOR signaling pathway is thought to be closely related to multidrug resistance in human colon cancer. It was reported that blocking of PI3K/AKT signaling pathway could enhance drug sensitivity of HCT-116/L-OHP resistant cells and reverse Pgp-mediated multidrug resistance in human colon cancer1,7. Common PI3K/Akt/mTOR pathway inhibitors in the past include PI3K inhibitors Wortmannin and Alpelisib, Akt inhibitors Perifosine and Miltefosine, as well as mTOR inhibitors Rapamycin and Everollmus. BEZ235 is a newly discovered inhibitor of the PI3K/Akt/mTOR signaling pathway1, which is well tolerated and has significant potential as a new anti-tumor drug. On the other hand, BEZ235 has a weak ability to induce apoptosis, and can trigger cell protective autophagy to offset its anti-tumor effect, so the anti-tumor effect of single drug is not ideal2. Paclitaxel (PTX) is a diterpenoid alkaloid extracted from Taxus plants3, which can promote the apoptosis of tumor cells, inhibit the division and proliferation of tumor cells4, and will not produce cross-resistance with a variety of drugs, while it is effective against multi-drug-resistant tumors. It has been applied to the treatment of malignant tumors such as breast cancer, ovarian cancer and pancreatic cancer5,6.
Previously, we have shown that PTX and BEZ235 have synergistic inhibitory effects on the growth of colon cancer cells and their drug-resistant cells. However, the combination of nanoemulsion loaded with PTX and BEZ235 showed more significant anti-tumor effect7,8. On this basis, according to the existing optimal compatibility ratio of PTX and BEZ235, we designed a Nanoemulsification of paclitaxel and BEZ235 (NEs-PTX-BEZ235) with high efficacy, low toxicity and high patient compliance.
In this study, a low energy self-emulsification method was used to prepare a Nanoemulsification of paclitaxel and BEZ235. This emulsifier has uniform particle size distribution, stable properties, and can be fully absorbed by tumor cells. In vitro anti-tumor experiments show that this emulsifier has good effects of synergistically inhibiting tumor proliferation, promoting apoptosis, reducing tumor drug resistance and reversing tumor cell stemness, and provides a promising anti-tumor strategy for future clinical treatment of colon cancer, especially drug-resistant colon cancer.
Materials and methods
Materials
Oxaliplatin-resistant (HCT116-LOHP) and cisplatin-resistant (HT29-DDP) human colon cancer cell lines were purchased from Shanghai Aurora Technology Co., LTD. HCT116 and HT29 human colon cancer cell lines were purchased from Shanghai Fuxiang Biotechnology Co., Ltd. Cisplatin and oxaliplatin, used to maintain drug resistance in two colon cancers, were purchased from Sigma in the United States. BEZ235 and PTX were purchased from Selleck Chemical, USA. Oxaliplatin and cisplatin are dissolved in saline, and PTX and BEZ235 are stored in dimethyl sulfoxide. Sources of other reagents related to cell culture are as follows: DMEM medium (Invitgen, USA), 0.25% EDTA trypsin (Solarbio, Beijing, China), fetal bovine serum (Biolnd, Israel), penicillin–streptomycin mixture (Solarbio, Beijing, China), dimethyl sulfoxide (Solarbio, Beijing, China), PBS (Shengong, Shanghai, China). CCK-8 cell proliferation toxicity assay kit (Tong Ren Chemical Research Institute, Japan) for cell proliferation, Nile Red (Solarbio, Beijing, China), FITC-labeled anti-rabbit IgG (ABCAM, USA), cell cycle assay kit (purchased from Unitech Biotechnology, China). Western blotting detected the antibody, and its concentration was PI3K (1:1000, Abcam, USA), p-Akt (1:2000, Abcam, USA), CD44 (1:2000, Abcam, USA), CD133 (1:1000, Abcam, USA), respectively. USA), Pgp(1:1000, Cst, USA), ABCC1(1:1000, Cst, USA), β-actin (1:1000, Abcam, USA); Hanks Buffer, Type IV collagenase, Tween 20 and propylene glycol were all purchased from Beijing Solarbio, China, Capryol 90 (Gattefosse, France).
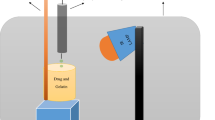
Synthesis of NEs-PTX-BEZ235
PTX and BEZ235 were dissolved in DMSO, and Tween 20 and propylene glycol were first mixed into the emulsifier by vortex shaking (with a volume ratio of Tween 20 to propylene glycol of 2:1, shaken for approximately 3–5 min); then the double drug (PTX and BEZ235 were added in different concentration ratios of 1:1, 1:2, 1:4, 1:8 and 1:10) was added with Capryol 90 was added to the emulsifier and vortex shaken for 5 min; finally, the above mixture was slowly added to double distilled water and whirlpool shaken for 5 min (volume ratio of Capryol 90, emulsifier and water was 20:40:40) to form the nano complex formulation. Nano complex formulation characterized by Transmission electron microscopy (TEM). The average particle size and stability of the nano complexed formulations (1:1 ~ 1:10) were examined by a Malvern laser particle size analyzer, and the prepared nano complexed formulations were stored at 4 °C.
CCK-8 cell viability determination
The four cell lines were cultured in DMEM medium containing 10% fetal bovine serum and 5% penicillin/streptomycin. The HT29DDP cell-resistant line and the HCT116-LOHP cell-resistant line were supplemented with cisplatin (1.5 μg/mL) and oxaliplatin (10 μg/mL), respectively, in the medium to maintain the corresponding resistant phenotypes of the two drug-resistant cells. Cells were inoculated on 96-well plates at a cell density of 4 × 103 cells/well. After 24 h, the original DMEM medium was removed and replaced with fresh DMEM medium containing different concentrations of BEZ235, PTX, PTX + BEZ235, NE-PTX, NE-PTX combined with BEZ235, NEs-PTX-BEZ235 (1:1, 1:2, 1:4, 1:8 and 1:10 groups) and albumin-paclitaxel (Nab-PTX), respectively. Among them, general cell lines were mixed with PTX or NE-PTX medium of different concentrations using 25 nm BEZ235. In contrast, drug-resistant cell lines were mixed with PTX or NE-PTX medium of different concentrations using 50 nm BEZ235 on 96-well plates. After 48 h of treatment, 10μL CCK-8 reagent was added to each well under light protection, and the 96-well plate was wrapped in aluminum foil and placed in the incubator. Two hours later, the absorbance OD value was measured at A450 nm using the BIO-RAD xMark microplate instrument, and the cell survival rate was calculated according to the following formula:
A combination index was calculated to determine the synergetic effect of combination treatment based on the following formula:
CI < 1, = 1 and > 1 indicated synergic, additive and antagonistic effect, respectively.
In vitro cellular uptake of drugs
NE-Nile red was prepared by encapsulating Nile red dye in nanoemulsion. Cells were seeded in 6-well plates at a cell density of 2 × 105cells/well. After 24 h, the original medium was removed and replaced by the medium containing NE-Nile red. After 0, 12, 24 and 48 h of incubation, the plates were washed with PBS, fixed with paraformaldehyde for 15 min, washed with PBS again, and incubated with DAPI for 15 min to stain the nuclei. Then the uptake of NE-Nile red by tumor cells was observed under a fluorescence microscope.
The expression of multidrug resistance, PI3K/Akt/mTOR pathway related molecules and dry protein were detected by Western blot.
The total protein was extracted after the cells were treated with different drugs for 48 h. The protein concentration was measured with a nanodrop spectrophotometer. Proteins were separated by Bio-RAD gel electrophoresis and transferred to PVDF membrane. After blocking for 2 H at room temperature (5% bovine serum albumin), the cells were incubated with rabbit anti-human Pgp, ABCC1, PI3K, p-AKt, CD133, CD44 and mouse anti-human β-actin antibodies overnight at 4 ℃, washed at room temperature, and treated with horseradish peroxidase-conjugated anti-rabbit and mouse antibodies for 2 H, then observed and imaged by ECL.
Note: After all antibody hybridization was completed, in order to obtain clearer and more visually appealing images, we cropped and photographed the imprinting blots. Original blots have been added to the supplementary materials.
Flow cytometry for cell cycle detection experiments
2 * 105 − 1 * 106cells were collected, washed once with PBS, and centrifuged to discard the supernatant. Precooled 80% ethanol at -20.degree. C. was added and fixed overnight. On the day of detection, the fixed cells were centrifuged, the supernatant was discarded, washed with PBS, added with 1 ml DNA Staining solution, vortexed for 5–10 s, and incubated for 30 min at room temperature in the dark. Detection was performed on a flow cytometer.
Colon cancer primary cell extraction
Primary cells were cultured by tissue block attachment method and collagenase digestion method. The fresh tissues of human colorectal cancer were collected and stored in the preservation solution (45 ml DMEM + 5 ml penicillin–streptomycin mixture). The tissues were taken out from the ultra-clean table, fat and necrotic tissues were removed, and washed with Hank’s solution. The washed tissues were cut into small pieces of 1mm3, washed with Hank’s solution again, and the supernatant was discarded. It was resuspended with preservation solution and evenly arranged at the bottom of the culture flask. After adding DMEM culture medium, the culture flask was placed with the bottom upward for 2–4 h. When there was cell growth around the tissue block, it was considered that the culture was successful. Collagenase digestion method: The tissue block was cut into small pieces of 1 mm3, washed with Hanks solution, added with type IV collagenase, and placed in a 37 °C water bath for 1 H until the tissue block was dispersed, and then the cell suspension was collected and filtered through a 200-mesh sterile cell filter. The liquid that passed through the screen was transferred to a flask that had been previously filled with DMEM medium. Cells were cultured for 2–3 weeks and then purified by trypsin digestion.
Statistical analysis
The data were analyzed by SPSS.20 statistical analysis software, and the results were presented in the form of mean ± standard deviation. The t-test was used to compare pairwise samples, and the analysis of variance was used to compare multiple samples. The difference was considered statistically significant at P < 0.05.
Results
Characterization of NEs-PTX-BEZ235
In this study, nanoemulsion was successfully synthesized by the oil-in-water method and characterized by Transmission electron microscopy (TEM) (Fig. 1A). The ratios of PTX to BEZ235 in the compound were set at 1:1, 1:2, 1:4, 1:8 and 1:10. The Malvern laser particle size analyzer examined the nanoparticle size, and the results showed that the particle size distribution of the nanoemulsion (NE) system was narrow, with an average particle size of 171.1 nm and a polydispersity index (PDI) of 0.142–0.202 (Fig. 1B). The particle size and PDI were similar in alkaline DMEM medium, neutral PBS and pH5.8 buffer. During the subsequent six days of continuous measurements (Fig. 1C), we found that the distribution and particle size of NEs-PTX-BEZ235 remained in the same range without significant changes, especially in the DMEM medium, indicating good stability of NEs-PTX-BEZ235.
Characterization of NEs-PTX-BEZ235. A. The synthesized NEs-PTX-BEZ235 was observed to be spherical with a smooth surface through TEM. B. The average particle size of 153.7 ± 2.16 nm. NEs-PTX-BEZ235 (1:1 ~ 1:10) has a narrow particle size distribution with a polydispersity index between 0.142 and 0.202, and has similar particle size and PDI in DMEM medium, PBS and pH 5.8 buffer; C. The particle size distribution of nanometer compound preparation (1:1 ~ 1:10) was measured for 6 consecutive days. It was found that the particle size did not change significantly in alkaline, neutral and acidic media, especially in alkaline DMEM medium.
In vitro cellular uptake of drugs
NE-Nile red was prepared by encapsulating Nile red dye in nanoemulsion. In colon cancer cells HT29, HCT116 and colon cancer drug-resistant cells HT29-DDP, HCT116-LOHP, the uptake of NE-Nile red by tumor cells at four time points of 0, 12, 24 and 48 h was observed (Fig. 2). The results showed that NE-Nile red was gradually absorbed and taken up by colon cancer cells and drug-resistant cells over time. It was almost completely absorbed into the cytoplasm of tumor cells at 48 H, indicating that there was a good uptake of NE by colon cancer cells.
Inhibitory effects on tumor cells of single drug group, double drug combination group, nano single drug group, NE-PTX combined with BEZ235 group, NEs-PTX-BEZ235 group and albumin-paclitaxel (Nab-PTX) group
Under the same drug concentration, the effect of the compound preparation 1:10 group was better than that of the other experimental groups, and its IC50 was 2.096 and 1.276 in HT29 and HCT116 cells, respectively (Fig. 3A, Table 1). 9.836 and 6.803 in the drug-resistant cell lines HT29-DDP and HCT116-LOHP, respectively (Fig. 3B, Table 1). The combination index (CI) of NEs-PTX-BEZ235 (1:10) was calculated (Table 2), demonstrating the synergistic effect of PTX and BEZ235 in the compound preparation.
CCK8 method was used to detect the effects of single drug group, nano single drug group, double drug combination group and NEs-PTX-BEZ235 group on the proliferation of tumor cells. A. The effect of different experimental groups on the proliferation of colon cancer cells HT29 and HCT116 was studied. The compound preparation 1:10 group had the best anti-cancer effect, and its IC50 was 2.096 and 1.276 in HT29 and HCT116 cells, respectively. B. The effect of different experimental groups on the proliferation of drug-resistant colon cancer cells HT29-DDP and HCT116-LOHP showed that the compound preparation 1:10 group had the best anti-cancer effect, and its IC50 in HT29-DDP and HCT116-LOHP cells were 9.836 and 6.803, respectively, * indicating P < 0.05. * * indicates P < 0.01.
NEs-PTX-BEZ235 can significantly reduce the expression of PI3K/Akt/mTOR pathway related proteins p-AKt and PI3K in colon cancer cells and drug-resistant cells
BEZ235 is an inhibitor of PI3K/Akt/mTOR signaling pathway, and blocking PI3K/AKT signaling pathway can enhance the drug sensitivity of drug-resistant human colon cancer cells1,9. In this study, Western blot was used to detect and compare the effects of different drug groups on the expression of PI3K and p-Akt in colon cancer cells and drug-resistant cells. As a result of detection in colon cancer cells HT29, HCT116, HT29-DDP, and HCT116-LOHP (Fig. 4A–B), The expressions of PI3K and p-Akt in the BEZ235 single drug group, PTX single drug group, PTX + BEZ235 group, NE-PTX group, NE-PTX combined with BEZ235 group and the NEs-PTX-BEZ235 groups with different double drug ratios are all down-regulated compared with the negative control group, and the down-regulation effect of the NEs-1: 10 group is the most obvious. The difference was statistically significant (P < 0.05), indicating that the inhibitory effect of NEs-1: 10 group was better than that of other experimental groups (Supplementary Table 1,2).
(A–B) Effects of different experimental groups on PI3K/Akt/mTOR pathway related proteins in tumor cells. * means P < 0.05, * * means P < 0.01. (C–D) Effects of different experimental groups on tumor cell stem Protein. * means P < 0.05, * * means P < 0.01. (E) Effects of different experimental groups on drug-resistant protein of colon cancer drug-resistant cells. * means P < 0.05, * * means P < 0.01.
NEs-PTX-BEZ235 preparation can significantly reduce the expression of CD44 and CD133 in colon cancer cells.
Within the tumor cell population, there are specific subsets known as cancer stem cells (CSCs) or tumor initiating cells (TICs)17,18. These cells have malignant biological potentials such as self-renewal, multi-directional differentiation, unlimited proliferation and tumor reconstruction, and are considered to be the root of tumorigenesis, progression, invasion and metastasis, chemoradiotherapy resistance and recurrence19,20. BEZ235 can inhibit the growth of colon cancer stem cells1,10. In order to further explore the possible mechanism of tumor inhibition by drugs, Western blot was used to detect and compare the effects of different drug groups on the expression of stemness related proteins CD133 and CD44 in colon cancer cells and drug-resistant cells. As a result, in the colon cancer cells HT29, HCT116, HT29-DDP, and HCT116-LOHP (Fig. 4C–D). Compared with the negative control group, the expressions of CD133 and CD44 in the BEZ235 single drug group, PTX single drug group, PTX combined with BEZ235 group, NE-PTX group, NE-PTX combined with BEZ235 group and NEs-PTX-BEZ235 groups with different double drug ratios were all down-regulated, and the down-regulation effect of the NEs-1: 10 group was the most obvious. The difference was statistically significant (P < 0.05), indicating that the inhibitory effect of NEs-1: 10 group was better than that of other experimental groups (Supplementary Table 3,4).
NEs-PTX-BEZ235 can significantly reduce the expression of Pgp and ABCC1 protein in drug-resistant cells.
Chemotherapy for colon cancer often leads to the mutation of some genes in the tumor, or stimulates normal cells to produce some chemical factors suitable for tumor growth, thus causing multidrug resistance11. ABCC1/MRP1 and ABCB1/Pgp are energy-dependent drug efflux pumps with an ATP-binding site and a drug-binding site. ATP can be hydrolyzed by binding to ABCC1 and Pgp to provide energy. This energy is used to pump out the drug entering the cell, resulting in the failure of the intracellular drug concentration to reach an effective level, thus causing drug resistance and leading to chemotherapy failure8,21. In order to explore the mechanism of PTX and BEZ235 on drug-resistant colon cancer cells, we compared the expression of P-glycoprotein (Pgp) and multidrug resistance-associated protein (ABCC1) in different treatment groups by Western blotting. It was found that in HT29DDP and HCT116-LOHP (Fig. 4E), Compared with the negative control group, the expressions of Pgp and ABCC1 in the BEZ235 single drug group, PTX single drug group, PTX combined with BEZ235 group, NE-PTX group, NE-PTX combined with BEZ235 group and NEs-PTX-BEZ235 groups with different double drug ratios are all down-regulated, and the down-regulation effect of the NEs-1: 10 group is the most obvious. The difference was statistically significant (P < 0.05), indicating that the inhibitory effect of NEs-1: 10 group was better than that of other experimental groups. (Supplementary Table 5).
Flow cytometry was used to analyze and compare the effects of different proportions of NEs-PTX-BEZ235 on the cell cycle of colon cancer cells and their drug-resistant cells.
In the flow cytometry results of colon cancer cells HT29 and HCT116 (Fig. 5A–B, Table 3) and colon cancer drug-resistant cells HT29-DDP (Figure) and HCT116-LOHP (Fig. 5C–D, Table 3), it was found that, compared with the untreated control group, NEs-PTX-BEZ235 groups could induce G2/M phase arrest of cells, thereby promoting apoptosis of tumor cells. Among them, the NEs-1: 10 group had the best apoptosis-promoting effect, and the difference was statistically significant (P < 0.05) (Fig. 5E), and the effect was better at high concentration, which also indicated that the induction of G2/M phase arrest by nano-compound drugs on colon cancer cells and their drug-resistant cells was concentration-dependent.
Flow cytometry was used to analyze and compare the effects of different proportions of NEs-PTX-BEZ235 on the cell cycle of tumor cells. In HT29 (A) and HCT116 (B), HT29-DDP (C) and HCT116-LOHP (D), different compound preparations could induce G2/M phase arrest of tumor cells, and the effect of NEs-1: 10 group was the most obvious. E. Comparison of the percentage of cells in G2/M phase after treatment between different administration groups, * and * * indicate P < 0.05 and P < 0.01, respectively, compared with the control group.
NEs-PTX-BEZ235 has significant inhibitory effect on primary colon cancer cells
The primary cells of colorectal cancer were extracted from human colorectal cancer specimens and purified by trypsin digestion after successful culture, and the extracted cells were tested by flow cytometry. The CCK-8 method was used to detect the primary colon cancer cells treated with the gradient concentration of NEs-PTX-BEZ235, and the results showed that in the primary colon cancer cells, after 48 h of drug administration, under the same drug concentration, the survival rate of tumor cells in the NEs-1:10 group decreased more significantly (Fig. 6). The IC50 values of PTX/BEZ235 nanocomposites (1:1, 1:2, 1:4, 1:8 and 1:10) were 5. 371 nM, 3.813 nM, 4.475 nM, 3.857 nM and 3. 471 nM, respectively.
The primary colon cancer cells were treated with different proportions of NEs-PTX-BEZ235 with gradient concentration, and the effects of different groups on the proliferation of primary colon cancer cells were detected and compared. (A) Extracted human colon cancer primary cells (100 ×); (B) The positive rate of CK20 was 90.5% by flow cytometry. The positive rate of CDX2 was 91.7% by flow cytometry. The IC50 of different proportions of NEs-PTX-BEZ235 on primary human colon cancer cells were 5.371 nM, 3.813 nM, 4.475 nM, 3.857 nM and 3.471 nM, respectively. * indicates P < 0.05, * * indicates P < 0.01.
Discussion
According to the NCCN Clinical Practice Guidelines in Oncology for Colon Cancer, 3rd Edition, 2024, the standard treatment for colon cancer primarily relies on surgical resection followed by postoperative chemotherapy. FOLFOX (fluorouracil, leucovorin, and oxaliplatin) and CapeOX (capecitabine and oxaliplatin) regimens are commonly used standard protocols in clinical practice. However, chemotherapy resistance remains a major challenge affecting patient prognosis and survival rates. Although paclitaxel (PTX) has demonstrated significant efficacy in multiple solid tumors12,13, its application in colon cancer is limited by issues such as low water solubility, high toxicity, and drug resistance14. Therefore, exploring novel drug delivery methods and combination therapy strategies to enhance the effectiveness of PTX in colon cancer treatment is an important direction of current research.
BEZ235, a dual inhibitor of the PI3K/Akt/mTOR signaling pathway, can downregulate the expression of ATP-binding cassette transporters (e.g., P-glycoprotein, Pgp), reverse Pgp-mediated multidrug resistance, and promote cell apoptosis. Reports indicate that BEZ235 can enhance the sensitivity of the colon cancer cell line HCT-116 to 5-fluorouracil (5-FU), inhibit the growth of colon cancer stem cells1,9, and is considered a novel target for the treatment of chemotherapy resistance15,16. Consequently, we hypothesized that BEZ235 and PTX may synergistically act on multiple targets in colon cancer cells, thereby reducing drug resistance and further promoting cell apoptosis. This hypothesis was also confirmed in our preliminary studies8.
Nanoemulsions (NEs) are stable, transparent, low-viscosity, uniform, and thermodynamically stable dispersion systems composed of oil, water, surfactants, and co-surfactants in specific proportions. They can increase the solubility of poorly soluble drugs, enhancing their stability and bioavailability22,23. In this study, NEs were used to deliver a combination of PTX and BEZ235, with the aim of overcoming PTX resistance and enhancing its antitumor activity. The research results demonstrate that this nanoemulsion formulation (NEs-PTX-BEZ235) exhibits superior antitumor effects in both colon cancer cell lines and their drug-resistant counterparts. By optimizing the drug concentration ratio (1:10), NEs-PTX-BEZ235 not only effectively reduced the IC50 value but also demonstrated significantly better efficacy than clinically commonly used nab-paclitaxel (Nab-PTX), suggesting potential advantages of this formulation in overcoming drug resistance.
Mechanism studies revealed that NEs-PTX-BEZ235 can enhance the sensitivity of colon cancer cells through multiple mechanisms. On the one hand, this combination formulation blocks the pro-proliferative and anti-apoptotic effects of the PI3K/Akt/mTOR signaling pathway in tumor cells by significantly inhibiting the expression of related proteins (PI3K and p-Akt) in this pathway. On the other hand, BEZ235 can downregulate the expression of drug resistance-related proteins ABCC1 and Pgp, thereby reducing drug efflux and increasing the intracellular accumulation of PTX. In addition, this study found that NEs-PTX-BEZ235 can induce G2/M phase arrest in colon cancer cells and promote cell apoptosis through a Caspase-8-dependent pathway. The synergistic effects of these mechanisms may be key reasons for the enhanced cytotoxicity and overcoming of drug resistance exhibited by this formulation in colon cancer cells. Compared with previous studies, this study further validates the potential of the nanoemulsion-loaded combination strategy of PTX and BEZ235 in the treatment of colon cancer.
Previous studies have shown that MEK inhibitors combined with PTX can enhance the killing effect on colon cancer cells. Building on this, the current study further optimized the delivery of PTX using nanoemulsion technology and combined it with the synergistic sensitizing effect of BEZ235, achieving stronger antitumor effects at lower doses. Compared with traditional PTX formulations, the advantages of NEs-PTX-BEZ235 lie in improved solubility and bioavailability of PTX, while also reducing systemic toxicity, offering a potentially better treatment option in clinical applications.
However, this study still has certain limitations. Firstly, it is primarily based on in vitro cell models and has not yet conducted in vivo animal experiments to verify its biodistribution, pharmacokinetic characteristics, and long-term safety. Secondly, although this study revealed that NEs-PTX-BEZ235 may function by inhibiting the PI3K/Akt/mTOR pathway, downregulating drug resistance proteins, and promoting cell apoptosis, other possible mechanisms for overcoming drug resistance, such as autophagy and gene expression regulation, still need further exploration. Therefore, future studies will further evaluate the therapeutic effects of NEs-PTX-BEZ235 in animal models and explore broader mechanisms of overcoming drug resistance, laying a more solid foundation for its clinical translation.
In summary, this study confirms the significant antitumor activity of NEs-PTX-BEZ235 in colon cancer cells, reveals its potential mechanism of action, and provides new research ideas for overcoming PTX resistance. This strategy is expected to become a new direction in the treatment of colon cancer drug resistance and provide an important basis for further preclinical studies.
Data availability
All data generated or analysed during this study are included in this published article [and its supplementary information files].
References
Roper, J. et al. The dual PI3K/mTOR inhibitor NVP-BEZ235 induces tumor regression in a genetically engineered mouse model of PIK3CA wild-type colorectal cancer. PLoS ONE 6, e25132 (2011).
Lidi, Z. et al. Research progress of NVP-BEZ235 combined with anti-tumor drugs. Basic Clin. Med. 36, 1450–1454 (2016).
Gang, C. et al. Research progress of endophytic fungi producing taxol. Chin. Wild Plant Resources 34, 24–29 (2015).
Pham, D. T., Saelim, N. & Tiyaboonchai, W. Paclitaxel loaded EDC-crosslinked fibroin nanoparticles: A potential approach for colon cancer treatment. Drug Deliv. Transl. Res. 10, 413–424 (2020).
Zhiwen, L. & Zhangjun, Q. Progress in clinical application of paclitaxel liposomes. Asia-Pac Trad Med. 8, 229–232 (2012).
Haitao Y. Progress in synthesis and application of anticancer drug paclitaxel. Heilongjiang Sci. Technol. Inf. 129 (2017).
Zou, H. et al. Synergistic inhibition of colon cancer cell growth with nanoemulsion-loaded paclitaxel and PI3K/mTOR dual inhibitor BEZ235 through apoptosis. Int. J. Nanomed. 11, 1947–1958 (2016).
Hu, Y. et al. Synergistic inhibition of drug-resistant colon cancer growth with PI3K/mTOR dual inhibitor BEZ235 and nanoemulsioned paclitaxel via reducing multidrug resistance and promoting apoptosis. Int. J. Nanomed. 16, 2173–2186 (2021).
Chen, Y. H. et al. Maintenance BEZ235 treatment prolongs the therapeutic effect of the combination of BEZ235 and radiotherapy for colorectal cancer. Cancer 11, 1204 (2019).
Chen, J. et al. PI3K/Akt/mTOR pathway dual inhibitor BEZ235 suppresses the stemness of colon cancer stem cells. Clin. Exp. Pharmacol. Physiol. 42, 1317–1326 (2015).
Zhang, Y. K. et al. Regorafenib antagonizes BCRP-mediated multidrug resistance in colon cancer. Cancer Lett. 442, 104–112 (2019).
Weaver, B. A. How Taxol/paclitaxel kills cancer cells. Mol. Biol. Cell 25, 2677–2681 (2014).
Tiwari, S., Tirosh, B. & Rubinstein, A. Increasing the affinity of cationized polyacrylamide-paclitaxel nanoparticles towards colon cancer cells by a surface recognition peptide. Int. J. Pharm. 531, 281–291 (2017).
Gonçalves, A. et al. Caspase-8 activation independent of CD95/CD95-L interaction during paclitaxel-induced apoptosis in human colon cancer cells (HT29-D4). Biochem. Pharmacol. 60, 1579–1584 (2000).
Arnold, M. et al. Global patterns and trends in colorectal cancer incidence and mortality. Gut 66, 683–691 (2017).
Matsuno, J. et al. Synthesis and characterization of nanoemulsion-mediated core crosslinked nanoparticles, and in vivo pharmacokinetics depending on the structural characteristics. J. Control. Release: Off. J. Control. Release Soc. 324, 405–412 (2020).
Dreesen, O. & Brivanlou, A. H. Signaling pathways in cancer and embryonic stem cells. Stem cell Rev. 3, 7–17 (2007).
Hennessy, B. T. et al. Exploiting the PI3K/AKT pathway for cancer drug discovery. Nat. Rev. Drug Discovery 4, 988–1004 (2005).
Feltbower, R. G. et al. Epidemiology of central nervous system tumors in children and young adults (0–29 years), Yorkshire, United Kingdom. Pediatric Hematol. Oncol. 21, 647–660 (2004).
Qiang, H. et al. Isolation and culture of tumor stem cells from human glioma tissue. Chin. J. Oncol. 28, 331–333 (2006).
Bao, S. et al. Glioma stem cells promote radioresistance by preferential activation of the DNA damage response. Nature 444, 756–760 (2006).
Eramo, A. et al. Chemotherapy resistance of glioblastoma stem cells. Cell Death Differ. 13, 1238–1241 (2006).
Wang, Z. et al. Dihydromyricetin reverses MRP2-induced multidrug resistance by preventing NF-κB-Nrf2 signaling in colorectal cancer cell. Phytomed.: Int. J. Phytotherapy Phytopharmacol. 82, 153414 (2021).
Funding
This research was funded by the National Natural Science Foundation of China (grant numbers 82373176) and the Zhejiang Province Basic Public Welfare Research Program Project (grant number LY23H160012). The funding bodies played no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
X.Z.: Data curation, Formal analysis, Methodology, Validation, Writing—original draft. R.Z.: Methodology, Resources, Writing—original draft. Y.L.: Data curation. C.Y.: Data curation. Q.D.: Data curation. W.G.: Supervision. H.Z.: Conceptualization, Formal analysis, Funding acquisition, Project administration.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The experiment has been approved by the Human Research Ethics Committee of the Second Affiliated Hospital, Medical College of Zhejiang University.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhu, X., Zhang, R., Liu, Y. et al. Nanoemulsification of PTX and BEZ235 inhibits colon cancer growth. Sci Rep 15, 16217 (2025). https://doi.org/10.1038/s41598-025-94620-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-94620-y