Abstract
Pneumonia is amongst the leading causes of death in the United States. In 2020, pneumonia accounted for over 53,000 deaths and 2.6 million emergency department visits. Further research is needed to study the evolution of country-wide trends and disparities. The centers for disease control and prevention wide-ranging online data for epidemiologic research (CDC WONDER) was used to identify pneumonia-related deaths within the United States from 1999 to 2022. Data on demographic and regional groups were analyzed by calculating age-adjusted mortality rates (AAMRs) and annual percentage change (APC) in AAMRs, for sex, race/ethnicity, age, urban-rural classification, region, and states. Overall, the AAMR per 100,000 from pneumonia-related deaths declined by 52.1% from 35.9 to 17.2 between 1999 and 2022. Both males and females experienced a similar decrease (Average APC −3.24%), though males maintained higher AAMR throughout 1999–2022. African American and Black people experienced the highest mortality throughout the duration of the study, while American Indians and Native Alaskans had the greatest reduction in mortality, by −59.5%. Nursing home deaths decreased over time, and in turn, hospice deaths substantially rose. AAMR in age groups ≥ 70 declined but not for younger age groups. Several geographical differences were found between urban-rural groups, states, and census regions. Despite a decrease in pneumonia-related mortality in the United States between 1999 and 2022, significant differences in AAMR have been observed to have persisted, with male sex, African American race, and rural areas being disproportionately affected. Improving access to timely and adequate health care and reducing disparities between population groups appear to be the most promising ways of continuing the downward trend.
Similar content being viewed by others
Introduction
Pneumonia is among the leading causes of death in the United States (US). In 2020, pneumonia accounted for over 53,000 deaths and 2.6 million emergency department visits in the US1. Pneumonia is not only a cause of high mortality but also a great financial expense. In 2017, influenza infections among elderly patients alone cost the US an estimated $34.7 billion2. The US healthcare system continually works to improve pneumonia outcomes and decrease the economic burden. This reduction in pneumonia mortality is due to medical advancements, such as the development of influenza and pneumococcal vaccines3. From the first pneumococcal conjugate vaccine in 2000 to guidelines recommending routinely vaccinating children and the elderly, the incidence of pneumonia has been dramatically reduced4. Other notable advancements in rapid testing for viral causes of pneumonia have allowed for earlier detection5. Moreover, treatments for pneumonia have evolved over the years to include antibiotics, antivirals, and steroids with more standardized guidelines available5.
Even with these advances in care, pneumonia ranks in the top ten causes of death6. Studying the mortality over the years is pivotal in understanding which medical improvements result in greater outcomes. Despite the vast amount of data analyzing pneumonia mortality across the US, further research is needed to study the evolution of country-wide trends and highlight disparities. This study aims to comprehensively evaluate differences in pneumonia mortality across sex, race, age, and geographical regions. Using the US Centers for Disease Control and Prevention Wide-ranging Online Data for Epidemiologic Research (CDC WONDER) from 1999 to 2022, trends in mortality were analyzed.
Methods
Centers for disease control and prevention wide-ranging online data for epidemiologic research (CDC WONDER) was used to identify pneumonia (including that caused by influenza but excluding COVID-19-associated pneumonia)-related deaths occurring within the United States7,8. The Underlying cause of death is a public-use database of death certificate records that list the cause of mortality. It was analyzed to determine pneumonia as the underlying cause of death on nationwide death certificate records8. This database has been previously used in several other studies to analyze nationwide trends in influenza mortality and vaccination status and the methods were modeled from previous CDC WONDER studies, including Sidney et al. and Achara et al.6,8,9. Pneumonia-related mortality was identified using the International Classification of Diseases, 10th Revision; Clinical Modification codes J09-J18 in patients ≥ 25 years (Supplemental Table S1)8,9. This age restriction was selected because we focused on the adult population due to pneumonia-related mortality in patients < 25 years of age being infrequent. The study was exempt from institutional review board approval because the CDC WONDER database contains anonymized, publicly available data.
We extracted data regarding pneumonia-related deaths and population sizes from 1999 to 2022. Data on demographic and regional groups were extracted, including sex, race/ethnicity, age, urban-rural classification, region, and states. Racial/ethnicity groups were defined as White, Black/African American, American Indian/Alaskan Native, Asian/Pacific Islander, and Hispanic people as identified on death certificates. Age groups were defined as 25 to 39, 40 to 54, 55 to 69, 70 to 84, and 85 + years of age. For urban-rural classifications, the National Center for Health Statistics Urban-Rural Classification Scheme was used to divide the population into urban (large metropolitan area [population ≥ 1 million], medium/small metropolitan area [population 50,000 to 999,999]) and rural (population < 50,000) counties per the 2013 United States census classification10. CDC provides urbanization data to 2020, limiting analysis for urbanization from 1999 to 2020. Regions were classified into Northeast, Midwest, South, and West according to the Census Bureau definitions7,10. The locations of death included medical facilities (outpatient, emergency room, inpatient, death on arrival, or status unknown), homes, hospice, and nursing homes/long-term care.
Pneumonia-related crude and age-adjusted mortality rates were calculated. Crude mortality rates were calculated by dividing the number of Pneumonia-related deaths by the corresponding United States population8. Age-adjusted mortality rates (AAMR) were standardized using the 2000 United States standard population as previously described8,11. The Joinpoint Regression Program (Joinpoint version 4.9.0.0 available from National Cancer Institute, Bethesda, Maryland) was used to determine trends in mortality within the study period12,13. This program identifies significant changes in annual mortality trends over time through Joinpoint regression, which fits models of linear segments where significant temporal variation occurred8. Annual percentage change (APC) with 95% confidence intervals (CIs) for the AAMRs were calculated for the line segments linking a Joinpoint using the Monte Carlo permutation test, which involves repeatedly rearranging the observed data and recalculating the test statistic to compare the observed data’s fit to alternative models. This randomization-based method evaluates the null distribution of the test statistic through resampling and ensures a non-parametric assessment of model fit without relying on strict distributional assumptions. We calculated the weighted mean of the APCs and reported as an average annual percentage change (AAPCs) and corresponding 95% CIs as a summary of the reported mortality trend for the entire study period. APC and AAPCs were considered to increase or decrease if the slope describing the change in mortality over the time interval significantly differed from zero using a 2-tailed t-test. Statistical significance was set at p ≤ 0.05 (represented by asterisk “*” in results, figures, and supplemental file).
Results
Overall
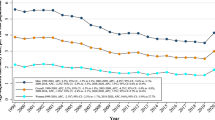
From 1999 to 2022, there were 63,550,429 total deaths in the United States. Of these deaths, 1,331,053 (2.1%) were due to pneumonia (Supplemental Table S2). Overall pneumonia associated AAMR decreased by 52.1% from 1999 to 2022 from 35.9 (95% CI 35.7 to 36.2) in 1999 to 17.2 (95% CI 17.0 to 17.3) in 2022, with an average annual percentage change (AAPC) of −3.1* (95% CI −3.6 to −2.6) (Supplemental Table S2, Fig. 1a; Table 1). Overall, AAMR increased to its highest point in 2000 at 36.3 (95% CI 36.1 to 36.6) and its lowest, 17.2 (95% CI 17.0 to 17.3) in 2022. Table 1 summarizes our study’s key findings, including the percentage change in AAMR and AAPC from 1999 to 2022 for each subgroup stratified by sex, race, census region, urbanization status, and age groups.
Demographic differences
Sex stratified
From 1999 to 2022, pneumonia caused 620,788 (46.6%) deaths in males and 710,265 (53.4%) deaths in females in the United States (Supplemental Table S2). The overall decline in AAMR was similar both groups (52.9% males, 53.5 females) (Table 1). The AAMR decreased in males from 43.7 (95% CI 43.2 to 41.7) in 1999 to 20.6 (95% CI 20.4 to 20.9) in 2022, with an AAPC of −3.2 (95% CI −3.6 to −2.8) (Supplemental Table S2, Fig. 1a). In females, the AAMR decreased from 31.4 (95% CI 31.1 to 31.7) in 1999 to 14.6 (95% CI 14.4 to 14.8) in 2022, with a steady AAPC of −3.2* (95% CI -3.7 to -2.8) (Supplemental Table S2, Fig. 1a).
Race stratified
Black or African American people had the highest AAMR over the years, with 38.5 (95% CI 37.5 to 38.1) in 1999 to 19.3 (95% CI 18.7 to 19.8) in 2022 and an AAPC of −2.7* (95% CI −3.4 to −2.1) (Supplemental Table S3). The APC in AAMR was −3.8* (95% CI −8.0 to −2.9) from 1999 to 2012, which reduced to −1.4 (95% CI −2.6 to 4.0) from 2012 to 2022 (Fig. 1b). The second highest AAMR was shown among White people, starting at 35.8 (95% CI 35.5 to 33.8) in 1999 and changing to 17.2 (95% CI 17.0 to 17.4) in 2022 (Supplemental Table S3). The AAPC from 1999 to 2022 was −3.2* (95% CI −3.8 to −2.8) (Fig. 1b). American Indian and Native Alaskan people had the most significant reduction in AAMR (59.5%) from 42.5 (95% CI 37.3 to 47.7) in 1999 to 17.2 (95% CI 15.5 to 18.9) in 2022 with an AAPC of −3.7* (95% CI −4.4 to −3.0) (Table 1, Supplemental Table S3). The lowest percentage change in AAMR was among the Hispanic population, with a decrease of 47.4% (Table 1). The APC of Asian and Pacific Islander people was −2.2* (95% CI −2.6 to −1.6) from 1999 to 2018 and continued to accelerate at -11.0* (95% CI −18.6 to −8.0) from 2018 to 2022 with an AAPC of −3.8* (95% CI −4.4 to −3.3) (Supplemental Table S3, Fig. 1b).
Age group stratified
The population of 85 years and older had the most decline in AAMR [67.5%] with 70–84 demonstrating the second largest decline (50.8%) while it stayed similar for two younger age groups, 25–39 and 55–69 and increased for 40–54 (Table 1). The 85 and older group had the highest overall mortality rate, which decreased from 751.8 (95% CI 743.4 to 760.1) in 1999 to 244.2 (95% CI 240.4 to 248.0) in 2022, with an AAPC of −4.6* (95% CI −5.2 to −4.1) (Supplemental Table S4, Fig. 2b). The 70–84 age group experienced a constant decline, with an AAPC of −3.3* (95% CI −3.9 to −2.8) throughout the study period (Fig. 2b). The 40–54 age group experienced an increase of 2.6% in AAMR (AAPC: 0.75*) (Supplemental Table S4, Fig. 2a).
Regional variation
Rural vs. urban
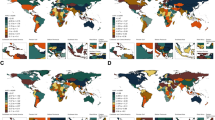
AAMRs were consistently highest in rural areas compared to small, medium, and large metropolitan regions. Large metropolitan zones experienced a decrease in APC between 1999 and 2010 by −4.2* (95% CI −8.9 to −3.3), which changed to −2.1 (95% CI −3.0 to 2.0) from 2010 to 2020 with an AAPC of −3.2* (95% −3.7 to −2.7) (Fig. 3a). From 1999 to 2010, the APC declined from −4.1 (95% CI −8.9 to 3.1) for medium/small metropolitan areas and slowed to −1.4 (95% CI −3.6 to 3.2) from 2010 to 2020 with an AAPC −2.8* (95% CI −3.7 to −2.1) (Fig. 3a). Rural zones saw AAMRs change from 39.6 (95% CI 38.9 to 40.3) in 1999 to 23.5 (95% CI 23 to 24) in 2020, with an AAPC of −2.5* (95% CI −3.1 to −2.0) (Supplemental Table S6, Fig. 3a).
Census region-based differences
Every census region saw a decrease in AAMR over time, with the Midwest seeing the greatest decrease in AAMR (54.3%) between 1999 and 2022 (Table 1). The South saw a decrease in AAMR from 36.6 (95% CI 36.1 to 37.0) in 1999 to 17.2 (95% CI 16.9 to 17.5) in 2022 with a consistent AAPC of −3.2 (95% CI −3.6 to -2.8) (Supplemental Table S8, Fig. 3b). The West steadily decreased with an AAPC of −3.8* (95% CI −4.5 to −3.2) (Fig. 3b). The Northeast’s AAPC was −2.8* (95% CI −3.4 to −2.3) (Fig. 3b). The Midwest witnessed a similar decrease with an AAPC of −2.8* (95% CI −3.5 to −2.3) from 1999 to 2022 (Fig. 3b, Supplemental Table S8).
State-level difference
The states with the highest AAMRs in 1999 were Kentucky, Tennessee, and Mississippi; while the states with the lowest AAMR in 1999 were California, New Hampshire, and Florida (Supplemental Table S7). In 2022 the states with the highest AAMR were Mississippi, West Virginia, and Arkansas (Supplemental Table S7). The states with the lowest AAMRs in 2022 were Colorado, Minnesota, and Oregon (Supplemental Table S7).
Montana, Rhode Island, and Colorado saw the largest decreases in AAMR with −28.5, −28, and −27.8 respectively (Supplemental Table S7, Fig. 4b). In comparison, Arkansas had a similar AAMR in 1999 of 38.8 (95% CI 36 to 41.6), but the AAMR only decreased to 26.1 in 2022 (−12.2%) (Supplemental Table S7, Fig. 4b). West Virginia and California had the smallest decreases from 1999 to 2022, with an average AAMR change of −6.2 and −7.7 respectively (Supplemental Table S7, Fig. 4b). State level changes in AAMR are summarized in (Fig. 4 and Supplemental Table S7).
Place of death
During the study period, the total number of deaths with a known place of death included 1,303,022 (97.8%) (Supplemental Table S5). 27.1% occurred outside medical facilities (19.2% nursing home/long-term care, 2.4% hospice, 5.5% home), and 72.9% occurred within medical facilities (Supplemental Table S5, Fig. 5). From 1999 to 2022, deaths in nursing homes decreased from 17,771 to 3496 (80.3% decline), while deaths in hospice surged, with a 3098.4% increase, from 62 in the year 2003 (Hospice deaths started being reported from 2003 onwards) to 1921 in the year 2022 (Supplemental Table S5, Fig. 5).
Discussion
This study reports several important findings regarding pneumonia-related mortality in the US from 1999 to 2022. While seeing overall mortality rates decrease, males had higher AAMR than females, African American and Black people experienced the highest mortality throughout the duration of the study, and American Indian and Native Alaskan people had the greatest reduction in mortality. Nursing home deaths decreased over time, and in turn, hospice deaths substantially rose. AAMR among people 70 and older declined, but not for younger age groups. Lastly, several geographical differences in AAMR were found between urban-rural groups, states, and census regions.
A decrease in pneumonia-related mortality rates reflects improvements made in pneumonia care. While our data was not linked to vaccination rates, there have been several advancements over the past 22 years in the sophistication of the pneumonia and influenza vaccines and an increase in vaccine utilization. The CDC has issued guidelines for annual influenza and pneumococcal vaccines for vulnerable populations14. Between 2005 and 2014, the CDC reported that the number of individuals receiving the influenza vaccine doubled (43.7%)7,15. Greater vaccine adherence may be reflected in lower mortality rates, as one study in Brazil found that overall mortality fell by 23.6% among individuals 65 and older who were vaccinated16. While vaccines play a vital role in reducing influenza incidence and preventing subsequent pneumonia, other key medical advances include risk stratification tools, rapid viral testing for early detection, and improved treatment methods17.
The next step after pneumonia prevention with vaccinations is diagnosing and treating pneumonia in patients. Risk assessment tools such as the pneumonia-severity index and CURB65 aid in estimating the mortality of a patient experiencing pneumonia18. These clinical prediction tools have allowed for a more systematic approach to treatment across providers and have been shown to accurately assess risk19. Risk stratification is often taken into consideration alongside diagnostic testing. Respiratory panels utilizing nucleic acid amplification testing have become more ubiquitous over the years, allowing for quick testing for multiple viruses in a sensitive manner5,17. Suspicion and early detection of respiratory viruses has been shown to reduce unnecessary antibiotic use and decrease admission rates for patients20. In addition to viral testing and treatment, treatments for bacterial causes of pneumonia have also enhanced. Improved testing techniques from sputum samples to bronchoscopies allow for samples to be cultured and bacteria susceptibility to quickly provide patients with targeted therapies. Diagnostic tests and treatments for pneumonia vary from hospital to hospital while vaccination records are often publicly reported and analyzed, which is why this discussion focuses on vaccination outcomes across demographics in addition to medical advances that may vary in their utilization.
While both sexes saw a decrease in mortality, AAMR for males decreased more than that of females. Males experience greater midlife mortality than females, with pneumonia being a factor that offsets the decline in life expectancy for both sexes21. Females have also reported higher vaccination rates than males15. Further research on differences between sex and pneumonia-related mortality is needed, as looking at mortality without separating males and females can mask specific trends21.
African Americans and Blacks had the highest overall mortality during the study. In addition to pneumonia-related mortality, this population experiences higher overall mortality22. There are many complex factors contributing to poorer health outcomes in African American and Black patients, which include social determinants of health such as socioeconomic status, insurance, and access to primary care22,23. These barriers to care may contribute to differences in vaccine rates as well. Studies have found that vaccine rates are lower amongst the Black population compared to other racial/ethnic groups2,14. Social determinants of health create issues surrounding vaccine accessibility, but increasing campaigns and education surrounding vaccinations in the African American and Black population may be an area of improvement24.
American Indian and Native Alaskan people had the greatest reduction in mortality from pneumonia25. Prior studies have highlighted this group as a higher risk for pneumonia complications. One hypothesis for this trend is increased vaccination adherence. The Office of Minority Health, a branch of the US Department of Health and Human Services, reported a vaccination ratio of 0.8 for American Indian and Alaskan people compared to non-Hispanic and White Americans for the 2019–2020 influenza season26.
As mortality changes among different populations, we have also seen shifts in where pneumonia deaths occur, with utilization of hospice services on the rise. A report from Medicare beneficiaries found that hospice services increased by 28.8% between 2000 and 201527. Nursing homes also contract with hospice facilities to move patients when their health needs change, leading to a greater number of patients dying in hospice care rather than nursing facilities28.
Advanced age leads to an increased risk for comorbid illnesses as well. Thus, the 85 and older age group has the greatest risk for complications regarding pneumonia. As medical improvements are made to treat these comorbidities, patients in this age category may have better outcomes regarding pneumonia-related illnesses. Additionally, vaccine efforts to target high-risk groups and patients over 65 years of age have helped reduce the spread of influenza and pneumonia29,30. Vaccine rates are highest among the 65 and older population, this could possibly explain why there was an increase in deaths for those below 657,15. In 2014, 58.7% of elderly adults reported receiving at least one kind of pneumococcal vaccine7,15. With greater improvements in decreasing mortality and higher vaccination rates, this outcome may support a larger effort to increase vaccinations among other age categories.
Another population comprised of older individuals is rural communities31. Rural areas had higher mortality rates and worse health outcomes due to increased distance from healthcare institutions, higher rates of poverty, and greater comorbidities due to lack of consistent care31,32. Another explanation for the improvement in mortality among population-dense areas is a greater concentration of college-educated people33. Vaccine campaigns have been shown to be successful in cities, especially when targeting high-risk populations24,34,35.
On a statewide level, there were several trends. States with the highest rates of pneumonia-related mortality were predominantly located in the South, except for New York, which was also among the states with the highest death rate from pneumonia. When comparing by regions, the Midwest had the greatest decrease in AAMR. Studies have found that overall mortality, especially in the rural South, is greater than in other geographical regions for proposed reasons of improved overall health outcomes and increased population density, leading to fewer rural southern communities31,32. Colorado was one of the states that saw the greatest change in AAMR. Compared to Arkansas, which had a similar AAMR in 1999, Colorado decreased its AAMR by over 27.8 and Arkansas by 11.4. This significant decrease in mortality compared to other states is an interesting finding, and understanding the factors that played a role in this improvement could be applied across the USA. A 2019 study by Woolf focused on life expectancy rather than pneumonia-related mortality and found that Colorado’s life expectancy difference increased between Colorado and Kansas from 1990 to 201633. This study hypothesized that outcome changes may reflect policy choices considering differences in demography and economies between the two states were low33. A 2004–2006 report from the CDC found Colorado to have the highest influenza vaccination and pneumococcal rates amongst their 65 and older population, at 76.5 and 71.4%, respectively, contributing positively to their lower AAMR36. While California’s vaccination rates from the same study were middle to lower in ranking, they saw the second smallest decrease in AAMR over the study duration (-7.7). Considering vaccination rates, factors resulting in consistent mortality outcomes may be related to lower overall mortality rates. Life expectancy in California ranks among the top five states37. This could be related to policies and projects such as the Healthy Cities and Communities Program, the oldest WHO campaign in the US to promote healthier lifestyles, focusing on social determinants of health38,39.
This study has several limitations. First, the CDC WONDER database is based on death certificates for US residents. Any errors in these certificates could affect data points in the study and lead to misclassification bias. Mortality data is coded by death certificates in the state where the deaths took place and may inaccurately represent deaths from patients who traveled for care. We only used the mortality data for pneumonia as the underlying cause of death, which does not consider the deaths where pneumonia might have contributed indirectly to mortality or acted as a secondary cause. While this strategy excluded excess deaths due to COVID-19-associated pneumonia from 2020 to 2022 and increased the specificity of non-COVID-19 pneumonia mortality for these years, it decreased sensitivity. As COVID-19 caused many deaths, especially in the older age group, it may have resulted in a smaller population at risk of dying from the non-COVID-19 pneumonia etiologies analyzed in our study. Data for Urbanization status is only available up to 2020, so we could not analyse data for 2021 and 2022. Hospice facilities started reporting data in 2003, so no earlier data could be assessed. Finally, given the cross-sectional nature of our study, we are only able to hypothesize associations but not prove causal relationships.
Conclusion
Despite a decrease in pneumonia-related mortality in the United States between 1999 and 2022, significant differences in AAMR have been observed to have persisted, with male sex, African American race, and rural areas being disproportionately affected. To continue the downward trend in pneumonia mortality, improving access to timely and adequate health care (including early detection, appropriate treatment, and vaccination) for all population groups and reducing disparities in the utilization of this access between population groups and across regions appear promising.
Data availability
Availability of data and materials: The datasets generated and analyzed during the current study are available on the CDC WONDER repository Underlying Cause of Death 1999-2022, https://wonder.cdc.gov/ucd-icd10.html.
References
Cairns, C. National hospital ambulatory medical care survey: 2020 emergency department summary tables. Natl. Cent. Health Stat. US https://doi.org/10.15620/cdc:121911 (2022).
Rothman, T. The cost of influenza disease burden in U.S population. Int. J. Econ. Manage. Sci. 06 (04). https://doi.org/10.4172/2162-6359.1000443 (2017).
Simonsen, L. et al. Impact of Pneumococcal conjugate vaccination of infants on pneumonia and influenza hospitalization and mortality in all age groups in the united States. mBio 2 (1), e00309–e00310. https://doi.org/10.1128/mBio.00309-10 (2011).
Centers for Disease Control and Prevention. About pneumococcal vaccine: For providers. https://www.cdc.gov/vaccines/vpd/pneumo/hcp/about-vaccine.html#references (2023).
Watkins, R. R. Using precision medicine for the diagnosis and treatment of viral pneumonia. Adv. Ther. 39 (7), 3061–3071. https://doi.org/10.1007/s12325-022-02180-8 (2022).
Rana, J. S., Khan, S. S., Lloyd-Jones, D. M. & Sidney, S. Changes in mortality in top 10 causes of death from 2011 to 2018. J. Gen. Intern. Med. 36 (8), 2517–2518. https://doi.org/10.1007/s11606-020-06070-z (2021).
Centers for Disease Control and Prevention. National Vital Statistics System, Mortality 1999–2020 on CDC WONDER Online Database. http://wonder.cdc.gov/mcd-icd10.html
Sidney, S. et al. Heterogeneity in National U.S. Mortality trends within heart disease subgroups, 2000–2015. BMC Cardiovasc. Disord. 17 (1), 192. https://doi.org/10.1186/s12872-017-0630-2 (2017).
Achara, K. E. et al. Trends and patterns in obesity-related deaths in the US (2010–2020): A comprehensive analysis using centers for disease control and prevention wide-ranging online data for epidemiologic research (CDC WONDER) data. Cureus 16 (9), e68376. https://doi.org/10.7759/cureus.68376 (2024).
Ingram, D. & Franco, S. 2013 NCHS Urban–Rural Classification Scheme for Counties. National Center for Health Statistics. Vital Health Stat.
Anderson, R. N. & Rosenberg, H. M. Age standardization of death rates: implementation of the year 2000 standard. National vital statistics reports: from the centers for disease control and prevention, national center for health statistics. Natl. Vital Stat. Syst. 47 (3), 1–16 (1998).
Kim, H. J., Fay, M. P., Feuer, E. J. & Midthune, D. N. Permutation tests for joinpoint regression with applications to cancer rates. Stat. Med. 19 (3), 335–351. (2000).
Program, J. R. [National Cancer Institute]. Statistical Methodology and Applications Branch, Surveillance Research Program (2023).
Centers for Disease Control and Prevention. Flu vaccination coverage, United States, 2020–21 influenza season. https://www.cdc.gov/flu/fluvaxview/coverage-2021estimates.htm
The American Lung Association Epidemiology and Statistics Unit. Trends in pneumonia and influenza morbidity and mortality. https://www.lung.org/getmedia/98f088b5-3fd7-4c43-a490-ba8f4747bd4d/pi-trend-report.pdf.pdf (2015).
Antunes, J. L. F., Waldman, E. A., Borrell, C. & Paiva, T. M. Effectiveness of influenza vaccination and its impact on health inequalities. Int. J. Epidemiol. 36 (6), 1319–1326. https://doi.org/10.1093/ije/dym208 (2007).
Merckx, J. et al. Diagnostic accuracy of novel and traditional rapid tests for influenza infection compared with reverse transcriptase polymerase chain reaction: A systematic review and meta-analysis. Ann. Intern. Med. 167 (6), 394. https://doi.org/10.7326/M17-0848 (2017).
Huang, L. et al. Performance of various pneumonia severity models for predicting adverse outcomes in elderly inpatients with community-acquired pneumonia. Clin. Microbiol. Infection: Off. Public. Eur. Soc. Clin. Microbiol. Infect. Dis. 30 (11), 1426–1432. https://doi.org/10.1016/j.cmi.2024.07.008 (2024).
Grudzinska, F. S. et al. Early identification of severe community-acquired pneumonia: A retrospective observational study. BMJ Open Respir. Res. 6 (1), e000438. https://doi.org/10.1136/bmjresp-2019-000438 (2019).
Rappo, U. et al. Impact of early detection of respiratory viruses by multiplex PCR assay on clinical outcomes in adult patients. J. Clin. Microbiol. 54 (8), 2096–2103. https://doi.org/10.1128/JCM.00549-16 (2016).
Acciai, F. & Firebaugh, G. Why did life expectancy decline in the united States in 2015? A gender-specific analysis. Soc. Sci. Med. 190, 174–180. https://doi.org/10.1016/j.socscimed.2017.08.004 (2017).
Williams, D. R. & Rucker, T. D. Understanding and addressing Racial disparities in health care. Health Care Financ. Rev. 21 (4), 75–90 (2000).
Cordoba, E. & Aiello, A. E. Social determinants of influenza illness and outbreaks in the united States. N. C. Med. J. 77 (5), 341–345. https://doi.org/10.18043/ncm.77.5.341 (2016).
Lippert, J. F., Buscemi, J., Saiyed, N., Silva, A. & Benjamins, M. R. Influenza and pneumonia mortality across the 30 biggest U.S. Cities: assessment of overall trends and Racial inequities. J. Racial Ethnic Health Disparit. 9 (4), 1152–1160. https://doi.org/10.1007/s40615-021-01056-x (2022).
Doxey, M., Chrzaszcz, L., Dominguez, A. & James, R. D. A forgotten danger: Burden of influenza mortality among american indians and alaska natives, 1999–2016.J. Public Health Manag. Pract. JPHMP S7–S10. https://doi.org/10.1097/PHH.0000000000001062 (2019).
Office of Minority Health. Immunizations and American Indians/Alaska natives. https://minorityhealth.hhs.gov/immunizations-and-american-indiansalaska-natives (2020).
Teno, J. M. et al. Site of death, place of care, and health care transitions among US medicare beneficiaries, 2000–2015. JAMA 320 (3), 264. https://doi.org/10.1001/jama.2018.8981 (2018).
Miller, S. C. & Mor, V. N. T. The role of hospice care in the nursing home setting. J. Palliat. Med. 5 (2), 271–277. https://doi.org/10.1089/109662102753641269 (2002).
Langer, J. et al. High clinical burden of influenza disease in adults aged ≥ 65 years: can we do better? A systematic literature review. Adv. Ther. 40 (4), 1601–1627. https://doi.org/10.1007/s12325-023-02432-1 (2023).
Nagata, J. M. et al. Social determinants of health and seasonal influenza vaccination in adults ≥ 65 years: A systematic review of qualitative and quantitative data. BMC Public. Health 13 (1), 388. https://doi.org/10.1186/1471-2458-13-388 (2013).
Centers for Disease Control and Prevention. About rural health. https://www.cdc.gov/ruralhealth/about.html#:~:text=Rural%20Americans%20are%20more%20likely,stroke%20than%20their%20urban%20counterparts (2023).
Miller, C. E. & Vasan, R. S. The Southern rural health and mortality penalty: A review of regional health inequities in the united States. Soc. Sci. Med. 268, 113443. https://doi.org/10.1016/j.socscimed.2020.113443 (2021).
Woolf, S. H. & Schoomaker, H. Life expectancy and mortality rates in the united States, 1959–2017. JAMA 322 (20), 1996. https://doi.org/10.1001/jama.2019.16932 (2019).
City of San Antonio. Immunization Program. https://www.sanantonio.gov/Health/HealthServices/Immunizations (2020).
23., C. of L. A. P. H. Immunization Coalition of Los Angeles County. http://publichealth.lacounty.gov/ip/ICLAC/index.htm (2020).
Gorina, Y., Kelly, T., Lubitz, J. & Hines, Z. Trends in influenza and pneumonia among older persons in the united States. Aging Trends (Hyattsville Md) 8, 1–11 (2008).
Kochanek, K., Murphy, S., Xu, J. & Arias, E. Deaths: final data for 2020. Natl. Vital Stat. Rep.: Centers Dis. Control Prev. Natl. Cent. Health Stat. Natl. Vital Stat. Syst. 72 (10), 63.
Twiss, J. M., Duma, S., Look, V., Shaffer, G. S. & Watkins, A. C. Twelve years and counting: California’s experience with a statewide healthy cities and community program. Public. Health Rep. (Washington D C : 1974) 115 (2–3), 125–133. https://doi.org/10.1093/phr/115.2.125 (2000).
Aronson, R., Norton, B. & Kegler, M. Achieving a broad view of health: findings from the California healthy cities and communities evaluation. Health Educ. Behav. 34 (3), 441–452.
Author information
Authors and Affiliations
Contributions
EH analyzed and interpreted the data and was a major contributor in writing the manuscript. AJ completed the data analyses and was a major contributor in writing the manuscript. MA was a contributor to writing and editing the manuscript. NA was a contributor to writing and editing the manuscript. KM was a contributor to writing and editing the manuscript. MM contributed editing the manuscript. AT contributed editing the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Holland, E., Jabbar, A.B.A., Asghar, M.S. et al. Demographic and regional trends of pneumonia mortality in the United States, 1999 to 2022. Sci Rep 15, 10103 (2025). https://doi.org/10.1038/s41598-025-94715-6
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-94715-6
This article is cited by
-
Demographic and geographic hotspots of Alzheimer’s disease and pneumonia-related mortality among older adults in the United States: a retrospective analysis
European Journal of Medical Research (2026)