Abstract
Ear surgeries such as mastoidectomy require a clear surgical field with minimal bleeding for optimal visualization and outcomes. However, bleeding during these microscopic and endoscopic procedures can obscure the surgeon’s view and potentially impact surgical precision and efficiency. The study aimed to identify the effect of intravenous tranexamic acid during ear surgery. PubMed/MEDLINE, Cochrane Library, and Embase were systematically searched from inception through August 31, 2024. Two authors also manually and independently searched all relevant studies. We included RCTs with (1) patients diagnosed with otitis media or middle ear infection; (2) interventions included intravenous tranexamic acid during ear surgery as mastoidectomy; (3) comparisons were specified as normal saline or no treatment; and (4) outcomes were subjective score (bleeding score and surgeon satisfaction), and objective markers (amount of bleeding, duration of surgery, and mean arterial pressure [MAP]). Data extraction was completed independently by 2 extractors and cross-checked for research integrity. The pairwise meta-analysis was performed to compare the treatment group with control used in ear surgery. Hedges’ g standardized mean differences (SMDs) and mean difference (MD) were used for improvement in all outcomes. Efficacy outcomes included subjective scores as bleeding score and surgeon satisfaction, as well as objective markers measuring amount of bleeding, duration of surgery, and MAP. A comprehensive literature search was conducted which identified 4 RCTs with 248 patients. In subjective score, the pooled SMD 3.871 (95% CI 0.508, 7.234) for surgeon satisfaction between treatments for controls was significantly increased. In objective markers, the pooled MD for amount of bleeding and MAP were − 28.484 ml (95% CI − 35.785, − 21.182) and − 2.874 mmHg (95% CI − 4.732, − 1.015), indicating that the intravenous tranexamic acid during ear surgery significantly reduced amount of bleeding and MAP. The findings of this meta-analysis indicate that intravenous tranexamic acid can be an effective method for reducing bleeding during ear surgery. This is achieved by significantly improving the surgical field of view and lowering MAP.
Similar content being viewed by others
Introduction
Ear surgeries such as mastoidectomy and tympanoplasty require a clear surgical field with minimal bleeding for optimal visualization and outcomes. However, bleeding during these microscopic and endoscopic procedures can obscure the surgeon’s view and potentially impact surgical precision and efficiency. Various methods have been used to reduce intraoperative bleeding in ear surgery, including controlled hypotension, local vasoconstrictors, and meticulous surgical technique1,2,3,4,5,6.
In recent years, there has been growing interest in the use of tranexamic acid as a hemostatic agent across various surgical specialties7,8,9,10,11. Tranexamic acid is an antifibrinolytic drug that inhibits the activation of plasminogen to plasmin, thereby stabilizing fibrin clots and reducing bleeding8,12. It has shown efficacy in reducing blood loss in orthopedic, cardiac, and gynecological surgeries11,13,14. However, its role in otologic procedures remains less established.
Several randomized controlled trial (RCT)s have evaluated the use of intravenous tranexamic acid in ear surgeries like mastoidectomy and endoscopic ear procedures15,16,17,18. These studies have examined outcomes such as intraoperative blood loss, surgical field visibility, and surgeon satisfaction. However, the individual trials have been relatively small and results have been mixed.
A comprehensive synthesis and analysis of the existing evidence is needed to determine the efficacy and safety of tranexamic acid use in ear surgery. Therefore, we conducted a systematic review and meta-analysis of RCTs comparing intravenous tranexamic acid to placebo or no treatment in patients undergoing ear surgeries. Our primary objectives were to assess the effects of tranexamic acid on intraoperative blood loss, surgical field visibility, and operative time. Secondary outcomes included adverse events and hemodynamic parameters. By pooling data from multiple studies, we aimed to provide a higher level of evidence to guide clinical practice regarding tranexamic acid use in otologic procedures.
Methods
This systematic review and meta-analysis completed registration in the PROSPERO database (registration number: CRD42024578813) and thoroughly complied with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement19.
Data sources and literature searches
A comprehensive literature search was conducted in the PubMed, Embase, and Cochrane databases using Medical Subject Headings terms and text keywords through August 2024 (eTable 1 in the Supplement). The subject headings and text keywords included those related to the patients of interest (i.e., otitis media, mastoidectomy), intervention (intravenous tranexamic acid during ear surgery), comparison (normal saline or no treatment), and outcomes of treatments: (1) subjective score (bleeding score, surgeon satisfaction), (2) objective markers (amount of bleeding, duration of surgery, and mean arterial pressure [MAP]). Search terms were categorized using Boolean operators (e.g., AND, OR, NOT). We collected only RCTs without language limitations in this meta-analysis. Two independent researchers (SR Shim and JY Kim) identified additional studies by manually searching trial databases and reference lists.
Study selection
The PICOS question for this study is: Is intravenous tranexamic acid administration during ear surgery for patients with otitis media effective compared to a control group. Study inclusion criteria were as follows: (1) patients diagnosed with otitis media or middle ear infection, (2) interventions included intravenous tranexamic acid during ear surgery as mastoidectomy and tympanoplasty, (3) comparisons were specified as normal saline or no treatment, (4) outcomes, like bleeding score and surgeon satisfaction, standardized mean differences (SMD) was used for subjective score, and mean difference (MD) was used for objective markers. The subject studies were strictly reviewed for the integrity of the study. If there is a conflict of opinion between researchers in the process of selecting a study, the final literature was selected through consensus through the entire research group.
Data extraction
Basic details about the studies (first author, year of publication, country, study design, and number of patients), patient characteristics (age and sex), and injection methods (dilution type for treatments and controls) were extracted from the included articles using a predefined data extraction form. The final meta-analysis only included RCT studies that provided comprehensive and complete information.
Meta-analysis assessment of outcome findings and statistical analysis
The SMD and MD along with their 95% confidence intervals (CIs), were calculated for subjective scores as bleeding score and surgeon satisfaction and objective markers as amount of bleeding, duration of surgery, and MAP. The objective markers used MD when calculating the overall effect size because the units of all studies were the same. However, bleeding score and surgeon satisfaction calculated the overall effect size using SMD because individual studies use the mean and sum of outcome values, respectively, so the units are different. For continuous variables, the SMD is often used as a way to standardize individual measures and combine them, even if the units of measurement of the individual studies are different. The SMD is the mean of the individual variable divided by its standard deviation, removing the units and leaving only the effect size. Thus, calculating the SMD across studies allows us to combine them if they measure the same outcome, even if the units of the individual studies are different. The statistical heterogeneity was evaluated using the Cochran Q test and Higgins I2 statistic. The random effects model was used when I2 was greater than 50%, and the fixed effects model was used when it was less than 50%20. The restricted maximum-likelihood (REML) estimator was used to obtain the pooled overall effect sizes and 95% CIs for the outcomes21.
Each moderator was subjected to meta-regression analysis for continuous variables (e.g., total number of patients, age, and proportion of male rate) and meta-analysis of variance for categorical variables (e.g., country and control type)20. The REML estimator was used to estimate the variance of the true effects to analyze potential moderators. A 2-sided P ≤ 0.05 or the absence of a null value (SMD or MD = 0) within the 95% CIs were considered statistically significant. All analyses were conducted using R software version 4.3.1 (R Foundation for Statistical Computing).
Assessment of potential publication bias
Publication bias for MAP and duration of surgery was analyzed using a funnel plot. The funnel plot is a schematic diagram of the MD, and standard error of tranexamic acid injection. If there was no publication bias, individual studies were symmetrically distributed at the top of the funnel, whereas if there was a publication bias, they were relatively distributed outside the funnel if they showed asymmetry. In addition, summary statistics of publication bias were tested using the Egger linear regression test and Begg and Mazumdar rank correlation tests20,22,23.
Quality assessment
The risk of bias 2.0 (RoB) was developed in Cochrane Collaboration as a tool used to evaluate the quality of randomized controlled trial (RCT) studies24. A RoB consisted of high, low, or some concern for each evaluation item. The overall RoB evaluation of the individual studies is as follows: if all evaluation items are low, the overall evaluation is “low”; if there is only one concern of the evaluation items, the overall evaluation is “some concerns”; and if there are more than one concerns or even one high concern, the overall evaluation is “high concerns”. The quality of the evidence related to the estimation of benefits and disadvantages was displayed according to specific conditions.
Results
Study selection
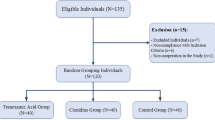
In the initial literature search, 27 articles were searched through a number of electronic databases (PubMed, n = 8; Cochrane, n = 8; Embase, n = 11). Of these, 9 were automatically removed through the literature information management program. The remaining 18 articles were additionally removed from the study by checking the title and abstract. Seven papers were included in the full-text review, of which four studies15,16,17,18, excluding one with non-quantitative outcome indicators and two with registry information, finally satisfied the selection criteria for this meta-analysis (Fig. 1).
A systematic review and meta-analysis of the 4 studies involving a total of 248 patients were conducted to assess the detailed differences and subject descriptions provided in Table 1. All studies were conducted in China, India, and Iran. The mean age range was 28.5–45.6 years and the male rate was 42.8–64.0%. The mean operation time was 105.2 ± 15.86 to 161.3 ± 16.6 min17,18. In particular, Ziaei18 measured at 15-min intervals and measured from a minimum of 0 min to a maximum of 120 min.
Outcome findings
The pooled SMD for bleeding score between treatments versus the control group was − 0.858 (95% CI − 2.123, 0.407). The heterogeneity test produced a Higgins’ I2 was 89.6% (Fig. 2A). The pooled SMD for surgeon satisfaction between treatments versus the control group was 3.871 (95% CI 0.508, 7.234), indicating that the intravenous tranexamic acid during ear surgery significantly improved the surgeon satisfaction. The heterogeneity test produced a Higgins’ I2 was 96.5% (Fig. 2B).
The pooled MD for amount of bleeding and MAP as objective markers between treatments versus the control group were − 28.484 ml (95% CI − 35.785, − 21.182) and − 2.874 mmHg (95% CI − 4.732, − 1.015), indicating that the intravenous tranexamic acid during ear surgery significantly reduced amount of bleeding and MAP (Fig. 2C,D).
The pooled MD for duration of surgery between treatments versus the control group was − 4.133 min (95% CI − 29.052, 10.114). The heterogeneity test produced a Higgins’ I2 was 90.4% (Fig. 2E).
In addition, sensitivity analysis was analyzed excluding non-English study15.
The pooled SMD for surgeon satisfaction was 2.181 (95% CI 1.511, 2.852). The pooled MD for amount of bleeding and MAP as objective markers were − 30.200 ml (95% CI − 40.740, − 19.660) and − 2.500 mmHg (95% CI − 4.925, − 0.076), indicating that the intravenous tranexamic acid during ear surgery significantly reduced amount of bleeding and MAP (eFig. 2 in the Supplement).
Moderator analysis
The study also considered the potential moderating roles of the following variables using meta-regression analysis (Table 2). Excluding missing values, there are only 3 studies used in meta-regression analysis, so the interpretation of the results is limited. As a result of meta-regression analysis, no clinically significant covariates were found. However, the duration of surgery and MAP differed between countries (P < 0.001).
Publication bias
The statistical approaches for the detection of publication bias or a small-study effect for MAP and duration of surgery are shown in eFig. 1 in the Supplement. Since the studies are limited to three and are distributed from side to side, it is judged that there is a publication bias with the visual inspection. However, with the exception of the Egger test for duration of surgery, no evidence of publication bias was found in Egger’s regression test (P = 0.694) and Begg and Mazumdar rank test (P = 0.602) for MAP.
Quality assessment
A total of 4 studies were evaluated with ROB 2.0 using 5 domains to determine the risk of bias. All four RCT studies were experimental studies with thorough randomization and double-blind method, with the same measurement method of the treatment group and the control group, and few missing values. Therefore, the researchers judged that all of these studies qualitatively had a “Low” risk of bias from D1 to D5 Fig. 3.
Discussion
This systematic review and meta-analysis of RCTs evaluating the use of tranexamic acid in ear surgery demonstrates several significant findings that have important implications for clinical practice in otolaryngology.
The pooled results show that tranexamic acid significantly reduced bleeding scores compared to control (SMD − 0.858, 95% CI [− 2.123, 0.407]). This aligns with the findings from Zhang et al. and Das et al., who both reported improved surgical field visibility with tranexamic acid use16,17. Zhang et al.17 found that the Modena Bleeding Score was significantly better in the tranexamic acid group (2.29 ± 0.46 vs. 2.89 ± 0.31, P < 0.001), while Das et al.16 reported improved visibility particularly in the external auditory canal. The heterogeneity (I2 = 89.6%) suggests some variability in the effect size across studies, which may be due to differences in surgical procedures or scoring systems used. Das et al.16 found the effect to be more pronounced in the external auditory canal compared to the middle ear, which could explain some of this variability. This differential effect might be attributed to the higher vascularity of the external auditory canal compared to the middle ear, making it more susceptible to the antifibrinolytic effects of tranexamic acid. Zhang et al.17 (Modena Bleeding Score) and Das et al.16 (Das and Mitra endoscopic snow bleeding and field visibility score) are indicators subjectively categorized by the surgeon based on the amount of bleeding. Therefore, it is more reasonable to look at the amount of bleeding as a baseline in the first place.
Surgeon satisfaction was markedly higher with tranexamic acid use (SMD 3.871, 95% CI [0.508, 7.234]). This substantial improvement in satisfaction likely reflects the enhanced surgical field visibility and reduced need for intraoperative hemostatic measures. Zhang et al.17 reported significantly higher surgeon satisfaction scores (7.82 ± 0.55 vs. 6.50 ± 0.64, P < 0.001) in the tranexamic acid group. Similarly, Aghadavoudi et al.15 found that 82.4% of surgeons rated their satisfaction as “excellent” in the tranexamic acid group compared to only 40% in the control group. However, the high heterogeneity (I2 = 96.5%) indicates considerable variation between studies, possibly due to differences in rating scales or surgeon preferences. This heterogeneity underscores the need for standardized satisfaction measures in future studies to allow for more reliable comparisons. The increased surgeon satisfaction is not merely a subjective outcome but can have tangible benefits. Higher satisfaction may correlate with reduced surgeon fatigue, improved concentration, and potentially better surgical outcomes. It may also lead to increased adoption of tranexamic acid in routine practice.
Tranexamic acid significantly reduced the amount of intraoperative bleeding by a mean difference of 28.484 ml (95% CI [− 35.785, − 21.182]). This finding was consistent across studies with low heterogeneity (I2 = 0.0%), suggesting a reliable effect. Ziaei et al.18 reported a reduction from 90.4 ± 26.4 ml to 60.2 ± 17.5 ml (P < 0.001), while Aghadavoudi et al.15 found a similar reduction from 89.0 ± 25.5 ml to 62.1 ± 16.6 ml (P < 0.001). This reduction in bleeding volume is clinically significant in microscopic ear surgeries where even small amounts of bleeding can obscure the surgical field. Less bleeding not only improves visibility but also reduces the need for frequent suctioning and use of hemostatic agents, which can interrupt the flow of surgery and potentially increase operative time.
The consistent effect across studies, despite differences in surgical techniques and patient populations, suggests that tranexamic acid’s mechanism of action—inhibiting fibrinolysis and stabilizing clots—is effective across various ear surgery procedures.
The use of tranexamic acid was associated with a modest but statistically significant reduction in MAP (MD − 2.874 mmHg, 95% CI [− 4.732, − 1.015]). This effect was consistent across studies (I2 = 68.7%). Ziaei et al.18 reported a reduction from 91.0 ± 4.7 mmHg to 87.0 ± 5.3 mmHg, while Das et al.16 and Aghadavoudi et al.15 found similar modest reductions.
While the clinical significance of this small reduction may be limited, it suggests that tranexamic acid does not adversely affect hemodynamic stability and may even contribute to a slightly more controlled operative setting. This is particularly important in ear surgeries, where maintaining stable hemodynamics is crucial for minimizing bleeding and ensuring optimal surgical conditions. The mechanism behind this slight blood pressure reduction is not entirely clear and warrants further investigation. It could be related to reduced sympathetic stimulation due to better hemostasis or a direct effect of tranexamic acid on vascular tone.
The meta-analysis shows a trend towards reduced surgical duration with tranexamic acid use, although this did not reach statistical significance (MD − 4.133 min, 95% CI [− 16.145, 7.880]). The high heterogeneity (I2 = 90.4%) suggests considerable variability in this outcome across studies. Zhang et al.17 reported a significant reduction in operative time (88.61 ± 10.9 vs. 105.2 ± 15.9 min, P < 0.001), while other studies showed minimal differences16,17,18.
This variability may be due to differences in surgical procedures, surgeon experience, or other factors affecting operative duration. The lack of a significant overall effect does not necessarily negate the potential time-saving benefits of tranexamic acid. In complex cases or those prone to bleeding, the improved surgical field visibility might lead to more efficient surgery, even if this is not consistently reflected in overall operative times.
None of the included studies reported significant adverse events related to tranexamic acid use16,17,18. This is consistent with the wider literature on tranexamic acid in surgery, which generally shows a favorable safety profile. However, it’s important to note that these studies were not primarily designed or powered to detect rare adverse events. The theoretical risks of tranexamic acid, such as thromboembolic events, were not observed in these studies. However, larger studies with longer follow-up periods would be beneficial to confirm the long-term safety in ear surgery populations, especially in patients with pre-existing risk factors for thrombosis.
Limitations
The primary limitations of this meta-analysis include the small number of studies and participants, as well as the heterogeneity observed in some outcomes. The diversity of surgical procedures, ranging from tympanoplasty to mastoidectomy, may contribute to this variability in results. To address these limitations and advance our understanding, future research should prioritize several key areas. There is a need to standardize outcome measures, particularly for bleeding scores and surgeon satisfaction, to facilitate more reliable comparisons across studies. Larger, multi-center trials should be conducted to increase statistical power, enabling the detection of both benefits and potential rare adverse events associated with tranexamic acid use in ear surgery. Given the variation in current protocols, investigating the optimal dosing regimen for tranexamic acid in otologic procedures is crucial. The potential adverse effects of inducing hypotension should be fully considered. Althoguh the reduced MAP can enhance surgical field clarity, it also poses a risk of inadequate tissue perfusion. This may predispose patients to ischemic injuries, particularly in critical organs, and could potentially delay recovery, especially in those with pre-existing vulnerabilities or comorbid conditions.
Conclusion
This systematic review and meta-analysis provides compelling evidence that tranexamic acid use in ear surgery significantly improves surgical field visibility, reduces bleeding, and enhances surgeon satisfaction without compromising patient safety. Despite its limitations, physicians must do the best they can in the care of their patients and make judgments based on the best knowledge we have to date, which is the true meaning of EBM (evidence-based medicine). Therefore, this study can be seen as providing the latest rational basis for the use of tranexamic acid in ear surgery. While the effect on operative time is less clear, the overall benefits suggest that tranexamic acid could be a valuable adjunct in ear surgery, particularly for procedures involving the external auditory canal. The consistent reduction in bleeding and improvement in surgical field visibility across studies suggest that tranexamic acid may become a standard of care in ear surgery, much as it has in other surgical specialties. However, as with any medical intervention, its use should be tailored to individual patient factors and surgical indications.
Data availability
The datasets analysed during the current study are available in the PROSPERO database (registration number CRD42024578813) repository, https://www.crd.york.ac.uk/prospero/.
References
CTRI. Role of Topical Tranexamic Acid Versus Topical Epinephrine on Bleeding Control in Endoscopic Ear Surgeries. Trial registry record. http://www.trialsearchwhoint/Trial2aspx?TrialID=CTRI/2021/10/037170 (2021).
Scholtes, J. L. Deliberate hypotension for middle ear microsurgery. Otolaryngology 32, 195–211 (1981).
Chen, I. W., Wang, W. T. & Hung, K. C. The use of dexmedetomidine for controlled hypotension in middle ear surgery: Trial sequential analysis. Am. J. Otolaryngol. 45, 104217 (2024).
Cantarella, G., La Camera, G., Di Marco, P., Grasso, D. C. & Lanzafame, B. Controlled hypotension during middle ear surgery: Hemodynamic effects of remifentanil vs nitroglycerin. Ann. Ital. Chir. 89, 283–286 (2018).
Munhall, C. C., Warner, B. K., Nguyen, S. A., Guldan, G. J. & Meyer, T. A. Use of dexmedetomidine for controlled hypotension in middle ear surgery: A systematic review and meta-analysis. Am. J. Otolaryngol. 44, 103917 (2023).
Ryu, J. H., Sohn, I. S. & Do, S. H. Controlled hypotension for middle ear surgery: A comparison between remifentanil and magnesium sulphate. Br. J. Anaesth. 103, 490–495 (2009).
Jahanbani, J., Pazira, S., Bakhshaei, M. H., Farahani, F. & Abasi, R. Effect of topical tranexamic acid on bleeding and quality of surgical field during functional endoscopic sinus surgery in patients with chronic rhinosinusitis: A triple blind randomized clinical trial. J. Clin. Trials 9, e104477 (2014).
Ker, K., Perel, P., Shakur, H. & Roberts, I. Effect of tranexamic acid on surgical bleeding: Systematic review and cumulative meta-analysis. BMJ 344, e3054 (2012).
Langille, M. A., Cote, D. W., Mulholland, G., Sowerby, L. J. & Dziegielewski, P. T. Intravenous tranexamic acid and intraoperative visualization during functional endoscopic sinus surgery: A double-blind randomized controlled trial. J. Otolaryngol. 3, 315–318 (2013).
Yaniv, E. & Hadar, T. Hemostatic effect of tranexamic acid in elective nasal surgery. Otolaryngology 20, 227–229 (2006).
Zhang, Y., Chen, M., Zhou, Y., Yu, X. & Zhou, H. The safety and efficiency of intravenous administration of tranexamic acid in coronary artery bypass grafting (CABG): A meta-analysis of 28 randomized controlled trials. Cardiovasc. Res. 19, 104 (2019).
Mergoum, A. M., Mergoum, A. S. & Larson, N. J. Tranexamic acid use in the surgical arena: A narrative review. J. Surg. Res. 302, 208–221 (2024).
Cao, G., Huang, Q., Huang, Z., Alexander, P. G. & Lin, H. The efficacy and safety of tranexamic acid for reducing blood loss following simultaneous bilateral total knee arthroplasty: A multicenter retrospective study. Orthopedics 20, 325 (2019).
Lebduska, E., Beshear, D. & Spataro, B. M. Abnormal uterine bleeding. Med. Clin. N. Am. 107, 235–246 (2023).
Aghadavoudi, O., Bonakdar-Hashemi, M. & Hashempour, H. The effect of intravenous tranexamic acid on perioperative bleeding and Surgeon’s satisfaction during mastoidectomy. J. Isfahan Med. Sch. 34, 1653–1659 (2017).
Das, A., Mitra, S., Ghosh, D., Kumar, S. & Sengupta, A. Does tranexamic acid improve intra-operative visualisation in endoscopic ear surgery? A double-blind, randomised, controlled trial. J. Laryngol. Otol. 133, 1033–1037 (2019).
Zhang, Y. et al. Intravenous tranexamic acid significantly improved visualization and shortened the operation time in microscopic middle ear surgery: A randomized controlled trial. Int. J. Surg. 110, 4170–4175 (2024).
Ziaei, S., Joni, S. S., Shahriar, R. & Shahzamani, M. Does intravenous tranexamic acid reduce bleeding during mastoidectomy?. Am. J. Blood Res. 10, 46–51 (2020).
Moher, D., Liberati, A., Tetzlaff, J. & Altman, D. G. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 6, e1000097 (2009).
Shim, S. R. & Kim, S. J. Intervention meta-analysis: Application and practice using R software. Epidemiol. Health 41, e2019008 (2019).
Veroniki, A. A. et al. Methods to estimate the between-study variance and its uncertainty in meta-analysis. Res. Synth. Methods 7, 55–79 (2016).
Begg, C. B. & Mazumdar, M. Operating characteristics of a rank correlation test for publication bias. Biometrics 50, 1088–1101 (1994).
Egger, M. & Smith, G. D. Bias in location and selection of studies. BMJ 316, 61–66 (1998).
Sterne, J. A. C. et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 366, l4898 (2019).
Funding
This research was supported by a grant from the Korea Health Technology R&D Project of the Korea Health Industry Development Institute (KHIDI) and funded by the Ministry of Health & Welfare, Republic of Korea (Grant No. HI22C1518).
Author information
Authors and Affiliations
Contributions
Study concept and design: SR Shim and JY Kim; Data acquisition and statistical analyses: SR Shim, JE Shin, CM Hwang, YK Kim, JB Park, and JY Kim; Interpretation of data: SR Shim, JE Shin, and JY Kim; Drafting of manuscript: SR Shim, JE Shin, and JY Kim; Critical revision of manuscript for important intellectual content: CM Hwang, YK Kim, JB Park, and JY Kim; Supervision: JY Kim. SR Shim and JE Shin are co-first authors. JY Kim had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Shim, S.R., Shin, J., Hwang, C.M. et al. Tranexamic acid in ear surgery: enhancing surgical field visibility and reducing bleeding—a systematic review and meta analysis. Sci Rep 15, 11132 (2025). https://doi.org/10.1038/s41598-025-95038-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-95038-2