Abstract
This study investigates the acceptability of Virtual reality (VR) technology for emotional regulation among cancer patients. Drawing from extensive literature, we enhanced external variables across user characteristics, product impact factors, and social environment influences, creating the "Theoretical Model of Cancer Patients’ Acceptance of VR Intervention for Self-Emotion Regulation." Surveying 489 Chinese cancer patients validated the model’s strong reliability through SPSS AMOS analysis. The acceptance of VR intervention for self-emotional regulation among cancer patients was assessed, revealing that the average scores across all 13 dimensions exceeded 3. This indicates that cancer patients hold a positive attitude toward VR-based emotional regulation interventions. Perceived usefulness, usage attitude, social norms, immersion, and personal innovation correlated positively with behavioral intention, while technological anxiety and perceived risk showed negative correlations. Findings support 15 hypotheses, offering theoretical backing for VR technology in emotional regulation for cancer patients. These insights provide medical institutions with valuable data on patient attitudes, facilitating the development of targeted treatment approaches.
Similar content being viewed by others
Introduction
In recent years, the global number of cancer patients has been steadily rising, with cancer ranking as the second leading cause of death worldwide, presenting an ongoing public health challenge1. Studies reveal that cancer occupies the top spot in causes of death in most economically developed nations. In developing countries, cancer often holds the second position on the list of leading causes of death2. For countries like China, with a substantial population, both the incidence and mortality rates of cancer remain alarmingly high, making it one of the nation’s carrying a significant burden of cancer worldwide. Researchers are fervently seeking solutions to alleviate the mounting pressure of cancer patients in China3. Addressing the threat of cancer effectively, especially before achieving breakthroughs in technology, mitigating and restraining cancer’s incidence and mortality rates, and assisting cancer patients in their recovery within the current technological landscape, have become vital concerns demanding attention from academia and society alike.
Virtual reality (VR), as an immersive form of human–computer interaction, utilizes computer-generated real-time expressions of the human perceptual world. Often referred to as a virtual environment, it enables individuals to explore and interact with computer-generated three-dimensional environments4. Achieving a complete VR experience involves the integration of various technologies, including head-mounted displays, headphones with sound and noise control functionalities5, controllers, haptic devices, all of which respond to users’ head movements6, creating a sense of presence7. Virtual reality technology has long been pivotal in military and aviation training, but in recent years, the focus of research has shifted towards clinical psychology and therapeutic applications, marking a burgeoning trend. With the decreasing costs of digital media, VR technology has demonstrated significant potential in reimagining traditional patient care methods8. This technology not only enhances the effectiveness of patients’ recovery processes but also imparts enjoyable experiences, aiding healthcare professionals in comprehensive treatment progress monitoring. Moreover, VR technology can address issues within conventional treatment methods, such as pre-operative planning based solely on mental simulations and seamless teamwork coordination. By amalgamating modern information technology advancements with medical science, VR technology presents an opportunity to enhance and innovate traditional medical approaches, thereby expanding the possibilities for treatment.
In the course of cancer treatment, due to its protracted nature, patients inevitably experience emotional fluctuations, including anxiety and depression, negatively impacting their ability to cope with the illness and quality of life9. These emotional distresses can significantly hinder patients’ ability to maintain a positive emotional state throughout the extended treatment period. Few patients can sustain a positive emotional state consistently during such prolonged treatments, with most enduring persistent negative emotions. Furthermore, emotional lows among patients can influence each other, leading to intense emotional fluctuations and affecting subsequent treatment outcomes10. While VR technology enjoys extensive use in sectors like military, its civilian application often centers around emotion regulation and expression. Though VR technology is primarily associated with entertainment products upon market introduction, its potential in emotional regulation remains evident11. A growing body of research investigates the application of VR technology in various psychological disorder treatments12,13. Integrating existing VR technology with the cancer treatment journey offers the prospect of maintaining positive emotions in patients experiencing emotional lows. VR technology can provide a secure space for patients to express negative emotions and alleviate emotional stress. The primary aim of this study is to explore the potential acceptance of VR technology among cancer patients.
Related works
Cancer treatment and patient emotions
The emotions of cancer patients significantly influence the trajectory of their illness, yet limited research has focused on assessing the correlation between cancer treatment and emotions. The diagnosis and treatment of cancer often entail immense suffering, which can result in notable adverse effects14. Studies indicate that patients’ psychological state can impact disease progression, with a high prevalence of negative emotions potentially severely disrupting treatment processes, lowering immune function, increasing the risk of infections, and even triggering disease recurrence15. Furthermore, emotions such as anxiety, depression, and suppressed anger can also affect the body’s immune system and circadian rhythms16. Research has also found that varying degrees of fears, such as worries, anxieties, and fears of death, can have a negative impact on the disease, hindering patients from seeking help17. Existing studies predominantly analyze how negative emotions hinder patients’ mechanisms, impeding disease treatment. The greater the extent of negative emotions, the more difficult it is for patients to comply with treatment, potentially leading to poor treatment outcomes18,19. Conversely, positive emotions contribute to the release of positive hormones like dopamine, β-endorphin, fostering higher-level positive emotions from a neurobiological perspective20. Positive emotions also initiate beneficial changes in thoughts and behaviors21. These emotions provide increased mental energy, enhance hormone secretion aiding cellular repair, reduce cortisol and adrenaline secretion associated with negative emotions, potentially lowering cancer incidence. Dr. Diana Fosha’s research suggests that positive emotions can enhance individuals’ resilience and vitality, reducing fear and shame when facing illness and encouraging a more proactive approach to treatment22. To improve the quality of life and reduce mortality among cancer patients, it is imperative to identify and treat depression in this population23, thereby accelerating treatment progress. In summary, the emotional state of cancer patients significantly impacts the course of their illness. Negative emotions such as anxiety, depression, and fear can weaken immune function, interfere with treatment, and increase the risk of disease recurrence. In contrast, positive emotions help activate neurobiological mechanisms, enhance resilience, and improve treatment outcomes. Therefore, effectively managing patients’ emotions and maintaining their psychological well-being are crucial for the success of cancer treatment.
Applications of virtual reality (VR) in the medical field
The application of VR in the medical domain has made significant progress24. Initially stemming from VR exposure therapy, VR therapy immerses patients in virtual environments to achieve exposure scenarios without actual harm. Presently, VR exhibits innovative applications in medical contexts, notably in medical training and simulated surgery, intervention therapy, disease diagnosis, and medical rehabilitation, forming four major domains. In medical training and simulated surgery, VR utilizes its interactivity and autonomy for detailed simulation based on virtual imaging. This technology precisely replicates various organ structures, from skin to deep bones, allowing medical scholars to study from life-like contexts25. Additionally, doctors can repetitively practice unfamiliar surgical steps, enhancing practical skills, thus boosting surgery success rates and safety26, thereby lowering initial training costs27. In intervention therapy, VR projects images and sounds to patients, achieving deep immersion, potentially blocking stimuli from competitive environments, becoming a more effective method than other intervention measures28-29. Successful VR distraction interventions require attention capture, enabling goal-oriented interventions30, heightening treatment enjoyment and efficacy31. In disease diagnosis, VR technology, through a three-dimensional perspective, aids doctors in observing and diagnosing patients’ internal brain structures and causes. Utilizing 3D virtual environments to navigate distinct brain regions combined with magnetic resonance imaging monitoring enables precise assessment of alterations in brain areas corresponding to different diseases, such as pinpointing specific neural systems within the human hippocampal system32. In medical rehabilitation, VR primarily addresses neural disorders, including dementia, stroke, Parkinson’s disease, and limb pain. Research demonstrates the substantial efficacy of VR rehabilitation for these conditions33. Compared to traditional approaches, VR maintains realism and entertainment in rehabilitation training34. It tailors training scenarios and tasks according to patients’ psychological states and treatment needs, offering real-time physiological and psychological feedback, motivating proactive engagement and achieving effects unattainable through conventional methods35. Evidently, VR’s extensive application in the medical field underscores its immense potential. VR technology empowers the medical domain to achieve training, treatment, disease diagnosis, and rehabilitation goals, providing more precise and effective medical and rehabilitation solutions for patients.
VR and emotion regulation
In today’s rapidly developing economy, the fast-paced nature of life and increasing societal pressures have led a significant number of individuals into a state of suboptimal health, often accompanied by negative emotions such as depression and anxiety. These emotional issues further elevate the risk of developing psychological disorders, including anxiety disorders, autism, and depression36. Research has shown that emotional fluctuations not only affect an individual’s psychological state but can also have profound impacts on physical health, with prolonged exposure to negative emotions significantly increasing the risk of illness. Consequently, effectively regulating emotions and preventing mental disorders has become a key research focus.
In recent years, digital interventions—including VR, augmented reality, internet-based therapies, and digital games—have demonstrated immense potential in emotional regulation and mental health interventions37,38,39. Among these, VR has been particularly prominent in treating anxiety disorders and regulating emotions, with empirical evidence confirming its ability to effectively reduce subjective anxiety levels and modulate physiological indicators40,41. As an emerging digital psychological intervention tool, VR provides immersive and interactive experiences, allowing individuals to express and regulate emotions in a safe and controlled environment. This, in turn, alleviates psychological distress and reduces the risk of mental disorders42. Further research by Wagener et al. suggests that VR can offer users a secure emotional expression space, enabling them to engage more deeply with their emotions, ultimately leading to relaxation and emotional recovery43. Moreover, VR can naturally evoke emotions through mechanisms such as motivation and empathy37 while also facilitating relaxation through the creation of specific scenarios or promoting emotional release through engaging interactive activities. Within virtual environments, individuals can channel their emotions in a positive manner, receiving constructive feedback that helps reduce both physiological and emotional stress44. Studies have shown that VR interventions effectively alleviate anxiety and depression, improve sleep quality, and enhance individuals’ emotional regulation abilities45. Additionally, VR offers a range of immersive gaming experiences that not only help mitigate negative emotions but also enhance self-efficacy, improving individuals’ emotional regulation and stress management skills46.
With advancements in VR technology, including higher-quality devices, reduced costs, and optimized user experiences, wearable biosensors are increasingly being integrated into VR applications. These integrations have gained widespread attention in fields such as psychology, medicine, and human–computer interaction47. As a result, the combination of VR and biofeedback systems has become a research hotspot. For instance, integrating biofeedback systems with VR-based intervention games has been shown to effectively help individuals manage stress and anxiety39. Overall, VR leverages multi-sensory interactions to regulate users’ behaviors, emotions, and cognition, making it adaptable to various functional needs and application scenarios throughout the entire user experience48. Beyond that, VR provides a secure space for emotional expression and, when combined with gaming and biofeedback systems, supports individuals in coping with stress and anxiety, enhancing self-efficacy, and improving mental well-being. Ultimately, VR serves as a promising tool for emotional regulation and mental health promotion.
VR Interventions for emotion regulation in cancer patients
VR technology is a novel form of adjunctive psychological therapy that has garnered attention for its significant efficacy in conditions such as anxiety and phobias14. Across various medical procedures, VR has proven to be an effective attention diversion tool49. Research indicates that VR technology, during chemotherapy and surgical processes for cancer patients, successfully mitigates anxiety and pain perception by shifting focus50. Furthermore, VR enables inpatients to experience a diversified life within a hospital setting, encompassing learning and entertainment, thus alleviating social disconnection stemming from prolonged activity limitations51. This, in turn, improves patients’ social skills, enhances quality of life, and mitigates negative emotions such as depression41.In the complex landscape of cancer treatment, adverse reactions can lead to treatment interruptions. Therefore, early psychological interventions play a crucial role in enhancing treatment tolerance. In interventions designed to improve treatment tolerance, attention diversion is considered one of the most promising strategies. Research reveals that VR interventions during cancer patients’ treatment processes significantly reduce negative emotions and feelings of anxiety. Attention diversion strategies encompass avoidance, minimization, distancing, and selective attention, all aimed at finding positive value within negative events, thus reducing stress and anxiety52. In another study, VR technology interventions assist cancer patients in acquiring knowledge related to the disease, surgery, and rehabilitation, thus alleviating psychological anxiety and preparing patients mentally for the treatment process53,54. In recent years, an increasing number of studies have integrated VR technology into this approach. For instance, Jimenez et al.'s study indicates that VR assists cancer patients in acquiring relevant knowledge and effectively reducing anxiety levels55. Additionally, some studies utilize VR’s natural scenes to guide cancer patients toward positive emotions28. Mohammad & Ahmad demonstrated that VR can alleviate pain and anxiety in breast cancer patients56, providing an effective method for emotional regulation in cancer patients. In conclusion, VR technology plays a positive role in emotion regulation among cancer patients. It not only alleviates negative emotions such as anxiety and fear but also aids patients in acquiring relevant knowledge, enhancing treatment tolerance, and improving their quality of life57. Through VR technology, cancer patients can better cope with the pressures and anxieties of the treatment process, leading to significant benefits in both psychological and physiological aspects.
Technology acceptance of VR interventions in healthcare
The rapid development of VR technology has improved people’s quality of life and has been applied in various fields. In the field of healthcare, the application of VR technology mainly encompasses patient treatment and medical personnel training58. However, despite the increasing popularity of VR technology, there are still many people unfamiliar with this concept. Additionally, VR technology is primarily applied in relatively niche areas of healthcare, leading to a slower adoption rate in medical settings. Many studies are limited to small-scale experimental research, and large-scale acceptance surveys are relatively rare. Moreover, many patients feel fear and concern about VR technology, which may result in their reluctance to participate in related trials59. In situations where patients are unfamiliar with VR technology, when doctors propose using this technology for treatment, many patients may refuse to accept it. This resistance is particularly evident among the elderly population who tend to resist new technologies. Therefore, researchers and clinical practitioners need to carefully consider the acceptance level of the target user group when promoting the use of VR technology in intervention treatments108. For instance, a study conducted in Taiwan involving 30 elderly participants demonstrated that VR technology is perceived as having significant value in health and medical applications by the elderly97. In another study regarding VR exposure therapy, with a sample of 15 participants, the intervention was highly satisfactory, with an 87% satisfaction rate60. Furthermore, a study simulating dementia experiences using VR technology indicated that the majority of participants had a positive attitude towards the experiment, believing that VR technology could help them better understand patients and increase confidence in caregiving tasks61. In summary, the current acceptance studies of VR intervention in healthcare are mostly limited to small-scale populations, and the study participants often come from the same region, lacking diverse geographical data support. However, when combined with existing literature reviews, participants generally exhibit a favorable acceptance of VR intervention in medical settings.
Technology acceptance model (TAM) and VR technology adoption
Through literature exploration, we have come to understand that the application of VR technology can effectively regulate the emotions of cancer patients. The acceptance level of cancer patients towards the intervention of VR technology in self-emotion regulation directly influences the application of VR technology in this field. To gain a deeper understanding of the acceptance level of cancer patients towards the intervention of VR technology in self-emotion regulation, this study draws on the Technology Acceptance Model (TAM) proposed by Davis. The model primarily consists of four core constructs: Perceived Usefulness (PU), Perceived Ease of Use (PEOU), Attitude towards Using (AT), and Behavioral Intention to Use (BI)62. Over time, Davis and others revised the TAM in 1993 and 1996. Subsequently, Venkatesh and Davis introduced TAM293, while Venkatesh et al. proposed the Unified Theory of Acceptance and Use of Technology (UTAUT)63, Lin introduced the Technology Readiness and Acceptance Model (TRAM)64, Venkatesh and Bala proposed TAM365, and Venkatesh et al. introduced UTAUT266. Today, the TAM model has become one of the most widely applied models and has been extensively validated in the field of technology acceptance, making it one of the influential and comprehensible theoretical models in the domain of information technology acceptance.
While the TAM model is a frequently used model for studying technology acceptance and has identified key factors, numerous external factors still need to be considered. Many researchers have expanded upon the original TAM67. Wixom and Todd summarized three main approaches for expanding the TAM, including relevant model variables (such as subjective norms, perceived behavioral control, etc.), other construct variables (such as compatibility, visibility, etc.), and external variables (such as personality traits, demographic characteristics, etc.). Analyzing 88 empirical studies on TAM, King found that most studies expanded upon the TAM model68, focusing on four main categories: prior factors (e.g., usage experience, self-efficacy), other theoretical factors (e.g., subjective norms, expectations, risk), contextual factors (e.g., gender, education, technical characteristics), and leading factors (e.g., affective use, actual usage)24. These studies indicate that the current extensions of the TAM primarily focus on "user characteristics," "product influence factors," and "social environmental influence factors."
VR technology has been widely applied across various fields69. Research on user acceptance of VR technology has also emerged as a critical area of study. Acceptance research helps determine whether users are willing to adopt VR and identifies the factors influencing their acceptance. Such insights provide a foundation for user-centered VR device design and development, as well as strategic guidance for manufacturers and retailers in production and marketing. In recent years, increasing attention has been given to VR acceptance across different domains, with research primarily focusing on healthcare70,71,72,73,74, education and training 75,76,77,78,114, entertainment and gaming79,80,81,82,83, marketing and promotion84, as well as social interaction and life support85. However, most of these studies primarily focus on completed application86 or overall VR acceptance87,122, with some proposing specific research models88.
When addressing patients with disorders where emotional distress is a primary symptom, VR technology has been introduced as an intervention tool to guide treatment, helping patients gradually alleviate negative emotions and shift their affective and perceptual states in a positive direction. However, despite its potential benefits, numerous barriers hinder the adoption of VR technology among cancer patients in practice. To date, little research has explored cancer patients’ acceptance of VR for emotional regulation from their perspective, nor has there been a comprehensive examination of the factors influencing their willingness to adopt such technology.
Theoretical models and research hypotheses
TAM for cancer patients’ acceptance of VR interventions in self-emotion regulation
Studies have shown that many scholars tend to extend the TAM model89, incorporating VR technology’s application in different fields, populations, or its own characteristics as external factors. Therefore, building upon an in-depth review of relevant literature on the acceptance of VR technology, this study constructs a TAM tailored for cancer patients’ acceptance of VR technology intervention in self-emotion regulation. The foundation of this model is the original TAM, while also integrating the three pathways of TAM extension: "User Characteristics," "Product-Related Factors," and "Social Environmental Influences." In this TAM based on the TAM framework, three user characteristic factors are introduced: self-efficacy, technology anxiety, and personal innovativeness. Simultaneously, five product-related factors are incorporated, encompassing performance expectations, user experience, immersion, perceived enjoyment, and perceived risk. Furthermore, a single social environmental factor, social norms, is considered. Constructing the TAM for cancer patients’ acceptance of VR technology intervention in self-emotion regulation, the TAM serves as the starting point, incorporating prior extension research and the application of VR technology in the medical domain. This model takes into account factors from diverse domains, aiming to comprehensively explain the extent of acceptance of VR technology among cancer patients.
Original TAM framework
During the period from 1975 to 1980, Ajzen and Fishbein introduced the Theory of Reasoned Action (TRA) for analyzing the influence of individuals’ self-will on behavior. This theory elucidated how attitudes consciously guide individual behavior90. Between 1985 and 1991, Ajzen further refined the TRA and proposed the Theory of Planned Behavior (TPB). This theory emphasized the impact of perceived risks on behavioral intentions. Individuals typically consider behavioral risk factors in decision-making, making perceived risk one of the key components of this model91. To date, the most widely applied model in the field of technology acceptance is the TAM proposed by Bagozzi, Davis, and others. Built upon the foundations of TRA and TPB, this model has been extensively used by researchers to explore users’ acceptance of new technologies92. In this study, we based our research on the TAM as formulated by Davis (1989) and constructed a TAM concerning cancer patients’ acceptance of VR technology for self-emotion regulation intervention. Within this model, the core framework consists of four dimensions: perceived ease of use, perceived usefulness, attitude toward use, and behavioral intention. Among these dimensions, perceived ease of use and perceived usefulness are the primary factors affecting attitude toward use and behavioral intention. Additionally, societal factors such as users’ understanding of technology may influence attitude toward use and behavioral intention. Consequently, building upon the original TAM framework, we introduced factors related to cancer patients’ acceptance of VR technology for self-emotion regulation intervention. This model aims to objectively demonstrate how internal perceptions of cancer patients impact their utilization of VR technology, facilitating the inference of their acceptance and intention to use the technology based on these attitudes. Building upon the foundation of the original TAM, we propose the following hypotheses.
H1
There is a significant positive correlation between Perceived Ease of Use (PEOU) and Perceived Usefulness (PU).
H2
There is a significant positive correlation between Perceived Ease of Use (PEOU) and Attitude towards Use (ATT).
H3
There is a significant positive correlation between Perceived Usefulness (PU) and Attitude towards Use (ATT).
H4
There is a significant positive correlation between Perceived Usefulness (PU) and Behavioral Intention (BI).
H5
There is a significant positive correlation between Attitude towards Use (ATT) and Behavioral Intention (BI).
Perceived enjoyment
In the continuous evolution of VR technology, the significance of sensory experiences obtained from the virtual world has become increasingly prominent. This has consistently been one of the goals pursued in the field of VR. Therefore, perceived enjoyment is defined as the degree of pleasure felt when using information technology93, and it holds a significant position in technology acceptance research94. In many studies related to VR technology, perceived enjoyment is introduced as a key element within the TAM model. This aspect is also affirmed in Hsiao et al.'s analysis of the TAM model, which demonstrates that perceived enjoyment significantly influences perceived usefulness and attitude towards use95. During individuals’ utilization of VR devices, the simulated environment provided by the device as well as the sensory feedback generated by the device itself greatly impact the sense of enjoyment. High levels of perceived enjoyment enhance the pleasure of the interaction process, leading to a more satisfying experience96. Consequently, this factor becomes one of the crucial determinants affecting users’ willingness to use VR devices94. Based on the aforementioned discourse, we propose the following hypotheses.
H6
There is a significant positive correlation between Perceived Enjoyment (PE) and Attitude towards Use (ATT).
User experience
For individuals who have personally experienced VR devices, various feedback is generated among different people. Some individuals might focus on the physical discomfort caused by VR devices, while others may be intrigued by the novel experiences facilitated by these devices. This subjective perception formed by users before, during, and after using VR devices is considered as user experience97. In the field of VR technology, efforts are consistently made to enhance user experience through various components, such as the emphasis on presence, immersion, and engagement that VR emphasizes98. More dynamic forms of human–computer interaction also pose greater challenges to users. Certain studies underscore the importance of achieving a favorable user experience in devices like VR99. A high-quality user experience can enhance the efficiency of users during the usage process.Based on the aforementioned perspectives, we propose the following hypotheses.
H7
There is a significant positive correlation between User Experience (UE) and Perceived Usefulness (PU).
Self-efficacy
Since Bandura introduced the concept of self-efficacy in 1977, this concept has been interpreted as an individual’s assessment of their capabilities, ultimately influencing their self-regulation system. Self-efficacy is a pattern of judgments individuals make about their ability to achieve desired outcomes100. Within the concept of self-efficacy, individual recognition of their own capabilities is particularly crucial101. Some studies indicate that individuals with high self-efficacy tend to exhibit higher efficiency102. In the realm of VR, self-efficacy refers to users’ confidence in being able to operate VR systems adeptly without external guidance103. In such cases, users with high self-efficacy are better positioned to quickly grasp the usage methods of VR devices. In research involving the application of VR devices to the treatment of cancer patients, some researchers have found that as patients’ self-efficacy increases, they are more likely to persist in exercising during the rehabilitation process, thereby achieving better treatment outcomes and achievements104. Based on this, we propose the following hypothesis.
H8
There is a significant positive correlation between Self-Efficacy (SE) and Perceived Usefulness (PU).
Performance expectancy
In introducing VR devices into the emotional therapy of cancer patients, the performance of the device or system meeting expected standards is a crucial factor. Performance here refers to the consistency of the system or component with its temporal requirements. In the study by Samaneh et al., they validated different performance criteria for devices used in cancer patient treatment, leading to a more objective model105. Abdulrahman et al.'s research involved validating device learning techniques through performance algorithms to determine metric outcomes, further developing proficiency performance benchmarks and applying them to the design of virtual devices106. When the device’s performance can meet expected standards and exhibits superiority in performance aspects, users will be more efficient in completing tasks. Thus, we propose the following hypothesis.
H9
There is a significant positive correlation between Perceived Performance (CP) and Perceived Usefulness (PU).
Understanding of VR technology
When people make product choices, they often tend to favor products they are more familiar with. When you have a comprehensive understanding of a particular product, you feel more confident and willing to use it compared to products that are relatively unfamiliar. In Gibson’s research, survey participants are also asked if they have previously used VR technology107. However, conducting surveys without providing information and usage instructions for the product may lead to users having negative attitudes toward the product108. In a study on how to apply VR devices to childhood cancer treatment, Remerci et al.'s research suggests that providing parents with a detailed explanation of the definition, research purpose, and methods of VR devices can reassure them and make them willing to involve their children in treatment109. Understanding VR technology and relevant product information is crucial for promoting people’s acceptance and use of VR technology. Hence, we formulate the following hypothesis.
H10
There is a significant positive correlation between Understanding of VR (UOVR) and Attitude towards Use (ATT).
Technological anxiety
When using advanced intelligent products such as VR devices, users often have concerns about whether they are operating the technology correctly due to its unfamiliarity and potential anxieties. They worry that improper use might lead to prolonged immersion in the virtual world, resulting in adverse physical effects59. This apprehension can lead to hesitation or even refusal to use related devices like VR59. In Philip et al.'s study, many participants also expressed complaints about technical issues, including device malfunctions, overheating, and software crashes110. The worry about potential negative consequences of technology operation can lead users to doubt the use of VR devices. This further emphasizes the importance of providing a positive user experience as well as effective technical support and solutions to alleviate users’ concerns and hesitations when using VR devices. Hence, we formulate the following hypothesis.
H11
There is a significant negative correlation between Technological Anxiety (TA) and Behavioral Intention (BI).
Perceived risk
In modern society, the rapid advancement of technology has led people to place greater emphasis on the quality and performance of products when making choices about their use. When deciding whether to use VR devices, individuals often express concerns about the varying quality of these devices and potential adverse effects on their bodies. A series of concerns may lead some individuals to perceive the use of VR devices as problematic, thereby making them reluctant to use them111, such as high costs, privacy breaches, content quality, and feelings of pressure112. A study involving two groups, older adults and students, aimed to explore their different perspectives on VR. The results indicated that both groups reported physical discomfort, with the older adults potentially experiencing more pronounced physical discomfort. Meanwhile, the student group was more concerned about device comfort and content quality. Some VR devices might even evoke concerns of claustrophobia, making users perceive the devices as expensive and thus exacerbating reservations about their usage113. These concerns underscore the need, in the promotion of VR technology, to focus not only on enhancing technological performance but also on user experience, device quality, and addressing users’ health and comfort considerations. This leads us to formulate the following hypothesis.
H12
There is a significant negative correlation between Perceived Risk (PR) and Behavioral Intention (BI).
Social norms
Social norms have a significant influence on individuals’ behavioral intentions114. Choices made by governments, friends, and family members can all play a crucial role in shaping an individual’s usage of a particular technology115. When institutions such as society, media, and hospitals intensify their promotion of VR devices, these influences can shape the public’s attitude towards VR technology, triggering conformity or curiosity, thereby making them more likely to choose to use VR devices116. In daily life, social norms intertwine various practices individuals engage in and strongly impact their subjective decisions117. The impact of these social norms suggests that when promoting VR technology, in addition to considering the advantages of the technology itself, attention needs to be given to the influence of social and environmental factors on individuals. Support from government and social institutions, recommendations from friends and family, and media coverage can all have a positive impact on an individual’s choice to use VR devices. Therefore, establishing a positive social environment, reinforcing positive perceptions and acceptance of VR technology, can facilitate its widespread adoption. This leads us to formulate the following hypothesis.
H13
There is a significant positive correlation between Social Norms (SN) and Behavioral Intention (BI).
Immersion
One of the key features of VR technology is its powerful immersive nature, which allows users to feel like they are truly present in a different environment. In the context of using VR technology to assist cancer patients with emotional regulation, the immersive characteristic plays a significant supportive role. It can help cancer patients divert their attention and alleviate their mental and even physical distress118, enabling them to immerse themselves in various virtual environments and temporarily escape the challenges of their current reality119. According to interviews conducted by Devon et al., many users seek the immersive experiences brought about by VR technology. They find that using VR devices enables them to be 100% focused, making them less likely to be distracted compared to other smart devices such as televisions and smartphones120. This immersive experience can provide cancer patients with a temporary respite from the harsh realities they face, helping them cope better with the emotional challenges of their treatment process. Therefore, the immersive nature of VR technology plays a crucial role in emotional regulation for cancer patients. This leads us to formulate the following hypothesis.
H14
There is a significant positive correlation between Immersion (IVE) and Behavioral Intention (BI).
Personal innovativeness
Across various social groups, each individual holds unique viewpoints and perspectives regarding VR devices. The diversity of opinions among individuals is influenced by the information they are exposed to, and the breadth of knowledge they have accumulated also affects their choices regarding VR devices. Groups with a high sense of innovation are generally more inclined to embrace technological advancements. They are more willing to try new smart products and provide imaginative personal insights when experiencing VR products, which can help improve the functionality and performance of the products121. In the study by Sagnier et al., it is also indicated that an individual’s sense of innovation can impact their acceptance of new technologies, with highly innovative individuals being more willing to try new technologies122. An individual’s sense of innovation significantly influences their intention to use VR technology. Research by Kim et al. found that individuals with higher technological readiness, indicating a stronger sense of innovation, have a more significant intention to use VR technology123. This suggests that there is a certain correlation between an individual’s sense of innovation and their acceptance of VR technology. People with a high sense of innovation are more likely to hold an open attitude towards VR technology and are willing to actively explore and use these new technologies124. Based on this, we propose the following hypothesis.
H15
There is a significant positive correlation between Personal Innovativeness (PI) and Behavioral Intention (BI).
Research hypothesis path
This study conducted an extensive literature review and combined the explanatory power of the original TAM model and its extended versions to expand the model from three dimensions: "User Characteristics," "Product Influencing Factors," and "Social Environmental Influencing Factors." Based on this foundation, a TAM for cancer patients’ engagement with VR technology in self-emotional regulation was constructed. Fifteen hypotheses (H1–H15) were proposed to describe the relationships between various factors within the model, as depicted in Fig. 1. The construction of this model aims to comprehensively analyze the acceptance of VR technology among cancer patients, considering the influence of individual characteristics, product factors, and social environmental factors on the intention to accept the technology. Through exploring the interrelationships among these factors, this study aims to gain a deeper understanding of cancer patients’ attitudes and intentions towards the use of VR technology for emotional regulation.
Methods
Research design
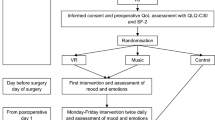
The study titled “Acceptance of VR Intervention for Self-Emotion Regulation Among Cancer Patients” aims to examine cancer patients’ willingness to adopt VR technology for emotional regulation during treatment, considering various influencing factors. The primary objective is to assess the feasibility of implementing VR technology among cancer patients in China. To achieve this, we employed the TAM to evaluate the extent to which cancer patients in China are receptive to VR-based emotional regulation interventions. This study was conducted in three main phases, as illustrated in Fig. 2.
Phase 1: Literature Review and Data Integration. In the first phase of this study, we will conduct an extensive literature review and data integration. Relevant literature aligned with or related to our research focus will be collected, from which key concepts and essential content will be extracted. These core elements will be further refined to identify key terms and factors, which will serve as multidimensional variables in constructing the virtual reality technology acceptance model in the third section of the questionnaire. The objective of this phase is to ensure that the questionnaire encompasses critical variables and enhances its reliability.
Phase 2: Questionnaire Survey. During the second phase, building upon the literature review and organization from the previous steps, and considering the specific characteristics and adjustments to the structural model of the research, a more comprehensive and relevant questionnaire will be designed. This questionnaire will include the keywords and elements extracted from the literature, as well as other factors related to the acceptance of VR technology. An expert panel meeting will be conducted to evaluate and refine the questionnaire, ensuring its content validity and feasibility. The revised questionnaire will be distributed to participants in an offline (paper-based) format, inviting them to complete the survey.
Phase 3: Data Statistical Analysis. In the third phase, data statistical analysis will be conducted. We will utilize statistical analysis software such as SPSS 26.00 and Amos to analyze the collected questionnaire data. Feasibility of the data from the questionnaire will be calculated, including relationships between variables and the extent of influence. Through analyzing this data, we will derive conclusions from the questionnaire survey regarding the acceptance of VR technology. Our research hypotheses will be validated.
By designing these three phases, our study aims to comprehensively explore the acceptance of VR technology for emotional regulation among cancer patients. We will construct a more complete and accurate model, enhancing the credibility and practicality of the research findings.
Questionnaire design
To ensure the scientific rigor, rationality, and clarity of the questionnaire, we invited a panel of eight scholars, researchers, and practitioners from relevant fields to form a questionnaire evaluation committee. An expert panel meeting was conducted to ensure a comprehensive and professional assessment. The meeting followed a structured process consisting of several key stages: First, the moderator introduced the background, objectives, and design rationale of the study, emphasizing the core variables to be measured and their theoretical foundations. Next, the expert panel members systematically reviewed the questionnaire, focusing on the following critical aspects: (1) Do the questionnaire items effectively measure the research objectives? (2) Are the questions clearly and concisely worded, ensuring comprehension by the general public? (3) Are the response options reasonable and sufficiently inclusive of all possible answers? (4) Are there any potential ambiguities or implicit biases in the wording? (5) Is the overall structure of the questionnaire coherent, with a clear logical flow? After an in-depth discussion, the expert panel proposed revisions to the questionnaire and reached a consensus on the necessary modifications.
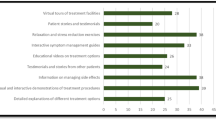
Based on expert feedback, we revised and refined the questionnaire to enhance the quality of data collection and the reliability of research findings. Ultimately, the questionnaire for this study is divided into two main sections. The first part focuses on eight personal factors of cancer patients, including gender, age, education level, living area, monthly income, occupation, treatment stage, and familiarity with VR. The second part aims to assess thirteen variable factors related to the acceptance of VR technology among cancer patients. These factors include Perceived Usefulness (PU), Perceived Ease of Use (PEOU), Attitude (ATT), Behavioral Intention (BI), Compatibility (CP), Self-Efficacy (SE), Technological Anxiety (TA), User Experience (UE), Immersiveness (IVE), Social Norm (SN), Perceived Enjoyment (PE), Personal Innovation (PI), and Perceived Risk (PR). The entire questionnaire consists of 51 items, covering detailed variable factors and related questions, as outlined in Table 1. In the questionnaire, all items use a 5-point Likert scale, where 1 represents "Strongly Disagree," 2 represents "Disagree," 3 represents "Neutral," 4 represents "Agree," and 5 represents "Strongly Agree." Respondents are required to rate each item within every construct, quantitatively assessing their attitudes and opinions. Through this design, the study will comprehensively examine various aspects of cancer patients’ acceptance of VR technology, including both personal and variable factors. This approach will lead to more in-depth and accurate research results.
Description of VR video playback
During the process of conducting the questionnaire survey, in order to assist cancer patients who may not be familiar with the concept of VR to better understand, we have included three educational videos related to VR in the questionnaire. The purpose of these videos is to help respondents gain a clearer understanding of VR technology and its applications. The first video is a short educational clip with a duration of only 53 s. It primarily aims to explain the definition, historical development, and application areas of VR. The second video, sourced from Science Popularization China, vividly presents the immersive feeling that VR technology brings. This video further introduces the applications of VR in various fields and its impacts on these fields. The third video is focused on showcasing the VR experience from a third-person perspective. This video depicts the user’s state within the VR environment and their viewpoint within the virtual world. Through this video, respondents can gain a more comprehensive understanding of VR technology. The inclusion of these videos aims to eliminate any potential barriers due to a lack of understanding of the concept of VR. This way, cancer patients can better comprehend VR technology and its application in emotional regulation. Consequently, they can participate in the questionnaire survey more accurately and confidently.
Data collection
The questionnaire survey primarily adopted an offline (paper-based) distribution approach, conducted from October 2, 2021, to June 25, 2023. The respondents consisted of Chinese cancer patients at different stages of treatment. Prior to the survey’s commencement, we obtained consent from the respective hospital administrators and established contact with them to assist in identifying suitable participants. These administrators also aided the respondents in understanding and filling out the questionnaire, ensuring the smooth progress of the survey. Recognizing that some respondents might not be familiar with the concept of VR, we specifically included three educational videos introducing VR technology to help them better comprehend the questionnaire’s content. We also offered assistance for questionnaire completion in special cases. Throughout the survey, we ensured that all respondents were well-informed about the research’s purpose. As a token of appreciation and care, we provided a small gift to respondents upon completing the questionnaire. In total, we collected 503 questionnaires during the survey process. Among these, 14 questionnaires were considered invalid, leaving 489 questionnaires as valid. Among the valid questionnaires, there were 272 from male respondents and 217 from female respondents. These data serve as the foundation for our research, enabling further analysis and study of cancer patients’ acceptance of VR technology for emotional regulation intervention.
Ethical approval and consent to participate
This study obtained approval and support from the Ethics Committee of Xiangtan Central Hospital (approval no. 2021–02-01). All participants voluntarily participated and provided written informed consent. All experiments were conducted in accordance with relevant guidelines and regulations.
Handling of missing data
After collecting the survey questionnaires, we initially conducted screening and sorting of the questionnaires. According to the requirements of this study, we excluded some questionnaires that did not meet the criteria. During this process, it was discovered that 7 questionnaires did not fill in the treatment stage, so we couldn’t ascertain whether these questionnaires were completed by cancer patients. Subsequently, during the process of organizing the questionnaires, it was found that 3 questionnaires only filled out the first page of personal information, and 4 questionnaires were missing information from some pages. Based on our preliminary observation, the proportion of non-random missing values in the entire dataset did not exceed ten percent, allowing us to assume that these missing values were completely random129. To further validate this, we conducted an independent variance t-test analysis to examine whether the missing value pattern influenced other variables. Additionally, we conducted an EM correlation test to verify the accuracy of the independent variance t-test.
Upon integrating the data, we utilized the EM algorithm in SPSS 26.00130 to validate the missing value pattern of the 8 personal factor variables (gender, age, education level, living area, monthly income, occupation, treatment stage, understanding of VR. Since there were no variables with missing value percentages exceeding 5%, an independent variance t-test table for missing data could not be generated. Likewise, indicator variables with missing percentages below 5% were not displayed in the missing value analysis. Based on these analyses, we can infer that these missing values belong to the category of completely random missing values. Subsequently, we conducted further EM correlation testing and performed the Little’s MCAR test131. In this test, the chi-square value was 9.444, and the significance was 0.802, far greater than 0.05, indicating that the missing values were of the completely random missing type. Therefore, the MCAR assumption is valid, meaning that these missing values are missing independently of other data. Given these results, we employed listwise deletion to handle the missing data in subsequent data analysis, without concern for estimation bias, as this will yield unbiased estimates. Detailed analysis results can be found in Table 2.
Data analysis
In the data analysis and processing section of this study, we primarily utilized IBM SPSS Statistics 26.0 and Amos software. Depending on the research objectives, we selected different data analysis methods and tools. For the demographic information section, we employed descriptive statistics methods. In the model evaluation section, we used the structural equation modeling (SEM) modeling tool Amos to construct the model. We measured the significance of variables through factor loading coefficients and screened out unreasonable measurement items. Subsequently, we conducted model evaluation, analyzing the factor loading of measurement indicators based on the average variance extracted and composite reliability results. Finally, we performed analysis and summarization. In the acceptance analysis section, we first calculated the average scores for each construct in the questionnaire (average score for each construct = sum of average scores of individual items / number of items). Then, we performed descriptive statistics and reliability analysis on the questionnaire, with descriptive statistics including mean, median, range, and standard deviation. Given the relatively small sample size of this study, we also employed non-parametric statistical methods, specifically the Wilcoxon’s Sign Rank Test, to analyze the data. We compared the average score of each construct with the median score of 3, where 3 represents an uncertain or neutral attitude. Overall, during the data analysis process, we applied various quantitative analysis methods to comprehensively and accurately assess the acceptance of VR technology intervention for emotional regulation in cancer patients.
Analysis of questionnaire validity
After excluding invalid questionnaires, we conducted the analysis using IBM SPSS Statistics 26. First, we calculated the reliability of the questionnaire, indicated by Cronbach’s alpha values. The results revealed that the Cronbach’s alpha value for all constructs was 0.938, and each construct’s Cronbach’s alpha value exceeded the threshold of 0.7. This indicates a high reliability of the questionnaire, effectively measuring the involved constructs. The scores for each construct are detailed in Table 3.
Results
Participants
A total of 489 valid questionnaires were collected for this study. In terms of socio-demographics, there were 272 males (accounting for 55.6% of the total participants) and 217 females (accounting for 44.4% of the total participants), with a slightly higher proportion of males. The age distribution was primarily centered between 45 and 59 years, with 17 participants aged 75 and above (accounting for 3.4% of the total participants), 122 participants aged 60–74 (accounting for 24.9% of the total participants), 166 participants aged 45–59 (accounting for 33.9% of the total participants), 94 participants aged 30 to 44 (accounting for 19.2% of the total participants), and 90 participants aged 29 and below (accounting for 18.4% of the total participants). The proportion of young and middle-aged individuals was relatively low. Regarding educational levels, the distribution of participants’ education was as follows: 60 participants with primary education or below (accounting for 12.3% of the total participants), 119 participants with junior high school education (accounting for 24.3% of the total participants), 147 participants with high school or vocational school education (accounting for 30.1% of the total participants), 156 participants with college or associate degree education (accounting for 31.9% of the total participants), and 7 participants with graduate or higher education (accounting for 1.4% of the total participants). In terms of living area, 305 participants lived in urban areas (accounting for 62.4% of the total participants), while 184 participants lived in rural areas (accounting for 37.6% of the total participants). The distribution of monthly income was as follows: 41 participants earned less than 1000 RMB (accounting for 8.4% of the total participants), 164 participants earned between 1001 and 3000 RMB (accounting for 33.5% of the total participants), 167 participants earned between 3001 and 5000 RMB (accounting for 34.2% of the total participants), 78 participants earned between 5001 and 8000 RMB (accounting for 16% of the total participants), 23 participants earned between 8001 and 12,000 RMB (accounting for 4.7% of the total participants), 7 participants earned between 12,001 and 18,000 RMB (accounting for 1.4% of the total participants), and 9 participants earned above 18,000 RMB (accounting for 1.8% of the total participants). Regarding occupation, participants were distributed across various occupations: 32 students (accounting for 6.5% of the total participants), 21 office workers and related staff (accounting for 4.3% of the total participants), 120 individuals engaged in agriculture, forestry, animal husbandry, fishing, and water conservancy (accounting for 24.5% of the total participants), 38 individuals in government agencies, enterprises, and institutions (accounting for 7.8% of the total participants), 90 individuals in commerce and service industry (accounting for 18.4% of the total participants), 32 individuals in production and transportation equipment operation (accounting for 6.5% of the total participants), 41 individuals in professional and technical roles (accounting for 8.4% of the total participants), 0 individuals in the military (0% of the total participants), and 115 individuals in other industries (accounting for 23.5% of the total participants). In terms of treatment stages, participants were distributed across different treatment stages: 123 participants were in the first stage of treatment (initial treatment phase) (accounting for 25.2% of the total participants), 273 participants were in the second stage (maintenance treatment phase) (accounting for 55.8% of the total participants), 45 participants were in the third stage (treatment gap phase) (accounting for 9.2% of the total participants), and 48 participants were in the fourth stage (relapse treatment phase) (accounting for 9.8% of the total participants). Participants’ understanding of VR technology was distributed as follows: 43 participants had a “very understanding” level (accounting for 8.8% of the total participants), 103 participants had an “understanding” level (accounting for 21.1% of the total participants), 152 participants had a “neutral” attitude (accounting for 31.1% of the total participants), 125 participants had a “not understanding” level (accounting for 25.6% of the total participants), and 66 participants had a "completely not understanding" level (accounting for 13.5% of the total participants).
Model evaluation results
To assess the construct validity of the scale, this study employed confirmatory factor analysis (CFA) using SPSS AMOS software. The primary purpose of CFA is to evaluate the convergent and discriminant validity of the scale by examining model fit. Initially, a descriptive statistical analysis was conducted on the sample. Then, factor loadings were computed to screen the measurement variables within each factor. For measurement variables meeting the criteria, significance tests (with significance levels below 0.05 or 0.01) were conducted, and variables with standardized loading coefficients exceeding 0.7 were considered to meet factor requirements. Measurement variables not meeting these conditions might be considered for deletion. For instance, in the statistical significance test of path coefficients or loading coefficients, if the path coefficient from latent variable “SE” to latent variable “PU” was 0.369, and the p-value was less than 0.01, even though the coefficient of determination (CR) was 6.521 and the SE value exceeded 0.05, based on this result, it can be inferred that this path coefficient exhibits significant differences from 0 at a 95% confidence level. Similarly, other path coefficients were analyzed using the same approach. Some unreasonable measurement items may have been removed. The final model validity test results are presented in Table 4.
Model fit indices
Based on the results presented in Table 5, the following model fit indices can be observed: The χ2/df ratio is 1.896, which is less than 3, indicating a good fit. The RMSEA value is 0.043, which is less than 0.1, suggesting a relatively good fit of the model. Additionally, the RMR value is less than 0.05, and CFI, NFI, TLI, and IFI values are all greater than 0.9, indicating a high level of fit according to these indices. Although GFI, PGFI, AGFI, and PNFI did not fully meet the standard requirements, they are within an acceptable range. Considering the overall model’s context, these values can also be considered acceptable. Taking all these factors into account, based on these model fit indices, the overall fit of the model is relatively good and aligns with the expectations of the study.
Model evaluation and discriminant validity
As shown in Table 6, we conducted a correlation analysis based on the means between factors to assess discriminant validity among the factors. In the analysis of discriminant validity, special attention was given to the square roots of the average variance extracted (AVE) values (indicated in bold). Typically, AVE values greater than 0.5 or composite reliability (CR) values greater than 0.7 indicate good convergent validity. Additionally, if the AVE value of a factor exceeds the highest absolute value of inter-factor correlations, it suggests good discriminant validity and indicates that the measurement indicators within the factor have strong extraction capabilities.For example, consider the “PU” factor. Its square root of AVE is 0.828, which exceeds the highest absolute value of inter-factor correlations. Moreover, the AVE value of the “PU” factor is also greater than 0.5. Based on this, its CR value of 0.897 exceeds the standard of 0.7. This indicates that the “PU” factor not only possesses good discriminant validity but also exhibits excellent extraction capabilities for its internal measurement indicators. Similar logic was applied to the data analysis of other factors. These results further reinforce the discriminant validity among the factors in our model, indicating that there are strong distinctions among the various factors. This analysis of discriminant validity helps ensure that the factors used in our model are indeed distinct from each other and accurately reflect their respective concepts.
Hypothesis verification results
By utilizing the results of factor covariance analysis, we typically validate the distinctiveness between different factors. In this analysis, attention is directed towards the standardized coefficient values between pairs of factors. Generally, as the standardized coefficient values approach 1, it indicates a stronger correlation between two factors. Through this analysis, we gain a deeper understanding of the interrelationships between factors and uncover the interactions among them when constructing the model. Furthermore, in considering the measurement relationships, we can observe the performance of each measurement relationship. When the absolute value of the standardized loading coefficient is greater than 0.6 and exhibits significance, it implies a strong measurement relationship. Relevant analysis results can be found in Table 7. Ultimately, when testing the hypotheses, all hypotheses were supported, as shown in Table 8. The relationship between hypothesis validation results and the research model is depicted in Fig. 3.
Acceptability of VR intervention for emotional regulation in cancer patients
To gain a deeper insight into the acceptability of VR technology intervention for emotion regulation among cancer patients, we conducted descriptive statistical analysis for each construct in the questionnaire. This analysis included measures such as mean, median, standard deviation, and range, with summarized results presented in Table 6. In the acceptability questionnaire covering 13 constructs, the mean scores for all constructs were above 3, as shown in Table 9. In order to comprehensively understand the acceptability of smart homes among respondents, we employed the single-sample Wilcoxon signed-rank test. By comparing the medians of each construct in the acceptability questionnaire with 3 (where 3 represents an uncertain or neutral attitude), we found that among the 13 constructs, 11 had medians exceeding 3, and 2 constructs had medians equal to 3 – PEOU and BI. In the acceptability questionnaire, both PEOU and BI had a median of 3. The data revealed that the medians for most constructs exceeded 3, and all constructs had p-values below 0.05, indicating statistical significance. Consequently, these results suggest that compared to a neutral attitude, cancer patients exhibit a positive and open-minded attitude towards the acceptability of VR technology intervention for emotion regulation.
Discussion
In order to comprehensively introduce VR technology into the emotion regulation of cancer patients, it is crucial to deeply understand their acceptability towards this technology. While many researchers have explored the application of VR technology in alleviating psychological disorders like anxiety, there have been limited studies that introduce VR technology into the emotion regulation domain for cancer patients. In this study, we based our model application and hypothesis validation on the TAM, tailored it to suit the research objectives, and designed questionnaire constructs and items accordingly, resulting in the formulation of 15 hypotheses. Among these hypotheses, the square roots of the AVE for each construct exceeded the absolute values of the inter-factor correlation coefficients, indicating good discriminant validity. All hypotheses were supported, indicating that the model constructed had undergone initial validation, providing a foundation for future in-depth research.
The results indicate that the driving factors of PU extend beyond the classic variable of PEOU to include UE, SE and CP, highlighting the multidimensional nature of technological functionality cognition in the adoption of intelligent tools. The formation of ATT is further reinforced by PE and understanding of VR technology, underscoring the interplay between hedonic motivation and technological familiarity. The predictive mechanism of BI exhibits complexity: beyond the core influences of PU and ATT, the inhibitory effects of technology TA and PR, along with the facilitating roles of SN and IVE, collectively reveal the dual social-technical drivers and the risk–benefit trade-off in cancer patients’ decision-making.
We observed that the understanding of VR technology does not significantly influence cancer patients’ attitudes toward its use. This suggests that even with limited knowledge of VR technology, cancer patients exhibit a strong interest in it and are willing to try it despite not fully understanding its mechanisms. However, we also noted that some patients expressed skepticism toward VR technology, which may stem from a lack of firsthand experience. In this study, a significant positive correlation was found between IVE and BI, confirming Hypothesis H14. This finding indicates that immersion has a positive impact on cancer patients’ intention to use VR technology. Therefore, when integrating VR technology into emotional regulation interventions for cancer patients, it is essential to enhance their immersive experience to achieve better therapeutic and rehabilitative outcomes.
Through statistical analysis of the questionnaire results across 13 dimensions, we found that the mean and median scores for PU, ATT, CP, SE, TA, UE, IVE, SN, PE, PI, and PR all exceeded 3, indicating that most cancer patients hold a positive attitude toward using VR technology for emotional regulation. However, the median scores for PEOU and BI were both 3, suggesting a neutral stance toward the perceived ease of use and behavioral intention. While patients do not express strong agreement, they remain willing to explore the application of VR in their cancer treatment. This neutrality likely stems from multiple factors. First, the complexity of technological interaction design—such as device-wearing requirements or interface navigation—may impose an operational burden on elderly patients, potentially leading to physical discomfort. Second, patients exhibit a lack of trust in the actual efficacy of VR in treatment. Particularly in the absence of firsthand experience, they remain skeptical about its direct applicability in cancer care.
Notably, the distinction between statistical significance and practical relevance highlights the unique characteristics of clinical settings—patients prioritize the functional value of VR in pain management (e.g., distraction) over its role in purely enhancing emotional well-being. These findings not only validate the applicability of the TAM in medical contexts but also expand its explanatory scope by emphasizing the need to enhance user trust and adoption willingness through technological optimization (e.g., simplifying interaction design) and treatment transparency (e.g., real-time feedback mechanisms). It is evident that cancer patients’ acceptance of VR is driven not only by functionality and ease of use but also by the credibility of its therapeutic efficacy and physiological adaptability. For instance, patients’ reliance on VR for pain management (e.g., attention diversion) outweighs their hedonistic expectations for emotional regulation, suggesting the need to introduce a new variable—perceived therapeutic efficacy—into the TAM framework. Perceived therapeutic efficacy can be defined as the extent to which patients expect the technology to directly improve clinical symptoms (e.g., pain, anxiety), potentially mediating the relationship between PU and ATT, thereby indirectly influencing BI.
The findings also indicate that older cancer patients are less likely to accept VR-based emotional therapy, potentially due to concerns about treatment costs. Notably, if VR interventions do not incur additional expenses, patients tend to be more willing to adopt this approach. However, disparities in regional development levels lead to variations in the availability of VR-related equipment. Despite this, our study reveals a negative correlation between the level of familiarity with VR technology and patients’ attitudes toward its use. This suggests that cancer patients with limited knowledge of VR tend to be more curious about it and more willing to try it. Therefore, future research should consider the potential additional treatment costs associated with VR-based emotional regulation for cancer patients, as well as the capacity of hospitals in different regions to support and implement VR interventions.
This study further reveals a dual pathway through which VR technology influences emotional regulation in cancer patients. First, VR provides immediate emotional relief through immersive experiences and attentional redistribution mechanisms, such as pain distraction. Second, patients exhibit a lack of trust in the long-term emotional regulation efficacy of VR (e.g., enhancing psychological resilience), leading to a neutral stance toward behavioral intention. This reflects a core contradiction—insufficient transparency regarding therapeutic outcomes. Notably, patients’ perceptions of VR’s emotional value display significant heterogeneity. Younger individuals tend to seek emotional release through gamified scenarios, whereas older patients prefer low-interactivity environments, such as meditation scenes. This divergence suggests that individualized emotional regulation preferences should be incorporated into VR design frameworks. Moreover, the neutral stance on perceived ease of use further exposes the shortcomings of age-friendly design. Factors such as device weight and interaction complexity may impose additional physiological burdens on elderly patients, undermining the sustainability of their emotional regulation experience. While VR offers an innovative tool for cancer patients’ emotional management, its full potential hinges on emotion-sensitive design, treatment efficacy visualization, and personalized adaptation. By integrating neuroscientific evidence with technological advancements, VR has the potential to become an indispensable emotional support paradigm in comprehensive cancer care, paving new pathways for improving patients’ quality of life.
This study validates the explanatory power of the TAM in medical contexts while expanding its theoretical boundaries. Specifically, it highlights the necessity of integrating treatment outcome transparency—such as real-time data visualization of short-term effects—and optimizing technology usability, including simplifying interaction logic and accommodating the physiological limitations of elderly users, into the core pathways for improving adoption mechanisms. Additionally, these findings offer valuable insights for healthcare professionals and VR technology designers, helping them better understand patients’ concerns regarding technology use. This understanding can guide the development of more appropriate strategies and policies to enhance emotional regulation and therapeutic outcomes. For younger patients, the study reveals a higher willingness to engage with emerging technologies, particularly high-tech products with entertainment value. They demonstrated greater responsiveness in the survey, often possessing more prior exposure to VR devices. Their feedback was notably creative, expressing a preference for incorporating gamification elements to facilitate relaxation and mental engagement during treatment.
Overall, this study reveals that patients generally hold a positive attitude toward emotion regulation technologies. However, the neutrality of PEOU and BI exposes a fundamental paradox in technology adoption. This paradox stems not only from the inherent complexity of the technology itself but also reflects the unique needs of patients in medical settings. Cancer patients expect VR technology to play a more significant role in future treatments, helping them cope with therapy with a more positive mindset and emotional state. Nevertheless, certain concerns and hesitations persist, particularly regarding factors such as age and treatment costs. These findings provide valuable insights for healthcare professionals and VR technology designers, helping them better understand patient concerns about technology adoption. In turn, this understanding can inform the development of more practical policies and strategies to achieve more effective emotion regulation and therapeutic outcomes. For younger patients, there is a greater willingness to engage with emerging technologies, particularly high-tech products with entertainment value. They demonstrated higher responsiveness during the survey, often having more prior exposure to VR devices and providing more creative feedback. Many expressed a preference for incorporating VR-based entertainment elements to facilitate relaxation during treatment. These findings offer critical guidance for the future development of VR applications in the field of emotion regulation for cancer patients, serving as an important reference for optimizing both technology design and implementation strategies.
Conclusions
This study focuses on cancer patients as the research participant, drawing on previous research findings and integrating the theoretical foundation of the TAM. By incorporating analyses of PU, PEOU, ATT, BI, PE, SE, TA, UE, IVE, SN, PEN PI, PR, this study examines the acceptability of VR technology for emotion regulation from the perspective of cancer patients. The study constructs a TAM distinct from prior research to explore cancer patients’ acceptance of VR-based emotion regulation interventions, while also refining the factors influencing VR adoption from their perspective.
The proposed model aligns with the core pathways of the classical TAM but extends its explanatory scope in medical contexts. Specifically, it reveals the dual driving effect of PE and PU on user attitudes. Compared to classical theories, this study expands the boundaries of the TAM by integrating novel user characteristics, product influence factors, and social environmental factors, thus enhancing its applicability to new technologies and user populations. Furthermore, it aligns with the refined analytical trends in technology anxiety research, particularly regarding concerns related to data privacy and other specific dimensions.
The survey, which involved 489 participants, demonstrates the feasibility of using the TAM to examine the acceptability of VR interventions for emotion regulation among cancer patients. The study systematically analyzes each construct to determine its impact on patients’ acceptance of VR-based emotion regulation. Identifying the factors that may lead to resistance toward VR technology will help future researchers refine and enhance its implementation. The findings indicate that cancer patients exhibit an open and positive attitude toward the use of VR for emotion regulation. They perceive the technology as an effective and efficient tool for emotional adjustment and express a willingness to adopt it to manage their emotional well-being.
From a theoretical perspective, this study constructs a conceptual framework for the acceptability of VR interventions for emotion regulation from the viewpoint of cancer patients. It integrates variables related to technological functionality (such as PU and CP), social-psychological factors (such as SN and TA), and IVE, providing empirical support for user behavior research on emerging medical technologies. However, further experimental studies are needed to elaborate on and confirm the findings. Based on the population of cancer patients in China, the structural model derived from the study has undergone preliminary testing, marking the first step toward understanding whether VR technology can be accepted and applied by cancer patients in future treatment scenarios. This study also provides a preliminary framework and background for future research in this area.
Limitations and future research directions
While this study provides valuable insights into the acceptability of VR technology for emotion regulation among cancer patients, several limitations must be acknowledged. First, the survey was conducted solely within the geographical scope of China, which limits the generalizability of the findings to other cultures and regions. Furthermore, the study was concentrated in cities with varying levels of development and geographic diversity, which may not fully represent the broader cancer patient population. Notably, many patients expressed pessimism and reluctance to participate in the study, which may have influenced the results. In subsequent research, we collaborated with medical professionals, sought their understanding and support, and expressed sincere apologies to cancer patients undergoing emotional distress, acknowledging that some of them may have refrained from participating. We hope that future studies can provide more meaningful assistance to cancer patients facing similar challenges.
While a larger and more diverse sample could yield more comprehensive findings, it is important to recognize that even patients who declined to participate in the questionnaire could provide valuable insights into the challenges associated with implementing VR interventions. However, due to time and resource constraints, we were unable to explore this aspect in greater depth. Nevertheless, previous studies suggest that even smaller sample sizes can provide valuable insights. Future research will aim to collect a broader and more varied dataset, not only from those who actively participate, but also from those who may decline participation, in order to achieve a more comprehensive understanding of the subject.
Secondly, although this study made initial progress in exploring the acceptability of VR technology for emotion regulation among cancer patients, it did not fully address the practical application and efficacy of VR interventions. Given the ongoing advancements in VR technology, future studies should consider conducting long-term experimental research to assess the effectiveness of VR interventions for emotion regulation during actual cancer treatment. This would allow for a more thorough evaluation of the therapeutic benefits of VR technology. Additionally, while this study focused on the general acceptability of VR, it did not fully explore the emotional regulation needs of different types of cancer patients. Future research should examine how various cancer types, treatment stages, and individual patient characteristics influence their attitudes and requirements for VR technology.
Finally, methodologically, while this study developed a systematic analytical framework based on the TAM, several latent psychological and socio-cognitive factors may further influence cancer patients’ acceptance of VR technology. Of particular importance is the lack of investigation into the dynamic changes in patient attitudes before and after VR intervention. While the study used the VR Understanding Scale to quantify prior knowledge, it did not differentiate between “theoretical cognition” and “embodied experience.” Participants’ self-reported acceptance could also be affected by cognitive biases, such as anchoring heuristics, which may have distorted the path coefficients of PEOU and PU in the TAM. Future research should incorporate a wider range of multimodal variables, including longitudinal data across pre-intervention, immersive, and post-intervention phases. Cross-lagged panel modeling could help differentiate cognitive patterns from physiological feedback, while enhancing the psychometric sensitivity of experiential indicators.
Despite these limitations, this study lays the groundwork for understanding VR-based emotion regulation in oncology contexts. Expanding sample diversity, employing mixed-methods approaches, and conducting controlled longitudinal trials will contribute to advancing VR research in cancer care and its potential to enhance patient well-being.
Data availability
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Yuan, H., Jiang, Y., Tan, Y. & Xiang, Y. Current status and time trends of cancer incidence and mortality worldwide. Cancer Res. Prev. Treat 48, 642–646 (2021).
Jemal, A. et al. Global cancer statistics. CA: Cancer J. Clin. 61(2), 69–90. https://doi.org/10.3322/caac.20107 (2011).
Wang, Y. & Feng, W. Cancer-related psychosocial challenges. Gen. Psychiatry 35(5), e100871. https://doi.org/10.1136/gpsych-2022-100871 (2022).
Crofton, E. C., Botinestean, C., Fenelon, M. & Gallagher, E. Potential applications for virtual and augmented reality technologies in sensory science. Innov. Food Sci. Emerg. Technol. 56, 102178. https://doi.org/10.1016/j.ifset.2019.102178 (2019).
Zhang, T. et al. A primer on usability assessment approaches for health-related applications of virtual reality. JMIR Serious Games 8(4), e18153. https://doi.org/10.2196/18153 (2020).
Dermody, G., Whitehead, L., Wilson, G. & Glass, C. The role of virtual reality in improving health outcomes for community-dwelling older adults: systematic review. J. Med. Internet Res. 22(6), e17331. https://doi.org/10.2196/17331 (2020).
Ali, N. S. & Nasser, M. Review of virtual reality trends (previous, current, and future directions), and their applications, technologies and technical issues. ARPN J. Eng. Appl. Sci. 12(3), 783–789 (2017).
Zhai, K. et al. Virtual Reality therapy for depression and mood in long-term care facilities. Geriatrics 6(2), 58. https://doi.org/10.3390/geriatrics6020058 (2021).
Pasquini, M. & Biondi, M. Depression in cancer patients: A critical review. Clin. Pract. Epidemiol. Mental Health 3, 2. https://doi.org/10.1186/1745-0179-3-2 (2007).
Brown, K. W., Levy, A. R., Rosberger, Z. & Edgar, L. Psychological distress and cancer survival: A follow-up 10 years after diagnosis. Psychosom. Med. 65(4), 636–643. https://doi.org/10.1097/01.PSY.0000077503.96903.A6 (2003).
Lyu, X. C., Jiang, H. J., Lee, L. H., Yang, C. I. & Sun, X. Y. Oncology nurses’ experiences of providing emotional support for cancer patients: a qualitative study. BMC Nurs. 23, 58. https://doi.org/10.1186/s12912-024-01718-1 (2024).
Maples-Keller, J. L., Bunnell, B. E., Kim, S. J. & Rothbaum, B. O. The use of virtual reality technology in the treatment of anxiety and other psychiatric disorders. Harv. Rev. Psychiatry 25(3), 103–113. https://doi.org/10.1097/HRP.0000000000000138 (2017).
Kim, S. & Kim, E. The use of virtual reality in psychiatry: a review. J. Korean Acad. Child Adolesc. Psychiatry 31(1), 26. https://doi.org/10.5765/jkacap.190037 (2020).
Ioannou, A. et al. Effectiveness of virtual reality vs guided imagery on mood changes in cancer patients receiving chemotherapy treatment: A crossover trial. Eur. J. Oncol. Nurs. 61, 102188. https://doi.org/10.1016/j.ejon.2022.102188 (2022).
Rutkowski, S. et al. Virtual reality as a chemotherapy support in treatment of anxiety and fatigue in patients with cancer: a systematic review and meta-analysis and future research directions. Complement. Ther. Med. 61, 102767. https://doi.org/10.1016/j.ctim.2021.102767 (2021).
Cardenal, V., Cerezo, M. V., Martínez, J., Ortiz-Tallo, M. & Blanca, M. J. Personality, emotions and coping styles: Predictive value for the evolution of cancer patients. Spanish J. Psychol. 15(2), 756–767. https://doi.org/10.5209/rev_SJOP.2012.v15.n2.38887 (2012).
Balasooriya-Smeekens, C., Walter, F. M. & Scott, S. The role of emotions in time to presentation for symptoms suggestive of cancer: A systematic literature review of quantitative studies. Psychooncology 24(12), 1594–1604. https://doi.org/10.1002/pon.3833 (2015).
Dunkel-Schetter, C. Social support and cancer: Findings based on patient interviews and their implications. J. Soc. Issues 40(4), 77–98. https://doi.org/10.1111/j.1540-4560.1984.tb01108.x (1984).
Hack, T. F., Degner, L. F. & Parker, P. A. The communication goals and needs of cancer patients: A review. Psycho-Oncol.: J. Psychol. Social Behav. Dimens. Cancer 14(10), 831–845. https://doi.org/10.1002/pon.949 (2005).
Gao, T., Zhang, T., Zhu, L., Gao, Y. & Qiu, L. Exploring psychophysiological restoration and individual preference in the different environments based on virtual reality. Int. J. Environ. Res. Public Health 16(17), 3102. https://doi.org/10.3390/ijerph16173102 (2019).
Williams, S. E., Ford, J. H. & Kensinger, E. A. The power of negative and positive episodic memories. Cogn. Affect. Behav. Neurosci. 22(5), 869–903. https://doi.org/10.3758/s13415-022-01013-z (2022).
Fosha, D. ‘Nothing that feels bad is ever the last step:’The role of positive emotions in experiential work with difficult emotional experiences. Clin. Psychol. Psychother.: Int. J. Theory Pract. 11(1), 30–43. https://doi.org/10.1002/cpp.390 (2004).
Mejareh, Z. N. et al. Global, regional, and national prevalence of depression among cancer patients: A systematic review and meta-analysis. Indian J. Psychiatry 63(6), 527–535. https://doi.org/10.4103/indianjpsychiatry.indianjpsychiatry_77_21 (2021).
Kim, G. J. A SWOT analysis of the field of virtual reality rehabilitation and therapy. Presence 14(2), 119–146. https://doi.org/10.1162/1054746053967094 (2005).
Trahan, M. H., Smith, K. S. & Talbot, T. B. Past, present, and future: Editorial on virtual reality applications to human services. J. Technol. Hum. Serv. 37(1), 1–12. https://doi.org/10.1080/15228835.2019.1587334 (2019).
Bracq, M. S. et al. Training situational awareness for scrub nurses: Error recognition in a virtual operating room. Nurse Educ. Pract. 53, 103056. https://doi.org/10.1016/j.nepr.2021.103056 (2021).
Stewart-Lord, A., Brown, M., Noor, S., Cook, J. & Jallow, O. The utilisation of virtual images in patient information giving sessions for prostate cancer patients prior to radiotherapy. Radiography 22(4), 269–273. https://doi.org/10.1016/j.radi.2016.05.002 (2016).
Latif, H. et al. Using virtual reality to promote mindfulness among medical trainees; a study of feasibility and acceptance. Blood 136(1), 39. https://doi.org/10.1182/blood-2020-136701 (2020).
Schneider, S. M. & Workman, M. L. Virtual reality as a distraction intervention for older children receiving chemotherapy. Pediatr. Nurs. 26(6), 593–597 (2000).
Birnie, K. A. et al. Usability testing of an interactive virtual reality distraction intervention to reduce procedural pain in children and adolescents with cancer. J. Pediatr. Oncol. Nurs. 35(6), 406–416. https://doi.org/10.1177/1043454218782138 (2018).
Bevilacqua, R. et al. Non-immersive virtual reality for rehabilitation of the older people: a systematic review into efficacy and effectiveness. J. Clin. Med. 8(11), 1882. https://doi.org/10.3390/jcm8111882 (2019).
Muff, J. L., Heye, T., Thieringer, F. M. & Brantner, P. Clinical acceptance of advanced visualization methods: A comparison study of 3D-print, virtual reality glasses, and 3D-display. 3D Print. Med. 8(1), 1–10. https://doi.org/10.1186/s41205-022-00133-z (2022).
Schiza, E., Matsangidou, M., Neokleous, K. & Pattichis, C. S. Virtual reality applications for neurological disease: a review. Front. Robot. AI 6, 100. https://doi.org/10.3389/frobt.2019.00100 (2019).
Feyzioğlu, Ö., Dinçer, S., Akan, A. & Algun, Z. C. Is Xbox 360 Kinect-based virtual reality training as effective as standard physiotherapy in patients undergoing breast cancer surgery?. Support. Care Cancer 28, 4295–4303. https://doi.org/10.1007/s00520-019-05287-x (2020).
Quan, W., Liu, S., Cao, M. & Zhao, J. A comprehensive review of virtual reality technology for cognitive rehabilitation in patients with neurological conditions. Appl. Sci. 14(14), 6285. https://doi.org/10.3390/app14146285 (2024).
Tennant, M. et al. Exploring the use of immersive virtual reality to enhance psychological well-being in pediatric oncology: A pilot randomized controlled trial. Eur. J. Oncol. Nurs. 48, 101804. https://doi.org/10.1016/j.ejon.2020.101804 (2020).
Somarathna, R., Bednarz, T. & Mohammadi, G. Virtual reality for emotion elicitation–a review. IEEE Trans. Affect. Comput. 14(4), 2626–2645. https://doi.org/10.1109/TAFFC.2022.3181053 (2022).
Bettis, A. H., Burke, T. A., Nesi, J. & Liu, R. T. Digital technologies for emotion-regulation assessment and intervention: A conceptual review. Clinical Psychological Science 10(1), 3–26. https://doi.org/10.1177/21677026211011982 (2022).
Montana, J. I. et al. The benefits of emotion regulation interventions in virtual reality for the improvement of wellbeing in adults and older adults: A systematic review. J. Clin. Med. 9(2), 500. https://doi.org/10.3390/jcm9020500 (2020).
Kothgassner, O. D. et al. Virtual reality biofeedback interventions for treating anxiety: A systematic review, meta-analysis and future perspective. Wien. Klin. Wochenschr. 134(1), 49–59. https://doi.org/10.1007/s00508-021-01991-z (2022).
Pira, G. L., Aquilini, B., Davoli, A., Grandi, S. & Ruini, C. The use of virtual reality interventions to promote positive mental health: systematic literature review. JMIR Mental Health 10(1), e44998. https://doi.org/10.2196/44998 (2023).
Riches, S., Azevedo, L., Bird, L., Pisani, S. & Valmaggia, L. Virtual reality relaxation for the general population: A systematic review. Soc. Psychiatry Psychiatr. Epidemiol. 56, 1707–1727. https://doi.org/10.1007/s00127-021-02110-z (2021).
Wagener, N., Duong, T. D., Schöning, J., Rogers, Y., & Niess, J. The Role of Mobile and Virtual Reality Applications to Support Well-Being: An Expert View and Systematic App Review. In Human-Computer Interaction–INTERACT 2021: 18th IFIP TC 13 International Conference, Bari, Italy, August 30–September 3, 2021, Proceedings, Part IV 18 262–283. (Springer International Publishing, 2021). https://doi.org/10.1007/978-3-030-85610-6_16.
Sun, Y. et al. Physiological and affective responses to green space virtual reality among pregnant women. Environ. Res. 216, 114499. https://doi.org/10.1016/j.envres.2022.114499 (2023).
Ma, J., Zhao, D., Xu, N. & Yang, J. The effectiveness of immersive virtual reality (VR) based mindfulness training on improvement mental-health in adults: A narrative systematic review. Explore 19(3), 310–318. https://doi.org/10.1016/j.explore.2022.08.001 (2023).
Boas, Y. A. G. V. (2013). Overview of virtual reality technologies. in Interactive Multimedia Conference. https://api.semanticscholar.org/CorpusID:8120179.
Guillen-Sanz, H., Checa, D., Miguel-Alonso, I. & Bustillo, A. A systematic review of wearable biosensor usage in immersive virtual reality experiences. Virtual Real. 28(2), 74. https://doi.org/10.1007/s10055-024-00970-9 (2024).
Wedel, M., Bigné, E. & Zhang, J. Virtual and augmented reality: Advancing research in consumer marketing. Int. J. Res. Mark. 37(3), 443–465. https://doi.org/10.1016/j.ijresmar.2020.04.004 (2020).
Pittara, M., Matsangidou, M., Stylianides, K., Petkov, N. & Pattichis, C. S. Virtual reality for pain management in cancer: A comprehensive review. IEEE Access 8, 225475–225489. https://doi.org/10.1109/ACCESS.2020.3044233 (2020).
Zeng, Y., Zhang, J. E., Cheng, A. S., Cheng, H. & Wefel, J. S. Meta-analysis of the efficacy of virtual reality–based interventions in cancer-related symptom management. Integr. Cancer Ther. https://doi.org/10.1177/1534735419871108 (2019).
Scates, D., Dickinson, J. I., Sullivan, K., Cline, H. & Balaraman, R. Using nature-inspired virtual reality as a distraction to reduce stress and pain among cancer patients. Environ. Behav. 52(8), 895–918. https://doi.org/10.1177/0013916520916259 (2020).
Chirico, A. et al. Virtual reality and music therapy as distraction interventions to alleviate anxiety and improve mood states in breast cancer patients during chemotherapy. J. Cell. Physiol. 235(6), 5353–5362. https://doi.org/10.1002/jcp.29422 (2020).
Northouse, L. et al. A tailored web-based psycho-educational intervention for cancer patients and their family caregivers. Cancer Nurs. 37(5), 321–330. https://doi.org/10.1097/NCC.0000000000000159 (2014).
Matsuda, A., Yamaoka, K., Tango, T., Matsuda, T. & Nishimoto, H. Effectiveness of psychoeducational support on quality of life in early-stage breast cancer patients: A systematic review and meta-analysis of randomized controlled trials. Qual. Life Res. 23, 21–30. https://doi.org/10.1007/s11136-013-0460-3 (2014).
Jimenez, Y. A. et al. Breast cancer patients’ perceptions of a virtual learning environment for pretreatment education. J. Cancer Educ. 33, 983–990. https://doi.org/10.1007/s13187-017-1183-x (2018).
Mohammad, E. B. & Ahmad, M. Virtual reality as a distraction technique for pain and anxiety among patients with breast cancer: A randomized control trial. Palliat. Support. Care 17(1), 29–34. https://doi.org/10.1017/S1478951518000639 (2019).
Wu, Y. et al. Effectiveness of virtual reality in symptom management of cancer patients: A systematic review and meta-analysis. J. Pain Symptom Manag. 65(5), e467–e482. https://doi.org/10.1016/j.jpainsymman.2023.01.023 (2023).
Javaid, M. & Haleem, A. Virtual reality applications toward medical field. Clin. Epidemiol. Glob. Health 8(2), 600–605. https://doi.org/10.1016/j.cegh.2019.12.01 (2020).
Spiegel, B. et al. Virtual reality for management of pain in hospitalized patients: A randomized comparative effectiveness trial. PLoS ONE 14(8), e0219115. https://doi.org/10.1371/journal.pone.0219115 (2019).
Yuen, E. K. et al. A pilot of acceptance and commitment therapy for public speaking anxiety delivered with group videoconferencing and virtual reality exposure. J. Context. Behav. Sci. 12, 47–54. https://doi.org/10.1016/j.jcbs.2019.01.006 (2019).
Appel, L. et al. Evaluating the impact of virtual reality on the behavioral and psychological symptoms of dementia and quality of life of inpatients with dementia in acute care: randomized controlled trial (VRCT). J. Med. Internet Res. 26, e51758. https://doi.org/10.2196/51758 (2024).
Fishbein, M. & Ajzen, I. Belief, attitude, intention and behavior: An introduction to theory and research. J. Bus. Venturing 5, 177–188 (1977).
Venkatesh, V., Thong, J. Y. & Xu, X. Unified theory of acceptance and use of technology: A synthesis and the road ahead. J. Assoc. Inform. Syst. 17(5), 328–376 (2016).
Lin, C. H., Shih, H. Y. & Sher, P. J. Integrating technology readiness into technology acceptance: The TRAM model. Psychol. Mark. 24(7), 641–657. https://doi.org/10.1002/mar.20177 (2007).
Venkatesh, V. & Bala, H. Technology acceptance model 3 and a research agenda on interventions. Decis. Sci. 39(2), 273–315. https://doi.org/10.1111/j.1540-5915.2008.00192.x (2008).
Williams, M. D., Rana, N. P. & Dwivedi, Y. K. The unified theory of acceptance and use of technology (UTAUT): a literature review. J. Enterp. Inf. Manag. 28(3), 443–488. https://doi.org/10.1108/JEIM-09-2014-0088 (2015).
Al-Emran, M. & Granić, A. Is it still valid or outdated? A bibliometric analysis of the technology acceptance model and its applications from 2010 to 2020. Recent Adv. Technol. Accept. Models Theor. https://doi.org/10.1287/mnsc.35.8.982 (2021).
King, W. R. & He, J. A meta-analysis of the technology acceptance model. Inf. Manag. 43(6), 740–755. https://doi.org/10.1016/j.im.2006.05.003 (2006).
Hamad, A. & Jia, B. How virtual reality technology has changed our lives: an overview of the current and potential applications and limitations. Int. J. Environ. Res. Public Health 19(18), 11278. https://doi.org/10.3390/ijerph191811278 (2022).
Wang, E. Y. et al. Predicting pediatric healthcare provider use of virtual reality using a technology acceptance model. JAMIA open 6(3), ooad076. https://doi.org/10.1093/jamiaopen/ooad076 (2023).
AlQudah, A. A., Al-Emran, M. & Shaalan, K. Technology acceptance in healthcare: a systematic review. Appl. Sci. 11(22), 10537. https://doi.org/10.3390/app112210537 (2021).
Halbig, A. et al. Opportunities and challenges of virtual reality in healthcare–a domain experts inquiry. Front. Virtual Real. 3, 837616. https://doi.org/10.3389/frvir.2022.837616 (2022).
Baghaei, N. et al. Virtual reality for supporting the treatment of depression and anxiety: scoping review. JMIR Mental Health 8(9), e29681 (2021).
Liu, H., Miao, X., Shi, C. & Xu, T. Exploring the acceptance of virtual reality training systems among construction workers: a combined structural equation modeling and artificial neural network approach. Front. Public Health 12, 1478615. https://doi.org/10.3389/fpubh.2024.1478615 (2024).
Di Natale, A. F., Bartolotta, S., Gaggioli, A., Riva, G. & Villani, D. Exploring students’ acceptance and continuance intention in using immersive virtual reality and metaverse integrated learning environments: The case of an Italian university course. Educ. Inf. Technol. 29, 14749–14768. https://doi.org/10.1007/s10639-023-12436-7 (2024).
Noble, S. M., Saville, J. D. & Foster, L. L. VR as a choice: what drives learners’ technology acceptance?. Int. J. Educ. Technol. High. Educ. 19, 6. https://doi.org/10.1186/s41239-021-00310-w (2022).
Fussell, S. G. & Truong, D. Using virtual reality for dynamic learning: an extended technology acceptance model. Virtual Real. 26(1), 249–267. https://doi.org/10.1007/s10055-021-00554-x (2022).
Cabero-Almenara, J., Barroso-Osuna, J. & Martinez-Roig, R. Mixed, augmented and virtual, reality applied to the teaching of mathematics for architects. Appl. Sci. 11(15), 7125. https://doi.org/10.3390/app11157125 (2021).
Capasa, L., Zulauf, K. & Wagner, R. Virtual reality experience of mega sports events: A technology acceptance study. J. Theor. Appl. Electron. Commer. Res. 17(2), 686–703. https://doi.org/10.3390/jtaer17020036 (2022).
Kari, T. & Kosa, M. Acceptance and use of virtual reality games: an extension of HMSAM. Virtual Real. 27, 1585–1605. https://doi.org/10.1007/s10055-023-00749-4 (2023).
Xu, W. et al. Acceptance of virtual reality exergames among Chinese older adults. Int. J. Hum.-Comput. Interact. 39(5), 1134–1148. https://doi.org/10.1080/10447318.2022.2098559 (2023).
Jang, Y. & Park, E. An adoption model for virtual reality games: The roles of presence and enjoyment. Telemat. Inform. 42, 101239. https://doi.org/10.1016/j.tele.2019.101239 (2019).
Kosa, M., Uysal, A., & Eren, P. E. Acceptance of virtual reality games: A multi-theory approach. In Research Anthology on Game Design. Development, Usage, and Social Impact, 31–61 https://doi.org/10.4018/978-1-6684-7589-8.ch003 (2023).
Sancho-Esper, F., Ostrovskaya, L., Rodriguez-Sanchez, C. & Campayo-Sanchez, F. Virtual reality in retirement communities: Technology acceptance and tourist destination recommendation. J. Vacat. Mark. 29(2), 275–290. https://doi.org/10.1177/13567667221080567 (2023).
Shao, D. & Lee, I. J. Acceptance and influencing factors of social virtual reality in the urban elderly. Sustainability 12(22), 9345. https://doi.org/10.3390/su12229345 (2020).
Snoswell, A. J. & Snoswell, C. L. Immersive virtual reality in health care: Systematic review of technology and disease states. JMIR Biomed. Eng. 4(1), e15025. https://doi.org/10.2196/15025 (2019).
Tsai, J. C., Chen, L. Y. & Peng, H. Y. Exploring the factors influencing consumer’s attitude toward using and use intention of virtual reality games. Int. J. Org. Innov. 13(4), 160–175 (2021).
Da Costa, R. M. E. M. & de Carvalho, L. A. V. The acceptance of virtual reality devices for cognitive rehabilitation: A report of positive results with schizophrenia. Comput. Methods Prog. Biomed. 73(3), 173–182. https://doi.org/10.1016/S0169-2607(03)00066-X (2004).
Nordhoff, S. & Lehtonen, E. Examining the effect of personality on user acceptance of conditionally automated vehicles. Sci. Rep. 15, 1091. https://doi.org/10.1038/s41598-024-84776-4 (2025).
Sharma, K., Aswal, C. & Paul, J. Factors affecting green purchase behavior: A systematic literature review. Bus. Strateg. Environ. 32(4), 2078–2092. https://doi.org/10.1002/bse.3237 (2023).
Ajzen, I. From intentions to actions: A theory of planned behavior. Action control: From cognition to behavior 179–211 (Springer Berlin Heidelberg, Berlin, Heidelberg, 1985). https://doi.org/10.1007/978-3-642-69746-3_2.
Bagozzi, R. P., Davis, F. D. & Warshaw, P. R. Development and test of a theory of technological learning and usage. Hum. Relat. 45(7), 659–686. https://doi.org/10.1177/001872679204500702 (1992).
Venkatesh, V. & Davis, F. D. A theoretical extension of the technology acceptance model: Four longitudinal field studies. Manag. Sci. 46(2), 186–204. https://doi.org/10.1287/mnsc.46.2.186.11926 (2000).
Lee, J., Kim, J. & Choi, J. Y. The adoption of virtual reality devices: The technology acceptance model integrating enjoyment, social interaction, and strength of the social ties. Telemat. Inform. 39, 37–48. https://doi.org/10.1016/j.tele.2018.12.006 (2019).
Hsiao, C. H. & Yang, C. The intellectual development of the technology acceptance model: A co-citation analysis. Int. J. Inf. Manag. 31(2), 128–136. https://doi.org/10.1016/j.ijinfomgt.2010.07.003 (2011).
Mishra, A., Shukla, A. & Sharma, S. K. Psychological determinants of users’ adoption and word-of-mouth recommendations of smart voice assistants. Int. J. Inf. Manag. 67, 102413. https://doi.org/10.1016/j.ijinfomgt.2021.102413 (2022).
Syed-Abdul, S. et al. Virtual reality among the elderly: a usefulness and acceptance study from Taiwan. BMC Geriatr. 19, 223. https://doi.org/10.1186/s12877-019-1218-8 (2019).
Kim, M. J., Lee, C. K. & Preis, M. W. The impact of innovation and gratification on authentic experience, subjective well-being, and behavioral intention in tourism virtual reality: The moderating role of technology readiness. Telemat. Inform. 49, 101349. https://doi.org/10.1016/j.tele.2020.101349 (2020).
Mäkinen, H., Haavisto, E., Havola, S. & Koivisto, J. M. User experiences of virtual reality technologies for healthcare in learning: an integrative review. Behav. Inf. Technol. 41(1), 1–17. https://doi.org/10.1080/0144929X.2020.1788162 (2022).
Bandura, A. Self-efficacy: Toward a unifying theory of behavioral change. Adv. Behav. Res. Ther. 1(4), 139–161. https://doi.org/10.1016/0146-6402(78)90002-4 (1978).
Alshammari, S. H. & Alkhwaldi, A. F. An integrated approach using social support theory and technology acceptance model to investigate the sustainable use of digital learning technologies. Sci. Rep. 15, 342. https://doi.org/10.1038/s41598-024-83450-z (2025).
Nissim, Y. & Weissblueth, E. Virtual reality (VR) as a source for self-efficacy in teacher training. Int. Educ. Stud. 10(8), 52–59 (2017).
Tai, K. H., Hong, J. C., Tsai, C. R., Lin, C. Z. & Hung, Y. H. Virtual reality for car-detailing skill development: Learning outcomes of procedural accuracy and performance quality predicted by VR self-efficacy, VR using anxiety, VR learning interest and flow experience. Comput. Educ. 182, 104458. https://doi.org/10.1016/j.compedu.2022.104458 (2022).
Hoffman, A. J. et al. Virtual reality bringing a new reality to postthoracotomy lung cancer patients via a home-based exercise intervention targeting fatigue while undergoing adjuvant treatment. Cancer Nurs. 37(1), 23–33. https://doi.org/10.1097/NCC.0b013e318278d52f (2014).
Siyar, S. et al. Machine learning distinguishes neurosurgical skill levels in a virtual reality tumor resection task. Med. Biol. Eng. Compu. 58, 1357–1367. https://doi.org/10.1007/s11517-020-02155-3 (2020).
Sabbagh, A. J. et al. Roadmap for developing complex virtual reality simulation scenarios: Subpial neurosurgical tumor resection model. World Neurosurg. 139, e220–e229. https://doi.org/10.1016/j.wneu.2020.03.187 (2020).
Gibson, A., & O’Rawe, M. Virtual reality as a travel promotional tool: Insights from a consumer travel fair. Augmented reality and virtual reality: Empowering human, place and business, 93–107. https://doi.org/10.1007/978-3-319-64027-37 (2018).
Huygelier, H., Schraepen, B., Van Ee, R., Vanden Abeele, V. & Gillebert, C. R. Acceptance of immersive head-mounted virtual reality in older adults. Sci. Rep. 9(1), 4519. https://doi.org/10.1038/s41598-019-41200-6 (2019).
Semerci, R., Akgün Kostak, M., Eren, T. & Avci, G. Effects of virtual reality on pain during venous port access in pediatric oncology patients: A randomized controlled study. J. Pediatr. Oncol. Nurs. 38(2), 142–151. https://doi.org/10.1177/1043454220975 (2021).
Lindner, P. et al. Experiences of gamified and automated virtual reality exposure therapy for spider phobia: Qualitative study. JMIR Serious Games 8(2), e17807. https://doi.org/10.2196/17807 (2020).
Bracq, M. S. et al. Learning procedural skills with a virtual reality simulator: An acceptability study. Nurse Educ. Today 79, 153–160. https://doi.org/10.1016/j.nedt.2019.05.026 (2019).
Yang, M. et al. Predicting m-health acceptance from the perspective of unified theory of acceptance and use of technology. Sci. Rep. 14, 339. https://doi.org/10.1038/s41598-023-50436-2 (2024).
Liu, Q., Wang, Y., Tang, Q. & Liu, Z. Do you feel the same as I do? differences in virtual reality technology experience and acceptance between elderly adults and college students. Front. Psychol. 11, 573673. https://doi.org/10.3389/fpsyg.2020.573673 (2020).
Jang, J., Ko, Y., Shin, W. S. & Han, I. Augmented reality and virtual reality for learning: An examination using an extended technology acceptance model. IEEE Access 9, 6798–6809. https://doi.org/10.1109/ACCESS.2020.3048708 (2021).
Castiblanco Jimenez, I. A., Cepeda García, L. C., Violante, M. G., Marcolin, F. & Vezzetti, E. Commonly used external TAM variables in e-learning, agriculture and virtual reality applications. Future Internet 13(1), 7. https://doi.org/10.3390/fi13010007 (2020).
Birkmeyer, S., Wirtz, B. W. & Langer, P. F. Determinants of mHealth success: An empirical investigation of the user perspective. Int. J. Inf. Manag. 59, 102351. https://doi.org/10.1016/j.ijinfomgt.2021.102351 (2021).
Parker, E. & Saker, M. Art museums and the incorporation of virtual reality: Examining the impact of VR on spatial and social norms. Convergence 26(5–6), 1159–1173. https://doi.org/10.1177/1354856519897 (2020).
Sarah, K., Oceane, S., Emily, F. & Carole, F. Learning from lockdown-Assessing the positive and negative experiences, and coping strategies of researchers during the COVID-19 pandemic. Appl. Anim. Behav. Sci. 236, 105269. https://doi.org/10.1016/j.applanim.2021.105269 (2021).
Restorick Roberts, A. & Allen, P. D. Strategies to improve psychosocial care in nursing homes. Innov. Aging 2(1), 546–546. https://doi.org/10.1093/geroni/igy023.2014 (2018).
Adams, D., Bah, A., Baltimore, U. O. M., & Barwulor, C. Ethics Emerging: the Story of Privacy and Security Perceptions in Virtual Reality. USENIX Symposium on Usable Privacy and Security (SOUPS) 2018. August 12–14, 2018, Baltimore, MD, USA, 443–458. https://www.usenix.org/conference/soups2018/presentation/adams (2018).
Rauschnabel, P. A., Brem, A. & Ivens, B. S. Who will buy smart glasses? Empirical results of two pre-market-entry studies on the role of personality in individual awareness and intended adoption of google glass wearables. Comput. Hum. Behav. 49, 635–647. https://doi.org/10.1016/j.chb.2015.03.003 (2015).
Sagnier, C., Loup-Escande, E., Lourdeaux, D., Thouvenin, I. & Valléry, G. User acceptance of virtual reality: An extended technology acceptance model. Int. J. Hum.-Comput. Interact. 36(11), 993–1007. https://doi.org/10.1080/10447318.2019.1708612 (2020).
Kim, Y. M., Rhiu, I. & Yun, M. H. A systematic review of a virtual reality system from the perspective of user experience. Int. J. Hum.-Comput. Interact. 36(10), 893–910. https://doi.org/10.1080/10447318.2019.1699746 (2020).
Zeng, F., Wang, M., Li, L. & Cai, S. Survey on the acceptance of smart cars amongst middle-aged and elderly in China. Technol. Soc. 73, 102234. https://doi.org/10.1016/j.techsoc.2023.102234 (2023).
Fagan, M., Kilmon, C. & Pandey, V. Exploring the adoption of a virtual reality simulation: The role of perceived ease of use, perceived usefulness and personal innovativeness. Campus-Wide Inf. Syst. 29(2), 117–127. https://doi.org/10.1108/10650741211212368 (2012).
Rasimah, C. M. Y., Ahmad, A. & Zaman, H. B. Evaluation of user acceptance of mixed reality technology. Australas. J. Educ. Technol. 27(8), 1369–1387. https://doi.org/10.14742/ajet.899 (2011).
Xu, X., Kang, J. & Yan, L. Understanding embodied immersion in technology-enabled embodied learning environments. J. Comput. Assist. Learn. 38(1), 103–119. https://doi.org/10.1111/jcal.12594 (2022).
Bogicevic, V., Liu, S. Q., Seo, S., Kandampully, J. & Rudd, N. A. Virtual reality is so cool! How technology innovativeness shapes consumer responses to service preview modes. Int. J. Hosp. Manag. 93, 102806. https://doi.org/10.1016/j.ijhm.2020.102806 (2021).
Graham, J. W. Missing data analysis: Making it work in the real world. Annu. Rev. Psychol. 60, 549–576. https://doi.org/10.1146/annurev.psych.58.110405.085530 (2009).
Newman, D. A. Missing data: Five practical guidelines. Organ. Res. Methods 17(4), 372–411. https://doi.org/10.1177/1094428114548590 (2014).
Little, R. J. A test of missing completely at random for multivariate data with missing values. J. Am. Stat. Assoc. 83(404), 1198–1202. https://doi.org/10.1080/01621459.1988.10478722 (1988).
Acknowledgements
We would like to express our gratitude to the editor and reviewers for their assistance in revising and improving this study. We also appreciate the support provided by Prof. Fangqun Cheng and Prof. Xingye Wang.
Funding
This research was funded by the Science Research Project of the Hunan Provincial Department of Education (23A0533) and the Xiangtan Medical Research Project (2023-xtyx-4).
Author information
Authors and Affiliations
Contributions
F.Z. was responsible for conceptualization, methodology, editing, project management, and fundraising. Data collection, data processing, data organization, and visualization were conducted by Q.L., X.C., W.Z., and S.C. All authors contributed to data management and interpretation. The first draft of the manuscript was written by F.Z., S.C., and Q.L. The manuscript revisions were completed by F.Z., Z.X., J.L., and Q.L. All authors participated in the review, commenting, and editing of the manuscript. All authors read and confirmed the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zeng, F., Li, Q., Cai, S. et al. Cancer patients’ acceptance of virtual reality interventions for self-emotion regulation. Sci Rep 15, 12185 (2025). https://doi.org/10.1038/s41598-025-95160-1
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-95160-1