Abstract
Asthma is a significant non-communicable disease affecting over 300 million people worldwide. This study aimed to evaluate the influence of socio-demographic, environmental, and clinical factors on asthma control among patients visiting community pharmacies in Lahore, Pakistan. A multicenter prospective observational study was conducted with 284 participants using a validated data collection tool. Data included demographics and potential confounders such as smoking, obesity, co-morbidities (e.g., allergic rhinitis, gastroesophageal reflux disease [GERD]), and adherence to treatment. Asthma control was classified into full, partial, and uncontrolled levels based on established guidelines. Statistical analyses, including chi-square tests and logistic regression, were performed to identify significant predictors. The results indicated that 53.5% of participants were female, 74.6% were aged above 40 years, and 42.3% were obese. A family history of asthma was reported in 55.6% of participants, while smoking was prevalent in 77.1%. Clinical co-morbidities, such as allergic rhinitis (49.3%) and GERD (50.7%), were notable. Participants who adhered to treatment (62.3%) and engaged in daily exercise (59.5%) exhibited significantly better asthma control. Multivariate analysis revealed that higher education, rural residence, and the absence of obesity were positively associated with asthma control, whereas passive smoking and prolonged asthma history had a negative impact. This study underscores the multifaceted nature of asthma management and the importance of addressing socio-demographic, environmental, and clinical factors. Improved asthma outcomes require targeted interventions, including promoting adherence to treatment plans, encouraging physical activity, and minimizing exposure to smoking and environmental allergens. The findings highlight the need for community-centered strategies to enhance asthma control and reduce its public health burden, particularly in middle-income countries like Pakistan.
Similar content being viewed by others
Introduction
Asthma is a non-communicable disease and a major public health issue all over the world1. The pathophysiology of asthma is not clearly defined2. The common symptoms of asthma are chest tightness and shortness of breath3. The asthmatic attack is controlled by reducing the exposure to allergen that triggers asthma attacks4. The risk factors of asthma are smoking, allergy history, environmental allergens, low socio-economic and older age5. Globally, more than 300 million people are affected with asthma6. It is expected that in 2025, the number of asthma cases will increase by 100 million7. The national health survey conducted in the United States from 2011 to 2016 found that approximately 160.7 million working adults have asthma annually8. The prevalence of asthma among adults is high, with 83% of cases triggered by exposure to dust in Karachi, Pakistan5.
Asthma is influenced by various extra-thoracic factors, such as allergic rhinitis, obesity, and gastroesophageal reflux disease (GERD), as well as intra-thoracic factors, including COPD, hypersensitivity, and airway obstructions9. Comorbidities are commonly present in asthma patients, further complicating disease management10. Research has linked periodontitis to increased asthma severity11, while obesity is recognized as a significant risk factor for asthma development12. In contrast, Cesarean section has not been associated with childhood bronchial asthma13, whereas maternal exercise during pregnancy—at least three times a week—has been shown to reduce the risk of asthma in children by half14. Additionally, psychological factors such as anxiety and depression are emerging concerns, particularly in school-going children, as asthma-related limitations affect their social and academic participation15.
The risk of asthma is increased with allergic rhinitis16,17. The exposure of children with particulate matter having size ≤ 2.5 μm increases the incidence of asthma with wheezing18. The 8-hour and 24-hour exposure of any person with Ozone (O2), Nitrous oxide (NO2), and Sulphur dioxide increased the possibility of having asthma19. Exposure to household cleaning agents, volatile organic compounds, chemicals, certain pesticides, fungicides, and insecticides increases the risk of asthma20. Asthma is treated with two types of drugs, preventers and relievers21. The class of drugs, Leukotrienes receptor antagonist (LTRA); montelukast, is a preventer medication that helps to reduce inflammation only20. Long-acting bronchodilators are reliever medicines that are not given alone because they do not treat inflammation21. Short-acting bronchodilators (SABA) are not recommended alone, both in adolescents and adults22. SABA acts as a symptomatic treatment, but the disease is not treated by its use23.
Instead of using separate preventers and relievers, combination therapy with MART (Maintenance and Reliever Therapy) inhalers offer a more effective treatment strategy24. ICS (Inhaled Corticosteroids)-formoterol serves as an anti-inflammatory preventer that opens airways and also acts as a reliever25. It is a more effective therapeutic option compared to using SABA alone or the SABA-ICS combination16. ICS-formoterol has been shown to control asthma and reduce the risk of exacerbations, both in mild attacks when used alone and in severe attacks when used with maintenance therapy26.
According to WHO, treating asthma with inhalers is the most efficient, and safest way but still challenging for middle-income countries27. The latest microbial treatment with T regulatory cells (Treg) is an advanced method for treating inflamed human cell-based dampened airways28. Advanced biological therapies, such as monoclonal antibodies (omalizumab, dupilumab), help improve QOL, reduce exacerbations, and minimize severe respiratory conditions in the worst asthma cases29. In patients above age 12, dupilumab helps reduce exacerbations much better than omalizumab30.
The control of asthma measures, such as lung function tests (LFTs) and IgE levels, depends on serum vitamin D levels in the body22. Various confounders can influence asthma control, either positively or negatively. Reducing risk factors that trigger asthma can significantly improve disease management. However, most previous research on asthma control has primarily focused on hospitalized patients, clinical settings, or specific biological markers, with limited emphasis on real-world factors affecting non-hospitalized individuals. Additionally, studies examining the combined impact of socio-demographic, environmental, and clinical predictors on asthma control remain scarce, particularly in the context of middle-income countries like Pakistan. Given the growing burden of asthma and the need for more comprehensive insights into disease management outside hospital settings, this study aimed to evaluate the effect of different confounders on asthma control in patients visiting community pharmacies across various areas of Lahore. By focusing on a diverse outpatient population, this research provides a broader understanding of real-world asthma management and helps identify practical interventions to improve disease control at the community level.
Methodology
The present study was a multicenter prospective and observational study in nature, which investigated asthma control with respect to different confounders affecting the control of asthma in multiple community pharmacies in Lahore, one of the largest cities in Pakistan.
A validated data collection tool was utilized to evaluate the impact of various confounding factors on asthma control. These confounders were identified based on recommendations from established guidelines, including the NICE guidelines and Asian asthma guidelines. The tool comprised two main sections: the first captured the demographic details of asthma patients, while the second focused on the confounders influencing asthma control. These confounders included socio-demographic, environmental, and clinical factors, all of which were derived from prior literature and guidelines. Asthma control was categorized into three levels: full control, partial control, and uncontrolled asthma.
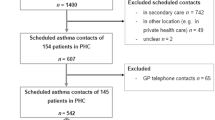
A convenience sampling technique was used to recruit asthma patients from various community pharmacies in Lahore. The study focused on three geographic areas: Harbanspura, Garhi Shahu, and Gulberg. Pharmacies within these areas were contacted, and prior approval was obtained from the respective pharmacists. All patients visiting these pharmacies were asked to provide written consent for participation in the study. Only those who voluntarily agreed to participate were included in the final analysis. The sample included asthma patients from chain pharmacies, community pharmacies, and independent pharmacies in these regions. The principal investigator visited multiple pharmacies to identify eligible asthma patients. These patients were selected because they regularly visited pharmacies to fill their prescriptions, a common practice in Pakistan, where most patients obtain their medications from community pharmacies.
Patients were approached with prior approval from the pharmacists in-charge at these pharmacies. Participation in the study required patients with asthma to provide informed consent. Only those who gave both oral and written consent were included in the research. Ultimately, 284 patients consented to participate and were enrolled in the study. Detailed interviews were conducted with these patients at the community pharmacies to gather comprehensive information on their demographics, confounding factors, and asthma control.
Ethical approval for the study was obtained from the Research and Ethics Committee of the University of Biological and Applied Sciences, Lahore. After a thorough review of all ethical aspects of the research tool, the committee issued formal written approval and assigned the ethical approval number MZI/49/23. The study was conducted in accordance with the guidelines and regulations of the ethical committee. All participants provided written informed consent for their participation in the study.
Statistical analysis
The experiment data was presented in both descriptive and analytical formats, with statistical analysis conducted using SPSS version 24.0. A significance level of P < 0.05 was applied to determine statistical significance. Non-parametric statistical analysis, which explores the relationship between a dependent variable and asthma control, was utilized. The analysis of asthma control data involved employing a chi-square test to ascertain the p-values of various variables. In the Current study statistical significance standard for the P value was set less than 0.05 for any kind of direct positive or negative relationship in variables. Additionally, the effect size was computed using Phi and Cramer’s V in the non-parametric analysis. These measures adjust the chi-square significance to account for sample size differences.
Results
The socio-demographic, environmental, and clinical characteristics of the participants in the study revealed diverse profiles. Among the 284 participants, 53.5% were female, and the majority (74.6%) were aged above 40 years. Most participants were employed in management-related jobs (27.5%) or technical roles (22.5%), with education levels ranging from school (35.9%) to university (29.2%). A more significant proportion of participants resided in urban areas (51.1%) and had more than two children (58.5%). Obesity was prevalent in 42.3% of the participants, and 35.9% reported having asthma for more than five years.
Family history of asthma was reported by 55.6%, while active or passive smoking was common, affecting 77.1% of participants. Co-morbidities such as allergic rhinitis (49.3%) and GERD (50.7%) were also notable. Treatment adherence was relatively high (62.3%), and 59.5% of participants engaged in daily exercise. These findings highlight a multifaceted interplay of factors influencing asthma control among the population. More details regarding the demographic characteristics can be obtained from Table 1 as follows:
In the current study, multiple logistic regression analysis was employed to evaluate the impact of various confounders on asthma control. The analysis identified significant predictors influencing asthma management among participants. Key socio-demographic factors, including age, gender, and education level, were found to be associated with asthma control. Clinical variables such as obesity, duration of asthma, family history of the disease, smoking habits, and co-morbid conditions (e.g., allergic rhinitis and GERD) also emerged as influential factors.
Participants who adhered to their prescribed treatment plans and engaged in daily exercise demonstrated significantly better asthma control. Conversely, factors like passive smoking and a prolonged history of asthma were negatively associated with effective control. These findings underscore the complex interplay of demographic, environmental, and clinical factors in determining asthma outcomes and emphasize the importance of addressing these confounders in asthma management strategies.
Table 2 presents the socio-demographic predictors influencing asthma control among the study participants. In univariate analysis, factors such as occupation, education level, residence, and obesity showed significant associations with asthma control. Participants with management-related jobs or university-level education had better asthma control compared to other groups (p < 0.001), with a weak positive association (effect size η² = 0.01). Rural residents exhibited significantly higher control rates than urban residents (p < 0.001), with a weak positive association (effect size η² = 0.04). Additionally, participants without obesity demonstrated better asthma control compared to those with obesity (p < 0.001).
Multivariate analysis confirmed the independent influence of education level and residence on asthma control, emphasizing the critical role of socio-demographic factors in asthma management. Gender, marital status, and number of children did not show significant associations in either univariate or multivariate analyses. Furthermore, details can be found in Table 2.
Table 3 Highlights the environmental and clinical predictors influencing asthma control among the participants. Univariate analysis revealed that a longer duration of asthma (> 5 years), family history of asthma, non-smoking status, and adherence to the treatment plan were significantly associated with better asthma control (p < 0.001), with a weak positive association (effect size η² = 0.01). Participants with no smoking exposure and those engaging in daily exercise also demonstrated improved asthma control (p < 0.001).
Conversely, factors such as GERD, allergic rhinitis, respiratory tract infections, and non-adherence to the treatment plan were associated with poor asthma control. Multivariate analysis confirmed the independent impact of smoking status, adherence to treatment, and daily exercise as key predictors of asthma management, underscoring the importance of lifestyle modifications and treatment compliance in improving clinical outcomes.
Tables 2 and 3 summarizes crude and adjusted odds ratios (OR) for the association between predictors influencing asthma control and outcome variable in form of control of asthma.
Table 2 summarize the socio-demographic and environmental/clinical predictors influencing asthma control among individuals visiting community pharmacies in Lahore, Pakistan. Table 2 (Socio-Demographic Predictors) presents crude and adjusted odds ratios (OR) for factors such as gender, age, education, and residence. Notably, rural residence (AOR = 0.276, p < 0.001) showed a weak positive association with improved asthma control (effect size η² = 0.04), while obesity (AOR = 0.302, p < 0.001) was also significantly associated with better asthma control, with a weak positive effect (effect size η² = 0.06), compared to their counterparts. However, variables such as marital status and the number of children showed no significant association after adjustment.
Table 3 (Environmental and Clinical Predictors) indicates that adherence to treatment plans (AOR = 2.630, p < 0.001, effect size η² = 0.05) and regular exercise (AOR = 2.124, p = 0.022, effect size η² = 0.03) were strong predictors of improved asthma control. Additionally, a family history of asthma (AOR = 2.682, p = 0.002, effect size η² = 0.01) was associated with a higher likelihood of controlled asthma. In contrast, passive smoking and respiratory tract infections were linked to poorer asthma control (AOR = 0.306, p = 0.007).
Discussion
Asthma is a chronic respiratory disease that effects millions worldwide. The avoidance of trigger factors that exaggerates the onset of acute asthma attacks is the main preventive factor in the management of asthma. However, there are a few socio-demographic and environmental factors that positively contribute towards the onset of acute asthma attacks. The repeated acute asthma exacerbations cause the scaring of the pulmonary tissues that is irreversible. In the similar manner, health related quality of patients is severely affected. The present study was conducted with the aim to observe the socio-demographic, environment and clinical factors that effects the asthma control of patients living in Lahore- capital of Punjab, Pakistan.
A total of 284 asthma patients, visiting multiple community pharmacies were recruited in the study, among which 53.5% of the patients were female while 46.5% of the patients were men, with majority of the patients over the age of 40 years. However, no statistical association of gender with asthma control is observed in the present study. Moreover, age as a socio-demographic factor is not statistically associated with asthma control in adult patients. In the similar manner, a cross sectional observational study conducted in Pakistan in the year 2023, presented similar results i.e., majority of the patients visiting pulmonary department for management of asthma were female patients i.e., 50.2% while most of the patients belonged to the age group of 45–64 years of age31. Similarly, a retrospective cohort study conducted in United Kingdom (UK), extracted primary healthcare data bases of 127,040 patients suffering from asthma in UK. The results of this study presented that majority of the patients with asthma were female patients (60.2%) and most of them belonged to the age group of 35–54 years of age32. The study also presented the findings that asthma is more prevalent in patients with deprived socio-economic status32. The reason might be the fact that patients with low socio-economic status cannot maintain a healthy and standardized quality of living standard as compared to patients with high socio-economic status.
According to the present study, educational status has a statistically significant correlation with asthma control of patients. The patients having college education are observed to have better asthma control as compared to the patients with only school level education. The job status of patients does not have any particular association with asthma control, as observed through the present study.
The current study presented a correlation with area of residence and asthma control of patients. It is observed that patients residing in rural areas have better asthma control as compared to the patients residing in urban areas (p < 0.001). The possible reason could be the better air quality in rural areas because of low traffic burden, agriculture and absence of industries which leads to less exposure to environmental pollutants that could act as trigger factors for asthma exacerbations. Urban areas have poor air quality comparatively, due to traffic burdens and urbanization leading to pollutants and toxins in air that acts as a base for respiratory conditions and asthma exacerbations.
This study highlights a statistically significant association between obesity and poor asthma control in adult patients (p < 0.001). Our findings indicate that 46.3% of non-obese patients had controlled asthma, whereas the majority of obese patients exhibited uncontrolled (30.8%) or partially controlled asthma (48.3%). Several pathophysiological mechanisms may explain this relationship. Obesity contributes to systemic inflammation through increased levels of pro-inflammatory cytokines such as interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α), which have been implicated in airway hyperresponsiveness and asthma exacerbations33. Additionally, increased body weight exerts mechanical pressure on the chest wall and diaphragm, reducing lung volumes and promoting airway narrowing, leading to worsened asthma symptoms34. These findings align with a cross-sectional study conducted at the Pakistan Institute of Medical Sciences (PIMS), Islamabad, on 207 adult asthma patients, which also reported a statistically significant association (p < 0.05) between high BMI and poor asthma control, particularly among obese women31. Similarly, another study recruiting data from 11,868 adults above the age of 18, across the regions of South Carolina presented similar results, stating that asthma tends to be more poorly controlled in obese patients as well as underweight patients. This study also proves a strong statistical association with asthma control and obesity (p < 0.05), emphasizing on the association of healthy lifestyle with asthma control35. A study conducted in Malabar, Kerala, India, involving 100 asthma patients, also demonstrated that obesity is a major factor contributing to poor asthma control in both men and women (p < 0.01), corroborating the global trends observed in different populations36. Obesity is increasingly recognized as a modifiable risk factor for asthma exacerbations, as evidenced by a randomized controlled trial conducted at Ankara University, Turkey. The study demonstrated that structured weight reduction through diet and lifestyle modifications led to significant improvements in asthma control among 55 obese adult patients, emphasizing the critical role of weight management in asthma care37. Similarly, a systematic review by Zeng et al. in 202338 highlighted that weight loss interventions, including dietary adjustments and bariatric surgery, significantly reduce asthma symptoms and the need for medication, further supporting the integration of weight management strategies in asthma treatment. Given the strong association between obesity and poor asthma control, it is imperative that healthcare providers incorporate weight management strategies into routine asthma care. Nutritional counseling, supervised physical activity programs, and behavioral interventions should be implemented alongside pharmacological treatments to achieve optimal asthma control. Future research should explore the long-term effects of structured weight-loss interventions on asthma severity across diverse populations. Additionally, further investigation is needed to determine whether anti-inflammatory therapies targeting obesity-related cytokines may serve as a novel approach to improving asthma outcomes in obese patients.
Our study found a statistically significant association between family history of asthma and asthma control (p < 0.002). Notably, adult patients with a family history of asthma demonstrated better asthma control (46.2%) compared to those without a family history. This finding aligns with a prospective study conducted in Pretoria, South Africa, on asthma patients aged 13–18 years, which identified family history as a strong predictor of asthma incidence. Interestingly, the study also reported that a majority of patients with a family history of asthma exhibited better-controlled asthma14. The improved asthma control observed in patients with a family history of the disease can be attributed to several factors. First, individuals with affected family members are likely to have greater awareness and understanding of asthma management, leading to better adherence to treatment plans and preventive strategies39. Additionally, such patients are more likely to recognize and avoid common asthma triggers, such as allergens and environmental pollutants, reducing the frequency of exacerbations40. Another possible explanation is that healthcare-seeking behavior is more proactive among individuals with a family history, resulting in earlier diagnosis, timely medication use, and better long-term disease control41. These findings highlight the importance of patient education and awareness in asthma management. Healthcare professionals should leverage family involvement in asthma education programs to reinforce disease knowledge and encourage adherence to treatment. Future research should explore the impact of genetic predisposition and environmental factors on asthma control to develop targeted interventions. Additionally, healthcare systems should emphasize early screening and preventive strategies for individuals with a strong family history of asthma to enhance disease management outcomes.
Our study found a statistically significant but weak association between cigarette smoking and asthma control (p < 0.05). This suggests that while smoking may influence asthma management, its impact is not as pronounced as other factors such as obesity or family history. These findings align with a study conducted among college students in South Africa, which reported that the majority of individuals with controlled asthma did not have a history of smoking14. Similarly, a prospective observational study involving 176 adult asthma patients across France and Spain demonstrated that current smokers exhibited worsened clinical outcomes and reduced asthma control42. The detrimental effect of smoking on asthma control is well-documented. Cigarette smoke—both active and passive—is a well-established trigger for asthma exacerbations, leading to increased airway inflammation, mucus hypersecretion, and bronchial hyperresponsiveness43. Long-term smoking has also been associated with corticosteroid resistance, making asthma treatment less effective and contributing to poor disease management44. Additionally, smoking-related oxidative stress can impair lung function and accelerate disease progression, further worsening asthma control45. Given the well-established link between smoking and poor asthma outcomes, healthcare providers should emphasize smoking cessation as a core component of asthma management. Public health campaigns should raise awareness about the risks of smoking in asthma patients, while targeted interventions—such as smoking cessation programs—should be integrated into asthma care plans. Future studies should explore the long-term effects of smoking cessation on asthma control to strengthen clinical recommendations. In summary, while our study observed a weak positive association between cigarette smoking and asthma control, existing literature strongly suggests that smoking contributes to worsened asthma outcomes. Proactive measures, including patient education and smoking cessation programs, are essential to improve disease management and enhance overall respiratory health in asthma patients.
Our study found a statistically significant association between respiratory tract infections (RTIs) and asthma control in adult asthmatics (p < 0.007). Among asthma patients with RTIs, only 24.2% had controlled asthma, whereas 32.8% had uncontrolled asthma and 43% had partially controlled asthma. These findings suggest that respiratory infections can negatively impact asthma management, leading to poorer disease control. This observation is consistent with existing literature, which indicates that bacterial and viral respiratory infections are major contributors to asthma exacerbations. A study by Johnston (2020) found that viral RTIs, particularly those caused by rhinoviruses, significantly increase airway inflammation, leading to bronchial hyperresponsiveness and worsened asthma symptoms46. Similarly, a large-scale cohort study conducted across European hospitals confirmed that bacterial infections in asthma patients are associated with increased airway obstruction and reduced response to standard asthma treatments47. The biological mechanism underlying this association is well-documented. Respiratory tract infections trigger an exaggerated immune response, leading to excessive inflammation, mucus hypersecretion, and airway remodeling, which contribute to airway narrowing and congestion48. Moreover, infections can impair mucociliary clearance, increasing the risk of secondary bacterial colonization and prolonged inflammatory episodes, further worsening asthma control49. Given the strong link between RTIs and asthma exacerbations, preventive strategies such as timely vaccination (influenza and pneumococcal vaccines) should be emphasized in asthma management. Additionally, early detection and treatment of infections with appropriate antibiotics or antiviral agents may help mitigate their impact on asthma control. Patients should also be educated on infection prevention strategies, including hand hygiene, avoiding close contact with sick individuals, and maintaining optimal asthma medication adherence.
According to the present study, adherence with the given treatment plan is positively associated with the asthma control, having a statistically significant association (p < 0.001). Majority of the respondents (45.2%) that presented adherence with the given treatment plan had controlled asthma. The probable reason could be the fact that, asthma treatment plan adherence would prevent asthma exacerbations leading to enhanced asthma control. Similar results were obtained in a prospective, observational cohort study conducted on 1011 adult asthma patients across fourteen health clinics of Malaysia, that presented a significant association of medication therapy adherence in asthma control of the patients. Among the patients presenting non-adherence (forgetting to take their medication on time) with medication treatment plan, 56% had partially controlled asthma and 52% had uncontrolled asthma as observed through the spirometry findings50. In a similar manner, a retrospective study conducted upon 155 asthma patients of Denmark belonging to the age group of 10–22, suggested similar results i.e., almost half of the respondents with uncontrolled asthma presented non-adherence with the prescribed medication, suggesting that special efforts should be put on to enhance adherence in children, especially with the inhaled corticosteroids51.
The findings of the present study illustrate the importance of exercise in asthma control. A statistically significant (p-value = 0.022) association of daily exercise is observed with control of asthma in patients. The possible reason could be the fact that, daily exercise and healthy life style helps in reducing inflammation, strengthening muscles and avoiding obesity. These factors positively contribute towards avoidance of asthma exacerbations and improving health related quality of life of asthma patients. The findings of our study are strengthened by the results of a randomized controlled trial conducted upon 53 children and adolescents of age 7–17 years, recruited from Madrid, Spain52. The intervention group performed exercise (aerobics and resistance) for a time period of 12 weeks, three days in a week for 1 h. The study presented the findings that combined- aerobic and resistance strength training exercise significantly improved muscle strength as well as respiratory muscles strength in interventional group, emphasizing the importance of daily exercise in asthma control52. Another systematic review and meta-analysis evaluating the impact of physical activity on asthma outcomes found that moderate-intensity exercise improves airway hyperresponsiveness and reduces exacerbation frequency in asthmatic patients, supporting the argument that physical training should be an integral part of asthma management53. Furthermore, a cohort study conducted in Brazil involving 150 adult asthmatics reported that individuals who engaged in at least 150 min of moderate exercise per week exhibited better asthma control, improved pulmonary function, and fewer emergency visits compared to sedentary individuals54. This evidence suggests that structured exercise programs tailored for asthmatic patients should be encouraged to optimize disease control and improve long-term outcomes.
Our study highlights the impact of various socio-demographic, environmental, and clinical factors on asthma control in adult patients. Key predictors identified include education level, residential area, obesity, disease duration, family history, smoking status, respiratory tract infections, daily physical activity, and adherence to prescribed medication. These factors demonstrated a positive association with effective asthma management. Given these findings, individualized patient counseling is essential, emphasizing smoking cessation, weight management, regular exercise, and medication adherence to improve asthma control and overall health outcomes.
Conclusion
In conclusion, this study emphasizes the significant impact of socio-demographic, environmental, and clinical factors on asthma control in adult patients. Key determinants such as education level, obesity, family history, smoking, respiratory tract infections, adherence to treatment, and physical activity were identified as crucial factors influencing asthma management. While some factors, like obesity and smoking, were linked to poorer asthma control, others, including educational attainment and rural residency, contributed to better asthma outcomes. The study highlights that environmental factors, such as urban area residence and poor living conditions, especially in lower-income countries like Pakistan, significantly influence disease management. Therefore, factors like obesity, smoking, daily exercise, and medication adherence should be addressed through patient counseling and public health interventions. A multifaceted approach, including patient education, lifestyle modifications, and personalized treatment plans, is essential for improving asthma control and enhancing patients’ quality of life. Future research should further explore the long-term effects of these factors and the potential benefits of targeted interventions, such as weight management and smoking cessation programs, to prevent asthma exacerbations and improve overall health outcomes.
Strengths and limitations
This study’s strengths include its comprehensive exploration of socio-demographic, environmental, and clinical factors influencing asthma control, making it one of the few studies to focus on a multifaceted approach. The inclusion of diverse variables such as education level, obesity, smoking, and treatment adherence provides a holistic view of asthma management. The findings are particularly relevant for lower-income countries like Pakistan, where socio-environmental factors play a critical role in disease outcomes. Moreover, the study’s emphasis on practical interventions, such as patient counseling and public health initiatives, offers actionable recommendations for improving asthma control and patient quality of life. These strengths contribute to the study’s overall relevance in shaping future research and health policies in asthma management.
Despite the valuable insights provided by this study, several limitations must be acknowledged. Firstly, the cross-sectional design limits the ability to establish causal relationships between the identified factors and asthma control. Additionally, the study’s reliance on self-reported data, particularly concerning lifestyle factors such as smoking, physical activity, and medication adherence, may introduce recall bias or inaccuracies. The sample size and demographic characteristics of the participants might also limit the generalizability of the findings, especially in rural or underrepresented populations. Furthermore, environmental factors, such as air pollution or occupational hazards, were not extensively examined, which may also play a significant role in asthma exacerbations. Lastly, the study’s focus on adult patients limits the applicability of the findings to pediatric or geriatric populations.
Data availability
All data generated or analysed during this study are included in this published article and the datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Dharmage, S. C., Perret, J. L. & Custovic, A. Epidemiology of asthma in children and adults. Front. Pead. 1–15. https://doi.org/10.3389/fped.2019.00246 (2019).
Cevhertas, L. et al. Advances and recent developments in asthma in 2020. Allergy: Eur. J. Allergy Clin. Immunol. 75 (12), 3124–3146. https://doi.org/10.1111/all.14607 (2020).
He, Z. et al. Frequency of signs and symptoms in persons with asthma. Respir. Care. 65 (2), 252–264. https://doi.org/10.4187/respcare.06714 (2020).
Murrison, L. et al. Environmental exposures and mechanisms in allergy and asthma development. J. Clin. Invest. 129 (4), 1504–1515. https://doi.org/10.1172/JCI124612 (2019).
Razzaq, S. et al. Epidemiology of asthma and associated factors in an urban Pakistani population: adult asthma Study-Karachi. BMC Pulm. Med. 18 (1), 1–13. https://doi.org/10.1186/s12890-018-0753-y (2018).
Sio, Y. Y. & Chew, F. T. Risk factors of asthma in the Asian population: A systematic review and Meta-Analysis. J. Physiol. Anthropol. 40 (1), 1–17. https://doi.org/10.1186/s40101-021-00273-x (2021).
Das, A. Living with Chronic Asthma: Navigating Lifelong Care and Healthcare Costs Living with Chronic Asthma : Navigating Lifelong Care and Healthcare Costs, no. July, 10–15. (2024). https://doi.org/10.62469/ijnhc.v02i04.001
Mazurek, J. M., Syamlal, G. & Emergency Department Visits for Asthma Among Working Adults — National Health Interview Survey. Prevalence of Asthma, Asthma Attacks, and, 2011– MMWR. Morbidity and Mortality Weekly Report 2018, 67 (13): 377–86. (2016). https://doi.org/10.15585/mmwr.mm6713a1
Gherasim, A., Dao, A. & Bernstein, J. A. Confounders of severe asthma: diagnoses to consider when asthma symptoms persist despite optimal therapy. World Allergy Organ. J. 11 (1), 1–11. https://doi.org/10.1186/s40413-018-0207-2 (2018).
Tomisa, G. & Horváth, A. Balázs Sánta, András Keglevich, and Lilla Tamási. Epidemiology of comorbidities and their association with asthma control. Allergy Asthma Clin. Immunol. 17 (1), 1–14. https://doi.org/10.1186/s13223-021-00598-3 (2021).
Soledade-Marques, K. et al. Simone Seixas da Cruz, Johelle de Santana Passos-Soares, Soraya Castro Trindade, Eneida de Moraes Marcílio Cerqueira, Julita Maria Freitas Coelho,. Association between Periodontitis and Severe Asthma in Adults: A Case–Control Study. Oral Diseases 24 (3): 442–48. (2018). https://doi.org/10.1111/odi.12737
Azizpour, Y., Delpisheh, A., Montazeri, Z., Sayehmiri, K. & Darabi, B. Effect of childhood BMI on asthma: A systematic review and Meta-Analysis of Case-Control studies. BMC Pediatr. 18 (1), 1–13. https://doi.org/10.1186/s12887-018-1093-z (2018).
Boker, F., Alzahrani, A. J., Alsaeed, A., Alzhrani, M. & Albar, R. Cesarean section and development of childhood bronchial asthma: is there A risk?? Open. Access. Macedonian J. Med. Sci. 7 (3), 347–351. https://doi.org/10.3889/oamjms.2019.085 (2019).
Garrach, B., Kalidas, K. & Mpe, M. J. Asthma control among teenagers attending the respiratory outpatient clinic of an academic hospital in Pretoria, South Africa. J. Pan Afr. Thorac. Soc. 5, 62–68. https://doi.org/10.25259/JPATS_4_2024 (2024).
Plaza-González, S., Zabala-Baños, M. D., Astasio-Picado, Á. & Jurado-Palomo, J. Psychological and Sociocultural determinants in childhood asthma disease: impact on quality of life. Int. J. Environ. Res. Public Health. 19 (5), 2652 (2022).
Dhar, R. et al. ICS/Ultra LABA in the treatment of obstructive airway diseases: A consensus of Indian experts. Adv. Respiratory Med. 90 (5), 407–424. https://doi.org/10.3390/arm90050051 (2022).
Tohidinik, H., Reza, N., Mallah & Takkouche, B. History of allergic rhinitis and risk of asthma; a systematic review and Meta-Analysis. World Allergy Organ. J. 12 (10), 100069. https://doi.org/10.1016/j.waojou.2019.100069 (2019).
Holst, G. J. et al. Air pollution and family related determinants of asthma onset and persistent wheezing in children: nationwide Case-Control study. BMJ 370, 1–9. https://doi.org/10.1136/bmj.m2791 (2020).
Zheng, X., Orellano, P., Lin, H. & Jiang, M. Short-Term exposure to Ozone, nitrogen dioxide, and sulphur dioxide and emergency department visits and hospital admissions due to asthma: A systematic review and Meta-Analysis. Environ. Int. 150, 106435. https://doi.org/10.1016/j.envint.2021.106435 (2021).
Agache, I. et al. The impact of indoor pollution on asthma-Related outcomes: A systematic review for the EAACI guidelines on environmental science for allergic diseases and asthma. Allergy: Eur. J. Allergy Clin. Immunol. 79 (7), 1761–1788. https://doi.org/10.1111/all.16051 (2024).
Papi, A. et al. Inhaled Long-Acting Muscarinic Antagonists in Asthma – A Narrative Review. European Journal of Internal Medicine 85 (October 2020): 14–22. (2021). https://doi.org/10.1016/j.ejim.2021.01.027
Batmaz, S. et al. Seasonal variation of asthma control, lung function tests and allergic inflammation in relation to vitamin D levels: A prospective annual study. Postepy Dermatologii I Alergologii. 35 (1), 99–105. https://doi.org/10.5114/ada.2017.71421 (2018).
Muneswarao, J., Hassali, M. A., Ibrahim, B., Saini, B. & Ali, I. A. H. It is time to change the way we manage mild asthma: an update in GINA 2019. Respir. Res. 20 (1), 1–6. https://doi.org/10.1186/s12931-019-1159-y (2019).
Hour, O. N. E. Managing asthma in the dental practice, 422–425. (2024). https://doi.org/10.1038/s41407-024-2786-9
Beasley, R., Bruce, P., Hatter, L. & Claire Houghton, and The ICS/Formoterol reliever therapy regimen in asthma: A review. J. Allergy Clin. Immunology: Pract. 11 (3), 762–772e1. https://doi.org/10.1016/j.jaip.2023.01.002 (2023).
Hatter, L. et al. ICS-Formoterol reliever versus ICS and Short-Acting Β 2 -Agonist reliever in asthma: A systematic review and Meta-Analysis. ERJ Open. Res. 7 (1), 00701–02020. https://doi.org/10.1183/23120541.00701-2020 (2021).
WHO. Asthma WHO. World Health Organization. (2022). https://www.who.int/news-room/fact-sheets/detail/asthma#:~:text=Asthma is a major non-communicable,of breath and chest tightness.
Reuter, S., Raspe, J. & Taube, C. Microbes little helpers and suppliers for therapeutic asthma approaches. Respir. Res. 25 (1), 1–20. https://doi.org/10.1186/s12931-023-02660-7 (2024).
Pelaia, C. et al. Molecular targets for biological therapies of severe asthma. Front. Immunol. 11 (November), 1–11. https://doi.org/10.3389/fimmu.2020.603312 (2020).
Bleecker, E. et al. Comparative effectiveness of dupilumab and Omalizumab on asthma exacerbations and systemic corticosteroid prescriptions: Real-World US ADVANTAGE study. J. Allergy Clin. Immunol. 1–11. https://doi.org/10.1016/j.jaci.2024.07.029 (2024).
Shahid, S. et al. The effect of obesity on severity of asthma: an observational prospective study from Pakistan. J. Pharm. Bioallied Sci. 16 (1), 38–43. https://doi.org/10.4103/jpbs.jpbs_238_23 (2024).
Busby, J. et al. Impact of socio-economic status on adult patients with asthma: a population-based cohort study from UK primary care. J. Asthma Allergy 2021 Nov 10:1375–1388. https://doi.org/10.2147/JAA.S326213
Zhou, Y., Wang, T., Zhao, X., Wang, J. & Wang, Q. Plasma metabolites and gut microbiota are associated with T cell imbalance in BALB/c model of eosinophilic asthma. Front. Pharmacol. 13, 819747. https://doi.org/10.3389/fphar.2022.819747 (2022).
Peters, U., Dixon, A. E. & Forno, E. Obesity and asthma. J. Allergy Clin. Immunol. 141 (4), 1169–1179. https://doi.org/10.1016/j.jaci.2018.02.004 (2018).
Liu, Y. et al. Body mass index, respiratory conditions, asthma, and chronic obstructive pulmonary disease. Respir. Med. 109 (7), 851–859. https://doi.org/10.1016/j.rmed.2015.05.006 (2015).
Chandrasekhar, D. et al. An observational study to assess the prevalence and impact of obesity in asthma management. J. Young Pharmacists. 11 (3), 291. https://doi.org/10.5530/jyp.2019.11.58 (2019).
Özbey, Ü. et al. The effects of diet-induced weight loss on asthma control and quality of life in obese adults with asthma: a randomized controlled trial. J. Asthma. 57 (6), 618–626. https://doi.org/10.1080/02770903.2019.1590594 (2020).
Zeng, N. et al. A systematic review and meta-analysis of long term physical and mental sequelae of COVID-19 pandemic: call for research priority and action. Mol. Psychiatry. 28 (1), 423–433. https://doi.org/10.1038/s41380-022-01614-7 (2023).
Forno, E. & Celedón, J. C. Asthma and ethnic minorities: socioeconomic status and beyond. Curr. Opin. Allergy Clin. Immunol. 9 (2), 154–160. https://doi.org/10.1097/ACI.0b013e3283292207 (2009).
Muneeb Hassan, M., Ameeq, M., Jamal, F., Tahir, M. H. & Mendy, J. T. Prevalence of covid-19 among patients with chronic obstructive pulmonary disease and tuberculosis. Ann. Med. 55 (1), 285–291. https://doi.org/10.1080/07853890.2022.2160491 (2023).
Castro-Rodríguez, J. A., Forno, E. & Asthma COVID-19 in children: A systematic review and call for data. Pediatr. Pulmonol. 55 (9), 2412–2418. https://doi.org/10.1002/ppul.24909 (2020).
Tiotiu, A. I. et al. Impact of air pollution on asthma outcomes. Int. J. Environ. Res. Public Health. 17 (17), 6212. https://doi.org/10.3390/ijerph17176212 (2020).
Thomson, N. C. The role of smoking in asthma and chronic obstructive pulmonary disease overlap. Immunol. Allergy Clin. North. Am. 42 (3), 615–630. https://doi.org/10.1016/j.iac.2022.03.004 (2022).
Kim, K. W. & Ober, C. Lessons learned from GWAS of asthma. Allergy Asthma Immunol. Res. 11 (2), 170–. https://doi.org/10.4168/aair.2019.11.2.170 (2018). 87.
Kerstjens, H. A. et al. Efficacy and safety of benralizumab in patients with severe asthma: a randomized, double-blind, placebo-controlled trial. Lancet Respir Med. 6 (10), 805–815. https://doi.org/10.1016/S2213-2600(18)30222-0 (2018).
Johnston, S. L. & Asthma COVID-19: is asthma a risk factor for severe outcomes? Allergy 75 (7), 1543–1545. https://doi.org/10.1111/all.14348 (2020).
Papadopoulos, N. G., Moustaki, M. & Tsolia, M. Management of acute asthma exacerbations in children: A review of current guidelines. Pediatr. Drugs. 21 (1), 1–14 (2019). https://pubmed.ncbi.nlm.nih.gov/30592856/
Hassan, M. M. et al. Risk factors identification of COVID-19 patients with chronic obstructive pulmonary disease: A retrospective study in Punjab‐Pakistan. Immun. Inflamm. Dis. 11 (8), e981. https://doi.org/10.1002/iid3.981 (2023).
Zhao, X. et al. The role of gut Microbiome in the complex relationship between respiratory tract infection and asthma. Front. Microbiol. 14, 1219942. https://doi.org/10.3389/fmicb.2023.1219942 (2023).
Isa, N. M. et al. Asthma control and asthma treatment adherence in primary care: results from the prospective, multicentre, non-interventional, observational cohort ASCOPE study in Malaysia. E Med. J. Malaysia. 75 (4), 331–337 (2020).
Marckmann, M., Hermansen, M. N., Hansen, K. S. & Chawes, B. L. Assessment of adherence to asthma controllers in children and adolescents. Pediatr. Allergy Immunol. 31 (8), 930–937. https://doi.org/10.1111/pai.13312 (2020).
Sanz-Santiago, V. et al. Effect of a combined exercise program on physical fitness, lung function, and quality of life in patients with controlled asthma and exercise symptoms: A randomized controlled trial. Pediatr. Pulmonol. 55 (7), 1608–1616. https://doi.org/10.1002/ppul.24798 (2020).
Kuder, M. M. et al. A systematic review of the effect of physical activity on asthma outcomes. J. Allergy Clin. Immunology: Pract. 9 (9), 3407–3421. https://doi.org/10.1016/j.jaip.2021.04.048 (2021).
de Andrade, L. B., Britto, M. C., Lucena-Silva, N., Gomes, R. G. & Figueroa, J. N. The efficacy of aerobic training in improving the inflammatory component of asthmatic children. Randomized Trial Respiratory Med. 108 (10), 1438–1445. https://doi.org/10.1016/j.rmed.2014.07.009 (2014).
Funding
The authors thank the Deanship of Scientific Research at King Khalid University for funding this work through the large Groups Project Under grant number (RGP.2/578/45).
Author information
Authors and Affiliations
Contributions
Conceptualization, MZI; Formal analysis, MZI; Funding acquisition, SSA; Investigation, SSA; Methodology, SS; Project administration, MZI; Resources, SSA; Supervision, MZI; Visualization, MZI; Writing – original draft, SS; Writing review & editing, SSA and MZI, NM; Revising – updated draft, SS; Writing review & editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Iqbal, M.Z., Alqahtani, S.S., Shahid, S. et al. Socio-demographic environmental and clinical factors influencing asthma control in community pharmacies of Lahore Pakistan. Sci Rep 15, 10587 (2025). https://doi.org/10.1038/s41598-025-95373-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-95373-4