Abstract
Studies examined one aspect of sleep health (sleep duration) as a risk factor for developing obesity. Approaching sleep health as a multidimensional model can better assess this association. This study investigated the role of gender in moderating the relationship between obesity and sleep health, adopting a multidimensional perspective on sleep health. This was a nationally representative cross-sectional survey using a multi-stage random clustering method. We included a cohort of 3198 individuals. We used STOP-BANG, Insomnia Severity Index, and self-report questions to define six sleep health domains: alertness, satisfaction, timing, efficiency, regularity, and duration. The Chi-square test evaluated the relationship between obesity and dichotomized sleep health dimensions. Logistic regression models determined the best predictors of obesity based on sleep health dimensions, adjusted for confounding factors. The mean age and body mass index of participants were 39.7 years and 26.5 kg/m2, respectively. Of all, 62.4%, 55.2%, 52.5%, 52.3%, and 49.2% had unhealthy traits of sleep satisfaction, alertness, sleep regularity, sleep timing, and sleep efficiency, respectively. Obesity in women was associated with unhealthy daytime alertness (Adjusted-OR 1.30, p 0.013), unhealthy sleep regularity (Adjusted-OR 1.23, p 0.016), and surprisingly healthy sleep efficiency (Adjusted-OR 0.80, p 0.019). Obesity in men was associated with unhealthy sleep satisfaction (Adjusted-OR 1.26, p 0.001) and healthy daytime alertness (Adjusted-OR 0.61, p 0.001). In conclusion, sleep regularity, satisfaction, and daytime alertness were associated with obesity, and gender moderated this association. Multiple domains of sleep health could influence maintaining a healthy weight that warrants the attention of public health agendas.
Similar content being viewed by others
Introduction
The International Classification of Diseases (ICD) defines obesity as a disease; obesity is now considered a significant risk factor for noncommunicable diseases (NCDs), including diabetes and cardiovascular diseases1,2. Over 1 billion individuals worldwide are expected to have body mass index (BMI) of ≥ 30 kg/m2 by 2030, meaning 1 in 5 women and 1 in 7 men. Unfortunately, none of the nations is on track to achieve the WHO’s 2025 goals for reducing obesity, and the prevalence of obesity is expected to rise globally. Iran is expected to have around 14 million women with obesity and 9 million men with obesity by 2030. Moreover, Iran is one of the eleven countries that account for 50% of the world’s women with obesity3.
Given the importance of obesity, being aware of its associated factors is necessary for preventive and therapeutic interventions. Previous studies have examined the relationship between sleep health and obesity4,5,6,7,8,9,10,11,12,13,14,15,16. Almost all of these studies examined one aspect of sleep health, mainly sleep duration, as a risk factor for developing obesity.
Circadian disruption significantly impacts metabolic processes, contributing to obesity and metabolic diseases. The circadian system orchestrates the timing of metabolic activities in peripheral tissues. Disruptions in the circadian clock, either through genetic mutations or environmental factors, disturb the coordination between the central clock and peripheral clocks. This misalignment affects the timing of food intake and energy expenditure, leading to metabolic dysregulation. This metabolic dysregulation underscores the potential link between sleep disorders and the development of obesity17.
A recent umbrella review found a strong association between short sleep duration and increased risk of obesity, overweight, and combined obesity and overweight risk. There is also suggestive evidence linking poor sleep quality to an increased risk of obesity and overweight. However, this evidence is not as strong or conclusive as that for sleep duration, indicating the need for further high-quality research to establish a definitive relationship18.
According to a recent review on the genetics of sleep and obesity, investigations of the associations between sleep and obesity for sleep disorders other than insomnia and in non-European populations are limited19. In addition, sleep is mainly ignored as an essential pillar of health in the pathogenesis and management of obesity at the national level in the different health sectors. Research on sleep health in low- and middle-income countries is significantly underdeveloped compared to high-income countries, despite a high prevalence of sleep problems. The limited research efforts in these countries are primarily due to scarce resources and competing health priorities, underscoring a critical need to focus more on sleep health to address this significant public health challenge20.
Several studies reported a significant association between sleep duration and obesity, most clearly in children and less consistently in adults4,5,6,7,8,9,12,13,14,16, while several other studies reported no significant association10,11,15. However, a recent umbrella study suggested a strong relationship between obesity and sleep duration but a less significant relationship between sleep quality and obesity, indicating the need for further research18.
Not only different studies have yielded different findings regarding the relationship between sleep duration and obesity, but focusing just on sleep duration is not a perfect strategy for investigating the association between sleep health and obesity. Sleep health is not limited to sleep length or sleep disorders. Different domains have been defined for this pillar of health, but it has received less attention from researchers worldwide. Compared to isolated sleep characteristics, operationalizing sleep as a multidimensional concept can provide a more accurate estimate of sleep’s role as a risk factor for obesity.
To the authors’ knowledge, limited studies have investigated sleep as a risk factor for obesity using multidimensional sleep health domains. In one study on 221 midlife white, African American, and Chinese women, improved sleep health was associated with lower adiposity in unadjusted but not adjusted models21. To evaluate the relationship between sleep and obesity, it is necessary to do a study with a large sample size of both women and men, especially in Middle Eastern populations, with a multidimensional view of sleep health.
This study aimed to investigate the relationship between obesity, a prevalent NCD, and sleep health as a major health concern and ignored pillar of health in a low and middle-income country and to study the role of gender in moderating this relationship.
Methods
Study design
We conducted a cross-sectional population-based study from 2017 to 2020 in 7 randomly selected provinces of Iran. We administered reliable and validated Persian questionnaires, and our trained staff collected self-reported symptoms and conducted physical examinations. The study received approval and funding from the Ethics Committee of the National Institute for Medical Research Development (IR NIMAD REC 1396 102) with grant number 957,726.
Sampling method
Selecting provinces and health care centers
Seven out of thirty-one provinces were randomly selected for this study, with the sample size for each province determined based on its total population. To achieve the desired sample size, both urban and rural healthcare centers (HCCs) were randomly chosen in each province. Approximately 75% of the targeted sample size was collected from urban HCCs, while 25% was collected from rural HCCs.
After selecting the provinces and HCCs, the funding institute (NIMAD) made the necessary arrangements with the vice-chancellors of health in the chosen provinces. Subsequently, a collaborator was designated for each province by the provincial deputy for further cooperation. An epidemiologist and a sleep medicine physician then visited each province to provide training to the staff on the study objectives, using the study instruments, and general education on sleep health, sleep disorders, obstructive sleep apnea (OSA), and treatment methods.
Selecting the participants
The population of each HCC was sampled using household codes recorded in the area. The executive team at the Occupational Sleep Research Center at Baharloo Hospital in Tehran was responsible for selecting the household codes for the healthcare center clusters.
In collaboration with the trained HCC personnel, two professional interviewers visited the selected households and provided an overview of the study objectives. Inclusion criteria required participants to be adults aged 18 years and older, residents of the selected provinces, and willing to participate in the study. Exclusion criteria included individuals with severe cognitive impairments or communication difficulties that would prevent them from completing the questionnaires, as well as non-residents or temporary visitors in the selected provinces. One male and one female, both Iranian and at least 18 years old, who consented to participate in the study were selected from each household. Oral informed consent was obtained, after which the interviewers moved on to the household to the right of the previously selected one and repeated the process. Sampling continued using this method until each cluster included 20 individuals, with 10 males and 10 females evenly distributed across five age groups (18–25, 25–35, 35–45, 45–55, and > 55 years old). If the eligible participant was not available in a household, the interviewers conducted further follow-up over the next few days or continued sampling until the designated cluster was complete.
Participants completed the Persian versions of the STOP-BANG22, the Insomnia Severity Index (ISI)23, and the International Restless Legs Syndrome Study Group (IRLSSG) questionnaires24, along with questions related to their sleeping habits. A STOP-BANG score of ≥ 3 indicated a high risk for OSA, an ISI score of ≥ 8 indicated insomnia, and four “yes” responses on the IRLSSG questionnaire indicated restless legs syndrome (RLS).
Following the completion of questionnaires, residents were provided with information on sleep health, sleep disorders, OSA, and treatment methods. This information was also provided to anyone who declined to participate. After the interviews and anthropometric measurements, each household was given a pamphlet that included the contact information of our research center and the logo of the province medical university. The pamphlet featured color illustrations and provided information on the symptoms, adverse health effects, methods of diagnosis, and treatments of OSA, as well as a table for calculating an individual’s risk of OSA based on the STOP-BANG score. We had three quality control checks. HCC supervisors conducted the first quality check after the questionnaires were completed, and the second quality check was done by the study executive manager after the questionnaires were sent to the research center. A methodologist did the third quality check before statistical analysis.
Sleep health domains
Building on previous studies by Bowman et al.21 and Chen et al.25, we used their definitions for the following six sleep health domains. Each domain was dichotomized into two categories, “healthy” and “unhealthy”21,25:
-
1.
Alertness: The alertness domain assesses the extent to which a person’s sleep problem interferes with their daily functioning. This includes factors such as daytime fatigue, mood, ability to function at work or perform daily chores, concentration, and memory. It was measured using the ISI questionnaire, where the individual rates the interference on a scale from 0 to 4 (0 being “Not at all” and 4 being “Very much”). Scores of 0–1 were considered healthy, while scores of 2–4 indicated unhealthy21,25.
-
2.
Sleep satisfaction: Sleep satisfaction measures how content a person is with their current sleep pattern. This is also assessed using the ISI questionnaire, where the satisfaction level is rated from 0 to 4 (0 being “Very Satisfied” and 4 being “Very Dissatisfied”). A score of 0–1 indicates healthy sleep satisfaction, whereas scores of 2–4 suggest unhealthy sleep satisfaction21,25.
-
3.
Sleep timing: This domain considers the mid-point between the self-reported exact time a person falls asleep and the self-reported wake-up time. The sleep timing was reported in “hour: minute” format. A healthy sleep timing was considered between 2:00 AM and 3:59 AM. Sleep timings falling before 2:00 AM or after 4:00 AM were categorized as unhealthy21,25.
-
4.
Sleep duration: Sleep duration is the total number of hours of actual sleep a person gets at night over the past month. This was gathered through a self-report question. A healthy sleep duration ranges between 7 and 9 h per night. Sleep duration of < 7 or ≥ 9 h was considered unhealthy21,25.
-
5.
Sleep efficiency: Sleep efficiency was calculated by subtracting sleep duration from the total time in bed, measured in minutes. Efficient sleep was defined as spending less than 30 min awake in bed, while spending ≥ 30 min in bed was considered unhealthy sleep efficiency21,25.
-
6.
Sleep regularity: Sleep regularity assessed the difference in the sleep duration between workdays and weekends. This was measured in minutes, with a healthy range being less than a 60-minute difference. A difference of ≥ 60 min between the two was considered unhealthy21,25.
We used the “PS 502 GR, MATHEO, Germany” weighing scale and the “NTT9650, NOVA, China” measurement tape to measure participants’ weight and height. BMI was calculated as weight in kilograms divided by the square of height in meters. Obesity was defined as BMI ≥ 30 Kg/m2.
Statistical analysis
All statistical analyses were performed using STATA software. Before analyzing the data, the Kolmogorov-Smirnov test was used to evaluate the normality of quantitative variables. Complex sample survey analyses were performed to extrapolate the results to the Iranian adult population. The weight was based on the 2016 national Iranian census to match the age (10-year strata), sex, and area of residence (rural/urban).
Twenty individuals reported a sleep duration of < 60 min; therefore, their information was labeled as missing data, and the mean value for sleep duration was replaced for their sleep duration.
Four hundred and nine participants misreported their time in bed less than their sleep duration, making calculating sleep efficiency not possible; Therefore, the final mean for sleep efficiency was replaced for missing values on sleep efficiency. We used the Chi-square test to assess the relationship between obesity and categorical variables, including dichotomized sleep health dimensions, OSA, RLS, insomnia, education, marital status, and medical history. We used a T-test to examine the age difference between groups. Logistic regression models were used to study the best model for predicting obesity based on sleep health dimensions, after controlling for confounding factors. P-values of less than 0.05 were considered statistically significant.
Results
There were 3198 participants, with a mean age of 39.7 years (95% CI 39.6–39.8), among whom 70.8% were married. BMI was 26.5 Kg/m2 (95% CI 26.1–26.9).
Sleep domains
In the total population, the proportion of healthy traits for each domain was 55.2% for alertness, 62.4% for sleep satisfaction, 52.3% for sleep timing, 49.2% for sleep efficiency, and 52.5% for sleep regularity. In the total population, there were significantly more individuals with unhealthy alertness (55.04% vs. 41.84%, p < 0.001) and sleep satisfaction (41.88% vs. 36.36%, p < 0.01) in the group with obesity compared to the group without obesity. Surprisingly, there were more individuals with unhealthy sleep regularity in the group without obesity (41.54% vs. 49.19, p < 0.01), see Table 1.
In women, there were significantly more individuals with unhealthy alertness (61.96% vs. 47.49%, p < 0.001) and sleep satisfaction (46.90% vs. 40.71%, p:0.04) in the group with obesity, see Table 1.
In men, there were no significant differences in sleep health domains between the groups with and without obesity, except for sleep duration, which was shorter in men with obesity (401.24 ± 92.55 vs. 415.58 ± 99.67, p:0.03), see Table 1.
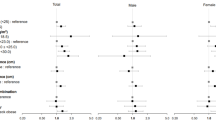
Multiple logistic regressions were done after adjusting for confounding factors of education, marital status, history of diabetes and cardiovascular diseases, RLS, insomnia, and OSA. Individuals with unhealthy sleep satisfaction and regularity were more likely to have obesity (OR: 1.15, 1.12, p-value: 0.09 and 0.04, respectively). Surprisingly, individuals with unhealthy sleep timing were less likely to have obesity (OR: 0.89, p:0.04), Table 2.
Women with unhealthy daytime alertness and sleep regularity were more likely to have obesity (OR: 1.30, 1.23, P-value: 0.013, 0.016, respectively), Table 2.
Men with unhealthy sleep satisfaction were more likely to have obesity (OR:1.26, p:0.001), while men with unhealthy daytime alertness were less likely to have obesity (OR: 0.61, p:0.001), Table 2.
Age trend
In the group with obesity, the lowest frequency of healthy alertness was observed in middle-aged women (50–60 years) and 30–40 year-old men. Middle-aged women (50–60 years) and men (40–50 years) reported the lowest levels of sleep satisfaction among individuals with obesity. Participants aged 18–20 years in women and 20–30 years in men had the least healthy sleep timing. Among individuals with obesity, both men and women aged 20–30 years old had the least efficient sleep, while women and men aged 30–40 years old had the least regular sleep pattern (supplementary Tables S1-S5).
Discussion
This study assessed the associations between obesity and multidimensional sleep health domains in women and men. After adjusting for confounding factors, obesity in women was associated with unhealthy daytime alertness, unhealthy sleep regularity, and surprisingly healthy sleep efficiency, and obesity in men was associated with unhealthy sleep satisfaction and healthy daytime alertness. However, there was no observed association between obesity and sleep duration or timing in both women and men.
Previous research studying the relationship between sleep health and obesity has concentrated chiefly on one aspect of sleep, mainly sleep duration. To date, we could find only two studies that investigated sleep as a risk factor for obesity using multidimensional sleep health domains21,26. Of these two studies, Bowman et al.21 studied only 221 women, and Hawkins et al.26 studied the effect of sleep health on individuals’ attempts to weight loss rather than obesity.
In our study and those of Bowman et al.21 and Hawkins et al.26, neither sleep duration nor timing was associated with a higher BMI. Throughout these years, the most studied aspect of sleep in relation to obesity was sleep duration, and different studies yielded different results. However, several meta-analyses investigated this relationship and found that short sleep duration (less than 7 h) is associated with obesity while longer sleep duration is not27,28,29. This discrepancy between our research and Bowman’s study with previous studies may be because we identified sleep duration as one dimension of sleep health and characterized it as a categorical variable defining unhealthy sleep duration as < 7 h or ≥ 9 h. Several prior research studies concur with our finding that, after adjusting for confounding factors, there was no association between sleep duration and obesity5,10,11.
One possible explanation for the association between sleep duration and obesity is the impact of sleep deprivation on various physiological factors. Sleep deprivation has been linked to decreased levels of leptin and insulin sensitivity, as well as elevated levels of ghrelin, salt retention, and inflammatory markers28. Obesity and sleep were found to have a bidirectional relationship. Sleep deprivation causes metabolic changes that raise body weight, insulin resistance, and blood pressure. As a result, treatments and primary prevention strategies for metabolic disorders such as obesity may involve interventions that increase the amount and duration of sleep. Sleep deprivation was linked to decreased levels of leptin and insulin sensitivity, as well as elevated levels of ghrelin, salt retention, and inflammatory markers. Obesity and sleep were found to have a bidirectional relationship. Although the mechanism is unclear, sleep deprivation causes metabolic changes that raise body weight, insulin resistance, and blood pressure30,31.
Furthermore, consistent with the results of Bowman and Hawkin’s studies, there was no significant association between sleep timing and obesity. However, Patel et al., in a study of 3053 men and 2985 women using actigraphy, found a significant association between late sleep mid-time and higher BMI in women32. It’s important to note that different methodologies and sample characteristics may contribute to the variations in findings. Further research is needed to better understand the relationship between sleep timing and obesity.
The concept of chronotype, which refers to an individual’s preference for morningness or eveningness, plays a crucial role in sleep patterns and overall health. Chronotype is closely linked to circadian rhythms, the natural, internal processes that regulate the sleep-wake cycle and repeat roughly every 24 h. Variations in chronotype can lead to circadian disruption, particularly when there is a misalignment between an individual’s internal clock and their external environment. This misalignment can contribute to various health issues, including metabolic disorders, obesity, and cardiovascular diseases33.
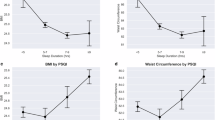
The analysis of sleep timing across different age groups revealed that individuals in the 18–20 and 20–30 age ranges, typically considered younger age brackets, and displayed less healthy sleep timing34 (Fig. 1a, b and c, and 1d; Supplementary Tables S1-S5). Sleeping late among young adults is common and influenced by various factors. One contributing factor is the natural biological changes that occur during adolescence and early adulthood. At this stage, there is a shift in the circadian rhythm, known as the “delayed phase”, which results in young individuals feeling more alert and staying awake later at night. Social and lifestyle factors also contribute to late sleep timing in young adults. The demands of academic commitments, work responsibilities, social activities, and personal interests often lead to busy schedules. Late-night studying, working evening shifts, and engaging in social events can keep young adults awake until late hours, thereby delaying their bedtime. The prevalence of modern technology further exacerbates the issue of sleeping late among young adults. Electronic devices like smartphones, tablets, and computers emit blue light, which suppresses the release of melatonin, a hormone that helps regulate the sleep-wake cycle. Engaging with these devices in the evening can disrupt the natural sleep-wake cycle, leading to delayed sleep onset.
Partonen highlights that evening chronotypes, or “night owls,” are more prone to circadian disruption due to their tendency to stay up late and sleep in late, which often conflicts with societal norms and schedules. This misalignment has been associated with metabolic syndrome, obesity, and type 2 diabetes33. Furthermore, circadian disruption, such as that experienced by shift workers, has been shown to impact glucose tolerance and insulin sensitivity, further linking circadian misalignment to metabolic health33.
Unhealthy sleep regularity, defined as the difference in nightly sleep duration between workdays and work-free days, was associated with higher BMI in women, even after adjusting for confounding factors in the present study. Nightly sleep duration difference between workdays and work-free days is also called social jetlag21. Bowman et al.21 also found the same association in unadjusted models; however, Hawkins et al.26 did not. Patel et al., using actigraphy, found that regardless of the average night sleep duration, men and women who had more night-to-night variation in their sleep duration had a higher risk of becoming overweight32. Notably, we, as well as Bowman21 and Hawkins26, defined sleep regularity as the difference in nightly sleep duration between workdays and weekends (Social Jetlag), while Patel et al.32 defined it as the standard deviation of the average night sleep duration measured by actigraphy during two to five nights. Furthermore, it was observed that sleep regularity tends to be less healthy among individuals aged 30–40 years across all groups. This finding may be attributed to factors such as increased job-related and social activities during this stage of life, leading to greater discrepancies between weekend and weekday sleep schedules (Fig. 1).
The observation that women exhibit an association between sleep regularity and obesity, while men did not, raises intriguing questions about the potential factors contributing to this gender disparity. One potential explanation could be the influence of biological differences between men and women. Hormonal variations, metabolism, and variations in body composition may play a role in how sleep regularity affects weight regulation31,35. Further investigation into the underlying physiological mechanisms could provide insights into these gender-specific associations. Another factor to consider is the impact of lifestyle differences. In this study, it was noted that men had higher levels of unhealthy sleep regularity compared to women, regardless of their obesity status. This suggests that there may be distinct lifestyle patterns that contribute to the gender differences in the relationship between sleep regularity and obesity. Factors such as job-related demands, social activities, and other lifestyle choices may differ between men and women, potentially interacting with sleep regularity to affect weight management.
In summary, the absence of an association between sleep regularity and obesity in men, coupled with higher levels of unhealthy sleep regularity in men compared to women, suggests that there may be complex interactions between gender, sleep regularity, and obesity. Further research is needed to delve deeper into the underlying mechanisms and to consider additional factors such as biological differences, lifestyle patterns, and employment status. This will help us gain a better understanding of the gender-specific effects of sleep regularity on obesity.
The results of this study demonstrated that a significant number of participants (45%) experienced compromised alertness during the day. In women, the group with obesity showed a higher prevalence of individuals with unhealthy alertness compared to the group without obesity. This suggests a potential association between impaired daytime alertness and obesity among women. Logistic regression analysis, adjusting for confounding factors, also confirmed this association, demonstrating that women with unhealthy daytime alertness had a 1.30 times higher likelihood of having obesity.
Interestingly, we observed a contradictory relationship between daytime alertness and obesity among men. Men with unhealthy alertness had lower odds of having obesity. This unexpected result needs further investigation. There is a potential that men who have unhealthy alertness might have compensatory mechanisms or lifestyle factors that help reduce the likelihood of obesity, but additional research is necessary to understand the potential mechanism for this inverse relationship.
Sleep satisfaction is an important dimension of sleep health. In the total population, individuals with unhealthy sleep satisfaction were more likely to have obesity compared to those. This suggests a possible association between dissatisfaction with sleep quality and an increased risk of obesity. However, the association between sleep satisfaction and obesity was significant only in men. This suggests that in women, sleep satisfaction alone may not be a strong predictor of obesity, and other sleep health dimensions may play a more prominent role. Moreover, logistic regression analysis, after adjusting for confounding factors, showed an association between unhealthy sleep satisfaction and obesity in the total population. Although the p-value (0.09) was not statistically significant, it suggests a potential relationship that could be better explored by more extensive investigations.
In examining the age trend in the association between sleep satisfaction and alertness with obesity, it was observed that women with obesity between the ages of 50–60 exhibited the least healthy sleep satisfaction and alertness. This finding may be attributed to several potential factors, such as the increased prevalence of OSA within this age group, the onset of menopause, or changes in circadian rhythm (refer to Fig. 1a and Supplementary file Table S1 and S2).
The gender-specific differences observed in the relationship between sleep health dimensions and obesity may be attributed to various factors. Biological and hormonal differences, variations in sleep patterns, and sleep disorders could contribute to the divergent associations. Further research is warranted to explore these gender differences and identify the underlying mechanisms.
Limitations
The strengths of this study were the large sample size, multi-stage random cluster sampling, and, most importantly, the use of multidimensional aspects of sleep health. One limitation is that the cross-sectional methodology did not include other important covariates, such as smoking, alcohol consumption, and physical activity. Another limitation of our study is that we assessed sleep duration and sleep efficiency by asking participants about the number of hours of actual sleep they obtained at night during the past month. This approach may introduce bias as it does not account for daytime napping. Consequently, our study does not capture the potential influence of daytime napping on sleep duration and efficiency. Moreover, assessing sleep efficiency may have introduced potential bias due to misreported data. Four hundred and nine participants misreported their time in bed shorter than their actual sleep duration. As a result, it was not possible to calculate sleep efficiency accurately.
Another limitation of this study is that we used self-reported questionnaires to assess sleep duration, timing, and satisfaction. Although these questionnaires were adapted and validated for our study population, they are not as precise as objective tools like actigraphy or polysomnography. Self-reported data can be biased due to recall inaccuracies or subjective views on sleep behaviors, which might affect the accuracy and comparability of our results.
Future directions
Despite its importance, sleep as a risk factor for obesity has not been investigated adequately regarding sleep health factors other than sleep duration. To learn how various sleep health domains relate to obesity, we need long-term longitudinal and trial studies. Moreover, research is required to investigate the differences between short-term and long-term unhealthy traits of daytime alertness, sleep quality, timing, efficiency, regularity, and duration. Considering the impact of sleep health on obesity, it seems essential to include sleep health in the national health agenda to manage and implement strategies for reducing obesity.
Conclusions
We found that sleep regularity, satisfaction, and daytime alertness can be associated with obesity regardless of sleep duration or timing. These results imply that other aspects of sleep health besides sleep duration may have a role in maintaining a healthy weight, highlighting the complicated relationship between sleep and metabolism. Using a multidimensional perspective on sleep health, more longitudinal and trial research is required to evaluate the association between obesity and sleep.
Data availability
Datasets are not publicly available but are accessible upon reasonable request from the corresponding author.
References
Harrison, J. E., Weber, S., Jakob, R. & Chute, C. G. ICD-11: An international classification of diseases for the twenty-first century. BMC Med. Inf. Decis. Mak. 21 (6), 1–10 (2021).
WHO. Obesity and overweight. (2021). https://www.who.int/news-room/fact-sheets/detail/obesity-and-overweight
Lobstein, T., Brinsden, H. & Neveux, M. World Obesity Atlas. (2022).
Nielsen, L., Danielsen, K. & Sørensen, T. Short sleep duration as a possible cause of obesity: Critical analysis of the epidemiological evidence. Obes. Rev. 12 (2), 78–92 (2011).
Deacon-Crouch, M., Begg, S. & Skinner, T. Is sleep duration associated with overweight/obesity in indigenous Australian adults? BMC Public. Health. 20 (1), 1–13 (2020).
Chaput, J-P. et al. Risk factors for adult overweight and obesity: The importance of looking beyond the ‘big two’. Obes. Facts. 3 (5), 320–327 (2010).
Kobayashi, D., Takahashi, O., Deshpande, G. A., Shimbo, T. & Fukui, T. Association between weight gain, obesity, and sleep duration: A large-scale 3-year cohort study. Sleep. Breath. 16 (3), 829–833 (2012).
Xiao, Q., Arem, H., Moore, S. C., Hollenbeck, A. R. & Matthews, C. E. A large prospective investigation of sleep duration, weight change, and obesity in the NIH-AARP diet and health study cohort. Am. J. Epidemiol. 178 (11), 1600–1610 (2013).
Watanabe, M., Kikuchi, H., Tanaka, K. & Takahashi, M. Association of short sleep duration with weight gain and obesity at 1-year follow-up: A large-scale prospective study. Sleep 33 (2), 161–167 (2010).
Vgontzas, A. N. et al. Unveiling the longitudinal association between short sleep duration and the incidence of obesity: The Penn state cohort. Int. J. Obes. 38 (6), 825–832 (2014).
Stranges, S. et al. Cross-sectional versus prospective associations of sleep duration with changes in relative weight and body fat distribution: The Whitehall II study. Am. J. Epidemiol. 167 (3), 321–329 (2008).
Sayón-Orea, C. et al. Association between sleeping hours and siesta and the risk of obesity: The SUN mediterranean cohort. Obes. Facts. 6 (4), 337–347 (2013).
Patel, S. R., Malhotra, A., White, D. P., Gottlieb, D. J. & Hu, F. B. Association between reduced sleep and weight gain in women. Am. J. Epidemiol. 164 (10), 947–954 (2006).
Nishiura, C., Noguchi, J. & Hashimoto, H. Dietary patterns only partially explain the effect of short sleep duration on the incidence of obesity. Sleep 33 (6), 753–757 (2010).
Nagai, M., Tomata, Y., Watanabe, T., Kakizaki, M. & Tsuji, I. Association between sleep duration, weight gain, and obesity for a long period. Sleep. Med. 14 (2), 206–210 (2013).
Itani, O., Kaneita, Y., Murata, A., Yokoyama, E. & Ohida, T. Association of onset of obesity with sleep duration and shift work among Japanese adults. Sleep. Med. 12 (4), 341–345 (2011).
Maury, E. Off the clock: From circadian disruption to metabolic disease. Int. J. Mol. Sci. 20 (7), 1597 (2019).
Gao, C. et al. Sleep duration/quality with health outcomes: An umbrella review of meta-analyses of prospective studies. Front. Med. 8, 813943 (2022).
Dashti, H. S. & Ordovás, J. M. Genetics of sleep and insights into its relationship with obesity. Annual Rev. Nutr. 41, 223–252 (2021).
Stranges, S., Tigbe, W., Gómez-Olivé, F. X., Thorogood, M. & Kandala, N. B. Sleep problems: An emerging global epidemic? Findings from the INDEPTH WHO-SAGE study among more than 40,000 older adults from 8 countries across Africa and Asia. Sleep 35 (8), 1173–1181 (2012).
Bowman, M. A. et al. Multidimensional sleep health is not cross-sectionally or longitudinally associated with adiposity in the study of women’s health across the Nation (SWAN). Sleep. Health. 6 (6), 790–796 (2020).
Sadeghniiat-Haghighi, K. et al. The STOP-BANG questionnaire: Reliability and validity of the Persian version in sleep clinic population. Qual. Life Res. 24, 2025–2030 (2015).
Yazdi, Z., Sadeghniiat-Haghighi, K., Zohal, M. A. & Elmizadeh, K. Validity and reliability of the Iranian version of the insomnia severity index. Malaysian J. Med. Sci. MJMS. 19 (4), 31 (2012).
Allen, R. P. et al. Restless legs syndrome: Diagnostic criteria, special considerations, and epidemiology: A report from the restless legs syndrome diagnosis and epidemiology workshop at the National institutes of health. Sleep Med. 4 (2), 101–119 (2003).
Chen, T-Y., Lee, S. & Buxton, O. M. Multidimensional sleep health is associated with physical frailty in a National sample of Taiwanese community-dwelling older adults: Sex matters. Sleep. Health. 8 (5), 528–535 (2022).
Hawkins, M. S. et al. Sleep health characteristics among adults who attempted weight loss in the past year: NHANES 2017–2018. Int. J. Environ. Res. Public. Health. 18 (19), 10170 (2021).
Li, L., Zhang, S., Huang, Y. & Chen, K. Sleep duration and obesity in children: A systematic review and meta-analysis of prospective cohort studies. J. Paediatr. Child. Health. 53 (4), 378–385 (2017).
Wu, Y., Zhai, L. & Zhang, D. Sleep duration and obesity among adults: A meta-analysis of prospective studies. Sleep. Med. 15 (12), 1456–1622 (2014).
Cooper, C. B., Neufeld, E. V., Dolezal, B. A. & Martin, J. L. Sleep deprivation and obesity in adults: A brief narrative review. BMJ Open. Sport Exerc. Med. 4 (1), e000392 (2018).
Gangwisch, J. Epidemiological evidence for the links between sleep, circadian rhythms and metabolism. Obes. Rev. 10, 37–45 (2009).
Chaput, J-P. et al. The role of insufficient sleep and circadian misalignment in obesity. Nat. Rev. Endocrinol. 19 1–16. (2022).
Patel, S. R. et al. The association between sleep patterns and obesity in older adults. Int. J. Obes. 38 (9), 1159–1164 (2014).
Partonen, T. Chronotype and health outcomes. Curr. Sleep. Med. Rep. 1, 205–211 (2015).
Bruce, E. S., Lunt, L. & McDonagh, J. E. Sleep in adolescents and young adults. Clin. Med. 17 (5), 424 (2017).
St-Onge, M-P., O’Keeffe, M., Roberts, A. L., RoyChoudhury, A. & Laferrère, B. Short sleep duration, glucose dysregulation, and hormonal regulation of appetite in men and women. Sleep 35 (11), 1503–1510 (2012).
Acknowledgements
We acknowledge vice chancellors of public health deputies at the time of study, Alireza Delavari, Tehran University of Medical Sciences; Shahnam Arshi, Shahid Beheshti University of Medical Sciences; Mohsen Aarabi, Mazandaran University of Medical Sciences; Rasool Entezarmahdi, Urmia University of Medical Sciences; Manoochehr Karami, Hamadan University of Medical Sciences; Seyyed Vahid Ahmadi Tabatabayi, Kerman University of Medical Sciences; Gholamali Javdan, Hormozgan University of Medical Sciences; Mohsen Moghadami, Shiraz University of Medical Sciences; Mohammad Mohsen Lotfi, Yazd Shahid Sadoughi University of Medical Sciences; Reza Malekzadeh, head of the National Institute for Medical Research Development (NIMAD); Vahid Malekinejad, faculty member of the University of California San Francisco (UCSF); Iraj Mohebbi, faculty member of Urmia University of Medical Sciences; Amir Houshang Mehrparvar, faculty member of the Yazd Shahid Sadoughi University of Medical Sciences; Ayeh Shams Al Dini, faculty member of Kerman University of Medical Sciences.We would also like to thank the staff members of the Tehran University of Medical Sciences’ deputy of public health (Zahra Begum Seyyed Aghamiri, supervisor, Masoumeh Adris, Maryam Shabanlou, Maryam Abdoli, Zahra Kazemi Asfa, Azita Ajlali, Azam Anami Iraqi, Shabnam Shirandami, Halimeh Hanafi, and Marziee Sarabi); Shahid Beheshti University of Medical Sciences’ deputy of public health (Zahra Karami, supervisor, Fatemeh Pourhaji , Nasrin Jafarnia, Parvaneh Mousavi, Shahla Ghanbari, Reza Ahmadi, Reza Nourozi, Fatemeh Parimi, Hajar Rezaee, Marzieh Siampour Nayini, and Mahshad Mahdiar); Iran University of Medical Sciences’ deputy of public health (Samaneh Akhavan Malayeri, supervisor, Elham Rakhshi, Nahid Safari, Azadeh Peivandi, Maryam Ghareh Osman, and Afsaneh Ashori); Kerman University of Medical Sciences’ deputy of public health (Maryam Hosseinpour, supervisor, Akram Khalili Mahani, Fatemeh Nobar, Mahbobeh Sadat Miri, and Shahla Ataollahi); Urmia University of Medical Sciences’ deputy of public health (Fahimah Zehtabi Azar, supervisor, Jebriel Nasirian, Mohammad Rostamlo, Solmaz Taghizadeh, Raziee Moazen, Parisa Mashmol, and Somayeh Rasouli); Hormozgan University of Medical Sciences’ deputy of public health (Roya Atehad, supervisor, Zahra Ahmadi, Fateme Hosseini, Hamid Reza Mirjalili, Sakineh Razamand, and Somayeh Samiee); Shiraz University of Medical Sciences’ deputy of public health (Neda Hadizadeh, supervisor, Zahra Taghipour, Mohammad Ali Moghimizadeh, Sahar Derakhshani, Ali Jafarian, Hessam Parvizi Emran, and Fariba Moradi Ardakani); Hamedan University of Medical Sciences’ deputy of public health (Razia Sadat Mir Moini, supervisor, Zahra Jalali, Saideh Zulfaghari, Rahime Rahbari Pasand, Khadijeh Gorgian, Mojtaba Zarei, and Nasser Fayazee); Yazd Shahid Sadoughi University of Medical Sciences’ deputy of public health (Behnam Bagheri Fahrji, supervisor, Hamid Reza Mirjalili, Leila Mirjalili, and Najma Sadat Haraji); Mazandaran University of Medical Sciences’ deputy of public health (Mohammad Reza Parsai, supervisor, Ali Akbar Ramezani, Reza Dosti, and Alireza Abbaspour); Occupational Sleep Research Center, Baharloo Hospital, Tehran University of Medical Sciences (Somayeh Ghodrati Asgharabadi, Parvin Shibani, Ghazal Dibai, Samane Delkash, Pariya Fallah, Mohammad Reza Mansouri, Ania Rahimi-Golkhandan, Amin Nakhostin-Ansari, Faezeh Aghajani, and Mohammad Alirezaei), and National Institute for Medical Research Development (Bita Mesgarpur, and Farzad Fatehi) for collaborating with us. Our special thanks go to the coordinator of the World Sleep Society’s ISRTP program, Dr. Mike Mutschelknaus, for his kind contribution to editing this manuscript and to WSS’s ISRTP mentorship team.
Funding
This work was supported by a grant from the National Institute for Medical Research Development (NIMAD), Iran (957726).
Author information
Authors and Affiliations
Contributions
SA has contributed to the conception, design of the work, data acquisition, and analysis. AB has contributed to the conception, and design of the work, interpreting data, drafting, and substantively revising the work. RM has contributed to the data analysis and substantively revised the manuscript. ZBA has contributed to the conception and design of the work and the acquisition and interpretation of data. RH has contributed to the acquisition and interpretation of data and revising the work. AHM has contributed to the conception and design of the work and the acquisition and interpretation of data. KSH has contributed substantially to the conception and design of the work and the acquisition of data. AN has contributed substantially to the conception, design of work, data acquisition, interpretation of data, drafting the work, and substantively revising it. All authors have read and approved the submitted version.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Akbarpour, S., Behkar, A., Moradzadeh, R. et al. The links between sleep health domains and male/female obesity: a nationwide survey on the Iranian general population. Sci Rep 15, 24111 (2025). https://doi.org/10.1038/s41598-025-95520-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-95520-x