Abstract
Diagnosing atypical melanocytic tumors can be challenging without molecular characterization, necessitating simple tools to enhance diagnostic accuracy in daily practice. This study retrospectively analyzed the utility of p16 immunohistochemistry (IHC) and 9p21 fluorescence in situ hybridization (FISH) on 206 tumors referred for expert second opinion. The performance of p16 and 9p21 was compared to histological diagnosis (both initial and final respectively without and with p16 and 9p21 status), histological subtype, and follow-up data. Negative p16 immunolabelling detected 90% of malignant cases, while only 11% of benign tumors were p16 negative. Homozygous 9p21deletion detected 42% of malignant tumors and excluded 95% of benign ones. Heterozygous deletion showed no diagnostic value. Homozygous 9p21 deletion significantly improved diagnostic confidence (P < 0.001), leading to tumor upgrading (n = 23) or melanoma confirmation (n = 22). Among 97 patients with follow-up, 17 had adverse outcomes. Kaplan–Meier analysis showed no significant difference in progression-free survival between groups (P = 0.64). Combining both techniques ultimately enhanced histological diagnostic confidence in daily practice. However, in cases where p16 is negative without homozygous deletion, or where histological malignancy is uncertain and p16 positive, other p16-inactivation mechanisms or molecular anomalies should be considered, necessitating further molecular investigations.
Similar content being viewed by others
Introduction
Confident histopathological differentiation between melanoma and atypical nevus can be challenging and such atypical melanocytic tumors are often sent to expert dermatopathologists for second opinions1. Reproducibility, even among experts, is poor2,3,4 and 10–25% of diagnoses lack interobserver agreement5. That situation is more attributable to the lack of specific criteria and opinion differences rather than experts’ faulty diagnostic skills. Melanoma poses additional difficulties; despite 90% of localized melanomas being cured by surgery, it remains the deadliest type of skin cancer6 and evidence of malignancy during follow-up may be elusive because of the prolonged latency required for metastatic spread7.
Molecular characterization has improved melanocytic tumor classification and made it possible, depending on specific molecular anomalies, to link these atypical tumors to different melanoma types. However, even with extensive and expensive molecular studies, diagnosing atypical melanocytic tumors as benign or malignant can remain difficult but that distinction is crucial for prognosis and patient management8. Moreover, molecular diagnosis must be obtained quickly: in the case of malignancy, reexcision (with margins conditioned by thickness/Breslow’s index) should be done within the 3 months following the initial excision; however, not all pathologists have access to rapid molecular testing for therapeutic decision-making.
By accruing molecular knowledge, pathologists can use simpler, more cost-effective tools that target common melanoma-related abnormalities, thereby improving histopathological diagnosis accuracy. Among those tools, p16 immunohistochemistry (IHC) is used to diagnose challenging melanocytic tumors, with a negative result suggesting malignancy. p16, a tumor-suppressor protein encoded by the cyclin-dependent kinase inhibitor 2A (CDKN2A) gene on chromosome 9p21 (also known as multiple tumor-suppressor (MTS-1)9, inhibitor of cyclin-dependent kinase 4 (INK4a) or p16INK4 gene)10, regulates cell proliferation by inhibiting the retinoblastoma protein–transcription factor (pRb–E2F) pathway. It is frequently modified in familial melanoma and other cancers through genetic changes, like point mutations, promoter hypermethylation or homozygous deletions9,11,12. The latter can easily be detected with 9p21 fluorescence in situ hybridization (FISH)13, an affordable and well-established technique that does not require complex equipment.
We undertook this study to retrospectively analyze, on 206 atypical melanocytic tumors received for expert second opinion, the p16-IHC and 9p21-FISH performances to obtain the final expert histopathological diagnoses and their impact on long-term prognoses. Based on this cohort, reflecting real-life cases including various types of atypical melanocytic tumors, we propose an algorithm using those 2 simple and inexpensive tools, and tested it on outcomes of patients with known follow-up.
Results
According to the selection criteria, we identified and studied 206 atypical melanocytic tumors that had been evaluated with 9p21 FISH and p16 IHC (summarized in Supplementary Table 1; see supplemental digital content containing 2 tables).
Clinical and histopathological findings
Among the 206 atypical melanocytic tumors (Table 1), the majority were Spitz–Reed tumors (SRT) (61%, n = 126). SRTs predominantly affected young patients (median age, 27 years; range: 4–69 years) and women (70%, n = 88). The lesions were mainly located on the limbs (56%, n = 71). Most of the tumors (55%, n = 69) were histologically diagnosed as benign: A– or DA–; the remaining 57 (45%) tumors were categorized as malignant: A+ or DA+.
The atypical thick nevoid tumors (ATNTs) was the second most common type (15%, n = 31), which primarily affected older patients (median age, 41 years; range 18–86 years). The lesions were commonly found on the limbs (39%, n = 12) and the trunk (32%, n = 10). Most of the diagnoses (84%, n = 26) were categorized as malignant: A+ or DA+.
The atypical thin tumors (AThinTs) type accounted for 12% (n = 24) of patients (median age, 42.5 years; range 20–68 years). Lesions were primarily located on the limbs (46%, n = 11). Only 4 (17%) tumors were categorized as benign: A– or DA–.
The 25 other atypical melanocytic tumors of uncertain malignant potential, MELTUMP (OMTs) included 5 blue cell tumors and related lesions (3: 1 borderline DA+, 2 malignant A+), 5 lesions suspected of activating the WNT pathway (3 suspected of being malignant: DA+), 5 melanocytic neoplasms with BAP1 inactivation (2 categorized as malignant: 1 DA+, 1 A+), 5 congenital lesions (2 malignant A+), 2 malignant lesions whose primary status could not be confirmed, 2 acral nevi, and 1 genital nevus.
Among the 206 patients, clinical follow-up information was obtained for 97 (47%), primarily those with SRTs (n = 54): 9 were categorized as A–, 19 as DA–, 41 as DA+ and 28 as A+. High percentages of patients with SRTs were lost to follow-up (57%; n = 72), particularly those with benign tumors (68%). The mean duration of follow-up was 5.7 years for ATNTs, 3.5 years for AThinTs, 4.5 years for OMTs and 6.2 years for SRTs, which was the longest among all tumor types.
Performance comparison of p16 and 9p21 with expert histopathological diagnoses (blinded to p16 and 9p21 status)
p16 IHC
For the entire cohort, clonal or diffuse p16 negativity was present in 90% of tumors that ultimately received a malignant diagnosis (Table 2). In contrast, only 11% of tumors later deemed benign exhibited p16 negativity. When p16 negativity was observed, 56% of those cases were confirmed as malignant on final diagnosis, whereas 46% of cases with p16 positivity were confirmed as benign. These detection rates were consistent among the main histological subtypes (SRT, ATNT, and AThinT), with malignant detection rates ranging from 86% in SRTs to 92% in ATNTs.
9p21 FISH
Technical evaluation of 9p21 FISH was successful in 95% of the tumors (195/206). Among p16-negative cases, homozygous deletion of 9p21 was observed in 27% (50/184) of tumors, and it was absent in p16-positive tumors. Overall, the pattern of homozygous 9p21 loss was found in cases that corresponded to malignant histology in 95% of instances. Furthermore, when homozygous deletion was present, 92% of tumors were confirmed as malignant, whereas the absence of deletion corresponded to benign histology in 55% of cases. These findings were comparable across the four histological subtypes, with a higher agreement for benign lesions in SRTs (66%) compared with the other types (25%). Importantly, all tumors exhibiting homozygous 9p21 deletion were p16-negative, indicating that p16 loss captured 100% of these cases, even though the overall concordance between p16 loss and 9p21 deletion was 14%.
Heterozygous 9p21-FISH status significance
Among the 206 cases, 89 had heterozygous 9p21 deletion. The receiver operating characteristics curve (Fig. 1) revealed that this deletion was close to the bisecting (orange) line, indicating limited value for predicting benign or malignant expert histological diagnosis of atypical melanocytic tumors.
Diagnostic confidence between initial and final histopathological diagnoses based on p16 and 9p21 findings
Detection of a homozygous 9p21 deletion significantly enhanced diagnostic confidence for 45/45 tumors, with no change for 2/161, while heterozygous 9p21 deletion enhanced confidence for 0/45, with 156/161 diagnoses unchanged (P < 0.001, chi2 test). The absence of a homozygous deletion had no diagnostic impact (i = 0), according to the before and after FISH diagnoses. Among the 50 tumors harboring homozygous 9p21 deletions, 23 (46%) were upgraded to malignancy (i = 2) and 22 (44%) melanomas were confirmed (i = 1).
The post-test positive-likelihood ratio for this sequential approach was 8.3, which is considered reasonably high17 and thus indicates diagnostic usefulness.
Proposed algorithm
Based on those results (see also Supplementary Table 2), we devised an algorithm for diagnosing atypical melanocytic tumors with tools accessible to any pathologist (Fig. 2). We applied this algorithm to tumors assigned to our 3 main types (SRT, ATNT and AThinT) to determine whether it correctly sorted them. We excluded the OMT group because the number of patients per category (blue cell tumors, Wint Activated Melanocytic tumors, BAP1 inactivated tumors…) in this group was too small for statistical analysis.
Algorithm for requesting complementary techniques to determine atypical melanocytic tumor type and category. This information for the “other” cases is not presented because of their heterogeneity. Blue, our case diagnoses according to the algorithm. Purple, our case outcomes based on available information. Note: OMTs (other melanocytic tumors), including acral and mucosal lesions common in Asia and Africa, were excluded from the diagnostic algorithm due to the limited number of cases. This exclusion may affect the generalizability of our findings. SRT Spitz–Reed tumor, ATNT atypical thick nevoid tumor, AThinT atypical thin tumor, IHC immunohistochemistry, NC noncontributory, FISH fluorescence in situ hybridization, CGH comparative genomic hybridization, + positive, – negative, A atypical, DA doubtful atypical, LN+ lymph-node metastases, M+ organ metastases, RMS remission.
For patients with atypical melanocytic tumors, p16 IHC should be evaluated first. If p16 is negative (diffuse or clonal), 9p21 FISH can be requested, but it is only informative when the deletion is homozygous. Homozygous 9p21-FISH deletion and p16-positivity were not found in any samples analyzed, which confirmed 9p21-FISH uselessness when p16 is positive.
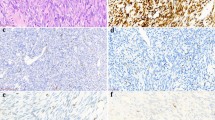
Testing the algorithm on the tumors of patients with known outcomes
We applied our diagnostic algorithm to the subset of 97 patients with available follow-up data, including 17 (18%) who developed adverse outcomes (metastases or death) (Table 3). These comprised 10 spitzoid tumors (SRTs), 6 atypical thick nevoid tumors (ATNTs; Fig. 3A–L), and 1 MELTUMP with BAP1 inactivation (OMT group). No patients with AThinTs experienced tumor-related events following complete excision. Of the 17 adverse outcomes, 1 patient died from another superficial spreading melanoma unrelated to the lesion under study, leaving 16 tumor-related events for progression-free survival (PFS) analysis. A Kaplan–Meier comparison of PFS between (1) p16-negative tumors with 9p21 homozygous deletion and (2) all other tumor statuses (p16-negative with 9p21 heterozygous deletion or no deletion, p16-positive, or no FISH result) revealed no significant difference in tumor-related outcomes (χ2 = 0.218, P = 0.64) (Fig. 4).
Tumor histology for patients 1, 3 and 16 who had adverse outcomes. Tumor 1 (A–D) exhibits Spitz architecture (A, HES ×10) and fusiform Spitz cytology (B, HES ×200), with p16-positivity (C, p16 IHC ×100) and no 9p21 deletion (D, FISH ×600). Tumor 3 (E–H) was a compound Spitz tumor (E, HES ×10) with epithelioid Spitz cytology (F, HES ×200), loss of p16 (G, p16 IHC ×100) and heterozygous 9p21 deletion (H, FISH ×600). Tumor 16 (I–L) was a densely cellular melanocytic dermal tumor (I, HES ×10) with nevoid cytology (J, HES ×200), p16-negativity (K, p16 IHC ×100) and homozygous 9p21 deletion (L, FISH ×600). For more detailed descriptions, see Table 3.
Kaplan–Meier curves depicting progression-free survival (PFS), expressed in months, among two groups: (1) tumors with p16 negativity and 9p21 homozygous deletion (red line) and (2) tumors with any other status (blue line). PFS was defined as the time (in months) from excision to the occurrence of a tumor-related event (local recurrence, lymph node metastasis, or distant metastasis). A total of 16 tumor-related events were analyzed. The difference in PFS between these groups was not statistically significant (log-rank test, P = 0.64).
Fifteen of the 17 adverse-outcome tumors (88%) showed p16 loss (11 diffuse, 4 clonal), underlining the importance of p16 negativity as an indicator of potential malignancy. Four of 23 patients (4 of 20 excluding AThinTs) with tumors categorized as DA + or A + and harboring homozygous 9p21 deletion developed metastases (lymph node in 3, organ in 1). Conversely, 8 of 30 DA + /A + tumors lacking 9p21 homozygous deletion (heterozygous or none) still led to poor outcomes in 8 patients, including 2 deaths, highlighting that other mechanisms can inactivate p16.
In such ambiguous cases, additional cytogenetic or molecular tests may be warranted, as demonstrated by our 7 p16-negative tumors without 9p21 homozygous deletion that displayed abnormalities on four-color FISH or CGH. The remaining 4 such tumors had no further investigations yet were diagnosed as malignant on histology alone. Only 2 of 17 adverse-outcome cases were p16-positive SRTs without 9p21 deletion: 1 developed an N1a lymph node metastasis but remains in remission, and the other died from a different melanoma. Notably, all 4 of 28 SRT patients with p16-negative, homozygous 9p21-deleted tumors categorized as A– or DA– are in remission. Among 14 tumors (12 SRTs, 1 ATNT, 1 AThinT) with p16 negativity but no homozygous 9p21 deletion and categorized as DA–, 1 SRT patient died and 1 ATNT patient relapsed, further illustrating the need for broader molecular investigation.
Discussion
Loss of p16, initially identified in familial melanoma18, plays a role in various stages of melanoma development19, including benign nevi, dysplastic nevi, radial growth and vertical growth20. However, p16 loss alone is insufficient to trigger melanoma development, even though it increases the risk, especially when accompanied by other driver mutations21.
The p16-IHC performance alone has been extensively studied11,22,23,24. It has improved confidence in all melanocytic tumor diagnoses, leading to management changes for 17.7% of them25. However, using p16 alone is not useful for differentiating between nevi and melanoma11. Combining p16 with Ki67 and human melanoma black-45 (HMB45) labeling is more informative for atypical melanocytic tumors22. Of course, the diagnosis of difficult melanocytic tumors can also benefit from the use of other markers such as BRAF, NRAS, ALK, and ROS1 to define their genetic background or, in certain cases, a marker like PRAME. However, the objective of this work was mainly to study p16 in its overall context without targeting any specific subtype of melanocytic tumor. A significant correlation between p16 IHC and homozygous 9p21 loss was reported (correlation coefficient, 0.6162; P < 0.000126), but this modification is common in melanoma (homozygous 9p21 deletion, 31% of tumors; promoter hypermethylation, 20–30% of tumors25,27). Our findings align with existing data, as 50 (27%) of our 184 p16-negative tumors also had homozygous 9p21 deletion. That observation underscores the notion that only homozygous 9p21 deletion carries informative value in terms of malignancy, with p16-negativity being suggestive but insufficient to conclusively establish it. Furthermore, our results demonstrated that heterozygous 9p21 deletion, regardless of the heterozygous nucleus count, lacked significance and was even seen in relatively benign melanocytic tumors. Consequently, counting heterozygous nuclei, at times cumbersome in routine FISH diagnoses, is not recommended and deemed unnecessary.
Although the p16-inactivation mechanism is well understood, few studies have linked p16 expression and 9p21 status with long-term clinical outcomes, and none has dealt with real-life second-opinion expertise referrals. Several studies focusing on spitzoid tumors28 found an association between a lack of malignancy-related cytogenetic abnormalities at the FISH-detected 9p21 locus and p16 expression29. The authors of 1 study30 concluded that p16 loss is specific to spitzoid neoplasms with borderline or malignant characteristics and can occur with or without genomic CDKN2A loss. Other studies that specifically examined atypical Spitz tumors observed regional melanoma progression only in patients with homozygous 9p21 deletion31,32. Spitz lineage was not addressed in another study33 that focused on pregnancy-related nevi and nevoid melanomas; p16 loss was found in melanomas. However, analysis of various atypical melanocytic tumors in 1 study34 led the authors to conclude that FISH alone was not sufficient for some diagnoses, because certain genetic abnormalities were only seen in specific subtype lesions. Although clinical outcomes were reported in some of those papers dealing with Spitz lesions, follow-up duration was not specified. The absence of adverse outcomes of our patients with p16-negative AThinTs, even those with homozygous 9p21 deletion, reinforces the concept that this type of thin lesion is associated with a favorable prognosis, as proposed by the “Melanocytic Pathology Assessment Tool and Hierarchy for Diagnosis (MPATH-Dx)” classification (such AThinTs are classified class 2)35.
Compared with the 4-color melanoma FISH assay36,37,38,39, few studies have assessed the performance of p16-IHC completed by 9p21-FISH in terms of final diagnoses and diagnostic confidence, necessitating the development of a simple algorithm for daily practice. Our algorithm integrates p16-IHC, a readily accessible and cost-effective method, for diverse types of atypical melanocytic tumors (SRTs, ATNTs and AThinTs). This strategy facilitates the identification of tumors that might require additional further investigation, balancing its strong ability to detect malignant cases with a limited capacity to exclude benign ones. In instances of p16-negativity, whether diffuse or clonal, 9p21-FISH is recommended to validate the diagnosis of malignancy, demonstrating excellent reliability in ruling in melanoma but a more limited ability to detect all malignant cases. Notably, 9p21-FISH is user-friendly, widely applicable, affordable (less expensive than next-generation sequencing, for example), and can be done in numerous laboratories.
Compared with other algorithms26,40,41, ours is based on real-life issues concerning atypical melanocytic tumors: frequent challenges in Spitz-lineage lesions or distinguishing between thin and thick lesions. However, our algorithm has some limitations, when p16 is negative and 9p21 heterozygous. Heterozygosity does not preclude malignancy, as other mechanisms, including promoter hypermethylation, may be involved. In such cases, if histology remains uncertain, additional molecular tools, such as 4-color melanoma FISH or chromosomal CGH, are recommended, by us and other authors37,38,40,41. More recently, attempts to replace FISH with preferentially expressed antigen in melanoma (PRAME) IHC by Harvey et al.42 and McAfee et al.43 failed to demonstrate its effectiveness.
To be as exhaustive as possible, we focused on patients with follow-up (including 17 patients with adverse outcomes) to demonstrate algorithm efficacy at malignancy detection (15/17 p16-negative with 4/15 homozygous 9p21 deletions). However, when histology alone is doubtful and not sufficient to affirm malignancy, supplementary 4-color melanoma FISH or advanced molecular techniques on a specialized platform could be recommended for tumors without homozygous deletion44. Complementary results should always be compared with histopathological analyses, as demonstrated by 4/17 tumors diagnosed as melanoma based solely on histology (including 1 p16-positive case). Our Kaplan–Meier and log-rank analysis indicate that while our diagnostic algorithm effectively stratifies atypical melanocytic tumors, it does not provide significant prognostic discrimination. This suggests that although molecular characterization aids in refining diagnostic accuracy, additional biomarkers or clinical parameters may be required for reliable prognostic assessment.
Our study has 4 main limitations. First, to increase relevance for daily practice and to allow statistical analyses, we used 4 histological types45 that align with the real-world challenges of second-opinion reviews46. Second, we had an overall loss-to-follow-up rate of 53%47; however, our series remains the largest on atypical melanocytic tumors with prolonged follow-up for 96 patients, averaging 4.7 years. It is noteworthy that the mean follow-up duration for spitzoid melanocytic tumors (SRTs) was longer than for other tumor groups despite a higher attrition rate. This may be attributable to extended clinical surveillance in patients with concerning features, and potential referral bias. Future studies are needed to explore these follow-up dynamics in greater detail. Third, we analyzed melanocytic tumors independent of the molecular changes defining the histological types, particularly those described for Spitz tumors (as TERT promoter mutations and fusion kinase gene alterations)48,49. Therefore, we suggest that biallelic 9p21 inactivation itself has value, independent of other molecular factors. For spitzoid neoplasms, the presence of a 9p21 homozygous deletion is a driver genetic event for malignancy, precluding the designation of this lesion as a nevus. This genetic event should be interpreted within its clinical context (notably the patient’s age) and morphological context (including the presence of atypia, mitoses, and necrosis), and is usually accompanied by a TERT promoter mutation in a bona fide Spitz melanoma48. Regarding other melanocytic neoplasms, the role of 9p21 homozygous deletion is less well defined, particularly in the context of BRAF or NRAS mutations; however, it remains a major driver event toward malignancy50, albeit not conclusive when considered as the sole molecular criterion. Pertinently, the outcomes of our patients with p16-negative and homozygous 9p21-deletion–harboring tumors seem to confirm this hypothesis. Last, but not least, we excluded OMTs from the diagnostic algorithm because of their small sample size. Given that OMTs include acral and mucosal lesions frequently seen in Asia and Africa, this exclusion limits the broader applicability of our results.
In conclusion, the results of this study provide a simple first-line algorithm that can be applied in daily practice by any dermatopathologist to sort some atypical melanocytic tumors with 2 accessible tools, enabling quick reexcision if needed. Doubtful cases will always remain, requiring further molecular analyses and, hence, expert second opinions.
Methods
Patients
After receiving approval from the local ethics board (no. CER-BDX-2023-55; 05/16/2023), we analyzed our Bordeaux University Hospital (Bordeaux, FRANCE) database of 5600 fully excised melanocytic tumors referred for a second opinion between 2010 and 2022. We focused specifically on atypical melanocytic tumors (doubtful diagnosis between atypical nevus and melanoma) assessed using p16 IHC and 9p21 FISH. We collected the following information: sex, age, lesion location (classified as head and neck, trunk or limbs), IHC phenotype and additional molecular results, if available (e.g, FISH or comparative genomic hybridization [CGH]). All information was anonymized, securely stored and password-protected throughout the study. We contacted clinicians to gather information on reexcision margins (if applicable), sentinel-node involvement (if evaluated), and current follow-up status (including remission, local recurrence, lymph-node or distant metastasis, and vital status).
p16 IHC
For p16 IHC (CINtec, Clone E6H4; Roche, Basel, Switzerland), the automated BOND-MAX labeling system (Leica Biosystems, Wetzlar, Germany) was used, and p16 was defined as diffusely negative (neither cytoplasmic nor nuclear labeling), clonal negative (regional loss of expression) or positive (cytoplasmic even weak, nuclear or both). Internal controls included sweat duct epithelium, sweat gland cells and keratinocytes.
FISH signal for 9p21 locus
Dual-color FISH was used to analyze interphase nuclei from formalin-fixed, paraffin-embedded tissue. The probe set contained chromosome-9 centromere-specific probes (CEP-9; SpectrumGreen) and 9p21 probes (SpectrumOrange; Abbott Molecular, Des Plaines, IA, USA). FISH analyses followed previously reported protocols14, with a homozygous loss threshold set at 29% affected nuclei15.
4-Color melanoma FISH
Abbott Molecular Inc.’s 4-color Vysis Melanoma FISH Probe kit (Abbott France, Rungis, France) targets 6p25 (RREB1: ras-responsive element-binding protein-1), 6q23 (MYB: myeloblastosis), 11q13 (CCDN1: cyclin D1) and chromosome 6 centromere (CEP6). These probes are labeled, respectively, with Spectrum Red, Spectrum Gold, Spectrum Green, and Spectrum Aqua. FISH was run on 5-mm-thick sections of formalin-fixed paraffin-embedded tissues, following the Abbott Molecular Inc. protocol.
Histopathological review
Two expert dermatopathologists (FB and BV) and a junior dermatopathologist (RV)—blinded to patients’ histories—reviewed all selected case-tumor samples, henceforth referred to as tumors. In the case of discordance, findings were reviewed collegially to obtain a consensus. Each lesion phenotype was completed as proposed by the WHO classification (2023) to specify the genetic background (e.g., BAP1, β-catenin, BRAF V600E, ALK, ROS1, Pan-TRK IHC).
The atypical melanocytic tumors were assigned to 4 major types: (1) atypical thin tumors (AThinTs) described as compound atypical melanocytic tumors thickness/Breslow’s index < 1 mm making a differential diagnosis between superficial spreading melanoma (thickness/Breslow’s index < 1 mm) and atypical or dysplastic nevus difficult; (2) atypical thick nevoid tumors, (ATNTs), described as thick melanocytic tumors of uncertain malignant potential with nevoid cytology, raise questions about a differential diagnosis between nevoid melanoma (thickness/Breslow’s index > 1 mm) and nevus; (3) Spitz–Reed tumors (SRTs) generally range from atypical nevus to melanoma; and (4) other atypical melanocytic tumors of uncertain malignant potential (MELTUMP) [OMTs]) include blue tumors, lesions suspected of activating the wingless-related integration site (WNT) pathway, melanocytic neoplasms with breast cancer-1 (BRCA1)-associated protein-1 (BAP1) inactivation, congenital lesions, acral and genital nevi.
Next, the tumors were distributed into 4 categories (more on less significant doubt with melanoma), based on the potential clinical usefulness for the therapeutic care of patients, considering their histological features, clinical context and degree of histopathological doubt between benign or malignant melanocytic tumor; first without considering the p16 IHC and 9p21-FISH findings, then using them: (1) atypical benign tumor/nevus A–(considered as nevus); (2) doubtful atypical borderline tumor with nevus:16 DA– (low grade melanocytoma); (3) doubtful atypical borderline tumor with melanoma16: DA+ (high grade melanocytoma); and (4) atypical malignant tumor/melanoma: A+(considered as melanoma).
Each pathologist completed an evaluation form for each tumor, indicating histopathological diagnosis, diagnostic confidence before and after reviewing the p16 IHC labeling, and 9p21-deletion type. Malignancy was suspected only for p16-negativity associated with homozygous 9p21 deletion. The p16 and 9p21 impact on the final diagnosis (i) was evaluated on a scale ranging from 0 to 2, where i = 0 indicated none, i = 1 confirmed malignancy and i = 2 diagnosis upgraded to malignancy.
Statistical analyses
Statistical analyses were computed with R software (v4.3.0; http://www.cran.r-project.org). A receiver operating characteristics curve was used to identify the optimal threshold for identifying the heterozygous status of the 9p21-locus deletion, ie, < 29% of nuclei exhibiting homozygous deletion compared to the expert histopathological diagnosis. A tumor was considered “diseased”, i.e. borderline or malignant, when the histological diagnosis was DA+ or A+, without knowing the p16-IHC or 9p21-FISH results. P16-IHC and 9p21-FISH test performances were defined as : detection rate (% of p16-IHC negativity (or 9p21-FISH homozygous deletion) on tumors considered histologically as malignant (A + /DA +)); exclusion rate (% of p16-IHC positivity (or 9p21-FISH heterozygous or no deletion) on tumors considered histologically as benign (A−/DA−); positive concordance (% of concordance between p16-IHC negativity (or 9p21-FISH homozygous deletion) and histological diagnosis of malignancy (A + /DA +); negative concordance (% of concordance between p16-IHC positivity (or 9p21-FISH heterozygous or no deletion) and histological diagnosis of benign tumor (A−/DA−)).
The association between 9p21-deletion status and diagnostic confidence was assessed using Pearson’s chi-square test. Progression-free survival (PFS) was analyzed using the Kaplan–Meier method. PFS was defined as the time in months from the date of excision to the occurrence of a tumor-related event (i.e., local recurrence, lymph node metastasis, or distant metastasis), with cases without such an event censored on October 31, 2023. Survival analysis was performed to compare event-free survival between two groups: (1) tumors with p16 negativity and 9p21 homozygous deletion and (2) tumors with any other status (p16 negativity with 9p21 heterozygous deletion, no deletion, no result available, or p16 positivity). Statistical significance between survival curves was determined using the log-rank test.
Data availability
The datasets generated and/or analyzed during the current study are not publicly available due to the presence of sensitive personal data of the patients in the raw data but are available from the corresponding author on reasonable request.
References
Chang, O. H. et al. Characterization of multiple diagnostic terms in melanocytic skin lesion pathology reports. J. Cutan. Pathol. 49(2), 153–162 (2022).
Gerami, P. et al. Histomorphologic assessment and interobserver diagnostic reproducibility of atypical spitzoid melanocytic neoplasms with long-term follow-up. Am. J. Surg. Pathol. 38(7), 934–940 (2014).
Corona, R. et al. Interobserver variability on the histopathologic diagnosis of cutaneous melanoma and other pigmented skin lesions. J. Clin. Oncol. 14(4), 1218–1223 (1996).
Farmer, E. R., Gonin, R. & Hanna, M. P. Discordance in the histopathologic diagnosis of melanoma and melanocytic nevi between expert pathologists. Hum. Pathol. 27(6), 528–531 (1996).
Lodha, S., Saggar, S., Celebi, J. T. & Silvers, D. N. Discordance in the histopathologic diagnosis of difficult melanocytic neoplasms in the clinical setting. J. Cutan Pathol. 35(4), 349–352 (2008).
Lopes, J., Rodrigues, C. M. P., Gaspar, M. M. & Reis, C. P. Melanoma management: from epidemiology to treatment and latest advances. Cancers 14(19), 4652 (2022).
Mervic, L. Time course and pattern of metastasis of cutaneous melanoma differ between men and women. PLoS ONE 7(3), e32955 (2012).
Genomic classification of cutaneous melanoma. Cell 161(7), 1681–1696 (2015).
Kamb, A. et al. A cell cycle regulator potentially involved in genesis of many tumor types. Science 264(5157), 436–440 (1994).
Serra, S., Chetty, R. p16. J. Clin. Pathol. 71(10), 853–858 (2018).
Koh, S. S. & Cassarino, D. S. Immunohistochemical expression of p16 in melanocytic lesions: an updated review and meta-analysis. Arch. Pathol. Lab. Med. 142(7), 815–828 (2018).
Li, J., Poi, M. J. & Tsai, M. D. The regulatory mechanisms of tumor suppressor P16INK4A and relevance to cancer. Biochemistry 50(25), 5566–5582 (2011).
Rákosy, Z. et al. Characterization of 9p21 copy number alterations in human melanoma by fluorescence in situ hybridization. Cancer Genet. Cytogenet. 182(2), 116–121 (2008).
Gammon, B., Beilfuss, B., Guitart, J. & Gerami, P. Enhanced detection of spitzoid melanomas using fluorescence in situ hybridization with 9p21 as an adjunctive probe. Am. J. Surg. Pathol. 36(1), 81–88 (2012).
Gerami, P. et al. A highly specific and discriminatory FISH assay for distinguishing between benign and malignant melanocytic neoplasms. Am. J. Surg. Pathol. 36(6), 808–817 (2012).
Yeh, I. New and evolving concepts of melanocytic nevi and melanocytomas. Mod. Pathol. 33, 1–14 (2020).
Jaeschke, R., Guyatt, G. H. & Sackett, D. L. Users’ guides to the medical literature. III. How to use an article about a diagnostic test. B. What are the results and will they help me in caring for my patients? The Evidence-Based Medicine Working Group. JAMA 271(9), 703–707 (1994).
Torres-Cabala, C., Li-Ning-Tapia, E. & Hwu, W. J. Pathology-based biomarkers useful for clinical decisions in melanoma. Arch. Med. Res. 51(8), 827–838 (2020).
Shain, A. H. et al. The genetic evolution of melanoma from precursor lesions. N. Engl. J. Med. 373(20), 1926–2136 (2015).
Haferkamp, S., Becker, T. M., Scurr, L. L., Kefford, R. F. & Rizos, H. p16INK4a-induced senescence is disabled by melanoma-associated mutations. Aging Cell 7(5), 733–745 (2008).
Damsky, W. et al. mTORC1 activation blocks BRAFV600E-induced growth-arrest, but is insufficient for melanoma formation. Cancer Cell 27(1), 41–56 (2015).
Uguen, A. et al. A p16-Ki-67-HMB45 immunohistochemistry scoring system as an ancillary diagnostic tool in the diagnosis of melanoma. Diagn. Pathol. 10(1), 195 (2015).
Terrell, J. R. et al. The influence of p16 immunohistochemistry on diagnosis and management recommendation of melanocytic neoplasms by dermatopathologists: a prospective study. J. Cutan. Pathol. 48(8), 1094–1097 (2021).
Bahmad, H. F., Oh, K. S. & Alexis, J. Potential diagnostic utility of PRAME and p16 immunohistochemistry in melanocytic nevi and malignant melanoma. J. Cutan. Pathol. 50(8), 763–772 (2023).
Newell, F. et al. Comparative genomics provides etiologic and biological insight into melanoma subtypes. Cancer Discov. 12(12), 2856–2879 (2022).
Uguen, A. et al. The p16-Ki-67-HMB45 immunohistochemistry scoring system is highly concordant with the fluorescent in situ hybridization test to differentiate between melanocytic nevi and melanomas. Appl. Immunohistochem. Mol. Morphol. 26(6), 361–367 (2018).
Ming, Z., Lim, S. Y. & Rizos, H. Genetic alterations in the INK4a/ARF locus: effects on melanoma development and progression. Biomolecules 10(10), 1447 (2020).
Raghavan, S. et al. Spitz melanoma is a distinct subset of spitzoid melanoma. Mod. Pathol. 33(6), 1122–1134 (2020).
Horst, B. A., Terrano, D., Fang, Y., Silvers, D. N. & Busam, K. J. 9p21 gene locus in Spitz nevi of older individuals: absence of cytogenetic and immunohistochemical findings associated with malignancy. Hum. Pathol. 44(12), 2822–2828 (2013).
Harms, P. W. et al. Loss of p16 expression and copy number changes of CDKN2A in a spectrum of spitzoid melanocytic lesions. Hum. Pathol. 58, 152–160 (2016).
Egnatios, G. L. & Ferringer, T. C. Clinical follow-up of atypical spitzoid tumors analyzed by fluorescence in situ hybridization. Am. J. Dermatopathol. 38(4), 289–296 (2016).
Yazdan, P. et al. Comparative analysis of atypical Spitz tumors with heterozygous versus homozygous 9p21 deletions for clinical outcomes, histomorphology, BRAF mutation, and p16 expression. Am. J. Surg. Pathol. 38(5), 638–645 (2014).
Koh, S. S., Lau, S. K., Roehmholdt, B. F. & Cassarino, D. S. Immunohistochemistry of p16 in nevi of pregnancy and nevoid melanomas: a clinical follow-up study. J. Clin. Pathol. 75(1), 68–70 (2022).
Muhlbauer, A. et al. The correlation of the standard 5 probe FISH assay with melanocytic tumors of uncertain malignant potential. Ann. Diagn. Pathol. 28, 30–36 (2017).
Barnhill, R. L. et al. Revision of the melanocytic pathology assessment tool and hierarchy for diagnosis classification schema for melanocytic lesions: a consensus statement. JAMA Netw. Open. 6(1), e2250613 (2023).
Vergier, B. et al. Fluorescence in situ hybridization, a diagnostic aid in ambiguous melanocytic tumors: European study of 113 cases. Mod. Pathol. 24(5), 613–623 (2011).
Gaiser, T. et al. Classifying ambiguous melanocytic lesions with FISH and correlation with clinical long-term follow up. Mod. Pathol. 23(3), 413–419 (2010).
Raskin, L. et al. Copy number variations and clinical outcome in atypical Spitz tumors. Am. J. Surg. Pathol. 35(2), 243–252 (2011).
Massi, D. et al. Atypical spitzoid melanocytic tumors: a morphological, mutational, and FISH analysis. J. Am. Acad. Dermatol. 64(5), 919–935 (2011).
Hilbers, M. L. et al. Standardized diagnostic algorithm for spitzoid lesions aids clinical decision-making and management: a case series from a Swiss reference center. Oncotarget 12(2), 125–130 (2021).
Cho-Vega, J. H. A diagnostic algorithm for atypical spitzoid tumors: guidelines for immunohistochemical and molecular assessment. Mod. Pathol. 29(7), 656–670 (2016).
Harvey, N. T. et al. Correlation of FISH and PRAME immunohistochemistry in ambiguous superficial cutaneous melanocytic proliferations. Am. J. Dermatopathol. 43(12), 913–920 (2021).
McAfee, J. L. et al. Combined utility of p16 and BRAF V600E in the evaluation of spitzoid tumors: superiority to PRAME and correlation with FISH. J. Cutan. Pathol. 50(2), 155–168 (2023).
Andea, A. A. Molecular testing for melanocytic tumors: a practical update. Histopathology 80(1), 150–165 (2022).
De La Fouchardiere, A. et al. ESP, EORTC, and EURACAN expert opinion: practical recommendations for the pathological diagnosis and clinical management of intermediate melanocytic tumors and rare related melanoma variants. Virchows Arch. 479(1), 3–11 (2021).
World Health Organization. WHO Classification of Skin Tumours, 5th ed. International agency for research on cancer; Online. (World Health Organization classification of tumours, Lyon).
Ebbelaar, C. F., Jansen, A. M. L., Bloem, L. T. & Blokx, W. A. M. Genome-wide copy number variations as molecular diagnostic tool for cutaneous intermediate melanocytic lesions: a systematic review and individual patient data meta-analysis. Virchows Arch. 479(4), 773–783 (2021).
Hagstrom, M., Fumero-Velázquez, M., Dhillon, S., et al. An update on genomic aberrations in Spitz naevi and tumours. Pathology (Phila). S0031302522003191 (2022).
Kervarrec, T. et al. Morphologic features in a series of 352 Spitz melanocytic proliferations help predict their oncogenic drivers. Virchows Arch. 480(2), 369–382 (2022).
Tran, T. P., Titus-Ernstoff, L., Perry, A. E., Ernstoff, M. S. & Newsham, I. F. Alteration of chromosome 9p21 and/or p16 in benign and dysplastic nevi suggests a role in early melanoma progression (United States). Cancer Causes Control. 13(7), 675–682 (2002).
Acknowledgements
We would like to thank all the pathologists who sent us the melanocytic tumor samples used in this study and who demonstrated their trust in us. We thank Professor Geneviève Chêne, from the University & CHU Bordeaux and Inserm 'Bordeaux Population Health’ Research Centre, for her invaluable contribution to the statistical analysis of this study.
Funding
This research was supported by funds from Bordeaux University Hospital.
Author information
Authors and Affiliations
Contributions
R.V. and E.L. conducted the research and wrote the paper. B.V. and F.B. designed the research study. A.d.l.F., A.G., and J.-P.M. contributed essential reagents or tools. M.G., C.D., and M.B.-B. provided clinical follow-up.
Corresponding author
Ethics declarations
Ethical standards
This study was conducted in accordance with the ethical standards set forth by the institutional and national research committees and with the 1964 Helsinki declaration and its later amendments. The research protocol was reviewed and approved by the Bordeaux University Hospital Ethics Committee. This study has been registered under registration number CER-BDX-2023-55 on May 16, 2023.
Informed consent
Informed consent was obtained from all individual participants included in the study, and patient confidentiality has been maintained in accordance with applicable privacy laws and regulations. The authors declare no conflicts of interest related to this research.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Vergara, R., Laharanne, E., de la Fouchardière, A. et al. Improving diagnostic accuracy in atypical melanocytic tumors using p16 immunohistochemistry and 9p21 fluorescence in situ hybridization: analysis of 206 second opinion cases. Sci Rep 15, 11425 (2025). https://doi.org/10.1038/s41598-025-95785-2
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-95785-2