Abstract
This study aimed to investigate whether idiopathic osteonecrosis of the femoral head (ONFH) is associated with alterations in the microstructure, histological characteristics, and transcriptomic signature in the trabecular region of the femoral head. For this purpose, we obtained trabecular bone explants from the femoral head and the intertrochanteric region of patients with idiopathic ONFH and age- matched patients with primary osteoarthritis (OA). Trabecular bone from the femoral head of ONFH patients showed lower trabecular thickness, bone volume fraction and degree of anisotropy, and a higher percentage of empty lacunae than bone samples from the intertrochanteric region of the same patients and from the femoral head of the OA group. The transcriptome analysis identified a substantial number of genes exclusively regulated in the femoral head of ONFH patients. Among these genes, we found that those highly expressed around the necrotic lesion were involved in cell division and immune response. By contrast, downregulated genes were mainly involved in cell adhesion, angiogenesis and bone formation, such as those encoding collagen type I, bone sialoprotein and several bone morphogenetic proteins. These data add new insights into mechanisms involved in the pathophysiology of idiopathic ONFH.
Similar content being viewed by others
Introduction
The most frequent diagnosis in young adults undergoing total hip arthroplasty (THA) is osteonecrosis of the femoral head (ONFH), an evolving and disabling condition that is increasingly prevalent worldwide1. ONFH is characterized by bone cell death as a result of local ischaemia. Despite efforts to stimulate subchondral bone healing and preserve the native joints, the affected bone does not usually remodel or heal normally2,3. Consequently, the lack of bone regeneration leads to femoral head collapse in a relatively short time and THA is required. The most common risk factors for developing ONFH are previous trauma, massive corticosteroid administration and alcohol abuse. However, a significant number of cases remain idiopathic, with no identifiable risk factors4. The pathological bases of non-traumatic ONFH are still not fully understood, given the difficulties of obtaining bone samples from patients in the early stages and the lack of animal models that faithfully recapitulate the disease. Most hypotheses on the potential ONFH initiation mechanism point towards an alteration in the blood supply to the subchondral bone, as a consequence of intravascular occlusion by fat emboli and thrombi, as well as intraosseous extravascular compression. Initial stages of the disease lead to the formation of a necrotic area in the weight-bearing region, often characterized by accumulation of empty lacunae5. A reparative sclerotic zone containing condensed trabecular bone is developed between the necrotic zone and the adjacent trabecular bone. The collapse of the femoral head is primarily driven by the formation of microfractures at the junction between the reparative zone and the necrotic bone due to bone remodeling imbalance and microstructural deterioration6,7. ONFH is frequently associated with bone marrow edema in the femoral head, which is closely linked with symptomatology and disease progression. Histological studies suggest that trabecular bone in the femoral head could be altered by surrounding medullary necrosis5,8. Providing further evidence on the extent of bone alterations in the femoral head of patients with ONFH may be helpful for surgeons in deciding the appropriate type of hip arthroplasty for this population.
Most studies on the pathophysiology of non-traumatic ONFH use bone explants from patients with glucocorticoid-induced ONFH undergoing THA9,10,11. However, abnormalities in the trabecular bone of these patients could be expected, given that glucocorticoids are recognized as promoting osteoblast apoptosis, reducing bone formation and prolonging the lifespan of osteoclasts12. Other studies provide limited descriptions of patients’ clinical features or combine different ONFH etiologies, making it difficult to clarify the disease mechanisms5,8,13,14,15. To date, the molecular mechanisms behind trabecular bone alterations in patients with ONFH without an obvious aetiological factor remain largely unexplored. Recent evidence indicates that idiopathic ONFH is associated with altered activity in bone-forming cells in trabecular bone of the femoral head16. In this study, we further investigate the pathophysiology of idiopathic ONFH by comparing the microstructure and histological features of trabecular bone obtained from two distinct zones of the proximal femur—the femoral head and the intertrochanteric region—in each patient. To explore the genes involved in ONFH pathophysiology, we conducted comparative analyses of the transcriptomic profile in the bone samples. For comparative purposes, bone samples from the same anatomical sites in patients with primary osteoarthritis (OA) of the hip were obtained and analysed. Both patient groups were adjusted by age and sex, which are known to affect bone structure and density17,18.
Methods
Patients and bone sample collection
Patients undergoing THA between January 2019 and December 2022 in our institution were considered for inclusion, with 29 patients younger than 70 years of age ultimately included in this study. The ONFH group included 15 cases of idiopathic Ficat and Arlet stage IV ONFH, defined after assessing conventional radiographs and magnetic resonance imaging19. Fourteen patients with primary OA of the hip were included as controls, with the groups matched by age and sex. OA was confirmed by conventional radiography. The disease period was defined as the interval between the patient’s reported symptom onset and the date of THA. Written informed consent was obtained from all patients. All procedures were approved by the Clinical Research Ethics Committee of our institution (PI- 3481; Date of Approval: 20/12/2018). Patients with risk factors such as dyslipidaemia, smoking, obesity and hypertension, which were highly prevalent in both groups, were also included. Patients with ONFH secondary to major trauma of the hips, corticosteroid treatment and excessive alcohol intake were excluded. Patients with sickle cell disease, congenital hip dysplasia, decompression sickness, Gaucher disease, haematopoietic or solid organ transplant, or who were receiving chemotherapy were also excluded, as these conditions significantly increase the risk for ONFH. Preoperative anteroposterior radiographs were used to assess femoral geometry according to the Dorr classification20. Cortical thickness indices were measured on lateral views at a point 10 cm distal and parallel to the mid-lesser trochanteric line, according to Dorr. The cortical thickness index (CTI) was calculated as the ratio of femoral diaphysis width minus medullary canal width divided by femoral diaphysis width. A lateral CTI threshold of ≤ 0.40 demonstrated high sensitivity and specificity in identifying patients with osteoporosis, as assessed by Dual Energy X-ray Absorptiometry21.
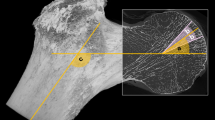
Trabecular bone explants from the femoral head of patients with ONFH were obtained intraoperatively with a curette during THA (Fig. 1). Cylindrical specimens of trabecular bone from the intertrochanteric region, located distant from the necrotic lesion, were obtained during femoral preparation using a box osteotome. Bone samples from the same anatomical sites in patients with OA were collected as controls for comparison with the ONFH samples. Due to the small size of the explants, samples from eight patients in each group were used for imaging techniques, while samples from the remaining patients were used for transcriptomic analyses.
Preoperative anteroposterior radiograph of a right hip in a 61-year-old man with osteoarthritis (OA) and in a 56-year-old man with osteonecrosis of the femoral head (ONFH). Trabecular bone explants were taken from the femoral head (1) and from the intertrochanteric region (2) in both patient groups.
Micro-computed tomography (µCT)
Trabecular bone explants were washed with PBS, fixed in 10% formalin for 24 h at 4 ºC and stored in 0.1% formalin until use. The bone samples were scanned with an X-ray microfocus computerized tomography machine (Nikon XT H 160 MedX Alpha, Nikon Metrology NV, Leuven, Belgium) at 123–130 kV and 73–85 µA. For each sample, we obtained 1500 projections that were reconstructed as 16-bit grey scale stacks with a voxel size from 10 to 13 μm. The reconstructed imaging data of bone explants were visualized using the 3D imaging software VG Studio 3.1 (Volume Graphics GmbH, Heidelberg, Germany) and analysed using the BoneJ plugin for ImageJ software22. Each region was binarised using a flat intensity threshold. A region of interest slightly smaller than the size of the specimen was defined for all cross-sections in order to avoid the inclusion of possible debris formed during sampling. The following morphometric indices were generated: trabecular thickness (Tb.Th); spacing (Tb.Sp) and number (Tb.N); bone volume fraction defined as bone volume versus total volume (BV/TV); connectivity density (Conn.D) and degree of anisotropy (DA). DA, which measures how substructures are oriented within a volume, was calculated using the mean intercept length and expressed as a normalized scalar value ranging from 0 to 1, where 1 represented fully anisotropic substructures.
Haematoxylin and eosin staining and imaging
After µCT scanning, the bone explants were decalcified in a commercial solution (Osteodec, Bio-Optica, Milan, Italy) containing EDTA for 24 h at 4 ºC. Next, the bone samples were dehydrated through a graded ethanol series, cleared in xylene and finally embedded in paraffin. After dewaxing and rehydration, 5-micron sections of retrieved samples were stained with haematoxylin and eosin and examined under an optical microscope. The percentage of empty lacunae per total lacunae and the number of cells per unit of bone surface were quantified using the ImageJ software.
Microarrays analysis of differential gene expression
Trabecular bone explants were cut into small fragments, rinsed in PBS and homogenized in QIAzol lysis reagent (Qiagen, Hilden, Germany) using an Ultra Turrax homogenizer (IKA Labor Technik, Staufen, Germany). Total RNA was purified using the RNeasy Plus Universal Mini Kit (Qiagen), demonstrating RNA Integrity Number (RIN) values greater than 6.5 for all samples. Detailed RIN values for each sample are provided in Supplementary Table S1. Subsequently, the samples were processed using the GeneChip WT PLUS Reagent Kit, hybridized to the GeneChip Human Gene 2.0 ST Array, and scanned with the GeneChip Scanner 3000 7G (all from Thermo Fisher Scientific, Waltham, MA). Log base 2 transformation of gene signals were conducted by the SST-RMA algorithm using the Transcriptome Analysis Console version 4.0 (Applied Biosystems). Fold changes between the groups were calculated as ratios of means of gene expression signals. Z scores used in heatmaps were calculated by subtracting the overall average gene intensity from the intensity for each gene and dividing the result by the standard deviation of all of the measured intensities. Conclusions gathered from microarray experiments were confirmed by reverse transcription-quantitative polymerase chain reaction analysis (RT-qPCR) for a representative number of genes (Supplementary Fig. S1). The cDNA was prepared from total RNA using a High-Capacity RNA-to-cDNA Kit (Life Technologies, Carlsbad, CA, USA). qPCR was performed using TaqMan Gene Expression Assays (Supplementary Table S2) and TaqMan Gene Expression Master Mix (both from Life Technologies) and run in a 7900HT Fast Real-TimePCR System (Applied Biosystems). Data analysis was performed using Sequence Detector Software version 2.4 (Applied Biosystems). A threshold cycle (CT) value was calculated from a log-linear plot of the PCR signal against the cycle number, and relative gene expression values were calculated using the 2−ΔΔCT method. B2M and GUSB were used as endogenous controls. Gene ontology analyses were performed using the Database for Annotation, Visualization and Integrated Discovery (DAVID; http://david.abcc.ncifcrf.gov) and the GOnet Internet application23.
Statistical analysis
Qualitative variables were described as counts and percentages and compared using the chi-squared test or Fisher’s exact test when appropriate. Quantitative variables were described as median and interquartile range or as mean and standard deviation or range and compared using the Mann-Whitney U test or the paired Wilcoxon test. The statistical analyses were performed using the R statistical package (R Foundation for Statistical Computing, Vienna, Austria) and the SPSS version 25.0 (IBM, Chicago, IL, USA). Microarray data were analysed using the Limma software included in the Transcriptome Analysis Console. The transcriptomic analyses considered genes with ≤ − 1.5 and ≥ 1.5-fold changes relative to the reference. The criterion for significance in all statistical analyses was set at p ≤ 0.05.
Results
Patients
Patient demographic and clinical characteristics are summarized in Table 1, with detailed patient-specific data in Supplementary Table S3. Both patient groups were similar in weight and BMI. No significant differences were observed between the groups in the prevalence of dyslipidemia, diabetes, obesity, or other conditions. The interval between symptom onset and severe joint function loss ranged from seven months to approximately four years, with mean durations of 27 months for OA patients and 24 months for ONFH patients. Although bilateral cases were more frequent in the ONFH group, this difference was not statistically significant. All patients exhibited a CTI greater than 0.4, with no significant difference in mean CTI between the groups. Similarly, the frequency of Dorr type B femurs was comparable between groups, and no Dorr type C femurs were observed.
Trabecular bone microstructure
Images of trabecular bone slides and volume rendering revealed differences between the femoral head and the intertrochanteric region of ONFH and OA patients (Fig. 2A-B). In both patient groups, Tb.Th, Tb.N, BV/TV, Conn.D and DA were lower in the femoral head compared with the intertrochanteric region, whereas Tb.Sp was higher. ONFH patients had lower Conn.D in the intertrochanteric region than OA patients (Fig. 2B). Interestingly, trabecular bone from the femoral head exhibited lower Tb.Th, BV/TV and DA in ONFH than in OA patients (Fig. 2A-B).
Microstructure analysis. Upper panels: Representative images of µCT slices (A) and volume rendering (B) of trabecular bone from the femoral head (FH) and the intertrochanteric region (IT) of OA and ONFH patients. Lower panels: Box plots showing (A) trabecular thickness (Tb.Th), trabecular separation (Tb.Sp) and trabecular number (Tb.N); and (B) bone volume to tissue volume ratio (BV/TV), connectivity density (Conn.D) and degree of anisotropy (DA) of trabecular bone in each group. Data are presented as medians and interquartile ranges. * p < 0.05.
Histological examination
Histological characterization of bone fragments showed that the percentage of empty lacunae was higher in the femoral head than in the intertrochancheric region of both ONFH and OA patients, as shown in representative sections of bone samples stained with haematoxylin and eosin (Fig. 3). We observed a significant increase in the number of empty lacunae in the femoral head of ONFH patients compared to the OA group. The number of bone cells on the trabecular surface was higher in the femoral head than the intertrochanteric region of ONFH patients whereas there were no differences in the OA group. It was notable that bone cells were more abundant along trabeculae from the femoral head of ONFH patients than OA patients.
Histological examination. Upper panel: Representative images of haematoxylin and eosin staining of trabecular bone from the femoral head (FH) and the intertrochanteric region (IT) of OA and ONFH patients. Arrows indicate empty lacunae while asterisks denote cells on bone surface. Lower panel: Box plots showing the percentage of empty lacunae per total lacunae and the number of bone cells (Cell.N) per bone perimeter in trabecular bone in each group. Data are presented as medians and interquartile ranges. * p < 0.05.
Transcriptomic analysis
The gene expression profile in trabecular bone from the femoral head, compared to the intertrochanteric region, was notably different between ONFH and OA patients, with a higher number of differentially expressed genes in the ONFH group (Fig. 4A). Pairwise comparisons of bone samples obtained from ONFH patients revealed 2362 protein-coding genes whose transcript levels changed by at least 1.5-fold (in either direction) (Supplementary Table S4). The changes detected in OA samples were more modest, with only 460 genes significantly affected (Supplementary Table S5). In addition, the magnitude of changes in genes regulated in the femoral head of OA patients was generally lower than in the ONFH group (Fig. 4A). The gene signature in the femoral head of ONFH and OA patients partially overlapped, with 261 genes regulated in the same direction in both groups (Fig. 4B) (Supplementary Table S6). The 30 genes whose expression changed the most in either direction in the femoral head of ONFH and OA patients are shown in Fig. 4C. One third of these genes, including ATF3, NR4A1 and CYR61, which encode proteins involved in bone maintenance and repair, were common to both patient groups and shared the same direction of change24,25,26. A range of common biological processes was enriched in genes differentially regulated in the femoral head of ONFH and OA patients (Fig. 4D) (Supplementary Table S7). The most commonly overexpressed genes in the femoral head of both groups were related to inflammation and cell division, while the most downregulated transcripts were involved in angiogenesis, cell migration and adhesion, and osteoblast differentiation (Fig. 4E). Interestingly, the number of genes associated with these biological processes was higher in the ONFH than in the OA group (Fig. 4D) (Supplementary Table S7).
Genes regulated in trabecular bone from the femoral head of ONFH and OA patients compared to the intertrochanteric region of the same patients. (A) Volcano plots showing the Log2 of the fold change (Log2 FC) values of protein-coding genes between trabecular bone from the femoral head (FH) and the intertrochanteric region (IT) of OA and ONFH patients plotted against their associated − Log10 of the p-values. Dots representing individual genes were divided in three different groups: p-value ≥ 0.05 (not significant), p-value < 0.05 and FC ≥ 1.5 (upregulated) and p-value < 0.05 and FC ≤ − 1.5 (downregulated). The top 20 differentially expressed genes are labelled. (B) Venn diagram of differentially expressed genes in the femoral head of ONFH and OA patients. (C) Heatmaps for the 30 genes with the highest fold change showing the z-score value calculated for each gene and sample. Asterisks denote genes regulated in the same direction in both patient groups. (D) Gene ontology analysis showing the most common enriched categories in biological processes in the FH of both patient groups. (E) Network representation showing 25 selected genes with the highest fold change (in either direction) annotated to the categories shown in D and commonly regulated in the FH of both groups. Genes represented in red and blue were upregulated and downregulated, respectively.
To understand the mechanisms behind alterations in trabecular bone around the necrotic lesion, we analysed the 2101 protein-coding genes that were regulated in the femoral head of ONFH patients but not in the OA group (Fig. 4B). Out of these genes, 1217 were upregulated and 884 downregulated (Fig. 5A) (Supplementary Table S8). The heatmap shows that some of the most highly regulated transcripts were involved in bone matrix formation and mineralization, such as COL1A1, SMAD6, IBSP and ENPP1 (Fig. 5B). Gene ontology analysis of the overexpressed genes in trabecular bone around the necrotic lesion revealed processes related to superoxide anion generation, oxygen transport, cell division and immune response (Fig. 5C) (Supplementary Table S9). Figure 5D depicts the genes with the highest fold change that are involved in these biological processes, such as RBM38, KIFC1 (cell cycle), HBG2 (oxygen transport) and CHI3L1 (inflammatory response). The subset of downregulated genes in the femoral head of ONFH patients were associated with angiogenesis, cell adhesion and migration, and response to hypoxia (Fig. 5E) (Supplementary Table S9). Among processes related to bone formation and response to mechanical stimulus, we found downregulated genes involved in extracellular matrix organization (COL1A1), osteoblast differentiation and bone mineralization (IBSP, SMAD6, ENPP1), and BMP signalling pathway (BMP2, BMP4, BMP6) (Fig. 5F).
Genes exclusively regulated in trabecular bone from the femoral head of ONFH patients compared to the intertrochanteric region of the same patients. (A) Volcano plot showing the Log2 of the fold change (Log2 FC) values of protein-coding genes between trabecular bone from the femoral head (FH) and the intertrochanteric region (IT) of ONFH patients plotted against their associated − Log10 of the p-values. Dots representing individual genes were divided in three different groups: p-value ≥ 0.05 (not significant), p-value < 0.05 and FC ≥ 1.5 (upregulated) and p-value < 0.05 and FC ≤ − 1.5 (downregulated). The top 20 differentially expressed genes are labelled. (B) Heatmap for the 30 genes with the highest fold change showing the z-score value calculated for each gene and sample. Gene ontology analysis showing the most enriched categories in biological processes for upregulated (C) and downregulated (E) genes in the FH. Network representation showing the 20 most highly upregulated (D) or downregulated (F) genes annotated to the categories shown in C and E, respectively. Genes represented in the round nodes were coloured according to the Log2 FC.
Next, we investigated whether the gene expression signature of trabecular bone from the femoral head differed between ONFH and OA patients. There were 336 differentially expressed genes in bone samples from the ONFH group, evenly distributed between 172 upregulated and 164 downregulated genes (Fig. 6A) (Supplementary Table S10). Genes whose expression was induced were related to biological processes such as immune response and chemotaxis, while downregulated genes were associated with cell adhesion and migration (Fig. 6B). Interestingly, the transcriptomic analysis identified 53 genes that were regulated in the femoral head of ONFH patients compared to bone samples from the intertrochanteric region of the same patients (Fig. 6C). Of these, 33 were modulated in the same direction (Supplementary Table S11), including genes that encode mediators of inflammation, such as CCL5, CCL18 and CHIT1, which were upregulated (Fig. 6D).
Differentially expressed genes in trabecular bone from the femoral head of ONFH and OA patients. (A) Volcano plot showing the Log2 of the fold change (Log2 FC) values of protein-coding genes in trabecular bone from the femoral head (FH) between ONFH and OA patients plotted against their associated − Log10 of the p-values. Dots representing individual genes were divided in three different groups: p-value ≥ 0.05 (not significant), p-value < 0.05 and FC ≥ 1.5 (upregulated) and p-value < 0.05 and FC ≤ − 1.5 (downregulated). The top 20 differentially expressed genes are labelled. (B) Number of differentially expressed genes in the FH of ONFH patients annotated to selected gene ontology terms. (C) Venn diagram of genes regulated in the FH of ONFH patients when compared to the intertrochanteric region (IT) of the same patients or to the FH of OA patients. (D) Graph showing the fold change of eight selected genes of the overlapping region shown in C.
Finally, we analysed data from a prior bioinformatics study by Duan et al.,13 which identified 481 genes regulated in the femoral head subchondral bone of ONFH patients when compared to bone samples from individuals with freshly incurred femoral neck fractures. Out of these genes, 101 were also differentially regulated in our study (Table 2). Overlapping genes downregulated in the subchondral and trabecular bone were associated with angiogenesis (4 genes, fold enrichment (FE) = 10.9), cell adhesion (3 genes, FE = 9.8), migration (4 genes, FE = 10.0) and differentiation (4 genes, FE = 4.1) (Supplementary Table S12). The comparison between genes identified by Duan et al. and the 336 genes identified in the present study as differentially regulated in the femoral heads of ONFH and OA groups revealed seven common genes that shared the same expression direction (Table 2). Two of them, KIF3A and HYOU1, which are involved in osteoblast differentiation and response to hypoxia, respectively, were downregulated27,28,29.
Discussion
This study included ONFH and OA patients with comparable demographic and clinical characteristics, including age and sex, which are known to influence bone quality30,31. The similarity in these characteristics, as well as comparable CTI values between the groups, enabled a more accurate comparison of the effects of ONFH on bone features relative to OA, thereby minimizing potential confounding factors. Bone microarchitecture varies between anatomical locations due to different mechanical loading environments and remodelling rates32. This study showed that trabeculae in the femoral head of ONFH and OA patients were thinner and more widely separated than in the intertrochanteric region, which correlated with lower bone volume fraction, connectivity density and degree of anisotropy. These differences may be expected, given that the femoral head has to withstand continuous high compressive forces, whereas the intertrochanteric region is also subjected to significant tensile forces33,34. More importantly, trabecular bone in the femoral head of ONFH patients exhibited some bone loss, as its trabeculae were thinner than those in the same sampling area in OA patients. Trabecular thinning was associated with a reduction in bone volume fraction and microstructural anisotropy, which are determinants of trabecular bone stiffness35. Previous data indicate that the affected subchondral bone area in the femoral head of ONFH patients shows signs of impaired mineralization15. The positive correlation between bone volume fraction determined by µCT and mineral content measured by dual-energy X-ray absorptiometry suggests that reduced trabecular bone volume in the femoral head of ONFH patients results from a lower mineralization capacity in bone-forming cells, as supported previous in vitro studies16,36,37.
An increase in osteocyte apoptosis has been linked to the pathogenesis of ONFH induced by corticosteroids or ethanol abuse38,39. The mechanism that initiates osteocyte death is not well understood, but involves microdamage formation in the bone matrix, which positively correlates with decreased bone stiffness40,41. The presence of empty lacunae is widely accepted as an indicator of osteocytic cell death. In our study, we observed a significant increase in the number of empty lacunae in the femoral head of ONFH and OA patients compared to the intertrochanteric region, probably as a result of differential bone adaptation to mechanical loading between the two anatomical sites. The significantly higher number of empty lacunae in trabecular bone of the femoral head of ONFH patients compared to OA patients might be a consequence of surrounding medullary necrosis, while the increased number of bone cells in this anatomical site likely reflects an active repair process in response to osteocyte dysfunction or death.
Trabecular bone in the femoral head and the intertrochanteric region exhibited different transcriptome profiles. Genes regulated in the femoral head of both ONFH and OA patients were involved in cell division, migration and osteoblast differentiation, processes tightly regulated by mechanical forces42. Importantly, a substantial number of genes were exclusively upregulated in the femoral head of ONFH patients, many of which encoded proteins related to cell division and immune response. Previous data showed that glucocorticoid-induced ONFH is associated with chronic inflammation and reactive oxygen species (ROS) generation43. Analysis of genes regulated in subchondral bone of ONFH patients compared to individuals with freshly incurred femoral neck fractures suggest a relationship between ONFH and an imbalance in levels of innate immune cells13. In our study, overexpressed genes in trabecular bone of the femoral head were associated with strong inflammatory processes, indicating that inflammation is a likely mechanism in the maintenance of the disease. This inflammatory signature coincided with the upregulation of genes involved in ROS generation and oxygen transport, probably because of persistent hypoxia-induced tissue damage. While protein levels were not quantified in the present study, a recent proteomic analysis identified differentially expressed proteins related to immune response, inflammatory reaction, and oxidative stress in the femoral heads of ONFH patients with bone marrow edema44. ONFH has been associated with endothelial dysfunction in the subchondral bone due to chronic inflammation and elevated ROS production following ischaemic injury45. Our findings suggest that bone vasculature damage is extensive in the femoral head, as a large number of genes related to angiogenesis, cell adhesion and migration were downregulated in the trabecular region. An insufficient vascular niche led to an inadequate oxygen and nutrient supply to affected areas, as well as impaired tissue repair.
An integrated analysis using available transcriptomic and proteomic datasets in hip cartilage and bone tissue, respectively, of ONFH patients showed elevated hypoxia and osteoclast differentiation as major pathways associated with the disease46. While our analyses did not detect genes related to altered bone resorption in the femoral heads of ONFH patients, we found downregulated genes associated with biological processes crucial for bone formation and response to mechanical stimuli, including COL1A1. A previous analysis of common differentially expressed genes in the subchondral bone and cartilage of ONFH patients identified altered COL1A1 expression levels, suggesting that collagen metabolism is likely affected by ONFH progression47. Complementing these genetic insights, metabolomic data indicated that ONFH pathophysiology is marked by inflammatory processes and osteoblast dysregulation, as evidenced by altered linoleic acid metabolism, yielding potential diagnostic biomarkers48. Our data show that genes involved in the bone mineralization process included IBSP, whose transcript levels were also reduced in osteoblasts isolated from the femoral head of patients with idiopathic ONFH16. IBSP expression in osteoblasts increases after stimulation with BMP2, which, together with BMP4 and BMP6, induces osteogenic differentiation of mesenchymal precursors49,50. The present study revealed that transcript levels of these growth factors decreased in the trabecular bone around the necrotic lesion. Altogether, these data suggest that reduced expression levels of genes involved in bone formation may account for the altered trabecular bone microstructure in the femoral head of patients with idiopathic ONFH. A recent proteomic study suggests that impaired bone formation may be associated with reduced protein levels involved in glucose metabolic processes, including glucose transporter member 1 51. Notably, while ONFH primarily affects the femoral head, accumulating evidence suggests it may also influence systemic bone metabolism. For example, studies have demonstrated that patients with ONFH exhibit decreased lumbar spine BMD52 and increased urinary deoxypyridinoline/creatinine ratios53 compared with healthy subjects, indicating altered systemic bone metabolism. Furthermore, compared to OA, patients with ONFH have shown higher serum levels of adiponectin, an adipocyte-derived hormone inversely related to BMD52,53. Future studies will integrate protein-level data to complement our current gene expression findings.
Our data identified a significant number of upregulated genes involved in the immune response in femoral head trabecular bone of ONFH patients compared to the OA group. Among these genes, CCL5 and CCL18 were also upregulated in the femoral head of ONFH patients compared to the intertrochanteric region of the same patients. These chemokines play an important role in the regulation of bone remodelling; however, their elevated levels have been observed in diseases associated with chronic inflammation, such as rheumatoid arthritis 54. Several downregulated genes involved in skeletal system development, including KIF3A, were detected in the femoral head of ONFH patients compared to OA patients. KIF3A encodes a protein essential for the formation of primary cilia, an important mechanosensor required for bone formation27,28. Interestingly, KIF3A expression was reduced in the subchondral bone of patients with ONFH13. In addition, pairwise comparisons showed a trend toward lower KIF3A transcript levels (fold change = − 1.45; p = 0.004) in the femoral head of ONFH patients compared to the intertrochanteric region. We suggest that KIF3A downregulation in trabecular bone of ONFH patients could potentially lead to decreased bone adaptability. Mechanotransduction, the process by which bone cells respond to mechanical stimuli and adapt their structure and density, is essential for bone remodeling. Therefore, a reduction in KIF3A expression levels could impair this process, potentially contributing to the trabecular bone microstructural fragility observed in ONFH.
This study has several limitations. First, the limited sample size and interindividual variability inherently reduce the statistical power of comparative studies between ONFH and OA patients and potentially affect the generalizability of our findings. However, pairwise comparisons between two anatomical regions, the femoral head and the intertrochanteric region, in the same patient remove subject-related variability and increase the power of the analysis. While our results provide valuable insights into the molecular mechanisms underlying ONFH, larger studies are needed to validate and expand upon these findings. Second, due to the ethical difficulties in obtaining bone biopsies from healthy donors, the control group consisted of patients with primary OA undergoing THA. Advanced OA is known to involve changes in bone density and microstructure in trabecular bone proximal to the osteotomy site and even distant from the affected joint55,56. Control samples obtained from patients with fractures due to osteoporosis or traumatic events would likely lead to even more confounding results. Finally, it should be noted that the present study includes patients with end-stage ONFH, from whom bone explants were collected during THA. Therefore, the results drawn from the collected data can only be applied to the end-stage disease.
In conclusion, this study identifies, for the first time, alterations in the microstructure, histological features, and transcriptomic signature in the macroscopically healthy region of the femoral head of patients with idiopathic ONFH. Bone quality in the distal area of the femoral head has been a concern in stemless hip arthroplasty such as hip resurfacing or those THA with ultra-short stems57,58. The present findings provide new insights into the extent of bone alterations in the femoral head of patients with late stage ONFH, which may aid surgeons in determining the appropriate type of hip arthroplasty.
Data availability
Transcriptomic datasets generated and analysed in this study are included as supplementary files. Remaining datasets are available from the corresponding author upon reasonable request.
References
Mayers, W. et al. National trends and in hospital outcomes for total hip arthroplasty in avascular necrosis in the united States. Int. Orthop. 40, 1787–1792 (2016).
Gómez-Barrena, E., Padilla-Eguiluz, N. G., López-Marfil, M., Ruiz de la Reina, R. & REBORNE Consortium. Volume and location of bone regeneration after autologous expanded mesenchymal stromal cells in hip osteonecrosis: a pilot study. Bone Joint Res. 11, 881–889 (2022).
Atilla, B., Bakırcıoğlu, S., Shope, A. J. & Parvızı, J. Joint-preserving procedures for osteonecrosis of the femoral head. EFORT Open. Rev. 4, 647–658 (2020).
Fukushima, W. et al. Nationwide epidemiologic survey of idiopathic osteonecrosis of the femoral head. Clin. Orthop. Relat. Res. 468, 2715–2724 (2010).
Mutijima, E., De Maertelaer, V., Deprez, M., Malaise, M. & Hauzeur, J. P. The apoptosis of osteoblasts and osteocytes in femoral head osteonecrosis: its specificity and its distribution. Clin. Rheumatol. 33, 1791–1795 (2014).
Narayanan, A. et al. Avascular necrosis of femoral head: a metabolomic, biophysical, biochemical, electron microscopic and histopathological characterization. Sci. Rep. 7, 10721 (2017).
Wang, C. et al. Analysis of early stage osteonecrosis of the human femoral head and the mechanism of femoral head collapse. Int. J. Biol. Sci. 14, 156–164 (2018).
Calder, J. D., Pearse, M. F. & Revell, P. A. The extent of osteocyte death in the proximal femur of patients with osteonecrosis of the femoral head. J. Bone Joint Surg. Br. 83, 419–422 (2001).
Wu, T. et al. Identification and validation of Endoplasmic reticulum stress-related genes in patients with steroid-induced osteonecrosis of the femoral head. Sci. Rep. 14, 21634 (2024).
Hou, W. et al. Plasma SQSTM1/p62 act as a biomarker for steroid-induced osteonecrosis of the femoral head. Sci. Rep. 14, 24932 (2024).
Ma, T. et al. Research progress in the pathogenesis of hormone-induced femoral head necrosis based on microvessels: a systematic review. J. Orthop. Surg. Res. 19, 265 (2024).
Gado, M., Baschant, U., Hofbauer, L. C. & Henneicke, H. Bad to the bone: the effects of therapeutic glucocorticoids on osteoblasts and osteocytes. Front. Endocrinol. 13, 835720 (2022).
Duan, X. et al. Bioinformatic analysis of related immune cell infiltration and key genes in the progression of osteonecrosis of the femoral head. Front. Immunol. 14, 1340446 (2023).
Ma, J. X. et al. Bone microarchitecture and biomechanics of the necrotic femoral head. Sci. Rep. 7, 13345 (2017).
Pascart, T. et al. Subchondral involvement in osteonecrosis of the femoral head: insight on local composition, microstructure and vascularization. Osteoarthr. Cartil. 30, 1103–1115 (2022).
Maestro-Paramio, L., García-Rey, E., Bensiamar, F. & Saldaña, L. Osteoblast function in patients with idiopathic osteonecrosis of the femoral head. Bone Joint Res. 10, 619–628 (2021).
Sigurdsson, G. et al. Increasing sex difference in bone strength in old age: the age, gene/environment Susceptibility-Reykjavik study (AGES-REYKJAVIK). Bone 39, 644–651 (2006).
Riggs, B. L. et al. Population-based study of age and sex differences in bone volumetric density, size, geometry, and structure at different skeletal sites. J. Bone Min. Res. 19, 1945–1954 (2004).
Ficat, R. & Arlet, J. Forage-biopsie de La tete femorale Dans i’osteonecrose primative. Observations histo-pathologiques portant Sur Huit forages. Rev. Rhum. 31, 257–264 (1964).
Dorr, L. D. et al. Structural and cellular assessment of bone quality of proximal femur. Bone 14, 231–242 (1993).
Sah, A. P., Thornhill, T. S., LeBoff, M. S. & Glowacki, J. Correlation of plain radiographic indices of the hip with quantitative bone mineral density. Osteoporos Int. 18, 1119–1126 (2007). (2007).
Doube, M. et al. BoneJ: free and extensible bone image analysis in ImageJ. Bone 47, 1076–1079 (2010).
Pomaznoy, M., Ha, B. & Peters, B. GOnet: A tool for interactive gene ontology analysis. BMC Bioinform. 19, 470 (2018).
Zhao, G. et al. CYR61/CCN1 regulates sclerostin levels and bone maintenance. J. Bone Min. Res. 33, 1076–1089 (2018).
Scholtysek, C. et al. NR4A1 regulates motility of osteoclast precursors and serves as target for the modulation of systemic bone turnover. J. Bone Min. Res. 33, 2035–2047 (2018).
Yang, J., Fan, Y. & Liu, S. ATF3 as a potential diagnostic marker of early-stage osteoarthritis and its correlation with immune infiltration through bioinformatics analysis. Bone Joint Res. 11, 679–689 (2022).
Qiu, N. et al. Disruption of Kif3a in osteoblasts results in defective bone formation and osteopenia. J. Cell. Sci. 125, 1945–1957 (2012).
Chen, J. C., Hoey, D. A., Chua, M., Bellon, R. & Jacobs, C. R. Mechanical signals promote osteogenic fate through a primary cilia-mediated mechanism. FASEB J. 30, 1504–1511 (2016).
Rao, S. et al. Biological function of HYOU1 in tumors and other diseases. Onco Targets Ther. 14, 1727–1735 (2021).
Becerikli, M. et al. Age- dependent alterations in osteoblast and osteoclast activity in human cancellous bone. J. Cell. Mol. Med. 21, 2773–2781 (2017).
Ingram, R. T., Park, Y. K., Clarke, B. L. & Fitzpatrick, L. A. Age- and gender- related changes in the distribution of osteocalcin in the extracellular matrix of normal male and female bone. Possible involvement of osteocalcin in bone remodeling. J. Clin. Invest. 93, 989–997 (1994).
Turunen, M. J., Prantner, V., Jurvelin, J. S., Kröger, H. & Isaksson, H. Composition and microarchitecture of human trabecular bone change with age and differ between anatomical locations. Bone 54, 118–125 (2013).
Rudman, K. E., Aspden, R. M. & Meakin, J. R. Compression or tension? The stress distribution in the proximal femur. Biomed. Eng. Online. 5, 12 (2006).
Lotz, J. C., Cheal, E. J. & Hayes, W. C. Stress distributions within the proximal femur during gait and falls: implications for osteoporotic fracture. Osteoporos. Int. 5, 252–261 (1995).
Maquer, G., Musy, S. N., Wandel, J., Gross, T. & Zysset, P. K. Bone volume fraction and fabric anisotropy are better determinants of trabecular bone stiffness than other morphological variables. J. Bone Min. Res. 30, 1000–1008 (2015).
Perilli, E. et al. Failure strength of human vertebrae: prediction using bone mineral density measured by DXA and bone volume by micro-CT. Bone 50, 1416–1425 (2012).
Zupan, J. et al. Osteoarthritic versus osteoporotic bone and intra-skeletal variations in normal bone: evaluation with ΜCT and bone histomorphometry. J. Orthop. Res. 31, 1059–1066 (2013).
Weinstein, R. S., Nicholas, R. W. & Manolagas, S. C. Apoptosis of osteocytes in glucocorticoid-induced osteonecrosis of the hip. J. Clin. Endocrinol. Metab. 85, 2907–2912 (2000).
Calder, J. D. F., Buttery, L., Revell, P. A., Pearse, M. & Polak, J. M. Apoptosis-a significant cause of bone cell death in osteonecrosis of the femoral head. J. Bone Joint Surg. Br. 86, 1209–1213 (2004).
Seref-Ferlengez, Z., Basta-Pljakic, J., Kennedy, O. D., Philemon, C. J. & Schaffler, M. B. Structural and mechanical repair of diffuse damage in cortical bone in vivo. J. Bone Min. Res. 29, 2537–2544 (2014).
Wu, Z., Laneve, A. J. & Niebur, G. L. In vivo microdamage is an indicator of susceptibility to initiation and propagation of microdamage in human femoral trabecular bone. Bone 55, 208–215 (2013).
Wang, L., You, X., Zhang, L., Zhang, C. & Zou, W. Mechanical regulation of bone remodeling. Bone Res. 10, 16 (2022).
Chen, K. et al. Steroid-induced osteonecrosis of the femoral head reveals enhanced reactive oxygen species and hyperactive osteoclasts. Int. J. Biol. Sci. 16, 1888–1900 (2020).
Mo, L. et al. The pathomechanism of bone marrow edema in the femoral head necrosis with pericollapse stage. Sci. Rep. 15, 1166 (2025).
Shao, W. et al. Unraveling the role of endothelial dysfunction in osteonecrosis of the femoral head: A pathway to new therapies. Biomedicines 12, 664 (2024).
Naik, A. A. et al. Systems analysis of avascular necrosis of femoral head using integrative data analysis and literature mining delineates pathways associated with disease. Sci. Rep. 22, 18099 (2020).
Wang, X. et al. Transcriptomic integration and ligand-receptor crosstalk reveal the underlying molecular mechanisms between hip cartilage and subchondral bone in osteonecrosis of femoral head. Gene 939, 149179 (2025).
Zhu, W. et al. GC-MS based comparative metabolomic analysis of human cancellous bone reveals the critical role of Linoleic acid metabolism in femur head necrosis. Metabolomics 19, 86 (2023).
Ingwersen, L. C. et al. BMP-2 Long-Term stimulation of human Pre-Osteoblasts induces osteogenic differentiation and promotes transdifferentiation and bone remodeling processes. Int. J. Mol. Sci. 23, 3077 (2022).
Lavery, K., Swain, P., Falb, D. & Alaoui-Ismaili, M. H. BMP-2/4 and BMP-6/7 differentially utilize cell surface receptors to induce osteoblastic differentiation of human bone marrow-derived mesenchymal stem cells. J. Biol. Chem. 283, 20948–20958 (2008).
Luo, H. et al. Elucidating the role of the GC/GR/GLUT1 axis in steroid-induced osteonecrosis of the femoral head: A proteomic approach. Bone 183, 117074 (2024).
Gangji, V. et al. Non traumatic osteonecrosis of the femoral head is associated with low bone mass. Bone 107, 88–92 (2018).
Tian, L., Baek, S. H., Jang, J. A. & Kim, S. Y. Imbalanced bone turnover markers and low bone mineral density in patients with osteonecrosis of the femoral head. Int. Orthop. 42, 1545–1549 (2018).
Floerkemeier, T. et al. Do biomarkers allow a differentiation between osteonecrosis of the femoral head and osteoarthritis of the hip? - a biochemical, histological and gene expression analysis. Osteoarthr. Cartil. 29, 1614–1623 (2021).
Naot, D., Musson, D. S. & Cornish, J. The activity of adiponectin in bone. Calcif Tissue Int. 100, 486–499 (2017).
Murayama, M. A., Shimizu, J., Miyabe, C., Yudo, K. & Miyabe, Y. Chemokines and chemokine receptors as promising targets in rheumatoid arthritis. Front. Immunol. 14, 1100869 (2023).
Auger, J. D., Naik, A. J., Murakami, A. M., Gerstenfeld, L. C. & Morgan, E. F. Spatial assessment of femoral neck bone density and microstructure in hip osteoarthritis. Bone Rep. 16, 101155 (2021).
Sánchez-Sabaté, E., Alvarez, L., Gil-Garay, E., Munuera, L. & Vilaboa, N. Identification of differentially expressed genes in trabecular bone from the Iliac crest of Osteoarthritic patients. Osteoarthr. Cartil. 17, 1106–1114 (2009).
Park, C. W., Lim, S. J., Kim, J. H. & Park, Y. S. Hip resurfacing arthroplasty for osteonecrosis of the femoral head: Implant-specific outcomes and risk factors for failure. J. Orthop. Translat. 21, 41–48 (2020).
McMinn, D. J. W., Daniel, J., Ziaee, H. & Pradhan, C. Indications and results of hip resurfacing. Int. Orthop. 35, 231–237 (2011).
Acknowledgements
We are indebted to the Immunohistochemistry Facility of the Hospital Universitario La Paz-IdiPAZ, the CT-SCAN laboratory of the National Museum of Science and Technology of Madrid and the Genomic Unit of the Complutense University of Madrid for excellent technical support. The authors would like to thank Fátima Bensiamar and Beatriz García (Hospital Universitario La Paz-IdiPAZ) for their excellent technical support and Dr Clara Escudero (Centro de Investigación Biomédica en Red de Bioingeniería, Biomateriales y Nanomedicina, CIBER-BBN) for her technical help in bone histology.
Funding
This work (including open access funding) was funded by grants PI18/00643 and PI22/00939 from Instituto de Salud Carlos III (ISCIII) and co-funded by the European Union (to L.S. and E.G.R.), grants S2022/BMD-7406 from Autonomous Community of Madrid, Spain and PID2021-126325OB-I00 from MCIN/AEI/10.13039/501100011033 and “ERDF A way of making Europe” (to N.V.) and Luis Alvarez grants from FIB-HULP (to L.S. and N.V.).
Author information
Authors and Affiliations
Contributions
L.S. conceived the project, designed and conducted the experiments, interpreted the results, and wrote the manuscript. G.V. conducted the experiments, interpreted the results, and reviewed the manuscript. N.V. interpreted the results and reviewed the manuscript. E.G.R. recruited the study participants, provided the biological samples, interpreted the results, and reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The protocol of this study was reviewed and approved by the Clinical Research Ethics Committee of Hospital Universitario La Paz. All experiments were carried out in accordance with the approved guidelines and regulations. Written informed consent was obtained from all patients.
Consent for publication
All participating authors give their consent for this work to be published.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Saldaña, L., Vallés, G., Vilaboa, N. et al. Microstructural and transcriptomic characterization of trabecular bone in idiopathic osteonecrosis of the femoral head. Sci Rep 15, 11999 (2025). https://doi.org/10.1038/s41598-025-96726-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-96726-9