Abstract
Mycolic acids, long-chain α-alkyl, β-hydroxy fatty acids, are characteristic for the genus Mycobacterium and play a critical role in the structural integrity and pathogenicity of mycobacterial cell walls. The unique structural diversity of mycolic acids among various Mycobacterium species offers a reliable biomarker for taxonomic differentiation. In this study, we applied flow injection analysis coupled with tandem mass spectrometry (FIA-MS/MS) for a comprehensive profiling of mycolic acids. Our findings demonstrate that the structural diversity of mycolic acids can be effectively utilized to enhance the accuracy, sensitivity, and scalability of mycobacterial identification methods. This technique has a broad applications for the rapid identification of mycobacterial pathogens and determination of drug resistance. Particularly in clinical diagnostics it may lead to improvement of patient management and treatment outcomes. Additionally, the method holds promise for epidemiological surveillance, enabling the tracking of mycobacterial outbreaks, as well as applications in environmental microbiology for the detection and monitoring of mycobacteria in diverse ecosystems.
Similar content being viewed by others
Introduction
The genus Mycobacterium encompasses a diverse range of species, including significant human pathogens such as Mycobacterium tuberculosis, the etiological agent of tuberculosis (TB), and Mycobacterium leprae, which causes leprosy1. This genus also includes numerous non-tuberculous mycobacteria (NTM), many of which are increasingly recognized as emerging pathogens, particularly in immunocompromised individuals2. The phenotypic and genetic diversity within this genus poses substantial challenges for species identification and classification. Mycobacteria possess complex, lipid-rich cell walls that play a crucial role in their pathogenicity, immune evasion, and resistance to antimicrobial treatments1. Among the key components of these cell walls are mycolic acids, which exhibit considerable variability between species in terms of chain length, degree of unsaturation, and functional group modifications3. These structural differences have been widely investigated as potential chemotaxonomic markers for distinguishing mycobacterial species. Precise differentiation of mycobacteria is critical for effective clinical diagnostics, epidemiological studies, and the development of public health strategies. Treatment regimens and disease outcomes vary significantly across species, necessitating accurate identification to guide appropriate therapeutic interventions. Additionally, the rise in antibiotic resistance among Mycobacterium species further underscores the need for robust diagnostic tools to enable targeted treatments. Advances in lipidomic and mass spectrometry technologies have enhanced the resolution of mycolic acid profiling, offering a promising avenue for improving the identification and characterization of mycobacterial species.
Traditional approaches to the identification of mycobacteria include culture-based methods, which involve growing the bacteria in specialized media, followed by biochemical tests and morphological characterization4,5. However, these techniques are laborious, time-consuming, and often yield results after several weeks due to the slow-growing nature of many mycobacterial species. Moreover, certain species exhibit overlapping biochemical profiles, making it difficult to distinguish them with these methods alone. Molecular techniques, such as polymerase chain reaction (PCR) and 16S rRNA gene sequencing, have improved the accuracy of identification, but these approaches also have limitations, including the need for specialized equipment and potential issues with genetic variability within species4.
In light of these challenges, lipid profiling has emerged as a complementary method for mycobacterial differentiation. The cell walls of mycobacteria are highly lipid-rich, consisting of complex lipids such as glycolipids, phospholipids, and, most importantly, mycolic acids. Mycolic acids are high-molecular-weight α-alkyl, β-hydroxy fatty acids that are unique to the genus Mycobacterium and play a key role in the structural integrity and impermeability of the mycobacterial cell wall6. These molecules confer resistance to desiccation, antibiotics, and host immune responses, making them critical to the survival and pathogenicity of mycobacteria7. Importantly, the structure of mycolic acids varies between species, particularly in terms of chain length, degree of unsaturation, and functional group modifications, making them excellent taxonomic markers for species differentiation8.
Given their structural variability, mycolic acids have been the focus of several studies aimed at differentiating Mycobacterium species. Earlier methods of analyzing mycolic acids involved thin-layer chromatography (TLC) and gas chromatography-mass spectrometry (GC-MS)9,10,11. While these techniques provided valuable insights into mycolic acid composition, they were often limited by the need for derivatization steps, lower sensitivity, and longer analysis times. Recent advancements in analytical techniques, particularly the development of liquid chromatography coupled with tandem mass spectrometry (LC-MS/MS), have revolutionized lipidomics by enabling the rapid and sensitive detection of lipids in complex biological samples without extensive sample preparation12. LC-MS/MS offers several advantages over traditional methods for mycolic acid profiling. First, it provides high sensitivity and specificity, allowing for the detection of mycolic acids at very low concentrations, which is particularly valuable in clinical samples where bacterial load may be low. Second, LC-MS/MS enables detailed structural elucidation of mycolic acids by analyzing their fragmentation patterns, which can reveal subtle differences in chain length, saturation, and functional group modifications. This level of detail is critical for distinguishing closely related species, such as those within the Mycobacterium tuberculosis complex (MTB) and between pathogenic and non-pathogenic NTMs.
In this study, we apply the FIA-MS/MS technique to profile the mycolic acids of various Mycobacterium species, with a focus on differentiating clinically relevant pathogens. By leveraging the unique structural features of mycolic acids, we aim to develop a rapid, accurate, and scalable method for the identification of Mycobacterium species. This approach has significant implications for improving diagnostic workflows in clinical microbiology laboratories, as well as for advancing our understanding of mycobacterial taxonomy and pathogenesis.
Results
Optimization of sample preparation
An extraction procedure adapted from published protocols was employed, involving successive alkaline hydrolysis in an organic solvent at elevated temperatures, followed by neutralization and liquid-liquid extraction12. The original protocol for isolating mycolic acids underwent extensive optimization, incorporating 18 distinct modifications. These focused on critical steps such as cell pretreatment, including the extraction and removal of surface lipids using methanol; adjustments to alkali hydrolysis parameters, including alkali concentrations, reaction temperatures, and incubation times; and improvements to the extraction process, such as optimizing the solvent volumes and extraction durations to maximize yield and efficiency. Each modification was meticulously evaluated for reproducibility and repeatability to ensure reliable and consistent results. Compared to the original protocol, the optimized method demonstrated significantly enhanced sensitivity, robustness, and overall analytical performance.
Validation of the analytical method
The validation method focused on evaluating all parameters characterizing the entire procedure, including sample preparation and FIA-MS/MS analysis, as a diagnostic method for the identification of Mycobacterium species and the potential assessment of their drug resistance. Validation encompassed a comprehensive set of parameters: recovery, sensitivity, limit of detection (LOD), lower limit of quantitation (LLOQ), working range, precision, repeatability, reproducibility, relative diagnostic sensitivity, and diagnostic specificity. Each parameter was rigorously tested to ensure the method’s reliability and applicability in clinical diagnostics. Recovery was assessed to verify the efficiency of the extraction and analytical steps, while sensitivity and LOD were evaluated to confirm the method’s ability to detect low concentrations of mycolic acids. Precision and reproducibility analyses included intra- and inter-assay variability to guarantee consistent performance across different runs, laboratories, and operators. Diagnostic sensitivity and specificity were validated against a library of reference strains and clinical isolates to ensure accurate identification of Mycobacterium species and their differentiation from non-mycobacterial samples.
The validated method demonstrated high reliability and robustness, making it suitable for routine clinical diagnostics and research applications. A detailed summary of the validation criteria and performance metrics is presented in Table 1.
Recovery rates and method performance
Recovery studies were performed concurrently on pooled urine and sputum samples collected from healthy volunteers. These samples were spiked with a commercially available mycolic acid mixture derived from Mycobacterium tuberculosis (Sigma-Aldrich) to evaluate the efficiency and accuracy of the extraction and quantification process. Enrichment levels of 1 µg/mL and 10 µg/mL of the mycolic acid mixture were used for the experiments. The recovery rates demonstrated excellent method performance, with values of 104.0% and 95.9% observed for sputum samples and 103.5% and 97.5% for urine samples at the 1 µg/mL and 10 µg/mL enrichment levels, respectively. These results indicate a robust and reliable method capable of efficiently extracting and quantifying mycolic acids across a range of concentrations. The slightly elevated recovery values at the lower enrichment level (1 µg/mL) suggest high sensitivity and minimal matrix interference, making this method particularly suited for detecting low concentrations of mycolic acids in clinical samples. Such consistent recovery rates across different biological matrices highlight the method’s versatility and potential applicability in diverse diagnostic and research settings.
Limits of detection, quantitation and working range
Tests were conducted to determine the analytical sensitivity and working range of the method for three selected reference strains of Mycobacterium: M. tuberculosis H37Rv ATCC 25618, M. smegmatis ATCC 19420, and M. abscessus ATCC 23045. Bacterial suspensions of defined densities were systematically diluted to achieve appropriate bacterial counts. In parallel, reduction cultures were performed on solid Löwenstein-Jensen (L-J) medium to confirm the exact number of bacteria. The resulting bacterial pellets were subjected to extraction and FIA-MS/MS analysis of mycolic acids. The working range limits of the method were established based on the XIC intensity for the most prominent mycolic acid in the profile of each selected strain. Detection limits (LOD) and the lower limit of quantification (LLOQ) were determined using the signal-to-noise ratio for the chosen XIC. The upper limit of quantification (ULOQ) was defined as the highest bacterial concentration at which the regression parameter (R²) remained greater than 0.990. As shown in Table 1, the developed method demonstrated exceptional analytical sensitivity, capable of detecting single mycobacterial cells. Additionally, it exhibited a wide working range spanning six orders of magnitude. These results highlight the robustness and reliability of the method for quantifying mycolic acids across diverse concentrations, making it well-suited for both low- and high-density bacterial samples in diagnostic and research applications.
Method precision, repeatability, and reproducibility
Precision, repeatability, and reproducibility studies were conducted in parallel on three Mycobacterium strains previously selected and used for analytical sensitivity testing. Mycobacterial pellets of 106 to 107 CFU (colony forming units), were subjected to mycolic acid extraction and FIA-MS/MS analysis. The area under the XIC curve for the most prominent mycolic acid signal of each strain was used to calculate these validation parameters. The method’s precision was assessed by performing 10 consecutive analyses of the same sample, while repeatability and reproducibility were evaluated through six independent extractions and FIA-MS/MS analyses conducted daily. Repeatability involved a single analyst performing all procedures, whereas reproducibility included the involvement of two different analysts to simulate variations in laboratory handling. The results, expressed as relative standard deviation (RSD), are summarized in Table 1. The findings demonstrate that the developed method, despite being based on the FIA-MS/MS technique, exhibits exceptional precision, repeatability, and reproducibility, ensuring its reliability for robust diagnostic and research applications.
Mycolic acids as chemotaxonomic biomarkers in the Mycobacterium genus
The PCA analysis of the obtained mycolic acid profiles from the reference strains (Fig. 1a) clearly demonstrates a distinct separation of all analyzed species, based on the simultaneous evaluation of 52 mycolic acids. These findings were further validated by an extended PCA analysis (Fig. 1b), which incorporated the MA profiles of 32 reference strains and 299 clinical isolates. Notably, the analysis of clinical isolates highlights the significant biological diversity of MA profiles, reinforcing their value as chemotaxonomic biomarkers within the Mycobacterium genus. Species such as M. xenopi and M. malmoense are characterized by relatively low heterogeneity and highly conserved MA profiles, reflecting their stable evolutionary traits. Conversely, members of the Mycobacterium tuberculosis complex exhibit a mix of high heterogeneity and conserved MA profiles, a pattern distinct from the Mycobacterium avium-intracellulare complex group, which is notable for its elevated heterogeneity and reduced profile conservativeness. Other non-tuberculous mycobacterial species display significant diversity among themselves while clustering according to their chemotaxonomic similarities.
As shown in Fig. 2a-b, the heat map illustrates the distribution of individual mycolic acids across different Mycobacterium groups and strains. Mycolic acid profiles typically consist of MAs from multiple classes present simultaneously, regardless of strain classification. However, an exception is observed with class α2-MAs, which are exclusively found in the MAI group and certain NTM strains. Among these, the highest proportions are detected in M. gordonae, M. fortuitum, and M. smegmatis. A much higher level of conservatism is noted in the relationship between α-alkyl chain lengths. Profiles dominated by molecules with the longest α-alkyl chain (C24) are characteristic of the MTB group, with only a few exceptions (M. xenopi, M. malmoense, and M. simiae). Mycolic acids with a C22 α-alkyl chain length are the most common across strains, while no strain with a predominant C20 α-alkyl chain was observed among the tested reference strains. The identification of pulmonary tuberculosis depends on detecting the distinctive MA profile specific to the MTB group. This profile is characterized by the presence of total mycolic acids ranging from C74 to C88, with a predominance of MAs containing a C24 α-alkyl chain.
Determination of the drug resistance based on mycolic acids profiles
Based on the culture extraction procedure, MA profiles from MTB and NTM strains with varying drug resistance (see Supplementary Table S1 and S2 online) profiles were examined using both the LC-MS/MS targeted method (MRM) and non-targeted methods (Precursor Ion). In the analysis of MTB strains, neither the targeted method (52 MRM pairs) nor the non-targeted methods yielded specific MA profiles that could precisely define the drug resistance profile (data not shown). However, the obtained profiles did allow for the determination of whether a tested strain is drug-resistant, which may hold significant value as supplementary information alongside species identification. This additional insight could facilitate both immediate clinical decision-making and partial personalization of antibiotic therapy. The observed relationship is effectively illustrated by the PCA analysis presented in Fig. 3, where, despite the inclusion of additional drug-sensitive reference strains, drug-resistant M. tuberculosis isolates form a distinct group within the PCA space. Non-targeted analyses also revealed that, in addition to changes in the intensities of certain MTB MAs used for species identification, there were notable variations in the relative intensities of additional MAs with masses above 1200 m/z. These variations were particularly evident in the C22 and C24 chains. These additional mycolic acids differentiate drug-resistant mycobacteria more effectively than those traditionally used for genus identification and could be incorporated into targeted methods specifically designed to identify general drug resistance based on the MA profile. In contrast, for NTM strains, no MA profiles were identified that could differentiate between drug-sensitive and drug-resistant strains or determine the drug resistance profile.
PCA analysis of C24 α-branch chain (precursor ion) mycolic acids for MTB reference strains with drug-resistant strains (A-B) and MTB reference strains with clinical isolates and drug-resistant strains (C-D), including multidrug-resistant (MDR) and extensively drug-resistant (XDR) tuberculosis, specifying resistance to isoniazid (i), rifampicin, streptomycin (s), ethambutol (e), pyrazinamide (p), amikacin (a), kanamycin (k), ciprofloxacin (c), moxifloxacin (m), and ofloxacin (o).
Interference testing and assay selectivity for mycolic acid profiling
To ensure the exclusion of false positives arising from the presence of mycolic acids in bacteria outside the Mycobacterium genus, mycolic acid extraction and FIA-MS/MS analysis were conducted on other mycolic acid-containing bacteria within the suborder Corynebacterinae. These included R. equi, N. asteroides, C. glutamicum, D. maris, G. bronchialis, G. sputi, and T. paurometabola. Remarkably, no false-positive signals were observed for any of these strains, underscoring the high specificity and reliability of the developed assay. This high degree of selectivity highlights the robustness of the method, particularly in differentiating Mycobacterium species from other genera that share similar biochemical characteristics. Such specificity is critical for ensuring the accuracy of diagnostic and research applications, reducing the likelihood of misidentification or erroneous conclusions.
Clinical validation of FIA-MS/MS mycolic acid profiling for the detection of Mycobacterium infections
The utility of mycolic acid profiling by FIA-MS/MS for detecting Mycobacterium infections was evaluated by analyzing clinical samples from patients with mycobacterial infections (n = 36), lower respiratory tract infections not caused by Mycobacterium (n = 235), and healthy volunteers (n = 94). Among patients with mycobacterial infections, a Mycobacterium-specific mycolic acid profile was detected in 33 samples using FIA-MS/MS. Of these profiles, 9 were identified as NTM strains, including M. avium (n = 5), M. chimaera (n = 2), M. malmoense (n = 1), and M. haemophilum (n = 1). The remaining 24 profiles were identified as M. tuberculosis. In three samples from patients with tuberculosis, M. tuberculosis-specific mycolic acids were not detected. Furthermore, no mycolic acids were detected by FIA-MS/MS in any of the samples from patients with lower respiratory tract infections caused by non-mycobacterial bacteria or in samples from healthy volunteers. The analysis of mycolic acid profiles was performed using M-Typer software, which demonstrated a high degree of similarity between the detected MA profiles and those in the reference library. Notably, in all positive samples, the match between the MA profiles and the library exceeded 90%, underscoring the accuracy and reliability of the method.
In summary, based on the analysis of the results obtained for the clinical samples presented in Table 2, the clinical performance parameters of the FIA-MS/MS test for the detection of Mycobacterium infections were calculated. The test demonstrated a specificity of 100%, a sensitivity of 91.6%, a negative predictive value (NPV) of 98.2%, and a positive predictive value (PPV) of 100%.
These results highlight the high reliability of the FIA-MS/MS method, particularly its exceptional ability to exclude false positives due to its perfect specificity. The strong NPV further underscores its utility in confidently ruling out Mycobacterium infections in negative cases, while the PPV confirms its precision in accurately identifying positive cases. Such robust diagnostic performance supports the method’s potential as a valuable tool in clinical settings for the rapid and accurate identification of Mycobacterium infections, ultimately facilitating timely and targeted patient management.
Discussion
Mycolic acids are a unique class of chemical molecules that largely define the structure and physiology of the cell wall of mycobacteria. This fact, combined with their physicochemical properties, such as molecular size, conservative structure and high resistance to environmental conditions, make them excellent biomarkers for the presence of mycobacteria in a variety of biological samples. The development of liquid chromatographic techniques in the 1990s allowed the development of a reference method for the classification of mycobacteria based on the profile of bromophenacyl esters of mycolic acids13. However, this method and its subsequent modifications did not have sufficient analytical sensitivity for use in the detection of mycobacteria directly from test material14. Nowadays, the development of advanced liquid chromatography and/or mass spectrometry techniques, including those combined with ion mobility, allows very detailed analysis of mycolic acid profiles in terms of particle size, structure, conformation and class15,16,17 for chemotaxonomic proposes. Still, the detection and differentiation of Mycobacterium species based on their mycolic acid profiles presents a compelling alternative to conventional culture-based and molecular techniques. Leveraging liquid chromatography coupled with tandem mass spectrometry (LC-MS/MS) enables rapid, specific, and sensitive identification of Mycobacterium species, significantly enhancing diagnostic workflows. This advancement is particularly vital in settings where prompt and accurate identification is critical, such as tuberculosis management.
The diagnostic sensitivity and specificity of the developed FIA-MS/MS method, reported at 92.66% and 100%, underscores its robustness compared to traditional techniques like bacterioscopy, BacTEC culture, and PCR18,19,20. Those parameters positioning it as a reliable tool for routine diagnostic applications. Unlike methods reliant on bacterial growth or genetic markers, FIA-MS/MS capitalizes on the unique structural diversity of mycolic acids, long-chain fatty acids that serve as biomarkers for species differentiation. These lipids provide a stable and direct basis for identification, circumventing limitations like slow growth rates, contamination, or genetic variability associated with culture and molecular methods.
While culture methods and PCR often exhibit lower sensitivity for certain non-tuberculous mycobacteria, the FIA-MS/MS approach has demonstrated high specificity in identifying species such as M. avium and M. chimaera. This capability is particularly advantageous for detecting both high-abundance and low-abundance species, including those that are challenging to identify using traditional approaches. By addressing these gaps, FIA-MS/MS strengthens diagnostic precision, especially in complex clinical cases. For instance, recent studies have shown that FIA-MS/MS can reliably differentiate pathogenic NTMs from environmental contaminants, thus enabling targeted therapeutic interventions and reducing misdiagnoses16.
The adaptability of FIA-MS/MS is evident in its application to diverse clinical samples, including sputum, bronchoaspirates, pleural fluids, and fine-needle aspiration biopsies. The method’s sensitivity and specificity for diagnosing extrapulmonary MTB and NTM infections highlight its suitability for complex and varied diagnostic needs. This adaptability broadens its clinical utility, ensuring accurate identification even in non-traditional sample types. For example, Fatima et al. (2024) demonstrated that coupling advanced chromatographic methods with LC-MS/MS improves the detection of mycolic acids in difficult-to-process specimens, such as cerebrospinal fluid and bone marrow aspirates17. Discrepancies between LC-MS/MS and conventional diagnostic methods, such as bacterioscopy, can often be attributed to the inherent limitations of microscopy in detecting non-tuberculous species. Similarly, the lower sensitivity of BacTEC culture and PCR reflects their dependency on bacterial growth and genetic markers, which may not always be sufficiently expressed or amplified. LC-MS/MS circumvents these issues by directly targeting the intrinsic lipid composition of bacteria, making it a more reliable diagnostic tool. Moreover, the incorporation of cyclic ion mobility-mass spectrometry has further enhanced the specificity of FIA-MS/MS in distinguishing between structurally similar mycolic acid isomers16.
The rapid identification capabilities of LC-MS/MS have far-reaching implications for public health. In tuberculosis management, faster diagnosis facilitates earlier and more targeted treatment interventions, potentially reducing transmission and improving patient outcomes. Furthermore, the method’s ability to differentiate NTMs is critical for personalized medicine, as these infections often require distinct therapeutic strategies. Liu et al. (2023) reported that ion mobility mass spectrometry could be used to study lipid variations between drug-resistant and sensitive strains of M. tuberculosis, offering insights into mechanisms of resistance and aiding in the development of tailored treatments21. Our findings show that the FIA-MS/MS method, despite not yielding profiles precise enough to define the complete drug resistance spectrum, can differentiate drug-resistant M. tuberculosis strains from sensitive ones. This capability, demonstrated in PCA analysis, underscores the method’s utility as a complementary diagnostic tool aiding species identification and resistance profiling. The detection of distinct mycolic acid profiles, including variations in C22 and C24 chains and additional mycolic acids with masses above 1200 m/z, suggests these molecules could serve as markers for resistance detection. In the context of drug susceptibility, this study highlights a critical application of mycolic acid profiling in identifying general resistance patterns in M. tuberculosis strains. While the method cannot yet pinpoint specific resistance mechanisms or profiles for individual drugs, its ability to broadly categorize strains as drug-resistant or susceptible has significant implications for clinical decision-making. This insight is particularly valuable in high-burden or resource-limited settings, where rapid and reliable identification of resistance is critical for initiating effective treatment. Early identification of drug resistance can reduce delays in tailoring therapy, limiting disease progression and minimizing transmission risk. Furthermore, our findings provide evidence that non-targeted analyses can uncover additional mycolic acids associated with resistance, particularly in high-molecular-weight fractions. These markers could form the basis for developing new diagnostic assays focused on resistance profiling, complementing existing molecular methods. Future work could refine these markers and validate their use across diverse M. tuberculosis strains to improve the specificity and sensitivity of LC-MS/MS in resistance detection. For non-tuberculous mycobacteria our results demonstrate the limitations of mycolic acid profiling in differentiating drug-sensitive and drug-resistant strains. This reflects the inherent diversity and metabolic complexity within non-tuberculous mycobacteria species which pose challenges for both molecular and lipid-based diagnostic methods. However, the specificity of FIA-MS/MS for non-tuberculous mycobacteria identification highlights its potential utility in clinical diagnostics.
From a research perspective, profiling mycolic acids provides new opportunities for studying their structural biology and role in pathogenesis. Insights gained from this lipid-focused analysis could uncover biomarkers for virulence, drug resistance, or environmental persistence, contributing to the development of novel therapeutic or diagnostic targets. For instance, Kumar et al. (2024) explored the use of thin-layer chromatography as a complementary technique to enhance mycolic acid detection in environmental samples, revealing potential applications in epidemiological studies and environmental monitoring of mycobacterial pathogens22. Despite its high diagnostic sensitivity, challenges remain in enhancing LC-MS/MS’s capabilities for detecting low-abundance mycobacteria in complex biological matrices. Optimizing sample preparation protocols, such as lipid extraction and enrichment methods, could further improve sensitivity. Additionally, validating the approach across larger, more diverse cohorts would strengthen its clinical applicability. Efforts to improve cost-effectiveness and feasibility in resource-limited settings are critical for the widespread adoption of LC-MS/MS-based diagnostics. Simplified workflows and portable instrumentation, such as miniaturized mass spectrometers, could facilitate implementation in these settings, where rapid and accurate diagnostics are most urgently needed15.
LC-MS/MS-based profiling of mycolic acids is a transformative tool for identifying and differentiating Mycobacterium species. Its high sensitivity, coupled with the ability to profile structural lipid diversity, positions it as a rapid and scalable diagnostic alternative to conventional methods. Future efforts should prioritize enhancing the method’s sensitivity for low-abundance mycobacteria and expanding its applications in environmental and clinical microbiology. Undoubtedly, LC-MS/MS has the potential to revolutionize diagnostic workflows, improve patient outcomes, and broaden research opportunities in microbial pathogenesis.
Materials and methods
Strains and culture conditions
Thirty-two reference strains of Mycobacterium were obtained from the ATCC, NCTC, and DSMZ collections (Table 3). Additionally, 299 clinical Mycobacterium isolates, primarily recovered from respiratory specimens (e.g., sputum and bronchoaspirates), were cultured under standard laboratory conditions (Table 3). These clinical isolates were collected at the Fryda Laboratory of the Regional Specialized Hospital of Tuberculosis, Lung Diseases, and Rehabilitation in Lodz, Poland and the Institute of Tuberculosis and Lung Diseases in Warsaw, Poland. The mycobacterial cultures were grown in 7H9 Middlebrook broth (Difco Laboratories Ltd., West Molesey, UK), supplemented with 0.05% Tween 80 (Sigma), at 37 °C with constant rotation (125 rpm) until reaching the mid-logarithmic phase. For colony-forming unit (CFU) determination, serial dilutions were plated onto Middlebrook 7H10 agar supplemented with OADC and incubated at 37 °C for up to six weeks. Furthermore, bacterial strains from the Corynebacterinae order—including Corynebacterium glutamicum PCM 1945, Rhodococcus equi PCM 559, Nocardia asteroides PCM 2138, Dietzia maris PCM 2292, Gordonia bronchialis PCM 2167, Gordonia sputi PCM 2144, and Tsukamurella paurometabola PCM 2453—were purchased from the Polish Collection of Microorganisms (PCM) and cultivated as liquid cultures under specific growth conditions. Careful monitoring of these cultures ensured optimal growth and consistency, which were critical for reproducibility in downstream analyses.
Clinical materials
Clinical samples were collected from 271 patients at the Regional Specialized Hospital of Tuberculosis, Lung Diseases, and Rehabilitation in Lodz, Poland. Among these, 36 patients were diagnosed with lung infections caused by mycobacteria, while 235 had infections caused by other bacteria (Table 4). Additionally, samples from 94 healthy volunteers were included as controls to provide a baseline for comparison. The study was conducted with the approval of the local Bioethics Committee (RNN/785/13/KB) ensuring compliance with ethical standards for the collection and analysis of human samples. Informed consent was obtained from all subjects and/or their legal guardian(s). All experiments were performed in accordance with relevant guidelines and regulations, specifically the recommendations of the Polish Society of Lung Diseases and the National Council of Laboratory Diagnosticians from 2014, as well as the 2018 standards of the Clinical and Laboratory Standards Institute (CLSI), M48 2nd Edition and M24 3rd Edition. The presence of Mycobacterium in clinical samples was assessed using a combination of advanced analytical techniques and standard microbiological diagnostic methods. Specifically, flow-injection analysis tandem mass spectrometry (FIA-MS/MS) was employed alongside conventional diagnostic approaches, which included bacterioscopy, culture in BACTEC liquid medium (BD Medical, USA), and the MTB-RIF genetic testing method (Cepheid, USA). All diagnostic results were independently verified to ensure accuracy and reliability. Additionally, the Hain GenoType Mycobacterium CM/AS molecular assay (Hain Lifescience, Germany) was utilized to differentiate between M. tuberculosis complex (MTB) and non-tuberculous mycobacteria (NTM). Samples from healthy volunteers underwent identical analyses to confirm the absence of Mycobacterium and to validate the specificity of the applied diagnostic methods. A summary of the number of volunteers in the study groups, alongside the types of clinical materials analyzed, is provided in Table 4.
Sample Preparation
Mycolic acid extraction was performed using the M-Typer Reagent Kit (DiMedical, Lodz, Poland) and comprised three main steps: alkaline hydrolysis at elevated temperature, neutralization, and liquid-liquid extraction. Briefly, a suspension of Mycobacterium cells (10⁷ cells/ml) or sputum samples was transferred into a conical glass tube and centrifuged at 3,500 rpm for 10 min at 4 °C. Prior to extraction, sputum samples underwent an additional pretreatment step to liquefy the material using an N-acetylcysteine solution. Only the resulting rinsed pellet, potentially containing Mycobacterium, cells was processed in the subsequent mycolic acid extraction steps. Alkaline hydrolysis was performed in a water bath at 90 °C for 60 min. After cooling, neutralization was carried out using a hydrochloric acid solution (18.5% HCl) at a 1:1 volume ratio, resulting in the precipitation of an insoluble salt. The neutralized mixture was then subjected to liquid-liquid extraction at a 2:1 volume ratio, conducted on a rotator-type shaker for 30 min. The organic phase, which settled at the bottom, was carefully collected into a chromatography vial, sealed with a teflon-coated septum cap, and either stored at -80 °C for future use or directly subjected to FIA-MS/MS analysis.
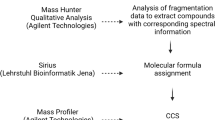
FIA-MS/MS analysis
The analysis of mycolic acid profiles by flow injection tandem mass spectrometry (FIA-MS/MS) was performed using a QTRAP 6500 + tandem mass spectrometer (Sciex, Toronto, Canada) coupled with an ExionLC AD liquid chromatograph (Sciex, Toronto, Canada). During the study, full compatibility and interchangeability of the M-Typer technology (DiMedical, Lodz, Poland) were demonstrated on a Triple Quad LCMS-8060 system coupled to an LC-20AD chromatograph (Shimadzu, Kyoto, Japan).
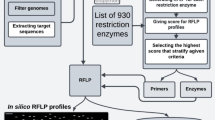
The analysis was carried out in negative electrospray ionization (ESI) mode, with the unique signals of mycolic acids (MAs) detected and monitored using the multiple reaction monitoring (MRM) mode. The MRM analysis included monitoring 52 specific transitions, each corresponding to a distinct mycolic acid. These transitions were selected to reflect both the molecular weight of the mycolic acids (Q1 mass) and the length of the α-alkyl chain (Q3 mass). Advanced scheduled MRM methodologies, incorporating MRM grouping and triggering thresholds, ensured sufficient dwell time (> 12 ms) per transition. The panel of 52 MRM transitions covered a broad range of mycolic acid masses, from 887 to 1295 Da, and accounted for variations in α-alkyl chain lengths of C20, C22, and C24. Additionally, the analysis included all major classes of mycolic acids: α-mycolic acids, methoxy-mycolic acids, and keto-mycolic acids (Table 5). As an alternative to targeted MRM analysis, untargeted mass spectrometry methods were employed to explore potential drug resistance profiles. Precursor ion scans detected ions within the range of 850 to 1350 m/z, with fragmentation patterns indicative of α-alkyl chain lengths of C20 (339 m/z), C22 (367 m/z), and C24 (395 m/z), respectively. These scans were conducted in negative ionization mode at a scanning speed of 1000 Da/s, with a defined declustering potential of -150 eV and a collision energy of -76 eV.
FIA-MS/MS analysis was performed using reagents (mobile phases and autosampler wash solutions) provided in the M-Typer Reagent Kit (DiMedical, Lodz, Poland). A 50 µL sample of the mycolic acid extract was directly injected into the flow of the ESI-MS/MS system. The gradient flow and mobile phase composition were optimized to achieve the desired “hump-like” shape of the MRM signals while minimizing carryover effects between sequential analyses (Fig. 4). Each analysis was completed within 1 min per sample, with a 30-second interval between consecutive injections.
Data analysis
The profiles of mycolic acids are represented as the percentage abundance of each mycolic acid relative to the most intense signal among all 52 analyzed. To generate the mycolic acid profile, the extracted ion chromatograms (XICs) for each “hump-like” MA signal obtained through FIA-MS/MS were integrated using M-Typer software. For each XIC, the software calculated the average intensity values that exceeded half the height (between Start – Stop) of the “hump-like” signal after subtracting the baseline noise (Fig. 4). The resulting mean values for all MAs were then compared and normalized against the most intense MA signal from the entire dataset.
The resulting mycolic acid profiles can either be subjected to external statistical analysis or directly analyzed within the M-Typer software framework. To facilitate clinical result interpretation, the M-Typer software compares the generated MA profiles with those stored in its library. This library contains reference data for the mycolic acid profiles characteristic of 331 Mycobacterium strains, including both reference strains and clinical isolates, representing 31 distinct species within the Mycobacterium genus. Each strain’s data was tested in triplicate and at varying bacterial culture densities (spanning up to four orders of magnitude), resulting in a comprehensive library of more than 4.000 individual mycolic acid profiles. The degree of similarity between an unknown profile and the library profiles is calculated, and a similarity score is assigned to each sample.
Principal component analysis (PCA) was employed to evaluate the discriminatory capacity of the normalized mycolic acid profiles, aiming to distinguish between various strains and groups within the Mycobacterium genus. PCA analysis was performed entirely using MarkerView 1.3.1 software (AB Sciex) to explore the potential for group- and species-specific differentiation. Additionally, within the Mycobacterium tuberculosis complex, PCA was applied to assess the feasibility of using mycolic acid profiles for drug susceptibility evaluation.
Data availability
Data can be available after reasonable request to the corresponding author (konrad.kowalski@dimedical.pl). Some of the research protocols presented in the publication are additionally protected by intellectual property rights (EP3978617).
References
Chai, Q., Zhang, Y. & Liu, C. H. Mycobacterium tuberculosis: an adaptable pathogen associated with multiple human diseases. Front. Cell. Infect. Microbiol. 15, 8:158. https://doi.org/10.3389/fcimb.2018.00158 (2018).
Rastogi, N., Legrand, E. & Sola, C. The mycobacteria: an introduction to nomenclature and pathogenesis. Rev. Sci. Tech. 20, 21–54. https://doi.org/10.20506/rst.20.1.1265 (2001).
Brennan, P. J. Structure, function, and biogenesis of the cell wall of Mycobacterium tuberculosis. Tuberculosis (Edinb). 83, 91–97 (2003). 10.1016/s1472-9792(02)00089 – 6.
O’Connor, J. A., O’Reilly, B., Corcoran, G. D., O’Mahony, J. & Lucey, B. Mycobacterium diagnostics: from the primitive to the promising. Br. J. Biomed. Sci. 72, 32–41. https://doi.org/10.1080/09674845.2015.11666793 (2015).
Al-Zamel, F. A. Detection and diagnosis of Mycobacterium tuberculosis. Expert Rev. Anti Infect. Ther. 7, 1099–1108. https://doi.org/10.1586/eri.09.92 (2009).
Liu, Y., Kaffah, N., Pandor, S., Sartain, M. J. & Larrouy-Maumus, G. Ion mobility mass spectrometry for the study of mycobacterial mycolic acids. Sci. Rep. 13, 10390. https://doi.org/10.1038/s41598-023-37641-9 (2023).
Marrakchi, H., Lanéelle, M. A. & Daffé, M. Mycolic acids: structures, biosynthesis, and beyond. Chem. Biol. 16, 67–85. https://doi.org/10.1016/j.chembiol.2013.11.011 (2014).
Nataraj, V. et al. Mycolic acids: Deciphering and targeting the Achilles’ heel of the tubercle Bacillus. Mol. Microbiol. 98, 7–16. https://doi.org/10.1111/mmi.13101 (2015).
Larsson, L. & Mårdh, P. A. Gas chromatographic characterization of mycobacteria: analysis of fatty acids and trifluoroacetylated whole-cell methanolysates. J. Clin. Microbiol. 3, 81–85. https://doi.org/10.1128/jcm.3.2.81-85.1976 (1976).
Leite, C. Q., de Souza, C. W. & Leite, S. R. Identification of mycobacteria by thin layer chromatographic analysis of mycolic acids and conventional biochemical method: four years of experience. Mem. Inst. Oswaldo Cruz. 93, 801–805. https://doi.org/10.1590/s0074-02761998000600019 (1998).
Maliwan, N., Reid, R. W., Pliska, S. R., Bird, T. J. & Zvetina, J. R. Identifying Mycobacterium tuberculosis cultures by gas-liquid chromatography and a computer-aided pattern recognition model. J. Clin. Microbiol. 26, 182–187. https://doi.org/10.1128/jcm.26.2.182-187.1988 (1988).
Szewczyk, R., Kowalski, K., Janiszewska-Drobinska, B. & Druszczyńska, M. Rapid method for Mycobacterium tuberculosis identification using electrospray ionization tandem mass spectrometry analysis of mycolic acids. Diagn. Microbiol. Infect. Dis. 76, 298–305. https://doi.org/10.1016/j.diagmicrobio.2013.03.025 (2013).
Butler, W. R. & Kilburn, J. O. High-performance liquid-chromatography patterns of mycolic acids as criteria for identification of Mycobacterium Chelonae, Mycobacterium fortuitum, and Mycobacterium smegmatis. J. Clin. Microbiol. 28, 2094–2098 (1990).
Butler, W. R. & Guthertz, L. S. Mycolic acid analysis by high-performance liquid chromatography for identification of Mycobacterium species. Clin. Microbiol. Rev. 14, 704–726 (2001).
Frankfater, C., Fujiwara, H., Williams, S. J., Minnaard, A. & Hsu, F. F. Characterization of Mycobacterium tuberculosis mycolic acids by Multiple-Stage linear Ion-Trap mass spectrometry. J. Am. Soc. Mass. Spectrom. 33, 149–159. https://doi.org/10.1021/jasms.1c00310 (2022).
de Prieto, L. H., Cole, H., Forbes, L. M., Palmer, S., Schwartz-Narbonne, R. & M. & Separation of mycolic acid isomers by Cyclic ion mobility-mass spectrometry. Rapid Commun. Mass. Spectrom. 38, e9917. https://doi.org/10.1002/rcm.9917 (2024).
Fatima, Z., Chugh, M., Nigam, G. & Hameed, S. Quantification of mycolic acids in different mycobacterial species by standard addition method through liquid chromatography mass spectrometry. J. Chromatogr. B. 15, 124297. https://doi.org/10.1016/j.jchromb.2024.124297 (2024).
Noordhoek, G. T. et al. Sensitivity and specificity of PCR for detection of Mycobacterium tuberculosis: a blind comparison study among seven laboratories. J. Clin. Microbiol. 32, 277–284. https://doi.org/10.1128/jcm.32.2.277-284.1994 (1994).
Lee et al. Rapid, sensitive, and specific detection of Mycobacterium tuberculosis complex by real-time PCR on paraffin-embedded human tissues. J. Mol. Diagn. 13, 390–394. https://doi.org/10.1016/j.jmoldx.2011.02.004 (2011).
Singh, A. & Kashyap, V. K. Specific and rapid detection of Mycobacterium tuberculosis complex in clinical samples by polymerase chain reaction. Interdiscip Perspect. Infect. Dis. 9, 654694. https://doi.org/10.1155/2012/654694 (2012).
Liu, Y., Kaffah, N., Pandor, S., Sartain, M. J. & Larrouy-Maumus, G. Ion mobility mass spectrometry for the study of mycobacterial mycolic acids. Sci. Rep. 27, 13. https://doi.org/10.1038/s41598-023-37641-9 (2023).
Kumar, K., Giribhattanavar, P., Sagar, B. K. C. & Patil, S. A. Exploring variations in lipids among Drug-resistant and sensitive Mycobacterium tuberculosis by thin layer chromatography and mass spectrometry. Mycobact. Dis. 14 https://doi.org/10.35248/2329-9509.24.14.494 (2024).
Acknowledgements
The research was supported by a grant from the European Funds within Regional Programme subtask Smart Growth (POIR.01.01.01-00-0798/1) titled „Research and development works in the field of developing an innovative method of diagnosing tuberculosis and other mycobacteriosis”. The funding sources had no role in the study process, including the design, sample collection, analysis, or interpretation of the results. We would like to extend our profound gratitude to the external researchers and clinicians, with particular recognition to Professor Ewa Augustynowicz-Kopec from the Institute of Tuberculosis and Lung Diseases in Warsaw, for their invaluable contributions to the successful implementation of the project.
Author information
Authors and Affiliations
Contributions
Conceptualization: R.S, K.K., M.D., K.M; Data curation: K.M, R.S; Formal analysis: K.K., K.M, M.D, R.S; Funding acquisition: K.M; Investigation: R.S, K.K, M.D, K.M Methodology: R.S, K.K; Supervision: K.M; Validation: R.S, K.K; Visualization: K.K, B.S; Writing original draft: K.K, K.M, M.D, R.S, B.S. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors, Bartłomiej Szulc and Karol Majewski, declare a potential conflict of interest due to their involvement with DiMedical, a company focused on implementing innovative methods for tuberculosis diagnostics including M-Typer technology. This disclosure is made in the interest of transparency and does not affect the integrity of the research findings presented. All the remaining authors declare no conflict of interest.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Rafał, S., Magdalena, D., Karol, M. et al. Detection and accurate identification of Mycobacterium species by flow injection tandem mass spectrometry (FIA-MS/MS) analysis of mycolic acids. Sci Rep 15, 13118 (2025). https://doi.org/10.1038/s41598-025-96867-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-96867-x