Abstract
As a predictor of mortality, accidental disability, depressive symptoms, and other adverse outcomes in the older population, social frailty has yet to receive attention among older adults living with HIV/AIDS. Therefore, this study, using Least Absolute Shrinkage and Selection Operator (LASSO) and Random Forest (RF), aims to analyze the current status and risk factors of social frailty in older adults living with HIV/AIDS and provides a basis for its prevention and reversal. From January to December 2024, a total of 335 older adults living with HIV/AIDS (≥ 50 years old) receiving outpatient treatment at a tertiary hospital in Zunyi, Guizhou, China, were selected using convenience sampling. Data were collected through a general information questionnaire (demographic and clinical disease), the HALFT scale for social frailty, the Geriatric Depression Scale-15 (GDS-15), the Barthel Index (BI), the Montreal Cognitive Assessment (MoCA), the Pittsburgh Sleep Quality Index (PSQI), and the Social Support Rating Scale (SSRS). Data processing and analysis were conducted using SPSS 29.0, Python 3.11, and R 4.3.1. Among the 335 older adults living with HIV/AIDS, 105 cases (31.34%) exhibited social frailty. LASSO regression was used for validation, and based on the lambda.min value (λ = 0.0127), 12 relevant variables with non-zero coefficients were selected from 26 variables. These 12 variables were then incorporated into the RF model, which identified that older adults living with HIV/AIDS with reduced activities of daily living (ADL), lack of exercise, cognitive impairment, depression, lower social support, older age, sleep disorders, low CD4+ lymphocyte counts, low per capita household income, complications, smoking history, and those enrolled in China’s free antiretroviral therapy (ART) program faced a higher risk of social frailty. The top five risk factors in order of importance were ADL, exercise, cognitive impairment, depression, and social support. The incidence of social frailty is relatively high among older adults living with HIV/AIDS. The risk factors include ADL, exercise, cognitive impairment, depression, social support, age, sleep disorders, CD4+ lymphocyte count, per capita household income, complications, smoking history, and participation in China’s free ART program. This highlights the importance of healthcare institutions and community healthcare workers addressing social frailty in older adults living with HIV/AIDS. Early identification of the risk factors can help prevent or reverse the onset and progression of social frailty, improving prognosis and quality of life. It also provides a theoretical foundation for developing targeted intervention measures.
Similar content being viewed by others
Introduction
As one of the major geriatric syndromes, frailty is a multidimensional condition that includes physical, cognitive, psychological, and social components1. Social frailty, a key aspect of frailty, has an incidence rate of 15–45.7% among the older population in China2. It refers to an individual’s prolonged lack of one or more essential social resources that support health, primarily including deficiencies in social behaviors, social activities, and self-management3. Research has shown that social frailty increases the risk of sarcopenia, disability, and other adverse outcomes in older patients and is significantly associated with all-cause mortality4. Thus, addressing social frailty in the older population is crucial in preventing negative outcomes and promoting healthy aging.
As one of the global public health issues, AIDS has been transformed from a fatal disease into a controllable and treatable chronic condition with the emergence of antiretroviral therapy (ART), which significantly extends the life expectancy of patients5. According to the Joint United Nations Programme on HIV/AIDS (UNAIDS), it is estimated that by 2023, approximately 39 million people worldwide will be infected with HIV6, and the number of HIV/AIDS patients aged ≥ 50 will increase from 5.4 million in 2015 to 8.2 million in 2022. In China, older adults living with HIV/AIDS (≥ 50 years old) account for 36.8% of the total HIV/AIDS population7. WHO defines individuals aged ≥ 60 in developing countries as the “older” population8. However, in AIDS research, patients experience accelerated immune aging, thus leading to geriatric syndromes (such as frailty and multimorbidity) approximately a decade earlier than the general population9. In order to differentiate them from the sexually active population aged 15–49, individuals aged ≥ 50 years with HIV/AIDS are typically classified as older adults living with HIV/AIDS10,11,12. Due to stigma, prejudice, negative emotions, multiple complications, and the economic burden of long-term treatment, older adults living with HIV/AIDS face increased depletion of psychological and social resources. This leads to reduced social participation and heightened feelings of loneliness, thereby further exacerbating social issues11,12. Studies have shown that social frailty in HIV/AIDS patients represents a significant proportion of frailty, and the most prominent issues are the weakening of social relationships and reduced social support in terms of social frailty13. Therefore, under an aging population, social frailty among older adults living with HIV/AIDS is becoming an increasingly critical issue. Existing research predominantly focuses on the physiological frailty in older adults living with HIV/AIDS, while little attention is given to social frailty in this group14. Early identification of social frailty in older adults living with HIV/AIDS and an exploration of related risk factors are urgent in clinical practices. This is essential for clinical staff and community healthcare institutions to formulate targeted intervention measures and prevent adverse clinical outcomes.
Research has shown that social frailty in the older population is influenced by multiple factors, including individual characteristics and external environments. For instance, a study based on older individuals in Chinese communities2 found that marital status and self-reported health were significantly related to social frailty. A meta-analysis7 highlighted that depression, chronic diseases, and sleep issues are risk factors for social frailty in community-dwelling older adults. In older adults with heart failure, social frailty was found to be associated with age, education, marital status, monthly household income per capita, living arrangements, exercise, disease duration, cognitive impairment, and activities of daily living (ADL)15. However, whether these factors affect social frailty in older adults living with HIV/AIDS requires further investigation. The Health Ecology Model (HEM) posits that health is the outcome of the interaction of individual factors and external environments, emphasizing the multi-level impacts of the environment on individuals and the complexity and diversity of influencing factors16. Due to the complexity and diversity of these factors, multicollinearity may arise. The Least Absolute Shrinkage and Selection Operator (LASSO) regression helps control model complexity by introducing a penalty that shrinks the coefficients of insignificant or minimally significant variables to zero, thus selecting the most relevant variables, as well as avoiding overfitting and multicollinearity. Unlike traditional regression models, LASSO allows for the simultaneous processing of all independent variables, significantly enhancing the model’s stability17. Random Forest (RF) helps identify key variables by providing more accurate and efficient comparisons of variable importance and analyzing complex nonlinear relationships18. The “black box” nature of machine learning means that it is difficult to understand how sample features influence the final results, but Shapley Additive Explanations (SHAP) provide the advantage of explaining individual prediction outcomes19. Therefore, based on the five aspects of HEM (personal traits, behavioral characteristics, interpersonal networks, living and working conditions, and policy environment), this study uses LASSO regression and the SHAP algorithm in RF to identify the risk factors of social frailty in older adults living with HIV/AIDSand provides a basis for the development of targeted intervention strategies.
Methods
Research design and participants
From January to December 2024, convenience sampling was used to select 335 older adults living with HIV/AIDS who visited the outpatient department of a tertiary Grade A hospital in Zunyi, Guizhou Province, China, as study participants.
Inclusion criteria:
(1) Meeting the diagnostic criteria outlined in the China HIV/AIDS Diagnosis and Treatment Guidelines (2021 Edition)20;
(2) Aged ≥ 50 years9;
(3) Able to communicate normally and be willing to participate in the study.
Exclusion criteria:
(1) Patients with coexisting mental disorders or severe systemic diseases;
(2) Patients with sensory impairments (e.g., visual or auditory) who are unable to provide valid information.
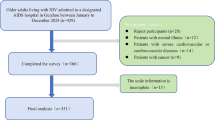
Sample size calculation: The event per variable (EPV)21 was used for sample size calculation. It is generally recommended to have at least 10 observations per predictor variable to achieve good prediction performance. In this study, 26 predictor variables were included. Considering a 20% rate of invalid questionnaires, the sample size should be at least 312 participants. Ultimately, 335 participants were included in the study. The selection of study participants is illustrated in Fig. 1. This study was reviewed and approved by the Ethics Committee of the Zunyi Medical University Affiliated Hospital (Ethics No: KLLY-2023-714). All participants provided informed consent, and the clinical investigation was conducted in accordance with the principles of the Declaration of Helsinki.
Variables
According to HEM16, independent variables were selected from five dimensions: personal traits, psychological behaviors, interpersonal networks, work and living conditions, and policy environment (the relationship between independent variables and HEM is shown in Fig. 2). The detailed content and value assignment of the independent variables are listed in Table 1. Some independent variables are defined as follows. (1) Smoking history: ever smoked or currently smoking; (2) Alcohol history: Alcohol consumption in the past year; (3) BMI: Weight (kg) / Height (m²). Underweight (< 18.5 kg/m²), Normal (18.5–25.0 kg/m²), Overweight or higher (≥ 25.0 kg/m²); (4) Exercise: Never (0), Sometimes (1–3 times/week), Frequently (> 3 times/week).
Measurement
Questionnaire of general information
Based on a literature review and consultations with experts, the general information questionnaire is designed to include demographic data and information on clinical diseases. Demographic data includes: gender, age, education, ethnicity, marital status, per capita monthly household income, smoking history, alcohol history, and exercise. The information of clinical diseases includes: time of HIV diagnosed, complications, ART payment, and CD4+ T lymphocyte count.
Social frailty
The Help, Participation, Loneliness, Financial, Talk (HALFT) scale, developed by Ma et al. in 2018 based on the Chinese context22, was used to assess social frailty in older adults living with HIV/AIDS. The scale consists of five items: (1) Help: Were you able to assist friends or family in the past year? (2) Participation: Did you engage in social or recreational activities in the past year? (3) Loneliness: Have you felt lonely in the past week? (4) Financial: Has your income in the past year been sufficient to sustain you for the entire year? (5) Talk: Do you have someone to talk to every day? Each item is scored based on a positive/negative response, with 0 or 1 point assigned. The total score ranges from 0 to 5, where a score of 0 indicates no social frailty, 1–2 points indicates the early stages of social frailty, and ≥ 3 points indicates social frailty. This scale has been widely applied in both community and clinical settings in China. After validation in the community-dwelling older population in China, Cronbach’s α was 0.602. In the older population in China, the test-retest Cronbach’s α was 0.723.
Depression
The Geriatric Depression Scale-15 (GDS-15)25, developed by Yesavage et al. in 198223, was used to assess depression in older adults living with HIV/AIDS. This scale is a specific tool for screening depression in older adults and was revised in 198626. It consists of 15 items, with items 1, 5, 7, 11, and 13 scored as 1 point for a “no” response, and the remaining items scored as 1 point for a “yes” response. The total score ranges from 0 to 15, and a score of ≥ 8 indicates the presence of depression. The scale has been validated in the older Chinese population, with a Cronbach’s α of 0.79327.
Cognitive impairment
Cognitive function in older adults living with HIV/AIDS was assessed using the Beijing version of the Montreal Cognitive Assessment (MoCA), developed by Yu et al. in 201228. The assessment includes seven dimensions: visuospatial and executive function, naming, attention, language, abstraction, delayed recall, and orientation, with a total score of 30 points. For individuals with ≤ 12 years of education, 1 point is added to the total score for correction. A score of < 26 is considered indicative of cognitive impairment. After validation in the Chinese older population, Cronbach’s α was 0.830. The scale has been widely used in the HIV-infected population29.
Sleep quality
The Pittsburgh Sleep Quality Index (PSQI), developed by Buysse et al. in 198930, was used to assess the sleep quality of older adults living with HIV/AIDS over the past month. It was adapted into Chinese by Liu et al.31. The scale consists of seven dimensions with 19 items and five scores rated by cohabitants (these are not included in the total score). The scale uses a Likert 4-point scoring system, with a total score range of 0 to 21 points. A PSQI score > 7 indicates the presence of sleep disorders. The Cronbach’s α for the scale was 0.83, with a test-retest Cronbach’s α of 0.85. Its sensitivity was 89.6%, and its specificity was 86.5%. After validation in the Chinese population, Cronbach’s α was 0.84231, demonstrating good reliability and validity.
ADL
The Chinese version of the Barthel Index (BI) was used to assess the ADL of older adults living with HIV/AIDS. The BI, developed by Mahoney et al. in 196532, was translated into Chinese by Hou et al.33. It includes 10 items: feeding, grooming, bathing, dressing, bladder control, bowel control, toilet use, mobility (on level surfaces), stair climbing, and transfers (bed to chair and back). The total score ranges from 0 to 100, with higher scores indicating better ADL ability. The scale has shown excellent reliability in the Chinese population, with a Cronbach’s α of 0.916.
Social support
The social support rating scale (SSRS), developed by Xiao34, was used to assess the level of social support among older adults living with HIV/AIDS. This scale consists of three dimensions and a total of 10 items: objective support (3 items), subjective support (4 items), and support utilization (3 items). The total score ranges from 12 to 66, with scores of 0–22 indicating low social support, 23–44 indicating moderate social support, and 45–66 indicating satisfactory social support. The Cronbach’s α for the scale items range from 0.890 to 0.940, demonstrating good reliability and validity. Its effectiveness has been confirmed in older adults living with HIV/AIDS in China35.
Data collection
To ensure the quality of the questionnaire, investigators received professional training. After informed consent was obtained from the participants, the questionnaires were distributed for the patients to complete, avoiding the use of suggestive language. For patients who were illiterate or unable to fill out the forms, the investigator read each survey item aloud to participants and recorded their responses accordingly. A total of 350 questionnaires were distributed, and those with logical errors or incomplete responses were excluded. Ultimately, 335 valid questionnaires were collected, resulting in a valid response rate of 95.7%.
Statistical analysis
Data processing and analysis were conducted using SPSS 29.0 (Version 29.0; IBM Corp., Armonk, NY, 2022), Python 3.11 (Version 3.11; Python Software Foundation, Wilmington, DE, 2022), and R 4.3.1 (Version 4.3.1; R Core Team, 2023). Qualitative data were presented as frequencies and percentages, with intergroup comparisons performed using the χ² test. Quantitative data were expressed as medians and interquartile ranges [M(P25, P75)], with intergroup comparisons conducted using the rank-sum test. LASSO combined with RF was employed to identify factors influencing social frailty. LASSO was implemented using the “glmnet” package in R, with 10-fold cross-validation to mitigate model overfitting and multicollinearity. Based on the regression coefficients at lambda.min, variables with non-zero coefficients were selected from an initial set of 26 variables. The selected variables were then incorporated into the RF model constructed using Python 3.11. Feature importance analysis was conducted to assess the contribution of each variable, and SHAP dependence plots were generated based on SHAP values to further examine the relationships between features and their SHAP values. A P-value of < 0.05 was considered statistically significant.
Results
General information about the surveyed subjects
This study included 335 older adults living with HIV/AIDS, with ages ranging from 50 to 89 (65.69 ± 9.02) years. Other general information is presented in Table 2.
Univariate analysis of social frailty in older adults living with HIV/AIDS
Among the 335 older adults living with HIV/AIDS, 105 (31.34%) experienced social frailty. The univariate analysis based on the HEM revealed that the following factors had statistically significant differences in social frailty among older adults living with HIV/AIDS (P < 0.05): Personal traits: age, complications, BMI, CD4+ lymphocyte count, HIV viral load, TC, LDL-C; Interpersonal network: marital status and social support; Behavioral characteristics: depression, sleep disorders, cognitive impairment, exercise, smoking history, alcohol history, and ADL; Living and working conditions: education and per capita monthly household income; Policy environment: ART payment. These results are shown in Table 2.
Variable selection using LASSO
To identify the most relevant variables associated with social frailty in older adults living with HIV/AIDS, LASSO17 was used for selection, and 26 variables were analyzed, with λ and binomial deviance calculated from the test data to evaluate the predictive performance of the fitted model. In Fig. 3(a), the red dot represents the target variable corresponding to the λ value, and the two dashed lines represent two specific λ values: the former one minimizes binomial deviance, while the latter one indicates the maximum λ value within one standard error of the minimum binomial deviance. In Fig. 3(b), each color represents a different variable. As the regularization parameter λ increases, the number of independent variables in the model gradually decreases. After ten-fold cross-validation, lambda.min (λ = 0.0127) and lambda.1se (λ = 0.035) were identified as the two parameters. Based on the regression coefficients at lambda.min, 12 variables with non-zero coefficients were selected from the 26 variables. These variables include age, per capita monthly household income, exercise, smoking history, complications, ART payment, CD4+ T lymphocyte count, depression, sleep disorders, cognitive impairment, ADL, and social support.
Variable selection using RF
Importance ranking
The 12 variables selected by LASSO were incorporated into the RF model, with the occurrence of social frailty as the dependent variable. By calculating the SHAP values of each variable (Fig. 4b), the importance ranking shown in Fig. 4(a) was derived. The variables, ranked by their importance, are ADL, depression, cognitive impairment, exercise, social support, per capita household monthly income, sleep disorders, age, complications, CD4+ T lymphocyte count, smoking history, and ART payment.
SHAP dependence plot of social frailty risk in older adults living with HIV/AIDS
The occurrence of social frailty was set as the dependent variable, and the value assignment of independent variables was detailed in Table 1. The SHAP dependence plot shows that older adults living with HIV/AIDS with lower ADL, lack of exercise habits, cognitive impairment, depression, inadequate social support, older age, sleep disorders, low CD4+ T lymphocyte count, insufficient per capita family monthly income, complications, smoking, and participation in the free ART program (dual or triple therapy) have a higher risk of experiencing social frailty. The SHAP dependence plots for the different independent variables are shown in Fig. 5.
Discussion
This study aims to analyze the current status and risk factors of social frailty in older adults living with HIV/AIDS. The results indicate that the incidence of social frailty in older adults living with HIV/AIDS is 31.34%, which is higher than the findings of Qi et al.2 and Huang et al.36. This may be attributed to factors such as chronic inflammatory responses caused by HIV infection, prolonged immune activation, and mitochondrial damage to cells caused by ART treatment, all of which accelerate the impact on the physiological, psychological, and social adaptation of older adults living with HIV/AIDS37 and results in a higher incidence of social frailty. Furthermore, there is currently no unified evaluation standard or assessment tool for social frailty, leading to different measurement outcomes. This emphasizes the need for healthcare staff at designated medical institutions and community healthcare workers to focus on identifying social frailty in older adults living with HIV/AIDS. Future studies should establish standardized criteria and evaluation tools for social frailty to facilitate the early identification of high-risk populations and the timely implementation of targeted interventions to improve clinical outcomes.
Based on the importance ranking from the RF model and the SHAP dependency plots, it was found that older adults living with HIV/AIDS with lower ADL, lack of exercise habits, cognitive impairment, depression, limited social support, older age, sleep disorders, low CD4+ lymphocyte count, insufficient per capita household income, complications, smoking history, and participation in free ART program have a higher risk of social frailty. These findings indicate that the factors influencing social frailty in older adults living with HIV/AIDS encompass personal traits, behavioral characteristics, living and working conditions, interpersonal networks, and the policy environment.
As the core component of HEM, personal traits mainly include biological characteristics such as physiological conditions and genetic factors, which are the most direct factors influencing social frailty in older adults living with HIV/AIDS. This study identified that under the category of personal traits, age, CD4+ T lymphocyte count, and complications are risk factors for the development of social frailty in older adults living with HIV/AIDS. Among these, age is the most important predictor under personal traits, which is consistent with Ragusa et al.38. With the combined effects of aging and the decline in CD4+ T lymphocyte count, the immune system of older adults living with HIV/AIDS is progressively compromised, leading to dysfunction in stress response, metabolism, and muscle function, which severely impacts overall health. This increases the risk of opportunistic infections and malignancies, thus causing a continuous decline in the ability of self-management and ultimately resulting in social isolation, reduced social interaction, and a lack of social roles1,39. CD4+ T lymphocyte count is a key indicator for assessing the disease progression, predicting clinical outcomes, and evaluating the effectiveness of antiviral therapy in older adults living with HIV/AIDS40. During follow-up, regular monitoring of CD4+ T lymphocytes and social frailty should be conducted. Multidisciplinary collaboration should be employed to further optimize treatment strategies, promote immune function recovery, reduce the incidence of complications, and support healthy aging in this population.
In behavioral characteristics, low ADL, lack of exercise habits, sleep disorders, cognitive impairment, depression, and smoking are associated with a higher incidence of social frailty in older adults living with HIV/AIDS, which is consistent with findings from other studies23,41. Among these, ADL and exercise are significant predictive factors. This is due to the fact that older adults living with HIV/AIDS are prone to developing other chronic conditions that can cause damage to important organs such as the brain or heart, thus further leading to a decline in physical function and a reduction in ADL42. Additionally, fatigue caused by the side effects of ART drugs can result in daytime lethargy and drowsiness, which disrupts regular routines, reduces physical activity, and suppresses the motivation to exercise43. The combined effects of these factors lead to lower social participation and social barriers in older adults living with HIV/AIDS44. Moreover, stigma and internalized discrimination caused by HIV infection make older adults living with HIV/AIDS more susceptible to negative emotions such as depression, which diminishes their social capital (personal relationships, social networks, social trust, social reciprocity, and social participation)45,46. Research has shown that older adults living with HIV/AIDS experience significant cognitive impairments in areas such as executive function, processing speed, language, recall, and psychomotor abilities due to neuroinflammation and apoptosis pathways activated by HIV and ART medications, which disrupt calcium homeostasis and promote oxidative stress, depleting neurotrophic factors47. This leads to a decline in their ability to access social resources, understand, and communicate, making it even more difficult for them to engage in social activities and establish connections with the outside world, thereby impairing their alternative compensatory mechanisms for social needs48. However, studies have shown that exercise not only improves the physical function of older adults living with HIV/AIDS but also enhances their psychological and sleep conditions, promotes social interactions, and increases social activities and participation49. It is recommended that healthcare professionals encourage exercise among older adults living with HIV/AIDS and incorporate multidisciplinary exercise interventions as a targeted strategy to prevent social frailty in this group, thus motivating patients to engage in social networks.
For the category of interpersonal network, the results of this study indicate that older adults living with HIV/AIDS with low social support have a higher incidence of social frailty, which is consistent with the findings of Qin et al.23. As a buffer against stress, adequate social support can expand the social support network of older adults living with HIV/AIDS, increase their social engagement and participation, and ultimately enhance their quality of life and sense of well-being50. Moreover, strong social support can provide patients with essential resources and information, including medical knowledge, medication guidance, material assistance, emotional support, and financial security, thereby improving their abilities for self-management51. With the rapid growth of older adults living with HIV/AIDS, traditional family, community, and outpatient service models are increasingly unable to meet their rising healthcare needs. The use of the internet and new media technologies has broken the information cocoon of the older population, creating more opportunities for social interaction. Therefore, healthcare professionals should integrate diverse resources to establish a multi-level, broad-ranging, refined, and personalized strategy for managing social support network management, thereby improving the health and well-being of older adults living with HIV/AIDS while also driving innovation and development in medical services.
In this study, per capita household monthly income under living and working conditions was identified as one of the predictive factors for social frailty in older adults living with HIV/AIDS. A study about the burden due to HIV across the world indicates that a higher proportion of HIV/AIDS patients reside in low- and middle-income countries, with disease burden closely linked to geographical location, healthcare systems, education, and socioeconomic status52. Most of the older adults living with HIV/AIDS in this study come from economically and culturally underdeveloped regions of China. Given the high likelihood of combinations associated with this disease, the costs of treatment and long-term ART monitoring impose a substantial financial burden relative to household income53. Additionally, low health literacy can lead to poor medication adherence, difficulties in health management, and frequent hospitalizations, and it is positively correlated with income levels54. This may explain why healthcare expenditures for older adults living with HIV/AIDS often exceed their financial capacity, further exacerbating economic burdens, lowering socioeconomic status, and increasing the risk of social isolation and negative coping toward the disease52,55. Therefore, it is crucial to consider the economic conditions of this population and facilitate their access to essential medical resources and social services to effectively lower the risk of social frailty.
For the policy environment, this study shows that older adults living with HIV/AIDS who choose the free ART program have a higher risk of social frailty. Since the implementation of China’s “Four Frees and One Care” policy, the free ART drug regimens have been continuously updated and optimized, with the current national free programs primarily consisting of dual or triple therapy regimens56. More than half of the study participants come from low-income rural areas, where financial constraints lead most patients to choose the national free program. Additionally, due to chronic inflammation and immune activation caused by HIV infection, along with aging-related factors, older adults living with HIV/AIDS are at increased risk of non-AIDS-defining illnesses. In order to manage symptoms in patients with multimorbidity and address disease-related challenges, polypharmacy has become increasingly prevalent, with its incidence ranging from 15 to 94% among older adults living with HIV/AIDS57. Polypharmacy increases the medication burden, raising the risk of adverse drug reactions, poor medication adherence, falls, and frailty58,59, thereby exacerbating the risk of social frailty in this population. These findings suggest that healthcare providers should adopt a multidisciplinary approach and leverage telemedicine technologies for dynamic follow-up of patients in free medication programs. By offering online consultations, medication guidance, and health monitoring services, medical professionals can better support these patients. Moreover, integrating resources from health and social welfare departments is crucial to providing older adults living with HIV/AIDS with comprehensive services, including medical care, financial assistance, and psychosocial support.
Research strengths and limitations
This study, based on HEM, used LASSO regression and RF to clarify the severity of social frailty among older adults living with HIV/AIDS and its influencing factors. However, it has several limitations: (1) As a cross-sectional study conducted in a single HIV/AIDS-designated hospital in China, the sample size is relatively small and lacks representativeness, making it difficult to identify the trajectory of social frailty changes in this population. (2) The cross-sectional design only establishes associations between independent and dependent variables without demonstrating causality. (3) The study focuses solely on older adults HIV/AIDS outpatients under follow-up, thus limiting its applicability to hospitalized patients. Therefore, further research is needed to address these limitations and enhance the reliability and generalizability of the findings.
Conclusion
This study reveals a high incidence of social frailty among older adults living with HIV/AIDS, underscoring the need for healthcare professionals to promptly assess social frailty in clinical practice and establish a dynamic monitoring mechanism. Based on the ranking of influencing factors, priority should be given to interventions targeting ADL, exercise, cognitive impairment, depression, and social support. Establishing a social support network for older adults living with HIV/AIDS based on HEM and strengthening health behavior interventions can effectively prevent or mitigate social frailty, thereby promoting healthy aging. Future research should further investigate the effectiveness of multidimensional intervention models to provide stronger evidence for enhancing the comprehensive care system for older adults living with HIV/AIDS.
Supplementary materials
The following supporting information can be downloaded at: https://www.kdocs.cn/l/ctLhFox4lz9o.
Data availability
The data analyzed in this study are not publicly available but available from the corresponding author upon reasonable request.
References
Kehler, D. S. et al. Frailty in older people living with HIV: current status and clinical management[J]. BMC Geriatr. 22 (1), 919 (2022).
Qi, X. et al. Prevalence of social frailty and its associated factors in the older Chinese population: a National cross-sectional study[J]. BMC Geriatr. 23 (1), 532 (2023).
Bunt, S. et al. Social frailty in older adults: a scoping review[J]. Eur. J. Ageing. 14 (3), 323–334 (2017).
Zhang, H. et al. Social frailty and the incidence of motoric cognitive risk syndrome in older adults[J]. Alzheimers Dement. 20 (4), 2329–2339 (2024).
Gandhi, R. T. et al. Antiretroviral drugs for treatment and prevention of HIV in adults: 2024 recommendations of the international antiviral Society-USA Panel[J]. JAMA 333(7), 609-628 (2024).
The path that ends AIDS. UNAIDS Global AIDS Update 2023 | UNAIDS[EB/OL]. [2025-03-08]. /en/resources/documents/2023/global-aids-update-2023.
Cao, D. et al. Molecular transmission network analysis reveals the challenge of HIV-1 in ageing patients in China: elderly people play a crucial role in the transmission of subtypes and high pretreatment drug resistance in developed Eastern China, 2019–2023[J]. Virol. J. 21 (1), 199 (2024).
Bhatia, N. S. & Chow, F. C. Neurologic complications in treated HIV-1 Infection[J]. Curr. Neurol. Neurosci. Rep. 16 (7), 62 (2016).
Blanco, J. R. et al. Definition of advanced age in HIV infection: looking for an age cut-off[J]. AIDS Res. Hum. Retroviruses. 28 (9), 1000–1006 (2012).
Tang, H., Jin, Y. & Lv, F. HIV/AIDS epidemic in the elderly and prevention and control challenges in China[J]. Chin. J. Epidemiol. 44(11), 1669–1672. (2023).
Iriarte, E. et al. HIV-Related stigma and multidimensional frailty among older Latinos with HIV[J]. Hisp Health Care Int. 22 (2), 99–108 (2024).
Ruiz, E. L. et al. From surviving to thriving: the current status of the behavioral, social, and psychological issues of aging with HIV[J]. Curr. Opin. HIV AIDS. 17 (2), 55–64 (2022).
Ye, Q. et al. Frailty status and influencing factors in people living with human immunodeficiency virus infection/acquired immunodeficiency syndrome[J]. Chin. J. Infect. Control. 23 (04), 522–526 (2024).
Zhou, Q. et al. The association between physical frailty and injurious falls and all-cause mortality as negative health outcomes in people living with HIV: A systematic review and meta-analysis[J]. Int. J. Infect. Dis. 126, 193–199 (2023).
Wu, H. et al. The level and determinants of social frailty among older patients with heart failure[J]. J. Nurs. Sci. 39 (03), 82–87 (2024).
Sallis, J. F. et al. An ecological approach to creating active living communities[J]. Annu. Rev. Public. Health. 27, 297–322 (2006).
Tibshirani, R. Regression shrinkage and selection via the lasso[J]. J. Royal Stat. Soc. Ser. B: Stat. Methodol. 58 (1), 267–288 (1996).
Qin, L. et al. Development and validation of machine learning models for postoperative venous thromboembolism prediction in colorectal cancer inpatients: a retrospective study[J]. J. Gastrointest. Oncol. 14 (1), 17 (2023).
Zhu, Z. et al. Integrating machine learning and the SHapley additive explanations (SHAP) framework to predict lymph node metastasis in gastric cancer patients based on inflammation indices and peripheral lymphocyte Subpopulations[J]. J. Inflamm. Res. 17, 9551–9566 (2024).
HIV and Hepatitis C Working Group of Infectious Diseases Society, Chinese Medical Association, Chinese Center for Disease Control and Prevention. Chinese guideline for diagnosis and treatment of human immunodeficiency virus infection/acquired immunodeficiency Syndrome(2021 Edition)[J]. Chin. J. Intern. Med. 60(12), 1106–1128. (2021).
Vittinghoff, E. & McCulloch, C. E. Relaxing the rule of ten events per variable in logistic and Cox regression[J]. Am. J. Epidemiol. 165 (6), 710–718 (2007).
Ma, L., Sun, F. & Tang, Z. Social frailty is associated with physical functioning, cognition, and depression, and predicts Mortality[J]. J. Nutr. Health Aging. 22 (8), 989–995 (2018).
Qin, Y. et al. Analysis of influencing factors of social frailty of community-dwelling older adults based on bayesian network model[J]. J. Nurs. Sci. 39 (20), 6–10 (2024).
Yesavage, J. A. et al. Development and validation of a geriatric depression screening scale: a preliminary report[J]. J. Psychiatr Res. 17 (1), 37–49 (1982).
Madeline, C. Linda, et al. Reporting on psychological well-being of older adults with chronic aphasia in the context of unaffected peers[J]. Disabil. Rehabil. 33(3), 219-228 (2011).
MD J A Y M. 9/Geriatric Depression Scale (GDS)Recent Evidence and Development of a Shorter Violence[J] (Clinical Gerontologist, 1986).
Tang, D. Application of short form geriatric depression scale (GDS-15) in Chinese elderly [J]. Chin. J. Clin. Psychol. 21 (03), 402–405 (2013).
Yu, J., Li, J. & Huang, X. The Beijing version of the Montreal cognitive assessment as a brief screening tool for mild cognitive impairment: a community-based study[J]. BMC Psychiatry. 12, 156 (2012).
Marquine, M. J. et al. The impact of ethnicity/race on the association between the veterans aging cohort study (VACS) index and neurocognitive function among HIV-infected persons[J]. J. Neurovirol. 22 (4), 442–454 (2016).
Buysse, D. J. et al. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research[J]. Psychiatry Res. 28 (2), 193–213 (1989).
Liu, X. et al. Reliability and validity of the Pittsburgh sleep quality index[J]. Chin. J. Psychiatry 29(02), 103–107. (1996).
Mahoney, F. I. & Barthel, D. W. Funtional evaluation: The Barthel index.[J]. (1965).
Hou, D. et al. Study on reliability and validity of Chinese version of Barthel Index[J]. Clin. Focus. 27 (03), 219–221 (2012).
Xiao, S. Theoretical foundations and research applications of the social support rating scale[J]. J. Clin. Psychiatry 4(02), 98–100. (1994).
Zou, Y. et al. Social Support Status and Influencing Factors among HIV-Infected Individuals Aged 50 and above in Chuxiong Prefecture[J]31196–198 (Chinese Journal of AIDS & STD, 2025). 02.
Huang, C. H. et al. The association of social frailty with intrinsic capacity in community-dwelling older adults: a prospective cohort study[J]. BMC Geriatr. 21 (1), 515 (2021).
Liu, Q. et al. HIV/AIDS knowledge, depression, and HIV-Related stigma among elderly men in rural China: A hierarchical regression Analysis[J]. Am. J. Mens Health. 17 (4), 1034099318 (2023).
Ragusa, F. S. et al. Social frailty increases the risk of all-cause mortality: A longitudinal analysis of the english longitudinal study of Ageing[J]. Exp. Gerontol. 167, 111901 (2022).
HIV and Hepatitis C Working Group of Infectious Diseases Society, Chinese Medical Association. Consensus on diagnosis and management of immunological non-responders in HIV infection (Version 2023)[J]. Chin. J. Infect. Dis. 42(01), 3–13. (2024).
HIV Working Group, Infectious Diseases Society, Chinese Medical Association. Chinese guideline for diagnosis and treatment of human immunodeficiency virus infection/acquired immunodeficiency Syndrome(2024 Edition)[J]. Chin. J. Clin. Infect. Dis. 17(03), 161–190. (2024).
Iriarte, E. et al. Factors related to multidimensional frailty among Hispanic people living with HIV aged 50 years and above: A Cross-sectional Study[J]. J. Assoc. Nurses AIDS Care. 34 (3), 259–269 (2023).
Ashwitha, S. K. et al. Management of cardiovascular diseases in HIV/AIDS patients[J]. J. Card Surg. 36 (1), 236–243 (2021).
Qin, P. et al. The role of depressive symptoms and physical activity levels in mediating the association between HIV status and neurocognitive functions among individuals aged at least 50 years in China: Cross-sectional Study[J]. JMIR Public. Health Surveill. 8 (8), e32968 (2022).
Ibeneme, S. C. et al. Impact of exercise training on symptoms of depression, physical activity level and social participation in people living with HIV/AIDS: a systematic review and meta-analysis[J]. BMC Infect. Dis. 22 (1), 469 (2022).
Perazzo, J. D. et al. Depression and social capital in people living with HIV[J]. J. Psychiatr Ment Health Nurs. 27 (1), 54–61 (2020).
Delbari, A. et al. Association between mental health and sleep condition with social frailty: evidence from Ardakan cohort study on aging (ACSA)[J]. Aging Ment Health. 28 (12), 1801–1807 (2024).
Deng, L. et al. Association of HIV infection and cognitive impairment in older adults: A meta-analysis[J]. Ageing Res. Rev. 68, 101310 (2021).
Ormel, J. et al. Quality of life and social production functions: a framework for Understanding health effects[J]. Soc. Sci. Med. 45 (7), 1051–1063 (1997).
Vancampfort, D. et al. The efficacy of physical activity counseling in Ugandan patients with HIV and a co-morbid mental disorder: a pilot study[J]. AIDS Care. 32 (6), 758–761 (2020).
Sun-Suslow, N. et al. Social support moderates D-dimer and self-rated successful aging within people with HIV and older adults[J]. J. Behav. Med. 43 (6), 979–988 (2020).
Huang, H. et al. Social support, self-efficacy, self-esteem, and self-management behaviors among people living with HIV/AIDS in China: a structural equation modeling analysis[J]. BMC Public. Health. 24 (1), 3070 (2024).
Payagala, S. & Pozniak, A. The global burden of HIV[J]. Clin. Dermatol. 42 (2), 119–127 (2024).
Negin, J. et al. Health expenditure and catastrophic spending among older adults living with HIV[J]. Glob Public. Health. 12 (10), 1282–1296 (2017).
Massaroni, V. et al. Association among therapeutic adherence, health literacy, and engagement in care: how to increase health-conscious management of HIV disease[J]. Int. J. STD AIDS. 36 (2), 132–140 (2025).
Nicholson, N. R. A review of social isolation: an important but underassessed condition in older adults[J]. J. Prim. Prev. 33 (2–3), 137–152 (2012).
National Center for STD and AIDS Prevention and Control. Chinese Center for Disease Control and Prevention. National Manual for Free Antiretroviral Therapy for AIDS[M]. People’s Medical Publishing House. (2023)
Back, D. & Marzolini, C. The challenge of HIV treatment in an era of polypharmacy[J]. J. Int. AIDS Soc. 23 (2), e25449 (2020).
Dhalwani, N. N. et al. Association between polypharmacy and falls in older adults: a longitudinal study from England[J]. BMJ Open. 7 (10), e16358 (2017).
Smit, M. et al. Future challenges for clinical care of an ageing population infected with HIV: a modelling study[J]. Lancet Infect. Dis. 15 (7), 810–818 (2015).
Acknowledgements
The work is supported by the department of Infection, department of Nursing, and respiratory and respiratory area of affiliated Hospital of Zunyi Medical University .Thank you to all the outpatient elderly HIV/AIDS patients and the medical and nursing staff of the department of Infection, department of Nursing, and respiratory and respiratory of affiliated Hospital of Zunyi Medical College in China.We thank Dr. Luo for his help in analyzing the data in this paper.
Funding
This work was supported by a project funded by the Science and Technology Fund Project of Guizhou Provincial Health and Wellness Commission (Grant No. 2024GZWJKJXM0600). and Science and Technology Plan Project of Zunyi City, Guizhou Province (Grant/Award Number: HZ (2024) 286).
Author information
Authors and Affiliations
Contributions
Li Mingdan, Xu Yali Yang Ping, Liu Qian; Made substantial contributions to conception and design, or acquisition of data, or analysis and interpretation of dataLi Mingdan, Zou Jie, Bao Zhiyan; Involved in drafting the manuscript or revising it critically for important intellectual contentLi Mingdan, Xu Yali, Zou Jie, Liu Qian, Bao Zhiyan, Zhang Xinyi, Zhang Ying, Yang Ping; Given final approval of the version to be published. Each author should have participated sufficiently in the work to take public responsibility for appropriate portions of the contentLi Mingdan, Xu Yali, Zou Jie, Liu Qian, Bao Zhiyan, Zhang Xinyi, Zhang Ying, Yang Ping;
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Institutional review board statement
This study was reviewed and approved by the Ethics Committee of the Zunyi Medical University Affiliated Hospital (Ethics No: KLLY-2023-714).
Informed consent
Informed consent was obtained from all subjects involved in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Li, M., Xu, Y., Zou, J. et al. Analysis of risk factors of social frailty in older adults living with HIV/AIDS. Sci Rep 15, 12769 (2025). https://doi.org/10.1038/s41598-025-97466-6
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-97466-6
Keywords
This article is cited by
-
Improving the care pathway for people living with HIV aged 70 years and older: the impact of geriatric screening in an infectious diseases unit (AUTO-HIV 70)
BMC Geriatrics (2025)
-
Associated Factors of Cognitive Frailty in People Living with HIV Aged 50 and Older: A Cross-Sectional Study
Infectious Diseases and Therapy (2025)