Abstract
Knee osteoarthritis (KOA) is a common, chronic, degenerative disease. Platelet-rich plasma (PRP) can significantly relieve KOA pain; however, the mechanism of PRP-induced analgesia remains to be studied. Macrophages are closely related to KOA pain, and regulating macrophage polarization may be an effective way to relieve KOA pain. Therefore, the aim of this study is: First, to explore whether PRP can effectively relieve pain in a KOA animal model and whether it relieves pain by regulating macrophage polarization. Second, to explore the mechanism by which PRP regulates macrophage polarization. Thirty-six healthy male SD rats were randomly divided into sham group, MIA group and PRP group. The KOA rat model was established by injecting 1 mg of MIA into the joint cavity. Behavioral tests, including weight-bearing asymmetry, hot plate, and von Frey hairs tests, were performed. The positive expression rates of inducible nitric oxide synthase (iNOS) and CD163 in the synovium were detected via immunohistochemical staining. Meanwhile, RAW 264.7 cells induced by lipopolysaccharide were treated with PRP in vitro. The production levels of the nuclear factor kappa-B (NF-κB) pathway-related proteins NF-κB p65, inhibitor-κ binding protein α (IκBα), p-NF-κB p65, p-IκBα and the iNOS and CD163 proteins were measured via western blotting. An enzyme-linked immunosorbent assay was used to detect the release of tumor necrosis factor-α (TNF-α), interleukin-1 beta (IL-1β), interleukin-10 (IL-10), and nerve growth factor (NGF). The behavioral results revealed that PRP relieved pain. PRP reduced the proportion of M1/M2 macrophages among synovial macrophages, significantly inhibited the secretion of TNF-α and IL-1β in the synovium, and increased the secretion of IL-10. In addition, in vivo experiments revealed that PRP decreased the protein expression of iNOS, p-IκBα/IκBα, and p-p65/p65 and increased the protein expression of CD163. Furthermore, PRP decreased TNF-α, IL-1β, and NGF levels in RAW 264.7 cells and increased the secretion of IL-10. Our findings indicate that PRP can improve long-term relief from KOA pain. The analgesic mechanism promotes the transformation of M1 macrophages to M2 macrophages by inhibiting the NF-κB signaling pathway, which reduces the release of downstream pain-causing factors, thus relieving inflammation and pain.
Similar content being viewed by others
Introduction
Knee osteoarthritis (KOA) is prevalent among elderly individuals and is one of the main causes of pain and disability worldwide1. KOA can induce joint pain, stiffness, and loss of function2. As there is currently no cure for KOA, pain relief is the main treatment goal3. Currently, there are medication and non-medication techniques for pain management4. Oral medication is the preferred option for patients with KOA, but long-term use can result in greater adverse effects and lower effectiveness5. Joint replacement surgery is a pain management strategy for patients with advanced KOA, but it also carries a significant risk of complications, including infection and functional dissatisfaction6. Therefore, additional safe and effective approaches are needed for managing KOA-related pain.
Platelet-rich plasma (PRP) is generated by centrifuging whole blood to concentrate platelets containing concentrated platelets and different growth factors7. Recent studies have focused on the effects of PRP on chondrocytes and cartilage tissue in KOA, including the promotion of chondrocyte proliferation and stroma-generating stimulation8. According to clinical reports, PRP has excellent potential for pain management in osteoarthritis patients9. Compared with hyaluronic acid injection and placebo, PRP can more effectively relieve KOA pain and significantly improve knee joint function10. The mechanism of pain relief by PRP is still being explored. Several studies have shown that PRP promotes cartilage formation by inhibiting catabolic factors such as interleukin (IL)-1β and tumor necrosis factor (TNF)-α and promoting fibroblast growth factor and transforming growth factor-β (TGF-β), thus further relieving pain11,12. However, cartilage is structurally free of blood vessels and nerves, and studies have shown a weak correlation between pain and defects of cartilage13. Thus, pain relief may not be due to cartilage repair14. Studies have shown a strong correlation between KOA pain and synovitis15. The production and release of TNF-α, IL-1β, and IL-6, which regulate central nervous system pain, were detected in the synovial fluid, synovial tissue, and serum of KOA patients. In addition, pain neurotransmitters such as nerve growth factor (NGF) are released into OA joints16. Several studies have suggested that PRP regulates inflammation by releasing pro-inflammatory and anti-inflammatory mediators from alpha granules in platelets and diluting pro-inflammatory cytokines in the joint environment to reduce pain and inflammation17,18. However, the exact mechanism through which PRP regulates inflammation and pain has rarely been studied.
Macrophages are basic cells involved in inflammation19. A growing number of studies have revealed a link between macrophages and KOA pain20. Synovial macrophages are a type of plastic cell21. Bone marrow-derived monocytes move to the damaged region and further differentiate into the M1 or M2 phenotype when tissue destruction results in inflammation21. M1 phenotype macrophages are typically activated and produce pro-inflammatory cytokines and chemokines that contribute to pain. In contrast, M2 phenotype macrophages are immunosuppressive cells that secrete anti-inflammatory cytokines and growth factors that promote tissue repair and pain relief22. An imbalance in the polarization of synovial macrophages to the M1 phenotype has been confirmed in OA patients and mice23,24. Consequently, targeting macrophage polarization as a therapeutic strategy may be an effective means of relieving pain in patients with KOA22. Recently, Naoko et al. reported that multiple intra-articular injections of PRP may improve synovitis, protect cartilage, and alleviate pain in a collagenase-induced OA animal model and that PRP can affect the phenotypic modifications of macrophages25. However, the relationship between PRP analgesia and phenotypic changes in macrophages and the mechanism through which PRP regulates phenotypic changes in macrophages remain unclear.
Therefore, the purpose of the study is: First, to explore whether PRP can effectively relieve pain in a KOA animal model and whether it relieves pain by regulating macrophage polarization. Second, we explored the mechanism by which PRP regulates macrophage polarization.
Materials and methods
Animals
Forty-four male Sprague–Dawley (SD) rats (weight 200 ± 20 g) were provided by the Experimental Animal Center of Qingdao University. Male SD rats were kept in a designated facility, which operates at a circadian rhythm of controlled temperature (22 ± 2 °C) for 12 h, with free access to clean water and food. All animal experiments in the study were conducted in strict accordance with the regulations on the use and care of experimental animals in China and were approved by the Experimental Animal Welfare Ethics Committee of Qingdao University (approval number: 20220728SD4420221203073). All methods are reported in accordance with ARRIVE guidelines.
PRP preparation
The rats were anesthetized with 5% isoflurane in O2, and whole blood was extracted from male SD rats via abdominal aorta puncture and injected into a syringe containing 3.8% sodium citrate. The samples were centrifuged at 800 rpm for 15 min, and PRP was obtained from the anticoagulant blood. The platelet concentration in PRP was three times higher than baseline whole blood. The platelet concentration in PRP was 3020,000 platelets/μL. Aliquot the PRP into small volumes (60 μl) and freeze at − 80 °C for 24 h. Thaw the frozen PRP at 37 °C in a water bath for 1 h until completely liquefied. Repeat the freeze–thaw cycle three times to ensure complete platelet activation26. After the final thawing step, visually inspect the PRP for the formation of a gel-like clot, which indicates activation27. PRP was frozen at − 80 °C until use.
Animal model
The rats were anesthetized with 5% isoflurane in O2, and the left knee of the hind leg was shaved and sterilized. Monosodium iodoacetate (MIA; 1 mg) was dissolved in 60 µl of 0.9% sodium chloride and injected into the cavity of the left knee joint through the infrapatellar ligament.
Experimental design
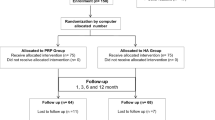
The rats were randomly divided into three groups: the Sham, MIA, and PRP groups. MIA was injected into the joint cavity on day-7 to induce osteoarthritis, and the sham group was injected with an equal amount of normal saline. The PRP group injected 60 μL PRP into the left knee joint cavity on days -4, -2, and 0. The control group received normal saline treatment. Pain behavior was observed on days -8, -6, -4, 1, 3, 5, 7, 14, and 21. On the 5th and 21st days after treatment, the rats were euthanized by cervical dislocation, and the synovium of the left knee joint was collected for histological evaluation (Fig. 1).
Schematic diagram of the experimental design. The picture was created using the WPS Office application (https://platform.wps.cn/?channel_no=20.3104). MIA monosodium iodoacetate, PRP platelet-rich plasma.
Behavioral testing
Weight-bearing asymmetry
When the rats were put into the double-foot balance tester, the weight-bearing ability of both feet changed after the operation, and the pain sensitivity of the hind limb was measured by measuring the weight-bearing ability of both feet. Zero no load is applied to both pedals. Before the experiment, the rats were allowed to adapt for 20 min in the tester, forcing the hind feet of each rat to be placed at the center of two independent pressure plates. The experimenter was unaware of the grouping of rats. After the animals were quiet, the average pressure on the left and right hind limbs was recorded for more than 5 s. In addition, the same rats were measured three times, and the average values of the three tests were recorded. According to the following formula, the bipedal balance test results were converted into a percentage of the affected side (left) hind foot bearing: left/(left + right) × 100%. Weight asymmetry was evaluated as the percentage difference in weight distribution between the hind limbs.
Thermal hyperalgesia
All the rats were allowed to adapt for 15 min on a hot plate before the formal test. The hot plate surface was kept at a constant temperature (55 ± 0.1 °C). After the rat was placed on the HP, the time of the first behavioral response (licking or jumping) was recorded as the paw retrieval latency (PWL). The cut-off time was 20 s to prevent injury. The measurement was repeated three times, and the average of the three tests was calculated.
Mechanical allodynia
The paw withdrawal threshold (PWT) was measured via Von Frey hairs (North Coast, USA) via the up-down method to evaluate mechanical hyperalgesia. Before the formal experiment, all the rats were placed on a unique plexiglass grid platform for 30 min. A series of Von Frey filaments was used as the starting point to stimulate the left plantar skin of the rats vertically for approximately 5 s. Each filament was repeated five times at a stimulation interval of 1 min. Rapid retraction or licking of the claws was considered a positive response. The 50% reaction threshold was calculated via the following formula: 50% g threshold = (10 [Xf + Kδ])/10,000.
Immunohistochemistry
Synovial tissue samples were collected immediately after surgery and fixed in 4% paraformaldehyde for 24 h at room temperature to preserve tissue integrity. The samples were then dehydrated through a graded ethanol series, cleared in xylene, and embedded in paraffin. Sections of 4 µm thickness were cut and mounted on glass slides. Throughout the process, care was taken to minimize the loss of liquid components by controlling fixation and dehydration times. The slices were placed in a sodium citrate buffer and heated in a microwave oven for 10 min. The slices were incubated with two drops of a 3% H2O2-methanol solution, sealed at room temperature for 10 min, and then incubated with 1% BSA at room temperature for 20 min. The slices were incubated overnight with CD163 rabbit polyclonal antibody (Bioss, 1:200 dilution, bs-2527R) or inducible nitric oxide synthase (iNOS) rabbit polyclonal antibody (Bioss, 1:200 dilution, bs-0162R) at 4 °C. The slices were incubated with an HRP-labeled goat anti-rabbit IgG secondary antibody (Bioss, 1:1000 dilution; bs-0295G), stained with DAB, restained with hematoxylin, dehydrated, and sealed. The stained sections were observed via an inverted fluorescence microscope, and immunohistochemical images were obtained. The positive rate was calculated by selecting the areas expressing CD163 and iNOS in each section via ImageJ software.
Cell culture and treatment
RAW 264.7 cells were obtained from Procell (Wuhan, CL-0190). RAW264.7 cells were cultured in a 5% CO2 incubator at 37 °C. The culture medium was Dulbecco’s modified Eagle’s medium containing 10% fetal bovine serum (ExCell; FSP500). In this study, BAY11-7082 (Beyotime, S1523), a specific inhibitor of NF-κB signaling, was used to assess the contribution of the NF-κB signaling pathway to phenotypic transformation of M1 and M2. The experimental groups were divided into four groups: the control, LPS, PRP, and BAY 11–7082 groups. The cells were inoculated at a density of 1 × 106 on a 6-well plate. When the cells reached 80% confluence, they were pretreated with BAY 11–7082 for 4 h, lipopolysaccharide (LPS) was added for 24 h, and PRP was added for 24 h.
Western blotting
After treatment, the cells were lysed on ice for 30 min with RIPA lysis buffer (Biotech, C500005) containing a protease inhibitor or phosphatase inhibitor and sonicated. The supernatant was subsequently collected via 4 °C centrifugation. The lysate was boiled at 100 °C for 10 min to denature the protein, and the protein concentration was measured via a BCA kit (Vazyme, E112-01). Protein samples were separated by SDS‒PAGE and transferred to a PVDF membrane. The membrane was blocked with 5% skim milk powder at room temperature for 1 h and then incubated with iNOS rabbit recombinant antibody (Proteintech, 1:2000 dilution, 80,517–1-RR), CD163 rabbit polyclonal antibody (Bioss, 1:1000 dilution, bs-2527R), phospho- IκBα-S32 rabbit mAb (ABclonal, 1:1000 dilution, AP0707), IκBα rabbit mAb (ABclonal, 1:1000 dilution, A19714), phospho- NF-κB p65 rabbit recombinant antibody (Proteintech, 1:2000 dilution, 82,335–1-RR), NF-κB p65 mouse monoclonal antibody (Proteintech, 1:2000 dilution, 66,535–1-Ig), and Beta actin mouse monoclonal antibody (Proteintech, 1:10,000 dilution, 66,009–1-Ig) overnight at 4 °C. The membrane was then incubated with an HRP-labeled goat anti-rabbit IgG secondary antibody (Bioss, 1:10,000 dilution; bs-0295G) for 1 h at room temperature. A hypersensitive chemiluminescence reagent was added to the membrane, and a gel imaging system (Bio-Rad Laboratories, Inc.) was used to quantify the protein concentration. The gray value was measured via ImageJ software.
Enzyme-linked immunosorbent assay
Synovial tissues were thawed on ice and cut into small pieces. The tissue pieces were homogenized in RIPA buffer containing protease inhibitors using a tissue homogenizer on ice. The homogenate was incubated at 4 °C for 15 min with intermittent vortexing, followed by centrifugation at 12,000 rpm for 10 min at 4 °C. The supernatant was carefully collected, and the levels of cytokines, including TNF-α, IL-1β, and IL-10, were measured via an ELISA kit. Cells were cultured to 80–90% confluency and treated as indicated. After treatment, cells were washed twice with ice-cold PBS and harvested by trypsinization. Cell pellets were collected by centrifugation at 1000 rpm for 5 min at 4 °C and lysed in RIPA buffer containing protease inhibitors. The lysates were incubated on ice for 30 min with intermittent vortexing, followed by centrifugation at 12,000 rpm for 10 min at 4 °C. The supernatant was collected, and the concentrations of cytokines, including TNF-α, IL-1β, IL-10, and NGF, were measured via the corresponding ELISA kits.
Statistical analysis
GraphPad Prism 8.0 software was used for statistical analysis, and all the data were expressed as the means ± SEMs. One-way ANOVA was used for comparison of multiple group means, followed by Tukey’s HSD or Bonferroni correction for pairwise comparison. P < 0.05 indicated that the difference was statistically significant.
Results
PRP relieves the pain associated with KOA.
We measured pain behavior in all the rats on day -8, and there were no significant differences. On days -6 and -4, compared with those in the Sham group, the weight-bearing percentage, PWT, and PWL of the affected side in the MIA group were significantly lower than those in the Sham group. Within 21 days of treatment, the weight-bearing percentage, PWT, and PWL of the affected side were significantly greater in the PRP group than in the MIA group (Fig. 2).
Effects of MIA and PRP on pain behavior. Intra-articular injection of 1 mg MIA significantly reduced the weight-bearing ability (A), PWT (B), and PWL (C) of the affected limb. After the injection of PRP, the weight-bearing (A), PWT (B), and PWL (C) of the affected limb increased. The arrows depict the time of injection of PRP. The bars represent the means ± SEMs (n = 6). ****p < 0.0001. Asterisks (*) denote differences between the Sham group and the MIA group. ##P < 0.01; ###P < 0.001; ####P < 0.0001. Hash signs (#) denote differences between the MIA group and the PRP group. PWT paw withdrawal latency, PWL paw withdrawal threshold.
Effects of PRP on the M1/M2 ratio of synovial macrophages
We performed immunohistochemical staining to detect the proportion of M1 and M2 phenotype-positive synovial macrophages. Compared with that in the Sham operation group, the proportion of iNOS-positive cells in the MIA group was significantly greater on days 5 and 21 after treatment, whereas there was no difference in the proportion of CD163-positive cells (Fig. 3; Table 1). The proportion of iNOS-positive cells was significantly lower in the PRP group than in the MIA group. The proportion of CD163-positive cells in the PRP group was significantly greater than that in the MIA group (Fig. 3; Table 1).
Effects of MIA and PRP on the immunohistochemical expression of iNOS (M1 macrophage marker) and CD163 (M2 macrophage marker). (A) Representative microphotographs of immunohistochemical staining for iNOS and CD163 in each group. Scale bars: 100 µm. (B,C) Proportion of iNOS (B)- and CD163 (C)-positive cells stained at 5 and 21 days after treatment. Data are presented as the means ± SEM (n = 3). *p < 0.05, **p < 0.01, ***p < 0.001. ns not significant.
Effects of PRP on cytokines secreted by M1/M2 synovial macrophages
We detected the expression of TNF-α, IL-1β, and IL-10 in the synovium. The ELISA results revealed that the expression levels of TNF-α and IL-1β in the MIA group were significantly greater than those in the Sham group (Fig. 4A, B), whereas the expression level of IL-10 was significantly lower (Fig. 4C). Compared with those in the MIA group, the expression levels of TNF-α and IL-1β in the PRP group were significantly lower (Fig. 4A, B), whereas the expression level of IL-10 was significantly greater (Fig. 4C).
PRP treatment inhibited the expression of TNF-α and IL-1β and increased the expression of IL-10. The expression levels of TNF-α (A), IL-1β (B) and IL-10 (C) were determined via ELISA at 5 and 21 days after treatment. The data are presented as the means ± SEMs (n = 3). *p < 0.05, **p < 0.01, ***p < 0.001.
PRP inhibits the polarization of RAW264.7 macrophages to the M1 phenotype
The expression levels of the macrophage phenotype-specific protein M1 marker iNOS and the M2 marker CD163 were detected via western blotting. Compared with that in the control group, the expression level of iNOS was significantly increased, and the expression level of CD163 was significantly decreased in the LPS group. However, compared with that in the LPS group, the expression level of iNOS in the PRP group was considerably lower, and the expression level of CD163 was significantly greater. After treatment with NF-κB inhibitor BAY11 -7082, the expression level of iNOS in the BAY group was lower than that in the LPS group, and the expression level of CD163 was significantly higher, and the effect was more obvious than that in the PRP group (Fig. 5).
PRP treatment can inhibit the transformation of macrophages to the M1 phenotype. (A) The protein levels of iNOS, CD163, and β-actin were detected by Western blotting. (B,C) Statistical analysis of the relative expression of iNOS (B) and CD163 (C) in each group. The data are presented as the means ± SEMs from three independent experiments. *p < 0.05, **p < 0.01, ***p < 0.001.
Effects of PRP on the NF-kB signaling pathway in macrophages
The phosphorylation levels and total protein expression levels of NF-κB p65 and IκBα in the NF-κB signaling pathway were detected by western blotting. The results revealed that the levels of p-NF-κB p65 and p-IκBα in the LPS group were significantly greater than those in the control group, whereas the levels of p-NF-κB p65 and p-IκBα in the PRP group were substantially lower than those in the LPS group. After adding NF-κB inhibitor BAY11-7082, the levels of p-NF-κB p65 and p-IκBα in the BAY group were much lower than those in the LPS group, and the effect was more obvious than that in the PRP group (Fig. 6).
PRP treatment can inhibit the activation of the NF-kB signaling pathway in macrophages. (A) The protein levels of p-IκBα, IκBα, p-NF-κB p65, and NF-κB p65 were detected via Western blotting. (B,C) Statistical analysis of the p-IκBα/IκBα and p-P65/P-65 ratios in each group. The data are presented as the means ± SEMs from three independent experiments. *p < 0.05, **p < 0.01, ***p < 0.001.
Effects of PRP on cytokines secreted by macrophages in vitro
To measure the levels of cytokines secreted by PRP on macrophages, the expression levels of TNF-α, IL-1β, IL-10, and NGF in the supernatant of cultured macrophages were detected via ELISA. Compared with those in the control group, the expression levels of TNF-α, IL-1β, and NGF were significantly increased, and the expression level of IL-10 was significantly decreased in the LPS group (Fig. 7). Compared with those in the LPS group, the expression levels of TNF-α, IL-1β, and NGF in the PRP group were significantly lower, whereas the expression level of IL-10 was significantly greater (Fig. 7). In addition, the results for the BAY11-7082 group were consistent with those for the PRP group (Fig. 7).
Discussion
KOA is a chronic inflammatory condition that can lead to pain, progressive destruction, and degeneration of cartilage function. Pain is often the main cause of patients seeking medical treatment28. Preclinical pain models are used to examine the pathogenic mechanism of pain caused by OA and to develop more effective treatment interventions29. The MIA chemical model is a classical model for the study of OA pain and a rapidly progressive model that can lead to rapid degeneration of articular cartilage, synovitis, and destruction of the subchondral bone30. According to Nwosu et al., high-dose (1 mg) MIA can result in prolonged hyperalgesia, weight-bearing asymmetry, and macrophage infiltration31. However, low-dose (0.2 mg) MIA cannot cause structural changes or persistent pain32. Therefore, we used high-dose (1 mg) MIA to establish a pain model for KOA. Our results revealed that, after MIA administration, the weight-bearing ability of the left hemisphere in the MIA group was significantly lower than that in the Sham group, the PWT and PWL decreased significantly, and these changes persisted throughout the experiment. These results are consistent with those of previous studies30.
In recent years, PRP has received significant attention as an emerging therapeutic agent33. A systematic review revealed that PRP injections were beneficial for pain relief in patients with KOA34. In our study, we found that the pain-like behavior of KOA rats improved considerably within 21 days of treatment. Compared with those of the MIA group, the weight-bearing ability on the left side of the PRP group was significantly greater, and the PWT and PWL of the PRP group were also significantly greater, suggesting that the pain was significantly relieved. It has been reported that pain in KOA is caused by both peripheral and central sensitization, in which weight-bearing asymmetry may be a combination of peripheral nociception and sensitization35. The decrease in PWT and PWL is thought to be caused by abnormal pain caused by central sensitization36. These results suggest that PRP can continuously relieve pain and reduce central sensitization.
An increasing number of studies have shown that macrophages are involved in the development of OA pain37,38. Synovial macrophages are a mixed population divided into M1 and M2 phenotypes according to different functional phenotypes19. Liu et al. confirmed that the proportion of M1/M2 macrophages in the synovial fluid and peripheral blood of OA patients was significantly greater than that in healthy controls39. Zhang et al. reported that an increase in the proportion of M1 macrophages aggravated pain associated with KOA40. In our study, we found that on days 5 and 21, the proportion of iNOS-positive cells in the MIA group was significantly greater than that in the sham group, whereas there was no difference in the proportion of CD163-positive cells, indicating that the proportion of M1/M2 macrophages increased and persisted throughout KOA. Synovial macrophages were polarized to the M1 phenotype, which is consistent with previous studies39.
Previous research has shown that macrophages can alter the activity of nociceptive receptors by secreting soluble factors41. Macrophages can produce a series of mediators that bind to receptors expressed by nociceptors and induce pain by directly activating nociceptors41. These mediators include cytokines such as IL-1β and TNF-α, which affect the activity of nociceptors, and NGF, which acts on nociceptors and increases their excitability through Tyrosine Kinase Receptor A42. Owing to the heterogeneity of macrophages, cytokines, such as TNF-α and IL-1β, are secreted by M1 phenotype macrophages to promote pain. In contrast, cytokines, such as IL-10 and TGF, are secreted by M2 phenotype macrophages to inhibit inflammation. Therefore, we focused on the expression levels of soluble factors secreted by macrophages to further explore the relationship between the phenotypic transformation of macrophages and pain. In our study, we found that, compared with those in the Sham group, the levels of TNF-α and IL-1β in the synovial membrane of the MIA group were significantly greater, and the levels of IL-10 were significantly lower. In addition, compared with those in the control group in the in vitro experiments, the levels of TNF-α, IL-1β, and NGF in the cell supernatant of the LPS group were also significantly increased, and the content of IL-10 was significantly decreased. Therefore, we can conclude that the polarization of macrophages to the M1 phenotype may increase the levels of downstream pain factors, which may be involved in the pain mechanism of KOA. Previous studies have shown that the anti-inflammatory mediator (IL-10) released by M2-type macrophages plays a positive role in pain relief. Bang et al. confirmed that G protein-coupled receptor 37 activation promotes macrophage M2 polarization and relieves inflammatory pain by increasing IL-10 and TGF-β release43. Furthermore, promoting the transformation of M1 macrophages to the M2 phenotype may be an effective means to relieve pain.
Consistent with previous studies25, we found that the proportion of iNOS-positive cells significantly decreased in the PRP group compared with the MIA group on either the 5th day or the 21st day following treatment, whereas the proportion of CD163-positive cells significantly increased, indicating that the proportion of M1/M2 macrophages continuously decreased. These findings demonstrate that PRP can constantly transform M1 phenotype macrophages into M2 phenotype macrophages. In addition, the in vitro and in vivo results of this study further showed that PRP could significantly reduce the content of TNF-α and IL-1β secreted by M1-type macrophages and increase the content of IL-10 secreted by M2-type macrophages. Interestingly, in vitro, the NGF content in the supernatant of cultured macrophages treated with PRP was significantly lower than that in the supernatant of cultured macrophages treated with LPS. Studies have shown that NGF can be released from macrophages, which have activation and sensitization effects on nociceptors44. In addition, Takano et al. confirmed that NGF expression in synovial macrophages and fibroblasts in OA mice may be regulated by TNF-α and IL-1β45. TNF-α and IL-1β upregulate the expression of nerve growth factors in synovial fibroblasts and macrophages45. In our study, the contents of TNF-α, IL-1β, and NGF decreased after PRP treatment, suggesting that the decrease in NGF content may be due to the decrease in TNF-α and IL-1β levels. Moreover, the inhibition of NGF activity has been demonstrated to reduce hyperalgesia in an OA animal model46. Therefore, we can conclude that PRP can achieve an analgesic effect by reducing the expression of the pro-inflammatory cytokines TNF-α and IL-1β, increasing the level of the anti-inflammatory cytokine IL-10, directly reducing nociceptor stimulation, and reducing sensitization. Moreover, it is possible to mitigate hyperalgesia by indirectly reducing NGF content and achieving long-lasting analgesic effects. In contrast to previous studies, PRP inhibits pain sensitization by reducing the concentration of the pain-related neuropeptide calcitonin gene-related peptide in the fat pad under the patella47. Unlike published research on the mechanism of PRP, published research on the mechanism of PRP mostly focuses on the repair of chondrocytes and inhibition of inflammation, thereby indirectly alleviating pain. This study reveals that PRP inhibits the release of inflammatory factors by regulating macrophage polarization, thereby directly or indirectly alleviating pain. This study shifts the focus from chondrocytes to macrophages, revealing a new mechanism by which PRP achieves analgesia by regulating macrophage polarization. This research perspective not only supplements the existing understanding of the role of PRP but also provides a new theoretical basis for the application of PRP in analgesia.
Many studies have confirmed that the polarization of macrophages is regulated by many signaling pathways, such as the mitogen-activated protein kinase (MAPK), signal transducer and transcriptional activator (STAT) family, and the NF-κB signaling pathway48,49,50. NF-κB is a nuclear factor that regulates gene transcription. By combining with transcription regulatory elements, NF-κB activates the transcription of many downstream inflammatory genes, thus triggering inflammation and the release of inflammatory factors51. NF-κB is essential for inducing a variety of inflammatory cytokines and mediators, including iNOS, TNF-α, and IL-1β, and is an important regulatory factor for macrophage polarization49,52. Activation of the NF-κB signaling pathway can promote the expression of inflammatory factors, and inflammatory factors themselves can regulate inflammatory responses by activating the NF-κB signaling pathway53. Phosphorylation is crucial for activating the NF-κB signaling pathway50. Zhou et al. confirmed that inhibition of IκBα phosphorylation in the cytoplasm further reduces the transport of downstream NF-κB p65 protein from the cytoplasm to the nucleus, thereby polarizing the M1 phenotype toward the M2 phenotype50. Therefore, we speculate that the regulation of macrophage polarization by PRP is related to the NF-κB signaling pathway in macrophages. Therefore, we conducted in vitro experiments to verify our hypotheses. Our data demonstrated that LPS stimulation significantly increased iNOS expression and reduced CD163 expression, transforming macrophages into the M1 phenotype. In addition, LPS dramatically increased the phosphorylation levels of IκBα and NF-κB p65 and activated the NF-κB signaling pathway. However, after PRP intervention, the above effects were reversed; the expression of iNOS decreased, whereas the expression of CD163 increased, suggesting that macrophages could transform from the M1 phenotype to the M2 phenotype. Furthermore, PRP significantly reduced the phosphorylation of IκBα and NF-κB p65. BAY11 -7082 is a specific NF-κB inhibitor. BAY11 -7082 inhibits the activation of NF-κB by inhibiting the phosphorylation of IκBα and preventing its degradation. In order to further evaluate the effect of the NF-κB signaling pathway on macrophage polarization, we added the NF-κB inhibitor BAY11 -7082 while treating PRP. The effect of PRP was further enhanced, indicating that the NF-κB signaling pathway plays an important role in the conversion of M1 phenotype to M2, and verified the mechanism by which PRP promotes the conversion of M1 phenotype to M2 by inhibiting the NF-κB signaling pathway.
This study has several limitations. First, synovial macrophages comprise a mixed population of different sources and functional phenotypes. M1 and M2 phenotype macrophages are the two extremes of macrophages in vitro, but they cannot fully reflect the complexity and plasticity of tissue macrophages in vivo. Second, we only measured NGF secreted by macrophages in vitro and did not measure the changes in NGF secreted by synovial macrophages in vivo. Third, the NF-κB signaling pathway was not further interfered with to explore the specific inhibitory effect of PRP on this pathway. All the issues raised above should be investigated further.
Conclusions
In conclusion, this study suggests that PRP treatment in KOA patients can relieve inflammation and pain in the long term. Its analgesic mechanism includes inhibiting the NF-κB signaling pathway to transform M1 phenotype macrophages to the M2 phenotype, reducing the expression of the pro-inflammatory cytokines TNF-α and IL-1β, increasing the level of the anti-inflammatory cytokine IL-10, directly reducing nociceptor stimulation, and reducing sensitization. Moreover, it is possible to mitigate hyperalgesia by indirectly reducing NGF content and achieving long-lasting analgesic effects. The results of this study provide a theoretical basis for PRP to relieve the inflammation and pain associated with KOA.
Data availability
All data used in this study are available from the corresponding author upon request.
References
Sharma, L. & Solomon, C. G. Osteoarthritis of the Knee. N. Engl. J. Med. 384, 51–59. https://doi.org/10.1056/NEJMcp1903768 (2021).
Zhao, Y. et al. Predictive value of the morphology of proximal tibiofibular joint for total knee replacement in patients with knee osteoarthritis. J. Orthop. Res. 39, 1289–1296. https://doi.org/10.1002/jor.24862 (2020).
Bennell, K. L., Hunter, D. J. & Hinman, R. S. Management of osteoarthritis of the knee. BMJ Br. Med. J. 345, 8. https://doi.org/10.1136/bmj.e4934 (2012).
Ferreira, R. M., Duarte, J. A. & Goncalves, R. S. Non-pharmacological and non-surgical interventions to manage patients with knee osteoarthritis: an umbrella review. Acta Reumatol. Port. 43, 182–200 (2018).
Zhang, Q., Young, L. & Li, F. Network meta-analysis of various nonpharmacological interventions on pain relief in older adults with osteoarthritis. Am. J. Phys. Med. Rehabil. 98, 469–478. https://doi.org/10.1097/phm.0000000000001130 (2019).
D’Apuzzo, M., Westrich, G., Hidaka, C., Jung Pan, T. & Lyman, S. All-cause versus complication-specific readmission following total knee arthroplasty. J. Bone Joint Surg. 99, 1093–1103. https://doi.org/10.2106/jbjs.16.00874 (2017).
Castillo, T. N., Pouliot, M. A., Kim, H. J. & Dragoo, J. L. Comparison of growth factor and platelet concentration from commercial platelet-rich plasma separation systems. Am. J. Sports Med. 39, 266–271. https://doi.org/10.1177/0363546510387517 (2010).
Boffa, A. et al. Platelet-rich plasma injections induce disease-modifying effects in the treatment of osteoarthritis in animal models. Knee Surg. Sports Traumatol. Arthrosc. 29, 4100–4121. https://doi.org/10.1007/s00167-021-06659-9 (2021).
Knezevic, N. N., Candido, K. D., Desai, R. & Kaye, A. D. Is platelet-rich plasma a future therapy in pain management?. Med. Clin. N. Am. 100, 199–217. https://doi.org/10.1016/j.mcna.2015.08.014 (2016).
Belk, J. W. et al. Platelet-rich plasma versus hyaluronic acid for knee osteoarthritis: A systematic review and meta-analysis of randomized controlled trials. Am. J. Sports Med. 49, 249–260. https://doi.org/10.1177/0363546520909397 (2020).
Daheshia, M. & Yao, J. Q. The interleukin 1β pathway in the pathogenesis of osteoarthritis. J. Rheumatol. 35, 2306–2312. https://doi.org/10.3899/jrheum.080346 (2008).
Park, K. H. & Na, K. Effect of growth factors on chondrogenic differentiation of rabbit mesenchymal cells embedded in injectable hydrogels. J. Biosci. Bioeng. 106, 74–79. https://doi.org/10.1263/jbb.106.74 (2008).
Kornaat, P. R. et al. Osteoarthritis of the knee: Association between clinical features and MR imaging findings. Radiology 239, 811–817. https://doi.org/10.1148/radiol.2393050253 (2006).
Sakamoto, T. et al. Intraarticular injection of processed lipoaspirate cells has anti-inflammatory and analgesic effects but does not improve degenerative changes in murine monoiodoacetate-induced osteoarthritis. BMC Musculoskelet. Disord. 20, 11. https://doi.org/10.1186/s12891-019-2710-1 (2019).
Neogi, T. et al. Association of joint inflammation with pain sensitization in knee osteoarthritis: The multicenter osteoarthritis study. Arthritis Rheumatol. 68, 654–661. https://doi.org/10.1002/art.39488 (2016).
Harth, M. & Nielson, W. R. Pain and affective distress in arthritis: relationship to immunity and inflammation. Expert Rev. Clin. Immunol. 15, 541–552. https://doi.org/10.1080/1744666x.2019.1573675 (2019).
Bocun, L. et al. Effects of platelet-rich plasma injection for pain control and cartilage repair in knee osteoarthritis. Medicine https://doi.org/10.1097/md.0000000000024107 (2021).
Grossen, A. A. et al. Platelet-rich plasma injections: Pharmacological and clinical considerations in pain management. Curr. Pain Headache Rep. 26, 741–749. https://doi.org/10.1007/s11916-022-01082-2 (2022).
Culemann, S. et al. Locally renewing resident synovial macrophages provide a protective barrier for the joint. Nature 572, 670. https://doi.org/10.1038/s41586-019-1471-1 (2019).
Wang, D., Chai, X. Q., Hu, S. S. & Pan, F. Joint synovial macrophages as a potential target for intra-articular treatment of osteoarthritis-related pain. Osteoarthr. Cartil. 30, 406–415. https://doi.org/10.1016/j.joca.2021.11.014 (2022).
Wynn, T. A. & Vannella, K. M. Macrophages in tissue repair, regeneration, and fibrosis. Immunity 44, 450–462. https://doi.org/10.1016/j.immuni.2016.02.015 (2016).
da Silva, M. D. et al. IL-10 cytokine released from M2 macrophages is crucial for analgesic and anti-inflammatory effects of acupuncture in a model of inflammatory muscle pain. Mol. Neurobiol. 51, 19–31. https://doi.org/10.1007/s12035-014-8790-x (2015).
Hsueh, M. F., Zhang, X., Wellman, S. S., Bolognesi, M. P. & Kraus, V. B. Synergistic roles of macrophages and neutrophils in osteoarthritis progression. Arthritis Rheumatol. 73, 89–99. https://doi.org/10.1002/art.41486 (2020).
Zhou, F. et al. Modified ZIF-8 nanoparticles attenuate osteoarthritis by reprogramming the metabolic pathway of synovial macrophages. ACS Appl. Mater. Interfaces. 12, 2009–2022. https://doi.org/10.1021/acsami.9b16327 (2019).
Khatab, S. et al. Intra-articular injections of platelet-rich plasma releasate reduce pain and synovial inflammation in a mouse model of osteoarthritis. Am. J. Sports Med. 46, 977–986. https://doi.org/10.1177/0363546517750635 (2018).
Roffi, A. et al. Does platelet-rich plasma freeze-thawing influence growth factor release and their effects on chondrocytes and synoviocytes?. Biomed. Res. Int. 2014, 692913. https://doi.org/10.1155/2014/692913 (2014).
Lu, C. F. et al. Combining chitin biological conduits with small autogenous nerves and platelet-rich plasma for the repair of sciatic nerve defects in rats. CNS Neurosci. Ther. 27, 805–819. https://doi.org/10.1111/cns.13640 (2021).
Thomas, E., Peat, G. & Croft, P. Defining and mapping the person with osteoarthritis for population studies and public health. Rheumatology 53, 338–345. https://doi.org/10.1093/rheumatology/ket346 (2013).
Fernihough, J. et al. Pain related behaviour in two models of osteoarthritis in the rat knee. Pain 112, 83–93. https://doi.org/10.1016/j.pain.2004.08.004 (2004).
Guzman, R. E., Evans, M. G., Bove, S., Morenko, B. & Kilgore, K. Mono-iodoacetate-induced histologic changes in subchondral bone and articular cartilage of rat femorotibial joints: An animal model of osteoarthritis. Toxicol. Pathol. 31, 619–624. https://doi.org/10.1080/01926230390241800 (2003).
Nwosu, L. N., Mapp, P. I., Chapman, V. & Walsh, D. A. Relationship between structural pathology and pain behaviour in a model of osteoarthritis (OA). Osteoarthr. Cartil. 24, 1910–1917. https://doi.org/10.1016/j.joca.2016.06.012 (2016).
Hoshino, T. et al. Persistent synovial inflammation plays important roles in persistent pain development in the rat knee before cartilage degradation reaches the subchondral bone. BMC Musculoskelet. Disord. 19, 11. https://doi.org/10.1186/s12891-018-2221-5 (2018).
Cook, C. S. & Smith, P. A. Clinical update: Why PRP should be your first choice for injection therapy in treating osteoarthritis of the knee. Curr. Rev. Musculoskelet. Med. 11, 583–592. https://doi.org/10.1007/s12178-018-9524-x (2018).
Nie, L. Y., Zhao, K., Ruan, J. Q. & Xue, J. Effectiveness of platelet-rich plasma in the treatment of knee osteoarthritis: A meta-analysis of randomized controlled clinical trials. Orthop. J. Sports Med. 9, 11. https://doi.org/10.1177/2325967120973284 (2021).
Suokas, A. K. et al. Quantitative sensory testing in painful osteoarthritis: a systematic review and meta-analysis. Osteoarthr. Cartil. 20, 1075–1085. https://doi.org/10.1016/j.joca.2012.06.009 (2012).
Li, S. et al. Bone marrow mesenchymal stem cell-derived exosomes shuttling miR-150–5p alleviates mechanical allodynia in rats by targeting NOTCH2 in microglia. Mol. Med. 28, 133. https://doi.org/10.1186/s10020-022-00561-x (2022).
Kraus, V. B. et al. Direct in vivo evidence of activated macrophages in human osteoarthritis. Osteoarthr. Cartil. 24, 1613–1621. https://doi.org/10.1016/j.joca.2016.04.010 (2016).
Pan, T. T., Pan, F., Gao, W., Hu, S. S. & Wang, D. Involvement of macrophages and spinal microglia in osteoarthritis pain. Curr. Rheumatol. Rep. 23, 7. https://doi.org/10.1007/s11926-021-00997-w (2021).
Liu, B. L., Zhang, M. Q., Zhao, J. M., Zheng, M. & Yang, H. Imbalance of M1/M2 macrophages is linked to severity level of knee osteoarthritis. Exp. Ther. Med. 16, 5009–5014. https://doi.org/10.3892/etm.2018.6852 (2018).
Zhang, H. et al. Synovial macrophage M1 polarisation exacerbates experimental osteoarthritis partially through R-spondin-2. Ann. Rheum. Dis. 77, 1524–1534. https://doi.org/10.1136/annrheumdis-2018-213450 (2018).
Chen, O., Donnelly, C. R. & Ji, R.-R. Regulation of pain by neuro-immune interactions between macrophages and nociceptor sensory neurons. Curr. Opin. Neurobiol. 62, 17–25. https://doi.org/10.1016/j.conb.2019.11.006 (2020).
Denk, F., Bennett, D. L. & McMahon, S. B. Nerve growth factor and pain mechanisms. Annu. Rev. Neurosci. 40, 307–325. https://doi.org/10.1146/annurev-neuro-072116-031121 (2017).
Zhang, Q., Bang, S., Chandra, S. & Ji, R. R. Inflammation and infection in pain and the role of GPR37. Int. J. Mol. Sci. https://doi.org/10.3390/ijms232214426 (2022).
Barker, P. A., Mantyh, P., Arendt-Nielsen, L., Viktrup, L. & Tive, L. Nerve growth factor signaling and its contribution to pain. J. Pain Res. 13, 1223–1241. https://doi.org/10.2147/jpr.S247472 (2020).
Takano, S. et al. Nerve growth factor regulation by TNF-αand IL-1βin synovial macrophages and fibroblasts in osteoarthritic mice. J. Immunol. Res. 1–8, 2016. https://doi.org/10.1155/2016/5706359 (2016).
Ashraf, S., Bouhana, K. S., Pheneger, J., Andrews, S. W. & Walsh, D. A. Selective inhibition of tropomyosin-receptor-kinase A (TrkA) reduces pain and joint damage in two rat models of inflammatory arthritis. Arthritis Res. Ther. 18, 11. https://doi.org/10.1186/s13075-016-0996-z (2016).
Araya, N. et al. Intra-articular injection of pure platelet-rich plasma is the most effective treatment for joint pain by modulating synovial inflammation and calcitonin gene-related peptide expression in a rat arthritis model. Am. J. Sports Med. 48, 2004–2012. https://doi.org/10.1177/0363546520924011 (2020).
Giurisato, E. et al. Myeloid ERK5 deficiency suppresses tumor growth by blocking protumor macrophage polarization via STAT3 inhibition. Proc. Natl. Acad. Sci. U. S. A. 115, E2801–E2810. https://doi.org/10.1073/pnas.1707929115 (2018).
Wu, J., Zhao, Y.-M. & Deng, Z.-K. Tangeretin ameliorates renal failure via regulating oxidative stress, NF-κB–TNF-α/iNOS signalling and improves memory and cognitive deficits in 5/6 nephrectomized rats. Inflammopharmacology 26, 119–132. https://doi.org/10.1007/s10787-017-0394-4 (2017).
Zhou, F. et al. Kinsenoside attenuates osteoarthritis by repolarizing macrophages through inactivating NF-κB/MAPK signaling and protecting chondrocytes. Acta Pharm. Sin. B 9, 973–985. https://doi.org/10.1016/j.apsb.2019.01.015 (2019).
Ma, X., Li, X., Ma, L., Chen, Y. & He, S. Soy isoflavones alleviate polycystic ovary syndrome in rats by regulating NF- κB signaling pathway. Bioengineered 12, 7215–7223. https://doi.org/10.1080/21655979.2021.1979864 (2021).
Han, R. et al. Perfluorooctane sulphonate induces oxidative hepatic damage via mitochondria-dependent and NF-κB/TNF-α-mediated pathway. Chemosphere 191, 1056–1064. https://doi.org/10.1016/j.chemosphere.2017.08.070 (2018).
Li, L. et al. Pharmacological inhibition of hmgb1 prevents muscle wasting. Front. Pharmacol. 12, 731386. https://doi.org/10.3389/fphar.2021.731386 (2021).
Acknowledgements
The authors thank Junwei Wang and Tieshan Li for their financial support.
Funding
This work was supported by grants from the National Key Research and Development Program of China (2022YFC2303900 and 2022YFD1301003) and the Natural Science Foundation of Shandong Province (ZR2023MH242).
Author information
Authors and Affiliations
Contributions
JW and TL designed the experiments. JX and XC generated and analyzed the data and drafted the manuscript. XZ and HZ were used for the statistical analysis. RL and XL performed critical analyses of the experiments and results. All the authors have read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Xu, J., Chen, X., Zhang, H. et al. Platelet-rich plasma relieves inflammation and pain by regulating M1/M2 macrophage polarization in knee osteoarthritis rats. Sci Rep 15, 12805 (2025). https://doi.org/10.1038/s41598-025-97501-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-025-97501-6