Abstract
Migraine is a highly prevalent and disabling neurological disorder characterized by abnormal encoding of pain perception, linked to structural and functional abnormalities in the insula. Insular subregions play critical but distinct roles in this process, however, the specific patterns and mechanisms remain elusive in migraineurs. In this study, voxel-based morphometry and seed-based functional connectivity (FC) were employed to investigate structural and functional alterations in insula subdivisions in 44 patients with migraine without aura (MWoA) compared with 51 matched healthy controls. Pain perception was evaluated using the intensity, frequency, and duration of migraine. Compared with healthy controls, patients exhibited(1) reduced gray matter volume in the bilateral dorsal anterior insula (dAI);(2) increased FC between the dAI/posterior insula and bilateral precuneus, the left dAI and left middle temporal gyrus, the left ventral AI and superior/middle frontal gyrus;(3) decreased FC between the left dAI and left middle frontal gyrus, left middle occipital gyrus and right pallidum. Moreover, the left dAI was correlated with the duration and frequency of migraine, the right dAI was correlated with the intensity and duration of migraine. Our results provide novel evidence in support of the insula abnormality hypothesis in migraine and highlight the pivotal role of alterations in the dAI in pain perception in migraineurs.
Similar content being viewed by others
Introduction
Migraine is a neurological disorder affecting up to 15% of the global population characterized by recurring unilateral, throbbing, and pulsating headaches1,2. The suggested mechanism underlying the occurrence of recurrent headaches and sensory amplifications in individuals with migraine is thought to be linked to aberrant pain perception encoding3,4,5. Accumulating evidence indicates that aberrant pain perception in individuals with migraine is closely associated with the dysfunction of the insula6,7. The insula, as the crucial part of the salience network, plays the gatekeeper in detecting and responding to internal and external information8. Its dysfunction may contribute to migraineurs’ perception of pain, including intensity, duration, and frequency by affecting the regions, circuits, and brain networks involved in pain processing9. Nevertheless, the specific neuroimaging mechanisms underlying these effects remain unknown.
Many MRI-based studies have commenced an investigation into alterations in the structure and function of the insula and to elucidate its roles in pain perception in migraineurs. For example, a study derived from a systematic review and meta-analysis of voxel-based morphometric (VBM) has revealed a reduction in gray matter volume (GMV) in the left insula in patients with migraine without aura (MWoA), which in turn affects the descending pain modulation systems10. Evidence from the surface-based morphometry (SBM) analysis also indicates that cortical atrophy occurred in the left insula of patients with migraine without aura11. Moreover, results based on functional imaging imply that the functional abnormalities of the insula in migraineurs are heterogeneous, which is consistent with the finding that there are structural and functional subregions in the insula12,13. For example, Lee et al. found that abnormal function in the posterior part of the insula is associated with impaired habituation to repeated sensory stimulation14. Chen et al. found that abnormalities in the bilateral anterior insula correlated with pain intensity in migraine15. These findings have indicated the specific association between abnormalities in different subregions of the insula in migraineurs and their clinical manifestations. However, the details of these aberrant patterns and their specific contribution to clinical symptoms in MWoA remain unclear. Therefore, it is urgent to comprehensively analyze the structural and functional abnormalities of the insula subregions in migraine patients and their contributions to clinical symptoms.
In the current study, we combined structural and functional analyses to investigate the aberrant patterns of the insula in migraineurs and to further assess the contribution of these changes to the clinical symptoms of pain perception in migraineurs. We hypothesized that structural and functional changes in the insula may vary across subdivisions or subcircuits and may play a unique role in the pain perception of migraine.
Materials and methods
Study design and participants
This study was registered in the Chinese Clinical Trial Registry (registration number: ChiCTR2000032308) and was approved by the Sichuan Regional Ethics Review Committee on Traditional Chinese Medicine (TCM; ethical approval number: 2020KL-003). This study was conducted in accordance with the Declaration of Helsinki (World Medical Association, 2013). Voluntary written informed consent was obtained from each subject after verbal and written explanations of the study.
All patients were independently diagnosed by the physician of neurology according to the ICHD III criteria16 (Headache Classification Committee of the International Head 2018) and Inclusion criteria were as follows:(1) 18–50 years old, right-handed;(2) fulfilling criteria for MWoA;(3) history of MWoA for 12 months or more;(4) did not receive preventive treatment within the last 3 months; and(5) no long-term use of analgesics. Patients and healthy controls with any of the following conditions were excluded:(1) macroscopic T2-visible brain lesions on MRI scans;(2) existence of additional psychiatric or neurological disorders;(3) taking any drugs affecting the central nervous system;(4) current or previous antipsychotic medication, immunodeficiency, bleeding disorders, or allergies;(5) MRI contraindications or claustrophobia; and(6) alcohol or drug abuse. For the healthy control (HC), they should either have no personal or family history of migraine or other headaches.
A total of fifty patients with MWoA were recruited from the outpatient clinic of the Departments of Neurology in two clinical centers:(1) the Hospital of Chengdu University of TCM; and(2) Sichuan Provincial People’s Hospital. Patients were enrolled in the study from May 2020 to December 2022. A total of fifty-three age-, gender-, and education- matched healthy controls were recruited from Chengdu University of TCM and communities in Chengdu. Clinical data evaluation and magnetic resonance imaging were performed on all the patients and HC was finally included. The flowchart and quality control of this study are shown in Fig. 1.
Clinical data collection
The age, weight, and height of the participants were recorded as demographic information. Before the magnetic resonance imaging (MRI) scan, it was confirmed that the recruited participants would complete a one-month headache diary, which included the pain perception items such as the frequency of migraine, the duration of each attack (hours) and the Visual Analogue Scale (VAS: 0 cm to 10 cm). The average scores of each item were used in the following analyses. All clinical characteristics of patients with MWoA were assessed according to the International Headache Society (IHS) Guidelines for Migraine Clinical Trials.
Magnetic resonance imaging data acquisition
All participants were scanned in the Hospital of Chengdu University of Traditional Chinese Medicine, China (GE Discovery MR750 3.0 T system). Patients with MWoA in this study were in their interval of migraine period and had been migraine-free for at least 24 h before the MRI scan. After scanning, all participants reported being awake and free of any headaches or migraine.
All subjects were instructed to rest with their eyes closed, not to think of anything, and not to fall asleep during the scan. The following parameters were used for high-resolution T1 weighted volumetric 3D images axially: repetition time/echo time (TR/TE) = 1900/2.26 ms, matrix = 256 × 256, flip angle = 9°, voxel size = 1 × 1 × 1 mm3 and 176 slices without interslice gap. Functional images were collected transversely using an echo-planar imaging sequence with the following settings: TR/TE = 2000 ms/30 ms, flip angle = 90°, 32 slices, 64 × 64 matrix, field of view = 240 × 240 mm2, interslice gap = 0 mm, and voxel size = 3.75 × 3.75 × 5 mm3. For each subject, 180 functional volumes were obtained. If a patient experienced a migraine attack during the scanning process, the scanning was stopped immediately, and the scanning time was postponed.
Data analyses
Definition of Insula subdivision
Three bilateral insula subdivisions were defined from a seminal study by Deen et al. who parcellated the human insula lobe based on the clustering of functional connectivity patterns17. Cluster analysis revealed 3 subregions of the insula for both left and right hemispheres: ventral anterior insula (vAI, mean coordinates, left: MNI = -33 13 − 7; right: MNI = 32 10 − 6), dorsal anterior insula (dAI, mean coordinates, left: MNI = -38 6 2; right: MNI = 35 6 2), and posterior insula (PI, mean coordinates, left: MNI = -38 -6 5; right: MNI = 35 − 11 6). The boundaries between the 3 bilateral insula regions have been described by Deen et al. and shown in Fig. 2. The left and right insula were defined anatomically by drawing insular gray matter on the Montreal Neurological Institute (MNI) 152 standard brain. The limits of the insula were taken to be the anterior, superior, and inferior per-insular sulci. These regions of interest (ROIs) were converted to Talairach space by normalizing the MNI brain in the same way that individual subject anatomical images were normalized.
The mean gray matter volume and time series of all voxels in the insula subdivisions were regarded as seeds for the subsequent structural and FC analysis in HC and MWoA groups.
Gray matter volume analysis
The VBM8 toolbox (http://dbm.neuro.uni-jena.de/vbm8) implemented in the SPM8 (http://www.fil.ion.ucl.ac.uk/spm) was employed to preprocess the structural T1-weighted images. First, all images were visually checked for artifacts and manually reoriented to set the image origin at the anterior commissure. Second, the images of each participant were normalized to the standard Montreal Neurological Institute template by using an affine followed by nonlinear transformation and resampled to 1.5 mm × 1.5 mm × 1.5 mm. Third, the normalized images were segmented into gray matter, white matter, and cerebral spinal fluid maps. The data quality of the segmented maps was checked. Fourth, each map of GM is modulated using the Jacobian modulation to obtain voxel-wise gray-matter volume maps. Finally, gray matter maps were smoothed with an isotropic Gaussian kernel (full width at half maximum = 6 mm). The smoothed gray matter images were subjected to the following analyses18.
Two-sample t-tests were used to assess the abnormal gray matter volume (GMV) of subregions in the insula in MWoA with the whole brain volume, age, and gender as covariates of no interest, compared with the HC group. The significance of group differences was set at P < 0.05 using the Gaussian random field (GRF) correction (voxel, P < 0.005; cluster, P < 0.05). Finally, brain regions showing significant differences based on the results of two-sample t-testing were defined as ROIs for correlation analysis. ROIs were defined as 8-mm spheres centered at the position of peak statistical difference. We extracted the average voxel-wise GMV of ROIs with significant differences and performed Pearson correlation analysis with the patient’s clinical symptoms using SPSS 22.0. Age and gender were controlled as covariates. The significance threshold was set at P < 0.05.
fMRI data analysis
Image preprocessing
Resting-state fMRI images were preprocessed using the toolbox for Data Processing &Analysis of Brain Imaging (DPABI, http://rfmri.org/DPABI). The first 5 volumes were discarded to avoid the nonequilibrium effects of magnetization, and slice timing and realignment correction were performed for the remaining images. Any participant with maximum head movement greater than 2.5 mm translation or more than 2.5° rotation was not included. Data were further normalized to the EPI template (resampled voxel size of 3 mm × 3 mm × 3 mm). Then, several covariates including Fristion 24 motion parameters, the global signal, the cerebrospinal fluid, and white matter signals were regressed as nuisance variables to reduce spurious variance. Afterward, detrending and band-pass filtering (0.01–0.08 Hz) were conducted. Finally, given that resting-state activity is sensitive to minor head movement, we calculated the mean frame-wise displacement (FD) to further determine the comparability of head movement across groups. “Bad” time points (FD > 0.5 mm), as well as their 1-back and 2-forward time points, were then scrubbed and interpolated by spline interpolation19.
FC analysis
To identify the abnormal subsystems of the insula in patients with MWoA compared HC group. FC analysis was carried out using the average time course obtained from the seed, and correlation analysis was then performed in a voxel-wise manner using the gray mask of the Anatomical Automatic Labeling template. The correlation coefficients were converted into z-values using Fisher’s r-to-z transformation. Contrast images were generated for each subject by estimating the regression coefficient between all brain voxels and each seed time series. A comparison of FC between the groups was performed using a two-sample t-test in SPM, with age and gender as covariates. Multiple comparisons correction was performed using a Gaussian random field at P < 0.05 (voxel, P < 0.005; cluster, P < 0.05).
Finally, brain regions showing significant differences based on the results of two-sample t-testing were defined as ROIs for correlation analysis. ROIs were defined as 6-mm spheres centered at the position of peak statistical difference. We extracted the average z-values for ROIs with significant differences and performed Pearson correlation analysis with the patient’s clinical symptoms using SPSS 22.0. Age and gender were controlled as covariates. The significance threshold was set at P < 0.05.
Results
After screening 110 participants, four participants were excluded due to failure to meet the inclusion or exclusion criteria, and eight participants (two in the HC group, and six in the MWoA group) were excluded due to head motion and missing data acquisition. Overall, 95 participants (51 in the HC group and 44 in the MWoA group) were included in the final analysis (Fig. 1).
Demographics and clinical symptoms
There was no statistically significant variation between HCs and patients with MWoA regarding baseline characteristics (age, gender, height and weight, P > 0.05, Table 1). Besides, there was no significant difference in the FD between MWoA and HC groups (HC: 0.09 ± 0.04; MWoA: 0.12 ± 0.03; mean ± SD, P = 0.43).
Pa-value was obtained by two-sample t-test. Pb-value was obtained by χ2 two-tailed test. HC, healthy controls; MWoA, patients with migraine without aura; SD, standard deviation; VAS, visual analog scale.
Voxel-based morphometry results
VBM analysis revealed region-specific abnormal GMV of the insula in the patients with MWoA, compared with the HC group (Fig. 2). The patients with MWoA only showed significantly reduced GMV in the dAI, though other subregions also showed a trend of reduction. Gaussian random field correction theory was employed to correct multiple comparisons (voxel P < 0.005, cluster P < 0.05, cluster size > 50 voxels) (in Fig. 2). The decreased GMV in the right dAI was significantly inversely correlated with the duration of each attack in the MWoA group.
Structural alteration of the insula in patients with MWoA compared with HC. Gaussian random field method was used for significance correction with voxel P < 0.005, cluster P < 0.05, cluster size > 50 voxels. The deeper red color represents the greater decreased GMV and the lighter red color represents less decreased GMV in the MWoA compared with HC. In the box plot, the red color represents the MWoA group, and the green color represents the HC group. MWoA, patients with migraine without aura; HC, healthy control; GMV, gray matter volume; vAI.L, left ventral anterior insula; vAI.R, right ventral anterior insula; dAI.L, left dorsal anterior insula; dAI.R, right dorsal anterior insula; PI.L, left posterior insula; PI.R, right posterior insula.
FC results
The functional topographic distribution of Insula subdivisions in the MWoA and HC groups
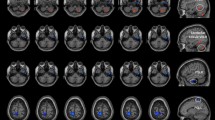
Figure 3 shows the distribution of the FC in insula subdivisions in patients with MWoA and HC, respectively. The vAI is mainly functionally connected with the other parts of the insula, middle and inferior frontal gyrus, superior temporal gyrus, anterior cingulate, and temporoparietal junction in both MWoA and HC groups. The dAI is mainly functionally connected with the other parts of the insula, parietal gyrus, dorsal cingulate, superior frontal gyrus, and temporoparietal junction in both MWoA and HC groups. The PI is mainly functionally connected with the sensorimotor cortex and dorsolateral frontal cortex in both MWoA and HC groups. Gaussian random field correction theory was employed to correct multiple comparisons (voxel P < 0.005, cluster P < 0.05, cluster size > 50 voxels) (In Table 2; Fig. 3).
The functional topographic distribution of insula subdivisions in the MWoA and HC groups respectively. Gaussian random field method was used for significance correction with voxel P < 0.005, cluster P < 0.05, cluster size > 50 voxels. The deeper black color represents the lower FC and the lighter yellow color represents the higher FC with the insula subdivisions in the MWoA and HC groups. In the ROIs plot, the cyan color represents the ventral anterior insula, the yellow color represents the dorsal anterior insula and the dark red color represents the posterior insula. MWoA, patients with migraine without aura; HC, healthy control; GMV, gray matter volume; vAI.L, left ventral anterior insula; vAI.R, right ventral anterior insula; dAI.L, left dorsal anterior insula; dAI.R, right dorsal anterior insula; PI.L, left posterior insula; PI.R, right posterior insula.
Between-group differences in FC of the Insula subregions between MWoA and HC groups
Inter-group comparisons on the FC maps revealed decreased FC between the left vAI and left posterior insula, the left dAI and right dorsal insula, the left ventral insula and pallidum, the right dAI and left dorsal insula as well as left middle occipital, the left PI and right posterior insula in MWoA compared with HC. Increased FC between the left vAI to superior and middle frontal gyrus, the right vAI to superior frontal gyrus and middle frontal gyrus, the left dAI to bilateral precuneus and middle temporal gyrus, the right dAI and bilateral precuneus, the left PI and right precuneus in MWoA, compared with HC (in Table 2and Fig. 4). Gaussian random field correction theory was employed to correct multiple comparisons (voxel P < 0.005, cluster P < 0.05, cluster size > 55 voxels). The underlying insula-related circuits of the hyperexcitable brain in patients with MWoA are shown in Fig. 4.
Group differences in FC of insula subdivisions between MWoA and HC. The warm color represents the increased FC and the cool color represents decreased FC with the insula subdivisions in the MWoA compared with the HC group. MWoA, patients with migraine without aura; HC, healthy control; vAI.L, left ventral anterior insula; vAI.R, right ventral anterior insula; dAI.L, left dorsal anterior insula; dAI.R, right dorsal anterior insula; PI.L, left posterior insula; PI.R, right posterior insula.
Patterns of aberrant FC in insula subregions in patients with MWoA. The green color line denotes the normal connectivity of insula subregions in the HC group. The blue color line denotes decreased FC in MWoA compared with the HC group. The brown color line denotes increased FC in MWoA compared with the HC group. vAI, ventral anterior insula; dAI, dorsal anterior insula; PI, posterior insula; MFG, middle frontal gyrus; SFG, superior frontal gyrus; PAI, pallidum; MTG, middle temporal gyrus, MOG, middle occipital gyrus; PCUN, precuneus; HC, healthy control; MWoA, patients with migraine without aura; L, left; R, right.
Relationships between the structural and functional changes in Insula subregions and clinical symptoms in MWoA
To test the relationship between the changes in structure and function in insula subdivisions and the clinical symptoms, a correlation analysis was conducted. With the increased duration of each attack, the GMV of the dAI is reduced more in MWoA (Fig. 2). We found that with the increased duration of each attack and frequency of migraine, the left dAI seed showed decreased FC with right pallidum (Fig. 6A, B); with increased duration of each attack, the right dAI seed showed increased FC with left precuneus in MWoA (Fig. 6, C); with increased VAS scores the right dAI seed showed increased FC with right middle temporal gyrus in MWoA (Fig. 6, D).
Discussion
The present study combined structural and functional MRI to elucidate the underlying neuroimaging mechanisms of aberrant pain perception in MWoA by assessing the alterations in insula subregions. First, patients exhibited a markedly reduced GMV, predominantly in the bilateral dAI in MWoA. Second, the functional topography of the insula subregions exhibited consistent three-subsystem organization, replicating the findings of the previous study: the vAI-pregenual anterior cingulate cortex subsystem, the dAI-dorsal anterior cingulate cortex and executive control subsystem, and the PI-primary secondary somatomotor cortex subsystem. Third, patients exhibited dysconnectivities among the DMN, salience network (SN) and basal ganglia, including increased FC between the dAI/PI and posterior DMN, the left dAI and middle of DMN, the left vAI and anterior DMN; and decreased FC between the left dAI and anterior DMN as well as basal ganglia compared with HC. Finally, the loss of GMV and changed FC in dAI were significantly correlated to the intensity, frequency, and duration of headaches in MWoA. Our findings provide more detailed structural and functional evidence in support of the insula abnormality hypothesis in migraine and highlight the strong association between the alteration of dAI and abnormal pain perception in migraineurs.
Alteration in GMV of the Insula in MWoA
In this study, we observed a reduction of GMV in the bilateral dAI, but not in the other subregions of the insula. This finding is consistent with the results of the previous study, which indicated that a reduction of GMV in the insular is an important biomarker for migraine10,20,21,22. Nevertheless, there is a paucity of reports concerning structural abnormalities in the insula subregions. Moreover, the evidence derived from the white matter fibers indicates that the insula can be broadly divided into two distinct parts: the anterior insula, which is closed to the limbic and paralimbic systems, as well as portions of the inferior frontal gyrus, and the posterior part, which is in contact with the parietal and posterior temporal lobes23. Further studies utilizing cellular constructs have demonstrated that the insula can be subdivided into three distinct subnuclei: ventral, dorsal and posterior24. These findings indicate that there are structural differences between the respective subregions. Our findings confirm the reduction of the insula GMV and provide detailed evidence that this reduction is mainly located in dAI in MWoA. The identification of the precise location of abnormalities in GMV within the insula may assist in elucidating the pathogenesis of migraine and the development of targeted treatments for the disease25,26,27,28. It is noteworthy that the connections between the left and right sides of the dAI were also partially biased, with the left dAI exhibiting stronger connections to areas of the language network and the DMN, while the right dAI demonstrated stronger connections to regions of the attention network and executive control network29. Further investigation of the patterns of functional alterations and their correlation with clinical symptoms will facilitate a more profound comprehension of the underlying mechanisms of migraine.
Abnormal FC amongst Insula subregions, DMN and basal ganglia in MWoA
The current study demonstrated increased FC between the left dAI and middle of DMN (left middle temporal gyrus), the left vAI and anterior DMN (superior and middle frontal gyrus), while decreased FC between the left dAI and anterior DMN (middle frontal gyrus) compared with HC. These findings are consistent with those of previous studies, which demonstrated a correlation between the processing/encoding of pain and the DMN and SN. However, Coppola et al. observed an increased FC between the anterior DMN (middle frontal gyrus) and bilateral insula in individuals experiencing acute migraine headaches30, while Tian et al. found decreased FC between the left insula and DMN (superior frontal gyrus)31. The disparate findings are most likely attributable to the functional heterogeneity of the insula subregions20,32,33,34,35. Our results elucidate the connectivity patterns between the insula and the DMN in MWoA, indicating that the increased FC was between the left vAI/dAI and the anterior DMN, while the decreased FC was between the left dAI and the anterior DMN. Meanwhile, studies that focused on patients with migraine with aura revealed a stronger functional connectivity (FC) between the insula and the cerebellum36, however, this was not observed in our study. This inconsistent result may be attributable to discrepancies in the selected samples. Previous studies have corroborated the existence of differential insula connectivity patterns between migraine with and without aura, with a notable distinction observed in the right insula37,38. Moreover, our findings revealed an enhanced FC between the dAI/PI and posterior DMN (bilateral precuneus), while decreased FC between the dAI and basal ganglia (pallidum) in MWoA. This finding further clarifies the pattern of connectivity in insula subregions and implies that the insula may be involved in the descending pain pathway by influencing the basal ganglia39. These findings reveal the abnormal pattern of connectivity between the insula subregions and DMN, basal ganglia in migraineurs and provide new perspectives for elucidating the mechanisms of migraine.
Association between dAI-related alteration and pain perception in MWoA
We performed a correlation analysis to further elucidate the association between the alteration of insula subregions and pain perception in MWoA. The results of the structural analyses indicated that the reduction of GMV in the left dAI was inversely correlated with the duration of each attack in MWoA. The results of the functional analyses indicated that FC between the left dAI and the pallidum was significantly inversely associated with the duration and frequency of the headache, while FC between the left dAI and middle temporal gyrus was significantly positively related to the duration of each attack in MWoA. These findings are in line with those of our previous studies, which indicated that alterations in the pallidum, middle temporal gyrus and insula are associated with migraine40,41. The pallidum is a constituent part of the basal ganglia and is connected with the cortical areas and the corpus striatum. Its functions include the control of movement, motivation, cognition, and the delivery of neurotransmitters. Its dysfunction is purported to be associated with the frequency of migraine42. The middle temporal gyrus, as a crucial component of DMN, plays a pivotal role in the processing of pain perception, pain emotion, and pain cognition10,43. Some studies have proposed that it may contribute to the prolongation of migraine attacks through altered connectivity with the insula, thalamus and other regions44,45,46. These results provide further clarification regarding the brain regions and patterns involved in the frequency and duration of pain in MWoA. Moreover, FC between the right dAI and precuneus was positively correlated with the VAS scores. The precuneus is a pivotal region of posterior DMN, involved in the integration of sensory information. Its connection with the regions responsible for pain processing and modulation, such as the insula, may influence the perception of pain intensity in migraine47,48. These findings expand our understanding of pain perception abnormalities in migraineurs. Specifically, they indicate that the frequency and duration of pain are associated with enhanced connectivity of the left dAI to the middle of the DMN and reduced connectivity to the basal ganglia. Conversely, the intensity of pain is associated with enhanced connectivity of the right dAI to the posterior DMN.
Conclusions
In conclusion, the current study elucidates the structural and functional abnormalities in the insula subregions in migraine and further reveals the specific association between the abnormal functional connectivity in the insula subregions and the frequency, duration and intensity of pain in migraine patients. Our results support the hypothesis of insular abnormalities in migraines and reveal the potential contribution of the abnormal connectivity between subregions of the insula and DMN, basal ganglia network to the altered pain perception in migraineurs.
Several limitations of the current study must be noted. First, although there is no significantly statistical difference in the male-female ratios between the MWoA group and the control group, an imbalance still exists. The impact of gender should be considered in future studies. Second, the sample size used in this study is relatively small, which limits the statistical power of our results. The small sample size weakens the correlation in this paper, which also limits the reliability of the research results. In the future, a larger sample size is necessary to confirm the results of the current study. Third, in this study, indicators related to the menstrual cycle and estrogen were not collected. These factors may affect the structural and functional changes in patients with migraine. In future studies, we will optimize the experimental design to clarify the possible impacts.
Data availability
The data and summary statistics of migraine are available by contacting the authors of the corresponding author.
References
Mokdad, A. H. GBD 2016 headache collaborators. global, regional, and National burden of migraine and tension-type headache, 1990–2016: a systematic analysis for the global burden of disease study 2016 (17, Pg 954, 2018). Lancet Neurol. 20 (2021), E7–E (2021).
Stovner, L. J. et al. Global, regional, and national burden of migraine and tension-type headache, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol. ;17(2018):954 – 76. (2018).
Russo, A. et al. Pain Perception and Migraine. Frontiers in neurology. ;9(2018):576. (2018).
Suryavanshi, P., Sawant-Pokam, P., Clair, S. & Brennan, K. C. Increased presynaptic excitability in a migraine with aura mutation. Brain 147 (2023), 680–697 (2023).
Geha, P. & Waxman, S. G. Pain perception: multiple matrices or one?? JAMA Neurol. 73 (2016), 628–630 (2016).
Vecchia, D. & Pietrobon, D. Migraine: a disorder of brain excitatory-inhibitory balance? Trends Neurosci. 35 (2012), 507–520 (2012).
Maizels, M., Aurora, S. & Heinricher, M. Beyond neurovascular: migraine as a dysfunctional neurolimbic pain network. Headache 52 (2012), 1553–1565 (2012).
Molnar-Szakacs, I. & Uddin, L. Q. Anterior insula as a gatekeeper of executive control. Neuroscience and biobehavioral reviews. ;139(2022):104736. (2022).
Zhang, M. M. et al. Glutamatergic synapses from the insular cortex to the basolateral amygdala encode observational pain. Neuron 110 (2022), 1993–2008e6 (2022).
Zhang, X. et al. A systematic review and meta-analysis of voxel-based morphometric studies of migraine. J. Neurol. 270 (2023), 152–170 (2023).
Zhang, S., Liu, W., Li, J. & Zhou, D. Structural brain characteristics of epilepsy patients with comorbid migraine without aura. Scientific Reports. ;14(2024):21167. (2024).
McBenedict, B. et al. The role of the Insula in chronic pain and associated structural changes: an integrative review. Cureus 16 (2024), e58511 (2024).
Gollion, C. et al. Insular functional connectivity in migraine with aura. J. Headache Pain. 23 (2022), 106 (2022).
Lee, J. et al. Reduced insula habituation associated with amplification of trigeminal brainstem input in migraine. Cephalalgia: an international journal of headache. ;37(2017):1026-38. (2017).
Chen, H. et al. Altered Dynamic Amplitude of Low-Frequency Fluctuations in Patients With Migraine Without Aura. Front Hum Neurosci. ;15(2021):636472. (2021).
Olesen, J. Headache Classification Committee of the International Headache Society (IHS) The International Classification of Headache Disorders, 3rd edition. Cephalalgia. ;38(2018):1-211. (2018).
Deen, B., Pitskel, N. B. & Pelphrey, K. A. Three systems of insular functional connectivity identified with cluster analysis. Cereb. Cortex. 21 (2011), 1498–1506 (2011).
John, A. & Karl, J. F. Voxel-Based Morphometry—The Methods. NeuroImage. ;11(2000):805 – 21. (2000).
Power, P. JD, BarnesKA, SnyderAZ, SchlaggarBL & PetersenSE Spurious but systematic correlations in functional connectivity MRI networks arise from subject motion (59, Pg 2142, 2012). Neuroimage 63 (2012), 999 (2012).
Borsook, D. et al. The Insula: A hub of activity in migraine. Neuroscientist: Rev. J. Bringing Neurobiol. Neurol. Psychiatry. 22 (2016), 632–652 (2016).
Valfre, W., Rainero, I., Bergui, M. & Pinessi, L. Voxel-based morphometry reveals Gray matter abnormalities in migraine. Headache 48 (2008), 109–117 (2008).
Dai, Z. et al. Gray matter correlates of migraine and gender effect: A Meta-Analysis of Voxel-Based morphometry studies. Neuroscience 299 (2015), 88–96 (2015).
Cerliani, L. et al. Probabilistic tractography recovers a rostrocaudal trajectory of connectivity variability in the human insular cortex. Hum. Brain Mapp. 33 (2012), 2005–2034 (2012).
Kittleson, A. R., Woodward, N. D., Heckers, S. & Sheffield, J. M. The insula: Leveraging cellular and systems-level research to better understand its roles in health and schizophrenia. Neuroscience and biobehavioral reviews. ;160(2024):105643. (2024).
Puledda, F. et al. Abnormal glutamatergic and serotonergic connectivity in visual snow syndrome and migraine with aura. Ann. Neurol. 94 (2023), 873–884 (2023).
Li, Y. et al. Alleviation of migraine related pain and anxiety by inhibiting calcium-stimulating AC1-dependent CGRP in the Insula of adult rats. J. Headache Pain. 25 (2024), 81 (2024).
Onay, A., Eser, H. Y., Ulasoglu-Yildiz, C., Aslan, S. & Tali, E. T. A combined VBM and DTI study of schizophrenia: bilateral decreased insula volume and cerebral white matter disintegrity corresponding to subinsular white matter projections unlinked to clinical symptomatology. Diagn Interv Radiol. ;23(2017):390-7. (2017).
Ceko, M., Seminowicz, D. A., Bushnell, M. C. & Olausson, H. W. Anatomical and functional enhancements of the Insula after loss of large primary somatosensory fibers. Cereb. Cortex. 23 (2013), 2017–2024 (2013).
Wang, Y. et al. Frequency dependent hub role of the dorsal and ventral right anterior Insula. Neuroimage 165 (2018), 112–117 (2018).
Coppola, G. et al. Resting state connectivity between default mode network and Insula encodes acute migraine headache. Cephalalgia 38 (2018), 846–854 (2018).
Tian, Z. L. et al. The Altered Functional Connectivity With Pain Features Integration and Interaction in Migraine Without Aura. Frontiers in Neuroscience. ;15(2021). (2021).
Kurth, F., Zilles, K., Fox, P. T., Laird, A. R. & Eickhoff, S. B. A link between the systems: functional differentiation and integration within the human Insula revealed by meta-analysis. Brain Struct. Funct. 214 (2010), 519–534 (2010).
Fu, T. et al. Cerebral blood flow alterations in migraine patients with and without aura: An arterial spin labeling study. J Headache Pain. ;23(2022). (2022).
Tso, A. R., Trujillo, A., Guo, C. C., Goadsby, P. J. & Seeley, W. W. The anterior Insula shows heightened interictal intrinsic connectivity in migraine without aura. Neurology 84 (2015), 1043–1050 (2015).
Niddam, D. M. et al. Reduced functional connectivity between salience and visual networks in migraine with aura. Cephalalgia. ;36(2016):53–66. (2016).
Gollion, C. et al. Insular functional connectivity in migraine with aura. J Headache Pain. ;23(2022). (2022).
Lo Buono, V. et al. Functional connectivity and cognitive impairment in migraine with and without aura. J Headache Pain. ;18(2017):72. (2017).
Faragó, P. et al. Interictal brain activity differs in migraine with and without aura: resting state fMRI study. J Headache Pain. ;18(2017):8. (2017).
Hazra, S. et al. A dysfunctional descending pain modulation system in chronic nonspecific low back pain: A systematic review and ALE Meta-Analysis. Neurol. India. 70 (2022), 1344–1360 (2022).
Yu, D. H., Yuan, K., Zhao, L., Liang, F. R. & Qin, W. Regional Homogeneity Abnormalities Affected by Depressive Symptoms in Migraine Patients without Aura: A Resting State Study. PLoS One. ;8(2013). (2013).
Gao, Q. et al. Decreased functional connectivity density in pain-related brain regions of female migraine patients without aura. Brain Res. 1632 (2016), 73–81 (2016).
d’Onofrio, F. et al. Migraine and movement disorders. neurological sciences: official journal of the Italian neurological society and of the Italian society of clinical neurophysiology. ;33 Suppl 1(2012):S55–S59. (2012).
Coppola, G. et al. Clinical neurophysiology of migraine with aura. J Headache Pain. ;20(2019):42. (2019).
Du, J., Liu, Y. & Zhu, W. The altered functional status in vestibular migraine: A meta-analysis. Brain Behav. ;14(2024):e3591. (2024).
Qin, Z. et al. Disrupted functional connectivity between sub-regions in the sensorimotor areas and cortex in migraine without aura. The Journal of Headache and Pain. ;21(2020):47. (2020).
Xu, J. et al. Delineating functional segregations of the human middle temporal gyrus with resting-state functional connectivity and coactivation patterns. Hum Brain Mapp. ;40(2019):5159-71. (2019).
Wang, Z. W. et al. Brain structural and functional changes during menstrual migraine: Relationships with pain. Frontiers in molecular neuroscience. ;15(2022):967103. (2022).
Meylakh, N. & Henderson, L. A. Exploring alterations in sensory pathways in migraine. J Headache Pain. ;23(2022):5. (2022).
Acknowledgements
We would like to thank all participants who participated in this study.
Funding
This work was supported by the National Natural Science Foundation of China (Grant No. 82204919, 82430124, 81973962, 82274664), China Postdoctoral Science Foundation (Grant No. 2022MD713681), the Department of Science and Technology of Sichuan Province (2024YFFK0168).
Author information
Authors and Affiliations
Contributions
L. Z, D. L. and X. L. designed the study and conceptualized the protocol for healthy subjects. Yt. Z., X. ouy, Z. W. adapted this protocol for patients with migraines without aura and evaluated them. H. L., W. Q., Y. Z., X. M. and Lc. Z. managed the literature searches and analyses. Z. Z. and X. G. undertook the statistical analyses, X. W. wrote the first draft of the manuscript. All authors contributed to and have approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All participants provided informed consent. This study was approved by the Sichuan Regional Ethics Review Committee on Traditional Chinese Medicine (TCM; ethical approval number: 2020KL-003).
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, X., Gao, X., Ouyang, X. et al. Structural and functional changes of insula subregions in migraine without aura and their relationships with pain perception. Sci Rep 15, 13342 (2025). https://doi.org/10.1038/s41598-025-98193-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-98193-8
Keywords
This article is cited by
-
Subcortical nuclei and glymphatic system alterations in migraine with aura: a comparative 7T multimodal MRI analysis
The Journal of Headache and Pain (2025)
-
Enhanced interhemispheric functional connectivity in patients with functional anorectal pain
Scientific Reports (2025)