Abstract
Congenital heart block (CHB) is the most high-risk and prognosis-poor phenotype of neonatal lupus erythematosus (NLE). This study aimed to investigate the clinical characteristics of NLE patients complicated by CHB. This was a multi-center retrospective study. Data were retrospectively collected from NLE patients diagnosed between January 1, 2011, and December 31, 2023, at the Affiliated Children’s Hospital of Soochow University, the Affiliated Suzhou Hospital of Nanjing Medical University, Yangzhou Maternity and Child Health Care Hospital, and Huai’an Maternity and Child Health Care Hospital. The patients were divided into CHB and non-CHB groups based on the presence or absence of CHB. Clinical data were compared between the two groups, and logistic regression analysis was performed to identify risk factors associated with CHB. The outcomes of patients in the CHB group were determined through follow-ups. Ninety-one NLE patients were included, with 15 cases complicated by CHB. Among the CHB patients, five had third-degree CHB (5.49%), four had second-degree CHB (4.40%), and six had first-degree CHB (6.59%). The CHB group had significantly higher levels of maternal allergic diseases and double-positive anti-SSA and anti-SSB antibodies compared with the non-CHB group, as well as higher serum levels of creatine kinase (CK), lactate dehydrogenase, and hydroxybutyrate dehydrogenase. Multivariate logistic regression analysis indicated that high serum CK levels predicted CHB in NLE patients. The most common organ involvement in the CHB group was hematologic, followed by the skin, structural heart abnormalities, digestive, and central nervous systems. However, no significant differences were observed between the two groups. In the CHB group, other symptoms resolved spontaneously within the first 2 years of life, and pacemaker implantation was performed in four patients with third-degree CHB at around 1 year of age. Elevated serum CK levels may indicate CHB in NLE patients. Hematologic involvement was most common in NLE patients with CHB. Pacemaker implantation was shown to effectively treat patients with third-degree CHB.
Similar content being viewed by others
Introduction
Neonatal lupus erythematosus (NLE) is an acquired autoimmune disorder where maternal autoantibodies pass through the placenta and bind to fetal antigens, causing tissue damage in the fetus or neonate1. The symptoms are typically temporary and improve once the antibodies are cleared2,3. Congenital heart block (CHB) is the most severe and life-threatening complication of NLE, but it is usually irreversible. CHB most frequently manifests between the 18th and 26th weeks of gestation. Severe cases of CHB may present in utero as fetal bradycardia, characterized by a normal atrial rate and a ventricular rate ranging from 40 to 80 beats per minute. The postnatal manifestations typically include sinus bradycardia and prolonged QT interval. These patients often require pacemaker implantation within the first year of life. The incidence of third-degree CHB is about 2%, with a mortality risk of 15–20%4,5,6. Although some reports on NLE-related CHB have been published, systematic studies are limited. Case reports and research on NLE complicated by CHB in China are also lacking.
Thus, this study aimed to retrospectively analyze the clinical data of NLE patients from four hospitals. The purpose was to investigate the clinical characteristics of NLE patients with CHB and provide long-term follow-up on their outcomes. This study intended to raise clinical awareness and offer valuable insight for the early diagnosis and management of such cases.
Methods
Study population and groups
This was a multi-center retrospective study. The study subjects were children diagnosed with NLE who were hospitalized at the Affiliated Children’s Hospital of Soochow University, the Affiliated Suzhou Hospital of Nanjing Medical University, Yangzhou Maternity and Child Health Care Hospital, and Huai’an Maternity and Child Health Care Hospital from January 1, 2011, to December 31, 2023. The study was approved by the Ethics Committee of the Children’s Hospital of Soochow University (2023CS024; Suzhou, China). The requirement for informed consent was waived by the Ethics Committee of the Children’s Hospital of Soochow University. All study procedures were performed according to the ethical standards in the Declaration of Helsinki.
The inclusion criterion was children who met the diagnostic criteria for NLE, as assessed by a duo of neonatologists and rheumatologists, based on the diagnostic standards of the American College of Rheumatology7. The exclusion criteria were: (1) the presence of severe congenital malformations of vital organs, chromosomal abnormalities, or genetic metabolic diseases; (2) a significant lack of clinical data that could lead to bias in the study results; and (3) refusal to participate in the study by the family.
The NLE patients were divided into the CHB group and the non-CHB group based on whether they met the inclusion criteria and had CHB. Clinical data between the two groups were compared, and the outcomes of the CHB patients were determined through outpatient visits and telephone follow-ups. Follow-up assessments are conducted monthly for infants up to 1 year of age and every 2–3 months thereafter. The primary focus was monitoring CHB-related symptoms in neonates with NLE and documenting the recovery status of other affected organs. Particular attention was paid to the progression of CHB-related symptoms and subsequent treatment outcomes.
Definitions and diagnostic criteria
The diagnosis of NLE was based on the criteria proposed by the American College of Rheumatology8, primarily referring to the presence of positive serum anti-SSA /SSB/U1RNP antibodies in mothers with autoimmune diseases and/or neonates exhibiting clinical manifestations of NLE. NLE was determined jointly by rheumatology and neonatology specialists. The diagnostic criteria for CHB related to NLE were based on those proposed by Pilar Brito-Zerón et al.9, specifically referring to the transplacental transfer of maternal autoantibodies to the fetal heart, leading to atrioventricular signal conduction block. CHB was classified into first through third degrees according to the involvement of the cardiac conduction system. Parental allergic diseases and maternal autoimmune diseases were confirmed through diagnoses made in the hospitals to minimize selection bias.
Data collection
This study involved reviewing patients’ electronic medical records and collecting data through outpatient visits and telephone follow-ups. Relevant data were extracted through outpatient visits and telephone surveys and used for further investigations. The data collected from electronic medical records included general information on the patients, family history of allergic diseases, maternal history of autoimmune diseases, clinical manifestations of the patients, laboratory test results, and imaging findings. General information on the patients included the delivery method, gender, gestational age, and birth weight. Imaging studies included ultrasound, echocardiography, computed tomography, and magnetic resonance imaging.
Statistical analysis
Statistical analyses were performed using SPSS 26.0 software. The categorical variables are presented as case numbers (%), and inter-group comparisons were made using chi-square tests (n ≥ 40, T ≥ 5) and the corrected chi-square test (n ≥ 40, 1 ≤ T < 5) or Fisher’s exact test (n ≥ 40, T < 1). The normality of continuous variables was assessed using the Kolmogorov-Smirnov test. Continuous variables that followed a normal distribution are expressed as the mean ± standard deviation (SD). Levene’s test was used to assess the homogeneity of variance. Further analyses were conducted using an independent samples t-test for equal variances or Welch’s t-test for unequal variances. Non-normally distributed continuous variables are expressed as the median (interquartile range, P25–P75), and comparisons were made using the Mann-Whitney U test. Variables with significant differences between the two groups were further analyzed using logistic regression. A P-value of < 0.05 was considered statistically significant.
Results
General characteristics
Between January 1, 2011, and December 31, 2023, 102 NLE patients were admitted to the four participating hospitals. Eleven patients with incomplete clinical data were excluded, leaving 91 patients who met the inclusion criteria. Among these 91 patients, 37 were male, and 54 were female, with a mean gestational age of 37 ± 2 weeks (range 36 ± 1 to 38 ± 4 weeks) and a mean birth weight of 2510.35 g (range 1960.20 to 3104.30 g). Of these, 15 patients (15.48%) were diagnosed with CHB. In the CHB cohort, six were male, and nine were female, with a mean gestational age of 37 weeks (range 35 ± 2 to 38 ± 4 weeks) and a mean birth weight of 2500.30 g (range 1910.00 to 3075.40 g). The distribution of CHB severity was as follows: five had third-degree CHB (5.49%), four had second-degree CHB (4.40%), and six had first-degree CHB (6.59%). No significant differences in gender, gestational age, birth weight, or mode of delivery were observed between the CHB and non-CHB groups (P > 0.05).
Among the 15 NLE patients with CHB, 10 had maternal allergic diseases, and 14 had maternal autoimmune disorders. The maternal autoimmune disorders included nine cases of SLE and two cases of mixed connective tissue disease syndrome. Two had abnormal autoantibodies, and one case each had no Sjögren’s syndrome or no autoimmune disease. No photosensitivity symptoms were observed. Notably, two mothers experienced mild pregnancy-associated lupus flares, which stabilized following steroid therapy. The CHB group had a significantly higher proportion of maternal allergic diseases than the non-CHB group. However, no significant differences were found between the two groups regarding paternal autoimmune disease history, maternal autoimmune disorders, or pregnancy-associated lupus flares. The clinical characteristics are presented in Table 1.
Serum autoimmune antibodies and associated laboratory results
The serum levels of autoimmune antibodies and associated laboratory test results were compared between the two groups (Table 2). The CHB group had significantly higher proportions of double-positive anti-SSA and anti-SSB antibodies compared to the non-CHB group, as well as elevated serum levels of creatine kinase (CK), lactate dehydrogenase (LDH), and hydroxybutyrate dehydrogenase (HBDH) (P < 0.05). However, the proportion of patients with anti-SSA, anti-SSB, and U1-RNP antibodies (P > 0.05) was not significantly different between the two groups.
Multivariate logistic regression analysis
Five variables that showed statistically significant differences in the univariate analysis were included in the multivariate logistic regression analysis. The results indicated that elevated serum CK levels (odds ratio (OR): 1.014, 95% confidence interval (CI): 1.002–1.025, P = 0.019) may be an indicator of CHB in NLE patients. The multivariate logistic regression analysis results are presented in Table 3.
Organ involvement and long-term follow-up
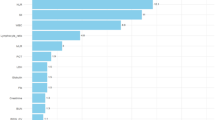
Hematologic involvement was the most prevalent in children with CHB, followed by the skin, heart, digestive, and central nervous systems. Anemia was the most common hematologic manifestation, with other findings that included thrombocytopenia, neutropenia/deficiency, hypocomplementemia, and coagulation abnormalities. No statistically significant differences in organ involvement were observed between the CHB and non-CHB groups (P > 0.05).
The median follow-up duration for CHB patients was 5 years (range 2 to 7 years). Two patients were lost to follow-up, while symptoms other than CHB resolved in the remaining patients by age 2. Among the five patients with third-degree CHB, one was lost to follow-up, and four underwent pacemaker implantation at approximately 1 year of age due to the inability to tolerate physical activity. The organs involved in patients with NLE complicated by CHB are presented in Table 4.
Discussion
This multi-center retrospective study was conducted at four tertiary hospitals in East China and aimed to investigate the clinical characteristics of NLE complicated by CHB and follow the long-term outcomes of these patients. The study found that NLE patients with CHB had significantly higher maternal rates of allergic diseases, a higher prevalence of double-positive antibodies, and elevated serum levels of CK, LDH, and HBDH. Elevated serum CK levels were identified as an independent risk factor for developing CHB in NLE patients. Long-term follow-up showed that all symptoms except CHB resolved spontaneously in the children at around 2 years of age, consistent with previous reports. Most current studies suggest that organ involvement resolves spontaneously as fetal lupus antibodies are depleted, probably within 6–12 months, and the prognosis of the children is mostly favorable10. Pacemaker implantation substantially improved activity intolerance in patients with third-degree CHB, suggesting that pacemaker therapy is an effective treatment for these patients.
CHB occurrence is directly related to maternal antibodies targeting fetal heart antigens. When anti-SSA and anti-SSB antibodies bind to fetal antigens, they inhibit the clearance of apoptotic cells during cardiac development, enhance Toll-like receptor signaling, and promote macrophage activation, leading to the increased secretion of fibrotic factors11. This process results in structural cardiac abnormalities and impaired cardiac function12,13. Additionally, L-type and T-type calcium channels in cardiomyocytes cross-react with these autoantibodies, disrupting calcium homeostasis and affecting the conduction of action potentials11. Further studies found that anti-U1-RNP antibodies were associated with the development of CHB14. Therefore, testing for maternal anti-U1-RNP antibodies should be considered in cases of CHB when both anti-SSA/Ro and/or anti-SSB/La antibodies are negative and no structural causes are found. Research indicates that the risk of NLE-related CHB increases significantly in patients with both anti-SSA/Ro and anti-SSB/La antibodies, and the likelihood of CHB is even higher in patients with anti-SSA, anti-SSB, and anti-U1-RNP antibodies14. In this study, the proportion of NLE patients with CHB and anti-SSA, anti-SSB, and anti-U1-RNP antibodies was significantly higher than in the non-CHB group. However, the proportion of patients having only both anti-SSA and anti-SSB antibodies was significantly different between the two groups, which may be attributed to the relatively small sample size in this study.
The incidence of allergic diseases in mothers of patients with CHB in this study was significantly higher than in the non-CHB group. IgE typically mediates allergic diseases, and a lack of IgE exchange between the mother and fetus was once a widely held belief. However, recent studies have shown that maternal IgE can activate fetal mast cells, thereby mediating allergic reactions in the fetus15. Allergic diseases during pregnancy have also been closely associated with adverse neonatal outcomes16. Mast cells, eosinophils, inflammatory cytokines, and IgE, which are involved in allergic reactions, have been shown to contribute to cardiac and vascular damage. IgE can activate the IgE-FcεR1 signaling pathway in cardiomyocytes and cardiac fibroblasts, leading to cardiomyocyte hypertrophy and fibroblast activation, and blocking the IgE-FcεR1 signaling pathway has been found to mitigate these effects17,18. However, no studies have explored the relationship between maternal allergic diseases and CHB. Future research should include large-scale, prospective, multi-center clinical studies and basic research to further investigate the correlation between maternal allergic diseases and the development of CHB.
CK, LDH, and HBDH are biomarkers that indicate inflammation and tissue damage19,20,21. Therefore, we assessed the levels of these biomarkers in patients with CHB. The serum levels of all three biomarkers were significantly elevated in the CHB group. However, only CK was identified as an independent risk factor for the development of CHB in NLE patients in the multivariate regression analysis. CK expression is enriched in the cytoplasm and mitochondria of cardiac, skeletal muscle, and brain tissue cells, and it is usually highly expressed in diseases such as myocardial injury, skeletal muscle injury, infections, autoimmune disorders, and inherited metabolic diseases22. Multiple organ damage in children with NLE due to lupus autoantibodies was associated with high CK expression levels and positively correlated with the degree of organ involvement. However, this needs to be confirmed through further clinical studies. Unfortunately, data on more specific myocardial injury markers, such as CK-MB and cardiac troponin T, were lacking, so we could not evaluate their effectiveness in predicting CHB in NLE patients. While skin involvement is the most common organ manifestation in NLE patients3,23, hematologic involvement was most prevalent in the patients with CHB in this study. However, given the relatively small number of these patients in our study, further research with larger sample sizes is needed to confirm these findings.
Pacemaker implantation effectively treats patients with congenital atrioventricular block (CAVB). Most CAVB patients require pacemaker implantation within the first year of life to maintain cardiac function24,25. Follow-up studies have reported a 9-year survival rate of 96% in CAVB patients with a pacemaker, although pacemaker implantation can also induce abnormal electrical activation patterns24. In this study, four patients underwent pacemaker implantation at approximately 1 year of age, and their activity tolerance significantly improved following the procedure.
This study identified the clinical characteristics and outcomes of neonates with NLE complicated by CHB, offering valuable insight for future research and clinical management. However, the sample size was limited despite accounting for the rarity of NLE and incorporating cases from four clinical centers. This limitation prevented the application of more advanced statistical methods to comprehensively investigate the risk factors for CHB development. Furthermore, the scarcity of clinical studies on NLE-associated CHB restricted the selection of clinical variables for multivariate analysis. Future research should aim to include larger, multi-center cohorts through prospective studies to further elucidate the risk factors contributing to CHB in neonates with NLE.
In conclusion, our study suggests that elevated serum CK levels may indicate an increased risk of CHB in neonates with NLE and that cardiac pacemaker implantation is an effective treatment for infants with third-degree CHB.
Data availability
The datasets generated in this study are available at the reasonable request of the corresponding author.
References
Sun, W. et al. Neurological and endocrinological involvement in neonatal lupus erythematosus: A retrospective study at a tertiary hospital in Eastern China. Clin. Rheumatol. 42, 2461–2468 (2023).
Morel, N. et al. « lupus néonatal » : Revue de La littérature. La Revue de Médecine Interne. 36, 159–166 (2015).
Sun, W., Jin, X., Li, Y., Li, M. & Zhu, X. Neonatal lupus erythematosus presenting with effusions: A 13-year retrospective study. Clin. Rheumatol. 43, 2927–2932 (2024).
Sheng, X. et al. Maternal and infant outcomes of pregnancy associated with anti-SSA/RO antibodies: A systematic review and meta-analysis. Pediatr. Rheumatol. 21, 22 (2023).
Ho, A. et al. Isolated complete heart block in the fetus. Am. J. Cardiol. 116, 142–147 (2015).
Brucato, A. et al. Risk of congenital complete heart block in newborns of mothers with anti-Ro/SSA antibodies detected by counterimmunoelectrophoresis: A prospective study of 100 women. Arthritis Rhuem. 44, 1832–1835 (2001).
Derdulska, J. M. et al. Neonatal lupus erythematosus—Practical guidelines. J. Perinat. Med. 49, 529–538 (2021).
Lee, L. A., Sokol, R. J. & Buyon, J. P. Hepatobiliary disease in neonatal lupus: Prevalence and clinical characteristics in cases enrolled in a National registry. Pediatrics 109, e11–e11 (2002).
Brito-Zerón, P., Izmirly, P. M., Ramos-Casals, M., Buyon, J. P. & Khamashta, M. A. The clinical spectrum of autoimmune congenital heart block. Nat. Rev. Rheumatol. 11, 301–312 (2015).
Liszewska, A. & Woźniacka, A. Neonatal lupus erythematosus—prevention is betterthan cure. Pdia 39, 1021–1026 (2022).
Izmirly, P., Saxena, A. & Buyon, J. P. Progress in the pathogenesis and treatment of cardiac manifestations of neonatal lupus. Curr. Opin. Rheumatol. 29, 467–472 (2017).
Wainwright, B. et al. Autoimmune-mediated congenital heart block. Best Pract. Res. Clin. Obstet. Gynecol. 64, 41–51 (2020).
Rumancik, B., Haggstrom, A. N. & Ebenroth, E. S. Neonatal lupus with left bundle branch block and cardiomyopathy: a case report. BMC Cardiovasc. Disord. 20, 352 (2020).
Izmirly, P. M. et al. Clinical and pathologic implications of extending the spectrum of maternal autoantibodies reactive with ribonucleoproteins associated with cutaneous and now cardiac neonatal lupus from SSA/Ro and SSB/La to U1RNP. Autoimmun. Rev. 16, 980–983 (2017).
Msallam, R. et al. Fetal mast cells mediate postnatal allergic responses dependent on maternal IgE. Science 370, 941–950 (2020).
Pfaller, B., Bendien, S., Ditisheim, A. & Eiwegger, T. Management of allergic diseases in pregnancy. Allergy 77, 798–811 (2022).
Ge, W. et al. The role of Immunoglobulin E and mast cells in hypertension. Cardiovasc. Res. 118, 2985–2999 (2022).
Zhao, H. et al. Role of IgE-FcεR1 in pathological cardiac remodeling and dysfunction. Circulation 143, 1014–1030 (2021).
Zhao, B. et al. Innovative engineering of superoxide dismutase for enhanced cardioprotective biocatalysis in myocardial ischemia-reperfusion injury. Int. J. Biol. Macromol. 286, 137656 (2025).
Zeng, J. et al. Tongmai hypoglycemic capsule attenuates myocardial oxidative stress and fibrosis in the development of diabetic cardiomyopathy in rats. Chin. J. Integr. Med. https://doi.org/10.1007/s11655-024-4002-3 (2024).
Xu, H., Wang, M., Zhao, T., Yu, X. & Wang, F. Protective effects of fructose-1,6-bisphosphate postconditioning on myocardial ischaemia-reperfusion injury in patients undergoing valve replacement: A randomized, double-blind, placebo-controlled clinical trial. Eur. J. Cardiothorac. Surg. 66, ezae306 (2024).
Kurapati, R. & Soos, M. P. CPK-MB. In StatPearls (StatPearls Publishing, 2025).
Yang, X. Clinical features autoantibodies, and outcome of neonatal lupus erythematosus. Fetal Pediatr. Pathol. 41, 436–442 (2022).
Eliasson, H. et al. Outcome in young patients with isolated complete atrioventricular block and permanent pacemaker treatment: A nationwide study of 127 patients. Heart Rhythm. 12, 2278–2284 (2015).
De Caluwé, E. et al. Long-Term Follow-Up of children with heart block born from mothers with systemic lupus erythematosus: A retrospective study from the database pediatric and congenital heart disease in university hospitals Leuven. Pacing Clin. Electrophis. 39, 935–943 (2016).
Acknowledgements
We acknowledge the parents of the infants for allowing us to use their data.
Funding
This work was supported by the General Program of the National Natural Science Foundation of China (82271741); Gusu Health Talent Plan Project (GSWS2022055); Key Medical Research Project of Jiangsu Provincial Health Commission (ZD2021013); Clinical Transformation of Scientific and Technological High-end Platform and Base Construction Project (ML13101523) and Suiyuan Clinical Research Project of Children’s Hospital of Soochow University (SY003).
Author information
Authors and Affiliations
Contributions
Xueping Zhu, Xinyun Jin and Wenqiang Sun conceptualized and designed the study. Xue Liu, Zexi Sun, Huawei Wang, Lili Li, Jie Huo and Jinhui Hu contributed to data collection by providing patient data. Xinyun Jin, Wenqiang Sun and Yihui Li performed data analysis. Xinyun Jin and Wenqiang Sun wrote the original draft of the manuscript. All authors critically reviewed and edited the manuscript. All authors approved the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Jin, X., Sun, W., Li, Y. et al. Clinical characteristics of neonatal lupus erythematosus complicated by congenital heart block: a multi-center retrospective study in East China. Sci Rep 15, 14031 (2025). https://doi.org/10.1038/s41598-025-98368-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41598-025-98368-3