Abstract
This study investigates the factors influencing user resistance to e-health services among older adults, focusing on the role of information inequality, digital distrust, low self-efficacy, perceived risk, and social influence. Structured questionnaires were used to gather data from 301 older adult participants, and the structural equation modeling method was used to analyze the results. The results show that digital distrust, perceived risk, and user resistance have a significant positive relationship, underscoring the significance of resolving trust and risk concerns in e-health interventions. The study also finds that the association between digital distrust and user resistance is moderated by anticipated regret, indicating that people who anticipate regretting not adopting electronic health services are less likely to oppose digital technologies despite their distrust. Surprisingly, the study did not find support for the hypothesized relationship between information inequality and user resistance, indicating the need for further exploration of this complex relationship. The study contributes to a better understanding of the factors influencing user resistance to e-health services among older adults, offering valuable insights for policymakers and practitioners seeking to promote the adoption of digital health technologies in aging populations.
Similar content being viewed by others
Introduction
A broad technical intervention for fundamental improvement in the healthcare sector, electronic health (e-health), has been viewed as a means of reducing the massive disparity between the supply and demand of healthcare in both affluent and developing countries. Recent advancements in digital technology have significantly improved healthcare systems, making them more effective and efficient in detecting and treating illnesses (Kumari et al., 2018; Tanwar et al., 2020). E-Health services improve healthcare supply in dire situations, as witnessed during the COVID-19 pandemic. As a result, it is reasonable to assume that e-health, or electronically delivered medical services, will become more integrated into the healthcare system. This may include online consultations and virtual rehabilitation. However, it has taken some time for this shift to take effect, and it was not until 2020 that e-health initiatives like telemedicine and Clinical Decision Support Systems were more widely adopted (Talwar et al., 2023). In technologically advanced countries, various stakeholders, including patients, medical staff, and hospital administration, oppose these initiatives (Talwar et al., 2023). For example, reports indicate that, as of early 2019, only a few healthcare systems in the United States had adopted virtual care services (Mehrotra and Prewitt, 2019). The situation underwent a dramatic shift with the emergence of the COVID-19 pandemic, especially following the World Health Organization’s declaration of a global health crisis in March 2020 (Laato et al., 2020). During the pandemic, patients embraced e-health services and considered them a good medium for healthcare. However, this prompts consideration of whether healthcare systems will revert to their traditional reliance on in-person consultations, treatments, and care once the pandemic subsides or if the landscape of healthcare, particularly in terms of e-health, has undergone permanent transformation. Traditional one-on-one health services still pose several challenges to older adults, as depicted in Fig. 1. Why is there resistance to using e-health services in different countries today despite the evident advantages e-health offers?
Patients nowadays are projected to live independently (as opposed to in care facilities) for as long as feasible due to changes made to long-term care. These changes include emphasizing home-based care options, implementing policies to support aging in place, expanding community-based services, integrating technological innovations, and promoting family and caregiver involvement in care. As a result of these changes, there is a growing projection that patients will increasingly choose independent living options over institutional care. E-health apps have been deemed resourceful for accomplishing this objective, along with heightened help from volunteers, family, and friends (de Veer et al., 2015). In countries with low or middle incomes in the year 2021, there were more than 300 million individuals aged 70 or above (United Nations, 2022). The number of people in low- and middle-income countries (LAMIC) who are 70 years of age or older is predicted to triple by 2050 compared to high-income nations, surpassing one billion by 2056 (United Nations, 2022). The aging population phenomenon in LAMIC occurs in settings with constrained healthcare resources and, at most, developing social care systems. These demographic trends have the potential to quickly exceed the capacity of the current service infrastructure in the absence of significant legislative and administrative solutions. The sustainability of health systems in high-income nations depends on the combination of social and health care, focusing on information- and technology-based services (AlBar and Hoque, 2019). The World Health Organization defines e-health as connecting patients, administrators, and healthcare professionals via information and communication technology (ICT) (World Health Assembly, 2005). Its goals include encouraging innovation in managing and providing healthcare, reducing costs, educating managers, consumers, and healthcare professionals, and improving the healthcare system overall.
Over the past two decades, there has been a significant surge in internet use worldwide. According to the Global Web Index, the number of Internet users globally has reached approximately 4.39 billion (Adeleke, 2021). Interestingly, Nigeria has actively contributed to this fantastic trend. Notably, according to Statista, in January 2024, Nigeria was the most Internet-savvy country in Africa (Statista, 2024). According to the latest released data by the National Bureau of Statistics, Nigeria recorded a combined total of 163,838,439 active internet users in the fourth quarter of 2023, a rise from 154,847,901 recorded in the same period of 2022, indicating a growth of 5.81% (National Bureau of Statistics, 2024). When compared quarter-on-quarter, this reflects an increase of 2.29%. Figure 2 shows the number of internet subscribers from the six geopolitical regions in Nigeria. Despite Nigeria’s relatively high digital literacy rate of 62%, around 38% of the population still lacks basic literacy skills (Adeleke, 2021). Factors such as education level, age, gender, and access to reliable power supply influence internet usage and digital proficiency levels. A study discovered that older people (aged 60 and above) in rural and northern Nigeria tend to use the internet less as they get older (Adeleke, 2021). However, this finding does not represent the entire country because it focuses on rural northern areas. Although some research suggests that older adults may use the internet to connect socially and alleviate loneliness (Morahan-Martin and Schumacher, 2003), the general pattern shows reduced internet usage among this demographic in specific areas (Adeleke, 2021). This may suggest that reduced internet usage also affects the acceptance of e-health services.
Applications for e-health show promise in helping older people in the community take care of themselves and control their health, which could reduce the cost of care (Marziali, 2009; Paré et al., 2007). Nevertheless, the scant evidence substantiating these advantages has been ascribed to deficiencies in the study design or insufficient execution (de Veer et al., 2015). The target group’s resistance to using e-Health presents a possible implementation challenge. Determining effective implementation strategies requires understanding the elements impacting the intention to utilize e-Health. The user’s resistance to e-health is not always simple across different contexts, even though e-health innovations can improve health services significantly at a lower cost and higher convenience. It might be difficult to understand people’s acceptance or rejection of new information systems in practice within the information system area (Wong et al., 2023). The willingness of users to adopt new technologies is often a determining factor in the implementation of e-health services (AlBar and Hoque, 2019).
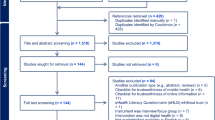
Nevertheless, implementing e-health systems presents difficulties for many nations, especially those in the developing world. The resistance behavior to e-health among senior community members has not been extensively studied through quantitative research. Out of 16 papers in a systematic review on the acceptance of technology to support aging at home, only three used a quantitative study approach (Peek et al., 2014). According to a recent literature review by Talwar et al. (2023), the sources of resistance identified across the 14 studies they employed can be grouped into four main categories: technological challenges, concerns related to patient care, reluctance to change, and perceived risks. Technological obstacles encompass issues like technology anxiety, resistance to new technologies, and lack of technical skills. Patients’ care-related concerns include dissatisfaction with diagnosis and treatment, mistrust in organizational effectiveness, and worries about healthcare staff motivation. Additionally, patients may exhibit resistance due to their reluctance to change, inertia, and the perceived costs of transitioning. Finally, perceived risks contributing to resistance include uncertainties, security and privacy concerns, lack of trust, identity threats, information overload, system complexity, fatigue, and technostress.
Talwar et al. (2023) identified several gaps in the literature related to resistance to e-health. These gaps include limitations in the theoretical background, such as the Technology Acceptance Model (TAM) and The Unified Theory of Acceptance and Use of Technology (UTAUT), which may be insufficient for studying technology resistance. These technology acceptance models focus on acceptance factors such as perceived ease of use and perceived usefulness. Although the constructs from TAM and UTAUT can provide some insights into user resistance behavior, we cannot entirely rely on technology acceptance theories to understand technology resistance. Adoption and resistance behavior differ (Talwar et al., 2023); in other words, adoption does not equate to resistance. Adoption refers to accepting or using something new, like a product, service, or idea. It involves actively incorporating the new element into one’s life or routine. On the other hand, resistance behavior involves actively opposing or not accepting something, often due to disagreement with its purpose, features, or values. The factors influencing acceptance, as studied previously, may not fully elucidate resistance behavior. Acceptance behavior typically pertains to the initial acceptance when users first encounter information products at the onset of the information system usage life cycle. However, resistance behavior can manifest throughout the entire system usage life cycle, including post-adoption stages (Cao et al., 2020).
Additionally, the research perspectives on acceptance and resistance differ. Acceptance studies primarily focus on users’ acceptance behavior, driven by perceptions, attitudes, and behavioral intentions. In contrast, resistance studies aim to understand the causes of users’ resistance to information technology, particularly considering the changes or negative influences resulting from system implementation. Thus, the factors identified within TAM and UTAUT frameworks may not comprehensively explain resistance behavior. Research directly addressing resistance behavior is warranted.
Furthermore, a previous study (Aslam, 2011) has indicated that negative emotions significantly contribute to resistance behavior. Yet, these factors have been largely overlooked in existing research on elderly users’ e-health services use. Hence, this study aims to bridge these gaps by investigating how specific external stimuli (information inequality, social influence, and perceived risk) and negative emotions (digital distrust and low self-efficacy) trigger resistance behavior among the elderly population in Nigeria. Additionally, most studies have been conducted in developed countries, leaving many geographical locations, such as Nigeria, understudied. Furthermore, few studies have focused solely on e-health service resistance, indicating a need for more research in this area.
As detailed in the National Health ICT Strategic Framework (Aririguzoh et al., 2021), Nigeria started e-health implementation plans in 2015. However, resistance to e-health health services is still a significant problem. To the best of our knowledge and during this research, no study has investigated the moderating role of anticipated regret on the relationship between digital distrust and resistance to e-health services. This relationship exposes implications for a better understanding of factors that promote resistance to e-health services among older adults. This knowledge adds depth to the existing literature on the relationship between the older population and resistance to e-health services by examining how anticipated regret may change the relationship between digital distrust, low self-efficacy, and user resistance behavior.
This research seeks to answer the following research questions (RQ):
RQ1. Why do older adults resist the use of e-health services?
RQ2. To what extent do digital distrust and low self-efficacy among older adults affect their resistance to e-health services?
RQ3. What is the moderate impact of anticipated regret on the nexus between psychological factors (digital distrust and low self-efficacy) and resistance to e-health services among older adults?
Numerous Sustainable Development Goals (SDGs) that support partnership, equality, justice, and health in Nigeria, as shown in Fig. 3, are supported by this study. Examining the elements influencing older individuals’ reluctance to use e-health services can improve their well-being and access to healthcare under SDG 3: Good Health and Well-Being. Addressing digital distrust and promoting the adoption of e-health services can result in better health and a higher standard of living. Additionally, in keeping with SDG 10: Reduced Inequalities, being aware of the obstacles older persons encounter when attempting to utilize e-health services because of digital distrust can aid in identifying and resolving discrepancies, which in turn helps to lessen inequalities in healthcare outcomes and access. It is important to investigate how information inequality may affect older adults’ self-efficacy. Enhancing older individuals’ trust in digital technology and e-health services can also help develop more inclusive and reliable institutions, which aligns with SDG 16: Peace, Justice, and Strong Institutions. Policymakers and healthcare professionals should endeavor to establish a more equal healthcare system by tackling digital distrust and resistance issues.
Last but not least, SDG 17: Partnerships for the Goals advocates cooperation across government agencies, healthcare organizations, technology developers, and civil society to increase the uptake of e-health services among older individuals in Nigeria. To remove obstacles to adopting e-health and promote innovation in healthcare delivery, this research can help organize collaborations and knowledge-sharing programs. The study has important theoretical implications, particularly regarding the Stimulus–Organism–Response (SOR) framework. We can enhance our theoretical understanding of technology adoption and healthcare utilization by identifying the factors that impact older adults’ reluctance to adopt e-health innovations. For instance, by applying the SOR framework to the study of older adults’ resistance to e-health innovations, we can better understand how various stimuli, such as information inequality, social influence, and perceived risks, affect their cognitive and emotional responses, ultimately influencing their resistance behavior. This more profound understanding of how people engage with and respond to technological innovations can inform the development of more effective interventions and strategies to promote the adoption of e-health services among older populations.
Theoretical foundation and research hypotheses
Stimulus–organism–response (SOR) Theory
The SOR theory provides a theoretical foundation for analyzing user behavior (Jacoby, 2002; Mehrabian and Russell, 1974). According to the notion, the user’s behavior is triggered by the state of the internal organism, which is determined by external stimuli. According to Mehrabian and Russell (1974), the SOR process occurs when an external stimulus (S) stimulates an organism’s (O) internal psychology, resulting in a behavioral response (R). According to Sampat and Raj (2022), SOR theory aids in assessing how progressive a user’s mental processes are when they anticipate, internalize, and respond to internal and external stimuli. SOR has been used to study user resistance (Cao et al., 2020; Fan et al., 2024). A previous study by Cao et al. (2020) examined how overload factors affect older users’ resistance to e-health applications. Cao et al. (2020) found that while intergenerational support reduces the effects of fatigue and technostress caused by information and system feature overload, resistance remains higher. SOR has also been used to study tourism (Kim et al., 2020), discontinuance intentions (Ma et al., 2022), and purchasing behavior (Chang et al., 2011; Hashmi et al., 2019; Laato et al., 2020). It is clear from the reviewed literature that the SOR theory provides a thorough framework for comprehending people’s behavioral reactions and psychological perceptions of environmental stimuli, especially those produced by information systems. The SOR theory, which closely aligns with the goals of this study, describes the process by which external stimuli interact with internal psychological elements to create behavioral reactions. Consequently, the current study intends to apply the SOR theory to investigate how older users’ psychological perceptions are influenced by external-related stimuli, resulting in resistance behavior towards e-health services applications.
Stimuli (S)
Information inequality
Information inequality arises from systemic societal disparities that dictate how individuals from various socioeconomic backgrounds access and utilize information. These disparities are impacted by people’s educational attainment and the technical infrastructure available in various locations. Equality of access to information technology and informational resources among varied groups is generally facilitated by vital social resources and high-quality education (Figueiredo, 2018). Information distribution inequality is mainly caused by the natural selectivity that comes with limiting access to information, which is frequently considered a crucial component of resource distribution (Hargittai and Hinnant, 2008). In the context of our proposed research on older adults’ resistance to e-health, information inequality plays a crucial role in shaping individuals’ scarce access to and utilization of digital health resources. Attention has shifted to the unequal distribution of information, especially on internet platforms, as nations have made progress in eliminating disparities in information access. Users’ views, comprehension, and trust are impacted by the selective distribution of information made possible by the control over its transmission on the internet. Different user groups may experience cognitive dissonance, communication difficulties, and a rise in unpleasant emotions due to this selective change in the information flow. To tackle these issues, we put out the following hypotheses:
H1a: Information inequality has a significant positive relationship with digital distrust.
H1b: Information inequality has a significant positive relationship with low self-efficacy.
H1c: Information inequality positively influences user resistance.
Social influence
As described by Bearden et al. (1989), Social Influence encompasses the significant impact of individuals within a social network on each other’s attitudes and behaviors. This influence extends to forming accurate perceptions of reality, developing social relationships, and maintaining a favorable self-concept, as articulated by Cialdini and Goldstein (2004). Slade et al. (2015) discovered that people frequently check their social networks before embracing new technology due to perceived social pressure from influential people around them. Chaouali et al. (2016) also noted the effects of social influence on the inclination to use online banking. Kleijnen et al. (2009) state that peer observation significantly impacts consumer decision-making processes. Users of socially unacceptable innovations may feel alone because of a lack of social support. Matsuo et al. (2018) investigated the impact of social influence on innovation resistance. In the SOR theory, a previous study (Ming et al., 2021) categorized social influence as an external stimulus, making it fitting for our study. Social influence plays a crucial role in determining the adoption of digital health services in the context of e-health. This influence is derived from seeking information from peers, role models, and social networks. Previous research (Coppolino Perfumi et al., 2019) investigated the two typologies of social influence: normative social influence and informational social influence. The first type, known as “normative,” occurs when individuals conform to meet the need for social belonging and adhere to societal norms, as demonstrated in Asch’s experiments (Asch, 1955). The second type, termed “informational,” occurs when individuals lack sufficient information to complete a task effectively, as seen in the autokinetic experiment by Deutsch and Gerard (1955). This research explores the role of informational social influence in the context of resistance to e-health services. A previous study (Ezeudoka and Fan, 2024) found that social influence positively influences the adoption of e-pharmacy services. While informational social influence typically has positive effects, it can inadvertently contribute to resistance and digital distrust in specific scenarios. For instance, individuals may be exposed to misinformation from unreliable sources, such as social media influencers or misinformation campaigns (van der Linden, 2022), leading them to adopt beliefs or behaviors that are not beneficial. This misinformation may increase distrust in reliable sources and e-health services.
Furthermore, individuals might rely too heavily on peer recommendations without critically evaluating the information, potentially leading to resistance if their choices do not align with personal values. When people do not fully comprehend complicated health-related matters, they can seek advice from informational social influence (Kim et al., 2015). On the other hand, misinterpretations or inflated expectations could arise from inadequate or oversimplified information, which would breed distrust (Langevoort, 1997) or resistance. Divergent recommendations from various sources can potentially exacerbate ambiguity and misunderstanding, undermining confidence in e-health systems. While informational social influence itself is not inherently harmful, its impact on resistance and digital distrust can be influenced by factors such as information reliability and individuals’ critical thinking skills. To make intelligent choices concerning their health, people must thus approach informational social influence attentively and look for reliable sources. Therefore, we put forward the following hypotheses:
H2a: Social influence (informational) has a significant positive relationship with digital distrust.
H2b: Social influence (informational) has a significant positive relationship with low self-efficacy.
H2b: Social influence (informational) has a strong positive influence on user resistance.
Perceived risk
Perceived risk, a vital construct in the context of this research, encompasses individuals’ subjective evaluations of potential negative outcomes or uncertainties associated with adopting e-health services (Dowling and Staelin, 1994; Haddock et al., 1993). It represents their expectations of loss rather than the actual probability of experiencing adverse consequences (Quintal et al., 2010; Reisinger and Mavondo, 2005). Perceived risk varies among individuals within the same context, as they uniquely identify different risk sources and assess associated risk levels. While perceived risk and uncertainty are often used interchangeably, they differ theoretically, with risk having a known probability while uncertainty lacks a definite (Quintal et al., 2010). In this study, perceived risk pertains to concerns about the security and privacy of personal health information, the reliability and accuracy of medical advice provided through digital platforms, and fears of financial loss or harm from using unfamiliar technologies. Perceived risk might act as a psychological barrier that prevents people, particularly older persons, from adopting e-health solutions by increasing digital distrust. This construct encompasses affective and cognitive elements, such as emotional reactions to perceived risks and logical evaluations of possible hazards. Comprehending the significance of perceived danger is imperative in clarifying the reasons behind users’ reluctance to use e-health services and formulating approaches to mitigate these apprehensions, ultimately fostering increased acceptance and utilization of digital health technologies. We therefore formulate the following hypotheses:
H3a: Perceived risk has a positive relationship with digital distrust.
H3b: Perceived risk has a positive relationship with low self-efficacy.
H3c: Perceived risk has a positive relationship with user resistance.
Organism (O)
Digital distrust
A research titled “Anticipating Well-Being in a Digital World” was released in April 2018 by the Pew Research Center (Anderson and Rainie, 2018). This study popularized the term “digital distrust,” characterizing it as a sense of alienation felt by those who utilize digital technology. Digital distrust occurs when people believe that others are more tech-savvy or skilled than they are. This reduces personal initiative and increases the spread of negative emotions like shock, fear, rage, and shame on the internet. Donath (2014) asserts that these unfavorable feelings fuel arguments and distrust among users. Trust is associated with positive emotions, while distrust is linked to negative emotions (Sha et al., 2015). Fan et al. (2021) also used digital distrust as an “organism” construct in studying cyber violence behavior. Digital distrust appears as fear or suspicion about using digital health solutions in the context of this study on older individuals’ resistance to e-health. This distrust could result from worries about digital health services and information security, dependability, or correctness. Several variables, such as low technological knowledge or experience, fear about revealing personal health information online, or unfavorable past encounters with digital platforms, might contribute to older persons’ display of digital distrust. The adoption of e-health services by older persons might be hindered by digital distrust, which can affect their attitudes, intentions, and actions regarding digital health solutions. Digital distrust has the potential to fragment user communities, foster negative emotions, and sow division in society, thereby increasing the likelihood of resistance to e-health innovations and other negative behaviors. Consequently, the following hypothesis is formulated:
H4: Digital distrust has a significant positive relationship with user resistance.
Low self-efficacy
In 1977, Bandura developed the self-efficacy theory, which defines self-efficacy as a person’s degree of confidence in their capacity to carry out a certain task (Bandura, 1977). Put another way, it measures the degree of confidence a person has in their ability to use technology to complete a task. According to Huang (2023), this idea is fundamental because it significantly predicts users’ behavior. Low self-efficacy emerges as a crucial consideration, particularly for elderly users. In the context of e-health, self-efficacy is essential because it connects older users’ efforts with outside support networks and makes it easier for them to use technology effectively. Previous studies (Ellen et al., 1991; George and Camarata, 1996) have investigated the role of self-efficacy in resistance to technological interventions. The nexus between self-efficacy and resistance has been studied in other fields, such as drug resistance (Choi et al., 2013) and education (Koyuncu and Dönmez, 2018). Users with high self-efficacy feel more empowered and satisfied with their interactions with technology, which increases their propensity and resolve to use it wisely (Baki et al., 2021). This increases self-assurance in their talents, creates a positive mindset, and motivates people to interact more readily with tech products and platforms. On the other hand, those who have lower levels of self-efficacy could feel more doubtful and hesitant about their capacity to use and navigate technology effectively. Their lowered self-esteem may prevent them from interacting with technology, leading to active resistance to these innovations, less-than-ideal engagement, and restricted exploration of its possible advantages. In previous research, Huang (2023) has studied self-efficacy as an organism in the SOR theory. In the context of this research, low self-efficacy refers to an individual’s lack of confidence or belief in their ability to effectively utilize or benefit from electronic health resources. Therefore, we put forward the following hypothesis:
H5: Low self-efficacy has a significant positive relationship with User Resistance.
Response
User resistance
User resistance behavior includes people’s adverse reactions and resistance to changes they expect from implementing an information system (Kim and Kankanhalli, 2009). Pre-, during-, and post-implementation stages of the system implementation process are all possible times for this resistance to appear (Klaus and Blanton, 2010). Active, passive, aggressive, and apathy are the four different levels of outward resistance behavior that users can exhibit, varying in severity (Joseph, 2010; Lapointe and Rivard, 2005). Apathy is a milder type of resistance defined by consumers’ lack of interest or apathy to the changes put into place. Apathy can be characterized by a lack of interest in or enthusiasm for the new system and low engagement or connection with it. A more subdued kind of opposition is passive resistance, in which users ostentatiously comply with the new system but have underlying misgivings or a reluctance to embrace its functions completely. Procrastination, a reluctance to fully exploit system functions, or subtly expressing mistrust are ways this resistance can appear. When users take an active stand against the changes put into place, they express their objections, critiques, and concerns about the new system. This is known as active resistance. People actively resisting may speak out against the system, argue against its necessity or efficacy, and promote other strategies or alternatives. The most overt and confrontational kind of resistance is aggressive resistance, defined by unfriendly or confrontational actions toward the new system’s supporters. Aggressive opposition users actively try to weaken or interfere with the implementation process by sabotaging, defiance, or outright confrontation. Elderly users usually have poor access to information due to the complexity of technological features, which may further promote digital distrust and low self-efficacy, which results in user resistance behavior.
The moderating impact of anticipated regret
The negative feelings people expect to feel when considering the potential of not engaging in a scheduled behavior are anticipated regret (Sandberg and Conner, 2008). For example, a person’s decision to move on with using e-health may be positively impacted if they expect to feel guilty about not taking advantage of the e-health benefits. Research has highlighted anticipated regret’s role in explaining acceptance behavior (Caso et al., 2019; Hamama-Raz et al., 2016). For example, anticipated regret affects the acceptance of vaccination (Caso et al., 2019). There is a predisposition to participate in loss avoidance when there is higher uncertainty since anticipated regret increases (Chua et al., 2021). This makes it more likely that customers will purchase or accept a good or service in a panic to avoid later regrets (e.g., higher pricing, stockouts) (Chua et al., 2021). An increase in acceptance behavior, such as panic buying or vaccination, can be influenced by anticipated regret (Brewer et al., 2017; Chua et al., 2021). Low vaccination rates correlate with low trust in vaccines, although immunization is predictably associated with anticipated regret about infectious diseases (Brewer et al., 2017). Anticipated regret is a powerful motivator for preventive health practices and health acceptance behaviors. Stronger intentions and a higher propensity to engage in health behaviors such as vaccination, exercise, or cancer screening are linked to anticipated regret from inaction (not performing a preventive action) (Brewer et al., 2016). People are motivated to take these actions to avoid the regret they would feel from not doing so.
In contrast, anticipated regret from taking action (like side effects from a vaccine) is associated with weaker intentions and a reduced likelihood of engaging in that health behavior (Brewer et al., 2016). The regret anticipated from potential negative consequences discourages acceptance. While distrust in digital systems may persist, people are likely to use them out of necessity to avoid the anticipated regret of missing out on potential benefits. Distrust is outweighed by regret over not using valuable technologies (O’Carroll et al., 2011). People use online banking, for instance, despite privacy issues, to prevent regretting lost money chances. Despite distrust, acceptance is motivated by the wish to avoid regret in the future (O’Carroll et al., 2011). Psychological resistance to embracing new behaviors or technologies might be overcome by this inclination to prevent possible regret (Lin et al., 2016). People may be resistant to change because of status quo bias or inertia. However, anticipating regret for passing up possible benefits through inaction helps overcome this barrier.
Previous studies have investigated the moderating roles of anticipated regret on risk perception (Nordgren et al., 2007), cost effects (Kwak and Park, 2012), entrepreneurship (Bae et al., 2024) and exercise (Abraham and Sheeran, 2004). In the context of this research, anticipated regret is considered a construct that buffers the relationship between digital distrust, low self-efficacy, and user resistance, respectively. Adoption can be limited by negative emotions like fear or repulsion (e.g., the “ick factor” regarding organ donation) (O’Carroll et al., 2012). Nonetheless, these negative emotional attitudes can be overcome by modest anticipated regret interventions that emphasize the regret of inaction (O’Carroll et al., 2012). The desire to avoid future regret is a more powerful motivator than negative anticipated emotions like anxiety or anger. Regret gives more weight to the potential benefits of acceptance. In summary, while obstacles like distrust, resistance, and negative emotions can prevent acceptance, the fear of regretting one’s actions in the future due to non-acceptance can overcome these obstacles by emphasizing the long-term advantages of acceptance. Therefore, we propose the following hypotheses:
H6: Anticipated regret negatively moderates the nexus between low self-efficacy and user resistance.
H7: Anticipated regret negatively moderates the nexus between digital distrust and user resistance.
Figure 4 summarizes all six constructs, the proposed hypotheses, and the research framework.
Methods
Research design
The research design for this study was a cross-sectional survey. In a cross-sectional survey, information was gathered at one specific moment from a wide range of respondents. The evaluation of correlations between variables and the investigation of patterns or trends within the population were made possible by this design. Convenience sampling was utilized in this study. This sampling approach has been used in a previous study (Scholtz, 2021). We also used purposeful sampling, which allowed us to consider only those who met the criteria for participation. These criteria include: (i)They reside in any of the six geopolitical regions of Nigeria. (ii) They are over 60 years of age. (iii) They understand their right to withdraw from the study and consent to participate in the survey. The study used convenience and purposeful sampling to collect data from a wide range of older adults. This approach ensured that the sample included individuals who met the criteria to provide valuable insights into the research topic while also maintaining efficiency. This hybrid approach improved the balance between practicality and relevance. An organized survey was conducted among senior citizens in Nigeria to gather data for this investigation. Questions about demographics, e-health use, social influence, information inequality, perceived risk, digital distrust, low self-efficacy, anticipated regret, and resistance to e-health services were all included in the questionnaire. Depending on the choices and availability of the participants, the survey was conducted electronically or in person. The data analysis used descriptive statistics, such as frequencies and percentages, to characterize the sample’s demographic features.
Furthermore, SmartPLS 4.0 was used to analyze the correlations between variables through structural equation modeling (SEM). SEM is a statistical method that systematically examines intricate correlations between numerous variables. It offers a thorough grasp of the underlying mechanisms guiding observed occurrences by allowing researchers to evaluate variables’ direct and indirect effects on one another. SEM was used in this study to examine the connections between older people in Nigeria’s demographics, social influence, information inequality, perceived risk, digital distrust, low self-efficacy, anticipated regret, and resistance to e-health services. Because of its robust capabilities in handling non-normal data and small sample sizes, as well as its user-friendly interface, SmartPLS 4.0, a capable tool for SEM analysis, was used. The study aimed to uncover the factors influencing older adults’ resistance to e-health services in Nigeria through SEM analysis, providing insights for healthcare practitioners and policymakers.
Pilot testing
According to Brooks et al. (2016), it is important to test research instruments to ensure their accuracy and feasibility for the study. To evaluate the viability and efficacy of the research instruments and protocols, 65 questionnaires were distributed, and 59 were answered, reflecting a response rate of 90.77%. Data were gathered for the study’s pilot testing phase for 3 weeks. After gathering the data, four independent experts reviewed and validated the research instruments. The chosen participants were chosen to exemplify the target population’s demographic traits. The participants were given the study instruments, including questionnaire items, their comprehensibility, clarity, and applicability. Participant feedback was gathered to find any errors or misunderstandings in the questions, response choices, or general questionnaire structure. With 59 participants completing the survey or interview within the allotted time, the pilot project also made it possible to evaluate the response rate. This response rate helped anticipate how long it would take to finish the primary survey and offered insightful information on the viability of the data-gathering methods. Additionally, by analyzing the internal consistency of questionnaire items and the coherence of interview responses, the researchers could assess the validity and reliability of the study instruments during the pilot testing phase. The feedback and insights obtained during the pilot testing phase were used to inform any necessary instrument or method modifications.
Participant recruitment and data collection method
The study’s target demographic was participants over 60 years old who reside in any of the six geopolitical regions of Nigeria. With Nigeria’s population totaling ~206 million people, as of 2020, there were 9.4 million individuals aged 60 years and older spread across the country’s six geopolitical zones (Statista, 2020). This data forms the foundation for establishing an appropriate representative sample size for the study. Hence, a sample size of N = 301 was utilized to construct the study model, which is considered adequate given that published SEM research typically incorporates 200–400 cases to fit models (Hox and Bechger, 1998; Kenny, 2020). They all have distinct backgrounds in terms of gender, age, education, and varying experiences using e-health. Regmi et al. (2016) suggest that a web-based questionnaire survey is helpful for data collection. Therefore, this survey used Microsoft Forms, distributed online via WhatsApp and Facebook. Several hospitals were visited, and we also shared the form with older people visiting the hospital. The marketplaces were also visited to collect responses by questionnaire distribution, targeting older adults. The questionnaire contents were read aloud through face-to-face interviews with older adults who had difficulty with reading. Two participants answered the questions orally on a Likert scale of 1–5 while the investigators noted their answers. Therefore, the investigator set up interviews via WhatsApp video call. Out of two respondents, we considered the response from only one participant who chose the interview method due to several skipped questions from the other. We collected a total of 71 paper-based responses. Participants also gained access to the online questionnaires by scanning the quick response (QR) code or clicking the link to the form containing the questionnaire items. We gathered 229 valid responses from the web-based survey.
In all, 400 questionnaires were distributed, and a total of 301 responses were considered for this research, representing a 75.25% response rate. All participants gave their informed consent for the survey. They were informed of their right to withdraw from the survey whenever they found it inconvenient. Survey invites were purposefully distributed to collect data across six months, from August 2023 to January 2024. There were variations in the time intervals between each distribution location. After the initial distribution, the invitations were resent every two weeks. This approach was implemented to lessen the possibility that respondents would reply more than once. Survey invitations were distributed across several months, with varying time intervals between dissemination. Additionally, the data collected were thoroughly examined manually to eliminate any suspicious responses or inconsistent response patterns. Lastly, the dataset was cleaned and prepared for analysis. This study ensured the participants’ privacy and obtained their informed consent, thereby adhering to research ethics. The demographic information is provided in Table 1.
Instruments
There are a total of 7 constructs in this study. The research instruments for each construct were measured using a Likert scale of 1–5, where 1 represents strongly disagree, and 5 represents strongly agree. Information inequality was measured with 4 instruments adapted from Fan et al. (2021). Social influence was measured with 3 instruments adapted from Shahzad et al. (2024). Perceived risk was assessed with 3 instruments adapted from Caso et al. (2022). Digital distrust was measured with 3 instruments adapted from Fan et al. (2021). Low self-efficacy was measured with items adapted from Huang (2023) and Tsai et al. (2020). Anticipated regret was measured with 4 items adapted from Caso et al. (2022). User resistance was measured using three items adapted from Cao et al. (2020) and Kim et al. (2017). All instruments used in this study are listed in Table 2.
Data analysis
The main statistical tool used in this study to examine the structural links between the variables in the research model was SmartPLS. For SEM, SmartPLS is a popular software program that works especially well for complicated models and small sample sizes in exploratory research (Hidayanto et al., 2020).
Results
Common method bias
The variance inflation factor (VIF) was analyzed to evaluate common method bias (CMB) in the data. VIF is a statistical measure that quantifies the severity of multicollinearity among predictor variables (Hair et al., 2011). Elevated VIF values suggest a high level of multicollinearity, which may be a sign of bias in the standard approach. The VIF values were calculated for every predictor variable included in the model. VIF levels above 3.3 indicate possible problems with multicollinearity, whereas values below 3.3 are generally regarded as acceptable according to Kock (2015). In this study, all predictor variables exhibited VIF values below the threshold of 3.3, as presented in Table 2, indicating that multicollinearity was not a significant concern.
Measurement model
To analyze the measurement model, the validity and reliability of the latent constructs and their indicators were evaluated using SmartPLS version 4.0. This procedure ensured the measurement model accurately represented the theoretical ideas being studied. A reliability analysis was done to assess the constructs’ internal consistency. For every latent variable, Cronbach’s alpha coefficients were calculated; values greater than 0.70 denote adequate reliability (Nunnally, 1978). Furthermore, composite reliability (CR) was evaluated; CR values greater than 0.70 were deemed appropriate (Bagozzi and Yi, 1988). Convergent and discriminant validity were established as the main goals of the validity investigation. The average variance extracted (AVE) for each construct was used to assess convergent validity; values above 0.50 indicated satisfactory convergent validity (Fornell and Larcker, 1981). The AVE indicates the variance recorded by the construct’s indicators about measurement error. All the values (Cronbach’s alpha coefficients, CR, and AVE) are presented in Table 2. Discriminant validity was evaluated by comparing the square root of the AVE for each construct with the correlations between the constructs. Discriminant validity was proven if the square root of the AVE for each construct was higher than the correlation between that construct and any other construct in the model (Fornell and Larcker, 1981). As described by Henseler et al. (2015), one approach to evaluating discriminant validity involves comparing the heterotrait–monotrait (HTMT) ratio to predefined thresholds, such as 0.85 or 0.9. Table 3 presents the Fornell and Larcker criterion and the HTMT ratio.
Furthermore, factor loadings presented in Table 4 were examined to guarantee that all indicators substantially loaded onto the corresponding constructs; values greater than 0.70 were deemed acceptable (Henseler et al., 2015). Items with low loadings or cross-loadings were considered for elimination or change to enhance model fit. The measurement model analysis supported the validity and reliability of the constructs, boosting trust in the study’s measurement tool.
Structural model evaluation
Direct effects
The direct effect evaluation under the structural model assessment demonstrates significant relationships between various constructs (Fig. 5). Information inequality significantly influences digital distrust (β = 0.130, p = 0.030) and low self-efficacy (β = 0.134, p = 0.036), while its impact on user resistance is not statistically significant (β = 0.069, p = 0.216). Perceived risk demonstrates a substantial positive effect on digital distrust (β = 0.384, p = 0.000), low self-efficacy (β = 0.310, p = 0.000), and user resistance (β = 0.145, p = 0.017). Similarly, social influence significantly influences digital distrust (β = 0.229, p = 0.000) and low self-efficacy (β = 0.186, p = 0.002), with no significant effect on user resistance (β = 0.048, p = 0.445). Table 5 Summarizes the direct effect results.
The moderating effects
The moderation analysis from SmartPLS indicates significant moderation effects on user resistance for both anticipated regret and digital distrust. The interaction between anticipated regret and digital distrust (β = −0.250, p = 0.000) demonstrates a substantial negative moderation effect on user resistance, indicating that as the interaction between anticipated regret and digital distrust increases, user resistance decreases significantly as shown in Fig. 6. Conversely, the interaction between anticipated regret and low self-efficacy (β = −0.021, p = 0.691) does not exhibit a significant moderation effect on user resistance, suggesting that the combined influence of anticipated regret and low self-efficacy does not significantly impact user resistance. The summary of the moderation effects is presented in Table 5.
Model fit
Several fit indices were used to assess the research’s model fit. The model showed strong predictive power as indicated by the Q2 value, a measure of predictive relevance, indicating that the model accurately predicts the observed data. Predictive relevance is indicated by Q2 values larger than 0. When the values are 0.02, 0.15, and 0.35, respectively, an endogenous construct is considered to have minimal, moderate, or vigorous predictive value for an external construct. There is a high correlation between the latent variables and their corresponding indicators, as evidenced by the F2 value, which represents the effect size of the endogenous latent variables. This explains the absence of F2 values for the exogenous variables, as presented in Table 6. The efficacy of the suggested model in describing the variability in the endogenous variables was demonstrated by the high degree of explanatory power represented by the R2 value, which quantifies the percentage of variance explained by the model. According to Cohen (2013), R2 values should be categorized as low, moderate, or robust if they are, respectively, 0.19, 0.33, and 0.6. R2 values up to 0.10 are reasonable, according to Falk and Miller (1992).
Furthermore, the standardized root mean square residual (SRMR) value, a measure of model fit, was within an acceptable range, indicating a good fit between the proposed model and the observed data. According to a study, an acceptable fit is defined as having an SRMR of <0.08 (Hu and Bentler, 1998). Finally, the Incremental predictive model assessment (IPMA) value (Table 6) provided additional evidence for the model’s predictive accuracy. It indicates that the model performs well in predicting future outcomes based on the observed data, as demonstrated in Fig. 7. Our findings highlight that low self-efficacy and digital distrust, treated as latent variables, exhibit notable importance, with IPMA values indicating their substantial influence on e-health service resistance among older adults. Additionally, social influence indicated the highest importance among the exogenous variables, while information inequality, anticipated regret, and perceived risk are identified as significant factors contributing to resistance to e-health services. These fit indices suggest that the proposed model adequately fits the data and provides a reliable framework for comprehending the relationships between the variables under investigation. All the values for the model fit are presented in Table 6.
Discussion
The structure based on the SOR theory and hypothesis assessment results offers insightful information about the connections between the variables being studied. First, the findings confirmed the validity of hypotheses 1a and 1b, which postulated that information inequality positively affects digital distrust and low self-efficacy. This implies that people subjected to information inequality are more likely to be skeptical of digital technology. This is consistent with the findings of Fan et al. (2021). Also, the findings suggest that older adults subjected to information inequality have low self-esteem regarding their ability to use e-health services efficiently.
The findings, however, did not support hypothesis 1c, which proposed a positive relationship between information inequality and user resistance. This surprising discovery would suggest that user resistance behavior is more significantly influenced by variables other than information inequality. This finding is contrary to a previous study (Khilnani et al., 2020). In the context of resistance to e-health technology among healthcare providers, a previous study has affirmed that physicians, nurses, and other practitioners in the United States healthcare system have opposed the switch from paper to electronic health records (Ngafeeson, 2015). Another study confirmed that unequal access to technology and information can exacerbate feelings of risk and encourage resistance actions among health professionals (Koehle et al., 2022). Therefore, while the findings of our study may be surprising, it is important to consider the broader body of research on this topic, which suggests that information inequality can indeed have a significant impact on user resistance.
Next, we looked at hypotheses 2a, 2b, and 2c, which examined how social influence related to the outcome variables. The findings indicated that social influence had a favorable impact on digital distrust and low self-efficacy but not user resistance. This shows that people’s attitudes and views of digital technology are shaped by social circumstances, which also affect their distrust and confidence in themselves. The finding that social influence positively affects digital distrust is consistent with that of Stoica (2020). Consistent with our findings, several previous studies (Dahri et al., 2023; Malau et al., 2022; Polizzi et al., 2021) have confirmed social influence as an influencing factor on self-efficacy. In the context of this study, we confirm that social influence (informational) contributes to digital distrust and low self-efficacy among older adults. According to Aseidu and Boateng (2020), social influence significantly explains user resistance. However, the finding from our current study is the opposite. A previous study (Yoo et al., 2021) examined the impact of social influence (normative and informational) on user resistance to accepting new technologies. They found a significant positive relationship between normative social influence and user resistance. In other words, individuals who conform to social norms may be more resistant to adopting new technologies or changes in behavior, even if those changes are beneficial. However, their findings confirmed a significant negative relationship between informational social influence and user resistance (Yoo et al., 2021). This suggests that individuals seeking information or advice from others may be less resistant to change as they are more likely to understand its benefits and rationale. This is consistent with our findings, as this current research did not find a significant positive relationship between social influence (informational) and user resistance. While it was initially expected that social influence would significantly contribute to user resistance among older adults, the actual findings of the study suggest the opposite. The study found that social influence (informational) contributes to digital distrust and low self-efficacy among older adults. This highlights the importance of considering the nuances of social influence and user behavior when designing digital technologies for older adult populations.
Similarly, there were substantial positive associations between perceived risk and digital distrust, low self-efficacy, and user resistance according to Hypotheses 3a, 3b, and 3c, which examined the effect of perceived risk on the outcome variables. This suggests that people’s levels of distrust, self-efficacy, and resistance toward e-health services are influenced by their views of the risks involved in using them. Previous studies (Jain and Raman, 2023; Noreen et al., 2021; Yuliati et al., 2020) have asserted that perceived risk has a positive influence on digital distrust, which is consistent with our study. Doan (2021) confirmed that PR influences self-efficacy. Multiple studies (Cambefort and Roux, 2019; Cheng et al., 2014; Kim and Park, 2017; Mohtar and Abbas, 2015) also confirmed that perceived risk positively influences user resistance. These findings are significant given that our study focuses on older persons. They draw attention to perceived risk’s critical role in influencing older people’s attitudes and actions regarding e-health services. The correlations between perceived risks, user resistance, low self-efficacy, and digital distrust highlight older persons’ particular difficulties and worries when embracing and using digital health technologies. The perceived risk associated with e-health services for older persons can originate from several factors, such as worries about data security and privacy, doubts about the accuracy of medical information found online, and issues about the usability and accessibility of digital platforms. These perceived risks can contribute to heightened levels of digital distrust, leading older adults to question the credibility and trustworthiness of e-health technologies. As a result, they may experience diminished self-efficacy, feeling less confident in navigating and utilizing these technologies effectively. Additionally, older adults may exhibit more excellent resistance to adopting e-health services, preferring traditional healthcare methods they perceive as more familiar and reliable.
Finally, in the direct relationship between variables, the findings supported hypothesis 4, which suggested a positive relationship between digital distrust and user resistance but did not support hypothesis 5, which postulated a positive association between low self-efficacy and user resistance. This suggests that resistance to e-health services may not be strongly influenced by an individual’s degree of self-efficacy. Consistently, previous research (Chouk and Mani, 2022; Prakash and Das, 2022) has found that digital distrust highly impacts user resistance in different contexts. This agrees with the results of our study. Previous studies (Yan, 2022; Zhang, 2023) have affirmed that resistance to innovation increases with low self-efficacy. People who fail at tasks more frequently have lower self-efficacy belief in their ability to complete the work successfully. As a result, they have become less open to embracing new technologies. Some other studies (Ellen et al., 1991; Zhang et al., 2017) confirmed a significant relationship between self-efficacy and user resistance, while our study did not find any significant relationship between low self-efficacy and user resistance. The results about the relationship between digital distrust, self-efficacy, and user resistance are significant in the context of our study, which focuses on older adults. According to the supported hypothesis, older persons with a higher level of distrust towards e-health technologies are also more likely to oppose utilizing them. This implies a positive correlation between digital distrust and user resistance. This emphasizes how reluctant older persons are to adopt and use e-health services and how much digital distrust impacts their hesitation.
Moreover, the absence of evidence to support hypothesis 5, which postulated a positive correlation between user resistance and low self-efficacy, implies that older persons’ perceived low self-efficacy may not significantly impact their resistance to e-health services. While low self-efficacy is commonly regarded as a crucial determinant of behavior, particularly in technology adoption contexts, our findings imply that for older adults, factors such as digital distrust may exert a more substantial influence on their resistance to e-health services. These observations shed light on the intricate interactions between psychological variables that influence older individuals’ perceptions of and actions related to e-health technologies. The adoption of digital technology is hindered by digital distrust, although self-efficacy has less of an impact on user resistance among older persons. Consequently, methods to reduce digital distrust and increase confidence in these technologies should be prioritized in treatments to address older individuals’ reluctance to e-health services.
To remove adoption barriers and encourage older individuals’ engagement with digital health solutions, it is imperative to cultivate trust and confidence in e-health services. Policymakers and healthcare professionals should be aware of older persons’ difficulties with digital technologies and design interventions tailored to their needs and concerns. This may involve implementing strategies to enhance transparency, data security, and privacy protections in e-health platforms and providing tailored education and support to improve older adults’ digital literacy and confidence in using these technologies.
Furthermore, the links between digital distrust, low self-efficacy, and user resistance were studied in hypotheses 6 and 7, respectively, to see how anticipated regret moderated those associations. The findings supported hypothesis 6 by showing that the interplay between anticipated regret and digital distrust significantly impacts user resistance. This implies that people who believe they will regret not using e-health services are less likely to resist when they distrust digital technologies. This is consistent with a previous study (Li et al., 2021) in a different context. This finding affirms that older people will adopt e-health services if they anticipate regret despite their distrust of digital technologies. For example, Stevens et al. (2019) discovered that intentions to engage in health-promoting actions are significantly influenced by anticipated regret. When participants expected to feel guilty for not adopting healthier habits, their motivation to do so increased. This also aligns with previous research showing that people often overestimate the impact of potential losses compared to gains, a phenomenon known as the “loss aversion bias.” Some studies (Conner et al., 2015; Ellis et al., 2018; Sniehotta et al., 2014; Stevens et al., 2019) additionally highlighted the significance of including anticipated regret in theoretical models of health behavior since it can offer insightful information about people’s intentions and actions.
On the other hand, as the nonsignificant coefficient for hypothesis 7 shows, the interaction between anticipated regret and low self-efficacy did not significantly affect user resistance. From this, the association between low self-efficacy and resistance behavior by users may not be substantially affected by anticipated regret. These findings emphasize that to promote increased acceptance and utilization of e-health services among older persons, it is critical to eliminate digital skepticism and cultivate a sense of anticipated regret. Techniques to reduce digital distrust, like increasing openness about data security and privacy, could lessen opposition from senior citizens. Furthermore, programs that foster a sense of impending regret—such as emphasizing the possible health advantages and favorable results linked to e-health adoption—might encourage senior citizens to overcome their apprehensions and use digital health technologies.
Theoretical and practical implications
Theoretical contributions
The study’s findings have significant theoretical ramifications for our comprehension of older Nigerians’ aversion to e-health services. First, it provides a thorough model for examining the psychological mechanisms underpinning resistance behavior in digital health technology using the SOR theory. The results corroborate the theoretical connections between user resistance and several variables, including information inequality, social influence, perceived risk, digital distrust, and anticipated regret. This broadens the applicability of SOR theory to the particular situation of older persons in Nigeria and proves its significance in understanding user behavior in the digital health arena.
The study has shown that anticipated regret can significantly reduce the impact of digital distrust on user resistance. This finding highlights the importance of understanding how individual perceptions and emotions affect behavioral responses to technology adoption. Psychological factors such as regret anticipation must be considered when designing interventions to promote the acceptance and utilization of e-health services, especially among older populations.
Practical contributions
For legislators, medical professionals, and developers of e-health services in Nigeria and elsewhere, the research’s conclusions have several applications. First, designing more user-centric e-health solutions can be aided by an awareness of the elements contributing to user resistance. By offering customized information and support resources to elderly users, for example, concerns about information inequality can be addressed, and their confidence and willingness to interact with digital health platforms can increase.
Furthermore, acknowledging the impact of social influence on user attitudes and behaviors highlights the significance of peer support networks and community-based interventions in fostering e-health adoption and literacy. Healthcare professionals can use already-existing social networks and neighborhood associations to help older people learn from one another, share knowledge, and receive training.
Policymakers can also use the results of this study to create focused plans for removing obstacles to older adults’ digital participation and e-health uptake. Enabling digital health solutions into current healthcare systems may entail funding infrastructure and technology training programs, guaranteeing the accessibility and affordability of e-health services, and promoting collaborations between government organizations, technology companies, and healthcare providers.
Sustainable development goals (SDGs) contribution
Addressing the obstacles preventing older people from using e-health services, this research advances the worldwide effort to enhance healthcare outcomes and access in line with SDG 3 (Good Health and Well-Being). This study aims to improve the effectiveness of digital health interventions for older populations in Nigeria and other developing countries by exploring why some users may resist using these interventions. By identifying the underlying factors contributing to user resistance, researchers hope to design more inclusive interventions that lead to better health outcomes and quality of life.
The results also illustrate how social influence and information inequality shape disparities in e-health access and consumption, which has implications for SDG 10 (Reduced Inequalities). Implementing policies that tackle these gaps and foster digital literacy and empowerment among vulnerable populations makes it possible to mitigate healthcare access discrepancies and enhance health equity for all.
Furthermore, the study highlights the significance of inclusive and participatory approaches to digital health policy and governance, which touches on SDG 16 (Peace, Justice, and Strong Institutions). Policies can promote social cohesion and trust in communities and bolster the resilience of healthcare systems by including older adults in the planning and execution of e-health projects and guaranteeing accountability and openness in the decision-making processes.
Finally, by highlighting the necessity of multi-stakeholder collaboration and cooperation in furthering e-health adoption and digital inclusion, the study aligns with SDG 17 (Partnerships for the Goals). To encourage innovation, scale up successful interventions, and solve systemic difficulties in delivering digital health services, stakeholders should use their unique skills and resources by forging collaborations between government, academia, civil society, and the commercial sector.
Conclusion
Finally, because digital technology is developing quickly and the healthcare industry is changing, it is necessary to do continuing studies to track e-health trends. This study clarifies the complex nature of older persons’ resistance to e-health services. Our findings show the need for interventions that foster trust and reduce risk perceptions in e-health programs, emphasizing the significance of addressing perceived risk and digital mistrust as major adoption hurdles. Anticipated regret is a potential moderator of the relationship between digital distrust and user resistance. This finding offers critical new insights into the psychological processes that underlie resistance behavior and suggests directions for focused interventions meant to lessen resistance that stems from distrust. Nonetheless, more investigation is necessary to fully understand the intricate interactions between these variables in light of the surprising lack of support for the proposed association between information inequality and user resistance. This study contributes to the growing body of literature on e-health adoption among older adults, offering practical implications for policymakers and practitioners seeking to enhance the uptake of digital health technologies in aging populations.
Limitations and ideas for further research
Although this work made significant contributions, several issues should be considered. First, the study’s exclusive emphasis on older people in Nigeria limited the applicability of its conclusions to other demographics and environments. Future studies could explore user resistance in diverse cultural settings and demographic groups to better understand its determinants and implications. Second, most of the variables used in the study were self-reported, leaving room for measurement error and social desirability bias. Subsequent investigations may utilize mixed-methods techniques, such as qualitative interviews and observational studies, to validate results and offer a more profound understanding of senior citizens’ actual experiences and viewpoints concerning the adoption of e-health. This study did not evaluate whether demographic groups with and without e-health experience differ in their resistance to e-health services. A potential research question could be: “What are the differences between the resistance of e-health adopters and nonadopters that influence opposition to e-health services?” This study did not investigate the relationship between demographic variables (such as gender) and the findings. Another potential research question is: “How does gender impact the acceptance of e-health services?”
Furthermore, although the study looked at how different factors, directly and indirectly, affect user resistance, the fundamental mechanisms underpinning these correlations still need to be better understood. In the future, the adoption and resistance to e-health services could be studied using longitudinal designs and mediation studies to determine the mediating variables and causal pathways.
Moreover, the study ignored more extensive structural and organizational issues that significantly impact user resistance in favor of concentrating primarily on individual-level factors. Subsequent studies may take a multilevel approach to investigate how organizational culture, healthcare infrastructure, policy frameworks, and organizational culture influence the uptake and application of e-health.
Data availability
All data generated or analyzed during this study are included in this published article.
Change history
09 October 2024
In this article the email for the corresponding author Mingyue Fan was incorrectly given as fanmy@js.edu.cn and should have been fanmy@ujs.edu,cn. The original article has been corrected.
References
Abraham C, Sheeran P (2004) Deciding to exercise: the role of anticipated regret. Br J Health Psychol 9(2):269–278. https://doi.org/10.1348/135910704773891096
Adeleke R (2021) Digital divide in Nigeria: the role of regional differentials. Afr J. Sci Technol Innov Dev 13(3):333–346. https://doi.org/10.1080/20421338.2020.1748335
AlBar AM, Hoque MR (2019) Patient acceptance of e-health services in Saudi Arabia: an integrative perspective. Telemed E-Health 25(9):847–852. https://doi.org/10.1089/tmj.2018.0107
Anderson J, Rainie L (2018) The future of well-being in a tech-saturated world. Pew Research Center: Internet, Science and Tech
Aririguzoh S, Amodu L, Sobowale I, Ekanem T, Omidiora O (2021) Achieving sustainable e-health with information and communication technologies in Nigerian rural communities. Cogent Soc Sci 7(1):1887433. https://doi.org/10.1080/23311886.2021.1887433
Asch SE (1955) Opinions and social pressure. Sci Am 193(5):31–35
Aseidu ST, Boateng R (2020) Exploring the scope of user resistance: a bibliometric review of 41 years of research. In: Boateng R (ed) Handbook of research on managing information systems in developing economies, edited. IGI Global, pp 548–572
Aslam M (2011) User resistance in post ERP implementation. Bus Process Manag J 17:266–275
Bae TJ, Lee CK, Lee Y, McKelvie A, Lee WJ (2024) Descriptive norms and entrepreneurial intentions: the mediating role of anticipated inaction regret. Front Psychol 14:1203394. https://doi.org/10.3389/fpsyg.2023.1203394
Bagozzi RP, Yi Y (1988) On the evaluation of structural equation models. J Acad Mark Sci 16:74–94
Baki R, Birgoren B, Aktepe A (2021) Identifying factors affecting intention to use in distance learning systems. Turk Online J Distance Educ 22(2):Article 2. https://doi.org/10.17718/tojde.906545
Bandura A (1977) Self-efficacy: toward a unifying theory of behavioral change. Psychol Rev 84(2):191–215. https://doi.org/10.1037/0033-295X.84.2.191
Bearden WO, Netemeyer RG, Teel JE (1989) Measurement of consumer susceptibility to interpersonal influence. J Consum Res 15(4):473–481. https://doi.org/10.1086/209186
Brewer NT, DeFrank JT, Gilkey MB (2016) Anticipated regret and health behavior: a meta-analysis. Health Psychol 35(11):1264–1275. https://doi.org/10.1037/hea0000294
Brewer NT, Chapman GB, Rothman AJ, Leask J, Kempe A (2017) Increasing vaccination: putting psychological science into action. Psychol Sci Public Interest 18(3):149–207. https://doi.org/10.1177/1529100618760521
Brooks J, Reed DM, Savage B (2016) Taking off with a pilot: the importance of testing research instruments. In: Benson V, Filippaios G (eds) ECRM2016—Proceedings of the 15th European Conference on Research Methodology for business management. Academic Conferences and Publishing Limited, pp 51–59
Cambefort M, Roux E (2019) A typology of the perceived risks in the context of consumer brand resistance. J Prod Brand Manag 28(5):575–585
Cao Y, Li J, Qin X, Hu B (2020) Examining the effect of overload on the mHealth application resistance behavior of elderly users: an SOR perspective. Int J Environ Res Public Health 17(18):Article 18. https://doi.org/10.3390/ijerph17186658
Caso D, Carfora V, Starace C, Conner M (2019) Key factors influencing Italian mothers’ intention to vaccinate sons against HPV: the influence of trust in health authorities, anticipated regret and past behaviour. Sustainability 11(23):Article 23. https://doi.org/10.3390/su11236879
Caso D, Capasso M, Fabbricatore R, Conner M (2022) Understanding the psychosocial determinants of Italian parents’ intentions not to vaccinate their children: an extended theory of planned behaviour model. Psychol Health 37(9):1111–1131. https://doi.org/10.1080/08870446.2021.1936522
Chang H-J, Eckman M, Yan R-N (2011) Application of the stimulus–organism–response model to the retail environment: the role of hedonic motivation in impulse buying behavior. Int Rev Retail Distrib Consum Res 21(3):233–249
Chaouali W, Yahia IB, Souiden N (2016) The interplay of counter-conformity motivation, social influence, and trust in customers’ intention to adopt Internet banking services: the case of an emerging country. J Retail Consum Serv 28:209–218
Cheng S, Lee S-J, Lee K-R (2014) User resistance of mobile banking in China: focus on perceived risk. Int J Secur Appl 8(2):167–172
Choi HJ, Krieger JL, Hecht ML (2013) Reconceptualizing efficacy in substance use prevention research: refusal response efficacy and drug resistance self-efficacy in adolescent substance use. Health Commun 28(1):40–52. https://doi.org/10.1080/10410236.2012.720245
Chouk I, Mani Z (2022) Does the learning ability of smart products lead to user resistance? J Eng Technol Manag 66:101706
Chua G, Yuen KF, Wang X, Wong YD (2021) The determinants of panic buying during COVID-19. Int J Environ Res Public Health 18(6):3247. https://doi.org/10.3390/ijerph18063247
Cialdini RB, Goldstein NJ (2004) Social influence: compliance and conformity. Annu Rev Psychol 55(1):591–621. https://doi.org/10.1146/annurev.psych.55.090902.142015
Cohen J (2013) Statistical power analysis for the behavioral sciences. Academic Press
Conner M, McEachan R, Taylor N, O’Hara J, Lawton R (2015) Role of affective attitudes and anticipated affective reactions in predicting health behaviors. Health Psychol 34(6):642–652. https://doi.org/10.1037/hea0000143
Coppolino Perfumi S, Bagnoli F, Caudek C, Guazzini A (2019) Deindividuation effects on normative and informational social influence within computer-mediated-communication. Comput Hum Behav 92:230–237. https://doi.org/10.1016/j.chb.2018.11.017
Dahri NA, Al-Rahmi WM, Almogren AS, Yahaya N, Vighio MS, Al-maatuok Q, Al-Rahmi AM, Al-Adwan AS (2023) Acceptance of mobile learning technology by teachers: influencing mobile self-efficacy and 21st-century skills-based training. Sustainability 15(11):8514
de Veer AJE, Peeters JM, Brabers AE, Schellevis FG, Rademakers JJJ, Francke AL (2015) Determinants of the intention to use e-Health by community dwelling older people. BMC Health Serv Res 15:103. https://doi.org/10.1186/s12913-015-0765-8
Deutsch M, Gerard HB (1955) A study of normative and informational social influences upon individual judgment. J Abnorm Soc Psychol 51(3):629–636. https://doi.org/10.1037/h0046408
Doan TTT (2021) The effect of perceived risk and technology self-efficacy on online learning intention: an empirical study in Vietnam. J Asian Financ Econ Bus 8(10):385–393
Donath J (2014) The social machine: designs for living online. MIT Press
Dowling GR, Staelin R (1994) A model of perceived risk and intended risk-handling activity. J Consum Res 21(1):119–134. https://doi.org/10.1086/209386
Ellen PS, Bearden WO, Sharma S (1991) Resistance to technological innovations: an examination of the role of self-efficacy and performance satisfaction. J Acad Mark Sci 19(4):297–307. https://doi.org/10.1007/BF02726504
Ellis EM, Elwyn G, Nelson WL, Scalia P, Kobrin SC, Ferrer RA (2018) Interventions to engage affective forecasting in health-related decision making: a meta-analysis. Ann Behav Med 52(2):157–174. https://doi.org/10.1093/abm/kax024
Ezeudoka BC, Fan M (2024) Determinants of behavioral intentions to use an E-Pharmacy service: insights from TAM theory and the moderating influence of technological literacy. Res Soc Adm Pharm 20(7):605–617. https://doi.org/10.1016/j.sapharm.2024.03.007
Falk RF, Miller NB (1992) A primer for soft modeling. University of Akron Press
Fan M, Ezeudoka BC, Qalati SA (2024) Exploring the resistance to e-health services in Nigeria: an integrative model based upon the theory of planned behavior and stimulus-organism-response. Humanit Soc Sci Commun 11(1):1–14
Fan M, Huang Y, Qalati SA, Shah SMM, Ostic D, Pu Z (2021) Effects of information overload, communication overload, and inequality on digital distrust: a cyber-violence behavior mechanism. Front Psychol 12:643981
Figueiredo A (2018) Information frictions in education and inequality. November 2018 meeting papers, vol 804. Society for Economic Dynamics
Fornell C, Larcker DF (1981) Evaluating structural equation models with unobservable variables and measurement error. J Mark Res 18(1):39–50
George G, Camarata MR (1996) Managing instructor cyberanxiety: the role of self-efficacy in decreasing resistance to change. Educ Technol 36(4):49–54
Haddock C, Wisheart P, New Zealand Mountain Safety Council (1993) Managing risks in outdoor activities/Cathye Haddock. In: Wisheart P (ed) (photographs, Haddock C, Goldring R; illustrations, Sunderland H), Mountain safety manual, 1st edn. New Zealand Mountain Safety Council
Hair JF, Ringle CM, Sarstedt M (2011) PLS-SEM: indeed a silver bullet. J Mark Theory Pract 19(2):139–152
Hamama-Raz Y, Ginossar-David E, Ben-Ezra M (2016) Parental regret regarding children’s vaccines—the correlation between anticipated regret, altruism, coping strategies and attitudes toward vaccines. Isr J Health Policy Res 5(1):55. https://doi.org/10.1186/s13584-016-0116-1
Hargittai E, Hinnant A (2008) Digital inequality: differences in young adults’ use of the Internet. Commun Res 35(5):602–621. https://doi.org/10.1177/0093650208321782
Hashmi H, Attiq S, Rasheed F (2019) Factors affecting online impulsive buying behavior: a stimulus organism response model approach. Market Forces 14(1). https://kiet.edu.pk/marketforces/index.php/marketforces/article/view/392
Henseler J, Ringle CM, Sarstedt M (2015) A new criterion for assessing discriminant validity in variance-based structural equation modeling. J Acad Mark Sci 43:115–135
Hidayanto AN, Anggorojati B, Abidin Z, Phusavat K (2020) Data modeling positive security behavior implementation among smart device users in Indonesia: a partial least squares structural equation modeling approach (PLS-SEM). Data Brief 30:105588
Hox JJ, Bechger TM (1998) An introduction to structural equation modeling [Article]. Struct Equ Model. https://dspace.library.uu.nl/handle/1874/23738
Hu L, Bentler PM (1998) Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychol Methods 3(4):424
Huang T (2023) Using SOR framework to explore the driving factors of older adults smartphone use behavior. Humanit Soc Sci Commun 10(1):Article 1. https://doi.org/10.1057/s41599-023-02221-9
Jacoby J (2002) Stimulus–organism–response reconsidered: an evolutionary step in modeling (consumer) behavior. J Consum Psychol 12(1):51–57. https://doi.org/10.1207/S15327663JCP1201_05
Jain N, Raman TV (2023) The interplay of perceived risk, perceive benefit and generation cohort in digital finance adoption. EuroMed J Bus 18(3):359–379
Joseph RC (2010) Individual resistance to IT innovations. Commun ACM 53(4):144–146. https://doi.org/10.1145/1721654.1721693
Kenny DA (2020) SEM: measuring model fit. https://davidakenny.net/cm/fit.htm. Accessed 30 Apr 2024
Khilnani A, Schulz J, Robinson L (2020) The COVID-19 pandemic: new concerns and connections between eHealth and digital inequalities. J Inf Commun Ethics Soc 18(3):393–403
Kim H-J, Lee J-M, Rha J-Y (2017) Understanding the role of user resistance on mobile learning usage among university students. Comput Educ 113:108–118
Kim H-W, Kankanhalli A (2009) Investigating user resistance to information systems implementation: a status quo bias perspective. MIS Q 33(3):567–582. https://doi.org/10.2307/20650309
Kim MJ, Lee C-K, Jung T (2020) Exploring consumer behavior in virtual reality tourism using an extended stimulus–organism–response model. J Travel Res 59(1):69–89. https://doi.org/10.1177/0047287518818915
Kim S, Park H-S (2017) Impacts of individual and technical characteristics on perceived risk and user resistance of mobile payment services. J Digit Converg 15(12):239–253
Kim W, Kreps GL, Shin C-N (2015) The role of social support and social networks in health information–seeking behavior among Korean Americans: a qualitative study. Int J Equity Health 14(1):40. https://doi.org/10.1186/s12939-015-0169-8
Klaus T, Blanton JE (2010) User resistance determinants and the psychological contract in enterprise system implementations. Eur J Inf Syst 19(6):625–636. https://doi.org/10.1057/ejis.2010.39
Kleijnen M, Lee N, Wetzels M (2009) An exploration of consumer resistance to innovation and its antecedents. J Econ Psychol 30(3):344–357
Kock N (2015) Common method bias in PLS-SEM: a full collinearity assessment approach. Int J E-Collab 11(4):1–10. https://doi.org/10.4018/ijec.2015100101
Koehle H, Kronk C, Lee YJ (2022) Digital health equity: addressing power, usability, and trust to strengthen health systems. Yearb Med Inform 31(1):20–32. https://doi.org/10.1055/s-0042-1742512
Koyuncu B, Dönmez P (2018) Predictive value of sense of self-efficacy and attitudes of high school students for their resistance to mathematics. Univers J Educ Res 6(8):1629–1636
Kumari A, Tanwar S, Tyagi S, Kumar N (2018) Fog computing for Healthcare 4.0 environment: opportunities and challenges. Comput Electr Eng 72:1–13
Kwak J, Park J (2012) Effects of a regulatory match in sunk-cost effects: a mediating role of anticipated regret. Mark Lett 23(1):209–222. https://doi.org/10.1007/s11002-011-9148-z
Laato S, Islam AKMN, Farooq A, Dhir A (2020) Unusual purchasing behavior during the early stages of the COVID-19 pandemic: the stimulus–organism–response approach. J Retail Consum Serv 57:102224. https://doi.org/10.1016/j.jretconser.2020.102224
Langevoort DC (1997) Organized illusions: a behavioral theory of why corporations mislead stock market investors (and cause other social harms). Univ PA Law Rev 146:101
Lapointe L, Rivard S (2005) A multilevel model of resistance to information technology implementation. MIS Q 29(3):461–491. https://doi.org/10.2307/25148692
Li B, Hu M, Chen X, Lei Y (2021) The moderating role of anticipated regret and product involvement on online impulsive buying behavior. Front Psychol 12. https://www.frontiersin.org/journals/psychology/articles/10.3389/fpsyg.2021.732459
Lin J-SC, Chou E-Y, Lin C-Y (2016) What if I make the wrong decision? The role of anticipated regret in switching barrier based customer retention. In: Groza MD, Ragland CB (eds) Marketing challenges in a turbulent business environment. Springer International Publishing, pp. 123–126
Ma W, Tariq A, Ali MW, Nawaz MA, Wang X (2022) An empirical investigation of virtual networking sites discontinuance intention: stimuli organism response-based implication of user negative disconfirmation. Front Psychol 13:862568
Malau M, Indartono S, Tianawati AKA (2022) Learning motivation and authoritative parenting for self-regulated learning: the mediation of self-efficacy. J Pendidik Indones 11(4). https://ejournal.undiksha.ac.id/index.php/JPI/article/view/49822
Marziali E (2009) E-Health program for patients with chronic disease. Telemed E-Health 15(2):176–181. https://doi.org/10.1089/tmj.2008.0082
Matsuo M, Minami C, Matsuyama T (2018) Social influence on innovation resistance in Internet banking services. J Retail Consum Serv 45:42–51. https://doi.org/10.1016/j.jretconser.2018.08.005
Mehrabian A, Russell JA (1974) An approach to environmental psychology. The MIT Press, pp. xii, 266
Mehrotra A, Prewitt E (2019) New marketplace survey: convenient care—opportunity, threat, or both? NEJM Catalyst 5(4)
Ming J, Jianqiu Z, Bilal M, Akram U, Fan M (2021) How social presence influences impulse buying behavior in live streaming commerce? The role of S–O–R theory. Int J Web Inf Syst 17(4):300–320. https://doi.org/10.1108/IJWIS-02-2021-0012
Mohtar S, Abbas M (2015) Consumer resistance to innovation due to perceived risk: relationship between perceived risk and consumer resistances to innovation. J Technol Oper Manag 10(1):1–13
Morahan-Martin J, Schumacher P (2003) Loneliness and social uses of the Internet. Comput Hum Behav 19(6):659–671. https://doi.org/10.1016/S0747-5632(03)00040-2
National Bureau of Statistics (2024) Reports. https://nigerianstat.gov.ng/elibrary/read/1241461. Accessed 26 Apr 2024
Ngafeeson M (2015) Understanding user resistance to information technology in healthcare: the nature and role of perceived threats. 3(1)
Nordgren LF, van der Pligt J, van Harreveld F (2007) Unpacking perceived control in risk perception: the mediating role of anticipated regret. J Behav Decis Mak 20(5):533–544. https://doi.org/10.1002/bdm.565
Noreen M, Ghazali Z, Mia MS (2021) The impact of perceived risk and trust on adoption of mobile money services: an empirical study in Pakistan. J Asian Finance Econ Bus 8(6):347–355
Nunnally J (1978) Psychometric methods, 2nd edn. McGraw-Hill, New York, NY
O’Carroll RE, Ferguson E, Hayes PC, Shepherd L (2012) Increasing organ donation via anticipated regret (INORDAR): Protocol for a randomised controlled trial. BMC Public Health 12(1):169. https://doi.org/10.1186/1471-2458-12-169
O’Carroll RE, Foster C, McGeechan G, Sandford K, Ferguson E (2011) The “ick” factor, anticipated regret, and willingness to become an organ donor. Health Psychol 30(2):236–245. https://doi.org/10.1037/a0022379
Paré G, Jaana M, Sicotte C (2007) Systematic review of home telemonitoring for chronic diseases: the evidence base. J Am Med Inform Assoc 14(3):269–277. https://doi.org/10.1197/jamia.M2270
Peek STM, Wouters EJM, van Hoof J, Luijkx KG, Boeije HR, Vrijhoef HJM (2014) Factors influencing acceptance of technology for aging in place: a systematic review. Int J Med Inform 83(4):235–248. https://doi.org/10.1016/j.ijmedinf.2014.01.004
Polizzi SJ, Zhu Y, Reid JW, Ofem B, Salisbury S, Beeth M, Roehrig G, Mohr-Schroeder M, Sheppard K, Rushton GT (2021) Science and mathematics teacher communities of practice: social influences on discipline-based identity and self-efficacy beliefs. Int J STEM Educ 8(1):30. https://doi.org/10.1186/s40594-021-00275-2
Prakash AV, Das S (2022) Explaining citizens’ resistance to use digital contact tracing apps: a mixed-methods study. Int J Inf Manag 63:102468
Quintal VA, Lee JA, Soutar GN (2010) Tourists’ information search: the differential impact of risk and uncertainty avoidance. Int J Tour Res 12(4):321–333. https://doi.org/10.1002/jtr.753
Regmi PR, Waithaka E, Paudyal A, Simkhada P, van Teijlingen E (2016) Guide to the design and application of online questionnaire surveys. Nepal J Epidemiol 6(4):640–644. https://doi.org/10.3126/nje.v6i4.17258
Reisinger Y, Mavondo F (2005) Travel anxiety and intentions to travel internationally: implications of travel risk perception. J Travel Res 43(3):212–225. https://doi.org/10.1177/0047287504272017
Sampat B, Raj S (2022) Fake or real news? Understanding the gratifications and personality traits of individuals sharing fake news on social media platforms. Aslib J Inf Manag 74(5):840–876. https://doi.org/10.1108/AJIM-08-2021-0232
Sandberg T, Conner M (2008) Anticipated regret as an additional predictor in the theory of planned behaviour: a meta-analysis. Br J Soc Psychol 47(4):589–606. https://doi.org/10.1348/014466607X258704
Scholtz SE (2021) Sacrifice is a step beyond convenience: a review of convenience sampling in psychological research in Africa SA J Ind Psychol 47(1):1–12
Sha Y, Yan J, Wang Z (2015) Public trust on the Red Cross Society of China after Ya’an earthquake: analysis based on sentiment analysis of microblog data. J Public Manag 12:93–104
Shahzad MF, Xu S, Baheer R (2024) Assessing the factors influencing the intention to use information and communication technology implementation and acceptance in China’s education sector. Humanit Soc Sci Commun 11(1):Article 1. https://doi.org/10.1057/s41599-024-02777-0
Slade EL, Dwivedi YK, Piercy NC, Williams MD (2015) Modeling consumers’ adoption intentions of remote mobile payments in the United Kingdom: extending UTAUT with innovativeness, risk, and trust. Psychol Mark 32(8):860–873. https://doi.org/10.1002/mar.20823
Sniehotta FF, Presseau J, Araújo-Soares V (2014) Time to retire the theory of planned behaviour. Health Psychol Rev 8(1):1–7. https://doi.org/10.1080/17437199.2013.869710
Statista (2020) Nigeria: old population by gender. https://www.statista.com/statistics/1260768/elderly-population-in-nigeria-by-gender/. Accessed 30 Apr 2024
Statista (2024) Africa number of internet users by country. https://www.statista.com/statistics/505883/number-of-internet-users-in-african-countries/. Accessed 26 Apr 2024
Stevens CJ, Gillman AS, Gardiner CK, Montanaro EA, Bryan AD, Conner M (2019) Feel good now or regret it later? The respective roles of affective attitudes and anticipated affective reactions for explaining health-promoting and health risk behavioral intentions. J Appl Soc Psychol 49(6):331–348. https://doi.org/10.1111/jasp.12584
Stoica A (2020) From social influence to cyber influence. The role of new technologies in the influence operations conducted in the digital environment. Int J Cyber Dipl 1(1):27–35
Talwar S, Dhir A, Islam N, Kaur P, Almusharraf A (2023) Resistance of multiple stakeholders to e-health innovations: integration of fundamental insights and guiding research paths. J Bus Res 166:114135
Tanwar S, Parekh K, Evans R (2020) Blockchain-based electronic healthcare record system for healthcare 4.0 applications. J Inf Secur Appl 50:102407. https://doi.org/10.1016/j.jisa.2019.102407
Tsai C-L, Cho M-H, Marra R, Shen D (2020) The Self-efficacy Questionnaire for online Learning (SeQoL). Distance Educ 41(4):472–489. https://doi.org/10.1080/01587919.2020.1821604
United Nations (2022) World population prospects—Population Division. https://population.un.org/wpp/. Accessed 28 Nov 2023
van der Linden S (2022) Misinformation: susceptibility, spread, and interventions to immunize the public. Nat Med 28(3):460–467. https://doi.org/10.1038/s41591-022-01713-6
Wong AKC, Bayuo J, Wang S, Kwan RYC, Lam SC, Wong FKY (2023) Factors associated with the perceptions of eHealth technology of Chinese nurses and nursing students. Nurse Educ Pract 69:103605. https://doi.org/10.1016/j.nepr.2023.103605
World Health Assembly (2005) Fifty-eighth World Health Assembly, Geneva, 16–25 May 2005: resolutions and decisions: annex (WHA58/2005/REC/1). World Health Organization. https://apps.who.int/iris/handle/10665/20398
Yan S (2022) Lack of self-efficacy and resistance to innovation impact on insufficient learning capabilities: mediating the role of demotivation and moderating the role of institutional culture. Front Psychol 13. https://doi.org/10.3389/fpsyg.2022.923577
Yoo J, Choi S, Hwang Y, Yi MY (2021) The role of user resistance and social influences on the adoption of Smartphone: moderating effect of age. J Organ End Use Comput 33(2):36–58. https://doi.org/10.4018/JOEUC.20210301.oa3
Yuliati LN, Dradjat HA, Simanjuntak M (2020) Online bike: role of perceived technology, perceived risk, and institution-based trust on service usage via online trust. Cogent Bus Manag 7(1):1798067. https://doi.org/10.1080/23311975.2020.1798067
Zhang H (2023) Technostress, academic self-efficacy, and resistance to innovation: buffering roles of knowledge sharing culture and constructive deviant behavior. Psychol Res Behav Manag 16:3867–3881. https://doi.org/10.2147/PRBM.S424396
Zhang X, Han X, Dang Y, Meng F, Guo X, Lin J (2017) User acceptance of mobile health services from users’ perspectives: the role of self-efficacy and response-efficacy in technology acceptance. Inform Health Soc Care 42(2):194–206. https://doi.org/10.1080/17538157.2016.1200053
Author information
Authors and Affiliations
Contributions
Brendan Chukwuemeka Ezeudoka and Mingyue Fan made equal and significant contributions to all aspects of the research, including conceptualization, design, data analysis, manuscript preparation, and final approval for submission. This work was supported by the National Social Science Funds of China under Grant [number 22BGL102].
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The study adhered to the ethical guidelines outlined by the American Psychological Association. It received approval from the Ethics Committee of the Management School at Jiangsu University. Approval was assigned ethical approval number JU-ECMS-2024-015, ensuring compliance with ethical standards for research involving human subjects.
Informed Consent
Prior to participation, all individuals were thoroughly briefed on the study’s objectives, procedures, risks, and benefits. They were assured of their right to withdraw at any stage without consequence. Written consent was obtained, aligning with ethical guidelines.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ezeudoka, B.C., Fan, M. Exploring the impact of digital distrust on user resistance to e-health services among older adults: the moderating effect of anticipated regret. Humanit Soc Sci Commun 11, 1190 (2024). https://doi.org/10.1057/s41599-024-03457-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1057/s41599-024-03457-9
This article is cited by
-
Uncovering ‘Weak signals’ through patient journey mapping to inform the future redesign of the medical consultation room
BMC Health Services Research (2026)
-
The potentials of digital technology in social prescribing: a qualitative study of key stakeholders’ perspectives
BMC Public Health (2025)
-
Identifying the challenges of a telecare system establishment for older adults and providing a solution: a qualitative study
BMC Geriatrics (2025)