Abstract
This study aims to explore how different forms and cumulative experiences of childhood maltreatment (CM) relate to cognitive biases. A total of 121 participants diagnosed with major depressive disorder (MDD) and 120 healthy controls (HC) were recruited for this cross-sectional study. CM and cognitive biases were assessed, respectively, utilizing the Childhood Trauma Questionnaire and the Cognitive Bias Questionnaire. The latter evaluates two distinct dimensions of cognitive biases: depression and distortion, according to which cognitive characteristics were categorized into four combinations: depressed-distorted (D-D), depressed-nondistorted (D-ND), nondepressed-distorted (ND-D), and nondepressed-nondistorted (ND-ND). The Childhood Maltreatment Count (CMC) was defined as the cumulative count of distinct CM types. The findings indicate the association between CM and cognitive bias among the participants. In the MDD cohort, a significant association was observed between higher physical neglect scores and diminished ND-ND scores (β = –0.297, p = 0.012). In the HC group, no comparable relationship was identified. Furthermore, CMC was significantly correlated with decreased ND-ND scores both in the MDD group (β = −0.273, p = 0.006) and the HC group (β = −0.234, p = 0.010). This study underscores the significance of investigating the repercussions of physical neglect in MDD patients. Moreover, increased childhood trauma counts may function as a predisposing factor for more pronounced cognitive bias, with potential implications for clinical interventions and future research in diverse cultural contexts.
Similar content being viewed by others
Introduction
Childhood maltreatment (CM), encompassing physical, emotional, and sexual abuse, as well as neglect, has a profound and long-lasting impact on individuals, influencing their emotional, social, and psychological development (Cohen et al., 2014). Research has consistently demonstrated that CM significantly increases the risk of various mental health disorders, particularly Major Depressive Disorder (MDD) (Zhou et al., 2022). MDD is a debilitating condition characterized by persistent feelings of sadness, worthlessness, and loss of interest, severely affecting an individual’s ability to function in daily life (Otte et al., 2016). Those who have experienced CM are at higher risk for depression due to the psychological and emotional scars left by early life adversities (Nelson et al., 2017a). One key psychological mechanism underlying MDD is the presence of cognitive biases (Fossati, 2018). Cognitive biases refer to the distorted thinking patterns and negative cognitive schemas that shape how individuals perceive and interpret the world around them (Korteling & Toet, 2020). These biases often manifest as negative self-schemas, where individuals view themselves in a consistently negative light, and attentional biases, where negative stimuli are more readily noticed and processed (Mehl et al., 2018). These cognitive distortions significantly contribute to the development and maintenance of depressive symptoms by reinforcing feelings of helplessness and hopelessness (Milligan, 2013). Existing literature has suggested that CM is a critical factor in the development of these cognitive biases (Su et al., 2019). Children who experience maltreatment are more likely to internalize negative beliefs about themselves and the world, which later emerge as maladaptive cognitive patterns in adulthood. These biases not only exacerbate depressive symptoms but also increase vulnerability to emotional dysregulation and interpersonal difficulties (Bennett et al., 2023). Thus, understanding how CM influences cognitive biases is essential for comprehending the complex dynamics that lead to depression, particularly among adults with MDD.
The relationship between CM and cognitive biases is complex and multifaceted. Cognitive biases such as negative self-schemas (Mehl et al., 2018), selective attention to negative stimuli (Ao et al., 2020), and biased interpretations of events (Marsh, 2022) have been shown to contribute to the onset and persistence of MDD significantly. These biases can be understood as cognitive distortions that cause individuals to interpret the world through a negative lens, reinforcing depressive symptoms and further perpetuating negative emotional states. Early experiences of CM have been found to shape cognitive patterns in such a way that individuals are more likely to adopt distorted and maladaptive thinking styles in adulthood (Pilkington et al., 2021). CM, particularly emotional and physical abuse, can distort an individual’s sense of self-worth, leading to a negative view of the world and an inability to process information in a balanced way. This cognitive distortion makes it harder for individuals to challenge negative thoughts and emotions, ultimately increasing their vulnerability to mental health issues such as MDD (Serine, 2016). Furthermore, cognitive biases, especially those related to negative self-perception and the tendency to ruminate on negative experiences, can significantly intensify the emotional distress caused by CM (Zhang et al., 2024). These biased thinking patterns may exacerbate feelings of helplessness and hopelessness, which are hallmark features of depression. Thus, understanding how CM contributes to the development of these cognitive biases is essential for identifying the pathways through which childhood experiences influence adult mental health. In sum, the interplay between CM and cognitive biases creates a cyclical pattern in which maltreated individuals are more likely to develop negative cognitive patterns that increase their susceptibility to depression. This study seeks to explore this relationship more deeply, focusing on how CM influences cognitive biases in Chinese adults with MDD.
Theoretical framework
The connection between CM and cognitive biases in the development of MDD can be explained through established psychological theories. One of the most influential frameworks in understanding depression is Beck’s Cognitive Theory of Depression (Beck, 1967), which posits that individuals with depression often hold negative cognitive schemas that shape how they perceive themselves, the world, and the future. These schemas lead to biased thinking, where negative events are overemphasized, and positive experiences are ignored or discounted. Individuals with MDD often interpret situations through a lens of hopelessness and helplessness, reinforcing the depressive cycle (Milligan, 2013). In the case of individuals who have experienced CM, these negative cognitive schemas are likely formed during early development, where experiences of abuse or neglect lead to the formation of distorted self-perceptions and maladaptive cognitive patterns (Mehl et al., 2018). CM can exacerbate existing cognitive vulnerabilities, making it harder for individuals to engage in adaptive coping mechanisms and leading to persistent cognitive biases that contribute to ongoing depressive symptoms (Serine, 2016). This theory aligns with the idea that CM acts as a catalyst for the formation of biased thinking and that these biases, in turn, fuel depression.
Additionally, the Broaden-and-Build Theory of positive emotions (Fredrickson, 2001) provides insight into how mindfulness, a key factor in emotional regulation, might mediate the effects of cognitive biases. The theory suggests that positive emotions foster resilience, flexibility, and cognitive reappraisal, which can mitigate the negative effects of maladaptive cognitive patterns. This theoretical backdrop supports the notion that enhancing mindfulness can help individuals with CM and MDD regulate emotional responses and reduce cognitive biases that perpetuate the depressive cycle. Finally, the Biopsychosocial Model (Engel, 1977) offers a comprehensive understanding by incorporating biological, psychological, and social factors in the study of mental health. CM is a social stressor that influences both biological (neurobiological changes) and psychological factors (cognitive patterns), which contribute to the development of depression (McCrory et al., 2022). This model underscores the need to explore both the individual psychological processes (cognitive biases) and the environmental factors (CM) that shape mental health outcomes.
The present study
Although substantial research has examined the individual effects of CM and cognitive biases in relation to mental health, particularly MDD, the link between CM and cognitive biases remains underexplored, especially in the context of Chinese adults. Many studies have separately investigated the impact of childhood adversities on depression, focusing on how experiences such as abuse or neglect contribute to emotional dysregulation and negative self-schemas (Engstrom et al., 2021). Similarly, extensive research has been conducted on cognitive biases in depression, exploring how biased thinking patterns perpetuate depressive symptoms (Dolan, 2018). However, few studies have directly addressed how CM influences the development of cognitive biases, particularly in adult populations suffering from MDD. Therefore, there is a significant gap in the literature regarding the relationship between CM and cognitive biases among Chinese adults with MDD. This study aims to address this gap by exploring how early-life adversities influence cognitive distortions in Chinese adults and how these biases contribute to depressive symptoms. By doing so, this research will provide valuable insights into the psychological mechanisms linking childhood experiences and adult depression and offer guidance for clinical interventions in a Chinese cultural context.
Consequently, this study aims to investigate the relationship between different forms and cumulative experiences of CM and the development of cognitive biases in individuals with MDD. Specifically, it explores how various types of CM, including emotional, physical, and sexual abuse, as well as neglect, contribute to the formation of biased cognitive patterns in adults diagnosed with MDD. By examining these associations, the study seeks to deepen our understanding of how early traumatic experiences may shape cognitive processing and mental health outcomes in adulthood. Specifically, the objectives of the study are:
-To investigate the association between CM and cognitive bias in Chinese adults with MDD.
-To examine whether specific forms of CM (e.g., emotional abuse, physical neglect) predict cognitive biases in MDD patients.
-To explore whether the number of different types of CM correlates with the severity of cognitive bias.
Methods
Participants and procedure
The data for this study were derived from a longitudinal project investigating the biological and psychological mechanisms of MDD (hypothalamic-pituitary-adrenal axis function and magnetic resonance imaging study of trauma-related depression, registration number: ChiCTR1800014591). Demographic and clinical characteristics, depression, anxiety, CM, and cognitive bias scores of 121 MDD patients and 120 healthy controls (HCs) were collected for analysis. The diagnosis for the MDD group was made according to the DSM-IV criteria, confirmed by two psychiatrists using the Structured Clinical Interview for DSM-IV (SCID-IV).
Inclusion criteria for MDD group follow: (a) participants aged 18 to 60 years, (b) diagnosed with MDD according to the DSM-IV criteria based on the SCID-IV clinical interview, and (c) a total score of ≥19 on the 24-item Hamilton Depression Rating Scale (HAMD-24), indicating moderate to severe depression. Exclusion Criteria for MDD Group follows: (a) suicidal ideation or history of suicide attempts; (b) severe physical conditions, such as neurological disorders, head injuries, or other major health issues; (c) history of other DSM-IV psychiatric disorders, (d) substance dependence or abuse, excluding tobacco use, and (e) perinatal period.
Inclusion criteria for HCs follow: (a) no history of mental illness or substance abuse (excluding tobacco), and (b) a HAMD-24 score ≤8, indicating no depressive symptoms. Participants with any history of psychiatric disorders or substance abuse were excluded from the HCs group.
Measures
Depression
Depression was assessed using the 24-item Hamilton Depression Rating Scale (HAMD24), a widely used clinician-report scale of depression (Max Hamilton, 1960). The scale includes 24 items that evaluate various aspects of depression, with its Chinese version demonstrating good reliability and validity within the Chinese population (Tang & Zhang, 1984).
Anxiety
Anxiety was assessed using the 14-item Hamilton Anxiety Rating Scale (HAMA14), a clinician-report scale consisting of 14 items, each rated from 0 to 4 (Hamilton M, 1959). The Chinese adaptation of the HAMA14 has demonstrated strong reliability and validity within the Chinese community (Wang C et al., 2011).
Childhood maltreatment
CM was assessed using the Childhood Trauma Questionnaire (CTQ), which contains 28 items scaled by a 5-point Likert to assess the extent of agreement (1 = never true; 5 = very often true). The CTQ, a retrospective assessment tool, has been proven reliable and valid within the Chinese population (Zhao et al., 2005). The CTQ assesses five subtypes of CM: emotional abuse (EA), physical abuse (PA), sexual abuse (SA), emotional neglect (EN), and physical neglect (PN). Participants meeting at least one of the following score criteria were identified as having CM history: EA ≥ 13, PA ≥ 10, SA ≥ 8, EN ≥ 15, and PN ≥ 10 (Bernstein et al., 2003). The Childhood Maltreatment Count (CMC) is determined by tallying up the CTQ components that exceed their designated threshold levels. Its score ranges from zero to five.
Cognitive bias
Cognitive bias was assessed using the Cognitive Bias Questionnaire (CBQ). The CBQ is designed to measure negative cognitive bias associated with depression. It consists of two dimensions: depression and cognitive distortion (Krantz & Hammen, 1979). The scale describes six common situations, three for interpersonal relationships and three for self-achievement. Responses to three or four questions in each situation reflect four combination types of both depression and distortion dimensions: depressed-distorted (D-D), depressed-nondistorted (D-ND), nondepressed-distorted (ND-D), and nondepressed-nondistorted (ND-ND). A total of 23 questions were asked, and the scores for each combination type were obtained based on the response count for each type, ranging from 0 to 23, which means the total score of four types was 23 for each participant. Dimension score of biased cognition (sum of D-D, D-ND, and ND-D scores) was denoted as the degree of biased cognition.
Statistical analysis
The analytic procedure was conducted using SPSS (v26.0), with a statistically significant threshold set at p < 0.05 (two-tailed). Differences in categorical and continuous variables between the MDD and HC groups were analyzed using the rank sum test. To test the first hypothesis, partial correlation analysis was performed on the entire sample, with age, gender, and education controlled as covariates. The distortion dimension score was a correlative variable for CM (CTQ total score) and MDD (HAMD24 total score). Hierarchical regression models were utilized to test the second and third study objectives to examine the impact of specific forms of CM and CMC on the CBQ subscale scores. Before conducting the regression analysis, multicollinearity was assessed, and the Durbin-Watson test was performed to ensure the statistical assumptions were met. The results indicated no significant issues with multicollinearity or autocorrelation, and therefore, the regression results were deemed valid. Then, hierarchical regression analyses were performed at three levels in MDD and HC groups to determine whether CM forms improved predictions of CBQ subscales. In the HC group, the three hierarchies of the regression model were as follows: level 1: age, gender, and education; level 2: HAMA14 and HAMD24 total scores; and level 3: EA, PA, SA, EN, and PN. As for the MDD group, three variables (total history, current history, and episodes) were added to level 2.
Results
Demographic and clinical information, CTQ scores, and CBQ scores
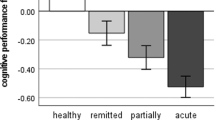
Two hundred forty-one participants met the eligibility criteria, including 121 MDD patients and 120 HC participants. There was no significant difference in age between the MDD and HC groups. The proportion of males was higher in the HC group (55.7%) than in the MDD group (43.1%), and the education level was higher in the HC group than in the MDD group (p < 0.01). The HAMD24 and HAMA14 total scores in the MDD group were significantly higher than in the HC group (p < 0.001). Table 1 demonstrates both groups’ clinical demographic data and CTQ and CBQ scores. The MDD group exhibited a higher prevalence of CM (59.5%) than the HC group (44.2%). On the CTQ, there were significant differences between the MDD and HC groups on the total score (p = 0.002) and the following three CM subscales: EA (p < 0.001), EN (p = 0.012), PN (p = 0.022) and CMC (p = 0.005). Significant differences were observed between the MDD and HC groups in all four categorical dimensions of CBQ (all p-values < 0.01). The MDD group had higher subscales D-D and D-ND scores, while the HC group had higher scores in the subscales ND-D and ND-ND.
In our entire sample, most participants (48.5%) reported at least one type of CM, 25.3% reported at least two types of CM, 6.1% reported at least three types of CM, 2.4% reported at least four types of CM, and none reported five types of CM.
Partial correlation analysis
The partial correlation analysis in Table 2 showed that in the HC group, CM was positively correlated with biased cognition (r = 0.259, p < 0.01) and depression (r = 0.218, p < 0.05), indicating that higher levels of CM were associated with increased cognitive biases and depressive symptoms. However, in the MDD group, there was no significant correlation between CM and depression (r = 0.070, p > 0.05), though a weak positive correlation existed between biased cognition and depression (r = 0.133, p > 0.05), suggesting that the relationship between CM and depressive symptoms may be less direct in individuals already diagnosed with MDD. These results suggested that CM had a more significant impact on cognitive biases and depression in healthy controls, whereas, in MDD patients, the relationship was less pronounced.
Hierarchical regression analysis of CM types on CBQ subscale scores
Table 3 and Table 4 showed the results of hierarchical regression analysis of CM types on CBQ subscale scores within the MDD and HC groups. The analysis was conducted in the MDD group at three levels, including level 1: age, gender, and education; level 2: HAMA14, HAMD24, total history, current history, episode; and level 3: CM. In the HC group, there were only two variables at level 2: HAMD24 and HAMA14. For the MDD group, introducing CM types into the model resulted in a statistically significant ΔR² of 12.0% (p = 0.012), with a standard coefficient (−0.297) for PN in ND-ND score. There was no statistically significant ΔR² in other CBQ subscales. In the HC group, no statistical significance of ΔR² was observed in any CBQ subscales.
Table 5 shows the results of the hierarchical regression analysis of CMCs on CBQ subscale scores in the MDD (n = 121) and the HC (n = 120) groups. In the MDD group, CMC was associated with lower scores in the ND-ND subscale (ΔR² = 6.1%, p = 0.006, β = −0.273). Within the HC group, elevated CMC was associated with higher scores in the D-D subscale (ΔR² = 3.1%, p = 0.046, β = 0.187) and lower scores in the ND-ND subscale (ΔR² = 4.9%, p = 0.010, β = −0.234).
Discussion
To the best of our knowledge, the present investigation is one of the few studies examining the association between CM and cognitive bias, specifically among Chinese MDD patients. The findings showed that physical neglect significantly influenced ND-ND among MDD patients. This study also observed that elevated CMC correlates with lower ND-ND scores in both groups.
In Beck’s model of depression, cognitive mechanisms are postulated as potential prerequisites for the presence of encompassing negative automatic thinking, negative beliefs (related to oneself, the world, and/or the future), and even the final depressive symptoms. It has been suggested that these negative cognitive biases might result from adverse childhood experiences (Beck AT, 1987; Mannarino & Cohen, 1996). We found that individuals with MDD had significantly higher cognitive bias scores compared to the HC group, consistent with previous research (Nelson et al., 2017b; Nieto et al., 2020). Furthermore, we also observed that the HC group exhibited higher scores in the ND-D dimension, which includes numerous items reflecting external attributions, where blame is attributed to external factors. Conversely, according to the hopelessness theory of depression, depressed patients are inclined to interpret the causes of adverse life events as their fault (Abramson et al., 1989), which seems to suggest a difference in attribution patterns between MDD patients and healthy individuals.
While cognitive theories posit an association between childhood events and bias processing, this linkage has recently received limited attention. There have also been efforts to explore the neurobiological underpinnings of Beck’s theory. For instance, researchers have found that the adverse cognitive bias in depression is facilitated through increased influence on subcortical emotion processing regions and diminished top-down cognitive control (Disner et al., 2011). Interestingly, studies have also identified a connection between childhood trauma and subcortical brain structural abnormalities associated with mental illnesses such as depression (Frodl et al., 2017). The existing literature primarily focuses on the relationship between CM and cognitive bias within psychiatric populations. For instance, a systematic review on psychosis identified an association between CM and external locus of control, a specific type of cognitive bias (Croft et al., 2021). Additionally, a survey of 6772 young individuals in Poland found that CM may indirectly influence psychotic experiences through cognitive bias and cannabis use (Frydecka et al., 2020). In contrast, our study addresses a significant gap in the literature by examining the relationship between CM and cognitive bias, specifically within the depressed population.
Our study revealed a negative association between physical neglect and ND-ND scores in the MDD group. On account of the sum of all four combination types of CBQ being a fixed value, it can be concluded that physical neglect is positively correlated with negative and distorted cognitive processes (D-D, D-ND, and ND-D dimensions). Prior research has indicated that individuals who have undergone sexual abuse during childhood are prone to external attributions in adverse situations (Mannarino & Cohen, 1996). However, our study did not observe a significant correlation between a history of childhood sexual abuse and cognitive biases in either group. This discrepancy may be attributed to the potential underreporting of sexual abuse influenced by feelings of shame, as well as the variations in the employment of diverse assessment tools.
Additionally, our investigation did not identify significant associations between other forms of CM and cognitive bias. Similarly, a survey conducted within a British cohort of 8,928 individuals found that all forms of childhood trauma were linked to diminished psychological well-being in adulthood. However, abuse was reported to be unrelated to cognitive abilities, emphasizing the impact of childhood neglect on cognitive and social burdens (Geoffroy et al., 2016).
Physical neglect has been an easily overlooked CM subtype in previous studies. The harms of physical neglect, which are not limited to cognitive problems associated with depression, are also frequently underestimated. A study found that childhood physical neglect was a strong predictor of violent behaviors among adolescent males (McGuigan, 2018). This finding is clinically relevant, as it suggests that early experiences of physical neglect may contribute to the development of dysfunctional cognitive patterns that persist into adulthood and are associated with depression. This association is consistent with Beck’s cognitive theory, which posits that childhood adversities, including physical neglect, contribute to the formation of negative self-schemas and cognitive distortions. These distorted cognitive patterns play a significant role in the onset and maintenance of depressive symptoms (Beck AT, 1987; Mannarino & Cohen, 1996). Additionally, our findings aligned with the metacognitive and cognitive processual perspectives, which emphasize that early maltreatment can lead to dysfunctional metacognitive beliefs, increased levels of repetitive negative thinking (rumination and worry), and impairments in social cognition and neurocognition. Several studies have shown that adults with a history of CM exhibit higher levels of rumination and worry, as well as deficits in social cognition and neurocognition (Mansueto, Caselli, et al., 2019; Mansueto et al., 2021). These dysfunctional cognitive processes, in turn, exacerbate emotional distress and contribute to the development of mood disorders such as MDD. Our findings are consistent with the broader cognitive perspective, which suggests that CM, particularly physical neglect, is associated with more dysfunctional cognitive processes in adulthood. These cognitive biases, including negative self-perception, selective attention to negative stimuli, and biased interpretations of life events, are core components of the cognitive mechanisms underlying depression. Therefore, individuals exposed to early maltreatment are more likely to develop maladaptive cognitive patterns that increase their vulnerability to depressive symptoms and hinder their ability to cope with stress in adulthood. We believe that integrating these insights into clinical practice can enhance the diagnosis and treatment of MDD patients with a history of physical neglect.
Despite the continuous development of rural revitalization in China, many left-behind children (LBC) remain in rural areas. They lack parental care and are prone to physical neglect. A meta-analysis of neglect among LBC in China showed that the incidence and severity of physical neglect in LBC were significantly higher than those in non-LBC (Wen et al., 2021). Neglected children can have serious lifelong consequences, such as anxiety, depression, suicide, and substance abuse (Varese et al., 2012). Given the strong correlation between physical neglect and cognitive bias, as well as the prediction of cognitive bias modification on the treatment outcome of mental disorders (Li et al., 2023), physical neglect in patients with mental disorders deserves more attention to better guide our clinical work. Meanwhile, there is an urgent need to strengthen the care and protection of neglected children and pay attention to the mental health problems of those suffering from physical neglect.
Although cognitive biases and CM are acknowledged as vulnerability factors for depression, limited focus has been directed toward the exploration of the impact of diverse CM types and CMC on cognitive biases with the same samples. Several epidemiological studies have investigated exposure to multiple types of childhood trauma being substantially correlated with the development of depression (Novelo et al., 2018) and posing a considerable risk of potential psychosocial consequences (Ford & Delker, 2018). Multiple childhood traumas may serve as an indicator of the development of mental health issues (Negele et al., 2015). According to Raj et al., an increase in specific CM types among MDD patients is associated with various forms of dysfunctional attitudes (Jugessur et al., 2021). Adverse childhood experiences often lead to the formation of dysfunctional core beliefs about oneself and the external world (Beck, 2008). These dysfunctional core assumptions play a fundamental role in cognitive bias, wherein information is construed and processed consistently with these underlying assumptions (Beck AT, 1987).
The present study contributes to and expands upon the existing body of knowledge. The findings revealed that increased CMC was associated with reduced ND-ND types in MDD and HC cohorts. This observation suggests that an elevated number of childhood trauma types is linked to increased cognitive difficulties. Furthermore, a positive correlation was observed between CMC and D-D dimension among individuals without preexisting mental health conditions, thereby emphasizing the link between experiencing multiple childhood traumas and the presence of D-D cognition associated with depression. This suggests that childhood traumas may powerfully shape later depressive and distorted cognitions, aiding in understanding and identifying key risk factors in depression development.
The findings of this study may be influenced by cross-cultural factors, particularly the Chinese cultural context in which the research was conducted. In China, cultural norms around family loyalty and the stigma associated with reporting abuse may affect the willingness of individuals to acknowledge or report the experiences of CM openly. In some cases, physical neglect and other forms of maltreatment may be underreported due to societal pressures or family-based dynamics that discourage disclosure. Furthermore, the impact of CM on cognitive biases may be shaped by Chinese attitudes towards mental health and emotional expression. In Chinese culture, there may be a tendency to minimize emotional vulnerability and emphasize resilience and family cohesion, which may influence how cognitive biases related to self-worth and stress are formed and manifested. The role of cultural values in shaping the cognitive processes involved in MDD suggests the need for culturally sensitive interventions when addressing the effects of CM and depression in Chinese populations.
Clinical implications
The findings of this study highlighted the significant role of CM, particularly physical neglect, in shaping cognitive biases among individuals with MDD. These results underscore the importance of integrating assessments of childhood trauma into clinical evaluations for individuals presenting with depressive symptoms. A more comprehensive approach to MDD diagnosis should include screening for CM history, as it may provide insight into underlying cognitive distortions that contribute to the persistence of depressive symptoms.
Given the observed association between physical neglect and cognitive biases, targeted interventions focusing on modifying maladaptive cognitive patterns may enhance treatment outcomes. Cognitive bias modification (CBM) and cognitive restructuring techniques, which have been shown to be effective in addressing distorted self-perceptions, may be particularly beneficial for this subgroup of MDD patients(Mansueto, Caselli, et al., 2019; Mansueto, Schruers, et al., 2019). Incorporating such strategies into psychotherapeutic approaches, such as Cognitive Behavioral Therapy (CBT), may help patients challenge negative cognitive schemas, improve emotional regulation, and reduce the severity of depressive symptoms.
The results also supported the growing emphasis on personalized treatment strategies for MDD. Patients with a history of CM, particularly physical neglect, may benefit from tailored interventions that specifically address the long-term effects of early trauma on cognitive and emotional functioning (Mannarino & Cohen, 1996; Mansueto, Caselli, et al., 2019; Mansueto et al., 2021). Approaches such as sequential treatment models and personalized medicine frameworks could offer more effective interventions by considering the unique childhood experiences that shape cognitive vulnerabilities in MDD patients (Cosci et al., 2020).
Moreover, the study’s findings highlighted the need for early intervention programs aimed at individuals who have experienced CM, even before the onset of clinical depression. Preventive measures, including early trauma screening, resilience-building interventions, and mental health education, could help mitigate the development of cognitive biases and reduce the risk of chronic depressive episodes later in life. From a public health perspective, these findings also reinforce the importance of policies and programs that aim to reduce CM and provide supportive environments for individuals with a history of neglect or abuse. Mental health professionals, educators, and policymakers should collaborate to integrate trauma-informed care into mental health services, ensuring that individuals affected by early-life adversity receive the necessary psychosocial support to improve long-term mental well-being.
Limitations
The present study is subject to several inherent constraints. Firstly, it should be acknowledged that the CTQ, as a retrospective assessment of CM, is susceptible to confounding factors, such as the presence of concurrent mental health conditions, including symptoms of depression (Colman et al., 2016). However, previous research has suggested that no significant disparity exists when comparing retrospective and prospective studies regarding CM (Scott et al., 2012). Secondly, the CBQ used in this study does not categorize specific subtypes of cognitive biases. This limitation aligns with our research objectives, which prioritize investigating the presence of cognitive biases rather than delving into specific instances. Future research should aim to elucidate the significance of various cognitive biases in the pathological progression of depression.
Additionally, our study’s cross-sectional design prevents the establishment of causal relationships and limits the ability to generalize the findings beyond the current study area. This preliminary exploratory study demonstrates the feasibility of its design but highlights the need for a more comprehensive longitudinal study across various cultural regions to establish causal relationships. Another limitation is related to the potential underreporting of certain forms of CM, such as sexual abuse, due to stigma and embarrassment. To mitigate this, we placed significant emphasis on safeguarding participants’ privacy and providing humanistic care during the data collection process. Nevertheless, the possibility of selective reporting remains a limitation. Lastly, it is important to note that medication use was not considered as a potential confounding factor in this study. Medications, particularly those used in the treatment of MDD, can influence cognitive biases and mental health outcomes. Future studies should incorporate an assessment of medication history to understand better its role in the relationship between CM and cognitive biases. This would provide a more holistic view of the cognitive and emotional mechanisms contributing to MDD.
Conclusion
The present study demonstrates a pioneering approach in utilizing various forms of CM to anticipate cognitive bias, distinguishing itself as a distinct contribution within the limited number of entities investigating the relationship between CM and cognitive bias among individuals with depression in China. Our study revealed a significant association between physical neglect and cognitive bias in individuals diagnosed with MDD. This finding emphasizes the societal importance of addressing physical neglect within the Chinese context, warranting further investigation and scholarly attention. Moreover, our findings conclude that elevated levels of CMCs can predict the heightened severity of cognitive bias. Hence, it can be argued that there is a need for increased societal involvement in conducting extensive screening and preventive measures for CM. Such societal involvement may facilitate the early identification of potential risks by medical professionals, enabling proactive interventions on behavioral and psychological levels to enhance the prognosis of MDD.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
References
Abramson LY, Metalsky GI, Alloy LB (1989) Hopelessness depression: a theory-based subtype of depression. Psychol Rev 96(2):358–372
Ao X, Mo L, Wei Z, Yu W, Zhou F, Zhang D (2020) Negative bias during early attentional engagement in major depressive disorder as examined using a two-stage model: High sensitivity to sad but bluntness to happy cues. Front Hum Neurosci 14:593010
Beck AT (1967) Depression: Clinical, experimental, and theoretical aspects. Harper Row Google Schola 2:103–113
Beck AT (2008) The evolution of the cognitive model of depression and its neurobiological correlates. Am J Psychiatry 165(8):969–977. https://doi.org/10.1176/appi.ajp.2008.08050721
Beck AT (1987) Cognitive models of depression. J Cogn Psychother Int Q 1:5–37
Bennett EM, Gray P, Lau JYF (2023) Early life maltreatment and adolescent interpretations of ambiguous social situations: Investigating interpersonal cognitions and emotional symptoms. J Child Adolesc Trauma 16(1):1–8
Bernstein DP, Stein JA, Newcomb MD, Walker E, Pogge D, Ahluvalia T, Stokes J, Handelsman L, Medrano M, Desmond D, Zule W (2003) Development and validation of a brief screening version of the Childhood Trauma Questionnaire. Child Abus Negl 27(2):169–190. https://doi.org/10.1016/S0145-2134(02)00541-0
Cohen LJ, Tanis T, Bhattacharjee R, Nesci C, Halmi W, Galynker I (2014) Are there differential relationships between different types of childhood maltreatment and different types of adult personality pathology? Psychiatry Res 215(1):192–201
Colman I, Kingsbury M, Garad Y, Zeng Y, Naicker K, Patten S, Jones PB, Wild TC, Thompson AH (2016) Consistency in adult reporting of adverse childhood experiences. Psychol Med 46(3):543–549
Cosci F, Mansueto G, Fava GA (2020) Relapse prevention in recurrent major depressive disorder. A comparison of different treatment options based on clinical experience and a critical review of the literature. Int J Psychiatry Clin Pract 24(4):341–348
Croft J, Martin D, Madley-Dowd P, Strelchuk D, Davies J, Heron J, Teufel C, Zammit S (2021) Childhood trauma and cognitive biases associated with psychosis: A systematic review and meta-analysis. PLoS ONE 16(2):e0246948. https://doi.org/10.1371/journal.pone.0246948
Disner SG, Beevers CG, Haigh EAP, Beck AT (2011) Neural mechanisms of the cognitive model of depression. Nat Rev Neurosci 12(8):467–477. https://doi.org/10.1038/nrn3027
Dolan H (2018) Childhood trauma, negative schemas, and trust: an exploration using virtual reality. UCL (University College London)
Engel GL (1977) The need for a new medical model: a challenge for biomedicine. Science 196(4286):129–136
Engstrom M, Liu G, Santana-Gonzalez C, Teoh JY, Harms M, Koy K, Quevedo K (2021) The impact of child abuse on the neurobiology of self-processing in depressed adolescents. Neurobiol Stress 14:100310
Ford JD, Delker BC (2018) Polyvictimization in childhood and its adverse impacts across the lifespan: Introduction to the special issue. J Trauma Dissociation 19(3):275–288. https://doi.org/10.1080/15299732.2018.1440479
Fossati P (2018) Is major depression a cognitive disorder? Rev Neurologique 174(4):212–215
Fredrickson BL (2001) The role of positive emotions in positive psychology: The broaden-and-build theory of positive emotions. Am Psychol 56(3):218
Frodl T, Janowitz D, Schmaal L, Tozzi L, Dobrowolny H, Stein DJ, Veltman DJ, Wittfeld K, van Erp TGM, Jahanshad N, Block A, Hegenscheid K, Völzke H, Lagopoulos J, Hatton SN, Hickie IB, Frey EM, Carballedo A, Brooks SJ, Grabe HJ (2017) Childhood adversity impacts on brain subcortical structures relevant to depression. J Psychiatr Res 86:58–65. https://doi.org/10.1016/j.jpsychires.2016.11.010
Frydecka D, Misiak B, Kotowicz K, Pionke R, Krężołek M, Cechnicki A, Gawęda (2020) The interplay between childhood trauma, cognitive biases, and cannabis use on the risk of psychosis in nonclinical young adults in Poland. Eur Psychiatry 63(1):e35. https://doi.org/10.1192/j.eurpsy.2020.31
Geoffroy M-C, Pinto Pereira S, Li L, Power C (2016) Child neglect and maltreatment and childhood-to-adulthood cognition and mental health in a prospective birth cohort. J Am Acad Child Adolesc Psychiatry 55(1):33–40.e3. https://doi.org/10.1016/j.jaac.2015.10.012
Hamilton M (1959) The assessment of anxiety states by rating. Br J Med Psychol 32:50–55. https://doi.org/10.1111/j.2044-8341.1959.tb00467.x
Jugessur R, Zhang Y, Qin X, Wang M, Lu X, Sun J, Dong Q, Zhang L, Liu J, Ju Y, Liao M, Wan P, Guo H, Zhao F, Liu B, Li L (2021) Childhood maltreatment predicts specific types of dysfunctional attitudes in participants with and without depression. Front Psychiatry 12:728280. https://doi.org/10.3389/fpsyt.2021.728280
Korteling JE, Toet A (2020) Cognitive biases. Encyclopedia of Behavioral Neuroscience
Krantz S, Hammen C (1979) Assessment of cognitive bias in depression. J Abnorm Psychol 88(6):611–619
Li J, Ma H, Yang H, Yu H, Zhang N (2023) Cognitive bias modification for adult’s depression: a systematic review and meta-analysis. Front Psychol 13:968638. https://doi.org/10.3389/fpsyg.2022.968638
Mannarino AP, Cohen JA (1996) Abuse-related attributions and perceptions, general attributions, and locus of control in sexually abused girls. J Interpers Violence 11(2):162–180. https://doi.org/10.1177/088626096011002002
Mansueto G, Caselli G, Ruggiero GM, Sassaroli S (2019) Metacognitive beliefs and childhood adversities: an overview of the literature. Psychol Health Med 24(5):542–550. https://doi.org/10.1080/13548506.2018.1550258
Mansueto G, Cavallo C, Palmieri S, Ruggiero GM, Sassaroli S, Caselli G (2021) Adverse childhood experiences and repetitive negative thinking in adulthood: a systematic review. Clin Psychol Psychother 28(3):557–568. https://doi.org/10.1002/cpp.2590
Mansueto G, Schruers K, Cosci F, van Os J, Alizadeh BZ, Bartels-Velthuis AA, van Beveren NJ, Bruggeman R, Cahn W, de Haan L, Delespaul P, Meijer CJ, Myin-Germeys I, Kahn RS, Schirmbeck F, Simons CJP, van Haren NEM, van Winkel R (2019) Childhood adversities and psychotic symptoms: the potential mediating or moderating role of neurocognition and social cognition. Schizophrenia Res 206:183–193. https://doi.org/10.1016/j.schres.2018.11.028
Marsh EM (2022) Cognitive biases in perfectionism: attention bias and memory bias for perfectionism-relevant and negative stimuli. Illinois State University
Hamilton Max (1960) A rating scale for depression. J Neurol Neurosurg Psychiatry 23(23):56–62. https://doi.org/10.1136/jnnp.23.1.56
McCrory E, Foulkes L, Viding E (2022) Social thinning and stress generation after childhood maltreatment: a neurocognitive social transactional model of psychiatric vulnerability. Lancet Psychiatry 9(10):828–837
McGuigan WM (2018) Physical neglect in childhood as a predictor of violent behavior in adolescent males. Child Abus 79:395–400
Mehl S, Schlier B, Lincoln TM (2018) Does CBT for psychosis have an impact on delusions by improving reasoning biases and negative self-schemas? Zeitschrift Für Psychologie 226(3):152–163. https://doi.org/10.1027/2151-2604/a000335
Milligan K (2013) Cognitive distortions as a mediator between early maladaptive schema and hopelessness. PCOM Psychol Diss 256. https://digitalcommons.pcom.edu/psychology_dissertations/256
Negele A, Kaufhold J, Kallenbach L, Leuzinger-Bohleber M (2015) Childhood trauma and its relation to chronic depression in adulthood. Depression Res Treat 2015:1–11. https://doi.org/10.1155/2015/650804
Nelson J, Klumparendt A, Doebler P, Ehring T (2017a) Childhood maltreatment and characteristics of adult depression: meta-analysis. Br J Psychiatry 210(2):96–104
Nelson J, Klumparendt A, Doebler P, Ehring T (2017b) Childhood maltreatment and characteristics of adult depression: meta-analysis. Br J Psychiatry 210(2):96–104. https://doi.org/10.1192/bjp.bp.115.180752
Nieto I, Robles E, Vazquez C (2020) Self-reported cognitive biases in depression: a meta-analysis. Clin Psychol Rev 82:101934. https://doi.org/10.1016/j.cpr.2020.101934
Novelo M, von Gunten A, Gomes Jardim GB, Spanemberg L, Argimon II, de L, Nogueira EL (2018) Effects of childhood multiple maltreatment experiences on depression of socioeconomic disadvantaged elderly in Brazil. Child Abus Negl 79:350–357. https://doi.org/10.1016/j.chiabu.2018.02.013
Otte C, Gold SM, Penninx BW, Pariante CM, Etkin A, Fava M, Mohr DC, Schatzberg AF (2016) Major depressive disorder. Nat Rev Dis Prim 2(1):1–20
Pilkington PD, Bishop A, Younan R (2021) Adverse childhood experiences and early maladaptive schemas in adulthood: a systematic review and meta‐analysis. Clin Psychol Psychother 28(3):569–584
Scott KM, McLaughlin KA, Smith DAR, Ellis PM (2012) Childhood maltreatment and DSM-IV adult mental disorders: comparison of prospective and retrospective findings. Br J Psychiatry 200(6):469–475
Serine A (2016) The relationship between cognitive distortions and ADHD after accounting for depression, anxiety, and personality pathology. PCOM Psychol Diss 403. http://digitalcommons.pcom.edu/psychology_dissertations/403
Su Y, D’Arcy C, Yuan S, Meng X (2019) How does childhood maltreatment influence ensuing cognitive functioning among people with the exposure of childhood maltreatment? A systematic review of prospective cohort studies. J Affect Disord 252:278–293
Tang H, Zhang M (1984) HAMD. Shanghai Ment Heal Cent 2:61–64
Varese F, Smeets F, Drukker M, Lieverse R, Lataster T, Viechtbauer W, Read J, van Os J, Bentall RP (2012) Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective- and cross-sectional cohort studies. Schizophrenia Bull 38(4):661–671. https://doi.org/10.1093/schbul/sbs050
Wang C, Chu Y, Zhang Y, Zhang N, Zhang J, Yang N (2011) Study on factor structure of hamilton rating scale for anxiety. J Clin Psychiatry 21:299–301
Wen Y-J, Hou W-P, Zheng W, Zhao X-X, Wang X-Q, Bo Q-J, Pao C, Tang Y-L, Tan T, Li X-B, Wang C-Y (2021) The neglect of left-behind children in China: a meta-analysis. Trauma, Violence, Abus 22(5):1326–1338. https://doi.org/10.1177/1524838020916837
Zhang Y, Xu W, McDonnell D, Wang J-L (2024) The relationship between childhood maltreatment subtypes and adolescent internalizing problems: the mediating role of maladaptive cognitive emotion regulation strategies. Child Abus Negl 152:106796
Zhao X, Zhang Y, Li L, Zhou Y (2005) Evaluation on reliability and validity of Chinese version of childhood trauma questionnaire. Chin J Clin Rehabilitat 9(16):209–211
Zhou J, Fan A, Zhou X, Pao C, Xiao L, Feng Y, Xi R, Chen Y, Huang Q, Dong B (2022) Interrelationships between childhood maltreatment, depressive symptoms, functional impairment, and quality of life in patients with major depressive disorder: a network analysis approach. Child Abus Negl 132:105787
Acknowledgements
We want to express our gratitude to all participants in the present study. This study was supported by the Natural Science Foundation of Hunan Province, China (2024JJ2085 to BL), the National Key Research and Development Program of China (2019YFA0706200 to LL and YZ), the STI2030-Major Projects (2021ZD0202000 to YZ), the National Science and Technologic Program of China (2015BAI13B02 to LL), the Defense Innovative Special Region Program (17-163-17-XZ-004-005- 01 to LL), the National Natural Science Foundation of China (81171286 & 91232714 to LL, and 81601180 to ML) and the Fundamental Research Funds for the Central Universities of Central South University (2024ZZTS0933 to JX).
Author information
Authors and Affiliations
Contributions
ML, BL, YZ, LL, and JX contributed to the study's conception and design. JX, JL, YJ, MW, JS, XL, QD, LZ, PW, HG, and FZ are responsible for participant recruitment and data collection. JX and JL did the data analysis and wrote the first draft of the manuscript and revisions. ML, BL, MX, SR, and JX contributed substantial revisions to the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
The study was conducted following the Declaration of Helsinki. The study was approved by the ethics committee of the Zhumadian Psychiatric Hospital [approval number: 2013 (002)] and the ethics committee of the Second Xiangya Hospital of Central South University [approval number: 2012 (238)]. All authors confirmed that all methods followed relevant guidelines and regulations.
Informed consent
All participants provided written informed consent prior to data collection. The consent process emphasized voluntary participation, anonymity of responses, and the exclusive use of data for academic research. Participants confirmed their understanding of these terms before proceeding with the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Xiong, J., Xu, M., Rehman, S. et al. Exploring the relationship between childhood maltreatment and cognitive bias in Chinese adults with major depressive disorder. Humanit Soc Sci Commun 12, 443 (2025). https://doi.org/10.1057/s41599-025-04732-z
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1057/s41599-025-04732-z