Abstract
Climate change and diabetes pose the dual challenges to human health, yet there is a lack of evidence regarding future health burden of diabetes attributable to climate change. In this study, we used three-stage analytic strategy to project the heat-related and heatwave-related diabetes deaths by demographic characteristics and regions, during 2010–2100 in 32 major Chinese cities. Under SSP5-8.5 (high carbon emission scenario), heat-related attributable fraction of diabetes mortality is projected to rise from 2.3% (95% empirical confidence interval [eCI]: 1.1%, 3.6%) in the 2010s to 19.2% (95% eCI: 10.2%, 32.5%) in the 2090s, and estimated heatwave-related attributable fractions will increase from 0.8% (95% eCI: 0.6%, 1.0%) in the 2010s to 9.3% (95% eCI: 6.7%, 11.8%) in the 2090s. We projected that the number of heat- and heatwave-related diabetes deaths would increase from 1525 (95% eCI: 759, 2431) and 529 (95% eCI: 382, 668) in the 2010s, to 12,956 (95% eCI: 6861, 21,937) and 6312 (95% eCI: 4557, 7972) in the 2090s, respectively. Under SSP1-2.6, SSP2-4.5, and SSP3-7.0 (lower carbon emissions), we projected much lower future heat- and heatwave-related diabetes mortality burdens. Our findings might provide new insights for the development of protecting patients with diabetes from increasing temperature.
Similar content being viewed by others
Introduction
Diabetes mellitus is a major public health concern. Without proper control, diabetes could lead to many health problems, including significant harm to the heart, kidneys, feet and eyes1,2. In 2021, the Global Diabetes Atlas published by the International Diabetes Federation, reported approximately 537 million cases of diabetes among individuals aged 20–79 worldwide, and 6.7 million diabetes deaths. The number of diabetes cases could reach 783 million by 20303. The prevalence of diabetes in China has increased due to changes in lifestyle, diet, and living environments, soaring from less than 1% in 19804 to 12.4% in 20185. Currently, China has the highest number of diabetes cases, with approximately 140 million diabetes patients aged 20–796.
To mitigate public burden from the serious consequences of diabetes, efforts have been made to identify potential risk factors in recent years7. In addition to changes in lifestyle and diet, environmental factors have become important risk factors for diabetes8. High temperatures were found to be associated with health outcomes of diabetes7. Individuals with diabetes are especially vulnerable to heat exposure due to underlying factors such as impaired thermoregulation and increased risk of dehydration9,10. However, current evidence regarding the effect of heat on diabetes mortality is inconclusive. For example, a multi-city study in China revealed that the mortality risk of diabetes increased by 29% (95%CI: 11%, 47%) during days with temperature over 90th percentile11. He and coauthors reported that high temperatures were associated with 10% (95%CI: 6%, 14%) increase of diabetes mortality in Thailand12.
As a prolonged period of extreme high temperature (ie, at least three consecutive days with daily temperature over 95th percentile13), heatwave was also reported to be linked with risk of diabetes. For instance, Xu and his colleagues conducted a cohort in Brisbane and found hospitalizations for diabetes increased by 37%, during high-intensity heatwave days (i.e., at least two consecutive days with temperature over 97th percentile)8. A systematic review reported an 18% increase in diabetes mortality associated with heatwave exposure14. Furthermore, these studies have primarily focused on present and historical associations, without exploring the future effects of extreme heat on diabetes mortality. In addition, previous research from single city or multiple cities do not accurately capture the national death toll9,10,15. China represents a typical example for assessing the impact of future climate change on diabetes mortality, with the largest diabetic population6. It is important to quantify its future heat- and heatwave-related diabetes mortality burdens.
The frequency and intensity of hot days and heatwaves are rapidly increasing as climate change accelerates16. For the planning of future diabetes prevention and control strategies in China, it is important for us to quantify and provide a clear picture of the future heat- and heatwave-related diabetes mortality burdens. This study aimed to project the future heat- or heatwave-related diabetes deaths by demographic characteristics and regions under different climate change scenarios.
Results
Descriptive results
A total of 127,300 deaths from diabetes were recorded in the 32 cities from 2007 to 2013, with 66,129 deaths in the southern cities and 61,171 deaths in the northern cities (Supplementary Table S1). The SSP5-8.5 scenario consistently exhibits a steep increase in projected ambient temperatures throughout this century (Fig. 1), while the SSP1-2.6 scenario indicates the slowest temperature rise after 2050. By 2100, the mean ambient temperature in China is projected to rise by 1.3 °C under the SSP1-2.6 scenario and by 5.1 °C under the SSP5-8.5 scenario, compared with 2010s. By the 2090s, the southern cities are projected to experience a higher temperature increase (5.2 °C compared with 2010s vs 4.9 °C in northern cities) under the SSP5-8.5 scenario (Supplementary Table S2).
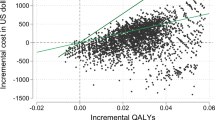
Baseline relationship between temperature and diabetes mortality
Figure 2 shows the overall cumulative relationship between temperature and diabetes mortality for 10 days between May and September during 2007–2013 in China. The baseline relationship between daily mean temperature and diabetes death during hot season shows a J-shaped curve, with the mortality risk increasing when temperature exceeds the minimum mortality temperature (MMT) of 28.3 °C.
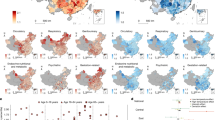
Heat-related attributable fraction of diabetes mortality
Under all climate change scenarios, the number of heat-related diabetes deaths shows an upward trend in the future (Fig. 3). Under the scenario characterized by high carbon emissions (i.e., SSP5-8.5), the heat-attributable fraction of diabetes deaths would increase from 2.3% (95% eCI: 1.1%, 3.6%) in the 2010s, 4.2% (95% eCI: 2.3%, 6.8%) in the 2030s, 7.4% (95% eCI: 4.4%, 12.9%) in the 2050s to 19.2% (95% eCI: 10.2%, 32.5%) in the 2090s (Supplementary Table S3). The projected heat-attributable fraction of diabetes deaths is the smallest under the SSP1-2.6, rising from 2.3% (95% eCI: 1.1%, 3.6%) in the 2010s to 3.8% (95% eCI: 2.0%, 5.7%) in the 2030s, 4.6% (95% eCI: 2.4%, 7.0%) in the 2050s and 4.6% (95% eCI: 2.1%, 7.6%) in the 2090s, respectively. The number of heat-related diabetes deaths is projected to be 1520 (95% eCI: 768, 2415) and 1525 (95% eCI: 759, 2431) in the 2010s, and 3097 (95% eCI: 1437, 5118) and 12,956 (95% eCI: 6861, 21,937) in the 2090s, under the SSP1-2.6 and SSP5-8.5 scenarios, respectively (Table 1).
The projected heat-attributable fraction of diabetes mortality under the SSP5-8.5 scenarios increases faster in the south compared to the north. Individuals aged over 75 years old, and the illiterate are projected to have higher heat-attributable fraction of diabetes mortality (Fig. 3 and Supplementary Table S3). For example, the projected fraction attributable to heat in the 2090s under SSP5-8.5 scenarios are 19.1% (95% eCI: 8.9%, 34.1%) for the youth, and 21.1% (95% eCI: −11.0%, 43.8%) for the elderly, respectively; 21.3% (95% eCI: 10.1%, 37.7%) and 15.4% (95% eCI: 5.1%, 29.5%) for the illiterate and individuals with higher levels of education, respectively. Table 1 presents the number of heat-related diabetes deaths by demographic characteristics.
Heatwave-related attributable fraction of diabetes mortality
Heatwave-related attributable fraction of diabetes mortality is comparatively smaller, compared to those of heat-related burden (Fig. 4). However, the heatwave-related attributable fraction of diabetes mortality increases at a faster rate. By the 2030s, heatwave-related mortality is projected to increase to more than twice the level observed in the 2010s, and will reach approximately 3.0-11.6 times the level observed in the 2010s by the 2090s (Supplementary Table S4). For instance, the estimated heatwave-related attributable fractions are 0.8% (95% eCI: 0.6%, 1.0%) in the 2010s, 2.1% (95% eCI: 1.5%, 2.7%) in the 2030s, 4.2% (95% eCI: 3.0%, 5.3%) in the 2050s and 9.3% (95% eCI: 6.7%, 11.8%) in the 2090s, respectively, under the SSP5-8.5 scenario. The number of heatwave-related deaths is expected to rise from 529 (95% eCI: 382, 668) in the 2010s to 6312 (95% eCI: 4557, 7972) in the 2090s under SSP5-8.5 scenario (Table 2). In addition, under other three climate change scenarios with lower carbon emissions (SSP1-2.6, SSP2-4.5, and SSP3-7.0), we projected much lower future heatwave-related diabetes mortality burdens (1588, 3223 and 4874 in 2090s respectively). Furthermore, people living in the southern cities, females, those under 74 years of age, and the illiterate are projected to be more adversely affected by future heatwaves. Compared to the 2010s, the heatwave-related attributable risk in the 2090s is projected to increase by 11.4 times in the southern region, 10.9 times among females, 11.0 times among individuals aged 75 years or older, and 10.8 times for the illiterate, under the SSP5-8.5.
Sensitivity analyses
The sensitivity analyses indicate the reliability of our results when we changed the dfs of covariates and additionally adjusted for API and GDP per capita (Supplementary Tables S5, 6). Furthermore, when excluding one city each time, the effect estimates remained stable (Supplementary Tables S7–10). For using different heatwave definitions, we observed slightly higher effect estimates of heatwave for those defined using lower temperature thresholds (Supplementary Tables S11, 12), which may be due to more heatwave days for the lower temperature thresholds.
Discussion
This study is the first projection of diabetes mortality associated with heat and heatwave under different climate change scenarios. Our findings indicated that, under the SSP5-8.5 scenario, heat- and heatwave-related diabetes mortality in China would increase by 1.6 times and 10.7 times from 2010s to 2090s, respectively. The future heat-related diabetes mortality is more prominent for people in the southern region, those with low educational attainment, and older adults.
Our study finds that heat and heatwave both elevate the risk of diabetes mortality, which is consistent with prior research about the association between heat and diabetes mortality11,12,17,18 (Supplementary Table S13). However, comparing our effect estimates with previous studies is challenging due to different health outcome variables. Most previous studies focused on the effects of heat or heatwave on non-accidental deaths and cardiopulmonary disease19,20,21,22. For example, Zhang et al. focused on the impact of heat on non-accidental mortality, and reported that heat-related number of non-accidental mortality during 2021–2040 would be 1.5–2.0 times higher than current levels under the SSP1-2.6 scenario22. However, our study estimated the impact of heat on diabetes mortality, and found that even under a low-emission pathway (SSP1-2.6), by 2090, the attributable number of diabetes mortality for heat-related or heatwave-related will still be 3,097 (95% eCI: 1437, 5118) and 1588 (95% eCI: 1146, 2005), that are two times and three times higher than in the 2010s. In addition, we found that the attributable fractions (AF) of heat have increased much more rapidly than those for heatwaves from the 2010s to the 2090s under the four shared socioeconomic pathways (SSPs) scenarios. This could be due to most heat-related deaths attributed to exposure to moderate heat23,24. Although heatwaves pose a higher relative risk to health, the number of heatwave days is fewer, contributing to a relatively smaller health burden compared to moderate heat23. Our study highlights stricter actions to reduce greenhouse gas emissions to mitigate climate change for improved population health outcomes.
The underlying mechanism for the association between heat/heatwave and diabetes mortality may be related to impaired thermoregulation due to autonomic neuropathy, including sweat gland dysfunction and reduced blood flow during heat exposure25. During hot weather, the peak effect of insulin may increase, thereby increasing the risk of hypoglycemic episodes26. The change in the insulin may predispose patients with type 1 diabetes to a diabetic ketoacidosis (DKA) state27,28, and patients with type 2 diabetes to hypertonic hyperglycemia status (HHS)9. The current evidence on the association between heat exposure and DKA is inconclusive. For instance, a Brazilian study reported that heat exposure was not associated with hospitalization for DKA29. However, Miyamura and coauthors reported that heat exposure (comparing 90th percentile of temperature to the 75th percentile of temperature) was associated with a higher risk of hospitalizations for DKA, with relative risk of 1.23 (95%CI: 1.13, 1.33)9. It could be speculated that the effect of high temperature on DKA is due to poorly administered insulin (such as insulin pump malfunction and reduced insulin bioactivity) during extreme heat days. Up to 30% of DKA cases were caused by insulin precipitating in liquid or bubbles leading to catheter blockage30. Lopez and colleagues reported that bubbles formed in insulin pump catheters and syringes when temperatures rise from 4 °C to 37 °C31. Additionally, insulin activity may decrease when exposed to high temperature. Pingel and coauthors reported that insulin stored at 25 °C would lose about 2% of its bioactivity over 5 weeks, and stored at 40 °C would lose 5% over 4 weeks32. Further experimental research is still warranted to elucidate the mechanism underlying the impact of heat exposure on DKA. In addition, diabetes patients always have other health conditions, such as stroke, heart attack and kidney failure. These comorbidities may further affect the ability of heat dissipation, increasing susceptibility to thermal effects in people with diabetes12,26.
Mortality burden of diabetes associated with future high temperature is significantly higher in southern China compared to northern China. Our results align with a previous study about heat-related mortality conducted across 195 sites in China22. In addition, a recent study conducted in 105 Chinese counties also confirmed that heat-related deaths in the southern region exceeded those in the northern region30. Moreover, the increase rate in the southern region is projected to surpass that of the northern region under various climate change scenarios33. The possible explanation may be that southern regions are generally warmer and more humid than northern regions, and people in this environment are more susceptible to heat stroke and other heat-related health problems. Secondly, the southern region has a higher degree of urbanization, a higher density of buildings, a lower coverage of green space, and a lack of proper shade and ventilation facilities, which may exacerbate the impact of high temperatures on deaths33. These findings provide useful evidence for developing tailored intervention strategies to address the burden of heat-induced diabetes deaths34. It is crucial to closely monitor the health status of diabetic patients in southern China, particularly in high-temperature conditions.
Our study finds that the elderly were more vulnerable to heat effects14,34, which can be attributed to the impaired thermoregulation of heat and chronic comorbidities35. In term of education, our findings indicate that future heatwaves could result in a higher number of diabetes deaths among people with lower educational levels. This trend may be attributed to the factor that those individuals with lower educational levels mainly engaged in outdoor physical work, have lower incomes, and were unable to access quality healthcare services and housing with cooling facilities34,36. Additionally, our study shows an interesting finding regarding the differential impact of future heat and heatwave on males and females. Specifically, females were more affected by heatwave, while males were generally more susceptible to moderate high temperature. We speculate that these disparities may be attributed to the physiological differences and workplace environments between males and females. Generally, males are more prone to exposure to outdoor high-temperature environment due to work-related factors, while during the continuous high temperature periods such as heatwaves, most outdoor job are halted due to government regulations, work health and safety policies, leading both men and women to stay indoors.
This study has several public health implications. Firstly, we projected that the number of diabetes mortality attributable to heat and heatwave-related will increase significantly, particularly, under the SSP5-8.5 scenarios. The SSP5-8.5 scenario assumes that future energy consumption will be dominated by fossil energy and emphasizes economic development as the orientation. The health sector should collaborate with other sectors to reshape our energy systems, consumption behaviors and lifestyles in order to reduce the adverse health impacts37. Relevant government departments should give priority to clean energy and coordinate economic development to build a sustainable environment. Heat-related diabetes deaths were more prevalent among the elderly and individuals with lower incomes, underscoring the importance of special care for vulnerable groups. Implementing heat early warning systems, along with and community education programs, ensuring well-insulated housing, and increasing greenspaces in urban areas can effectively mitigate this risk37. Simultaneously, long-term planning for climate-resilient urban settlements is needed38. For individuals with diabetes, enhancing the awareness of climate change hazards is imperative to reduce their health risks in the context of high temperatures. During hot weather, it is recommended to minimize outdoor activities, use air conditioning or adequate ventilation, adhere to medication regimens, and regularly monitor blood sugar levels.
The limitations of this study should be acknowledged. Firstly, historical air temperature data collection relied on stationary weather monitoring stations, which may be subject to exposure measurement bias34. Secondly, changes in the population adaptation and MMT over time were not considered. Previous studies often used scenarios where adaptation improves by a fixed percentage each decade, but the actual degree of this adaptation remains uncertain and challenging to predict accurately39. Thirdly, we applied current heat-mortality association to projecting the future heat-related burden, which may result in an underestimation of heat-related excess deaths. Finally, we failed to consider future demographic shifts that could potentially lead to an overestimation or underestimation of the future heat-related burden. Thus, future research should incorporate these factors for a more comprehensive assessment and projections.
In conclusion, the burden of heat-related diabetes mortality in China is projected to increase significantly in the future, especially under the high carbon emission scenario. People living in southern China, the elderly, and people with lower educational levels will bear a more substantial burden of heat-related diabetes mortality as climate change progresses. This study highlights the importance of integrating climate change considerations into the design, planning and implementation of future diabetes prevention programs.
Methods
Study region
This study included 32 major cities from 2007 to 2013 (Supplementary Fig. S1), covering a wide range climate zones in China40. To examine the differences in the impact of heat and heatwaves between northern and southern regions, we divided the cities along the North-South Line of China41.
Data collection
We collected daily diabetes death counts of the 32 cities from 2007 to 2013 from the Chinese Center for Disease Control and Prevention. International Classification of Diseases (10th Revision) was utilized to categorize deaths from diabetes, with codes of E10-E14. The daily counts of diabetes mortality were further stratified by demographic characteristics such as age (0–74 years and above 75 years), gender, and educational level (illiterate and primary school or above).
Daily meteorological data at the city level were obtained from the China Meteorological Data Service Center (http://data.cma.cn/), including daily mean temperature, maximum temperature, minimum temperature, relative humidity, and average wind speed34. Daily air quality index (API) data were collected from the Chinese Ministry of Ecology and Environment. The annual gross domestic product (GDP) per capita for each city was collected from city-level or country-level statistical yearbook.
Projected temperature data under four climate change scenarios (shared socioeconomic pathways [SSP] SSP1-2.6, SSP2-4.5, SSP3-7.0, SSP5-8.5) from 1961 to 2100 were downscaled from 27 general circulation models (GCMs) provided in Phase 6 of the Coupled Model Intercomparison Project Phase 6 (CMIP6)42. We used the NWAI-W statistical downscaling model to perform both spatial and temporal downscaling of the projected GCM datasets43,44. Spatial downscaling approach was conducted using inverse distance-weighted interpolation of the monthly GCM data, based on the four closest grid points. The monthly values of the spatial downscaled GCMs were then bias-corrected using, adjusting for deviations from historical recorded temperatures. Finally, an updated version of the Weather Generator was then employed to convert the deviation-corrected monthly GCM data into daily time series.
Statistical analysis
A three-stage analytic strategy was employed to project the heat- and heatwave-related diabetes mortality in 32 Chinese major cities during hot season (1 May to 30 September) under four climate change scenarios.
In the first stage, we used distributed lag nonlinear model (DLNM) to establish the baseline relationship between high temperature (and heatwave) and diabetes mortality for each city, after adjusting for potential covariates. The formula is as follows.
where Yi,t denotes the number of diabetes deaths in city i (i = 1,2,3,…,32) at day t during hot season; α represents the regression intercept; \(S\left(t;\beta \right)\) is a natural cubic spline with four degrees of freedom (df) to control for the seasonal trend of daily counts of diabetes deaths; \(S\left({Hum};\eta \right)\) represents a natural cubic spline with three df for relative humidity. \(\gamma\) and \(\lambda\) are the regression coefficient for each term; \({{Year}}_{i,t}\) denotes the effect of the year in city \(i\) on day \(t\). Day of the week (\({Do}{w}_{i,t}\)) was introduced in the model as categorical variable. A cross-basis term of daily mean temperature (\({T}_{{obs}}\)) was generated by DLNM, with a natural cubic spline by locating knots at 50th and 90th percentile of temperature dimension, and a natural cubic spline with three df for lag dimension, with 10 days as the maximum lag. High temperatures were defined as temperatures above the MMT. For the heat wave, it was defined as lasting for at least three consecutive days with daily temperature over 95th percentile, which is consistent with previous study13. And the cross-basis function using a linear function for the exposure dimension and a natural cubic spline with three df for lag dimension (maximum lag of 10 days) was applied for heatwave.
In the second stage, the multivariate meta-analysis based on restricted maximum likelihood estimation was used to pool the city-specific relationship between temperature (or heat wave) and diabetes mortality, and then to obtain the best linear unbiased prediction (BLUP) for city-specific associations. We used the Cochran’s Q approach and I2 statistic to test the heterogeneity between cities.
In the third stage, the number of heat-related diabetes deaths was calculated by aggregating subsets of days with temperatures above the MMT. And heatwave-related number of deaths was calculated using Ni × (RRi − 1) × DURi. N is the annual average number of deaths on non-heatwave days in the i city, RRi represents the relative risk of mortality associated with a heatwave based on the BLUP, and DURi is the number of days identified as heatwave days each year. Then, the attributable fraction of heat-related (or heatwave-related diabetes deaths) was computed by dividing the number of heat-related (or heatwave-related) diabetes deaths by the total number of diabetes deaths.
We calculated the excess mortality related to heat and heatwaves on a decadal basis for each city, SSP scenario, and general circulation model. We then computed the attributable fractions as the GCM-ensemble averages based on the region, decade, and SSP. Monte Carlo simulation was utilized to produce the empirical confidence intervals, generating 1000 samples of coefficients from cross-basis function and followed a multivariate normal distribution45.
Estimating the mortality burden associated with climate change involves various uncertainties stemming from the complex uncertain future relationships between temperature and mortality. We considered sources of uncertainty in the estimated deaths include the relative risk (RR) parameters and their confidence intervals, as well as the variability in temperature projections across different climate models. For this assessment, we assumed no changes in baseline mortality rates, MMT for temperature-mortality association and adaptations to high temperature.
To evaluate the reliability of our primary results, we conducted a series of sensitivity analyses: 1) by varying the degrees of freedom (df) for the time variable from 4 to 7, and for relative humidity from 3 to 5; 2) by incorporating the air pollution index (API) variable to control for the potential confounding effect by air pollution; 3) by additionally including GDP per capita for each city to adjust for the socioeconomic status; 4) by testing whether the main results were affected by one single city through pooling the estimates after excluding the city; and 5) by extending the heatwave definitions as daily mean temperature ≥90.0th, 92.5th or 95.0th with duration ≥ two, three or four days.
Data availability
Raw data were collected under a data sharing agreement, and the authors are not authorized to redistribute the data.
Code availability
Code sources are available from the corresponding authors upon request.
References
Peng, B.-Y. et al. Addressing Stem Cell Therapeutic Approaches in Pathobiology of Diabetes and Its Complications. J. Diabetes Res. 2018, 7806435 (2018).
Song, X. et al. Impact of short-term exposure to extreme temperatures on diabetes mellitus morbidity and mortality? A systematic review and meta-analysis. Environ. Sci. Pollut. R. 28, 58035–58049 (2021).
Sun, H. et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res. Clin. Pract. 183, 109119 (2022).
Xu, Y. et al. Prevalence and Control of Diabetes in Chinese Adults. JAMA 310, 948–959 (2013).
Wang, L. et al. Prevalence and Treatment of Diabetes in China, 2013-2018. JAMA 326, 2498–2506 (2021).
Magliano, D. J. et al. International diabetes federation. in IDF Diabetes Atlas, 10th edition. 2021.
Tao, J. et al. Urban-rural disparity in heatwave effects on diabetes mortality in eastern China: A case-crossover analysis in 2016–2019. Sci. Total Environ. 858, 160026 (2023).
Xu, Z. et al. Heatwaves and diabetes in Brisbane, Australia: a population-based retrospective cohort study. Int. J. Epidemiol. 48, 1091–1100 (2019).
Miyamura, K., Nawa, N., Nishimura, H., Fushimi, K. & Fujiwara, T. Association between heat exposure and hospitalization for diabetic ketoacidosis, hyperosmolar hyperglycemic state, and hypoglycemia in Japan. Environ. Int. 167, 107410 (2022).
Westphal, S. A. et al. Managing Diabetes in the Heat: Potential Issues and Concerns. Endocr. Pract. 16, 506–511 (2010).
Yang, J. et al. The effect of ambient temperature on diabetes mortality in China: A multi-city time series study. Sci. Total Environ. 543, 75–82 (2016).
He, Y. et al. Geographical disparities in the impacts of heat on diabetes mortality and the protective role of greenness in Thailand: A nationwide case-crossover analysis. Sci. Total Environ. 711, 135098 (2020).
Xu, Y. et al. Differences on the effect of heat waves on mortality by sociodemographic and urban landscape characteristics. J. Epidemiol. Community Health 67, 519 (2013).
Moon, J. The effect of the heatwave on the morbidity and mortality of diabetes patients; a meta-analysis for the era of the climate crisis. Environ. Res. 195, 110762 (2021).
Gu, S. et al. Projections of temperature-related cause-specific mortality under climate change scenarios in a coastal city of China. Environ. Int. 143, 105889 (2020).
Trancoso, R. et al. Heatwaves intensification in Australia: A consistent trajectory across past, present and future. Sci. Total Environ. 742, 140521 (2020).
Seposo, X. T., Dang, T. N. & Honda, Y. How Does Ambient Air Temperature Affect Diabetes Mortality in Tropical Cities? Int. J. Environ. Res. Public Health 14, 385 (2017).
Li, Y. et al. Extremely cold and hot temperatures increase the risk of diabetes mortality in metropolitan areas of two Chinese cities. Environ. Res. 134, 91–97 (2014).
Baccini, M. et al. Impact of heat on mortality in 15 European cities: attributable deaths under different weather scenarios. J. Epidemiol. Community Health 65, 64 (2011).
Gasparrini, A. et al. Projections of temperature-related excess mortality under climate change scenarios. Lancet Planet. Health 1, e360–e367 (2017).
Vicedo-Cabrera, A. M. et al. The burden of heat-related mortality attributable to recent human-induced climate change. Nat. Clim. Change 11, 492–500 (2021).
Zhang, G. et al. Avoidable heat-related mortality in China during the 21st century. npj Climate and Atmospheric Science 6(2023).
Hajat, S., et al. Impact of High Temperatures on Mortality: Is There an Added Heat Wave Effect? Epidemiology 17, 632–638 (2006).
Gasparrini, A. et al. Mortality risk attributable to high and low ambient temperature: a multicountry observational study. Lancet 386, 369–375 (2015).
Yardley, J. E., Stapleton, J. M., Sigal, R. J. & Kenny, G. P. Do heat events pose a greater health risk for individuals with type 2 diabetes? Diabetes Technol. Ther. 15, 520–529 (2013).
Al-Qaissi, A. et al. Environmental effects of ambient temperature and relative humidity on insulin pharmacodynamics in adults with type 1 diabetes mellitus. Diabetes, Obes. Metab. 21, 569–574 (2019).
Burge, M. R., Garcia, N., Qualls, C. R. & Schade, D. S. Differential effects of fasting and dehydration in the pathogenesis of diabetic ketoacidosis. Metabolism 50, 171–177 (2001).
Manz, F. & Wentz, A. The Importance of Good Hydration for the Prevention of Chronic Diseases. Nutr. Rev. 63, S2–S5 (2005).
Xu, R. et al. Association between Heat Exposure and Hospitalization for Diabetes in Brazil during 2000–2015: A Nationwide Case-Crossover Study. Environ. Health Perspect. 127, 117005 (2019).
Renard, E., Guerci, B., Leguerrier, A.-M. & Boizel, R. Lower Rate of Initial Failures and Reduced Occurrence of Adverse Events with a New Catheter Model for Continuous Subcutaneous Insulin Infusion: Prospective, Two-Period, Observational, Multicenter Study. Diabetes Technol. Therapeutics 12, 769–773 (2010).
Lopez, P. E., King, B. R., Goss, P. W. & Chockalingam, G. Bubble formation occurs in insulin pumps in response to changes in ambient temperature and atmospheric pressure but not as a result of vibration. BMJ Open Diabetes Res. Care 2, e000036 (2014).
Pingel, M. & Vølund, A. Stability of Insulin Preparations. Diabetes 21, 805–813 (1972).
Sun, Z. et al. Projection of Temperature-Related Excess Mortality by Integrating Population Adaptability Under Changing Climate - China, 2050s and 2080s. China CDC Wkly 3, 697–701 (2021).
Yang, J. et al. Projecting heat-related excess mortality under climate change scenarios in China. Nat. Commun. 12, 1039 (2021).
Glen, P. K., Jane, Y., Candice, B., Ronald, J. S. & Ollie, J. Heat stress in older individuals and patients with common chronic diseases. Can. Med. Assoc. J. 182, 1053 (2010).
Lu, C. et al. Educational disparities in ischaemic heart disease among 0.5 million Chinese adults: a cohort study. J. Epidemiol. Community Health 75, 1033 (2021).
McMichael, A. J. Globalization, Climate Change, and Human Health. N. Engl. J. Med. 368, 1335–1343 (2013).
Hunt, A. & Watkiss, P. Climate change impacts and adaptation in cities: a review of the literature. Climatic Change 104, 13–49 (2011).
Carter, J. G. et al. Climate change and the city: Building capacity for urban adaptation. Prog. Plan. 95, 1–66 (2015).
Yang, J. et al. Heatwave and mortality in 31 major Chinese cities: Definition, vulnerability and implications. Sci. Total Environ. 649, 695–702 (2019).
Niu, Y. et al. The main and added effects of heat on mortality in 33 Chinese cities from 2007 to 2013. Front. Environ. Sci. Eng. 17, 81 (2023).
Huang, Y., Li, C., Liu, D. L. & Yang, J. Projection of temperature-related mortality among the elderly under advanced aging and climate change scenario. npj Clim. Atmos. Sci. 6, 153 (2023).
Liu, J. et al. Projecting the excess mortality due to heatwave and its characteristics under climate change, population and adaptation scenarios. Int. J. Hyg. Environ. Health 250, 114157 (2023).
Liu, D. L. & Zuo, H. Statistical downscaling of daily climate variables for climate change impact assessment over New South Wales, Australia. Clim. Change 115, 629–666 (2012).
Zhu, Q. et al. Projecting heat-related cardiovascular mortality burden attributable to human-induced climate change in China. eBioMedicine 103, 105119 (2024).
Acknowledgements
We thank the support of the National Natural Science Foundation of China (No. 82003552, 82204131).
Author information
Authors and Affiliations
Contributions
Y.J., and Q.L. conceptualized and designed the study. Y.J., S.C., and M.Z. were responsible for statistical analysis. Y.J., S.C., M.Z., and D.L. engaged in the interpretation of data. S.C. wrote the draft of the manuscript. Y.J., S.J., S.T., Z.X., M.L., M.T., and M.Z. re-viewed and edited the manuscript. All authors contributed to discussion and approved the final version of the manuscript. Y.J., Q.L., S.J., and M.Z. are the guarantors of this work and, as such, had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chen, S., Zhou, M., Liu, D.L. et al. Mortality burden of diabetes attributable to high temperature and heatwave under climate change scenarios in China. npj Clim Atmos Sci 7, 289 (2024). https://doi.org/10.1038/s41612-024-00839-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41612-024-00839-3
This article is cited by
-
Economic burden, health burden and predictive analysis of diabetes attributed to non-optimal temperature in global from 1990 to 2030
Journal of Diabetes & Metabolic Disorders (2025)