Abstract
Digital counselling can alleviate the burden on healthcare systems and patients. While it has been evaluated as a supplement to standard care or a substitute for follow-up visits, its use for initial triaging and counselling remains unstudied. We developed a Digital Intake Tool (DIT) to facilitate the entire pre-colonoscopy counselling process for FIT-positive participants of a colorectal cancer screening program digitally, replacing the need for physicians. In this multicentre prospective non-inferiority study, we evaluated if the DIT could replace in-person counselling. DIT-counselling resulted in adequately prepared participants in 96.5%, compared to 97.6% after in-person counselling, demonstrating non-inferiority. Outpatient visits were significantly reduced, with only 3.4% requiring face-to-face consultations. Patient experiences were highly positive, without increased psychological distress or anxiety, and effective knowledge transfer. This approach benefits patients and healthcare systems, allowing patients to receive care at home, reducing travel and carbon emissions, while increasing outpatient capacity. ICTRP-registration: NL9315, March 8, 2021.
Similar content being viewed by others
Introduction
The increasing demand for healthcare services, driven by factors such as population aging, the rise in chronic diseases, and the widespread adaptation of population screening and surveillance initiatives, all contribute to a growing amount of patients that require healthcare and has led to immense pressure on healthcare systems worldwide1,2,3,4. To address this challenge, innovative solutions are urgently needed to ensure accessible, affordable, and high-quality care. In recent years, a digital transformation has unfolded, integrating digital technologies in healthcare. This evolution has led to developments in digital health, which seek to alleviate the growing pressure on healthcare systems5. The onset of the COVID-19 pandemic further accelerated this transition, prompting rapid exploration and implementation of various digital innovations.
Telemedicine, a component of digital health, provides an opportunity for remote patient interaction and data exchange. By facilitating remote consultations, telemedicine reduces the burden on outpatient clinics and patients, while potentially enhancing the quality of care delivered6. Integrating telemedicine into standard care has shown great promise. For example, incorporating telemedicine in the management of patients with heart failure showed a reduction in short-term cardiovascular-related hospitalizations and mortality rates and better treatment adherence in patients with diabetes mellitus7,8,9,10. Many of the assessed interventions enable direct communication between the patient and the healthcare provider through phone or video calls. Despite the advantage of saving travel time for patients, this setup may not offer the flexibility of receiving care at patients’ preferred times, a limitation also faced by healthcare providers. Mobile and web-based applications, hereafter referred to as digital counselling, overcome this limitation and have demonstrated efficacy in various contexts. Digital counselling has primarily been used in chronic disease management, follow-up, and referral consultations, including open-access endoscopy11,12,13,14. In patients with inflammatory bowel disease, digital counselling reduced outpatient consultations and hospital admissions15. Digital counselling could even replace in-person care in a pre-colonoscopy care setting without compromising procedure-related quality parameters and patient satisfaction13. However, these scenarios involve patients who are already familiar with their conditions or, in the case of an intervention, have undergone prior triaging and informed consent procedures.
Thus far, digital counselling has not yet been evaluated in patients who have not previously consulted or been triaged by a physician, and for whom no prior information about their medical condition is available at the endoscopic outpatient clinic. To bridge this gap, we have developed a Digital Intake Tool (DIT) for participants of a faecal immunochemical testing-based colorectal cancer screening (CRC) programme16. Participants with a positive Faecal immunochemical test (FIT) are selected from the general population and referred for in-person pre-colonoscopy counselling without prior consultation of a physician. In this study, we evaluated whether we could replace in-person counselling with digital counselling by using the DIT application.
Results
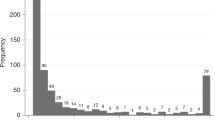
Between October 2021 and October 2023, 1690 FIT-positives were approached for inclusion, 1000 (59.2%) were successfully enroled. Among the 690 non-participants, characterized by a median age of 66.0 (60.0-71.0) and 41.6% being female, reasons for non-participation varied. In 43.6% a preference for in-person over DIT-counselling was expressed, 32.8%,reported a lack of digital literacy as a barrier, this subgroup was characterized by a median age of 70.0 (64.0–73.0), 17.2% desired more interactive counselling, 7.1% declined due to comorbidity, and 2.3% reported other reasons for non-participation.
Of the 1000 included patients, 971 (97.1%) successfully underwent DIT-counselling. The median response time was one day, with almost half of the participants completing DIT-counselling outside regular working hours (49.4%). Only 29 patients (2.9%), transitioned to in-person counselling at the outpatient clinic after inclusion. The majority of participants (96.7%) underwent colonoscopy after counselling. In 50 participants, protocol deviations in bowel preparation led to their exclusion from the per-protocol (PP) analysis.
An overview of the study and participants included in the PP and intention-to-treat (ITT) analyses is illustrated in Fig. 1. Patient characteristics of participants receiving DIT- and in-person counselling are shown in Table 1. No major differences were observed in age and sex. The percentage of participants with a low American Society of Anaesthesiologist Classification (ASA), ASA I or II, was higher in the DIT cohort. However, ASA classification was not reported in 38.4% of the in-person counselling cohort.
Colonoscopy data
Total Boston Bowel Preparation Scale (BBPS) scores, a bowel cleanliness scoring system ranging from zero to nine, were available for 949 (94.9%) participants. In 22 participants, the last segment was not inspected due to premature termination of the procedure for the following reasons: poor bowel preparation, discomfort, and technical issues. The median BBPS score (P5-P95) of the digital and in-person counselling cohort was the same, 9.0 (6.0–9.0). The primary outcome, adequate bowel preparation, was achieved in 96.5% and 96.6% of the PP and ITT study populations, respectively. In the in-person counselling cohort, this percentage was 97.6%, resulting in an absolute risk difference for adequate bowel preparation of −1.1% (95% CI −2.64–0.44) for the PP analysis and −1.0% (95% CI −2.49–0.49) for the ITT analysis (Fig. 2). Both analyses demonstrated non-inferiority. A sensitivity analysis was conducted to evaluate whether the results remained consistent if all colon segments had a minimum score of two. Although the adequate bowel preparation rates were slightly lower for all cohorts, the risk difference and 95% CI remained above the non-inferiority margin, with risk differences of − 1.2% (−2.91–0.51) and −1.2% (−2.87–0.47) for PP and ITT, respectively. Incomplete and repeat colonoscopies occurred in only a small proportion of the DIT-counselling participants and were comparable to the in-person counselling cohort (Table 2).
Outpatient reduction
After inclusion, 29 (2.9%) participants opted out of digital counselling and switched to the traditional in-person counselling. The DIT identified 932 (96.0%) participants with at least one red flag out of the 971 that completed the digital counselling (Supplementary Table 1). In line with the study protocol, all 971 participants received an additional telephone consultation after completing the DIT. Retrospective evaluation showed that this consultation was unnecessary for 409 (42.2%) of the 971 DIT participants. For 557 (57.4%) participants, the additional consultation was necessary, mainly to address matters such as the discontinuation of anticoagulants or anti-diabetes medication. Only five participants (0.5%) required additional face-to-face counselling subsequent to the DIT. In two cases, this was due to the patient-reported comorbidities, in two cases at patient’s request, and in one case to obtain a signature for approval to access medical history elsewhere. As a result, traditional in-person counselling was averted in 966 (96.6%) participants, with 409 (40.9%) needing only digital counselling. The remaining 557 (55.7%) participants required a brief telephone consultation based on the red flags. Detailed reasons for telephone outpatient consultations are provided in Supplementary Table 2.
Patient-reported outcomes
Patient-reported outcomes were obtained from 971 DIT participants and 100 in-person participants. Patient characteristics are presented in Table 3. The majority (77.7%) of participants reported no prior experience with colonoscopy. DIT participants reported more frequent utilization of digital health resources and higher levels of comfort (Supplementary Figure 1). Satisfaction ratings for digital counselling were high, with nearly all participants (98.8%) rating it above average (score >5), and a median score of 8.0 (8.0–9.0) on a scale from 0–10. After colonoscopy, satisfaction levels remained high (median 9.0, 8.0–10.0), and 95.4% of the participants would recommend DIT-counselling to others. In-person counselling received a slightly higher rating of 9.0 (8.0–9.0, p = 0.002) (Table 4).
After digital counselling, the majority, 523 (59.4%) of the participants reported to worry less about the potential colonoscopy findings on an 11-point-Likert scale (z-value −6.136, p < 0.001) (Table 5). Main contributors to this reduction were the information provided regarding the possible colonoscopy findings (32.1%) and the delivery of information through animated videos (25.5%). Conversely, worries were increased due to the information provided about the potential procedural complications (6.7%). Similarly, although with a smaller proportion, 32.0% of participants reported a decrease in anxiety on the STAI-6 (z-value −3.210, p = 0.001) after digital counselling. An increase in anxiety was reported by 24.3% of the participants, while 43.7% reported no change (median: 11.0). A comparable increase in anxiety was observed after in-person counselling, but 55.7% reported decreased anxiety levels. Significant differences between digital and in-person counselling were observed; however, the effect size (r), consistently hovered around 0.1, indicating a very small effect. The mean differences within patient regarding psychological distress and anxiety pre- and post-counselling were very small for both digital and in-person counselling (Supplementary Table 3). Descriptive results of the statements and STAI-6 for both cohorts pre- and post-counselling results are presented in Supplementary Table 4.
Knowledge transfer
The information-recall test comprises of 16 true and false statements, with a total score ranging from zero indicating the lowest knowledge transfer to 16, representing the highest (Supplementary Table 5). After establishing content validity as outlined in the published protocol16, the information recall test was evaluated among 807 DIT participants and 89 participants who received in-person counselling. The analysis revealed a Cronbach’s alpha coefficient of 0.19, indicating limited internal consistency among the test items. Nevertheless, the information-recall test represents essential post-counselling knowledge. To evaluate the objective knowledge transfer of the DIT, the in-person participants were retained as a reference for establishing a benchmark. The mean score of in-person participants was 13.9 (1.5), showing no significant difference compared to DIT participants, who scored a mean of 14.2 (SD 1.1, p-value 0.087). Only 5.6% of the digital counselled participants achieved a score below the reference SD (1.5), in contrast to 18% observed in the in-person cohort.
Experience from a healthcare perspective
The experiences of nine physicians involved in the DIT-trial were evaluated and analysed. The median reported time spent on the digital counselling was 15 minutes (11.0-27.5), and the majority (77.8%) of physicians experienced it less time-consuming compared to the current standard in-person counselling. Almost everyone (88.9%) recommended the DIT for future counselling, with 77.8% advising the availability of both digital and in-person counselling options. The median rating from a healthcare standpoint was 8.0 (7.5-9.5). The main point of feedback for future consideration was the integration of the digital counselling system with the electronic patient records.
Discussion
In this prospective multicentre cohort study, we evaluated whether digital counselling could replace the traditional in-person counselling visit for FIT-positive participants of a CRC screening programme prior to colonoscopy. Our findings demonstrate that the DIT is non-inferior to in-person counselling in terms of procedural preparation. A high adequate bowel preparation rate of >96% was achieved, meeting the 90% requirement of the CRC screening programme. Furthermore, a substantial reduction in face-to-face outpatient visits was established, and >40% of the participants could be scheduled for colonoscopy based on DIT-counselling only. Additionally, patient-reported experiences after digital counselling were highly positive, without any increase in psychological distress or anxiety, and a highly effective knowledge transfer.
Previous research supports our findings, indicating that digital technologies effectively educate patients on the complex process of bowel preparation17,18,19. Comparable high adequate bowel preparation rates were found in another study that evaluated digital counselling among symptomatic patients for whom face-to-face informed consent was already obtained13. Additionally, a meta-analysis illustrated that educational videos led to reduced anxiety levels among patients undergoing diagnostic procedures20. Our intervention did not mainly decrease anxiety levels. This may be due to the fact that the interventions were supplementary to standard care rather than replacements. Additionally, the presence of test-retest bias might have made it challenging to distinguish a true change in our study. Interestingly, also after in-person counselling, no or minimal reductions in anxiety and psychological distress were observed. More importantly, there was no observed increase in anxiety or psychological distress.
Compared to other studies that evaluated digital health interventions, this is one of the few studies that evaluated digital counselling in a patient population without prior consultation or triaging. This shift towards a home-based counselling approach offers several obvious advantages from a patient’s perspective. Hence, the DIT enables patients to receive care at the comfort of their own home at their own time. With half of the participants completing the DIT during weekends or evenings, our findings underscore the need for healthcare accessibility outside regular working hours. Also, it saves travelling time and expenses, one of the main reasons participants cited for joining this study. Additionally, the ability to review information and carefully consider responses enhances well-informed patients. However, while digital counselling offers benefits, it should remain an option rather than the sole modality, ensuring accessibility for all patients as such taking into account individual preferences. From the perspective of healthcare providers, the implementation of the DIT presents significant time-saving opportunities and outpatient capacity optimization. Given the current challenges of long waiting lists at outpatient clinics, the DIT offers a cost-effective approach while maintaining similar levels of quality that could annually save at least 34,000 hours of in-person counselling in a CRC screening population in the Netherlands. Also, in the event of future pandemics, digital counselling could prevent the complete suspension of CRC screening programmes. Instead, patients at high risk for CRC could be scheduled for colonoscopy based on the information obtained through their digital intake21. Beyond individual and healthcare provider benefits, the adoption of digital counselling has broader societal implications. By reducing the need for in-person appointments, the DIT contributes to environmental sustainability, minimizing carbon emissions associated with travelling. Furthermore, in regions where patients face large distances to healthcare facilities, the DIT could enhance healthcare accessibility, thus promoting equitable access to healthcare and enhance screening participation rates. This study could be an example for other medical disciplines in replacing face-to-face informed consent procedures, offering an innovative solution to reduce the growing pressure on the healthcare systems.
Several limitations of this study should be acknowledged. Firstly, the non-randomized design of the study might introduce selection bias, potentially limiting the generalizability of our results to a broader demographic in terms of age and digital health literacy. The higher median age of non-participants reporting low digital literacy suggests that DIT-counselling could be more feasible for younger populations. Due to the limited sample size of age subgroups, the statistical power to conduct detailed age-based analyses is restricted, necessitating larger studies to validate these findings. Our results also indicate that the DIT was evaluated within a population more experienced with digital health. However, approximately 35% of all included participants reported low digital literacy, yet still achieved adequate bowel preparation and high patient satisfaction. Nevertheless, the potential bias reflects real-world scenarios and underscores the importance of offering digital counselling as an option rather than an obligation. With increasing digital literacy over time, the impact of this bias is likely to diminish. Secondly, we were unable to evaluate safety in relation to (post) procedural complications due to the fact that this was not registered in Screen-IT. Nevertheless, no (serious) adverse events were reported during the study period. Thirdly, we had a relatively small number of inclusions in the in-person counselling cohort for patient-reported outcomes. This could potentially bias the comparative analysis, limiting the generalizability of the results and reducing the statistical power to detect differences between the two groups. Despite this limitation, the within subject analyses of the digital counselling cohort remain intact, demonstrating a high level of patient satisfaction and knowledge transfer without an increase in anxiety or psychological distress. Lastly, the inclusion criteria limited participation to individuals with a good understanding of the Dutch language, and therefore excluding individuals with language barriers. However, existing research suggests that digital technologies can effectively engage populations facing language barriers and have the possibility of more inclusive and accessible healthcare by providing digital counselling tailored to individual language preferences. Further validation of the DIT in this context is warranted in future studies.
Another aspect that warrants a more comprehensive evaluation is the cost-effectiveness of implementing digital counselling. Nevertheless, another study on the expenses associated with digital counselling estimated an annual licence fee of €40 per patient using digital counselling, which is almost seven times less than the cost of in-person counselling22. Given the significant reduction in outpatient visits, it is likely that digital counselling is associated with reduced costs. Prior to implementation, as recommended by the physicians involved in this study, it is crucial to carefully strategize the integration of digital counselling into existing workflows. This should be done in collaboration with the application’s end-users to ensure optimal usability and effectiveness. Moreover, integration with electronic health records can further enhance efficiency, highlighting the importance of collaborative efforts between healthcare and development providers. Building further on clinical implementation, future research should focus on determining which patient and clinical predictors are positively related to digital counselling. This would enable automatic allocation of patients to the appropriate patient journey on an individual level based on their intake results, ruling out involvement of physicians.
In conclusion, this study indicates that in-person counselling could be replaced by a Digital Intake Tool. The DIT resulted in well-prepared patients in terms of colonoscopy preparation, high satisfaction, knowledge transfer, and a significant reduction in outpatient visits. Hence, digital counselling has been shown to be a valuable alternative counselling technique to inform and triage patients, facilitating informed consent without direct interaction with a physician.
Methods
Study setting and participants
In the Netherlands, a FIT-based colorectal cancer screening programme has been implemented since 2014. Biennial FIT tests are distributed to individuals between 55 and 75 years of age. In case of a positive FIT, participants are advised to undergo a colonoscopy. Therefore, they are referred to the outpatient clinic of a certified endoscopy centre for in-person counselling prior to colonoscopy. During this pre-colonoscopy consultation, typically lasting between 30 to 45 minutes, patients undergo triaging, receive information, including bowel preparation instructions, and procedural informed consent is obtained, all mandatory before proceeding to colonoscopy. Refraining from colonoscopy only occurs when patients decline or if significant comorbidities are present23. A high-quality colonoscopy depends on adequate bowel preparation, which ensures optimal lesion detection and minimizes the need for repeat colonoscopies. However, achieving adequate bowel preparation requires patients to adhere to strict dietary restrictions and follow instructions for laxative use. Therefore, patient education, provided during the pre-colonoscopy consultation, plays a crucial role. The Boston Bowel Preparation Scale (BBPS), a scoring system ranging from zero to nine, is used to evaluate bowel cleanliness. According to the auditing programme of the national screening organisation, the percentage of colonoscopies achieving a BBPS of ≥6, indicating sufficient cleanliness to inspect the mucosa, must exceed 90% for all participants24.
This trial was carried out in seven CRC screening certified endoscopy centres. These included one academic hospital, four regional hospitals, and two private endoscopy centres. Study participants eligible for inclusion were FIT-positives referred for colonoscopy, without a Dutch illiteracy or audiovisual disability and with access to the DIT.
Study design
The DIT-trial was a multicentre, non-randomized, cohort study with a non-inferiority design. All study participants were assigned to the intervention. The trial design and study protocol have been published previously16. The study protocol was approved by the Medical Ethical Committee of the Erasmus University Medical Centre, Rotterdam, the Netherlands (MEC-2021-0098) and has been registered online on the International Clinical Trials Registry Platform (NL9315) on March 8, 2021.
Intervention
The intervention has been described elsewhere16. In summary, the DIT is a web application designed to facilitate the pre-colonoscopy consultation process in a population FIT-based CRC screening programme. Without prior involvement of a health care provider, FIT-positive screenees are guided through a series of medical questions, used for the purpose of triaging, alternated with spoken animated videos that provide patient education created by Informed B.V. Based on pre-determined criteria, the DIT presents the intake result to physicians as a ‘red flag’ or ‘green flag’ triage result. Answers resulting in a ‘red flag’ are presented in Supplementary Table 1. Physicians are required to review patients with at least one ‘red flag’ and discuss any necessary additional information with them. The follow-up patient journey was determined based on the triage results, which could involve scheduling colonoscopy, additional phone or in-person counselling to discuss medical conditions or questions before colonoscopy was scheduled. All participants received a brief phone call outlining their patient journey, all additional procedural information was provided by the DIT. Once the colonoscopy was scheduled, participants received personalized instructions for bowel preparation via spoken animations and a digital bowel preparation schedule. All participants were prescribed a split-dose laxative, either a low-volume one-litre polyethylene glycol (PEG) combined with ascorbate-based bowel preparation (Pleinvue®, Norgine), or in cases where extended bowel preparation was indicated due to slow transit constipation, a three litre PEG preparation (Moviprep®, Norgine).
Outcomes
The primary outcome was adequate bowel preparation, defined as a BBPS of ≥6. Included participants were linked to the national information system of the CRC screening programme: Screen-IT. It is obligated for endoscopists to register colonoscopy data in ScreenIT. Additionally, colonoscopy data, including BPPS, were obtained from 1000 participants who received traditional in-person counselling.
Secondary outcomes were participation rate, response rate, number of outpatient visits, occurrences of incomplete procedures due to poor bowel preparation, and necessity for repeat colonoscopies. The patient-reported outcomes, knowledge transfer, satisfaction, a change in anxiety measured with the STAI-6, and psychological distress were evaluated among all included DIT participants and in 100 patients of the CRC screening programme that received in-person counselling.
For assessment of the impact on reduction in outpatient visits, four patient journeys were defined: in-person counselling, digital counselling only, digital counselling followed by face-to-face counselling, and digital counselling followed by telephone consultation.
Statistical analyses
Statistical analyses were performed using IBM SPSS Statistics version 25. Continuous variables were summarized as mean (standard deviation) and assessed using the independent samples t-test or in the case of skewed data as median (quartile 1 - quartile 3) and tested using the Mann–Whitney U nonparametric test or independent t-test with bootstrapping in cases where there was an unequal distribution between compared variables. Categorical variables were presented as proportions. For within-subject analyses, we used either the dependent t-test or Wilcoxon signed-rank, as appropriate.
This study was powered on the primary outcome, the sample size calculation has been described previously, resulting in a total of 1000 participants allocated to both the DIT-counselling study arm and the in-person counselling arm with a non-inferiority margin of −8%. Data were analysed on a PP and an ITT basis. The absolute risk difference with corresponding 95% confidence interval, was calculated for the proportion of participants achieving an adequate bowel preparation, comparing patients who received DIT-counselling with patients who underwent in-person counselling. For participants with an incomplete colonoscopy, where only one or two colon segments were scored, the total BBPS was calculated under a worst-case scenario assumption, assigning a score of zero for the colon segments that were not visualized.
Data availability
The patient datasets generated during this study are not publicly available. However, they can be shared on reasonable request to the corresponding author.
Code availability
The underlying code used for this study can be provided upon reasonable request to the corresponding author.
Abbreviations
- DIT:
-
Digital Intake Tool
- FIT:
-
Fecal Immunochemical Test
- CRC:
-
colorectal cancer screening
- BBPS:
-
Boston Bowel Preparation Scale
- PEG:
-
Polyethylene glycol
- SD:
-
Standard deviation
- Q1:
-
Quartile 1
- Q3:
-
Quartile 3
- ASA:
-
American Society of Anesthesiologists
- CI:
-
Confidence Interval
- PP:
-
Per-protocol
- ITT:
-
Intention-to-treat
References
Anderson, G. & Horvath, J. The growing burden of chronic disease in America. Public Health Rep. 119, 263–270 (2004).
Ritchie H., R. M. Age Structure, https://ourworldindata.org/age-structure#the-global-population-pyramid (2024).
Navarro, M., Nicolas, A., Ferrandez, A. & Lanas, A. Colorectal cancer population screening programs worldwide in 2016: An update. World J. Gastroenterol. 23, 3632–3642 (2017).
Shah, T. A. & Guraya, S. S. Breast cancer screening programs: Review of merits, demerits, and recent recommendations practiced across the world. J. Microsc Ultrastruct. 5, 59–69 (2017).
Marques, I. C. P. & Ferreira, J. J. M. Digital transformation in the area of health: systematic review of 45 years of evolution. Health Technol. Ger. 10, 575–586 (2020).
Su, D. et al. Does telemedicine improve treatment outcomes for diabetes? A meta-analysis of results from 55 randomized controlled trials. Diabetes Res Clin. Pr. 116, 136–148 (2016).
Scholte, N. T. B. et al. Telemonitoring for heart failure: a meta-analysis. Eur. Heart J. 44, 2911–2926 (2023).
Gurcay, B., Yilmaz, F. T. & Bilgin, A. The effectiveness of telehealth interventions on medication adherence among patients with Type 2 diabetes: a meta-analysis. Telemed. J. E Health 30, 3–20 (2024).
Kuan, P. X. et al. Efficacy of telemedicine for the management of cardiovascular disease: a systematic review and meta-analysis. Lancet Digit Health 4, e676–e691 (2022).
de la Torre Díez, I., Garcia-Zapirain, B., Méndez-Zorrilla, A. & López-Coronado, M. Monitoring and follow-up of chronic heart failure: a literature review of eHealth applications and systems. J. Med Syst. 40, 179 (2016).
Zuidema, X., Tromp Meesters, R. C., Siccama, I. & Houweling, P. L. Computerized model for preoperative risk assessment. Br. J. Anaesth. 107, 180–185 (2011).
Zhang, K., Rashid-Kolvear, M., Waseem, R., Englesakis, M. & Chung, F. Virtual preoperative assessment in surgical patients: A systematic review and meta-analysis. J. Clin. Anesth. 75, 110540 (2021).
Veldhuijzen, G. et al. Computer-based patient education is non-inferior to nurse counselling prior to colonoscopy: a multicenter randomized controlled trial. Endoscopy 53, 254–263 (2021).
ASGE Standards of Practice Committee et al. Open-access endoscopy. Gastrointest. Endosc. 81, 1326–1329 (2015).
de Jong, M. J. et al. Telemedicine for management of inflammatory bowel disease (myIBDcoach): a pragmatic, multicentre, randomised controlled trial. Lancet 390, 959–968 (2017).
Marijnissen, F. E. et al. A digital intake tool to avert outpatient visits in a FIT-based colorectal cancer screening population: study protocol of a multicentre, prospective non-randomized trial - the DIT-trial. BMC Gastroenterol. 24, 38 (2024).
Li, P. et al. Patient education by smartphones for bowel preparation before colonoscopy. J. Gastroenterol. Hepatol. 37, 1349–1359 (2022).
Cardoso, R., Guo, F., Heisser, T., Hoffmeister, M. & Brenner, H. Utilisation of colorectal cancer screening tests in European countries by type of screening offer: results from the European Health Interview Survey. Cancers (Basel) 12, 1409 (2020).
Park, J. S. et al. A randomized controlled trial of an educational video to improve quality of bowel preparation for colonoscopy. BMC Gastroenterol. 16, 64 (2016).
Monteiro Grilo, A. et al. Effectiveness of educational videos on patient’s preparation for diagnostic procedures: Systematic review and Meta-Analysis. Prev. Med. Rep. 28, 101895 (2022).
Toes-Zoutendijk, E. et al. Impact of COVID-19 and suspension of colorectal cancer screening on incidence and stage distribution of colorectal cancers in the Netherlands. Eur. J. Cancer 161, 38–43 (2022).
de Jong, M. J. et al. Cost-effectiveness of Telemedicine-directed Specialized vs Standard Care for Patients With Inflammatory Bowel Diseases in a Randomized Trial. Clin. Gastroenterol. Hepatol. 18, 1744–1752 (2020).
van Iersel, C. et al. Landelijke evaluatie van het bevolkingsonderzoek darmkanker in Nederland 2018-2021. 51 (https://www.rivm.nl/documenten/landelijk-evaluatierapport-bevolkingsonderzoek-darmkanker-2018-2021, 2023).
Bronzwaer, M. E. S. et al. Quality assurance of colonoscopy within the Dutch national colorectal cancer screening program. Gastrointest. Endosc. 89, 1–13 (2019).
Acknowledgements
This trial received PPP-allowance provided by Health-Holland, Top Sector Life Sciences & Health, to stimulate public-private partnerships. The funder played no role in study design, data collection, analysis and interpretation of data, or the writing of this manuscript.
Author information
Authors and Affiliations
Contributions
M.C.W.S. conceived the idea for the study. F.E.M. and M.C.W.S. designed the protocol. F.E.M. coordinated the study, F.E.M. and E.E.C.R. executed the study and M.C.W.S. and P.J.F.J. supervised study execution. F.E.M., E.E.C.R., A.N.R. and S.M.B. included study participants. F.E.M., E.E.C.R., M.C.W.S., I.L.V., S.Y.I. and F.E.M. analysed and interpreted data. P.J.F.J., M.M.T., D.N., L.M.M.W., J.M.J., I.S., F.C.B., T.W., M.M. and R.G. interpreted data. F.E.M., E.E.C.R. and M.C.W. drafted the first version of the manuscript. All authors provided critical revision of the manuscript for important intellectual content and approved the final draft of the protocol for submission.
Corresponding author
Ethics declarations
Competing interests
M.C.W.S. received research support from Norgine, Sentinel, and Sysmex. P.J.F.J. has received consultancy and lecture fees from Boston Scientific, Cook Medical and Fujifilm. All other authors declare no financial or non-financial competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Marijnissen, F.E., Rijnders, E.E.C., Tielemans, M.M. et al. Reducing outpatient visits for FIT-positive participants of colorectal cancer screening programs with home-based digital counselling. npj Digit. Med. 8, 285 (2025). https://doi.org/10.1038/s41746-025-01683-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41746-025-01683-2