Abstract
Depressive symptoms pose a serious global threat to well-being, highlighting the need for scalable mental health interventions. E-mental health interventions offer promising population-level solutions, yet few are grounded in theory or tested on large samples. This study utilizes an innovative e-mental health intervention based on the Extended Process Model of Emotion Regulation and examines the effectiveness of this theory-based intervention across a randomized controlled trial (RCT, N = 187; Chinese Clinical Trial Registry: ChiCTR2400081964; registration date: March 18th, 2024) and two extensive real-world studies (Nstudy 2 = 11,554, Nstudy 3 = 44,018) conducted with adults in China. The RCT confirmed the efficacy of this intervention, and both of the real-world e-mental health intervention studies showed a decrease in depressive symptoms (35–36%) and an increase in well-being (14–16%) over 21 days. These findings highlight the potential of theory-based e-mental health interventions as scalable solutions for early depression intervention and prevention, offering substantial societal and economic advantages.
Similar content being viewed by others
Introduction
Experiencing depressive symptoms, such as persistent sadness, hopelessness, and loss of interest (anhedonia), exerts a significant toll on individuals’ lives, impairing their cognitive and social functioning, lowering productivity, and adding healthcare costs1,2,3. Already highly prevalent worldwide, depressive symptoms continued to rise during the COVID-19 pandemic. For example, a nationally representative survey of US adults showed an increase from 8.5% before to 27.8% during the pandemic, based on a cutoff of 10 on the PHQ-9 (Patient Health Questionnaire-9)4. A meta-analysis of the global prevalence of subclinical depressive symptoms also showed an increase from 25.25% before February 2020 to 30.51% during March to April 20205. In the post-COVID era, approximately 14 percent of U.S. adults have continued to report depressive symptoms within a two-week period6,7. This sustained prevalence of depressive symptoms has contributed to a significant and growing demand for mental health services4,8.
Unfortunately, high-quality mental health services are often insufficient to meet this growing demand, particularly in low- and middle-income countries (LMICs)9. The inaccessibility and high cost of traditional treatments such as medication and counseling limit the feasibility of scalable implementation for the general public10,11. To address these implementation gaps, electronic mental health (e-mental health) interventions have emerged12. These interventions leverage the internet and related technologies such as websites and mobile apps to deliver mental health services12,13,14,15. A notable example is Step-by-Step, a guided self-help digital intervention developed by the World Health Organization (WHO), which is designed for use in low-resource settings16. Randomized controlled trials have demonstrated the effectiveness of this program in reducing depressive symptoms, including population in LMICs16,17. Such evidence highlights the potential of e-mental health solutions to address unmet mental health needs on a global scale.
E-mental health interventions offer several advantages over traditional approaches. They are more accessible and allow individuals to access support almost anytime and anywhere via the Internet, which proved especially valuable during the COVID-19 pandemic when in-person mental health services were often disrupted or unavailable12,18,19. Additionally, e-mental health interventions are cost-effective, providing an affordable option for mental health treatment14. The anonymity of these interventions can also provide an appealing alternative to those who are hesitant about seeking face-to-face treatment15. Moreover, research suggests that e-mental health is effective in alleviating depressive symptoms (Hedges g = 0.60 in LMICs and Hedges g = 0.51–0.58 in HICs), thus has the potential of preventing the development of major depressive disorders12,20,21,22. Collectively, these features contribute to the scalability of e-mental health interventions, namely, the ability to deliver effective, accessible care to large and diverse populations without compromising fidelity10,13.
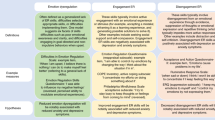
To alleviate depressive symptoms, most e-mental health intervention programs include techniques for improving emotion regulation capabilities. Emotion regulation refers to the processes by which individuals influence their emotional experiences, expressions, and responses23. Adaptive emotion regulation strategies help individuals cope with stressful life events, reduce negative emotional intensity, and promote resilience; whereas maladaptive strategies, such as rumination, are linked to heightened risks for severe depressive symptoms24,25. Despite the growing popularity of including content on enhancing emotion regulation skills, one limitation of recent interventions is the lack of a theoretical basis for determining the targeted intervention components. The present research addresses this limitation by employing a theory-based e-mental health intervention based on the Extended Process Model of Emotion Regulation26. This model is suitable because it provides clear intervention targets. Specifically, the core mechanism of the Extended Process Model of Emotion Regulation is the valuation system, containing three key components: perception, value, and action. Individuals with maladaptive valuation systems might be more likely to focus on negative information in an emotion-eliciting situation (maladaptive perception), to have negative appraisals (maladaptive evaluations), and then to have maladaptive mental and physical responses (maladaptive action), leading to a vicious downward spiral.
Another limitation of many e-mental health intervention efforts is the use of small sample sizes drawn from highly selected populations, often recruited from WEIRD (western, educated, industrialized, rich, and democratic) countries, which limits the generalizability and ecological validity of their findings13,27. Real-world studies (research that uses data collected outside the context of randomized controlled trials, typically from routine care settings and with fewer exclusion criteria) in LMICs, which account for over 80% of the world’s population, are sorely needed28,29. However, existing real-world studies often suffer from low completion rates (usually less than 15%), which can limit the reliability of the results30,31,32,33,34, and tend to focus exclusively on reducing mental distress, thereby neglecting the potential of e-mental health interventions to promote well-being.
The present research leverages an academic-industry collaboration, an advantageous approach that combines the design and development resources of industry partners with the research expertise in academia11. Across one RCT and two large-scale real-world studies, we systematically examined the efficacy and effectiveness of a theory-based e-mental health intervention (Pauselab EBP for Emotion) in China. Aiming to break the maladaptive valuation cycle, this intervention first trains the users to be aware of what happened in the external world and their internal feelings, especially the positive side, which might have been overlooked (i.e., forming adaptive “perception”, 1st module). Then, users are trained to accept the feelings in the mind, trying to objectively appraise and interpret them (i.e., forming adaptive “value”, 2nd module). Next, users are trained to act towards the value-aligned direction even when accompanied by discomfort (i.e., forming adaptive “action”, 3rd module). In Study 1 (N = 187), we conducted an RCT to assess the efficacy of the intervention. In Study 2 (N = 11,554), we examined the effectiveness of this intervention in a real-world setting based on the users’ data of the e-mental health intervention platform. Finally, in Study 3 (N = 44,018), we sought to replicate these results in a larger real-world sample with naturalistic quasi-comparison groups. Given the potential heterogeneity of depressive symptoms within the population, we investigated how intervention effects differed for participants with varying levels of pre-intervention symptom severity in the real-world studies. Specifically, in Study 1, participants receiving the intervention were expected to show a greater reduction in depressive symptoms and a greater increase in well-being from baseline to post-intervention, compared to those in the control group. In Studies 2 and 3, we expected participants to exhibit reductions in depressive symptoms and improvements in well-being following the intervention. We also hypothesized that the effectiveness of the intervention in Study 3 would be more salient in users who completed all the components of the intervention as compared with the non-completers. Furthermore, we hypothesized that the intervention would be particularly effective for individuals with more severe depressive symptoms when enrolled.
Results
Study 1: participants
Given that this study is part of a larger study (see Fig. 1) and only the intervention process of Group 5 was identical to the intervention used in the two real-world studies (i.e., Study 2 & 3), we included two out of the five groups: the wait-list group (Group 1, n = 94), with a mean age of 27.85 years (SD = 5.79), and the “mindfulness practice + writing practice + human support” intervention group (Group 5, n = 94). One participant from the intervention group withdrew from the study due to other therapeutic needs identified after completing the pre-intervention assessments, leaving 93 individuals with a mean age of 27.85 years (SD = 7.47) for the final analysis in the intervention group. There were no significant differences between participants in the two groups in terms of gender, age, pre-intervention depressive symptoms, and pre-intervention well-being (ps > 0.129).
Among the 187 participants, ages ranged from 18 to 70 years (M = 27.85, SD = 6.67), and 85.03% were female. A total of 151 (80.75%) were successfully followed up and completed the post-intervention assessment. Dropouts and non-dropouts did not significantly differ in terms of gender, age, pre-intervention depression symptoms, and pre-intervention well-being (ps > 0.174).
Study 1: preliminary analyses
Before conducting the primary analyses, we examined the assumptions of homogeneity of variance for ANCOVA using Levene’s test. For depressive symptoms, the homogeneity assumption was satisfied at both pre-intervention, F(1, 185) = 0.15, p = 0.699, and post-intervention assessments, F(1, 185) = 0.43, p = 0.554. Similarly, for well-being, the homogeneity assumption was met at pre-intervention, F(1, 185) = 0.27, p = 0.604, and post-intervention assessments, F(1, 185) = 3.50, p = 0.077.
Study 1: efficacy of the randomized controlled trial
The Group (intervention vs wait-list group) × Time (pre-intervention vs post-intervention assessment) interaction was significant for the depressive symptoms model, F(1, 183) = 6.58, p = 0.013, ηp2 = 0.035. Specifically, both groups showed a decrease in depressive symptoms from pre- to post-intervention; however, the decrease was significantly larger for individuals in the intervention group (ΔMestimate = −3.92), t(183) = −6.06, p < .001, d = −0.75, 95% CI of d [−0.99, −0.51], compared with those in the wait-list group (ΔMestimate = −1.94), t(183) = −2.83, p = 0.007, d = -0.37, 95% CI of d [−0.63, −0.11].
A similar pattern emerged for the well-being model, where the Group × Time interaction was significant, F(1, 183) = 10.96, p = 0.003, ηp2 = 0.056. The intervention group demonstrated significant increases in well-being from pre- to post-intervention (ΔMestimate = 0.45, SE = 0.09), t(183) = 4.80, p < 0.001, d = 0.60, 95% CI of d [0.35, 0.84] whereas the wait-list group did not show any changes (ΔMestimate = 0.08, SE = 0.10), t(183) = 0.83, p = 0.427, d = 0.11, 95% CI of d [−0.15, 0.37]. (see Supplementary Table 3 for details).
As illustrated in Fig. 2, these results indicate that the intervention group experienced greater improvements in both depressive symptoms and well-being compared to the wait-list group, highlighting the efficacy of the intervention. More details of the analyses are presented in Supplementary Section 1.1.
A Changes in depressive symptoms in Study 1; B changes in well-being in Study 1. Boxes display the interquartile range (IQR), whiskers display the 1.5 IQR values of the distribution of depressive symptoms and well-being. Results about mean scores are summarized in Supplementary Table 3.
Study 2: user characteristics
Participants (N = 11,554; age range = 18–81 years, M = 33.24, SD = 6.89; 82.40% female) were first-time users of the intervention between January 6, 2020, and February 19, 2021. Additional demographic and usage details are provided in Supplementary Table 4.
Comparisons in users’ characteristics indicated that females (82.40%) accounted for a higher percentage than males (17.52%), χ²(1) = 4868.34, p < 0.001, Phi(φ) = 0.649. Significant differences emerged in the proportions across age groups, χ²(54) = 17599.98, p < 0.001, Phi(φ) = 1.236. The primary age group was 18−35 years old (69.09%). Only 2.25% of the users were older than 50 years old. There were significant differences in the frequencies of individuals with different severities of depressive symptoms, χ²(4) = 3141.92, p < 0.001, Phi(φ) = 0.521. Most users had mild (33.81%) to moderate (30.19%) depressive symptoms. About a quarter of the users had moderately severe (17.72%) or severe (7.08%) symptoms. The remaining 11.58% of users had minimal depressive symptoms. Supplementary Table 4 and 5 present more details of the user characteristics.
Study 2: user engagement
Completion of the e-mental health intervention required users to finish launch day tasks (Day 0), all components of the 21 days of practice, and both pre- and post-intervention assessments within 25 days of starting. Among all users, 59.80% met this completion criteria, which represents a strong engagement rate for an e-mental health intervention in a real-world setting (vs. typically below 5%)30,35. On average, users completed 17.79 days (SD = 6.72) out of the 22 possible days (80.86%), indicating high adherence. Supplementary Section 2.1 presents more details of the user engagement. Supplementary Table 6 presents completion rates by gender, age groups, and symptom severities; Supplementary Table 7 provided the detail of number of completion of days; Supplementary Table 8 provided completion days by gender, age groups, and symptom severities.
Study 2: effectiveness of the e-mental health intervention
We conducted a series of one-way repeated measures analysis of covariance (re-ANCOVA) to examine the changes in depressive symptoms and well-being from pre- to post-intervention. As shown in Fig. 3A, users’ depressive symptoms showed a significant 34.37% reduction (ΔMestimate = −3.67), t(6,885) = −50.12, p < 0.001, d = −0.82, 95% CI of d [−0.85, −0.78]. Users’ well-being also increased by 14.87% (see Fig. 3C; ΔMestimate = 0.50), t(6,667) = 37.44, p < 0.001, d = 0.64, 95% CI of d [0.60, 0.67]; for more details, see Supplementary Section 2.2 & Supplementary Table 10.
A Changes in depressive symptoms in Study 2; B changes in depressive symptoms in Study 3; C changes in well-being in Study 2; D changes in well-being in Study 3. Boxes display the interquartile ranges and whiskers display the 1.5 IQR values of the distribution of depressive symptoms and well-being. Results about mean scores are summarized in Supplementary Table 10 and 18.
Study 2: heterogeneity of the effectiveness by symptom severity categories
We investigated whether users with different categories of depressive symptom severities experienced varying changes in depressive symptoms and well-being after completing the intervention. The two-way mixed-design ANCOVA indicated heterogeneity in changes of depressive symptoms for users with differential severities of symptoms, F(4, 6,881) = 1037.57, p < 0.001, and ηp2 = 0.38. As shown in Fig. 4A, users who initially had severe pre-intervention depressive symptoms exhibited the most substantial reduction in their depressive symptoms after the intervention (ΔMestimate = −9.40), t(6,881) = −53.70, p < 0.001, d = −2.63, 95% CI of d [−2.73, −2.54], followed by users with moderately severe symptoms (ΔMestimate = −7.25), t(6,881) = −65.27, p < 0.001, d = −2.04, 95% CI of d [−2.10, −1.98], moderate symptoms (ΔMestimate = −4.35), t(6,881) = −49.56, p < 0.001, d = −1.22, 95% CI of d [−1.27, −1.18], and mild symptoms (ΔMestimate = −1.67), t(6,881) = −20.29, p < 0.001, d = 0.47, 95% CI of d [−0.51, −0.42] (for more details, see Supplementary Section 2.3 & Supplementary Table 11).
A Changes in depressive symptoms in Study 2 by severity categories; B changes in depressive symptoms in Study 3 by severity categories; C changes in well-being in Study 2 by severity categories; D changes in well-being in Study 3 by severity categories. Boxes display the interquartile ranges and whiskers display the 1.5 IQR values of the distribution of depressive symptoms and well-being. Results about mean scores are summarized in Supplementary Table 11 and 19.
Similarly, users with higher symptom severity also had larger increases in well-being after the intervention, as indicated by the significant “Severity” × “Time” interaction, F(4, 6,663) = 64.42, p < 0.001, ηp2 = 0.04. As shown in Fig. 4C, users with severe (ΔMestimate = 0.69), t(6,663) = 17.81, p < 0.001, d = 0.89, 95% CI of d [0.79, 0.99] or moderately severe symptoms (ΔMestimate = 0.68), t(6,663) = 27.88, p < 0.001, d = 0.89, 95% CI of d [0.82, 0.95] showed greater increases in well-being, followed by users with moderate symptoms (ΔMestimate = 0.56), t(6,663) = 28.62, p < 0.001, d = 0.72, 95% CI of d [0.67, 0.77] and mild symptoms (ΔMestimate = 0.42), t(6,663) = 22.91, p < 0.001, d = 0.54, 95% CI of d [0.50, 0.59]. Notably, even for individuals with minimal symptoms before the intervention, where a ceiling effect on well-being might be expected, their well-being increased significantly (ΔMestimate = 0.15), t(6,663) = 5.01, p < 0.001, d = 0.20, 95% CI of d [0.12, 0.28] (for more details, see Supplementary Section 2.3 & Supplementary Table 11).
To test the robustness of the effectiveness, we conducted intention-to-treat analysis with a multiple imputation approach, and all the patterns of the results were replicated (see Supplementary Section 2.7).
Study 3: user characteristics
Study 3 aimed to replicate the findings from Study 2 using a larger sample. Study 3 also included naturalistic quasi-comparison groups. Individuals in comparison groups filled the post-intervention measurements but did not complete all components of the intervention. The intervention methods and assessments of depressive symptoms and well-being remained nearly identical, with some changes to several well-being measures (see Supplementary Table 9 & 17 for details).
Participants (N = 44,018; age range = 18–80 years, M = 31.51, SD = 7.50; 83.60% female) were first-time users of the intervention between November 1, 2021, and September 22, 2023. Additional demographic and usage details are provided in Supplementary Table 12.
Females (83.60%) accounted for a higher percentage than males (16.38%), χ²(1) = 19903.70, p < 0.001, Phi(φ) = 0.672. User ages ranged from 18 to 80 years old (M = 31.51 years old, SD = 7.50 years) with significant differences in the proportions across age groups, χ²(6) = 22,688.37, p < 0.001, Phi(φ) = 0.718. The primary age group was 18–35 years old (74.78%). Only 3.02% of the users were older than 50 years old. There were significant differences in frequencies of individuals with different severities of depressive symptoms, χ²(4) = 12,551.41, p < 0.001, Phi(φ) = 0.534. Most users had mild (34.28%) to moderate (30.45%) depressive symptoms. About a quarter of the users had moderately severe (16.95%) or severe (6.64%) symptoms. The remaining 11.68% of users had minimal depressive symptoms. Supplementary Table 12 presents more details of the user characteristics.
Study 3: user engagement
Applying the same completion criteria as in Study 2, 60.53% of users in Study 3 met the requirements, demonstrating similarly high engagement. Users completed an average of 17.81 days (SD = 6.60) out of the possible 22 days (80.95%), indicating high adherence. Supplementary Section 3.1 and Supplementary Tables 14–16 presents more details of the user engagement.
Study 3: effectiveness of the e-mental health intervention
Results from the one-way repeated measures ANCOVA in Study 3 replicated the results in Study 2, indicating that users’ depressive symptoms measured by PHQ-9 reduced 36.00% from pre- to post-intervention (ΔMestimate = −3.74), t(26,636) = −100.50, p < 0.001, d = −0.83, 95% CI of d [−0.85, −0.82]; see Fig. 3B. Additionally, users’ well-being increased 16.31% from pre- to post-intervention (ΔMestimate = 0.53), t(26,631) = 90.07, p < 0.001, d = 0.75, 95% CI of d [−0.73, −0.76]; see Fig. 3D. Supplementary Section 3.2 presents more details of the averaged changes in depressive symptoms and well-being after intervention. (see Supplementary Table 18 for details)
Study 3: heterogeneity of the effectiveness by symptom severity categories
Replicating the results in Study 2, the two-way mixed-design ANCOVA indicated heterogeneity in changes of depressive symptoms for users with differential severities of symptoms, F(4, 26,632) = 3957.21, p < 0.001, ηp2 = 0.37. As shown in Fig. 4B, users who initially had severe pre-intervention depressive symptoms exhibited the most substantial reduction (ΔMestimate = −9.95), t(26,632) = −106.89, p < 0.001, d =−2.80, 95% CI of d [−2.85, −2.75], followed by users with moderately severe symptoms (ΔMestimate = −7.32), t(26,632) = −125.73, p < 0.001, d = −2.06, 95% CI of d [−2.09, −2.03], moderate symptoms (ΔMestimate = −4.52), t(26,632) = -101.63, p < 0.001, d = −1.27, 95% CI of d [−1.30, −1.25], and mild symptoms (ΔMestimate = −1.84), t(26,632) = −44.33, p < 0.001, d = −0.52, 95% CI of d [-0.54, −0.50] (see Supplementary Table 19 for details).
Consistent with the results for depressive symptoms, users with higher symptom severity also had larger increases in well-being after the intervention, as indicated by the significant “Severity” × “Time” interaction, F(4, 26,627) = 138.10, p < 0.001, ηp2 = 0.02. As shown in Fig. 4D, users with severe (ΔMestimate = 0.73), t(26,627) = 40.38, p < 0.001, d = 1.06, 95% CI of d [1.01, 1.11] or moderately severe symptoms (ΔMestimate = 0.62), t(26,627) = 54.27, p < 0.001, d = 0.89, 95% CI of d [0.86, 0.92] had more prominent increases in well-being, followed by users with moderate symptoms (ΔMestimate = 0.58), t(26,627) = 66.01, p < 0.001, d = 0.83, 95% CI of d [0.80, 0.85] and mild symptoms (ΔMestimate = 0.47), t(26,627) = 57.95, p < 0.001, d = 0.68, 95% CI of d [0.65, 0.70]. Notably, even for individuals with minimal symptoms before the intervention, their well-being increased significantly following the intervention (ΔMestimate = 0.33), t(26,627) = 25.77, p < 0.001, d = 0.47, 95% CI of d [0.44, 0.51]. Supplementary Section 3.3 presents more details of the heterogeneous changes in depressive symptoms and well-being after intervention.
The intention-to-treat analysis with multiple imputation approach replicated the per-protocol results of both averaged and heterogeneous effectiveness (see Supplementary Section 3.7 and 3.8), suggesting the robustness of the effectiveness.
Study 3: secondary analyses with naturalistic quasi-comparison groups
In secondary analyses, we examined whether the effectiveness of the intervention varied across users with differential levels of completion. The e-mental health intervention used in the present study could be segmented into three stages: Stage 1 (Days 1–8; “Opening the space of awareness”), Stage 2 (Days 9–14; “Understanding emotions from new perspectives”), and Stage 3 (Days 15–21; “Acting autonomously and effectively”). We then differentiated the non-completers of the intervention into three naturalistic quasi-comparison groups: non-completers of Stage 1 (users who practiced the intervention for less than 8 days), non-completers of Stage 2 (users who practiced the intervention for 8 to 14 days), and non-completers of Stage 3 (users who practiced the intervention for 15–20 days).
The two-way mixed-design ANCOVA between “Completion stages” and “Time” showed that the interaction was significant in the model of depressive symptoms, F(3, 27,733) = 5.37, p < 0.001, ηp2 = 0.001. The intervention had large effect sizes in reducing the depressive symptoms for both completers (ΔMestimate = −3.74, SE = 0.04), t(27,733) = −101.27, p < 0.001, d = -0.83, 95% CI of d [−0.85, −0.81] and non-completers of Stage 3 (ΔMestimate = −3.74), SE = 0.15, t(27,733) = −25.14, p < 0.001, d = −0.83, 95% CI of d [−0.89, −0.77]; however, the effect size of reducing depressive symptoms was smaller for non-completers of Stage 2 (ΔMestimate = −2.79, SE = 0.44), t(27,733) = −6.31, p < 0.001, d = −0.62, 95% CI of d [−0.81, −0.43] and non-completers of Stage 1 (ΔMestimate = −1.62, SE = 0.63), t(27,733) = −2.58, p = 0.010, d = −0.36, 95% CI of d [−0.63, −0.09].
The “Completion stages” by “Time” interaction was also significant in the model of well-being, F(3, 28,007) = 8.12, p < 0.001, ηp2 = 0.001). The intervention had moderate effect sizes in enhancing well-being for both completers (ΔMestimate = 0.53, SE = 0.01), t(28,007) = 91.51, p < 0.001, d = 0.75, 95% CI of d [0.73, 0.76] and non-completers of Stage 3 (ΔMestimate = 0.51, SE = 0.02), t(28,007) = 22.78, p < 0.001, d = 0.72, 95% CI of d [0.66, 0.78]; however, the effect size in enhancing well-being was smaller for non-completers of Stage 2 (ΔMestimate = 0.32, SE = 0.07), t(28,007) = 4.64, p < 0.001, d = 0.45, 95% CI of d [0.26, 0.64] and non-completers of Stage 1 (ΔMestimate = 0.18, SE = 0.09), t(28,007) = 1.89, p = 0.059, d = 0.25, 95% CI of d [−0.01, 0.51].
Discussion
The present research aimed to investigate whether a theoretically motivated and scalable emotion regulation e-mental health intervention could reliably reduce depressive symptoms and increase well-being in Chinese samples. Study 1 confirmed the efficacy of the intervention with an RCT design. Studies 2 and 3 extended the intervention into the real world and obtained robust real-world evidence for its effectiveness. Further analysis indicated significant benefits for individuals across varying severity levels of depression.
In Studies 2 and 3, it was encouraging that the user completion (over 60%) and adherence (over 80%) rates were much higher than those reported in prior real-world studies, which generally ranged from 1−15%30,31,32,33,34. A high user engagement rate is critical for the implementation of e-mental health interventions because sufficient engagement is crucial for effectiveness33. Potential explanations for the high engagement rates in the present studies might include the majority of participants were not clinically diagnosed with depression, the use of diverse online platforms for delivery, and the integration with popular social media software, which facilitated easy access and adherence to the intervention components36,37. Daily reminder messages, together with on-demand guidance and professional support, may also have facilitated user engagement11. Therefore, the novel intervention delivery and motivation promotion systems of the e-mental health intervention in the present study might be used as a successful reference point by future e-mental health services.
The real-world studies showed that the e-mental health intervention, on average, reduced users’ depressive symptoms by 35% and enhanced well-being by 15%. These findings suggest that this theoretically motivated e-mental health intervention was generally helpful for users with depressive symptoms via two inferred mechanisms outlined in the Extended Process Model of Emotion Regulation: 1) directly, by alleviating depressive symptoms through disrupting the maladaptive valuation cycle; and 2) indirectly, by enhancing well-being through the construction of a new, adaptive valuation cycle, helping individuals better cope with stress and reduce vulnerability to future depressive symptoms. While previous studies have shown that e-mental health interventions can reduce depressive symptoms, most have relied on RCTs or small-scale real-world samples, limiting the generalizability of their findings16,17,27. This study addresses that limitation by combining an RCT with two large-scale real-world studies, providing stronger empirical support for both the effectiveness and scalability of e-mental health interventions.
Importantly, users with the most severe symptoms exhibited the largest decrease in depressive symptoms following the intervention. However, their symptoms, on average, remained above the cutoff score for severe depression. This finding suggests that e-mental health interventions alone may not be sufficient in successfully treating those with severe depressive symptoms. Supplementation with more intensive treatment methods, such as face-to-face psychotherapy and medication, may therefore be necessary in this subpopulation. In contrast, for users with moderate and moderately severe symptoms, their depressive symptoms decreased on average by 36–43% and fell below the depression cutoff score after the intervention, suggesting the effectiveness of early intervention.
Holding a problem-oriented perspective, existing mental health interventions predominantly pay attention to reducing mental illness, ignoring positive aspects of human life. The present study, in contrast, shows that e-mental health intervention promotes well-being for individuals with depressive symptoms. This finding suggests that mental health intervention is beneficial for not only individuals with heightened depressive symptoms, but also those with minimal-to-mild depressive symptoms, facilitating individuals’ personal growth and improving their resilience to future adversities11,38. Considering the large population base of individuals with minimal-to-mild depressive symptoms, a small-to-moderate effect size in enhancing well-being could have a potentially profound impact on improving public mental health.
Although the present findings are promising, several limitations warrant consideration. First, the real-world studies were conducted using a pre-post-test design to achieve high user engagement rates and facilitate academic-industry collaboration. Even though we included quasi-comparison groups with individuals who did not complete all intervention components, future studies that include an active control group are needed to more rigorously evaluate the intervention’s effectiveness. For example, future trials could include a time-matched psychoeducation program, a placebo control involving daily neutral activities, or a minimal intervention group that receives only general guidance without structured training. These comparisons would help isolate the specific effects of the intervention from general engagement or expectancy effects. Second, targeting individuals from a single country and mainly young adults enabled us to study a much larger real-world sample than would have been possible otherwise; however, this limited the generalizability of our findings to younger populations (e.g., adolescents) or older adults, who may differ in important factors such as digital health literacy, technology access, and attitudes toward e-mental health services39,40,41. Future studies should include users from more diverse backgrounds (e.g., different sociocultural and age groups) to better examine the universality and heterogeneity of the e-mental health intervention. In addition, it is important to develop and evaluate tailored versions of such interventions to meet the specific needs and preferences of different demographic groups. Third, considering the scarcity of real-world evidence in prior research, the primary goal of the current study was to assess the effectiveness of an e-mental health intervention in relieving depressive symptoms and enhancing well-being in real-world settings. However, this study did not examine the potential mechanisms of the e-mental health intervention, which should be further investigated. Fourth, although the intervention is grounded in established adaptive emotion regulation strategies, it does not yet incorporate the emerging concept of regulatory flexibility, which emphasizes the importance of matching strategies to contextual demands42,43. Future research could explore how such a dynamic and context-sensitive approach may enhance the effectiveness of e-mental health interventions. Fifth, the short duration of the measurement period limits our ability to draw conclusions about the long-term effects of the intervention. As no follow-up data were collected, it remains unclear whether the observed improvements in depressive symptoms and well-being are sustained over time. Future studies should incorporate longitudinal follow-up assessments to evaluate the durability of intervention effects and better understand long-term user outcomes.
The present study has several important implications for research, practice, and policy. Through academic-industry collaboration, this study provides real-world evidence for the effectiveness of a publicly available mental health platform. Although thousands of platforms of e-mental health interventions, such as commercially developed mobile apps, are now widely available, few platforms have any peer-reviewed evidence44,45. Strengthening partnerships between researchers and industry stakeholders is therefore essential to ensure that interventions are not only accessible but also evidence-based. It would be beneficial for researchers and practitioners of e-mental health companies to collaborate, conducting real-world studies with diverse populations to test an intervention’s effectiveness13. Broad dissemination of such evidence-based interventions could play a crucial role in promoting population-level mental health.
Building on this, our real-world evidence suggests that the e-mental health intervention is effective in reducing depressive symptoms, indicating its potential utility in preventing the onset of clinical disorders. The direct and indirect costs of major depressive disorders (MDD) are substantial, including healthcare costs (e.g., primary care, medical specialty, pharmacy), household-related costs (e.g., reduction in income due to living with an MDD patient), work-related costs (e.g., unemployment, absenteeism, presenteeism), and mortality46. By targeting early-stage symptoms and preventing their progression, scalable e-mental health interventions may offer a cost-effective solution to reducing the societal and economic burden of depression. That said, further empirical research is warranted to determine whether the integration of e-mental health interventions with traditional clinical treatments can support symptom reduction and relapse prevention among individuals diagnosed with clinical disorders.
These findings also carry important implications at the policy level. Further action is required to facilitate academic-industry collaboration in rigorously evaluating and promoting the effectiveness of the commercially available e-mental health platforms. At the same time, regulatory frameworks must be strengthened to protect users from untested or potentially harmful tools and to build public confidence in e-mental health47. Policy makers should also advocate for the implementation of evidence-based mental health interventions. Within healthcare settings, e-mental health interventions may have potential as adjunctive tools to support existing treatments such as medication or psychotherapy, particularly in early intervention or relapse prevention contexts. Community- and school-based infrastructure is also needed to improve the public’s mental health literacy and deliver evidence-based interventions to individuals with mild to moderate levels of mental distress. Importantly, even individuals without significant symptoms may benefit from using e-mental health tools to build positive psychological resources and reduce vulnerability to future distress.
Taken together, with sustained collaboration among academia, industry, and government, theory-based e-mental health interventions could serve as scalable solutions for preventing and early intervention for depression, yielding meaningful benefits for individuals, communities, and society at large.
Methods
Study 1: participants and procedure
We recruited the participants for the study (Chinese Clinical Trial Registry: ChiCTR2400081964; retrospective registration date: March 18th, 2024) through WeChat, the most widely used social media platform in China. The invitation included a registration link along with an informed consent form. To be eligible for participation, individuals had to meet specific inclusion criteria: they were required to be at least 18 years old and to have recently experienced depressive symptoms. Furthermore, participants had to consent to random group assignment and demonstrate proficiency in using WeChat or a web browser to complete the online intervention. Additionally, fluency in reading, writing, and comprehending Chinese was mandatory.
This recruitment strategy resulted in 740 individuals expressing interest in participating in the study. The exclusion criteria encompassed individuals with a prior diagnosis of mental illness, particularly psychiatric disorders. Those meeting this criterion were advised to seek professional medical assistance and were ineligible for participation. Furthermore, individuals currently engaged in other psychological counseling or interventions, such as one-on-one or group therapy sessions or psychological training programs exceeding three days, were excluded to prevent confounding effects on the study’s outcome assessment. As part of the screening process, participants also underwent an evaluation using the Patient Health Questionnaire-9 (PHQ-9); individuals with scores below 5 (indicative of minimal symptoms) or above 19 (indicative of severe symptoms) were excluded. Ultimately, 469 eligible participants were successfully enrolled and randomly assigned to one of the five groups (see Fig. 1) with different intervention combinations using a Python script developed by a research assistant involved in participant recruitment. The allocation sequence remained concealed from both participants and experimenters until the intervention was implemented. Throughout the trial, participants were provided with procedural information, including task instructions and intervention materials; however, they remained unaware of their specific group assignment or the underlying hypotheses of the study.
This study has been ethically approved by the Beijing Normal University’s Institutional Review Board (IRB) [202304200079].
Study 1: components of the e-mental health intervention
The development of the e-mental health intervention aligned with a recent guideline proposed by a group of twenty-five international experts on e-mental health12. The intervention spans 22 days, including a launch day (Day 0) and 21 practice days. On the launch day, users are required to complete the pre-intervention assessment and the “My original intention and commitment” section. Days 1 to 21 included daily practices that users were required to complete each day. All practices were framed by the Extended Process Model of Emotion Regulation26 (see Fig. 5). For individuals experiencing heightened emotional distress, when an event occurs, they might be more likely to focus on negative information, leading to negative appraisal, rumination, and adoption of maladaptive experiential and behavioral responses (see Fig. 5, the first-level valuation cycle).
W = emotion-eliciting situation; P1 = maladaptive perception (e.g., failure, loss, deterioration); V1 = maladaptive value (e.g., awful, hopeless, terrible); A1 = maladaptive action (e.g., depressed, fatigue, avoidance); P2 = more adaptive perception (e.g., “It is not a bad thing,” “Is it a failure?”); V2 = more adaptive value (e.g., “Is it awful?”, “What’s my true feelings?”, “Thoughts are just thoughts, which may not happen”); A2 = more adaptive action (e.g., “Have a try,” “I can do it”). This figure is adapted based on the prior literature. ①–④ represent the key intervention components of the e-mental health intervention. ①=be aware of what happened in the external world and their internal feelings (especially the positive side). ②=accept the feelings and try to objectively appraise and interpret them (more adaptive value). ③=act towards the value-aligned direction even if accompanied by discomfort. ④=change from self-defeating to self-enhancing recursive cycles.
This e-mental health intervention targeted the three key processes of the model – “perception”, “value”, and “action” – to break this vicious cycle and foster an adaptive emotional system (Fig. 5, the second-level valuation cycle). Specifically, the intervention first trained the users to form adaptive perception – being aware of external events and their internal feelings, especially the positive emotions which might be overlooked due to heightened emotional distress (Days 1–8). Then, users were trained to form adaptive evaluation, accepting their feelings and trying to appraise and interpret them objectively (Days 9–14). Next, users were trained to form adaptive action, rebuilding their response patterns by acting towards their values even when accompanied by discomfort (Days 15–21). These practices aimed to reduce emotional distress, prevent depression, and enhance well-being by reshaping users’ valuation system.
In order to reshape users’ valuation system, each practice day consisted of two main components: a 10-to-15-minute guided mindfulness practice and a therapeutic journaling writing exercise. The mindfulness practice included psychoeducational readings and daily audio exercises. The readings introduced foundational mindfulness concepts and techniques for applying mindfulness in daily life to manage mental distress. The audio exercises guided formal mindfulness practices, with the 21-day curriculum covering various modules (e.g., mindful breathing, body scan, mindful eating, mindful walking, mindful yoga, etc.). The writing practice provided a set of designed daily prompts (e.g., recording positive events, differentiating thoughts and emotions, clarifying values and goals) along with explanatory readings on the intentions and hypothesized benefits of each exercise. All intervention content was designed and authored by a team of four with at least a master’s degree in clinical psychology, including a mindfulness expert with over 15 years of research experience (see Fig. 6). The content is also based on the evidence-based practice, which includes cognitive behavioral therapy (CBT), mindfulness-based stress reduction (MBSR), mindfulness-based cognitive therapy (MBCT), acceptance and commitment therapy (ACT), and positive psychology intervention (PPI). Different techniques of intervention have been combined systematically to guide the users’ practice.
All the procedures of daily practice are shown in Fig. 7. Completion of tasks is determined by user behavior. For reading tasks, participants must click a “Finished” button upon completion (Fig. 7A). Listening tasks require participants to fill out an experience rating scale afterwards (Fig. 7B). Writing tasks need to be submitted based on specified formats (Fig. 7C). Tests require completion of designated questions. On the task completion page, frequently asked questions and answers related to the practices are provided (Fig. 7D). Once all tasks are finished for the day, participants receive a motivational quote card as a reward for completing the interventions (Fig. 8). This allows participants to conveniently access the intervention content daily through popular digital platforms. The variety of task types and the progression system with daily refresh help maintain engagement. Tracking task completion based on user behaviors allows for precise measurement of adherence. All the components of the daily practices are listed in Supplementary Table 1.
The intervention leverages emotion regulation strategies rooted in cognitive mechanisms that demonstrate cross-cultural validity (e.g., reappraisal techniques shown effective across cultures). Rather than modifying core content, we enhanced cultural relevance by including diverse peer examples representing different Chinese demographics (white-collar workers, mothers, students, etc.). These scenario-based illustrations help participants contextualize universal principles within their specific life circumstances while maintaining intervention fidelity.
The intervention followed a self-help format delivered through an online website (ebp.gesedna.com) accessible via a link on electronic devices, including smartphones, tablets, and computers. Considering most Chinese users’ familiarity with the WeChat app, a shortcut link was also embedded in the menu bar of an official WeChat subscription account.
After account registration, users completed a user survey and a pre-intervention assessment about depressive symptoms and well-being. On the last day of the practice period, users were asked to complete the post-intervention assessment within the next 10 days.
Study 1: supportive systems of the intervention
To facilitate user engagement and intervention effectiveness, the intervention program provides users with three forms of support during the practice period (see Fig. 9).
A Live Q&A with the lead experts; in this picture, the lead experts of the development team were answering the questions that were frequently asked by users. B Real-time Q&A in user communities; in the upper of the picture, one user asked a question in the user community; below the question is the answer from a teaching assistant. C FAQ section embedded in the program; in this picture, the user was searching answers for his questions in the program (“Cannot concentrate during the practice”); below the search box were potentially matching answers provided by the team.
First, there is a live Q&A with the lead experts. During the practice period, users can submit questions anonymously or using their nickname on the website. There are three live video Q&A sessions per period, with the number determined by the volume of questions in that period. The Q&A sessions are hosted by the 4 lead experts who designed the intervention program. Drawing from their respective areas of expertise in clinical psychology, they assign and answer submitted questions. All four lead experts have Master’s or PhD degrees in psychology, as well as years of applied psychology experience. The live sessions are recorded and can be replayed by all participants throughout the practice period.
Second, there is real-time Q&A in user communities: Users in the same period are added to a practice WeChat group with 300-500 peers who have similar levels of distress, as assessed beforehand. The lead experts and teaching assistants provide real-time Q&A support in these WeChat groups. Any practice-related questions are answered within 24 h on weekdays. Most teaching assistants have Master’s degrees in psychology. Before answering questions independently, each teaching assistant undergoes at least 3 months of training. They also receive regular professional group supervision and skills training. There are currently 14 teaching assistants serving a total of approximately 8000–10,000 people (including returning users) per period.
Third, an FAQ section is embedded in the program. After users complete an exercise, the webpage where they submit their work displays some common questions and answers that people often ask related to that exercise. At the same time, users can search by keywords on relevant webpages to find questions and answers they are interested in.
The support system serves vital functions in facilitating program effectiveness. The timely guidance from experts builds users’ capabilities to apply the practices to daily life. The empathetic approach also provides interpersonal support through a judgment-free community for emotional expression. This social support system increases engagement and motivation needed for behavior change.
Study 1: data flow, data storage, access, and transparency
All user data and information are stored on proprietary servers. Two datasets are handled separately: 1) personal order and account details are accessible only by customer service for troubleshooting, and 2) anonymized research data, including practice records, surveys, and assessments, are stored securely for analysis. During account registration, a prominent privacy policy outlines data collection, usage for scientific research on psychological patterns and mechanisms, potential publishing of aggregated non-identifiable results, and user rights to access and control their information. Users must consent before proceeding. Research data are anonymized by assigning randomized identifiers without personal details. Summary results may be published openly for scientific benefit, but the data is sufficiently aggregated to prevent identification. The secure storage, limited access, and transparency are aimed at protecting user privacy while enabling researchers to conduct studies to improve services. Participants are informed of all data practices and must explicitly consent to the privacy policy upon registering.
All study data were collected through a custom website hosted on a private server (https://ebp.gesedna.com). Participants accessed the platform exclusively via encrypted links distributed through social media, with no data interaction occurring on third-party platforms. Identity verification information (e.g., account credentials for login) and research data were stored in physically isolated systems, ensuring no technical or administrative possibility of linking participants’ social media profiles to their study responses. Additionally, the platform intentionally omitted the collection of digital identifiers such as IP addresses to further anonymize participation.
Study 1: risk management
The suicide risk evaluation protocol employs a validated two-stage screening process consistent with the Columbia Suicide Severity Rating Scale (C-SSRS). During the initial registration phase, all participants complete a preliminary screening comprising two binary-response items (0 = no, 1 = yes) assessing recent suicidal ideation (“Have you experienced suicidal ideation in the past month?”) and perceived worthlessness (“Do you currently hold strong beliefs that your life is worthless?”). An affirmative response to either item triggers a secondary assessment involving two additional binary-response items evaluating suicide planning (“Have you formulated a specific suicide plan within the past month?”) and means preparation (“Have you acquired means for suicide implementation?”). At each stage, a response is classified as positive if the participant selects “yes” for either question; otherwise, it is classified as negative.
Following risk stratification, participants receive information tailored to their level of suicide risk: (a) those categorized as “no risk” (negative on the first-stage screening) receive access to standard crisis resources, which remain available to them indefinitely; (b) individuals classified as “low risk” (positive on the first stage but negative on the second stage) complete a guided safety planning session utilizing the Stanley-Brown template and confirm their readiness before proceeding. Their safety plan remains accessible via their dashboard throughout the intervention period; (c) participants identified as “potentially high risk” (positive on both the first and second stages) trigger an alert recommending immediate psychiatric evaluation and are strongly advised to seek high-intensity professional assistance (e.g., appropriate medical intervention). All participants receive 24/7 crisis hotline information. For ethical considerations, those classified as high-risk may still be allowed to participate in the study if they provide verifiable proof of seeking professional care.
All personnel involved in participant interaction, including customer service representatives and teaching assistants, undergo regular crisis management training delivered by qualified mental health professionals. Teaching assistants additionally receive continuous group supervision to enhance their crisis intervention skills when supporting at-risk users. Furthermore, while mindfulness exercises may occasionally induce transient physical discomfort or perceived time constraints when practiced daily, these effects typically subside upon discontinuation and do not pose significant harm. Participants in guided intervention programs experiencing such difficulties can access real-time support via group chats or live sessions, whereas those engaged in unguided interventions can refer to online instructional materials provided by the program developers.
Study 1: pre- and post-intervention assessments
Depressive symptoms were assessed via the Patient Health Questionnaire-9 (PHQ-9; see Supplementary Table 2 for more details)48. Participants rated the frequency of experiencing each depressive symptom during the preceding two weeks on a four-point Likert scale (0 = not at all, 1 = several days, 2 = more than half the days, and 3 = nearly every day). Total scores range from 0 to 27, with higher scores indicating higher levels of depressive symptoms. Internal consistencies for the scale were adequate at pre-intervention (α = 0.70) and post-intervention (α = 0.86) assessments.
Well-being was assessed using the 14-item Mental Health Continuum-Short Form (MHC-SF; see Supplementary Table 2 for more details)36. Participants rated their feelings during the last month on a 6-point Likert scale (1 = never, 2 = very rarely, 3 = once a week, 4 = 2–3 times a week, 5 = almost every day, and 6 = every day). Mean scores (1–6) were computed by averaging all items, with higher scores indicating higher levels of well-being. Internal consistencies for the scale were good at pre-intervention (α = 0.88) and post-intervention (α = 0.93) assessments.
Study 1: analytical approach
Analyses were conducted with R 4.3.1. To determine the required sample size for detecting an interaction between “Group” (intervention vs. wait-list) and “Time” (pre- and post-intervention) in a mixed-design ANOVA, we conducted a power analysis using G*Power 3.1. Assuming a medium effect size (Cohen’s f = 0.175, equivalent to Cohen’s d = 0.35)49, a correlation among repeated measures of 0.3, α = 0.05, 1-β = 0.8, the analysis indicated that a total sample size of 92 participants would be necessary. We conducted a 2 × 2 mixed-design analysis of covariance, where the “Group” was the between-person factor, and the “Time” served as the within-person factor (see Supplementary Table 3 for details). Gender and age were included as covariates, as previous research has shown that both variables are associated with levels of depressive symptoms and well-being50,51. Missing data were dealt with the multiple imputation, which preserves the sample size and avoids the loss of information39.
Study 2: participant and procedure
Participants (N = 11,554, user ages ranged from 18 to 81 years old, M = 33.24 years, SD = 6.89; 82.40% females) were individuals who used the intervention for the first time between January 6, 2020 and February 19, 2021 (see Supplementary Table 4 for more details). Users were sourced from all 31 provinces and regions within the Chinese mainland (93.77%, n = 10,834). The remaining users came from the regions of Hong Kong, Macau, and Taiwan (0.61%, n = 71) and overseas (5.53%, n = 639).
The typical registration fee is 699 RMB (about $95), with varying discounts depending on the source of acquisition. Early adopters, in the first batch, could purchase the program for 399 RMB (about $55). This price covers the exercise costs, human service fees, and motivation maintenance expenses. For each period, individuals who complete 22 days of intervention (comprising the start-up task and 21 days of exercises) receive a 100 RMB (about $14) reward.
The e-mental health intervention included integrated pre-and post- intervention assessments to aid users understand and clarify their current psychological condition and to direct targeted practice. Both assessments used the same structure, allowing users to review their status and easily compare their pre- and post-intervention scores to observe changes over time. These comparisons aimed to foster user confidence and motivation to persist with the intervention and apply techniques in their daily lives. Users reported their depressive symptoms and well-being (see Supplementary Section 2.1 for more details).
The components of the e-mental health intervention, user privacy, and risk management are the same as that in Study 1.
All the procedures were approved by the Beijing Normal University’s Institutional Review Board (IRB) [BNU202310300164].
Study 2: pre- and post-intervention assessments
As in Study 1, depressive symptoms were assessed via the Patient Health Questionnaire-9 (PHQ-9). Pre-intervention PHQ-9 summed scores (0–27) were further categorized to classify users in different depression severity levels: minimal (0–4), mild (5–9), moderate (10–14), moderately-severe (15–19), and severe (20–27). The measures of depressive symptoms demonstrated satisfactory reliabilities during both the pre-intervention assessment (α = 0.84) and the post-intervention assessment (α = 0.83).
To ensure contextual relevance and user engagement in a real-world setting, a custom well-being scale was developed for Study 2. The items were theoretically grounded in established frameworks52,53,54, including Basic Psychological Needs Theory and Ryff’s Model of Psychological Well-being, and were reviewed by psychometric and clinical experts to ensure conceptual and methodological rigor. Each item was rated on a six-point Likert scale (1 = completely disagree, 2 = disagree, 3 = somewhat disagree, 4 = somewhat agree, 5 = agree, and 6 = completely agree). Items were generated based on relevant theories and then aligned with intervention content by the intervention designers. The final questionnaire contained four dimensions: competence (3 items; e.g., “I have the capability to manage the things that are important to me.”), vitality (3 items; e.g., “I perceive myself as imbued with vitality and dynamism.”), meaningfulness (3 items; e.g., “I comprehend the meaning of my life.”), and autonomy (3 items; e.g., “I experience a sense of autonomy in my actions.”). Mean scores (1–6) of each dimension were computed and then averaged into an overall well-being score. Internal consistencies of each well-being dimension showed good reliabilities at the pre- and post-intervention assessments (αs = 0.72–0.85). Items of the overall well-being also had good reliabilities at both the pre-intervention assessment (α = 0.90) and the post-intervention assessment (α = 0.91).
Study 2: analytical approach
All the Analyses were conducted with R 4.3.1. We described the distributions and compared the frequencies of indicators of user characteristics (e.g., gender, age groups, severities of depressive symptoms) and user engagement (completion rate, adherence) via Chi-square tests and t-tests.
To examine the intervention’s effectiveness in reducing depressive symptoms and enhancing well-being, we conducted one-way repeated measures analysis of covariance (re-ANCOVA). The pre- vs. post-intervention assessment of depressive symptoms or well-being was the within-person factor (i.e., time). Users’ gender and age were covariates.
To examine whether users with different levels of depressive symptoms severity had differential changes in depressive symptoms and well-being after completing the intervention, we conducted a two-way mixed-design ANCOVA, where the pre- vs. post-intervention assessment of depressive symptoms or well-being was the within-person factor (i.e., time) and the category of symptom severity (5 categories) was the between-person factor. Participants’ gender and age were treated as covariates across the models.
The primary analyses were per-protocol analyses based on individuals who completed the intervention. To test the robustness of our findings, we also conducted intention-to-treat analysis with a multiple imputation approach, which preserves the sample size and avoids the loss of information.
Study 3: participant and procedure
Participants (N = 44,018, user ages ranged from 18 to 80 years old, M = 31.51 years, SD = 7.50; 83.60% females) were individuals who used the intervention for the first time between November 1, 2021 to September 22, 2023 (see Supplementary Table 12 for more details). Users were sourced from all 31 provinces and regions within the Chinese mainland (92.37%, n = 40,663). The remaining users came from the regions of Hong Kong, Macau, and Taiwan (0.77%, n = 337) and overseas (6.32%, n = 2781).
Participants reported their depressive symptoms and well-being during both the pre- and post-intervention assessments. Notably, on the last day of the intervention period, the platform sent a reminder to all users to invite them to complete the post-intervention assessment (the assessment remained open for 10 days after the final day of practice), regardless of whether they completed the practices. A total of 1100 out of 17,375 (6.33%) non-completers (participants who did not complete all stages of the intervention but still completed both the pre- and post-intervention assessments) filled the post-intervention assessment, which allowed us to examine whether the dose of intervention influenced the effectiveness of the e-mental health intervention. The 21-day practice could be divided into three stages (Stage 1: Day 1–8, Stage 2: Day 9–14, Stage 3: Day 15–21) as shown in Fig. 6. We therefore divided the non-completers with post-intervention assessment into three subgroups based on their adherence: non-completers of Stage 1 (having less than 8 days of practice; n = 52), non-completers of Stage 2 (having 8–13 days of practice; n = 104), and non-completers of Stage 3 (having 14–20 days of practice; n = 944).
Components of the E-Mental Health Intervention, user privacy, and risk management are the same as those in Study 1.
All the procedures were approved by Beijing Normal University’s Institutional Review Board (IRB) [BNU202310300164].
Study 3: pre- and post-intervention assessments
Depressive symptoms were assessed via the Patient Health Questionnaire-9 (PHQ-9), exhibiting acceptable reliabilities (α = 0.84 for the pre-intervention assessment, α = 0.84 for the post-intervention assessment).
As in Study 2, well-being was assessed based on items about competence (3 items), vitality (3 items), meaningfulness (3 items), and autonomy (3 items). Mean scores (1–6) of each dimension were computed and then averaged into an overall well-being score. Internal consistencies of each well-being dimension were good at the pre- and post-intervention assessments (αs = 0.78–0.91). The overall well-being items also had good reliabilities (α = 0.89 for the pre-intervention assessment, α = 0.91 for the post-intervention assessment).
Study 3: analytical approach
Primary analyses of Study 3 were the same as that of Study 2 and were conducted with R 4.3.1. To examine whether intervention effectiveness varied across users with different levels of completion (i.e., non-completers of Stage 1, non-completers of Stage 2, non-completers of Stage 3, and completers), we conducted a two-way mixed-design ANCOVA between “Completion stages” and “Time”, where the pre- vs. post-intervention assessment of depressive symptoms or well-being was the within-person factor (i.e., time) and the completion levels of the intervention was the between-person factor. Participants’ gender and age were treated as covariates across the models.
Data availability
All the data from this study are available from https://osf.io/5wkqr/?view_only=b73e1c5b83564522a0019574f1de8802.
Code availability
All the codes from this study are available from https://osf.io/5wkqr/?view_only=b73e1c5b83564522a0019574f1de8802.
References
Nafilyan, V., Avendano, M. & de Coulon, A. The causal impact of depression on cognitive functioning: evidence from Europe. SSRN Electron. J. 14049 (2021).
Fried, E. I. & Nesse, R. M. The impact of individual depressive symptoms on impairment of psychosocial functioning. PLoS ONE 9, e90311 (2014).
Bock, J.-O. et al. Excess health care costs of late-life depression–results of the agemoode study. J. Affect. Disord. 199, 139–147 (2016).
Santomauro, D. F. et al. Global prevalence and burden of depressive and anxiety disorders in 204 countries and territories in 2020 due to the covid-19 pandemic. Lancet 398, 1700–1712 (2021).
Mahmud, S., Mohsin, M., Dewan, M. D. N. & Muyeed, A. The global prevalence of depression, anxiety, stress, and insomnia among general population during COVID-19 pandemic: a systematic review and meta-analysis. Trends Psychol. 31, 143–170 (2022).
Percentage of respondents in the U.S. who reported symptoms of depressive disorder in the last seven days or two weeks from April 2020 to September 2024. https://www.statista.com/statistics/1132438/depressive-symptoms-us-adults-in-last-week/ (Statista, 2025)
Liu, X., Cheng, G., Li, C. & Zeng, Y. The current status and epidemic-related influencing factors of the symptoms of anxiety, depression and insomnia among residents in mainland china in the post-epidemic era. Chin. J. Dis. Control Prev. 28, 709–713 (2024).
Schleider, J. L. et al. A randomized trial of online single-session interventions for adolescent depression during COVID-19. Nat. Hum. Behav. 6, 258–268 (2021).
Patel, V., Flisher, A. J., Hetrick, S. & McGorry, P. Mental health of young people: a global public-health challenge. Lancet 369, 1302–1313 (2007).
Dodge, K. A. et al. Population mental health science: guiding principles and initial agenda. Am. Psychol. 79, 805–823 (2024).
Lattie, E. G. et al. Digital mental health interventions for depression, anxiety, and enhancement of psychological well-being among college students: systematic review. J. Med. Internet Res. 21, e12869 (2019).
Seiferth, C. et al. How to e-mental health: a guideline for researchers and practitioners using digital technology in the context of mental health. Nat. Ment. Health 1, 542–554 (2023).
Lattie, E. G., Stiles-Shields, C. & Graham, A. K. An overview of and recommendations for more accessible digital mental health services. Nat. Rev. Psychol. 1, 87–100 (2022).
Schueller, S. M. & Torous, J. Scaling evidence-based treatments through digital mental health. Am. Psychol. 75, 1093–1104 (2020).
Graham, A. K. et al. Implementation strategies for digital mental health interventions in health care settings. Am. Psychol. 75, 1080–1092 (2020).
Cuijpers, P. et al. Effects of a who-guided digital health intervention for depression in syrian refugees in Lebanon: a randomized controlled trial. PLoS Med. 19, e1004025 (2022).
Cuijpers, P. et al. Guided digital health intervention for depression in Lebanon: randomised trial. BMJ Ment. Health 25, e34–e40 (2022).
Riboldi, I. et al. Digital mental health interventions for anxiety and depressive symptoms in university students during the covid-19 pandemic: a systematic review of randomized controlled trials. Rev. Psiquiatr. Salud Ment. 16, 47–58 (2023).
Witteveen, A. B. et al. Remote mental health care interventions during the covid-19 pandemic: an umbrella review. Behav. Res. Ther. 159, 104226 (2022).
Kim, J. et al. Effectiveness of digital mental health tools to reduce depressive and anxiety symptoms in low- and middle-income countries: systematic review and meta-analysis. JMIR Ment. Health 10, e43066 (2023).
Fu, Z., Burger, H., Arjadi, R. & Bockting, C. L. Effectiveness of digital psychological interventions for mental health problems in low- and middle-income countries: a systematic review and meta-analysis. Lancet Psychiatry 7, 851–864 (2020).
Serrano-Ripoll, M. J., Zamanillo-Campos, R., Fiol-DeRoque, M. A., Castro, A. & Ricci-Cabello, I. Impact of smartphone app-based psychological interventions for reducing depressive symptoms in people with depression: systematic literature review and meta-analysis of randomized controlled trials. JMIR mHealth uHealth 10, e29621 (2022).
Gross, J. J. Antecedent- and response-focused emotion regulation: divergent consequences for experience, expression, and physiology. J. Pers. Soc. Psychol. 74, 224–237 (1998).
Daros, A. R. et al. A meta-analysis of emotional regulation outcomes in psychological interventions for youth with depression and anxiety. Nat. Hum. Behav. 5, 1443–1457 (2021).
Lincoln, T. M., Schulze, L. & Renneberg, B. The role of emotion regulation in the characterization, development and treatment of psychopathology. Nat. Rev. Psychol. 1, 272–286 (2022).
Gross, J. J. Emotion regulation: current status and future prospects. Psychol. Inq. 26, 1–26 (2015).
Firth, J. et al. The efficacy of smartphone-based mental health interventions for depressive symptoms: a meta-analysis of randomized controlled trials. World Psychiatry 16, 287–298 (2017).
Population, total - Low & middle income. https://data.worldbank.org/indicator/SP.POP.TOTL?locations=XO&name_desc=false (World Bank Group, 2023)
Catarino, A. et al. Economic evaluation of 27,540 patients with mood and anxiety disorders and the importance of waiting time and clinical effectiveness in mental healthcare. Nat. Ment. Health 1, 667–678 (2023).
Fleming, T. et al. Beyond the trial: systematic review of real-world uptake and engagement with digital self-help interventions for depression, low mood, or anxiety. J. Med. Internet Res. 20, e199 (2018).
Ghosh, A. et al. An unguided, computerized cognitive behavioral therapy intervention (treadwill) in a lower middle-income country: pragmatic randomized controlled trial. J. Med. Internet Res. 25, e41005 (2023).
Montgomery, R. M. et al. The effects of a digital mental health intervention in adults with cardiovascular disease risk factors: analysis of real-world user data. JMIR Cardio 5, e32351 (2021).
Nahum-Shani, I., Shaw, S. D., Carpenter, S. M., Murphy, S. A. & Yoon, C. Engagement in digital interventions. Am. Psychol. 77, 836–852 (2022).
Oehler, C., Scholze, K., Reich, H., Sander, C. & Hegerl, U. Intervention use and symptom change with unguided internet-based cognitive behavioral therapy for depression during the COVID-19 pandemic: log data analysis of a convenience sample. JMIR Ment. Health 8, e28321 (2021).
Baumel, A. & Kane, J. M. Examining predictors of real-world user engagement with self-guided ehealth interventions: analysis of mobile apps and websites using a novel dataset. J. Med. Internet Res. 20, e11491 (2018).
Lamers, S. M. A., Westerhof, G. J., Bohlmeijer, E. T., ten Klooster, P. M. & Keyes, C. L. M. Evaluating the psychometric properties of the Mental Health Continuum-Short Form (MHC-SF). J. Clin. Psychol. 67, 99–110 (2011).
Sinharay, S., Stern, H. S. & Russell, D. The use of multiple imputation for the analysis of missing data. Psychol. Methods 6, 317–329 (2001).
Clarke, A. M., Kuosmanen, T. & Barry, M. M. A systematic review of online youth mental health promotion and prevention interventions. J. Youth Adolesc. 44, 90–113 (2015).
Lee, H. Y. et al. Role of health literacy in health-related information-seeking behavior online: cross-sectional study. J. Med. Internet Res. 23, e14088 (2021).
Barreda Gutiérrez, M., Cantarero-Prieto, D. & Pascual Sáez, M. Age, technology, and the digital divide: are they directly related to mental health problems? Healthcare 12, 2454 (2024).
Győrffy, Z., Boros, J., Döbrössy, B. & Girasek, E. Older adults in the digital health era: insights on the digital health related knowledge, habits and attitudes of the 65 year and older population. BMC Geriatr. 23, 779 (2023).
Bonanno, G. A. & Burton, C. L. Regulatory flexibility. Perspect. Psychol. Sci. 8, 591–612 (2013).
Chen, M. S., Bi, K., Han, X., Sun, P. & Bonanno, G. A. Emotion regulation flexibility and momentary affect in two cultures. Nat. Ment. Health 2, 450–459 (2024).
Anton, M. T. et al. Evaluation of a commercial mobile health app for depression and anxiety (ableto digital+): retrospective cohort study. JMIR Form. Res. 5, e27570 (2021).
Larsen, M. E. et al. Using science to sell apps: evaluation of mental health app store quality claims. npj Digit. Med. 2, 1–6 (2019).
Greenberg, P. E. et al. The economic burden of adults with major depressive disorder in the United States (2005 and 2010). J. Clin. Psychiatry 76, 155–162 (2015).
Torous, J. et al. The growing field of digital psychiatry: current evidence and the future of apps, social media, chatbots, and virtual reality. World Psychiatry 20, 318–335 (2021).
Kroenke, K., Spitzer, R. L. & Williams, J. B. The PHQ-9: validity of a brief depression severity measure. J. Gen. Intern. Med. 16, 606–613 (2001).
Sommet, N., Weissman, D. L., Cheutin, N. & Elliot, A. J. How many participants do I need to test an interaction? conducting an appropriate power analysis and achieving sufficient power to detect an interaction. Adv. Methods Pract. Psychol. Sci. 6, 1–21 (2023).
Liu, C. et al. Prevalence of depression, anxiety, and insomnia symptoms among patients with COVID-19: a meta-analysis of quality effects model. J. Psychosom. Res. 147, 110516 (2021).
Nguyen, H. T. & Zonderman, A. B. Relationship between age and aspects of depression: consistency and reliability across two longitudinal studies. Psychol. Aging 21, 119–126 (2006).
Ryan, R. M. & Frederick, C. On energy, personality, and health: subjective vitality as a dynamic reflection of well-being. J. Pers. 65, 529–565 (1997).
Ryff, C. D. Psychological well-being revisited: advances in the science and practice of eudaimonia. Psychother. Psychosom. 83, 10–28 (2014).
Seligman, M. E. P. Flourish: a visionary new understanding of happiness and well-being. Choice Rev. Online 48, 48–7217 (2011).
Acknowledgements
Preparation of this article was supported by the National Natural Science Foundation of China (32130045). We wish to thank the PauseLab team for their contributions to developing the intervention, collecting data, and implementing the experiment.
Author information
Authors and Affiliations
Contributions
X.J. designed the research and wrote the main manuscript; H.Z., Q.S., G.J., & Z.Z. gave critical feedback and edited the manuscript; L.X., C.L., M.N., Z.H. analyzed the data and wrote the results; G.M. helped write the introduction and discussion; H.Y. helped analyze the data. All authors reviewed the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Xu, J., Han, Z.R., Lv, X. et al. A scalable mental health intervention for depressive symptoms: evidence from a randomized controlled trial and large-scale real-world studies. npj Digit. Med. 8, 491 (2025). https://doi.org/10.1038/s41746-025-01888-5
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s41746-025-01888-5
This article is cited by
-
Increasing engagement with cognitive-behavioral therapy (CBT) using generative AI: a randomized controlled trial (RCT)
Communications Medicine (2026)