Abstract
This systematic review examines the role of technology-based interventions in supporting lung cancer patients during their treatment. It identifies (1) the different technologies utilized, (2) their functions and benefits, and (3) the barriers encountered by patients. The authors searched six databases for literature examining the use of technology to support treatment among lung cancer patients. Twenty-three papers were included. We mapped each technology, telehealth platforms, online portals, and mobile apps, to specific treatment phases (pre-treatment, active treatment, post-treatment) and symptom domains (symptom management (N = 17), emotional distress (N = 12), and patient–provider communication (N = 7)). Our results demonstrate that technology can effectively alleviate treatment-related symptoms, reduce emotional burden, and enhance communication. Key barriers included low digital literacy and limited device access. By explicitly linking intervention types to treatment stages and patient needs, this review provides a practical framework for designing and implementing tailored digital support strategies in lung cancer care.
Similar content being viewed by others
Introduction
Lung cancer remains a significant public health concern worldwide, with an estimated 2.5 million new cases diagnosed and 1.8 million deaths in 20201. The burden of lung cancer is projected to increase to 4.62 million new cases and 3.55 million deaths by 20501. Lung cancer mortality has been decreasing, reflecting successes in early detection and treatment advancements2,3. Lung cancer treatment has advanced significantly, offering various options tailored to the cancer’s type and stage4. Treatment selection is highly individualized, considering factors such as the cancer’s specific characteristics and the patient’s overall health4. For early-stage non-small cell lung cancer (NSCLC), curative surgery is often the primary treatment. In cases where surgery is not feasible, radiation therapy is an alternative4. For both locally advanced and metastatic NSCLC, there is an increasing array of systemic therapy options, including chemotherapy, immunotherapy, and biomarker-directed targeted therapies. Mutations in EGFR and ALK, for instance, are considered highly targetable with oral tyrosine kinase inhibitors. These have transformed our approach to treating patients with lung cancer.
Patients undergoing lung cancer treatment often experience a combination of physical, psychological, and financial challenges that may adversely affect outcomes. Treatments such as chemotherapy, radiation, and surgery can lead to fatigue, nausea, immune suppression, or respiratory complications, while the disease itself often causes persistent symptoms5,6,7. These burdens are compounded by emotional distress, uncertainty, and financial strain, making the treatment experience especially difficult for many.
Various review studies have highlighted the role of informatics in supporting cancer patients across different phases of the cancer continuum, including prevention, diagnosis, treatment, survivorship, and end-of-life care8. For instance, as Hong and colleagues reported, digital interventions have been applied to facilitate patient-provider communication, with studies reporting positive outcomes in symptom management and decision-making among cancer patients and survivors8. A review by Samadbeik and colleagues examined mobile health (mHealth) technologies to provide educational resources to cancer survivors and connect with healthcare providers electronically9. Another review by van Deursen et al. showed that eHealth interventions positively affect sleep quality, fatigue, and physical activity in cancer patients10. However, these prior syntheses did not focus specifically on lung cancer patients during active treatment, a period characterized by severe symptom burden, treatment complexities (e.g., multimodal regimens, biomarker-driven therapies), and pronounced disparities in care access1. By concentrating solely on the treatment phase in lung cancer, our review diverges from general oncology overviews and instead provides a targeted analysis of (1) which technologies have been deployed, (2) how they address the unique clinical and psychosocial challenges of lung cancer therapy, and (3) the specific barriers and facilitators to their implementation in this high-need population.
Results
The reviewed articles demonstrated high methodological quality (A and B score), primarily using appropriate qualitative approaches and adequate data collection methods. Thus, all studies were included. While all randomized controlled studies showed no selection bias and comparable groups, one faced attrition bias11, and the blinding of assessors was not reported, raising detection bias concerns11. Most non-randomized studies had representative samples, but only a few adequately addressed confounders12,13. Mixed-method studies provided solid rationale and integration of methods, but only one study adequately addressed divergences in results. The entire appraisal results are shown in Supplementary Table 1.
Data extraction and study characteristics
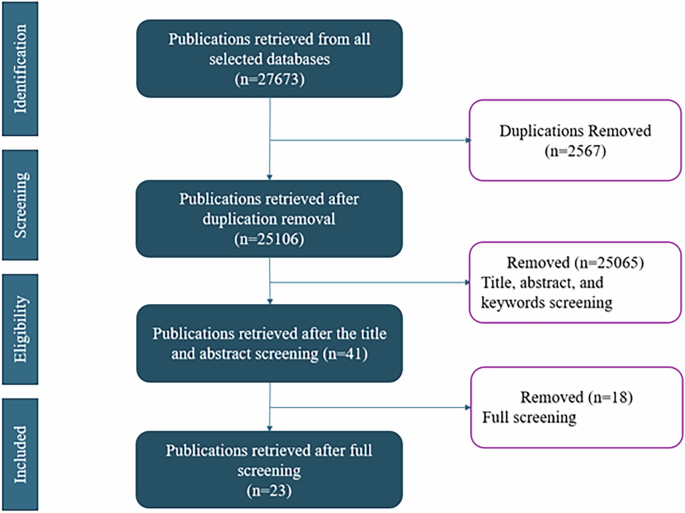
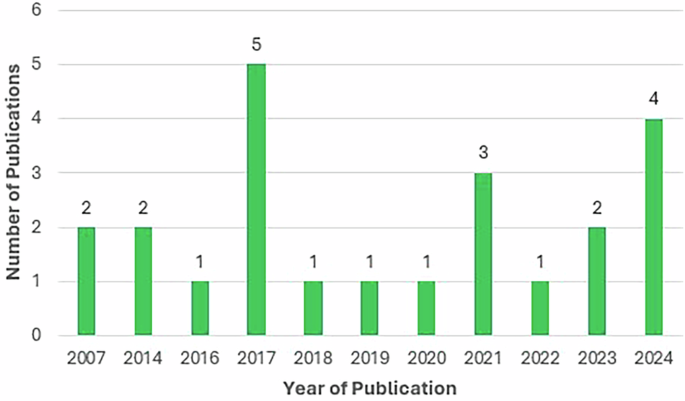
A total of 27673 articles were retrieved from the databases. We included 5345 articles for the title review after removing 2567 duplicates and 209 reviews and meta-analysis. We screened the title and abstract of the studies and found 41 eligible articles. Eventually, we found 23 eligible articles through a full review, as shown in Fig. 1. Figure 2 indicates the yearly distribution of the included studies. Studies included were published between 2007 and 2024, with two studies published before 2010 14,15, 10 published between 2010 and 201912,13,16,17,18,19,20,21,22,23, and 11 published between 2020 and 202411,24,25,26,27,28,29,30,31,32,33. All findings are summarized in Table 1 and Supplementary Table 2.
Figure 3 maps out the geographic distribution of the countries where the studies were conducted. Eleven studies were conducted in Europe13,16,17,18,19,20,25,27,28,31,32, including four studies in France18,19,25,28, and three studies in the Netherlands16,17,20. Nine studies were conducted in North America, all in the United States11,14,15,21,24,26,29,30,33. Three studies were conducted in Asia12,22,23.
The studies used different technologies, including telehealth (n = 9)11,13,15,18,24,26,28,29,33, online portals (n = 8)12,16,17,20,27, mobile applications or mHealth (n = 8)18,19,21,23,30,31,32, electronic assessment tools (n = 3)13,22,25, and virtual reality (n = 1)14.
Twenty-three interventions were delivered by healthcare providers (HCPs): five studies utilized a multidisciplinary team involving various providers, such as oncologists, physiologists, and nurses16,24,25,27,33, five studies involved nurses13,14,15,21,22,30, six studies involved physicians11,17,18,19,23,26, two studies involved physical therapists24,28, one study involved emergency department HCPs12, and one study resorted to specialized trainers to deliver the intervention sessions29. Primarily, the interventions were delivered in home settings (n = 20)11,12,13,15,16,17,18,19,20,21,23,24,26,27,28,29,30,31,32,33, clinic settings (n = 2)14,22, and in both settings (n = 1)25, with a reported duration ranging from one single session12,19 to up to 30 months25. The median duration of the 25 interventions with a specified delivery length was three months. Seven of the included studies were guided by theoretical frameworks. The theories used were social cognitive theory29, user-centered design principles16, value-based healthcare principles27, chronic care self-management model24, and Lazarus and Folkman’s stress and coping model14.
Study Populations and Treatment Challenges
The study included cancer patients at different stages of the diagnosis. Eight studies included patients with both local and metastatic cancer15,17,18,19,20,21,23,25,26,27,29, eight studies had only patients with advanced-stage or metastatic cancer11,28,30,31,32, one study included only patients with stage I cancer16, and eight studies did not specify the stage of cancer of the study population12,13,14,22,24,33. These patients were undergoing a variety of treatment regimens: 15 included patients undergoing chemotherapy11,13,14,15,17,18,19,20,21,23,25,27,29,31,32, nine included surgical patients12,13,17,18,19,20,24,26,29, six included patients undergoing radiotherapy13,18,19,20,26,29, two included patients undergoing targeted therapy18,25 and in three studies, patients had immunotherapy25,27,28. One study included patients in hospice care30.
Issues faced by patients in the different treatment regimen
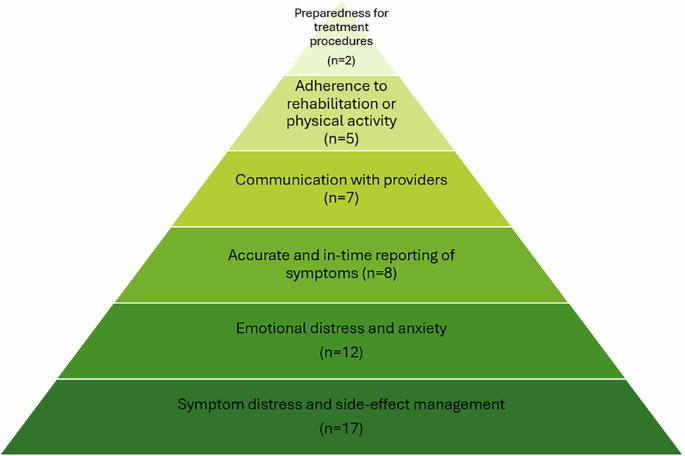
The included studies presented technology as a solution to different physical, mental, social, and treatment-related issues. Overall, 17 out of 23 studies covered symptom distress and side-effect management11,12,14,15,18,19,20,21,23,24,25,27,29,30,31,32,33, making it the most frequently addressed patient issue, followed by emotional distress and anxiety (n = 12)11,12,14,17,20,24,27,28,29,30,33, accurate and in-time reporting of symptoms (n = 8)18,19,21,22,25,27,30,32, communication with providers (n = 7)13,19,20,23,24,25,26,27,28,29,31,32, adherence to rehabilitation or physical activity (n = 5)20,23,24,28,29, and preparedness for treatment (n = 2)16,17,24. Intervention targets differed by treatment regimen. For instance, studies covering patients undergoing chemotherapy focused on symptom distress and side-effect management (n = 13)11,14,15,18,19,20,21,23,25,27,29,31,32, emotional distress and anxiety (n = 6)11,14,17,20,27,29, accurate and in-time reporting of symptoms (n = 6)18,19,21,25,27,32, and communication with providers (n = 6)13,19,25,27,31,32. The most common intervention focus for people undergoing surgery were symptom distress and side effect management (n = 6)12,18,19,20,24,29 and emotional distress and anxiety (n = 5)12,17,20,24,29. Studies reporting on patients who had radiotherapy reported symptom distress and side-effect management (n = 4)18,19,20,29 and communication with providers (n = 3)13,19,26 as the most common challenges addressed. Figure 4 summarizes the patients’ needs going from the most cited in the basis to the least cited in the top.
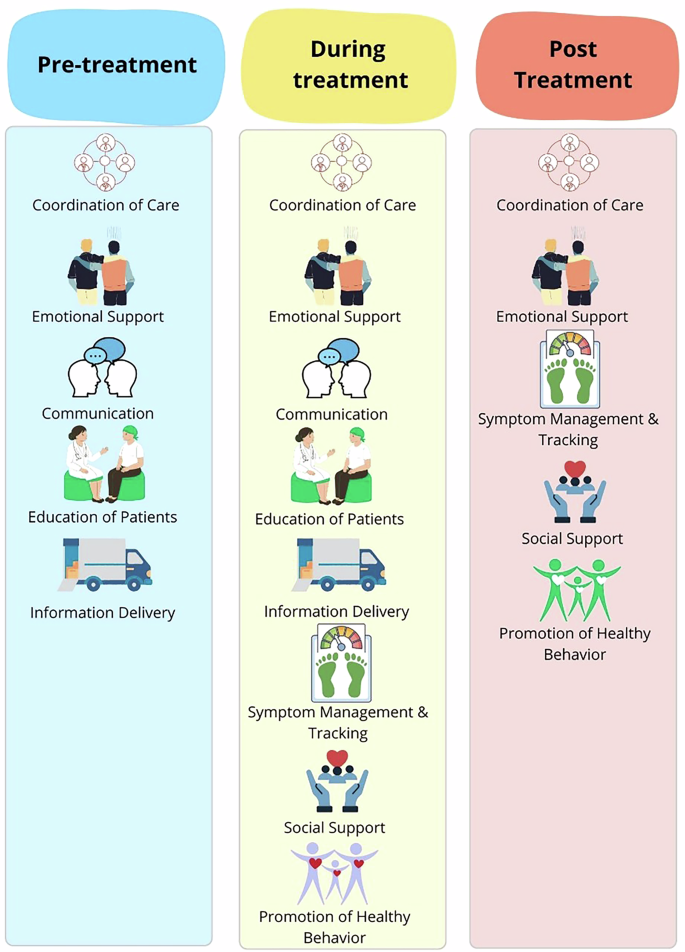
In developing study tools, the research teams either adapted commercial technologies or created specific ones tailored to their studies. Mobile applications utilized study-specific design (n = 7)18,19,21,23,30,32 and commercial tools (n = 1)31. Four of the eight telemedicine tools were designed for the study11,15,29,33, while four used commercial tools13,24,26,28. The interventions using web-based portals (n = 5) involved study-specific design (n = 4)12,16,20,27 and commercial tools (n = 1)17. Electronic questionnaires (n = 2) were designed specifically for the study22,25. One intervention used virtual reality and adopted a commercial tool14. Figure 5 illustrates how technology was utilized to meet patient needs in the pre-treatment, active, and post-treatment phases.
Technology-based tools developed to support lung cancer treatment (Pre-treatment)
Technology was used to support communication and coordination, education and information exchange, and the emotional needs of lung cancer patients in the pre-treatment phase.
Telemedicine supported communication and coordination of care in the pre-treatment phase. During the pandemic, telemedicine visits for thoracic cancer patients demonstrated significant efficiency. Newly diagnosed patients seen via telemedicine reported significantly shorter median time from referral to initial visit (5·0 vs. 6·5 days, p <·001) compared to the in-person visit group, with no difference found for the time from initial visit to treatment initiation26.
Websites effectively supported education and information exchange in the pre-treatment phase. For instance, Schook et al. implemented a web-based Q&A portal called “Ask the Physician” on the Dutch Lung Cancer Information Center’s website, allowing patients and caregivers to ask lung specialists questions17. Similarly, Hopmans et al. used a patient information website for stereotactic ablative radiotherapy for early-stage lung cancer patients16. Patients reported an increased understanding of treatment and disease trajectory after using the websites16,17.
In the pre-treatment phase, websites helped reduce patients’ emotional distress. The “Ask the Physician” portal promptly responded to patients’ questions. Some patients reported reduced anxiety while awaiting their next visit in the follow-up interview. Patients also felt emotionally supported as they became more prepared for the disease trajectory and future treatment after utilizing the website17.
Technology-based tools developed to support lung cancer treatment (active treatment)
Technology supports patients in communication and care coordination during active treatment, education and information exchange, emotional and social support, monitoring and tracking, and promoting healthy behaviors.
Technologies supporting communication included electronic questionnaires, mHealth apps, telemedicine, and websites. Electronic questionnaires enhanced care coordination during patient visits. Mouillet et al. assessed the adaptation of a health-related quality of life (QoL) questionnaire with cancer patients before each visit, after which physicians prescribed supportive care (8.3%) and adapted patient management (5.2%)25. Tang et al. developed a symptom assessment tool targeting fatigue, pain, dyspnea, and anxiety, with patients reporting that the tool filled the gap in the current oncology service as symptoms were rarely discussed22. Kathi et al. conducted a randomized control trial on a mHealth application, Symptom Care at Home (SCH), that combined symptom reporting, automated self-management coaching, and follow-up calls with nurse practitioners. The SCH group showed a significantly higher reduction in severe and moderate symptoms compared to enhanced usual care. (both p < ·001)21. Two studies used telehealth in the active treatment phase to support the improvement of patients’ health-related QOL during chemotherapy15 and early palliative care11. Telehealth with a registered nurse increased health-related QOL for older adults by 8.14 points at six months (p = ·007)15. Video-based palliative care showed an equivalent effect on QoL (mean difference 2.0, 90% CI: 0·1–3·9) compared to in-person care for advanced NSCLC patients11. Several studies used web-based portals to support patients’ communication with HCPs. One study by Misplon et al. created a multidisciplinary team to support a digital portal for online follow-up and collection of patient-reported outcomes, which showed the potential to facilitate conversations between patients, caregivers, and providers27.
MHealth applications were used to educate patients in the active treatment phase. The interventions supported patients by increasing exercise capacity23, reducing symptom severity21,23, and preventing unexpected visits to emergency departments23. Park et al. provided patients with an Internet of Things (IoT) wearable device and the Smart Aftercare application, containing a comprehensive pulmonary rehabilitation program with videos for physical exercise, symptom management, and nutritional support. Patients had significant improvement on symptom scale scores for fatigue (p < ·001), anorexia (p = ·047), and diarrhea (p = ·01), but there was no significant improvement in QoL (p = 0.06) or severity of pain (p = ·24)23. The SCH app designed by Mooney et al. significantly improved patients’ outcomes since substantially less severe symptoms severity were reported for all symptoms (p < 0.001)by SCH participants compared to participants with usual care21. The MyAVL online patient portal offered personalized education materials about disease and physical activity. There was no significant improvement in patient outcome, including physical activity and quality of life20. Tang et al. provided patients with tailored symptom self-management videos. Patients reported that learning from a tablet with videos facilitated the mastery of self-management skills22.
Various technologies provided emotional support in the active treatment phase. Rose et al. used an online questionnaire, the electronic Sheffield Profile for Assessment and Referral for Care (eSPARC), with lung cancer patients to enhance follow-up care and support satisfaction. Patients reported appreciation for emotional support and reduced anxiety during the qualitative interviews13. Schneider et al. utilized virtual reality to address symptom distress during chemotherapy treatment. Patients reported an altered perception of time (p < 0.001) but no significant difference in symptom distress measured through the State Anxiety Inventory for Adults (p = ·15)14 Additionally, Misplon et al.’s digital portal increased conversations with psychologists compared to standard care. Seven out of 15 patients in the intervention arm had contact with a psychologist, while two out of 15 patients in the control arm had done so27.
Multiple studies used mobile applications to monitor patients’ symptoms in the active treatment phase. The Lalaby app by Asensio et al. collected patient symptoms through self-report and mobile sensors. They found significant correlations between app usage and emotional and symptomatic scores. For instance, the number of calls was negatively correlated with emotional scores (p = ·025) and positively correlated with the symptomatic dimension score (p = ·012)32. Patients who participated in the study on eSPARC (an electronic questionnaire combined with phone consultations) reported increased satisfaction with cancer care and QoL13. There was a 20% increase in the number of patients who reported satisfaction with the supportive care needs survey between the first and third surveys. Compared to the first and third Functional Assessment of Cancer Therapy—Lung, there was a 25% increase in patients who reported content with their quality of life13. The Kaiku Health mobile application allowed patients to report their symptoms weekly and alert HCPs about critical symptoms. Patients agreed that the use of Kaiku Health helped them to be better informed about the disease (65%), improved conversations between patients and providers (70%), and improved cancer care (51%)31. Two studies applied an integrated automated symptom reporting tool with symptom management coaching, and patients who used the mobile app showed a reduction in severe and moderate symptoms compared to the group with usual care21,30. Patients under chemotherapy who used SCH indicated significant reduction for severe (67% less) and moderate (39% less) symptoms compared to patients with usual care (both p < ·001)21. For patients in hospice care and caregivers supported by the same tool, SCH produced a symptom reduction of 4·89 severity points (95% CI 2·86–6.92, p < ·001)30.
Park et al.‘s mobile application has a pulmonary rehabilitation program and access to symptom management resources, and it is linked to an Internet of Things wearable device23. It improved the exercise capacity of the patients, as patients had a significant increase in score for the 6-minute walk test (6MWT) at 6 and 12 weeks (both p < ·001)23. Telemedicine was applied in multiple studies to promote rehabilitation for patients in active treatment. Loy et al. created a Virtual Integrative Oncology Shared Medical Appointment Series (VIOSMAS) that covered various topics, including nutrition, culinary arts, herbs/botanicals, exercise, narrative medicine, etc. Patients could incorporate recommended lifestyle changes, and they reported that the tool addressed and improved symptom distress, including sleep, fatigue, anxiety/fear, gastrointestinal symptoms, and pain/weakness in the post-session assessment, while no direct measure on patient outcome was reported33. The PACTIMe-FEAS study by Charlet et al. applied telehealth sessions on physical activity, finding a significant 2.1-point mean decrease in fatigue (p = ·0161)28. Lastly, MyAVL, an online patient portal, provided tailored physical activity support to patients, but we did not find any significant improvement in patient outcomes20.
Technology-based tools developed to support lung cancer treatment (Post-treatment)
In the post-treatment phase, patients’ support consisted of monitoring and coordination of care, emotional and social support, and promotion of healthy behavior.
Mobile applications play a crucial role in post-treatment care and early relapse detection. Denis et al. randomized patients to use a mobile application, “sentinel,” or regular follow-up post-treatment18. Similarly, another team of researchers in France performed a randomized trial to compare patient outcomes using a web-mediated follow-up algorithm with regular surveillance19. The two applications required the patients to complete a weekly symptom self-assessment form between follow-up visits. The app sends real-time data and alerts oncologists of alarming symptoms of relapse. Subsequently, the medical team adjusted the current supportive care and organized imaging and follow-up visits18,19. Denis et al. found that the median survival time was significantly longer for patients using the sentinel app (22·4 months) compared to patients who received regular follow-up (16 months, p = ·0014)19. The algorithm study found that the median overall survival was 19·0 months for the experimental group compared to 12·0 months for the control group (p = ·001). There is a significant difference in the number of patients who initiated optimal treatment in the experimental arm compared to the control arm (p < ·001)18.
Li et al. explored a telemedicine program’s efficacy for lung cancer patients with chronic post-surgical pain. Patients were randomized to receive treatment and psychological support in person or via the Internet. There were no significant differences in the QoL or the satisfaction rate in the group with in-person care versus the group with telemedicine (p > ·05)12.
Several studies have used telemedicine to support patients in post-treatment rehabilitation. Li et al.’s program educated patients on lifestyle adjustment and pain management12. Ha et al. delivered a 12-week intervention on exercise training, education, and behavior change to lung cancer survivors29. The research team found significant improvement in the health-related QoL measured by the St. George’s Respiratory Questionnaire of patients who participated in telemedicine intervention compared to the control group at baseline (standardized effect size: −1·03 to −1·30)29. In contrast, Li et al. found no difference in QoL for patients in the telemedicine group compared to patients who received in-person care assessed by the 36-Item Short Form Health Survey(SF-36) (p > 0.05)12. Lafaro et al. discovered that telehealth sessions on occupation and physical therapy improved the functional capacity measured by 6MWT by 6 points, while the difference was not significant compared to baseline (p = ·70). However, patients showed significant improvement in short physical performance battery score compared to baseline (p = ·01)24.
Barriers to technology use for treatment support
The studies also reported various technological barriers, including low digital skills, confusion and information overload, cost, access to technology, preference for in-person care, and reliability regarding electronic reporting. Access to technology was one of the most prevalent challenges highlighted by the studies18,21,26,28,29. This included barriers such as unreliable phone signals29, difficulty accessing and affording the Internet, and access to digital devices like smartphones21. Low digital literacy was a significant concern, as some patients struggled with navigating tools and understanding content and required setup assistance due to limited experience or competence with technology18,19,20,22,25,27,31,33. Complex visual representations, complicated login processes, and limited compatibility with specific operating systems exacerbated these challenges20. Confusion and information overload emerged as another challenge, with participants feeling overwhelmed by excessive information, leading to reduced technology use17,24. In a few studies, patients preferred in-person care, citing challenges with remote instructions and greater comfort with in-person interactions compared to internet-based alternatives12,17. Finally, reliability regarding reporting was an issue, as some patients found it difficult to accurately report their symptoms or align their perceived quality of life with structured questionnaires22,32. These themes highlight the multifaceted barriers to effective technology use in healthcare, emphasizing the need for improved accessibility, support, and user-centered design.
Discussion
This review study explored the role of health informatics in supporting lung cancer patients in the pre-, active, and post-treatment phases, supporting people at different stages of cancer. Twenty-three studies were included for review covering various technologies, including nine telehealth applications11,13,15,18,24,26,28,29,33, eight patient portals12,16,17,20,27, eight mHealth 18,19,21,23,30,31,323 electronic assessment tools13,22,25, and one virtual reality tool14.
These tools were developed to help patients undergo various treatment regimens, including chemotherapy (n = 15), surgery (n = 9), radiotherapy (n = 6), targeted therapy (n = 2), and immunotherapy (n = 3). The emphasis on chemotherapy and surgery likely reflects their historical predominance and the clear benefits of controlling treatment-related symptoms, studies show that well-managed nausea, fatigue, and pain lead to better adherence and improved quality of life34,35,36. Immune checkpoint inhibitors were not approved for lung cancer until 2015, before then, chemotherapy was the main systemic option, and targeted agents became widely available only subsequently, for a smaller subset of patients37,38. Consequently, fewer digital or VR supports exist for immunotherapy and targeted therapy, though as these treatments become more common and evidence mounts that early symptom management (e.g., addressing immune-related adverse events) reduces interruptions, development in this area is expected to grow39,40.
Support was given to different challenges faced by patients, including symptom distress and side-effect management11,12,14,15,18,19,20,21,23,24,25,27,29,30,31,32,33, making it the most covered challenge, followed by emotional distress and anxiety11,12,14,17,20,24,27,28,29,30,33, accurate and in-time reporting of symptoms18,19,21,22,25,27,30,32, communication with providers13,19,20,23,24,25,26,27,28,29,31,32, adherence to rehabilitation or physical activity20,23,24,28,29, and preparedness for treatment procedures16,17,24. Cancer treatments, especially chemotherapy and radiotherapy, often cause severe physical side effects such as nausea and pain6,41,42. Tools may be prioritized to manage these symptoms as they directly affect patients’ quality of life and can lead to treatment discontinuation if unmanaged42. After addressing the physical symptoms, the next logical focus should be mental health support, as the physical toll of treatment, together with uncertainty and fear, causes emotional distress among patients42. This order of coverage of challenges reflects a patient’s needs based on their importance, from the most pressing to the least pressing.
Our study revealed that technology-based interventions for lung cancer patients vary significantly across the cancer treatment continuum, with different technologies helping patients in the pre-, active, and post-treatment phases.
In the pre-treatment phase, technology, such as telemedicine, was used to support communication and coordination between patients and healthcare providers, ensuring patients conveniently received timely information about their diagnosis, treatment options, and care logistics. This aligns with existing literature highlighting the importance of clear communication during pre-treatment to alleviate uncertainty and facilitate informed decision-making43,44.
Additionally, providing educational and informational support through mhealth, telehealth, and patient portals was prominent in this phase. This finding reflects a growing recognition of patient education as a critical component of pre-treatment in lung cancer. Prior research has recognized that well-informed cancer patients are more likely to make decisions and adhere to the recommended care plans44,45. The successful implementation of web-based portals, such as Hopmans et al.’s educational website on stereotactic ablative radiotherapy16, aligns with previous findings that digital portals enhance patient knowledge and preparedness44. Such solutions bridge the knowledge gaps and mitigate the risks of overwhelming diagnosis by providing timely and reliable information to foster patients’ empowerment and reduce decisional regret46.
Furthermore, using emotional support tools during the pre-treatment phase highlights the integrality of psychosocial care in oncology17. Using tools such as the “Ask the Physician” portal to reduce anxiety and provide emotional reassurance mirrors results from previous research that links pre-treatment distress alleviation to patients’ preparedness17, which aligns with the Stress and Coping Theory by Lazarus et al47., suggesting that reducing uncertainty can enhance emotional well-being.
In the treatment phase, diverse technology-based interventions were captured, highlighting the increasing reliance on digital solutions to improve the treatment experience for patients. The widespread use of communication and coordination tools such as mHealth apps, telemedicine, and web-based portals demonstrates the essential role of continuous interaction between patients and healthcare providers in active treatment and the importance of technology in supporting the quality of this communication. This finding aligns with prior studies emphasizing that practical communication tools improve patient outcomes48.
The review also revealed that several tools have been developed to provide patients with educational and informational support16,17. The significance of educating and informing patients extends throughout the treatment process, not merely before its commencement20,21,22,23. In the pre-treatment phase, information was predominantly provided regarding treatment regimens; however, the various tools featured in the reviewed studies also offered insights into exercise programs, nutrition, symptom management, and dietary considerations16,17. These studies evidenced improvements in symptom management, corroborating existing literature that suggests well-informed patients are more likely to adhere to prescribed treatment regimens49. Nonetheless, in contrast to inconclusive research findings that advocate for the positive influence of patient information on their quality of life, specific tools utilized in these studies did not yield any discernible impact on patients’ overall quality of life23. This discrepancy raises an important consideration: it may not be the technology itself that is inherently limited in improving quality of life, but rather the methods used to assess it. Many commonly used patient-reported outcome measures (PROMs) may lack the sensitivity to detect the nuanced benefits of educational tools, such as increased confidence, empowerment, or reduced decisional conflict, which may not be fully captured in general quality of life scores. Additionally, it is possible that the impact of education is moderated by other unaddressed factors, such as ongoing physical symptoms or emotional distress, which may overshadow improvements in patient knowledge. Such mixed results illuminate the persistent challenge of reconciling information dissemination with patient engagement, a gap acknowledged within digital health literature. Therefore, future research should consider both refining outcome measurement tools and designing multifaceted interventions that target multiple dimensions of patient experience.
The utilization of technology in facilitating patient care in active treatment has also encompassed the provision of emotional reassurance and social support through innovative tools such as eSPARC and virtual reality13,14. This observation corresponds with the increasing recognition of the importance of psychosocial well-being among patients undergoing cancer treatment50. However, the limited effects of these interventions on symptom distress in certain studies imply that, while technology can augment emotional support, there is a necessity for more personalized and integrative approaches as corroborated by Northouse et al51. Northouse et al. demonstrated that truly holistic care combines structured psychoeducation, skills-based coping workshops, caregiver involvement, and spiritual or meaning-centered support, components shown to improve both patient and family quality of life51. Furthermore, these insights highlight the critical demand for tailored interventions that effectively address patients’ unique psychological needs throughout their treatment journey.
In addition, utilizing technologies for monitoring and tracking symptoms has proven beneficial for patients by facilitating real-time symptom assessments, thus ensuring prompt interventions and enhancing patient satisfaction with care18. This observation corroborates earlier research that underscores the significance of continuous monitoring in fostering communication between patients and healthcare providers while concurrently mitigating symptom severity52,53. Innovations such as the Symptom Care at Home application and telehealth services have not only streamlined the process of symptom reporting but have also refined treatment regimens54. This aligns with the findings of Basch et al. (2016), which indicate that regular symptom monitoring through digital portals is instrumental in improving survival outcomes in oncology contexts55. However, these promising results should be interpreted cautiously given the potential for publication bias toward positive findings in digital-health research. Nevertheless, the discrepancies in effectiveness across various monitoring tools underscore the critical need for user-centric designs and their seamless integration into clinical workflows to achieve optimal results56.
Finally, the emphasis on fostering healthy behaviors via mobile applications and telemedicine interventions underscores a transformative trend toward holistic cancer care, wherein lifestyle alterations, including individualized exercise prescriptions, dietary coaching, stress-management techniques, and peer or clinician-led motivational support, are essential for successful treatment outcomes23,33.
The noteworthy advancements in physical activity and symptom distress documented in these studies align with the findings articulated by Pinto and Trunzo (2005), which underscore that physical rehabilitation in active treatment significantly enhances both patient well-being and treatment adherence57.
In the post-treatment phase, technological advancements have significantly enhanced the monitoring and coordination of care support. The authors’ findings substantiated the integration of mobile health solutions for follow-up care and early relapse detection, highlighting that applications such as Sentinel and web-mediated follow-up algorithms facilitate continuous symptom monitoring and enable timely interventions19. An accumulating body of evidence underscores that early detection and prompt relapse management can substantially improve survival outcomes in lung cancer patients58. The marked extension of median survival time observed in studies conducted by Denis et al. and others illustrates that real-time data collection, coupled with automated alerts59, can markedly enhance clinical decision-making and ensure the timely initiation of optimal treatment, a notion further corroborated by earlier research on remote monitoring in oncology60,61. These findings reinforce the imperative for the broader adoption of digital follow-up tools within lung cancer care while highlighting the potential barriers—such as digital literacy and data security—that must be diligently addressed to guarantee equitable access to these technological advancements27.
Emotional and social support remain critical in the post-treatment phase for all cancer patients and lung cancer patients precisely62. Li et al.’s study revealed that virtual psychological support can be as practical as in-person care to manage chronic post-surgical pain and maintain patient satisfaction12. This finding is consistent with prior studies indicating that telehealth interventions provide comparable psychological benefits to face-to-face consultations63. However, the lack of significant differences in quality of life (QoL) between the two groups also underscores the need for further research into personalized telemedicine approaches that can better address the unique emotional needs of lung cancer survivors, particularly those with complex post-treatment challenges.
Finally, telemedicine also facilitated the promotion of healthy behaviors, such as lifestyle adjustments, pain management, and rehabilitation exercises in the post-treatment phase12,24,29. This highlights the role of digital interventions in supporting long-term survivorship12,24,29. Studies such as those by Ha et al. and Lafaro et al. demonstrate that structured telehealth programs can improve functional capacity and QoL24,29, reinforcing findings from Alfano et al. that physical rehabilitation is critical for enhancing cancer survivorship64. However, the mixed results in QoL improvements call for further investigation into tailored rehabilitation interventions and the long-term impact of telemedicine on survivorship outcomes, particularly in diverse lung cancer populations.
The barriers associated with technology use in supporting lung cancer patients during treatment manifest critical obstacles that may impede the efficacy and uptake of digital health interventions. Access to technology—characterized by unreliable telecommunications, affordability of internet services, and limited access to digital devices—correlates with broader literature findings that underscore the persistent digital divide in healthcare65.
This divide disproportionately impacts older adults, rural communities, and socioeconomically disadvantaged populations, raising significant concerns about equitable access to digital health solutions in the realm of lung cancer care27,66,67. Inadequate digital literacy remains a significant barrier, making it essential for technologies to incorporate user-centered design principles such as simplified interfaces, clear instructions, and accessible technical support68,69. When platforms are not intuitive, patients may disengage entirely, leading to poorer health outcomes. Information overload is another persistent barrier. Digital platforms that present excessive or poorly curated content may overwhelm patients, diminishing their engagement¹⁷. This highlights the importance of tailoring content to patients’ needs and structuring information in digestible formats17. Despite the convenience of telehealth, many patients continue to prefer in-person care, particularly when managing complex treatment regimens12,70,71. Such preferences may also reflect deeper trust in face-to-face relationships, cultural norms around caregiving, or data-privacy concerns, rather than solely digital literacy issues. These findings suggest that hybrid models, combining digital tools with traditional consultations may be more acceptable and effective for lung cancer patients. Lastly, challenges relating to the reliability of electronic reporting draw attention to patients’ difficulties in accurately documenting symptoms and health-related quality of life metrics via digital portals. This is consistent with literature indicating that subjective self-reports often exhibit inconsistency, particularly when patients lack familiarity with structured electronic assessments. Additionally, many patients struggle with reliably reporting symptoms and health-related quality of life through electronic tools32. This may stem from unfamiliarity with structured digital assessments72,73, underscoring the potential value of automated symptom monitoring using wearables or AI-based tools. Together, these challenges highlight the need to move beyond one-size-fits-all digital interventions and toward more inclusive, accessible, and patient-centric designs. Future efforts should focus on bridging digital literacy gaps, improving usability, and promoting equitable access, ensuring that all patients can benefit from digital innovations in lung cancer care. Future research endeavors should investigate advanced solutions, such as automated symptom detection through wearable sensors and AI-driven assessments, to enhance the accuracy and reliability of patient-reported data. However, the heterogeneity of outcome measures across studies, as well as frequent reliance on small, single-center samples, may limit direct comparisons and generalizability, underscoring the need for larger, multi-site trials using standardized metrics. These challenges highlight the imperative for more inclusive, accessible, and patient-centric technological solutions in lung cancer care. Addressing barriers such as inadequate digital literacy, access, and user fatigue is essential to ensure that all patients benefit from digital health interventions equally. Future initiatives should develop adaptive technologies that meet patients’ diverse needs, provide robust technical support, and promote digital literacy to bridge the divide between technological innovation and practical, equitable healthcare delivery. Future work should also examine whether these short-term improvements translate into sustained quality-of-life gains over multiple years.
Our research yields significant implications for advancing, implementing, and scaling technology-based interventions in lung cancer care. Firstly, the prevalent utilization of technologies assisting chemotherapy patients underscores an imperative to reallocate resources toward enhancing digital interventions for other treatment regimens, such as immunotherapy and targeted therapy. These modalities are increasingly adopted yet remain inadequately supported. This disparity presents a substantial opportunity for healthcare technology developers to innovate and engineer customized digital tools tailored to these emergent treatment modalities. This ensures equitable access to technological advancements across diverse patient populations. Yet, no included study conducted a formal cost-effectiveness analysis, leaving unanswered questions about scalability in resource-constrained settings.
Furthermore, the study’s identification of symptom distress management as the predominant challenge underscores the critical necessity of symptom monitoring tools in enhancing patient quality of life and adherence to treatment protocols. Healthcare providers and technology developers need to prioritize the integration of comprehensive symptom management functionalities into digital portals, particularly for patients undergoing treatment regimens with substantial physical demands, such as chemotherapy and radiotherapy. Moreover, the pronounced emphasis on emotional distress management suggests a concomitant need for psychosocial support interventions, indicating that prospective digital solutions ought to incorporate resources for mental health, counseling services, and peer support networks to mitigate the emotional burdens associated with cancer treatment.
The study elucidates the role of technology in facilitating communication, ensuring timely symptom reporting, and promoting physical rehabilitation, implying that oncology care teams should systematically integrate digital tools into standard care protocols. Deploying mobile applications, patient portals, and telehealth services as integral components of routine cancer care may significantly enhance communication between patients and healthcare providers, enable real-time symptom tracking, and support rehabilitation efforts, ultimately optimizing patient outcomes and diminishing hospital visits.
Importantly, future technology implementations must adopt a patient-centered design philosophy, emphasizing usability, accessibility, and inclusivity. Digital tools should be co-developed with patients, incorporating their feedback to ensure features align with their lived experiences, cultural contexts, and specific needs. This participatory approach not only fosters greater adoption but also strengthens trust and perceived relevance of digital interventions.
Equally essential is the application of human-computer interaction (HCI) principles to optimize user engagement and reduce cognitive burden. Interfaces should be intuitive, responsive, and adaptable to diverse literacy levels. Employing personalization features—such as simplified dashboards, language translation, voice guidance, and customizable alerts—can help reduce digital fatigue and ensure consistent user interaction. Furthermore, leveraging behavioral nudges and gamification within apps may encourage adherence to treatment and self-monitoring behaviors without overwhelming users.
Moreover, the findings delineate the order of importance in patient needs, wherein physical symptom management assumes paramount significance, followed by emotional support and communication requirements. This revelation suggests that healthcare providers should adopt a phased approach in introducing digital interventions, initially concentrating on managing acute physical symptoms before expanding to encompass psychosocial support and long-term rehabilitation. This strategic framework prioritizes patient needs, fostering enhanced engagement with digital tools.
Additionally, the review highlights the necessity of addressing inherent challenges such as digital literacy, access to technology, and user fatigue. Practical measures to alleviate these challenges include providing patient training programs on digital health tools, financial assistance, or subsidized devices for underserved demographics and creating user-friendly portals with intuitive interfaces. Collaborative efforts between healthcare institutions and policymakers are paramount to successfully implementing these solutions, ensuring equitable access to digital health interventions across varied patient demographics.
Lastly, the comprehensive exploration of technology utilization throughout the pre-treatment, treatment, and post-treatment phases accentuates the necessity for integrated digital care pathways supporting lung cancer patients throughout their treatment continuum. Healthcare providers should harness these insights to design cohesive digital ecosystems that facilitate patient navigation from diagnosis to survivorship, enhancing their overall care experience and improving clinical outcomes.
In sum, the practical implications of this review extend beyond technological deployment to a call for deeper integration of user experience design, inclusive development, and human-centered evaluation frameworks. By aligning technological innovation with the principles of patient-centered care and HCI, digital interventions can achieve greater efficacy, equity, and sustainability in lung cancer treatment.
Building on the findings of our study, several future directions can help advance the use of digital health interventions for lung cancer care support focusing on the design, implementations and impact of the technologies. First, prioritization should be given to participatory approaches that actively involve different stakeholders (patients, caregivers, and providers) in the development of the technologies. Second, there is a pressing need to deepen the application of HCI principles in the development of patient-facing technologies. For example, developers might implement context-aware symptom alerts that adjust notification thresholds based on real-time patient-reported severity and integrate these into existing EHR workflows to minimize clinician burden74,75. Future work should explore adaptive user interfaces, multimodal interaction (e.g., voice, touch, gesture), and AI-driven personalization to accommodate users with limited digital literacy, physical impairments, or high emotional distress. Usability testing and user experience (UX) evaluation must become standard components of intervention development. While digital health use is important, research should focus on bridging the digital divide for equitable access, by developing low-bandwidth or offline-capable solutions, designing interventions for older adults or low-literacy users, and evaluating the effectiveness of training and support programs to improve digital literacy. There is also a need for rigorous, long-term studies evaluating the clinical effectiveness, cost-effectiveness, and patient-reported outcomes of digital interventions across the treatment continuum. To support the effective use of technology in lung cancer care, future efforts should include training programs for clinicians and allied health professionals on digital tools, human factors, and patient-centered design. Educational initiatives can help bridge the gap between clinical care and technological innovation.
Methods
We systematically reviewed the literature according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines. A PRISMA checklist is attached in Supplementary Table 3. On November 1st, 2024, we searched for the following databases for articles that fit our scope: ProQuest CENTRAL, Scopus, ScienceDirect, PubMed, Web of Science, and IEEE Xplore. The review was conducted following the PICO framework.
Population: lung cancer patients
Intervention: Technology-based treatment support
Comparison: based on the type of support given
Outcome: the effectiveness of the different technologies in supporting this population
Search strategy
We used keywords related to lung cancer, screening and treatment, and technology, as summarized in Table 2. We combined these terms using the Boolean operators “AND/OR” to identify the studies relevant to the scope of the review through MeSH terms such as (“lung cancer” AND “treatment” AND “e-health”). These search words were identified by an initial literature review and then modified by feedback from content experts and the librarian. We exported the records retrieved to Endnote 20.1 (New Jersey, USA) for duplication removal and selection processes.
Inclusion and exclusion criteria
We defined our eligibility criteria to capture studies that (1) were published on or before November 1, 2024; (2) presented empirical evidence, whether quantitative (e.g., surveys, experiments, observational cohorts) or qualitative (e.g., interviews, focus groups), pertaining to technology-facilitated oncology treatment; (3) focused specifically on interventions aimed at supporting lung cancer patients; (4) appeared in peer-reviewed journals; and (5) were available in English.
To minimize bias and preserve methodological rigor, we systematically excluded any records that did not meet these standards. In particular, we omitted (a) opinion pieces, commentaries, editorials, reviews, and other non–empirical formats; (b) articles not centered on the use of technology to support treatment processes (for example, studies of purely diagnostic devices without treatment support functions); (c) publications outside the peer-reviewed literature, including conference abstracts, white papers, dissertations, and grey-literature reports; (d) studies published in languages other than English; and (e) any empirical study judged to have a high risk of bias (quality grade “C”) under our Mixed Methods Appraisal Tool assessment, as such studies could unduly skew our synthesis despite the novelty of the field.
By applying these exclusion criteria consistently, we ensured that our review reflects high-quality, directly relevant evidence on technology-based treatment support for lung cancer patients.
Quality assessment and risk of bias
To ensure high-quality reporting, all selection steps were subject to consensus by all authors. The snowball method was also employed, where the references of included papers were reviewed to identify any relevant literature that might have been missed.
We assessed the quality of the selected studies using the Mixed Methods Appraisal Tool (MMAT), which evaluates qualitative, quantitative, and mixed-methods studies based on methodological rigor. Specifically, for qualitative studies, we examined aspects such as the appropriateness of participant recruitment strategies, data collection methods, and the coherence of data analysis. For quantitative studies, we evaluated study design, sample representativeness, measurement validity, and statistical analyses, distinguishing between randomized and nonrandomized clinical trials. For mixed-methods studies, we assessed the integration of qualitative and quantitative components, including whether the study design appropriately aligned with its research questions and how data from different methodologies were synthesized. Reviewers independently assigned a risk-of-bias judgment to each study, categorizing it as low risk, high risk, or unclear risk for each criterion. Based on these assessments. Studies meeting all criteria with a low likelihood of bias received a quality grade of “A”. Studies partially meeting criteria with a moderate risk of bias received a quality grade of “B”. Studies failing to meet criteria with a high likelihood of bias received a quality grade of “C”. Only studies with an overall quality grade of A or B were included, while those graded C were excluded from further analysis. This structured approach ensured a rigorous evaluation of study quality and minimized potential biases in our synthesis.
Data availability
The data extracted from the included articles is summarized in table 1.
Code availability
We do not have any code associated with this systematic review.
References
Zhou, J. et al. Global burden of lung cancer in 2022 and projections to 2050: Incidence and mortality estimates from GLOBOCAN. Cancer Epidemiol. 93, 102693 (2024).
Institute, N. C. Cancer Stat Facts: Lung and Bronchus Cancer, https://seer.cancer.gov/statfacts/html/lungb.html (2021).
American Cancer Society, A. Lung Cancer Statistics, https://www.cancer.org/cancer/types/lung-cancer/about/key-statistics.html?utm_source=chatgpt.com (2025).
Centers for Disease Control and Prevention, C. Treatment of lung cancer, https://www.cdc.gov/lung-cancer/treatment/index.html#:~:text=Treatment%20options&text=it%20has%20spread.-,People%20with%20non%2Dsmall%20cell%20lung%20cancer%20can%20be%20treated,with%20radiation%20therapy%20and%20chemotherapy. (2022).
Society, A. C. Radiation Therapy Side Effects, https://www.cancer.org/cancer/managing-cancer/treatment-types/radiation/effects-on-different-parts-of-body.html (2022).
Polanski, J., Jankowska-Polanska, B., Rosinczuk, J., Chabowski, M. & Szymanska-Chabowska, A. Quality of life of patients with lung cancer. OncoTargets and therapy, 1023-1028 (2016).
Society, A. C. Signs and Symptoms of Lung Cancer, https://www.cancer.org/cancer/types/lung-cancer/detection-diagnosis-staging/signs-symptoms.html (2022).
Hong, Y. A., Hossain, M. M. & Chou, W. S. Digital interventions to facilitate patient-provider communication in cancer care: A systematic review. Psychooncology 29, 591–603 (2020).
Samadbeik, M., Garavand, A., Aslani, N., Sajedimehr, N. & Fatehi, F. Mobile health interventions for cancer patient education: a scoping review. International Journal of Medical Informatics, 105214 (2023).
van Deursen, L. et al. eHealth interventions for Dutch cancer care: systematic review using the triple aim lens. JMIR cancer 8, e37093 (2022).
Greer, J. A. et al. Telehealth vs In-Person Early Palliative Care for Patients With Advanced Lung Cancer: A Multisite Randomized Clinical Trial. JAMA (2024).
LI, M. et al. The Efficacy of Internet-based Intervention on Quality of Life for Patients with Chronic Post-surgical Pain. Iran. J. Public Health 45, 1604–1609 (2016).
Rose, P., Quail, H., McPhelim, J. & Simpson, M. Experiences and outcomes of lung cancer patients using electronic assessments. Cancer Nurs. Pract. 16, 26–30 (2017).
Schneider, S. M. & Hood, L. E. Virtual Reality: A Distraction Intervention for Chemotherapy. Oncol. Nurs. forum 34, 39–46 (2007).
Mkanta, W. N., Chumbler, N. R., Richardson, L. C. & Kobb, R. F. Age-Related Differences in Quality of Life in Cancer Patients: A Pilot Study of a Cancer Care Coordination/Home-Telehealth Program. Cancer Nurs. 30, 434 (2007).
Hopmans, W. et al. Communicating cancer treatment information using the Web: utilizing the patient’s perspective in website development. BMC Med. Inform. Decis. Mak. 14, 116 (2014).
Schook, R. M. et al. Why Do Patients and Caregivers Seek Answers From the Internet and Online Lung Specialists? A Qualitative Study. J. Med. Internet Res. 16, e2842 (2014).
Denis, F. et al. Randomized Trial Comparing a Web-Mediated Follow-up With Routine Surveillance in Lung Cancer Patients. JNCI: J. Natl Cancer Inst. 109, djx029 (2017).
Denis, F. et al. Improving Survival in Patients Treated for a Lung Cancer Using Self-Evaluated Symptoms Reported Through a Web Application. Am. J. Clin. Oncol. 40, 464 (2017).
Groen, W. G. et al. Supporting Lung Cancer Patients With an Interactive Patient Portal: Feasibility Study. JMIR Cancer 3, e7443 (2017).
Mooney, K. H. et al. Automated home monitoring and management of patient-reported symptoms during chemotherapy: results of the symptom care at home RCT. Cancer Med. 6, 537–546 (2017).
Tang, F. W. K. et al. A feasibility study on using tablet personal computers for self-reported symptom assessment in newly diagnosed lung cancer patients. Int. J. Nurs. Pract. 24, e12658 (2018).
Park, S. et al. Mobile Phone App–Based Pulmonary Rehabilitation for Chemotherapy-Treated Patients With Advanced Lung Cancer: Pilot Study. JMIR mHealth uHealth 7, e11094 (2019).
Lafaro, K. J. et al. Pilot study of a telehealth perioperative physical activity intervention for older adults with cancer and their caregivers. Supportive Care Cancer 28, 3867–3876 (2020).
Mouillet, G. et al. Feasibility of health-related quality of life (HRQoL) assessment for cancer patients using electronic patient-reported outcome (ePRO) in daily clinical practice. Qual. Life Res. 30, 3255–3266 (2021).
Nimgaonkar, V. et al. Impact of telemedicine adoption on accessibility and time to treatment in patients with thoracic malignancies during the COVID-19 pandemic. BMC Cancer 21, 1094 (2021).
Misplon, S., Marneffe, W., Himpe, U., Hellings, J. & Demedts, I. Evaluation of the implementation of Value-Based Healthcare with a weekly digital follow-up of lung cancer patients in clinical practice. Eur. J. Cancer Care 31, e13653 (2022).
Charles, C. et al. Delivering adapted physical activity by videoconference to patients with fatigue under immune checkpoint inhibitors: Lessons learned from the PACTIMe-FEAS feasibility study. J. Telemed. Telecare 29, 716–724 (2023).
Ha, D. M. et al. Telemedicine-based inspiratory muscle training and walking promotion with lung cancer survivors following curative intent therapy: a parallel-group pilot randomized trial. Supportive Care Cancer 31, 546 (2023).
Mooney, K. et al. Technology-Assisted mHealth Caregiver Support to Manage Cancer Patient Symptoms: A Randomized Controlled Trial. J. Pain. Symptom Manag. 66, 33–43 (2023).
Arriola, E. et al. Feasibility and User Experience of Digital Patient Monitoring for Real-World Patients With Lung or Breast Cancer. Oncologist 29, e561–e569 (2024).
Asensio-Cuesta, S. et al. Testing Lung Cancer Patients’ and Oncologists’ Experience with the Lalaby App for Monitoring the Quality of Life through Mobile Sensors and Integrated Questionnaires. Int. J. Human–Computer Interact. 40, 640–650 (2024).
Loy, M. H., Prisco, L. & Parikh, C. Implementation of Virtual Integrative Oncology Shared Medical Appointment Series (VIOSMAS) Within Mixed Diagnosis Population. Integr. Cancer Therapies 23, 15347354231223969 (2024).
Kluetz, P. G., O’Connor, D. J. & Soltys, K. Incorporating the patient experience into regulatory decision making in the USA, Europe, and Canada. Lancet Oncol. 19, e267–e274 (2018).
Balitsky, A. K. et al. Patient-reported outcome measures in cancer care: an updated systematic review and meta-analysis. JAMA Netw. Open 7, e2424793 (2024).
Yang, L. Y., Manhas, D. S., Howard, A. F. & Olson, R. Patient-reported outcome use in oncology: a systematic review of the impact on patient-clinician communication. Supportive Care Cancer 26, 41–60 (2018).
Reck, M. et al. Pembrolizumab versus chemotherapy for PD-L1–positive non–small-cell lung cancer. N. Engl. J. Med. 375, 1823–1833 (2016).
Solomon, B. J. et al. First-line crizotinib versus chemotherapy in ALK-positive lung cancer. N. Engl. J. Med. 371, 2167–2177 (2014).
Society, C. C. Immunotherapy drugs used to treat small cell lung cancer, https://cancer.ca/en/cancer-information/cancer-types/lung/treatment/immunotherapy#:~:text=Immunotherapy%20is%20not%20used%20for,Side%20effects (2020).
Araghi, M. et al. Recent advances in non-small cell lung cancer targeted therapy; an update review. Cancer Cell Int. 23, 162 (2023).
Carnio, S., Di Stefano, R. F. & Novello, S. Fatigue in lung cancer patients: symptom burden and management of challenges. Lung Cancer: Targets and Therapy. 73-82 (2016).
Morrison, E. J. et al. Emotional problems, quality of life, and symptom burden in patients with lung cancer. Clin. lung cancer 18, 497–503 (2017).
Li, J. et al. Communication Needs of Cancer Patients and/or Caregivers: A Critical Literature Review. J. Oncol. 2020, 7432849 (2020).
ElKefi, S. & Asan, O. How technology impacts communication between cancer patients and their health care providers: a systematic literature review. Int. J. Med. Inform. 149, 104430 (2021).
Reyna, V. F., Nelson, W. L., Han, P. K. & Pignone, M. P. Decision making and cancer. Am. Psychol. 70, 105–118 (2015).
Joseph-Williams, N., Elwyn, G. & Edwards, A. Knowledge is not power for patients: a systematic review and thematic synthesis of patient-reported barriers and facilitators to shared decision making. Patient Educ. counseling 94, 291–309 (2014).
Lazarus, R. S. & Folkman, S. Stress, appraisal, and coping. (Springer publishing company, 1984).
Mooney, A., Beale, N. & Fried-Oken, M. in Seminars in Speech and Language. 257-269 (Thieme Medical Publishers).
Elkefi, S., Blecker, S. & Bitan, Y. Health Information Technology Supporting Adherence Memory Disorder Patients: A Systematic Literature Review. Appl. Clin. Inform. 15, 085–100 (2024).
Shiraz, F., Rahtz, E., Bhui, K., Hutchison, I. & Korszun, A. Quality of life, psychological wellbeing and treatment needs of trauma and head and neck cancer patients. Br. J. Oral. Maxillofac. Surg. 52, 513–517 (2014).
Northouse, L. et al. A tailored web-based psychoeducational intervention for cancer patients and their family caregivers. Cancer Nurs. 37, 321–330 (2014).
Breen, S. et al. The Patient Remote Intervention and Symptom Management System (PRISMS)–a Telehealth-mediated intervention enabling real-time monitoring of chemotherapy side-effects in patients with haematological malignancies: study protocol for a randomised controlled trial. Trials 16, 1–17 (2015).
Haleem, A., Javaid, M., Singh, R. P. & Suman, R. Telemedicine for healthcare: Capabilities, features, barriers, and applications. Sens Int 2, 100117 (2021).
Mooney, K., Whisenant, M. S. & Beck, S. L. Symptom Care at Home: A Comprehensive and Pragmatic PRO System Approach to Improve Cancer Symptom Care. Med Care 57, S66–s72 (2019).
Basch, E. et al. Symptom monitoring with patient-reported outcomes during routine cancer treatment: a randomized controlled trial. J. Clin. Oncol. 34, 557–565 (2016).
Walden, A., Garvin, L., Smerek, M. & Johnson, C. User-centered design principles in the development of clinical research tools. Clin. trials 17, 703–711 (2020).
Pinto, B. M., Frierson, G. M., Rabin, C., Trunzo, J. J. & Marcus, B. H. Home-based physical activity intervention for breast cancer patients. J. Clin. Oncol. 23, 3577–3587 (2005).
Jeannot, E. et al. Circulating HPV DNA as a marker for early detection of relapse in patients with cervical cancer. Clin. Cancer Res. 27, 5869–5877 (2021).
Denis, F. & Krakowski, I. How should oncologists choose an electronic patient-reported outcome system for remote monitoring of patients with cancer?. J. Med. Internet Res. 23, e30549 (2021).
Ostermann, M., Bagshaw, S. M., Lumlertgul, N. & Wald, R. Indications for and timing of initiation of KRT. Clin. J. Am. Soc. Nephrol. 18, 113–120 (2023).
Frosch, Z. A. et al. Trends in patient volume by hospital type and the association of these trends with time to cancer treatment initiation. JAMA Netw. open 4, e2115675 (2021).
Hofman, A., Zajdel, N., Klekowski, J. & Chabowski, M. Improving social support to increase QoL in lung cancer patients. Cancer Management and Research, 2319–2327 (2021).
Shaffer, K. M. et al. Digital health and telehealth in cancer care: a scoping review of reviews. Lancet Digital Health 5, e316–e327 (2023).
Alfano, C. M. et al. Roadmap for Connecting Cancer Rehabilitation with Survivorship to improve patient outcomes and clinical efficiency. Am. J. Phys. Med. Rehabilitation 103, S10–S15 (2024).
Fareed, N., Swoboda, C. M., Jonnalagadda, P. & Huerta, T. R. Persistent digital divide in health-related internet use among cancer survivors: findings from the Health Information National Trends Survey, 2003–2018. J. Cancer Survivorship 15, 87–98 (2021).
Morris, B. B., Rossi, B. & Fuemmeler, B. The role of digital health technology in rural cancer care delivery: a systematic review. J. Rural Health 38, 493–511 (2022).
Saeed, S. A. & Masters, R. M. Disparities in health care and the digital divide. Curr. psychiatry Rep. 23, 1–6 (2021).
Yao, R. et al. Inequities in health care services caused by the adoption of digital health technologies: scoping review. J. Med. Internet Res. 24, e34144 (2022).
Göttgens, I. & Oertelt-Prigione, S. The application of human-centered design approaches in health research and innovation: a narrative review of current practices. JMIR mHealth uHealth 9, e28102 (2021).
Greer, J. A. et al. Telehealth vs in-person early palliative care for patients with advanced lung cancer: a multisite randomized clinical trial. JAMA 332, 1153–1164 (2024).
Freeman, J. Q. et al. Assessing the Relationship Between Neighborhood Socioeconomic Disadvantage and Telemedicine Use Among Patients With Breast Cancer and Examining Differential Provisions of Oncology Services Between Telehealth and In-Person Visits: Quantitative Study. JMIR cancer 10, e55438 (2024).
Williams, M. T. et al. Compliance with mobile ecological momentary assessment of self-reported health-related behaviors and psychological constructs in adults: systematic review and meta-analysis. J. Med. Internet Res. 23, e17023 (2021).
Dang, J., King, K. M. & Inzlicht, M. Why Are Self-Report and Behavioral Measures Weakly Correlated?. Trends Cogn. Sci. 24, 267–269 (2020).
Simon, B. A. et al. Association between electronic patient symptom reporting with alerts and potentially avoidable urgent care visits after ambulatory cancer surgery. JAMA Surg. 156, 740–746 (2021).
Dai, W. et al. Patient-reported outcome-based symptom management versus usual care after lung cancer surgery: a multicenter randomized controlled trial. J. Clin. Oncol. 40, 988–996 (2022).
Acknowledgements
The project was supported by funds from the Herbert Irving Comprehensive Cancer Center (HICCC) of Columbia under the VELOCITY grant.
Author information
Authors and Affiliations
Contributions
S.E., L.C., S.F., and A.K.M. helped in securing the funding for this project. P.W. and S.E. worked on the data collection and data extraction. S.E., R.S., and P.W. helped in the writing of the initial manuscript. All authors, including G.H. helped edit the final manuscript. All authors have read and approve the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Elkefi, S., Wu, P., Sabra, R. et al. Systematic review on the technology’s role in supporting lung cancer patients in the treatment journey. npj Digit. Med. 8, 516 (2025). https://doi.org/10.1038/s41746-025-01913-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41746-025-01913-7