Abstract
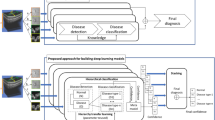
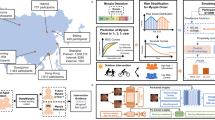
Understanding causal mechanisms in deep learning is essential for clinical adoption, where interpretability and reliability are critical. Most existing AI systems act as black boxes, limiting transparency in medicine. We propose a causal inference framework integrated into neural networks to assess the influence of individual features on predictions. Using a prospective pediatric ophthalmology cohort of over 3000 children with longitudinal follow-up, our method estimates direct and indirect causal effects through intervention. Applied to myopia progression in children, our approach not only achieved good performance but also identified clinically plausible causal pathways. Refutation experiments with multiple falsification strategies confirm the robustness and reliability of causal effects. The approach is model-agnostic and suitable for digital health interventions requiring explainability. By incorporating unit-level causal reasoning into deep learning, this work advances transparent and reliable AI systems aligned with the goals of precision medicine and equitable healthcare.

Similar content being viewed by others
Data availability
The datasets analyzed in the current study are not publicly available due to patient privacy purposes, but are available upon reasonable request to the corresponding author Shi-Ming Li (lishiming81@163.com).
Code availability
The code can be made available upon reasonable request to the corresponding author Xu Yang (pyro_yangxu@bit.edu.cn).
References
Liang, J. Trend and projection of myopia in children and adolescents from 1990 to 2050: a comprehensive systematic review and meta-analysis. Br. J. Ophthalmol. 362, 109 (2025).
Lee, Y., Keel, S. & Yoon, S. Evaluating the effectiveness and scalability of the World Health Organization myopiaed digital intervention: mixed methods study. JMIR Public Health Surveill. 10, e66052 (2024).
Yang, B.-Y. Significance of school greenspaces in preventing childhood myopia. Innovation 5, 100551 (2024).
Morgan, I. G., Ohno-Matsui, K. & Saw, S.-M. Myopia. Lancet 379, 1739–1748 (2012).
Rose, K. A., French, A. N. & Morgan, I. G. Environmental factors and myopia: paradoxes and prospects for prevention. Asia-Pac. J. Ophthalmol. 5, 403–410 (2016).
Dolgin, E. The myopia boom. Nature 519, 276 (2015).
Morgan, I. G., He, M. & Rose, K. A. Epidemic of pathologic myopia: what can laboratory studies and epidemiology tell us?. Retina 37, 989–997 (2017).
Ng, D. S. & Lai, T. Y. Insights into the global epidemic of high myopia and its implications. JAMA Ophthalmol. 140, 123–124 (2022).
Ghorbani Mojarrad, N., Williams, C. & Guggenheim, J. A. A genetic risk score and number of myopic parents independently predict myopia. Ophthalmic Physiol. Opt. 38, 492–502 (2018).
Chua, S. Y. et al. Age of onset of myopia predicts risk of high myopia in later childhood in myopic Singapore children. Ophthalmic Physiol. Opt. 36, 388–394 (2016).
Huang, T. et al. Artificial intelligence for medicine: progress, challenges, and perspectives. Innov. Med 1, 100030 (2023).
Xie, Y. Values and limitations of statistical models. Res. Soc. Stratif. Mobil. 29, 343–349 (2011).
Yang, Y. et al. Computational modeling for medical data: from data collection to knowledge discovery. Innov. Life 2, 100079–1 (2024).
Grebovic, M., Filipovic, L., Katnic, I., Vukotic, M. & Popovic, T. Overcoming limitations of statistical methods with artificial neural networks. In 2022 International Arab Conference on Information Technology (ACIT), 1–6 (IEEE, 2022).
Almeida, J. S. Predictive non-linear modeling of complex data by artificial neural networks. Curr. Opin. Biotechnol. 13, 72–76 (2002).
Patra, J. C., Pal, R. N., Chatterji, B. & Panda, G. Identification of nonlinear dynamic systems using functional link artificial neural networks. IEEE Trans. Syst. Man Cybern. Part b (Cybern.) 29, 254–262 (1999).
Aziz, R., Verma, C. & Srivastava, N. Artificial neural network classification of high dimensional data with novel optimization approach of dimension reduction. Ann. Data Sci. 5, 615–635 (2018).
Aggarwal, C. C. et al. Neural Networks and Deep Learning Vol. 10 (Springer, 2018).
Luo, M. et al. Artificial intelligence for life sciences: a comprehensive guide and future trends. Innov. Life 2, 100105–1 (2024).
He, C., Ma, M. & Wang, P. Extract interpretability-accuracy balanced rules from artificial neural networks: a review. Neurocomputing 387, 346–358 (2020).
Zhang, Y., Tiňo, P., Leonardis, A. & Tang, K. A survey on neural network interpretability. IEEE Trans. Emerg. Top. Comput. Intell. 5, 726–742 (2021).
Fan, F.-L., Xiong, J., Li, M. & Wang, G. On interpretability of artificial neural networks: a survey. IEEE Trans. Radiat. Plasma Med. Sci. 5, 741–760 (2021).
Zhang, Z. et al. Opening the black box of neural networks: methods for interpreting neural network models in clinical applications. Ann. Transl. Med. 6, 216 (2018).
Lundberg, S. M. & Lee, S.-I. A unified approach to interpreting model predictions. Adv. Neural Inf. Process. Syst 30, 4765–4774 (2017).
Cremades, A., Hoyas, S. & Vinuesa, R. Additive-feature-attribution methods: a review on explainable artificial intelligence for fluid dynamics and heat transfer. Int. J. Heat Fluid Flow 112, 109662 (2025).
Moraffah, R., Karami, M., Guo, R., Raglin, A. & Liu, H. Causal interpretability for machine learning-problems, methods and evaluation. ACM SIGKDD Explor. Newsl. 22, 18–33 (2020).
Ahmad, O., Béreux, N., Baret, L., Hashemi, V. & Lecue, F. Causal analysis for robust interpretability of neural networks. In Proc. of the IEEE/CVF Winter Conference on Applications of Computer Vision 4685–4694 (IEEE, 2024).
Xu, G., Duong, T. D., Li, Q., Liu, S. & Wang, X. Causality learning: A new perspective for interpretable machine learning. arXiv preprint arXiv:2006.16789 (2020).
Pearl, J. Causality (Cambridge University Press, 2009).
Spirtes, P., Glymour, C. N. & Scheines, R.Causation, Prediction, and Search (MIT Press, 2000).
Ramsey, J. D. et al. Tetrad–a toolbox for causal discovery. In Proc. 8th International Workshop on Climate Informatics (eds Ebert-Uphoff, I., Gagne II, D. J. & Monteleoni. C.) 1–4 (National Center for Atmospheric Research, 2018).
Baksh, J. et al. Myopia is an ischemic eye condition: a review from the perspective of choroidal blood flow. J. Clin. Med. 13, 2777 (2024).
Li, S. et al. Effects of physical exercise on macular vessel density and choroidal thickness in children. Sci. Rep. 11, 2015 (2021).
Yang, Y. S. & Koh, J. W. Choroidal blood flow change in eyes with high myopia. Korean J. Ophthalmol. 29, 309 (2015).
SHIH, Y.-F. et al. Ocular pulse amplitude in myopia. J. Ocul. Pharmacol. Ther. 7, 83–87 (1991).
Zhang, D. et al. Correlation analysis of myopia and dietary factors among primary and secondary school students in Shenyang, China. Sci. Rep. 14, 20619 (2024).
Hao, Z. et al. Association between sugar-sweetened beverages intake and myopia: results from the National Health and Nutrition Examination Survey 2001–2008. Ophthal. Epidemiol. 1–8 https://doi.org/10.1080/09286586.2025.2548001 (2025).
Kim, J.-M. & Choi, Y. J. Association between dietary nutrient intake and prevalence of myopia in Korean adolescents: evidence from the 7th Korea National Health and Nutrition Examination Survey. Front. Pediatr. 11, 1285465 (2024).
Mrugacz, M. et al. Interdependence of nutrition, physical activity, and myopia. Nutrients 16, 3331 (2024).
Dutheil, F. et al. Myopia and near work: a systematic review and meta-analysis. Int. J. Environ. Res. Public Health 20, 875 (2023).
Huang, H.-M., Chang, D. S.-T. & Wu, P.-C. The association between near work activities and myopia in children—a systematic review and meta-analysis. PLoS ONE 10, e0140419 (2015).
Lingham, G., Mackey, D. A., Lucas, R. & Yazar, S. How does spending time outdoors protect against myopia? A review. Br. J. Ophthalmol. 104, 593–599 (2020).
Mei, Z. et al. Efficacy of outdoor interventions for myopia in children and adolescents: a systematic review and meta-analysis of randomized controlled trials. Front. Public Health 12, 1452567 (2024).
Philipp, D. et al. The relationship between myopia and near work, time outdoors and socioeconomic status in children and adolescents. BMC Public Health 22, 2058 (2022).
He, M. et al. Effect of time spent outdoors at school on the development of myopia among children in China: a randomized clinical trial. JAMA. 314, 1142–1148 (2015).
Kearney, S., Strang, N. C., Cagnolati, B. & Gray, L. S. Change in body height, axial length and refractive status over a four-year period in caucasian children and young adults. J. Optom. 13, 128–136 (2020).
Tao, L. et al. Correlation between increase of axial length and height growth in Chinese school-age children. Front. Public Health 9, 817882 (2022).
Kuoliene, K., Danieliene, E. & Tutkuviene, J. Eye morphometry, body size, and flexibility parameters in myopic adolescents. Sci. Rep. 14, 6787 (2024).
Zhang, J. et al. The association between physical stature and myopia in elementary and junior high school graduates in Chongqing, China. Front. Med. 12, 1530960 (2025).
Wang, D., Zhao, C., Huang, S., Huang, W. & He, M. Longitudinal relationship between axial length and height in Chinese children: Guangzhou twin eye study. Eye Sci. 30, 12 (2015).
Wang, D., Ding, X., Liu, B., Zhang, J. & He, M. Longitudinal changes of axial length and height are associated and concomitant in children. Investig. Ophthalmol. Vis. Sci. 52, 7949–7953 (2011).
Lu, T. L. et al. Axial length and associated factors in children: the Shandong children eye study. Ophthalmologica 235, 78–86 (2016).
Alrasheed, S. H. & Alghamdi, W. Systematic review and meta-analysis of the prevalence of myopia among school-age children in the Eastern Mediterranean region. East. Mediterr. Health J.30, (2024).
Zhao, L. et al. Prevalence and risk factors of myopia among children and adolescents in Hangzhou. Sci. Rep. 14, 24615 (2024).
Rudnicka, A. R. et al. Global variations and time trends in the prevalence of childhood myopia, a systematic review and quantitative meta-analysis: implications for aetiology and early prevention. Br. J. Ophthalmol. 100, 882–890 (2016).
Groot, A. L., Lissenberg-Witte, B. I., van Rijn, L. J. & Hartong, D. T. Meta-analysis of ocular axial length in newborns and infants up to 3 years of age. Surv. Ophthalmol. 67, 342–352 (2022).
Terasaki, H. et al. Sex differences in rate of axial elongation and ocular biometrics in elementary school students. Clin. Ophthalmol 15, 4297–4302 (2021).
Zadnik, K. et al. Ocular component data in schoolchildren as a function of age and gender. Optom. Vis. Sci. 80, 226–236 (2003).
He, X. et al. Normative data and percentile curves for axial length and axial length/corneal curvature in Chinese children and adolescents aged 4–18 years. Br. J. Ophthalmol. 107, 167–175 (2023).
Hashemi, H., Fotouhi, A. & Mohammad, K. The age-and gender-specific prevalences of refractive errors in Tehran: the Tehran eye study. Ophthalmic Epidemiol. 11, 213–225 (2004).
Lee, D. C., Lee, S. Y. & Kim, Y. C. An epidemiological study of the risk factors associated with myopia in young adult men in Korea. Sci. Rep. 8, 511 (2018).
Pandian, A. et al. Accommodative facility in eyes with and without myopia. Investig. Ophthalmol. Vis. Sci. 47, 4725–4731 (2006).
Scheiman, M. et al. Longitudinal changes in corneal curvature and its relationship to axial length in the correction of myopia evaluation trial (COMET) cohort. J. Optom. 9, 13–21 (2016).
Jiang, L. et al. Associations between corneal curvature and other anterior segment biometrics in young myopic adults. Sci. Rep. 14, 8305 (2024).
Carney, L. G., Mainstone, J. C. & Henderson, B. A. Corneal topography and myopia. A cross-sectional study. Investig. Ophthalmol. Vis. Sci. 38, 311–320 (1997).
Fan, Q. et al. Genome-wide association meta-analysis of corneal curvature identifies novel loci and shared genetic influences across axial length and refractive error. Commun. Biol. 3, 133 (2020).
Wang, Y.-M. et al. Myopia genetics and heredity. Children 9, 382 (2022).
Jiang, X. et al. Association of parental myopia with higher risk of myopia among multiethnic children before school age. JAMA Ophthalmol. 138, 501–509 (2020).
Martínez-Albert, N., Bueno-Gimeno, I. & Gené-Sampedro, A. Risk factors for myopia: a review. J. Clin. Med. 12, 6062 (2023).
Koomson, N. Y. et al. Relationship between peripheral refraction, axial lengths and parental myopia of young adult myopes. J. Optom. 15, 122–128 (2022).
Kurtz, D. et al. Role of parental myopia in the progression of myopia and its interaction with treatment in COMET children. Investig. Ophthalmol. Vis. Sci. 48, 562–570 (2007).
Ishikuro, M. et al. Parental axial lengths and prenatal conditions related to child axial length: the TMM birthree cohort study. AJO Int. 2, 100088 (2025).
Mutti, D. O., Mitchell, G. L., Moeschberger, M. L., Jones, L. A. & Zadnik, K. Parental myopia, near work, school achievement, and children’s refractive error. Investig. Ophthalmol. Vis. Sci. 43, 3633–3640 (2002).
Hui, J., Peck, L. & Howland, H. C. Correlations between familial refractive error and children’s non-cycloplegic refractions. Vis. Res. 35, 1353–1358 (1995).
Xiang, F., He, M. & Morgan, I. G. The impact of parental myopia on myopia in Chinese children: population-based evidence. Optom. Vis. Sci. 89, 1487–1496 (2012).
Ma, Y. et al. Effect of parental myopia on change in refraction in Shanghai preschoolers: a 1-year prospective study. Front. Pediatr. 10, 864233 (2022).
Tang, S. M. et al. Independent influence of parental myopia on childhood myopia in a dose-related manner in 2,055 trios: the Hong Kong Children Eye Study. Am. J. Ophthalmol. 218, 199–207 (2020).
Onyeahiri, C. Approach to cycloplegic refraction. Can. J. Optom. 86, 11–30 (2024).
Hinkley, S., Iverson-Hill, S. & Haack, L. The correlation between accommodative lag and refractive error in minors under 18. Austin J. Clin. Ophthalmol. 1, 1–5 (2014).
Lim, L. S. et al. Dietary factors, myopia, and axial dimensions in children. Ophthalmology 117, 993–997 (2010).
Xue, C. C. et al. Omega-3 polyunsaturated fatty acids as a protective factor for myopia. Am. J. Ophthalmol. 268, 368–377 (2024).
Yin, C. et al. Dietary patterns and associations with myopia in Chinese children. Nutrients 15, 1946 (2023).
Jin, G. et al. Corneal biometric features and their association with axial length in high myopia. Am. J. Ophthalmol. 238, 45–51 (2022).
Merriam, J. & Zheng, L. The relationship of corneal curvature and axial length in adults. Investig. Ophthalmol. Vis. Sci. 46, 864–864 (2005).
Aljuhani, G., Alharbi, M., Alsaidi, R. & Alharbi, A. Axial length and keratometry characteristics of patients undergoing cataract surgery in Saudi Arabia. J. Med. Life 17, 620 (2024).
Li, S.-M. et al. Corneal power, anterior segment length and lens power in 14-year-old Chinese children: the Anyang Childhood Eye Study. Sci. Rep. 6, 20243 (2016).
Tideman, J. W. L., Polling, J. R., Jaddoe, V. W., Vingerling, J. R. & Klaver, C. C. Environmental risk factors can reduce axial length elongation and myopia incidence in 6-to 9-year-old children. Ophthalmology 126, 127–136 (2019).
He, X. et al. Axial length/corneal radius ratio: association with refractive state and role on myopia detection combined with visual acuity in Chinese schoolchildren. PLoS ONE 10, e0111766 (2015).
Grosvenor, T. & Scott, R. Role of the axial length/corneal radius ratio in determining the refractive state of the eye. Optom. Vis. Sci. 71, 573–579 (1994).
Angie, E., Amra, A. A. & Sari, M. D. Correlation between axial length and amplitude of accommodation in myopia patients. J. Public Health Pharm. 4, 300–317 (2024).
Hughes, R. P., Read, S. A., Collins, M. J. & Vincent, S. J. Changes in ocular biometry during short-term accommodation in children. Ophthalmic Physiol. Opt. 40, 584–594 (2020).
Woodman, E. C., Read, S. A. & Collins, M. J. Axial length and choroidal thickness changes accompanying prolonged accommodation in myopes and emmetropes. Vis. Res. 72, 34–41 (2012).
Read, S. A., Collins, M. J., Woodman, E. C. & Cheong, S.-H. Axial length changes during accommodation in myopes and emmetropes. Optom. Vis. Sci. 87, 656–662 (2010).
Flitcroft, D. I. et al. Imi–defining and classifying myopia: a proposed set of standards for clinical and epidemiologic studies. Investig. Ophthalmol. Vis. Sci. 60, M20–M30 (2019).
Mutti, D. O. et al. Refractive error, axial length, and relative peripheral refractive error before and after the onset of myopia. Investig. Ophthalmol. Vis. Sci. 48, 2510–2519 (2007).
Meng, W., Butterworth, J., Malecaze, F. & Calvas, P. Axial length of myopia: a review of current research. Ophthalmologica 225, 127–134 (2011).
Tharwat, E. et al. Effect of cycloplegia on the refractive status of children. Afr. Vis. Eye Health 83, 916 (2024).
Fotedar, R. et al. Necessity of cycloplegia for assessing refractive error in 12-year-old children: a population-based study. Am. J. Ophthalmol. 144, 307–309 (2007).
Khan, H. A. et al. Comparison between cycloplegic and noncycloplegic refraction in young adult myopes. Optom. Vis. Sci. 101, 470–476 (2024).
Sharma, A. & Kiciman, E. Dowhy: An end-to-end library for causal inference. arXiv preprint arXiv:2011.04216 (2020).
Li, S.-M. et al. Effect of text messaging parents of school-aged children on outdoor time to control myopia: a randomized clinical trial. JAMA Pediatr. 176, 1077–1083 (2022).
Doshi-Velez, F. & Kim, B. Towards a rigorous science of interpretable machine learning. arXiv preprint arXiv:1702.08608 (2017).
Sundararajan, M., Taly, A. & Yan, Q. Axiomatic attribution for deep networks. In International Conference on Machine Learning (eds. Precup D. & Whye Teh Y.) 3319–3328 (PMLR, 2017).
Adebayo, J. et al. Sanity checks for saliency maps. In Advances in Neural Information Processing Systems (ed. Bengio, S., Wallach, H., Larochelle, H., Grauman, K., Cesa-Bianchi, N. & Garnett R.) Vol. 31 (Curran Associates, Inc., 2018).
Samek, W., Wiegand, T. & Müller, K.-R. Explainable artificial intelligence: understanding, visualizing and interpreting deep learning models. ITU Journal: ICT Discoveries 1, 39–48 (2018).
Alvarez-Melis, D. & Jaakkola, T. S. On the robustness of interpretability methods. arXiv preprint arXiv:1806.08049 (2018).
Salih, A. M. et al. A perspective on explainable artificial intelligence methods: Shap and lime. Adv. Intell. Syst. 7, 2400304 (2025).
Kelodjou, G. et al. Shaping up shap: enhancing stability through layer-wise neighbor selection. In Proc. of the AAAI Conference on Artificial Intelligence (ed. Michael W., Jennifer N. & Iryna G.) Vol. 38, 13094–13103 (AAAI Press, 2024).
Li, S.-M. et al. Design, methodology and baseline data of a school-based cohort study in central China: the Anyang Childhood Eye Study. Ophthalmic Epidemiol. 20, 348–359 (2013).
Pearl, J. & Mackenzie, D. The Book of Why: The New Science of Cause and Effect (Basic Books, 2018).
Meek, C. Causal inference and causal explanation with background knowledge. In Proceedings of the Eleventh Conference on Uncertainty in Artificial Intelligence (UAI'95), 403–410 (Morgan Kaufmann, 1995).
Andrews, B., Ramsey, J. & Cooper, G. F. Learning high-dimensional directed acyclic graphs with mixed data-types. In The 2019 ACM SIGKDD Workshop on Causal Discovery, (ed. Zhang, K. Huang, B., and Glymour, C.)4–21 (PMLR, 2019).
Venter, J. H. On estimation of the mode. Ann. Math. Stat 38, 1446–1455 (1967).
Keith. Battocchi., et al. EconML: A Python Package for ML-Based Heterogeneous Treatment Effects Estimation, Version 0.x https://github.com/py-why/EconML (2019).
Acknowledgements
This research was funded by National Key Research and Development Program of China 2025YFE0112100, the Key Laboratory of Epidemiology of Major Diseases (Peking University), Ministry of Education (Grant No. 2025102), the National Outstanding Young Physician Project, the Beijing High-Level Innovation and Entrepreneurship Talent Support Program Leading Talent Projects (G202512030), the National Key R&D Program of China (2022YFC3502502), the Fundamental Research Funds for the Central Universities 2025XC11020, the National Natural Science Foundation of China (82471113), the Beijing Natural Science Foundation (L248023), the Excellent Youth Talents Program of Capital Medical University (A2307), the Capital Health Research and Development of special grant (2024-2G-1081), and the Beijing New-star Plan of Science and Technology Cross-cooperation Project (20250484983).
Author information
Authors and Affiliations
Contributions
Conceptualization: X.Y., Z.J., and W.S.; methodology: Z.J. and M.K.; investigation: Z.J., W.Z., W.G., and W.S.; visualization: W.Z. and Z.J.; data collection: H.L., Y.T., and Y.H.; data analysis: N.W. and S.L.; funding acquisition: X.Y., C.Y., and S.L.; project administration: X.Y. and W.S.; supervision: X.Y.; writing—original draft: Z.J., M.K., and W.Z.; writing—review and editing: all authors.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Jin, Z., Kang, M., Zhao, W. et al. Robust and interpretable unit level causal inference in neural networks for pediatric myopia. npj Digit. Med. (2026). https://doi.org/10.1038/s41746-026-02442-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41746-026-02442-7