Abstract
Hematologic malignancies cause significant morbidity/mortality in both children and young adults (CYAs) as well as older adults (OAs). Yet their biological underpinnings remain inadequately understood. Here, we analyzed clinical and genomic disparities between CYAs and OAs in various hematologic malignancies. We found substantial differences in clinical features such as patient sex, ethnicity, metastasis rates, and tumor subtypes. Genomically, most CYA hematologic malignancies indicated lower mutational burden. Subsequently, we identified differentially mutated genes (DMGs) with varying mutation rates between CYAs and OAs, noting fewer mutations in CYAs for most genes such as TP53, TET2, and DNMT3A. In contrast, several DMGs (i.e., NRAS, KRAS, SMARCA4, ID3, PTPN11, WT1, and KIT) were overrepresented in CYAs. We further investigated human protein interacting partners of these identified DMGs that were highly mutated in CYAs/OAs, respectively, and found significant differences in network topological and functional roles. Notably, CYA malignancies demonstrated extensive copy number alterations (CNAs) and more driver gene fusions. In particular, four CNA differential genes (i.e., ARID1B, MYB, TP53, and ESR1) were overrepresented as amplifications and deletions in CYAs and OAs, respectively. Ultimately, we demonstrated a landscape comparative view of clinically actionable genetic events in CYAs and OAs, providing clues for age-related personalized treatment.
Similar content being viewed by others
Introduction
Hematologic malignancies are a type of cancer that mainly originate from the hematopoietic system and affect both children and adults. In 2022, hematologic malignancies have led to over 1.3 million diagnoses and caused 700 thousand deaths worldwide, ranking fifth and fourth among all cancers in terms of prevalence and mortality, respectively1. Although great treatment efforts have been made2,3,4,5, the current therapeutic effects of such highly heterogeneous cancers are still limited. The prognosis of different hematologic tumor types at different age stages varies as a consequence of different treatment strategies6,7. For instance, current disease risk stratification and intensive chemotherapy protocols substantially improve the therapeutic outcomes of children and young adults (CYAs) with acute lymphoblastic leukemia (ALL), while the outcomes for older adults (OAs) remain poor8. Therefore, the characterization and comparison of clinical and genetic features of patients with hematologic malignancies across different age groups (e.g., CYAs and OAs) is critical for the identification of novel therapeutic targets and the development of personalized treatment strategies. However, previous studies predominantly focused on clinical and genetic characterization of a certain tumor subtype of all patients without considering different age bins or in one age group only9,10.
Although the detection of morphology plays an important role in the clinical diagnostic and prognostic assessment of patients with hematologic malignancies, genomic profiling has increasingly become essential for accurate diagnosis, risk assessment, and treatment decision-making11,12,13,14,15. Recent advances in next-generation sequencing technologies have enhanced our ability to detect mutations and identify potential targeted therapies using gene panels, augmenting traditional cytogenetic and sequencing approaches16,17. These genomic sequencing techniques are not only employed to detect somatically acquired gene mutations but also to identify germline gene mutations that are associated with inherited predisposition to hematologic malignancies. The International Consensus Classification of various hematologic malignancies extensively utilizes genomic data, underscoring its importance18,19. Taken together, a systematic comparison of genomic profiles of CYA and OA hematologic malignancies may provide new insights into age-related mechanisms of carcinogenesis and progression.
Here, we use cancer gene panel sequencing data from AACR GENIE to explore the clinical and genetic distinctions between CYAs and OAs in hematologic malignancies. We compared their sex, ethnicity, and metastasis rates at the levels of various hematologic tumor types/subtypes. As for genomic feature characterization, we calculated and compared their tumor mutational burden (TMB), gene mutation rates, copy number alterations (CNAs), and gene fusions. By integrating human protein interactions and functional gene sets, we analyzed the network topologies and functional implications of our identified differentially mutated genes (DMGs) of CYAs and OAs. Finally, we investigated the clinical actionability of these genetic variations, providing a comprehensive landscape view of their therapeutic implications.
Results
Clinical disparities in CYAs and OAs with hematologic tumors
Hematologic tumors constituted 10.05% (n = 14,893) of the total cases in the GENIE cohort (v13.1) where we excluded cases lacking precise age information (i.e., ‘unknown’) or comprehensive follow-up details. In particular, our refined cohort comprised 6684 hematologic tumor cases including 1047 CYAs and 5637 OAs. We categorized these cases into four primary types of hematologic tumors [i.e., myeloid tumor, lymphoid tumor, mixed phenotype acute leukemia (MPAL), and plasma cell (PC) tumor], covering 28 distinct subtypes (Fig. 1a, Supplementary Tables 1 and 2).
a Number distribution, (b) sex ratio distribution and (c) metastasis ratio distribution of CYAs and OAs in four hematologic tumor types covering 28 hematologic tumor subtypes. Circle size corresponds to case counts of the specific hematologic tumor subtypes. Circle color corresponds to the specific hematologic tumor types. d Comparison of race and ethnicity between hematologic tumor CYA and OA cases. Color depth denotes the average likelihood ratio. Red, >1; blue, <1; gray, NA. Superscript stars indicate statistically significant differences (FDR < 0.05).
Comparing bins of CYAs and OAs, we generally found a significant overrepresentation of myeloid tumors (CYA/OA percentage, 49.67% vs. 67.15%) and PC tumors in OAs (CYA/OA percentage, 0.67% vs. 3.85%) and lymphoid tumors in CYAs (CYA/OA percentage, 48.90% vs. 28.61%) (two-tailed Fisher’s exact test, FDR < 0.001; Fig. 1a and Supplementary Table 1). As for the 28 hematologic tumor subtypes, OAs were predominant in three myeloid subtypes i.e., acute myeloid leukemia (AML), myelodysplastic syndrome (MDS), and myeloproliferative neoplasms (MPN) (Fig. 1a, reference background: all tumors), whereas CYAs were more prevalent in two lymphoid subtypes i.e., T lymphocytic leukemia (TLL) and B lymphocytic leukemia (BLL), indicating an age-related distribution trend (Fig. 1a). In particular, we identified 14 subtypes with significant distribution differences, where six subtypes including AML, chronic myelocytic leukemia (CML), Mastocytosis, BLL, TLL, and Hodgkin lymphoma (HL) were overrepresented in CYAs (Supplementary Table 2, reference background: corresponding tumor types).
In terms of sex distribution of CYA and OA hematologic tumor cases, we found a significant increase in females in CYA myeloid tumors (49.81% vs. 40.69%; FDR < 0.05; Fig. 1b and Supplementary Table 3). However, no significant sex disparities were observed across the other three hematologic tumor types when we compared CYAs and OAs. When analyzing hematologic tumor subtypes in detail, we observed no significant sex ratio distribution differences between CYAs and OAs (Supplementary Table 4). Such findings suggest that sex is an important etiological factor in the broad category of myeloid tumors but appears to be insignificant in hematologic tumor subtypes.
The incidence of metastatic disease also varied significantly between the CYA and OA groups in the context of myeloid tumors (1.92% vs. 0.45%; FDR < 0.05; Fig. 1c and Supplementary Table 5). Focusing on the 28 subtypes of hematologic tumors, only AML exhibited a higher rate of metastatic cases among CYAs compared to OAs (2.17% vs. 0.29%; FDR < 0.05; Supplementary Table 6), suggesting CYAs with AML potentially ran the risk of delayed diagnosis and suffered from elevated metastatic rates compared to other hematologic tumors.
Furthermore, our investigation of the effect of race and ethnicity on the four broad types and 28 subtypes of hematologic tumors revealed notable differences. In particular, we observed a significant increase in non-Spanish Black/Asian and Spanish CYAs diagnosed with myeloid tumors, and the corresponding rise in non-Spanish White OAs with the same tumor type (FDR < 0.05; Supplementary Table 7). Lymphoid tumors showed a significant increase among non-Spanish Asian CYAs, while non-Spanish White OAs exhibited a decreasing trend (FDR < 0.05; Supplementary Table 7). When examining specific subtypes, two myeloid subtypes (i.e., AML and MDS) showed significant ethnic and racial disparities in the CYA and OA groups (Fig. 1d and Supplementary Table 8). Specifically, we observed a significant predominance of non-Spanish Black/Asian and Spanish patients with AML in CYAs and a significant increase of non-Spanish White patients with MDS in OAs (FDR < 0.05; Fig. 1d and Supplementary Table 8). This nuanced analysis reaffirms and extends previous findings, emphasizing ethnic and racial variations not just at the level of broad tumor types but also within specific hematologic tumor subtypes.
Multiple influencing factors of genomic differences between CYAs and OAs in hematologic tumors
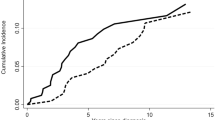
To elucidate genomic disparities between CYAs and OAs across various hematologic malignancies, we initially assessed the TMB across four broad types of hematologic tumors, subsequently narrowing our focus to 28 specific subtypes. Recognizing the limitations of gene panels with insufficient coverage to infer TMB20,21,22,23,24, we excluded cases that were sequenced using panels, covering less than 0.9 Mb of exon regions, thereby refining our dataset to 3215 cases for TMB analysis. Our findings revealed pronounced differences in TMB between CYAs and OAs, particularly notable in lymphoid tumors, where the median TMB in OAs was 1.35-fold higher than in CYAs (FDR < 0.001, Wilcoxon rank sum test; Fig. 2a and Supplementary Table 9).
a Tumor mutational burden (TMB) (i.e., the number of coding mutations per megabase) of CYAs and OAs in various hematologic tumor types/subtypes. Tumor types/subtypes are ordered by the median TMB of corresponding tumor cases. Tumor types/subtypes show (non-)significant differences between CYAs and OAs (****FDR < 0.0001; *FDR < 0.05; ns FDR > 0.05). b Genes with significant differences in mutation rates comparing CYAs and OAs in hematologic tumor types. The bar length in the left panel represents the absolute value of the difference between CYA and OA mutation rates. Pink indicates higher mutation rates in CYAs, and blue indicates higher mutation rates in OAs. Bar lengths in the right panel represent the negative logarithm of FDR of mutation rate difference between CYAs and OAs (FDR < 0.05). Greater bar lengths indicate more significant differences. c Genes with significant differences in mutation rates between CYAs and OAs in hematologic tumor subtypes. Circle size represents the absolute value of the difference between CYA and OA mutation rates. Pink indicates higher mutation rates in CYAs, and blue indicates higher mutation rates in OAs. The transparency of the circle indicates the negative logarithm of FDR of mutation rate difference between CYAs and OAs (FDR < 0.05). Darker colors indicate more significant differences.
Delving deeper into the subtype-specific analysis, we observed TMB differences between CYAs and OAs on the subtype level, highlighting age-related nuances of genomic profiles. Specifically, we found substantial differences in two lymphoid subtypes, i.e., unclassified mature B-cell neoplasms (MBN) and follicular lymphoma (FL). CYAs with MBN exhibited significantly higher TMBs compared to OAs (average of TMB, 9.214 vs. 3.905), whereas in FL, TMB was notably lower in CYAs (average of TMB, 3.731 vs. 5.945) (FDR < 0.05; Fig. 2a and Supplementary Table 10), underscoring the unique age-related dynamics within these subtypes. Such observations suggest that the mutational burden in MBN and FL is particularly sensitive to age-related factors. While the median TMB of AML in OAs was 2.74-fold higher than in CYAs (FDR < 0.05; Fig. 2a and Supplementary Table 10), we did not find this trend in other myeloid tumors, indicating that the influence of age on genomic mutations may vary significantly across different types and subtypes of hematologic malignancies. This nuanced understanding highlights the complexity of cancer genomics across different age groups and emphasizes the need for age-specific considerations in the diagnosis and treatment of hematologic malignancies.
Mutation rate differences between CYAs and OAs in hematologic tumors
We next compared mutation rates of hematologic tumor genes in CYAs and OAs. The gene panels of these cases in GENIE were designed by different centers and institutions. To ensure a comprehensive analysis, we amalgamated all available gene panels, thereby maximizing our sample size and enabling a robust comparison across different tumor genes. Specifically, we aggregated all samples of each gene from any gene panel if it covered the corresponding gene. Based on this approach, we obtained a slightly different pool of samples for each comparison, improving the sensitivity of the detection of differences with the larger sample size. In total, we collected 2095 genes and 5471 samples from 34 panels.
We identified 28 significant gene-hematologic tumor pairs differing in mutation rates of CYAs and OAs using Fisher’s exact test, covering myeloid and lymphoid tumors (FDR < 0.05; Fig. 2b and Supplementary Table 11). Further analysis revealed mutation rate disparities within specific histological subtypes of hematologic tumors. Specifically, we identified 15 gene-hematologic tumor subtype pairs with significant differences in mutation rates between the two age groups, capturing three myeloid (i.e., AML, MDS, and MPN) and two lymphoid [i.e., MBN and diffuse large B-cell lymphomas (DLBCL)] tumor subtypes (FDR < 0.05; Fig. 2c and Supplementary Table 12). Recurrent genes TET2, DNMT3A, and TP53 consistently showed significantly higher mutation rates in OAs compared to CYAs in both myeloid and lymphoid tumors. Specifically, mutations in TET2, DNMT3A, and TP53 are frequently implicated in clonal hematopoietic (CH) conditions25,26,27,28,29,30, a phenomenon more prevalent among the elderly population. This heightened prevalence could potentially lead to the elevated mutation rates observed in these genes in OAs compared to CYAs. The presented data unambiguously demonstrate that older individuals frequently exhibit clonal “skewing” within their hematopoietic systems, pointing to a contributing factor to the onset and development of hematologic malignancies. Most genes (n = 20) showed higher mutation rates in OAs, and only 7 genes shared higher mutation rates in CYAs (i.e., NRAS, KRAS, SMARCA4, ID3, PTPN11, WT1, and KIT), aligning with the generally lower TMB observed in this younger demographic.
Genes from different hematologic tumor subtypes, including TP53, TET2, SRSF2, RUNX1, DNMT3A, IDH2, ASXL1 in AML, TET2 in MPN, and MYD88 in DLBCL, displayed lower mutation rates in CYAs, which was consistent with our previous observation of genes in myeloid and lymphoid tumors. In contrast, SMARCA4, ID3 in MBN had higher mutation rates in CYAs, indicating the same trend of mutation rate difference without subtype classifications. In particular, we observed elevated mutation rates in CYAs in three novel genes (i.e., EP300 in MDS, PRTOR, MYC in MBN). These findings underscore the complex interplay of genetic factors influencing hematologic malignancies and highlight the variability of mutation rates across different age groups, necessitating age-specific considerations in the clinical management and treatment of these diseases.
Network and functional analysis of key human genes
We conducted a network and functional role analysis of human interacting proteins (i.e., targets) of the DMG sets (i.e., ‘Myeloid CYA’, ‘Myeloid OA’, ‘Lymphoid CYA’, and ‘Lymphoid OA’) between CYAs and OAs. Specifically, we mapped human protein-protein interactions (PPIs) onto these DMGs comparing CYAs and OAs with myeloid and lymphoid tumors and obtained 55 in ‘Myeloid CYA’, 265 in ‘Myeloid OA’, 202 in ‘Lymphoid CYA’, and 266 human targets in ‘Lymphoid OA’, respectively (Fig. 3a and Supplementary Table 13). These targets were involved in 549 human PPIs that composed 21 human PPI subnetworks (Fig. 3b and Supplementary Fig. 1). We found that TP53, which had a significantly high mutation rate in OAs, interacts with other three significantly highly mutated genes (i.e., CREBBP and BCL2 in OAs, and EP300 in CYAs), suggesting potential interaction associations and intricate regulatory relationships between these genes across different age groups. To characterize network patterns of targets of such DMGs, we determined their connectivity in the human PPI network of each target. We observed that targets of highly mutated genes in ‘Myeloid CYA’ exhibited significantly higher degrees compared to those in ‘Myeloid OA’ (Wilcoxon rank sum test, P = 0.026; Fig. 3c), indicating that genes with high mutation rates in CYAs were more likely to influence key proteins in the interaction networks compared to genes with high mutation rates in OAs.
a Interacting targets of differentially mutated genes between CYAs and OAs in myeloid and lymphoid tumors. b Protein interaction subnetwork of differentially mutated genes between CYAs and OAs. c In the human protein interaction network, the numbers of interacting proteins (i.e., degree) of differentially mutated genes in myeloid and lymphoid tumors are shown. The proportions of scaffold proteins (d), essential genes (e) and innate immune-related proteins (f) of interacting proteins of differentially mutated genes in myeloid and lymphoid tumors. g Enriched GO terms of the interacting partners of differentially mutated genes in myeloid and lymphoid tumors.
We also examined the functionality of the targets of these DMG sets. First, we focused on scaffold proteins, which promote functional complex assembly by providing scaffolds and thus play critical roles in various cellular signaling pathways. We compared proportions of scaffold proteins in targets of these four DMG sets and observed a significantly higher proportion of scaffold proteins in targets of highly mutated genes in ‘Myeloid CYA’ compared to ‘Myeloid OA’ (two-tailed Fisher’s exact test, P = 0.047; Fig. 3d). Such an observation indicated that the correct assembly of human functional protein complexes may be more severely disrupted in CYAs than in OAs within myeloid tumors. Second, we assessed the distribution of essential genes and innate immune-related proteins within these targets. We found that the proportion of essential genes targeted by highly mutated genes in ‘Lymphoid CYA’ was significantly greater than those in both ‘Lymphoid OA’ and ‘Myeloid CYA’ (two-tailed Fisher’s exact test, P < 0.05; Fig. 3e). Conversely, the proportion of innate immune-related proteins was notably higher in targets of ‘Myeloid CYA’ and ‘Lymphoid OA’ (two-tailed Fisher’s exact test, P < 0.05; Fig. 3f). Such findings indicated that highly mutated genes in ‘Lymphoid CYA’ tend to target more essential genes and fewer innate immune-related proteins, which may cause more severe impairment of cellular life activities with a relatively smaller impact on innate immune responses. In contrast, highly mutated genes in ‘Myeloid CYA’ tend to target fewer essential genes and more innate immune-related proteins, which may prompt the production of stronger immune responses to repair damage and clear tumors or produce relatively stronger immune responses to lead to immune damage and dysregulation.
Our functional enrichment analysis further highlighted that proteins targeted by highly mutated genes in CYA tumors were predominantly involved in ‘positive regulation of cell population proliferation’ (Fig. 3g and Supplementary Table 14). In contrast, targets of highly mutated genes in OA tumors were enriched with biological processes such as ‘apoptotic process’ and ‘regulation of telomerase’ (Fig. 3g and Supplementary Table 14). In particular, targets of highly mutated genes in ‘Myeloid CYA’ shared several specific biological processes such as ‘protein phosphorylation’ and ‘glucose homeostasis’, while targets of highly mutated genes in ‘Lymphoid CYA’ were usually enriched with cell cycle related processes (Fig. 3g and Supplementary Table 14).
To demonstrate the convincing power of these features based on our network-based analysis, we further incorporated two publicly accessible large-scale myeloid tumor cohorts14,15 from cBioPortal31 to perform differential expression and functional enrichment analysis between CYAs and OAs (Fig. 4). Our analysis revealed that up-regulated genes (CPNE8, SYT1, RPH3A, and ARHGAP32) in ‘Myeloid CYA’ were enriched with molecular functions such as ‘calcium-dependent phospholipid binding’ and ‘phosphatidylinositol phosphate binding’ (Fig. 4). Conversely, up-regulated genes (LTK, AGT, DLX1, POU4F1, and NFATC4) in OAs were enriched with biological processes like ‘positive regulation of cardiac muscle cell apoptotic process’ and ‘neuron apoptotic process’ (Fig. 4). Such findings not only align with our previous observations but also provide additional support for the reliability of our network-based analysis of targets of differentially mutated genes between CYAs and OAs.
a Enriched GO terms of differentially expressed genes between CYAs and OAs in myeloid tumor. b Highly expressed genes (CPNE8, SYT1, RPH3A, and ARHGAP32) in CYAs are involved in molecular functions such as ‘calcium-dependent phospholipid binding’ and ‘phosphatidylinositol phosphate binding’. Conversely, in OAs, the highly expressed genes include LTK, AGT, DLX1, POU4F1, and NFATC4, which participate in biological processes like ‘positive regulation of cardiac muscle cell apoptotic process’ and ‘neuron apoptotic process’.
Gene level CNA and gene fusions comparison between CYAs and OAs
Comparing gene level CNAs between CYAs and OAs, we identified 84 significant gene-lymphoid tumor pairs, including 77 amplifications and 7 deletions (Fig. 5, Supplementary Tables 15 and 16). No significant gene-cancer pair emerged in other hematologic tumor categories. Upon closer inspection, we found that amplifications were predominant in CYAs (n = 50, 65%) while deletions were exclusively observed in OAs (n = 7, 100%). In particular, four genes (i.e., ARID1B, ESR1, MYB, and TP53) exhibited both amplifications and deletions, with each alteration type more prevalent in CYAs and OAs, respectively (Fig. 5a–c).
a 50 gene level CNAs (amplifications) were significantly frequent in CYAs compared to OAs (i.e., CYA > OA) in lymphoid tumors. b 27 gene level CNAs (amplifications) were significantly frequent in OAs compared to CYAs (i.e., OA > CYA) in lymphoid tumors. c 7 gene level CNAs (deletions) were significantly frequent in OAs compared to CYAs (i.e., OA > CYA) in lymphoid tumors. Comparison of gene fusions (d) and genes involved in fusions (e) between CYAs and OAs. The horizontal and vertical coordinates represent the CYA and OA ratios, respectively. The circle below the diagonal indicates that the fusions/genes involved in fusions were more frequent in CYAs than OAs while the circle above the diagonal shows the opposite. Circle size corresponds to -lg FDR. Circles filled with yellow color indicate statistically significant differences (FDR < 0.05). Dashed and solid lines denote different tumor types i.e., myeloid and lymphoid tumors, respectively.
The genes identified in CNA comparisons primarily appeared in crucial signaling pathways such as the p53 and PI3K-AKT pathways, echoing patterns observed in our mutation analysis. Within the p53 pathway, genes like TP53 and PTEN (inhibition of IGF-1/mTOR pathway) showed increased CNAs in CYAs, indicative of heightened activation or disruption in younger patients in CYAs (Fig. 5a), whereas MDM2 (oncogene activation) exhibited fewer CNAs in this group (Fig. 5b). In turn, TP53 and ATM (DNA damage) were more frequently deleted in OAs, suggesting different regulatory disruptions in older patients (Fig. 5c). As for the PI3K pathway, PTEN, MYB, FGFR2, FGFR3, PDGFRA, KIT, KDR, RET, and AKT1 showed more amplifications in CYAs compared to OAs (Fig. 5a), pointing to an active involvement in tumor progression in younger patients. Meanwhile, amplifications of oncogenes like KRAS, ERBB3, and MET were more frequent in OAs (Fig. 5b), potentially influencing tumor behavior differently in this age group. The transcription factor MYB, known for its role in various cancers including lymphoma, colorectal cancer, and breast cancer32,33,34, was found to have more deletions in OAs than in CYAs, suggesting a potential loss of function with aging (Fig. 5c). Additionally, ESR1, another key transcription factor implicated in hormone-responsive cancers like breast and ovarian cancer35,36, showed more amplifications and fewer deletions in CYAs (Fig. 5a, c), raising concerns about potential resistance to therapies such as tamoxifen, given previous associations between ESR1 amplification and treatment resistance37.
As for gene fusions, we identified disparities in their prevalence between CYAs and OAs, including 2 differential fusion-myeloid tumor pairs and 10 differential fusion-lymphoid tumor pairs (P < 0.05). Specifically, the BCL2-IGH fusion was more common in OAs, whereas other fusions, such as ETV6-RUNX1 (FDR < 0.05), were predominantly found in CYAs (Fig. 5d and Supplementary Table 17). Such observations suggest that certain fusions may confer distinct pathological features or therapeutic vulnerabilities in different age groups. Since only a few fusions were a consequence of their scarcity, we expanded our analysis to fusion partner genes. We identified 7 and 15 gene-cancer pairs at a P-value threshold of 0.05 in myeloid and lymphoid tumors, respectively (Fig. 5e and Supplementary Table 18). At an FDR control of 0.05, we further retrieved four gene-cancer pairs that frequently occurred in CYAs, capturing KMT2A in myeloid tumors, ETV6, RUNX1, and KMT2A in lymphoid tumors. RUNX1 was frequently amplified in CYA lymphoid tumors. These findings indicate the potential for targeted fusion-based therapies that could benefit a substantial segment of CYA patients, particularly those with lymphoid malignancies.
Overall, our study illustrates that both CNAs and gene fusions manifest distinctly between CYAs and OAs, suggesting the need for age-tailored approaches in the diagnosis and treatment of hematologic tumors, based on the specific genetic alterations prevalent in each group.
Clinically actionable tiers in CYAs and OAs
In our final analysis, we focused on delineating the pathogenicity and treatment implications of mutations in CYAs and OAs, using robust annotation frameworks. Each mutation was classified according to its clinical actionability based on NCCN guidelines and OncoKB, a manually curated database for gene alterations with pathogenicity/diseases and targeting drugs (Fig. 6). Within this framework, alterations classified as levels 1/2/3 A/R1 are considered Tier I, indicating strong clinical significance, while levels 4/R2 are categorized as Tier II, reflecting potential clinical significance. Detailed explanations of these evidence levels are provided in the Methods section. All mutations, corresponding levels, and site-associated drugs are provided in Supplementary Table 19, offering a more complete landscape of gene mutations that underline the development and progression of various hematological malignancies.
Mutation levels of sites in CYAs and OAs suffering from myeloid/lymphoid tumors are shown in the left panel (a), while corresponding levels of mutation sites in CYAs suffering from various tumor subtypes are shown in the right panel (b). Mutation levels of sites were obtained from OncoKB. For each patient sample, the highest level of any mutation is considered if multiple mutations were identified. Level_1~Level_4 evidence from strong to weak (i.e., standard care, investigational, hypothetical). Level_R1 and Level_R2 are associated with drug resistance, i.e., standard care resistance and investigational resistance, respectively.
Our analysis revealed that 77.81% (277 of 356) of myeloid tumors in CYAs suffered a level 1 or 2 alteration, while 0.84% (n = 3) suffered a level 4 alteration. In contrast, in myeloid tumor OAs, a higher proportion, 91.11% (2735 out of 3002), exhibited level 1 or 2 alterations. Additionally, a small fraction, 0.30%, experienced alterations at level 3 A, and 0.20% at level 4, underscoring a generally higher tier of clinical actionability in OAs compared to CYAs in myeloid tumors. Similar patterns were observed across lymphoid tumors as well (Fig. 6).
A notable finding was the higher incidence of resistance-associated drug sites (levels R1/R2) among CYAs compared to OAs. Specifically, 23.88% CYAs and 13.86% OAs in myeloid tumors exhibited these resistance markers. This disparity was even more pronounced in lymphoid tumors, where 18.99% CYAs and only 4.55% OAs displayed resistance to therapeutic agents (two-tailed Fisher’s exact test, P = 3.31E-16 in lymphoid tumors; P = 8.23E-5 in myeloid tumors) (Fig. 6a).
Diving deeper into specific tumor subtypes within CYAs, we observed that the frequency of clinically significant alterations (levels 1/2) was relatively consistent across MDS, AML, and MPN. However, AML stood out with a notable high proportion of resistance-associated alterations (levels R1/R2; 31.20%, 73 out of 234), which was significantly higher than in other subtypes (Fig. 6b). Similarly, in lymphoid tumors, BLL showed the highest resistance drug proportion (levels R1/R2; 34.29%, 72 of 210) of annotated gene mutation sites in all lymphoid tumor subtypes (Fig. 6b).
These data and insights underscore the critical need for tailored therapeutic strategies based on the unique genetic profiles of CYAs and OAs, particularly given the distinct patterns of drug resistance that may influence treatment outcomes across different age groups and tumor subtypes.
Discussion
The genomic landscapes of hematologic malignancies in different age groups, specifically CYAs and OAs, are intricately varied and underexplored. The age of onset of different hematologic malignancies is different, which may be closely related to the genomes of patients. In this work, we analyzed the clinical and genomic disparities between CYA and OA hematologic malignancies, uncovering substantial differences in clinical features such as patient sex, metastatic status, ethnicity, and tumor subtypes. We also found differential age distribution (i.e., the ratios of CYAs and OAs) of patients with different hematologic tumors. Genomically, CYA hematologic tumors generally showed a lower tumor mutational burden, particularly noticeable in lymphoid tumors of the four hematologic tumor types. Focusing on the 28 hematologic tumor subtypes, FL and AML showed significantly lower TMBs in CYAs, whereas MBN indicated the opposite trend. In accordance, most hematologic tumor genes showed lower mutation rates in CYAs. However, we observed exceptions such as higher NRAS, KRAS, SMAPRCA4, ID3, and PTPN11 mutations in CYA lymphoid tumors as well as higher WT1 and KIT mutations in CYA myeloid tumors.
Network analyses further revealed that CYA myeloid tumors had a greater number of interacting proteins of highly mutated genes compared to those in OAs, suggesting that highly mutated genes in CYAs are more likely to interact with hub proteins in the human interaction network. Additional functional role analyses indicated that interacting proteins (i.e., targets) targeted by these differentially mutated genes in CYA myeloid tumors showed higher proportions of scaffold proteins and innate immune-related proteins, while CYA lymphoid tumors presented a higher proportion of essential genes in targets. Such observations indicated a stronger mutational impact on protein complex assembly and immune response in CYA myeloid tumors as well as a stronger mutational impact on cell survival in CYA lymphoid tumors. Our functional enrichment analysis indicated that proteins targeted by differentially mutated genes in CYAs were predominantly enriched with ‘positive regulation of cell population proliferation’ while targets in OAs were enriched with biological processes such as ‘apoptotic process’ and ‘regulation of telomerase’, indicating differing pathological mechanisms influenced by age.
In our CNA comparison, we observed predominant amplifications in CYA lymphoid tumors, while deletions were more common in OAs. In particular, we found that four genes i.e., ARID1B, ESR1, MYB, and TP53 were frequently amplified in CYA lymphoid tumors but frequently deleted in OA lymphoid tumors. Despite being the same molecules, this intriguing finding suggests that these genes may play roles in tumorigenesis through different functional mechanisms. Deletion of TP53, a well-established tumor suppressor gene, is well understood in the context of tumorigenesis due to its functional inactivation. However, the role of highly amplified TP53 in carcinogenesis necessitates further scientific scrutiny. To further understand the significance of TP53 amplification, we conducted a preliminary investigation of TP53 CNAs in the ClinVar database (https://www.ncbi.nlm.nih.gov/clinvar/). In particular, we observed six amplifications annotated as pathogenic or likely pathogenic (ClinVar accessions: VCV003063486.1, VCV000149166.2, VCV000145484.2, VCV002579287.1, VCV000149531.2, and VCV000154089.2). Such data hint at a potentially oncogenic role for amplified TP53, albeit the mechanisms remain largely unknown. Given the complexity and multifaceted nature of TP53 function, elucidating the precise mechanisms by which amplification affects tumorigenesis requires rigorous scientific investigation. Therefore, further research endeavors are needed to comprehensively understand the role of TP53 amplification in carcinogenesis. Such investigations will not only deepen our understanding of TP53 biology but may also identify new therapeutic strategies for treating cancers driven by TP53 amplification.
Additionally, we observed that RAS family members, specifically NRAS and KRAS, exhibited elevated mutation rates in CYAs. Conversely, in the CNA comparison, increased frequency of KRAS amplification was exclusively observed in OAs. Closer examination of specific mutation sites revealed that nearly all NRAS/KRAS sites, including G12, G13, and Q61, possess oncogenic and gain-of-function characteristics, thereby carrying significant therapeutic and diagnostic implications. These mutations are classified as Level 1/2, R1, Dx2, and FDA Level 2, as detailed in Supplementary Table 19. As for amplifications in OAs, KRAS amplification inclined to be likely oncogenic and indicative of likely gain-of-function. Such studies on solid tumors associated KRAS with tumor metastasis and drug resistance38,39,40,41. In the context of endometrial cancer, Birkeland et al. reported that KRAS amplification and overexpression, rather than mutation, are linked to cancer metastasis38. In vitro studies have further shown that this amplification leads to resistance against various inhibitors, including the tyrosine kinase inhibitor crizotinib, EGFR inhibitors cetuximab and panitumumab, MET inhibitors, and MEK inhibitors, in patient-derived cancer cell line models39,40,41. Meanwhile, NRAS amplification did not significantly differ between CYAs and OAs, while its clinical significance remains inconclusive (https://oncokb.org/).
As for gene fusions, we observed that CYA hematologic malignancies generally harbor more gene fusions, especially the most significant ETV6-RUNX1 fusion in CYA lymphoid tumors. Such CNA-associated differential genes and differential fusions between CYA and OA tumors provide an entry point for the development of personalized treatments for different age and mutant groups. From a clinical perspective, we found that the proportion of actionable genetic alterations was lower in CYAs compared to OAs in both myeloid and lymphoid tumors, with CYAs exhibiting a higher frequency of drug resistance sites, especially in AML and BLL subtypes. Such observations suggested that more specialized strategies of drug use should be applied in CYA hematologic malignancies to overcome drug resistance effectively.
Furthermore, we presented a comparative landscape of clinically actionable genetic events in CYAs and OAs, revealing a higher incidence of resistance-associated drug sites (levels R1/R2) in CYAs compared to OAs, particularly in lymphoid tumors. It is well-established that younger patients with hematopoietic malignancies, including ALL, often exhibit superior treatment responses compared to their older counterparts, such as higher remission rates and improved survival. This advantage is attributed to factors such as better overall health, fewer comorbidities, and potentially more responsive immune systems in younger individuals. However, the observation of a higher proportion of Level R1 alterations associated with drug resistance in CYAs presents a complex scenario. This finding may suggest several underlying mechanisms: (i) Genetic heterogeneity: younger patients might harbor distinct genetic alterations that confer resistance to specific therapies. These alterations could be more prevalent or exclusive to this age group, highlighting the necessity for age-stratified genetic profiling to tailor personalized treatment strategies. (ii) Tumor biology: the biological characteristics of tumors in younger patients may fundamentally differ from those in older patients, leading to varied responses to therapy. This could involve distinct signaling pathways, metabolic activities, or interactions with the tumor microenvironment. (iii) Drug metabolism and pharmacodynamics: age-related variations in drug metabolism, distribution, and elimination could impact treatment efficacy. Younger patients may metabolize drugs differently, affecting therapeutic outcomes and potentially selecting for resistant clones. (iv) Treatment tolerance and adherence: although not directly linked to genetic alterations, younger patients’ ability to tolerate intensive treatment regimens may lead to more aggressive therapy, inadvertently selecting for resistant mutations.
To address these discrepancies, future research should focus on: (i) Comprehensive genetic and molecular profiling of tumors of both younger and older patients to identify age-specific alterations and their functional implications. (ii) Investigation of the biological underpinnings of age-related differences in treatment response, including potential differences in tumor microenvironment, immune response, and metabolic pathways. (iii) Exploration of pharmacokinetic and pharmacodynamic differences across age groups to optimize drug dosing and scheduling. (iv) Implementation of prospective clinical trials that stratify patients by age to better understand and target age-specific resistance mechanisms. In conclusion, while the superior treatment outcomes observed in younger patients with hematopoietic tumors are well-acknowledged, the higher proportion of Level R1 alterations associated with drug resistance in this group underscores the complexity of tumor biology and the pressing need for tailored therapeutic approaches. Our future research endeavors will strive to elucidate these discrepancies and enhance precision medicine for all patient populations.
Lastly, the potential role of germline mutations, which was not addressed in this study due to data limitations, remains a crucial area for future research. Understanding the impact of germline mutations could provide insights into predisposition and resistance mechanisms in younger patients as germline mutations may disproportionately affect younger patients with hematologic malignancies. For instance, approximately 4% of children with ALL carry a germline cancer predisposition gene mutation42, and germline RUNX1 and ETV6 mutations lead to thrombocytopenia43. In particular, we also observed enriched RUNX1 amplifications as well as ETV6-RUNX1 fusion in CYA lymphoid tumors, although it remained unclear if the enrichments were associated with thrombocytopenia. Germline TP53 mutations lead to Li-Fraumeni syndrome (LFS), and ERBB3 amplification is enriched in LFS-associated tumors such as breast, gastric, and ovarian cancer and frequently co-occurred with amplification of other members of the epidermal growth factor receptor family, including EGFR or ERBB244. Interestingly, we also observed enriched TP53 deletions and ERBB3 amplifications in OA lymphoid tumors, although it is unclear if this amplification was associated with LFS. Nevertheless, the current enrichment of TP53 deletions and ERBB3 amplification in OAs indicated functional collaboration between the oncogenic variations in driving OA lymphoid tumors.
In summary, our study lays a foundation for further exploration into the ways somatic and potentially germline mutations influence the diagnosis, prognosis, and treatment of hematologic malignancies across different age groups. Future research will be vital in developing comprehensive, age-adapted treatment strategies to enhance outcomes for all patients affected by these diverse and challenging diseases.
This study is not devoid of limitations, which warrant careful consideration. First, the sample size, although representative to a certain extent, may not be sufficient to capture the full spectrum of variations within the myeloid and lymphoid tumor categories. Second, the inherent heterogeneity within these tumor types introduces complexity, potentially obscuring subtler age-related differences in their molecular profiles. Therefore, it is crucial to interpret our findings with these limitations in mind. To fully dissect the age-related differences in the molecular underpinnings of these tumors, future research endeavors with expanded sample sizes and more granular subtype analyses are indispensable.
Methods
Data collection and processing
Clinical and somatic mutation data were obtained from the AACR GENIE project via Synapse (release 13.1, https://www.synapse.org/#!Synapse:syn51355584). This study was conducted in strict accordance with the recommendations of the AACR project GENIE data access guidelines. In total, the released data contained cancer gene sequencing data from 167,358 samples and 104 gene panels. We used ‘CANCER_TYPE’ and ‘CANCER_TYPE_DETAILED’ to obtain hematologic tumor samples with specific subtypes. Subsequently, we used ‘AGE_AT_SEQ_REPORT’ to obtain two groups i.e., children and young adults (CYAs) (≤40 years) and older adults (OAs) (>40 years), assuming that the time of clinical sequencing is close to the time of disease diagnosis as a consequence of rapid turnaround of clinical sequencing. Furthermore, samples with unknown ages and follow-up (survival status or the last follow-up time) were removed. We employed a two-tiered approach to analyze the data. Initially, we categorized the tumors into broader groups (myeloid tumor, lymphoid tumor, MPAL, and PC tumor) to identify overarching patterns and age-related differences. This categorization allowed us to identify common themes and age-related trends that might be obscured when analyzing each subtype independently. However, we also conducted a more refined analysis based on 28 specific hematological tumor subtypes within these broader categories to capture unique molecular features of each subtype.
Clinical and population characteristic comparison
Only hematologic tumors with specific subtypes in both CYAs and OAs were retained for clinical and population characteristic comparisons. In total, we obtained 6684 samples from 40 gene panels covering four hematologic tumor categories and 28 specific subtypes. We compared numbers of CYAs and OAs, sex, metastasis rate, race, and ethnicity (non-Spanish White, non-Spanish Black, non-Spanish Asian, and Spanish) using Fisher’s exact test, followed by Benjamini–Hochberg (BH) correction of multiple hypothesis testing. The metastasis rate was defined as the proportion of extramedullary recurrence, including local recurrence, lymph node metastasis, and distant organ metastasis.
Tumor mutational burden calculation and comparison
To calculate TMB, we excluded gene panels with coverage less than 0.9 Mb as smaller panels are not reliable in estimating TMB20. After filtering, we obtained 576 CYA samples and 2639 OA samples. TMB was calculated as the total number of nonsynonymous mutations divided by the length of total exonic target regions captured by the probe hybridization assay. Information of the specific captured regions was obtained from the file ‘genomic_information.txt’.
Gene mutation rate comparison
To obtain somatic mutations, variants with a Genome Aggregation Database (gnomAD) allele frequency of 0.0005 or greater were flagged as potential germline variants and removed from the analysis. To compare somatic mutations between CYAs and OAs that were sequenced with different gene panels, we adopted different sample reference background strategies. For each gene, we only retained patient samples whose sequencing panel included the corresponding gene as a reference background set. In total, we curated 2095 genes and 34 panels, including 806 CYA samples and 4665 OA samples. We identified genes with significantly different mutation rates in CYAs and OAs as DMGs. Our analysis captures all mutations within the targeted gene panels specifically designed for hematological malignancies. Panels include genes that are relevant to clinical diagnosis, treatment, and prognosis, reflecting a comprehensive approach to identifying both potential driver or passenger mutations.
Network and functional analysis of differentially mutated genes
To characterize the network and functional features of these DMGs, we divided such DMGs into four subsets. In myeloid tumors, we considered genes in the ‘Myeloid CYA’ group with a mutation rate in CYAs that was significantly higher than in OAs. In turn, we collected genes in ‘Myeloid OA’ that showed the opposite. In lymphoid tumors, we considered genes with a mutation rate in CYAs that was significantly higher than in OAs in the ‘Lymphoid CYA’ group, while we considered the opposite in the ‘Lymphoid OA’ group.
We collected human protein-protein interactions (PPIs) from the IntAct database45 to identify interacting proteins (i.e., targets) of the DMGs. To characterize network patterns of DMGs, we calculated the number of interacting proteins of DMGs in the human PPI network (i.e., degree) by using the R package ‘igraph’ (https://igraph.org/). To characterize the functional roles of interacting partners of DMGs, we focused on three functional genes/proteins capturing essential genes, scaffold proteins, and human innate immune-related proteins. First, we collected 5169 human essential genes that were indispensable in diverse human cellular processes from refs. 46,47. Subsequently, we obtained 273 scaffold proteins from ScaPD48 and 1044 human innate immune-related proteins from InnateDB49. Scaffold proteins play important roles in a variety of cellular signaling pathways as a consequence of their ability to promote complex assembly. Innate immune-related proteins not only play a critical role in the first line of defense against viral invasion but are also related to the regulation and formation of subsequent adaptive immunity responses.
To find functional enrichments of the identified targets of DMGs, we downloaded GO annotation data of human proteins from http://current.geneontology.org/50. Using all human proteins mapped to Cellular Component, Biological Process and Molecular Function ontologies as reference sets, GO terms were deemed significantly enriched with human targets of each DMG set through hypergeometric tests, if the corresponding Benjamin-Hochberg corrected P-values were ≤ 0.05.
Gene level CNA and fusion comparison
We used the file ‘data_CNA.txt’ from GENIE v13.1 which contains 983 gene-level copy number alterations from 115,548 samples. Gene-level CNAs of 2,637 hematologic tumor samples were available for our follow-up analysis. Gene-level copy numbers were discretized into −2, −1, 0 (neutral), 1, and 2. We used −2/−1 for deletions and 2/1 for amplifications. Gene fusions were obtained from ‘data_fusion.txt’, allowing us to collect 385 unique fusions from 577 hematologic tumor samples. Fisher’s exact test was used to detect differential CNAs and fusions comparing CYAs and OAs.
Clinical actionability assessment and comparison
To assess the clinical actionability and pathogenicity of specific mutation sites, we annotated mutations according to the NCCN guidelines and OncoKB database (http://oncokb.org)51. Briefly, mutations were classified as level 1 if they can be targeted with an FDA-approved drug; level 2 alterations are standard care biomarkers that can predict response to an FDA-approved drug; level 3 alterations are likely targetable by an investigational drug, and level 4 alterations are likely targetable through preclinical trials or a few case reports without consensus. Level R1 alterations show resistance to an FDA-approved drug, and level R2 alterations are likely resistant to a drug in preclinical trials or a few case reports without consensus.
Statistics and reproducibility
The R package (v4.2.0) was employed to perform all statistical analyses. We used Fisher’s exact test to compare the clinical and population features in CYAs and OAs and the Benjamini–Hochberg method to correct for multiple testing, reporting significant results with false discovery rate (FDR) < 0.05. TMBs of CYAs and OAs were compared by using the Wilcoxon rank sum test followed by Benjamini–Hochberg correction.
Data availability
Genomic profiling datasets of hematologic malignancies that are publicly accessible can be retrieved from AACR GENIE (https://www.synapse.org/#!Synapse:syn51355584). Additionally, two publicly accessible large-scale gene expression profiling datasets of myeloid tumors can be obtained through cBioPortal (https://www.cbioportal.org/). All data analyzed during this study are included in this paper. Datasets used and analyzed are available in Supplementary Data 1. All other data will be available from the corresponding authors upon reasonable request.
Code availability
All the scripts used to implement the analyses presented in this manuscript are available at https://github.com/XiaodiYangpku/HMGA/.
References
Ferlay, J. et al. Global Cancer Observatory: Cancer Today (version 1.1). Lyon, France: International Agency for Research on Cancer. Available from: https://gco.iarc.who.int/today, https://doi.org/10.3322/caac.21660 (2024).
Dufva, O. et al. Immunogenomic landscape of hematological malignancies. Cancer Cell 38, 380–399 (2020).
Sterner, R. C. & Sterner, R. M. CAR-T cell therapy: current limitations and potential strategies. Blood Cancer J. 11, 69 (2021).
Dong, W. et al. The mechanism of anti–pd-l1 antibody efficacy against pd-l1–negative tumors identifies nk cells expressing pd-l1 as a cytolytic effector. Cancer Discov. 9, 1422–1437 (2019).
Zhang, J. et al. Non-viral, specifically targeted CAR-T cells achieve high safety and efficacy in B-NHL. Nature 609, 369–374 (2022).
DiNardo, C. D. et al. Molecular patterns of response and treatment failure after frontline venetoclax combinations in older patients with AML. Blood 135, 791–803 (2020).
Shlush, L. I. Age-related clonal hematopoiesis. Blood 131, 496–504 (2018).
Malard, F. & Mohty, M. Acute lymphoblastic leukaemia. Lancet 395, 1146–1162 (2020).
Hochberg, J. et al. Risk-adapted chemoimmunotherapy using brentuximab vedotin and rituximab in children, adolescents, and young adults with newly diagnosed Hodgkin’s lymphoma: a phase II, non-randomized controlled trial. J. Immunother. Cancer 10, e004445 (2022).
Lacy, S. E. et al. Targeted sequencing in DLBCL, molecular subtypes, and outcomes: a haematological malignancy research network report. Blood 135, 1759–1771 (2020).
Duncavage, E. J. et al. Genomic profiling for clinical decision making in myeloid neoplasms and acute leukemia. Blood 140, 2228–2247 (2022).
Lachowiez, C. A. et al. Contemporary outcomes in IDH-mutated acute myeloid leukemia: the impact of co-occurring NPM1 mutations and venetoclax-based treatment. Am. J. Hematol. 97, 1443–1452 (2022).
Wilson, W. H. et al. Effect of ibrutinib with R-CHOP chemotherapy in genetic subtypes of DLBCL. Cancer Cell 39, 1643–1653.e3 (2021).
Tyner, J. W. et al. Functional genomic landscape of acute myeloid leukaemia. Nature 562, 526–531 (2018).
Bottomly, D. et al. Integrative analysis of drug response and clinical outcome in acute myeloid leukemia. Cancer Cell 40, 850–864.e9 (2022).
Ball, S. et al. Molecular annotation of extramedullary acute myeloid leukemia identifies high prevalence of targetable mutations. Cancer 128, 3880–3887 (2022).
Clesham, K. et al. Identification of a c-MYB-directed therapeutic for acute myeloid leukemia. Leukemia 36, 1541–1549 (2022).
Arber, D. A. et al. International consensus classification of myeloid neoplasms and acute leukemias: integrating morphologic, clinical, and genomic data. Blood 140, 1200–1228 (2022).
Campo, E. et al. The International Consensus Classification of Mature Lymphoid Neoplasms: a report from the Clinical Advisory Committee. Blood 140, 1229–1253 (2022).
Wang, X., Langevin, A. M., Houghton, P. J. & Zheng, S. Genomic disparities between cancers in adolescent and young adults and in older adults. Nat. Commun. 13, 7223 (2022).
Garofalo, A. et al. The impact of tumor profiling approaches and genomic data strategies for cancer precision medicine. Genome Med. 8, 79 (2016).
Chalmers, Z. R. et al. Analysis of 100,000 human cancer genomes reveals the landscape of tumor mutational burden. Genome Med. 9, 34 (2017).
Qiu, P., Poehlein, C. H., Marton, M. J., Laterza, O. F. & Levitan, D. Measuring tumor mutational burden (TMB) in plasma from mCRPC patients using two commercial NGS assays. Sci. Rep. 9, 114 (2019).
Buchhalter, I. et al. Size matters: dissecting key parameters for panel-based tumor mutational burden analysis. Int. J. Cancer 144, 848–858 (2019).
Gibson, C. J. et al. Donor clonal hematopoiesis and recipient outcomes after transplantation. J. Clin. Oncol. 40, 189–201 (2022).
Fabre, M. A. et al. The longitudinal dynamics and natural history of clonal haematopoiesis. Nature 606, 335–342 (2022).
Saiki, R. et al. Combined landscape of single-nucleotide variants and copy number alterations in clonal hematopoiesis. Nat. Med. 27, 1239–1249 (2021).
Xie, M. et al. Age-related mutations associated with clonal hematopoietic expansion and malignancies. Nat. Med. 20, 1472–1478 (2014).
Umeda, M. et al. A new genomic framework to categorize pediatric acute myeloid leukemia. Nat. Genet. 56, 281–293 (2024).
Liu, Y. F. et al. Genomic profiling of adult and pediatric B-cell acute lymphoblastic leukemia. EBioMedicine 8, 173–183 (2016).
Cerami, E., Gao, J., Dogrusoz, U., Gross, B. E. & Sumer, O. S. The cBio Cancer Genomics Portal: an open platform for exploring multidimensional cancer genomics data. Cancer Discov. 2, 401–404 (2012).
Nakano, K., Uchimaru, K., Utsunomiya, A., Yamaguchi, K. & Watanabe, T. Dysregulation of c-Myb pathway by aberrant expression of proto-oncogene MYB provides the basis for malignancy in adult T-cell leukemia/lymphoma cells. Clin. Cancer Res. 22, 5915–5928 (2016).
Li, Y. et al. c-Myb enhances breast cancer invasion and metastasis through the Wnt/β-catenin/Axin2 pathway. Cancer Res. 76, 3364–3375 (2016).
Guerrero Llobet, S. et al. An mRNA expression-based signature for oncogene-induced replication-stress. Oncogene 41, 1216–1224 (2022).
Lee, J. J. K. et al. ERα-associated translocations underlie oncogene amplifications in breast cancer. Nature 618, 1024–1032 (2023).
Yu, K. D. & Shao, Z. M. ESR1 gene amplification: another mechanism regulating the cellular levels of ERα. Nat. Rev. Cancer 11, 823 (2011).
Thomas, C. & Gustafsson, J. Å. The different roles of ER subtypes in cancer biology and therapy. Nat. Rev. Cancer 11, 597–608 (2011).
Birkeland, E. et al. KRAS gene amplification and overexpression but not mutation associates with aggressive and metastatic endometrial cancer. Br. J. Cancer 107, 1997–2004 (2012).
Wong, G. S. et al. Targeting wild-type KRAS-amplified gastroesophageal cancer through combined MEK and SHP2 inhibition. Nat. Med. 24, 968–977 (2018).
Bahcall, M. et al. Amplification of wild-type KRAS imparts resistance to crizotinib in MET exon 14 mutant non–small cell lung cancer. Clin. Cancer Res. 24, 5963–5976 (2018).
Valtorta, E. et al. KRAS gene amplification in colorectal cancer and impact on response to EGFR-targeted therapy. Int. J. Cancer 133, 1259–1265 (2013).
Bloom, M., Maciaszek, J. L., Clark, M. E., Pui, C. H. & Nichols, K. E. Recent advances in genetic predisposition to pediatric acute lymphoblastic leukemia. Expert Rev. Hematol. 13, 55–70 (2020).
Klco, J. M. & Mullighan, C. G. Advances in germline predisposition to acute leukaemias and myeloid neoplasms. Nat. Rev. Cancer 21, 122–137 (2021).
Ma, J., Lyu, H., Huang, J. & Liu, B. Targeting of erbB3 receptor to overcome resistance in cancer treatment. Mol. Cancer 13, 105 (2014).
Del Toro, N. et al. The IntAct database: efficient access to fine-grained molecular interaction data. Nucleic Acids Res. 50, D648–D653 (2022).
Funk, L. et al. The phenotypic landscape of essential human genes. Cell 185, 4634–4653.e22 (2022).
Blomen, V. A. et al. Gene essentiality and synthetic lethality in haploid human cells. Science 350, 1092–1096 (2015).
Han, X. et al. ScaPD: a database for human scaffold proteins. BMC Bioinforma. 18, 386 (2017).
Breuer, K. et al. InnateDB: systems biology of innate immunity and beyond—recent updates and continuing curation. Nucleic Acids Res. 41, D1228–D1233 (2013).
The Gene Ontology Consortium. The gene ontology resource: 20 years and still GOing strong. Nucleic Acids Res. 47, D330–D338 (2019).
Suehnholz, S. P. et al. Quantifying the expanding landscape of clinical actionability for patients with cancer. Cancer Discov. 14, 49–65 (2024).
Acknowledgements
This work was supported by the Beijing Natural Science Foundation (J230024) and the National High Level Hospital Clinical Research Funding (Interdisciplinary Clinical Research Project of Peking University First Hospital) (2022CR38).
Author information
Authors and Affiliations
Contributions
X.Y., Y.D., and Z.L. initiated and designed the research; X.Y., Q.W., and Y.S. collected and analyzed the data; X.Y. wrote the manuscript; X.Y., Y.D., Z.L., S.W., and Z.Z. interpreted the results and provided feedback. X.Y., S.W., Z.Z., Z.L., and Y.D. revised the manuscript. All authors reviewed the manuscript critically.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Communications Biology thanks Cosimo Cumbo, June Takeda and Yasunobu Nagata for their contribution to the peer review of this work. Primary Handling Editors: John Mulley and Kaliya Georgieva. [A peer review file is available].
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Yang, X., Wang, Q., Sun, Y. et al. Genomic differences of patients with hematologic malignancies in different age groups. Commun Biol 7, 1630 (2024). https://doi.org/10.1038/s42003-024-07293-0
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s42003-024-07293-0