Abstract
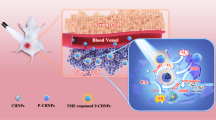
Cancer cells promote tumor growth and metastasis through tumor extracellular vesicle (TEV)-mediated intercellular and intertissue communication. Inhibiting TEVs represents a promising strategy to suppress metastasis; however, effectively and selectively disabling TEVs remains challenging. Herein, we developed palmitic acid surface-displayed nanoparticles using an adjacent hydrophilic molecular engineering strategy. Unexpectedly, these lipidated nanoparticles were not only efficiently taken up and distributed within tumor cells but also coupled with TEV generation, enabling active tracing of TEVs. Exploiting their dual tumor spatial distribution (intracellular and intra-TEV), a lipidated nanophotosensitizer was constructed for metastasis therapy. Under near-infrared light irradiation at the primary tumor site, both intracellular and intra-TEV reactive oxygen species were generated synchronously. This led to photodynamic suppression of the primary tumor and blocked intercellular and intertissue communication by disabling TEVs, effectively inhibiting tumor growth and metastasis in multiple tumor models in female mice. Overall, this work reports a therapeutic paradigm for concurrently inhibiting tumor growth and metastasis.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$32.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
Data availability
The data that support the findings of this study are available within the article and Supplementary Information or from the corresponding author upon request. Source data are provided with this paper.
References
Andre, F. et al. Genomics to select treatment for patients with metastatic breast cancer. Nature 610, 343–348 (2022).
Ganesh, K. & Massagué, J. Targeting metastatic cancer. Nat. Med. 27, 34–44 (2021).
van Zijl, F., Krupitza, G. & Mikulits, W. Initial steps of metastasis: cell invasion and endothelial transmigration. Mutat. Res. 728, 23–34 (2011).
Chaffer, C. L. & Weinberg, R. A. A perspective on cancer cell metastasis. Science 331, 1559–1564 (2011).
Mahvi, D. A., Liu, R., Grinstaff, M. W., Colson, Y. L. & Raut, C. P. Local cancer recurrence: the realities, challenges, and opportunities for new therapies. CA Cancer J. Clin. 68, 488–505 (2018).
Sang, W., Zhang, Z., Dai, Y. & Chen, X. Recent advances in nanomaterial-based synergistic combination cancer immunotherapy. Chem. Soc. Rev. 48, 3771–3810 (2019).
Drake, C. Combination immunotherapy approaches. Ann. Oncol. 23, viii41–viii46 (2012).
Yap, T. A. et al. Development of immunotherapy combination strategies in cancer. Cancer Discov. 11, 1368–1397 (2021).
Keklikoglou, I. et al. Chemotherapy elicits pro-metastatic extracellular vesicles in breast cancer models. Nat. Cell Biol. 21, 190–202 (2019).
Guan, X. et al. Nanoparticle-enhanced radiotherapy synergizes with PD-L1 blockade to limit post-surgical cancer recurrence and metastasis. Nat. Commun. 13, 2834 (2022).
Li, T. et al. Therapeutic nanocarriers inhibit chemotherapy‐induced breast cancer metastasis. Adv. Sci. 9, 2203949 (2022).
Zhong, Y. et al. Targeting proinflammatory molecules using multifunctional MnO nanoparticles to inhibit breast cancer recurrence and metastasis. ACS Nano 16, 20430–20444 (2022).
Tu, Z. et al. Scavenging tumor‐derived small extracellular vesicles by functionalized 2D materials to inhibit tumor regrowth and metastasis following radiotherapy. Adv. Funct. Mater. 32, 2205663 (2022).
Chang, M., Hou, Z., Wang, M., Li, C. & Lin, J. Recent advances in hyperthermia therapy‐based synergistic immunotherapy. Adv. Mater. 33, 2004788 (2021).
Qu, X., Tang, Y. & Hua, S. Immunological approaches towards cancer and inflammation: a cross talk. Front. Immunol. 9, 563 (2018).
Liu, Q. et al. Nano-immunotherapy: unique mechanisms of nanomaterials in synergizing cancer immunotherapy. Nano Today 36, 101023 (2021).
Peinado, H. et al. Pre-metastatic niches: organ-specific homes for metastases. Nat. Rev. Cancer 17, 302–317 (2017).
Liu, Y. & Cao, X. Characteristics and significance of the pre-metastatic niche. Cancer Cell 30, 668–681 (2016).
Becker, A. et al. Extracellular vesicles in cancer: cell-to-cell mediators of metastasis. Cancer Cell 30, 836–848 (2016).
Tkach, M. & Théry, C. Communication by extracellular vesicles: where we are and where we need to go. Cell 164, 1226–1232 (2016).
Shao, H. et al. New technologies for analysis of extracellular vesicles. Chem. Rev. 118, 1917–1950 (2018).
Théry, C. et al. Minimal information for studies of extracellular vesicles 2018 (MISEV2018): a position statement of the International Society for Extracellular Vesicles and update of the MISEV2014 guidelines. J. Extracell. Vesicles 7, 1535750 (2018).
Pathan, M. et al. Vesiclepedia 2019: a compendium of RNA, proteins, lipids and metabolites in extracellular vesicles. Nucleic Acids Res. 47, D516–D519 (2019).
Yang, H. et al. RETRACTED: Exosome-derived miR-130a activates angiogenesis in gastric cancer by targeting C-MYB in vascular endothelial cells. Mol. Ther. 26, 2466–2475 (2018).
Bhome, R. et al. Exosomal microRNAs (exomiRs): Small molecules with a big role in cancer. Cancer Lett. 420, 228–235 (2018).
Morrissey, S. M. et al. Tumor-derived exosomes drive immunosuppressive macrophages in a pre-metastatic niche through glycolytic dominant metabolic reprogramming. Cell Metab. 33, 2040–2058 (2021).
Maacha, S. et al. Extracellular vesicles-mediated intercellular communication: roles in the tumor microenvironment and anti-cancer drug resistance. Mol. Cancer 18, 1–16 (2019).
Tang, D., Liu, S., Shen, H., Deng, G. & Zeng, S. Extracellular vesicles promote the formation of pre-metastasis niche in gastric cancer. Front. Immunol. 13, 813015 (2022).
Yang, X. et al. Colorectal cancer-derived extracellular vesicles induce liver premetastatic immunosuppressive niche formation to promote tumor early liver metastasis. Signal Transduct. Target. Ther. 8, 102 (2023).
Tey, S. K. et al. Patient pIgR-enriched extracellular vesicles drive cancer stemness, tumorigenesis and metastasis in hepatocellular carcinoma. J. Hepatol. 76, 883–895 (2022).
Chen, G. et al. Exosomal PD-L1 contributes to immunosuppression and is associated with anti-PD-1 response. Nature 560, 382–386 (2018).
Qi, M. et al. Lin28B-high breast cancer cells promote immune suppression in the lung pre-metastatic niche via exosomes and support cancer progression. Nat. Commun. 13, 897 (2022).
Yu, P. et al. The incorporation of acetylated LAP–TGF-β1 proteins into exosomes promotes TNBC cell dissemination in lung micro-metastasis. Mol. Cancer 23, 82 (2024).
Zhang, H., Lu, J., Liu, J., Zhang, G. & Lu, A. Advances in the discovery of exosome inhibitors in cancer. J. Enzyme Inhib. Med. Chem. 35, 1322–1330 (2020).
Kim, J. H., Lee, C.-H. & Baek, M.-C. Dissecting exosome inhibitors: therapeutic insights into small-molecule chemicals against cancer. Exp. Mol. Med. 54, 1833–1843 (2022).
Yáñez-Mó, M. et al. Biological properties of extracellular vesicles and their physiological functions. J. Extracell. Vesicles 4, 27066 (2015).
Shin, S. et al. Curvature-sensing peptide inhibits tumour-derived exosomes for enhanced cancer immunotherapy. Nat. Mater. 22, 656–665 (2023).
Xie, S. et al. Preparation and evaluation of ofloxacin-loaded palmitic acid solid lipid nanoparticles. Int. J. Nanomedicine 6, 547–555 (2011).
Gong, T. et al. Palmitic acid-modified bovine serum albumin nanoparticles target scavenger receptor-A on activated macrophages to treat rheumatoid arthritis. Biomaterials 258, 120296 (2020).
Verma, A. & Stellacci, F. Effect of surface properties on nanoparticle–cell interactions. Small 6, 12–21 (2010).
Liu, M. et al. A transistor-like pH-sensitive nanodetergent for selective cancer therapy. Nat. Nanotechnol. 17, 541–551 (2022).
Zalba, S. & Ten Hagen, T. L. Cell membrane modulation as adjuvant in cancer therapy. Cancer Treat. Rev. 52, 48–57 (2017).
Zhong, Z. et al. RhoA vesicle trafficking-mediated transglutaminase 2 membrane translocation promotes IgA1 mesangial deposition in IgA nephropathy. JCI insight 8, e160374 (2023).
Agostinis, P. et al. Photodynamic therapy of cancer: an update. CA Cancer J. Clin. 61, 250–281 (2011).
Yang, B., Chen, Y. & Shi, J. Reactive oxygen species (ROS)-based nanomedicine. Chem. Rev. 119, 4881–4985 (2019).
Hak, A., Ali, M. S., Sankaranarayanan, S. A., Shinde, V. R. & Rengan, A. K. Chlorin e6: a promising photosensitizer in photo-based cancer nanomedicine. ACS Appl. Bio Mater. 6, 349–364 (2023).
Poon, I. K. et al. Moving beyond size and phosphatidylserine exposure: evidence for a diversity of apoptotic cell-derived extracellular vesicles in vitro. J. Extracell. Vesicles 8, 1608786 (2019).
Jin, L. et al. Breast cancer lung metastasis: molecular biology and therapeutic implications. Cancer Biol. Ther. 19, 858–868 (2018).
Lu, Z. et al. Regulation of intercellular biomolecule transfer-driven tumor angiogenesis and responses to anticancer therapies. J. Clin. Invest. 131, e144225 (2021).
Grum-Schwensen, B. et al. Suppression of tumor development and metastasis formation in mice lacking the S100A4(mts1) gene. Cancer Res. 65, 3772–3780 (2005).
Fang, T. et al. Tumor-derived exosomal miR-1247-3p induces cancer-associated fibroblast activation to foster lung metastasis of liver cancer. Nat. Commun. 9, 191 (2018).
Liang, S., Deng, X., Ma, P. A., Cheng, Z. & Lin, J. Recent advances in nanomaterial‐assisted combinational sonodynamic cancer therapy. Adv. Mater. 32, 2003214 (2020).
Mi, P. et al. A pH-activatable nanoparticle with signal-amplification capabilities for non-invasive imaging of tumour malignancy. Nat. Nanotechnol. 11, 724–730 (2016).
Lu, K. et al. Low-dose X-ray radiotherapy–radiodynamic therapy via nanoscale metal–organic frameworks enhances checkpoint blockade immunotherapy. Nat. Biomed. Eng. 2, 600–610 (2018).
Kim, K., Jang, S., Jeon, J., Kang, D. & Sohn, B.-H. Fluorescent supracolloidal chains of patchy micelles of diblock copolymers functionalized with fluorophores. Langmuir 34, 4634–4639 (2018).
Liu, J., Cui, L., Kong, N., Barrow, C. J. & Yang, W. RAFT controlled synthesis of graphene/polymer hydrogel with enhanced mechanical property for pH-controlled drug release. Eur. Polym. J. 50, 9–17 (2014).
Yin, J., Hu, H., Wu, Y. & Liu, S. Thermo- and light-regulated fluorescence resonance energy transfer processes within dually responsive microgels. Polym. Chem. 2, 363–371 (2011).
Tan, G. et al. Bioinspired poly(cation–π) micelles drug delivery platform for improving chemotherapy efficacy. J. Control. Release 349, 486–501 (2022).
Im, E.-J. et al. Sulfisoxazole inhibits the secretion of small extracellular vesicles by targeting the endothelin receptor A. Nat. Commun. 10, 1387 (2019).
Chen, S. et al. Enhanced tumour penetration and prolonged circulation in blood of polyzwitterion–drug conjugates with cell-membrane affinity. Nat. Biomed. Eng. 5, 1019–1037 (2021).
Acknowledgements
We greatly appreciate the financial support of the National Natural Science Foundation of China (22375086, 31972928 and 21905130 to X.W.), GuangDong Basic and Applied Basic Research Foundation (2024A1515010631 to X.W.), Science and Technology Projects in Guangzhou (202201011127 to X.W.) and research funds from Southern Medical University.
Author information
Authors and Affiliations
Contributions
G.M., Z.S. and Xiaorui W. conceptualized and designed the experiments. G.M., Z.S., Xinyue W., J.Z., M.X., P.H. and Q.Z. performed the experiments. G.M., Z.S., Xinyue W., J.Z., P.H., X.Z., G.T. and Xiaorui W. collected and analyzed the data. Xiaorui W. supervised the project. G.M., Z.S. and Xiaorui W. wrote the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Cancer thanks Susanne Gabrielsson, Young Pil Kim, Conroy Sun and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Dual tumour spatial distribution of NP1.
a,b, Representative TEM images of NP1 (a) and Ctrl-NP1 (b). Scale bars, 100 nm. c,d, Zeta-potentials recorded for NP1 (c) and Ctrl-NP1 (d). e,f, Size changes of NP1 (e) and Ctrl-NP1 (f) dispersed in water, PBS, or DMEM medium supplemented with 10% FBS at 4 °C at different times. g-i, CLSM images of MDA-MB-231 cells treated with NP1 (g) or Ctrl-NP1 (h,i) for 1 h. Scale bars, 10 μm. j-l, CLSM images of MDA-MB-231 cells after incubation with fresh medium containing 10% FBS and NP1 for 1 h. Scale bars, 20 μm in (j,k) and 50 μm in (l). m, CLSM images of MDA-MB-231 cells after incubation with NP1’ foe 1 h. Scale bar, 10 μm. The boxes shown the fields of (1 and 2) coexistence of cells and TEVs. n, CLSM images of MDA-MB-231 cells after incubation with NP1’ for 5, 15, 30, 60, or 180 min. Scale bar, 20 μm. o, Z-stack images of MDA-MB-231 cells after incubation with NP1’ for 1 h. Scale bar, 20 μm. p, Number-weighted size distribution of SEVs isolated from MDA-MB-231 cells by NTA after incubation with NP1 (SEVsNP1), Ctrl-NP1 (SEVsCtrl-NP1), or PBS (SEVs) for 1 h, followed by fresh medium for 8 h. q,r, The fluorescence spectra (q) and quantitative analysis (r) of SEVsNP1, SEVsCtrl-NP1, and SEVs. s, Number-weighted size distribution of LEVs isolated from MDA-MB-231 cells by NTA after incubation with NP1 (LEVsNP1), Ctrl-NP1 (LEVsCtrl-NP1), or PBS (LEVs) for 1 h, followed by fresh medium for 8 h. t,u, The fluorescence spectra (t) and quantitative analysis (u) of LEVsNP1, LEVsCtrl-NP1, and LEVs. v,w, Representative confocal fluorescence images for observing the colocalization of NP1 (red) with TEVs markers CD63 (green) (v) and TSG101 (green) (w), respectively. MDA-MB-231 cells were treated with NP1 for 1 h. The cell nuclei were stained with DAPI and are shown in blue. Scale bars, 5 μm. x, Excitation and emission fluorescence spectra of NP1BODIPY (NP1’) and NP1RhB (NP1). y, Time dependent fluorescence spectra change recorded for NP1BODIPY/RhB dispersed in PBS at 37 °C. z, FRET ratio (I580/I538) of NP1BODIPY/RhB in PBS at 37 °C. aa, CLSM images of MDA-MB-231 cells after incubation with NP1BODIPY/RhB for 1 h. Scale bars, 20 μm. In all experiments, the concentration of NPs was 0.1 g/L. In e,f,r,u,z, n = 3 biologically independent samples. Data are presented as the mean ± s.d. Statistical significance was calculated via unpaired two-tailed Student’s t-test (r,u). In a-aa, experiments were repeated three times independently with similar results; representative images are shown in a,b,g-o,v,w,aa.
Extended Data Fig. 2 Tumour-specific cellular uptake and TEVs localization of NP1.
a-d, CLSM examination of the cellular uptake and TEVs localization of NP1 in tumour cells, 4T1 (a), B16F10 (b), HepG2 (c), and PC9 (d), after 60 min of incubation. Scale bars, 10 μm. e,f, CLSM images of 4T1, B16F10 (e), HepG2, and PC9 (f) cells after incubation with fresh medium containing 10% FBS and NP1 for 1 h. Scale bars, 20 μm. g-i, CLSM examination of the cellular uptake and exocytosis behaviors of NP1 in non-tumour cells, NIH-3T3 (g), RAW264.7 (h), and CTLL-2 (i), after 60 min of incubation. Scale bars, 10 μm. j, Cellular uptake of NP1 and Ctrl-NP1 in MDA-MB-231, 4T1, B16F10, HepG2, PC9, NIH-3T3, RAW264.7, and CTLL-2 cells after 60 min of incubation determined by flow cytometry analyses. k, CLSM images of NIH-3T3, RAW264.7, and CTLL-2 cells after incubation with fresh medium containing 10% FBS and NP1 for 1 h. Scale bars, 20 μm. l, CLSM images of 4T1, B16F10, HepG2, PC9, NIH-3T3, RAW264.7, and CTLL-2 cells after incubation with fresh medium containing Ctrl-NP1 for 1 h. Scale bars, 20 μm. m-t, The binding constants and parameters of NP1 (palmitic acid-equiv. concentration: 5 mM) with the cell membranes (lipid-equiv. concentration: 1 mM) from different cells, including tumour cells, MDA-MB-231 (m), 4T1 (n), B16F10 (o), HepG2 (p), PC9 (q), and non-tumour cells, NIH-3T3 (r), RAW264.7 (s), and CTLL-2 (t), calculated from the ITC. u, Number-weighted size distribution of SEVs isolated from these different cells by NTA after NP1 treatment for 1 h, followed by fresh medium for 8 h. v, The fluorescence spectra of SEVs obtained from these different cells. w, Quantitative analysis of the fluorescence intensity of SEVs obtained from tumour cells, MDA-MB-231, 4T1, B16F10, HepG2, PC9, and non-tumour cells, NIH-3T3, RAW264.7, and CTLL-2 cells. x, Number-weighted size distribution of LEVs isolated from these different cells by NTA after NP1 treatment for 1 h, followed by fresh medium for 8 h. y, The fluorescence spectra of LEVs obtained from these different cells. z, Quantitative analysis of the fluorescence intensity of LEVs obtained from tumour cells, MDA-MB-231, 4T1, B16F10, HepG2, PC9, and non-tumour cells, NIH-3T3, RAW264.7, and CTLL-2 cells. aa, The fluorescence spectra of TEVs obtained from MDA-MB-231, 4T1, B16F10, HepG2, PC9, NIH-3T3, RAW264.7, and CTLL-2 cells after treatment with NP1 for 1 h followed by fresh medium for 8 h. All the protein concentrations of TEVs were 2 mg/mL. ab, Quantitative analysis of the fluorescence intensity of TEVs obtained from tumour cells, MDA-MB-231, 4T1, B16F10, HepG2, PC9, and non-tumour cells, NIH-3T3, RAW264.7, and CTLL-2 cells. In all experiments, the concentration of NP1 and Ctrl-NP1 was 0.1 g/L. In j,w,z,ab, n = 3 biologically independent samples. Data are presented as the mean ± s.d. Statistical significance was calculated via unpaired two-tailed Student’s t-test (j) and one-way ANOVA with Tukey’s multiple comparisons test (w,z,ab). In a-ab, experiments were repeated three times independently with similar results; representative images are shown in a-i,k,l.
xtended Data Fig. 3 The dual tumour spatial distribution function is unique to palmitic acid surface-displayed nanoparticles.
a,b, CLSM images of MDA-MB-231 cells after incubation with FP-RhB for 1 h. Scale bars, 50 μm. c, Schematic of the construction of nanoparticles with different fatty acids (acetic acid, SA; hexanoic acid, HA; decanoic acid, DA; palmitic acid, PA) displaying on their surface. d,e, The particle sizes (d) and zeta potentials (e) of NP1, NP4, NP5, and NP6. f, CLSM examination of the cellular uptake and exocytosis behaviors of NP1, NP4, NP5, and NP6 in MDA-MB-231 cells after 60 min of incubation. Scale bar, 50 μm. g, Quantification of the fluorescence intensity of MDA-MB-231 cells with different treatments. h, Quantitative analysis of the fluorescence intensity of TEVs obtained from MDA-MB-231 after treatment with NP1, NP4, NP5, or NP6 for 1 h, or without treatment (termed TEVs), respectively. The protein concentrations of TEVsNP1, TEVsNP4, TEVsNP5, TEVsNP6, and TEVs were 2 mg/mL. i, Schematic of the preparation of the traditional tumour-targeting nanoparticles, for example Ctrl-NP1@RGD. j,k, The particle size (j) and zeta potentials (k) of Ctrl-NP1 and Ctrl-NP1@RGD. l, CLSM examination of the cellular uptake of Ctrl-NP1 and Ctrl-NP1@RGD in MDA-MB-231 cells after 60 min of incubation. Scale bars, 50 μm. m, Quantification of the fluorescence intensity of MDA-MB-231 cells after treatment with Ctrl-NP1 or Ctrl-NP1@RGD for 1 h. n, 3D confocal Z-stack images of MDA-MB-231 cells treated with Ctrl-NP1@RGD for 1 h. Scale bar, 50 μm. In all experiments, the concentration of NPs was 0.1 g/L. In d,e,h,j,k, n = 3 biologically independent samples; in g,m, n = 4 biologically independent samples. Data are presented as the mean ± s.d. Statistical significance was calculated via one-way ANOVA with Tukey’s multiple comparisons test (g,h) and unpaired two-tailed Student’s t-test (m). In a-b,d-h,j-n, experiments were repeated three times independently with similar results; representative images are shown in a,b,f,l,n.
Extended Data Fig. 4 TEVs-mediated intercellular communications traced by NP1.
a, CLSM images of MDA-MB-231 cells after incubation with NP1 for 1 h in the absent (untreated) of FP. Scale bar, 10 μm. b, Cell viabilities of MDA-MB-231 cells after treatment with PBS (untreated control, Unt), wortmannin, cytochalasin D, sucrose, dynasore, and lipid raft inhibitors (MβCD and Nystatin) at 37°C, as well as PBS at 4 °C, respectively. c, Representative confocal fluorescence images for observing the colocalization of NP1 (red) with lipid raft marker CTxB (green). MDA-MB-231 cells were treated with NP1 for 1 h. Scale bar, 10 μm. d,e, Experimental schemes of transwell systems for co-culture of donor tumour cells (cells incubated with NP1 (d) or Ctrl-NP1 (e)) and recipient tumour cells. f, CLSM images of the uptake of TEVsNPs (TEVsNP1 or TEVsCtrl-NP1) by recipient tumour cells after co-incubation with donor tumour cells for 12 h. DAPI is used to stain nuclei. NP1 and Ctrl-NP1 are shown in red. Scale bars, 10 μm. g, Representative CLSM images of NIH-3T3 cells pretreated with NP1 for 1 h co-cultured with NIH-3T3EGFP cells for 4 h. Scale bar, 20 μm. The results showed that after 4 h of co-culture, both the fluorescence intensity of the donor cells (NIH-3T3 cells) and recipient cells (NIH-3T3EGFP cells) were very weak but observable, reflecting the inefficient cellular uptake by normal cells and inter-normal cell communications. h, Effect of GW4869 (one inhibitor of SEVs secretion, 10 μM) on the intercellular communication between MDA-MB-231 cells and MDA-MB-231EGFP cells observed by confocal microscopy. Scale bar, 5 μm. i, Statistical analysis of the relative MFI of MDA-MB-231EGFP cells after different treatments. In all experiments, the concentration of NP1 and Ctrl-NP1 was 0.1 g/L. In b, n = 4 biologically independent samples; in i, n = 3 biologically independent samples. Data are presented as the mean ± s.d. Statistical significance was calculated via one-way ANOVA with Tukey’s multiple comparisons test (b) and unpaired two-tailed Student’s t-test (i). In a-c,f-i, experiments were repeated three times independently with similar results; representative images are shown in a,c,f,g,h.
Extended Data Fig. 5 Enhanced cellular uptake and superior tumour inhibition of NP3.
a, TEM image of NP3. Scale bar, 100 nm. b, TEM and Cryo-TEM (inset) images of Ctrl-NP3. Scale bars, 100 nm. c, Size distribution and zeta-potential (inset) of Ctrl-NP3. d,e, Size changes of NP3 (c) and Ctrl-NP3 (d) dispersed in water, PBS, or DMEM medium supplemented with 10% FBS at different times. f, CLSM images of MDA-MB-231 cells after incubation with Ce6, Ctrl-NP3, or NP3 (Ce6-equiv. concentration: 3.5 μg/mL) for 1 h. Scale bar, 50 μm. g, CLSM examination of the cellular uptake and exocytosis behaviors of the NP3 after 60 min of incubation. Scale bars, 10 μm. The boxes shown the fields of (1 and 2) coexistence of cells and TEVs. h, CLSM images of DCFH-DA-stained MDA-MB-231 cells incubated with Ce6, Ctrl-NP3 or NP3 (Ce6-equiv. concentration: 3.5 μg/mL) for 1 h, followed by light irradiation for 1 min. Scale bars, 10 μm. i, CLSM images of DCFH-DA-stained 4T1 and B16F10 cells incubated with NP3 (Ce6-equiv. concentration: 3.5 μg/mL) for 1 h, followed by light irradiation for 1 min. Scale bars, 10 μm. j,k, Cell viabilities of MDA-MB-231 cells after treatment with Ce6, Ctrl-NP3, or NP3 in the absence of light irradiation (j) or Ce6, Ctrl-NP3, or NP3 in the presence of light irradiation for 2 min (k). l,m, Cell viabilities of 4T1 (l) and B16F10 (m) cells after treatment with PBS, Ce6, Ctrl-NP3, or NP3 (Ce6-equiv. concentration: 3.5 μg/mL) in the presence or absence of light irradiation for 2 min, respectively. n, Flow cytometry analysis for apoptosis of MDA-MB-231 cells treated with PBS, Ce6, Ctrl-NP3, or NP3 in the presence or absence of light irradiation for 2 min. The cells only incubated with PBS were employed as the control. o, Live/dead cell staining of MDA-MB-231 cells after treatment with PBS, Ce6, Ctrl-NP3, or NP3, in the presence or absence of light irradiation for 2 min, respectively. Scale bar, 100 μm. p,q, Western blot analysis of Lin28B, PD-L1, and TGF-β1 in MDA-MB-231 cells (p) and TEVs obtained from MDA-MB-231 cells (q) after treatment with PBS, Ctrl-NP3, or NP3, in the presence or absence of light, respectively. ‘+’ represented the addition of light irradiation for 2 min. r,s, NTA (r) and TEM (s) characterizations of the TEVs extracted and isolated from the culture supernatant of MDA-MB-231 cells after treatment with NP3 (L+) or without treatment. Scale bars, 500 nm. t, Relative change in number concentration of MDA-MB231-derived SEVs and LEVs after treatment. In all experiments, the PDT irradiation was performed using 660 nm laser at 50 mW/cm2. In d,e,t, n = 3 biologically independent samples; in j,k, n = 4 biologically independent samples; in l,m, n = 5 biologically independent samples. Data are presented as the mean ± s.d. Statistical significance was calculated via one-way ANOVA with Tukey’s multiple comparisons test (l,m) and unpaired two-tailed Student’s t-test (t). In a-t, experiments were repeated three times independently with similar results; representative images are shown in a,b,f-i,n-q,s.
Extended Data Fig. 6 Pharmacokinetics, biodistribution, and antitumour efficacy of NP3.
a, The blood clearance kinetics during 24 h post-intravenous administration of Ce6, Ctrl-NP3, and NP3 (Ce6-equiv. dose, 2.5 mg/kg), respectively. b-d, In vivo distribution of Ce6 (b), Ctrl-NP3 (c), and NP3 (d) in main organs and tumours during 24 h post-intravenous administration of Ce6, Ctrl-NP3, and NP3 (Ce6-equiv. dose, 2.5 mg/kg), respectively. e, In situ biodistribution of NP3 and Ctrl-NP3 in specific time points (6 h and 24 h) after intravenous injection into MDA-MB-231 tumour-bearing nude mice, at a Ce6 dose of 2.5 mg/kg, respectively. The white cycles indicate the tumour regions. f, Fluorescence of tumours at different time points. g, In situ biodistribution of Ce6 in specific time points (6 h and 24 h) after intravenous injection into MDA-MB-231 tumour-bearing nude mice, at a dose of 2.5 mg/kg. The white cycles indicate the tumour regions. h, Fluorescence of tumours at different time points. i, In situ biodistribution of Ce6, Ctrl-NP3 and NP3 in specific time points (6 h and 24 h) after intravenous injection into 4T1 tumour-bearing mice, at a dose of Ce6 2.5 mg/kg, respectively. The white cycles indicate the tumour regions. j, Fluorescence of tumours at different time points. k,l, Fluorescence images (k) and quantitative calculation (l) of tumour and different organs at 24 h after intravenous administration of NP3 or Ctrl-NP3 (Ce6-equiv. dose, 2.5 mg/kg). m,n, Fluorescence images (m) and quantitative calculation (n) of tumour and different organs at 24 h after intravenous administration of Ce6 at a dose of 2.5 mg/kg. o, Tumour inhibition rate of PBS (+), Ce6 (L-), Ctrl-NP3 (L-), NP3 (L-), Ce6 (L+), Ctrl-NP3 (L+), and NP3(L+) in MDA-MB-231 tumour-bearing mice model, respectively. p, Quantification of the percentages of TUNEL positive area in tumours with different treatments in MDA-MB-231 tumour-bearing mice model. Three random fields were observed for each mouse under the microscope. q, H&E staining images for histological analysis of major organs (heart, liver, kidney, and spleen) collected from MDA-MB-231 tumour-bearing mice in different treatment groups. Scale bars, 100 μm. r,s, Effect of the PDT therapy of NP3 on EV numbers in circulation in mice. r, 4T1 tumour-bearing BALB/c mice were treated with NP3 at a Ce6 dose of 2.5 mg/kg and 660 nm laser (200 mW/cm2, 5 min) on selected days post-inoculation. s, Relative change in EV numbers in circulation post NP3/light treatment, as measured by NTA. The results indicated that the total number of EVs in circulation remained consistent before and after NP3/light treatment. In a-j,m-n,p, n = 3 mice; in k,l, n = 1 mouse; in o,s, n = 4 mice. Data are presented as the mean ± s.d. Statistical significance was calculated via unpaired two-tailed Student’s t-test (f, h, j, o) and one-way ANOVA with Tukey’s multiple comparisons test (p, s). In q, the representative images are shown from three mice per group.
Extended Data Fig. 7 PDT therapy of NP3 for concurrent inhibition of primary and metastasis tumours in 4T1 tumour-bearing mice model.
a, Treatments schedule of the antitumour and anti-metastatic study. The 4T1 tumour-bearing BALB/c mice were intravenous (i.v.) administered with PBS, Ce6, Ctrl-NP3, or NP3, at a Ce6 dose of 2.5 mg kg−1. The groups of PBS (L+), Ce6 (L+), Ctrl-NP3 (L+), and NP3 (L+) were exposed to light irradiation (660 nm, 200 mW/cm2, 5 min) after 6 h post injection. The groups of PBS (L-), Ce6 (L-), Ctrl-NP3 (L-), and NP3 (L-) without light irradiation were used as controls. b, Primary tumour growth curves of tumour-bearing BALB/c mice after different treatments. c, Photographs of 4T1 tumours dissected from the mice on day 21 after exposure to different treatments. d, Tumour weight after indicated treatments. e, Tumour inhibition rate of PBS (+), Ce6 (L-), Ctrl-NP3 (L-), NP3 (L-), Ce6 (L+), Ctrl-NP3 (L+), and NP3(L+) in 4T1 tumour-bearing mice model, respectively. f, H&E staining and TUNEL assays of the excised tumour tissues from different groups. Scale bars, 200 μm. g, Optical images of lung tissues stained with Bouin’s solution and the H&E staining of lung tissues at the end of treatments. The areas pointed by the arrows were tumour metastasis nodules. h, Quantification of the percentages of TUNEL positive area in tumours with different treatments in 4T1 tumour-bearing mice model. Three random fields were observed for each mouse under the microscope. i, The calculated lung metastasis nodes of the BALB/c mice at the end of treatments. j, Dynamic body weights of tumour-bearing mice. In b-e,i,j, n = 4 mice; in h, n = 3 mice. Data are presented as the mean ± s.d. Statistical significance was calculated via one-way ANOVA with Tukey’s multiple comparisons test (b,d,e,h,i). In f,g, the representative images are shown from three mice per group.
Extended Data Fig. 8 PDT therapy of NP3 for concurrent inhibition of primary and metastasis tumours in B16F10 tumour-bearing mice model.
a, Therapeutic schedule of the antitumour and anti-metastatic study. b, Primary tumour volume curves of the B16F10 tumour-bearing C57BL/6 mice after treatment with PBS, Ce6, Ctrl-NP3, or NP3 (Ce6-equiv. dose, 2.5 mg/kg) in the presence or absence of light irradiation (660 nm, 200 mW/cm2, 5 min) over 10 days. c, Photographs of B16F10 tumours dissected from the mice at the end of treatments. d, Changes in the body weights of B16F10 tumour-bearing mice during different treatments. e, The mean tumour weight of B16F10 tumours from the mice at the end of treatments. f, Tumour inhibition rate of PBS (+), Ce6 (L-), Ctrl-NP3 (L-), NP3 (L-), Ce6 (L+), Ctrl-NP3 (L+), and NP3(L+) in B16F10 tumour-bearing mice model, respectively. g, Optical images and the H&E staining of lung tissues at the end of treatments. h, The calculated lung metastasis nodes of the C57BL/6 mice at the end of treatments. In b-f,h, n = 4 mice. Data are presented as the mean ± s.d. Statistical significance was calculated via one-way ANOVA with Tukey’s multiple comparisons test (b,e,f,h). In g, the representative H&E images are shown from three mice per group.
Extended Data Fig. 9 Disablement of the function of TEVs on promoting cancer cell metastasis and activating CAFs.
a, Representative microscopy images of B16F10 cells after a wound-healing assay. TEVs were isolated from B16F10 cells after treatment with PDT effect of Ce6, Ctrl-NP3, and NP3, respectively, along with controls (saline and TEVs), were incubated with B16F10 cells. Scale bar, 200 μm. b, Quantification of the wound healing rate from three independent biological samples. c, Migration assay schematic of B16F10 cells. TEVs were isolated from B16F10 cells after treatment with PDT effects of Ce6, Ctrl-NP3, and NP3, respectively, along with controls (saline and TEVs), were loaded in the lower chamber. d,e, Representative optical microscopy images (d) and quantitative analysis (e) of B16F10 cells after migration through a transwell. Scale bar, 50 μm. f, Trans-endothelial migration assay schematic of CFSE-labelled B16F10 (B16F10CFSE) cells. TEVs were isolated from B16F10 cells after treatment with PDT effects of Ce6, Ctrl-NP3, and NP3, respectively, along with controls (saline and TEVs), were loaded in the upper chamber. C166 cells, mouse endothelial cells. g,h, Representative CLSM images (g) and quantitative analysis (h) of B16F10CFSE cells after trans-endothelial migration through a transwell. Scale bar, 100 μm. i,j, Representative CLSM images (i) and quantitative analysis (j) of α-SMA-expressing CAFs (MC-6071m). Blue, cell nuclei; green, α-SMA. Scale bar, 50 μm. k, Representative microscopy images of CAFs after a wound-healing assay. TEVs were isolated from B16F10 cells after treatment with PDT effects of Ce6, Ctrl-NP3, and NP3, respectively, along with controls (saline and TEVs), were incubated with CAFs. Scale bar, 200 μm. l, Quantification of the wound healing rate from three independent biological samples. m, Migration assay schematic of CAFs. TEVs were isolated from B16F10 cells after treatment with PDT effects of Ce6, Ctrl-NP3, and NP3, respectively, along with controls (saline and TEVs), were loaded in the lower chamber. n,o, Representative optical microscopy images (n) and quantitative analysis (o) of CAFs after migration through a transwell. Scale bar, 100 μm. In b,e,h,j,l,o, n = 3 biologically independent samples, and data are presented as the mean ± s.d. Statistical significance was calculated via one-way ANOVA with Tukey’s multiple comparisons test. In all the data sets, similar results were observed in three independent experiments.
Extended Data Fig. 10 Immunosynergistic PDT therapy of NP3 via enhanced immune checkpoint blockade (ICB).
a, Schematic view of the treatment schedule of NP3 against primary and distant tumours. b, Changes in the body weights of 4T1 dual-tumour-bearing mice during different treatments. c, Primary tumour volume changes of the 4T1 tumour-bearing BALB/c mice after treatment with PBS, Ce6 (L+), Ctrl-NP3 (L+), NP3 (L+), αPD-L1, Ce6 (L+) + αPD-L1, Ctrl-NP3 (L+) + αPD-L1, and NP3 (L+) + αPD-L1 over 11 days. d,e, Sacrificed primary tumour images (d) and mean tumour weight (e) of the mice at the end of treatments. f, Tumour inhibition rate of primary tumours after treatment with PBS, Ce6 (L+), Ctrl-NP3 (L+), NP3(L+), αPD-L1, Ce6 (L+) + αPD-L1, Ctrl-NP3 (L+) + αPD-L1, and NP3(L+) + αPD-L1 over 11 days. g, Distant tumour volume changes of the 4T1 tumour-bearing BALB/c mice after treatment with PBS, Ce6 (L+), Ctrl-NP3 (L+), NP3(L+), αPD-L1, Ce6 (L+) + αPD-L1, Ctrl-NP3 (L+) + αPD-L1, and NP3(L+) + αPD-L1 over 11 days. h,i, Sacrificed distant tumour images (h) and mean tumour weight (i) of the mice at the end of treatments. j, Tumour inhibition rate of distant tumours after treatment with PBS, Ce6 (L+), Ctrl-NP3 (L+), NP3(L+), αPD-L1, Ce6 (L+) + αPD-L1, Ctrl-NP3 (L+) + αPD-L1, and NP3(L+) + αPD-L1 over 11 days. k-m, The percentages of dendritic cells (DCs) (k), cytotoxic T cells (CTLs) (l), and myeloid-derived suppressor cells (MDSCs) (m) infiltrating primary tumour tissues. n-p, The percentages of DCs (n), CTLs (o), and MDSCs (p) infiltrating distant tumour tissues. q, Illustration of concurrent inhibition of tumour growth and metastasis by a lipidated nanophotosensitizer tracing and disabling TEVs. After uptake by tumour cells, the TEVs-tracing nanophotosensitizer distributes both in cells (retaining in tumour cells) and TEVs (LEVs and SEVs). Through irradiating the primary tumour with 660 nm laser (NIR light), the lipidated nanophotosensitizer can not only kill the primary tumour cells via producing intracellular ROS, but also efficiently disable the TEVs-mediated communications via producing intra-TEVs ROS and destroying the Lin28B, PD-L1, and TGF-β1. The latter process prevents TEVs-mediated lung metastasis and restores T cell function, and enhances synergistic immunotherapy effects. In b-j, n = 4 mice; in k-p, n = 3 mice. Data are presented as the mean ± s.d. Statistical significance was calculated via one-way ANOVA with Tukey’s multiple comparisons test.
Supplementary information
Supplementary Information
Supplementary Tables 1 and 2, Figs. 1–33 and Note.
Supplementary Data
Source data provided for Supplementary Information.
Source data
Source Data Fig. 1
Statistical source data.
Source Data Fig. 2
Statistical source data.
Source Data Fig. 2
Unprocessed western blots.
Source Data Fig. 3
Statistical source data.
Source Data Fig. 4
Statistical source data.
Source Data Fig. 5
Statistical source data.
Source Data Fig. 6
Statistical source data.
Source Data Fig. 6
Unprocessed western blots.
Source Data Fig. 7
Statistical source data.
Source Data Fig. 8
Statistical source data.
Source Data Extended Data Fig. 1
Statistical source data.
Source Data Extended Data Fig. 2
Statistical source data.
Source Data Extended Data Fig. 3
Statistical source data.
Source Data Extended Data Fig. 4
Statistical source data.
Source Data Extended Data Fig. 5
Statistical source data.
Source Data Extended Data Fig. 5
Unprocessed western blots.
Source Data Extended Data Fig. 6
Statistical source data.
Source Data Extended Data Fig. 7
Statistical source data.
Source Data Extended Data Fig. 8
Statistical source data.
Source Data Extended Data Fig. 9
Statistical source data.
Source Data Extended Data Fig. 10
Statistical source data.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Miao, G., Shang, Z., Wang, X. et al. Concurrent inhibition of tumor growth and metastasis by a lipidated nanophotosensitizer tracing and disabling tumor extracellular vesicles. Nat Cancer 6, 1438–1457 (2025). https://doi.org/10.1038/s43018-025-00997-0
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s43018-025-00997-0