Abstract
Singapore’s rapidly aging population and increasing healthcare demands highlight the need for projections to inform policy planning. Here we adapted a previously published dynamic Markov microsimulation model, the Future Elderly Model, to estimate disease trajectories and healthcare expenditure among adults aged 51 years and older in Singapore. The model simulated four long-term lifestyle interventions aligned with the Healthier SG program from 2020 to 2050. Our projections indicate an increasing prevalence of chronic conditions, comorbidities, obesity and disabilities, with ethnic differences. The projected lifetime healthcare expenditure is the highest among Indians (US $93,900; 95% credible interval (CI), US $68,900–119,000), followed by the Chinese (US $75,700; 95% CI, US $57,600–93,800) and Malays (US $70,000; 95% CI, US $52,000–88,000). Despite having a higher chronic disease burden, Malays are expected to incur lower lifetime expenditure due to their shorter life expectancy. Implementing all 4 interventions could save US $505 million (95% CI, US $462–547 million) in healthcare use by 2050. Sustained lifestyle interventions may moderate the increase in future burdens. Policy strategies should prioritize preventive care tailored to the specific needs of diverse population subgroups.
Similar content being viewed by others
Main
The world’s older adult population continues to grow1. Globally, the proportion of older adults aged 65 years and above is estimated to increase from 10% in 2022 to 16% by 2050 (ref. 1), with the populations of East and Southeast Asia showing the fastest increase (from 13% in 2022 to 26% by 2050)1. The rapid growth of the older adult population increases the risk of chronic diseases and disabilities, reduces quality of life, and inflates healthcare expenses2. Singapore, a country with one of the highest life expectancies in the world (83.2 years as of 2019)3, faces health disparities among its multiethnic population.
The average life expectancy varies among ethnicities, with ethnic minorities tending to have a lower life expectancy4,5. Malays have a shorter life expectancy than Chinese individuals, with a gap of 5 years in 1965–2009 (ref. 6). The differences in mortality are due to multiple factors, such as a higher prevalence of lifestyle-related risk factors and chronic diseases among ethnic minorities6. According to a national survey in Singapore, smoking is more prevalent among Malays, and diabetes is more prevalent among Malays and Indians7.
With the demographic shift, policy planning is necessary to address the increasing disease burden and healthcare expenditure while considering ethnic differences. Over a decade, the Singapore government’s health expenditure has increased by more than 300% from Singapore $2.3 billion (US $1.7 billion) in 2007 to Singapore $9.8 billion (US $7.1 billion) in 2017 (ref. 8). In addition, 6% and 11% of the Ministry of Health’s operating expenditure in 2017 was spent on aged care and diabetes mellitus, respectively9. Developing a robust model to project the future prevalence of chronic diseases and disabilities, as well as future healthcare expenditure, is essential for health policy planning in a multiethnic society. A previous study provided projections on diabetes complications, guiding policymakers in the war on diabetes10. Although healthy lifestyles are known to be beneficial, most previous studies failed to model the long-term impacts of lifestyle interventions11,12,13,14. Among the studies that succeeded in this task, most were conducted in Western countries15,16,17.
Singapore, which has one of the world’s longest life expectancies and expects one in four citizens to be aged 65 years and older by 2030, is facing challenges18. Thus, evaluating the long-term influences of various interventions for Singapore’s fast-aging society is imperative. In this study, we used a dynamic Markov microsimulation model to project future health outcomes and expenditures by incorporating Singapore-specific sociodemographic covariates, transition probabilities and chronic diseases while also accounting for individual-level heterogeneity. A primary focus is investigating disparities and the impacts of long-term lifestyle interventions among the three main ethnic groups in Singapore.
Results
Regarding risk factors, we projected a decreasing trend in smoking prevalence overall and by ethnic groups. In 2050, Malays are projected to have the highest smoking prevalence of 13.1% (Fig. 1a), whereas the prevalence among the Chinese and Indians will be 5%. For obesity, in 2050, the Chinese are projected to show a relatively flat trend, with a prevalence of 20.7%; Malays and Indians are expected to share a similar increasing trend, both with a prevalence of above 50% (Fig. 1b).
a, Smoking prevalence. b, Obesity (body mass index ≥27.5 kg m−2) prevalence. The center point represents the mean, and the shaded area represents the 95% credible interval with a significance level of 5% based on a two-sided test.
We projected that chronic disease prevalence would increase from 2020 to 2050 as the cohort ages. Overall, diabetes prevalence is estimated to increase by 4.2% (Fig. 2a). The Chinese are projected to have the lowest prevalence (11.3%) in 2050 and the smallest increment. Although Malays and Indians are both estimated to have higher diabetes prevalence, the trend is steeper for Malays (Fig. 3a). Overall, hypertension prevalence will increase by approximately 4.5% (Fig. 2a). Malays and Indians will have a similar prevalence of 58% in 2050, much higher than that in the Chinese (35.5%) (Fig. 3b). Heart disease prevalence is predicted to show a slightly increasing trend for the overall population, the Chinese and Malays (all below 10%). Indians are projected to have the highest prevalence, more than double that in the other ethnic groups in 2050 (Figs. 2a and 3c). Stroke prevalence is projected to increase slightly, with minor ethnic differences (Figs. 2a and 3d). Among older adults aged 51 years and above, 50% are projected to have at least one chronic disease in 2050 (Fig. 2a). Chinese individuals are projected to have the lowest comorbidity prevalence of 43.2%, whereas Malays and Indians are predicted to show a prevalence of more than 70% (Fig. 3e).
a, Prevalence of chronic disease. b, Prevalence of any disability in ADLs and IADLs. ADL disability is defined as having any disability in dressing, feeding, toileting, washing, mobility and transferring. IADL disability is defined as having any disability in performing shopping tasks, making phone calls, managing money, taking transportation, preparing meals and doing household chores.
a, Diabetes. b, Hypertension. c, Heart disease. d, Stroke. e, Comorbidity. f, ADL disability. g, IADL disability. The center point represents the mean, and the shaded area represents the 95% credible interval with a significance level of 5% based on a two-sided test.
Disability prevalence is also projected to increase as the cohort ages (Fig. 2b). The prevalence of disabilities in activities of daily living (ADLs) will almost double in 30 years, with Malays and Indians showing similar increasing trends. Malays are predicted to have the highest disability prevalence of 14.0%, more than double that in the Chinese in 2050 (Fig. 3f). The prevalence of disabilities in instrumental ADLs (IADLs) is also projected to increase. Malays are predicted to have the highest prevalence of 37.8% in 2050, followed by the Indian and Chinese ethnic groups (Fig. 3g). Supplementary Fig. 1a–f shows the prevalence of chronic diseases, comparing the National Health Survey (1992–2010) data and Future Elderly Model (FEM) projections (2020–2050) for Singapore.
The lifetime healthcare costs for older adults aged 51 years and above are projected to be the highest among Indians (Fig. 4a). We assumed a 2% discount rate19. We projected that Malays would have the lowest lifetime total healthcare spending of US $70,000 with a 3% healthcare inflation. The Chinese are projected to spend US $5,700 (8.14%) more than Malays, whereas Indians are projected to spend the most, US $23,900 (34.1%) more than Malays (Fig. 4a). Similarly, Malays are projected to have the lowest lifetime primary healthcare costs (US $4,690). The Chinese will spend around US $100 more, and Indians will spend the most, over US $700 more than Malays (Fig. 4b). Supplementary Fig. 11 shows the annual healthcare cost under four inflation scenarios.
a, Total healthcare cost. b, Primary care cost. The center point represents the mean, and the black lines represent the 95% credible interval with a significance level of 5% based on a two-sided test. Ethnicity-specific sample sizes: Chinese (n = 1,291,402), Malay (n = 188,230) and Indian (n = 124,377).
Four intervention scenarios influenced the disease projections (Fig. 5). We projected that stroke prevalence would be reduced by less than 1% across the four interventions. Improved blood pressure (BP) management will have the largest impact in reducing stroke prevalence by 0.587%. Heart disease prevalence will be reduced by 0.713% to 1.33%, with ‘All’ interventions having the largest impact (resulting in a 1.33% reduction) (Fig. 5). Implementing these interventions could lead to healthcare cost savings by reducing the incidence of diseases (Fig. 6a). The fourth scenario (all interventions together) is expected to produce the largest total savings of US $505 million across 30 years, as it covers almost the entire population. Improved BP management has the least coverage, as it targets only the population with poor control of BP, and is predicted to save US $52.4 million (Fig. 6a). Supplementary Figs. 2–5 show the disease prevalence by ethnicity. Indians are projected to have the largest reduction in disease prevalence in all intervention scenarios. Supplementary Fig. 6 shows the healthcare cost savings by ethnicity. The Chinese are expected to save the most (US $349 million). Malays and Indians will have similar savings of around US $70 million.
The center point represents the mean, and the shaded area represents the 95% credible interval with a significance level of 5% based on a two-sided test. The prevalence differs by scenario because of the different eligible populations for the interventions.
a, Difference in healthcare spending. M, million. b, Life-year gains. c, ADL disability-free life-year gains. Intervention 1 targets 22.4% of the cohort (n = 366,649 persons with uncontrolled BP). Intervention 2 targets 72.2% of the cohort (n = 1,180,774 persons with lower PA levels). Intervention 3 targets 89.9% of the cohort (n = 1,470,382 persons with high sodium intake). Intervention 4 targets 98.1% of the cohort (n = 1,604,909 persons eligible for interventions 1–3). The center point represents the mean, and the black lines represent the 95% credible interval with a significance level of 5% based on a two-sided test.
At the individual level, among those with different health conditions between the respective intervention and control scenarios, we projected that the lifetime healthcare cost would be reduced by more than US $4,000 across scenarios (Extended Data Fig. 1). Physical activity (PA) intervention will produce the most savings (US $5,220, 4.90%). All four interventions will also increase the average life years and disability-free life years (Fig. 6b,c). PA intervention will have the greatest impact, adding 0.5 life year (Fig. 6b). Improved BP management will provide the longest disability-free life extension of 1.77 years (Fig. 6c). The proportion of individuals with different health conditions across the four intervention scenarios ranges between 2.89% (PA intervention) and 7.03% (all interventions together). Supplementary Fig. 7 shows the cost savings by ethnicity. Indians are predicted to save the most in the three individual intervention scenarios, among which PA intervention will have the greatest impact. Supplementary Fig. 8 demonstrates the average life years and ADL disability-free life years by ethnicity. The average life-year extension is projected to be the longest in Malays with PA intervention (0.611 years), significantly longer than that in Indians (0.450 years). The longest average ADL disability-free life-year gain is projected in Malays with improved BP management (1.920 years), with no ethnic differences observed.
Discussion
Risk factors
Our projections show significant disparities in risk factors among different ethnic groups in Singapore. While the overall smoking prevalence is projected to decrease, Malays are projected to maintain a persistently higher rate. Smoking is positively associated with the risk of hypertension, and the risk is amplified with age20. The proportion of people who smoke daily is the highest among Malays7, similar to our simulation. Being a previous or current smoker increases the risk of hypertension. Obesity is a risk factor for diabetes and hypertension among older adults21, and these conditions are the main drivers of the fast increase in prevalence projections for Malays and Indians. Similar obesity trends are reported in the National Population Health Survey in Singapore, where Malays and Indians have a higher obesity prevalence7 and are more prone to overweight or obesity22. These risk factors establish a concerning linkage with future chronic diseases.
Chronic disease trends
Due to population aging, the overall prevalence of chronic diseases is projected to be increasing. A similar increasing trend in diabetes prevalence was also reported in a previous study23. Malay and Indian older adults are projected to have a high prevalence of diabetes and hypertension in 2050. This trend can be partially attributed to the increasing obesity rates. Insulin resistance is often observed in individuals with hypertension, who are also at higher risk of developing diabetes than people with normal BP24. Hypertension is more frequently observed in individuals with diabetes24. People with type 2 diabetes are nearly 2.5 times more likely to have hypertension than their counterparts without diabetes25. Older adults with hypertension are more likely to be diagnosed with diabetes, partly explaining the higher prevalence of diabetes and hypertension in Malays and Indians in Singapore26. In addition, environmental and sociodemographic factors possibly contribute to ethnic disparities27. Disparities in diabetes prevalence are also found in other countries28,29.
Our simulation shows that the prevalence of heart disease will be the highest among Indians in 2050, partly driven by high diabetes and hypertension prevalence. Compared to Malay and Chinese individuals, Indians with diabetes are much more likely to develop ischemic heart disease than their counterparts without diabetes30. Similar findings suggest that the rates of myocardial infarction events are significantly greater for Indians than for Chinese individuals31. The Chinese had the lowest incidence of acute myocardial infarction from 2010 to 2020 and the oldest median age of onset of the disease32. Older age of onset delays the occurrence of the disease and potentially affects ethnic disparities. Among men, Asian Indians are at the highest risk of having coronary heart disease33. Other factors, including diabetes and hypertension, also add to the risk of coronary heart disease33. In addition, more Indians have abdominal obesity, insulin resistance, lower levels of high-density lipoprotein cholesterol, and glucose intolerance than Malay and Chinese people in Singapore34.
Comorbidity and disability
Comorbidities are projected to increase, with a higher prevalence in Malays and Indians. Other studies also report that comorbidities significantly increase with age and that Indians have a higher risk of physical disorders35,36. Ethnic disparities in comorbidities are also found in other countries37,38. The rising chronic disease prevalence not only indicates increasing public health challenges but also contributes to disabilities39. The prevalence of ADL disability is expected to nearly double. Malays and Indians have a higher prevalence of ADL and IADL disabilities. Compared to Chinese ethnicity, Malay and Indian ethnicities are reported to be associated with ADL disability40. Differences in health-related variables largely explain the difference in functional disability prevalence between Malay and Chinese individuals but do not sufficiently explain the higher rate in Indians40. Malay and Indian ethnicities are both associated with greater dependence on physical and cognitive IADLs compared to Chinese ethnicity41. Besides Malay and Indian ethnicities, old age, low education, a retired or homemaker status, and the presence of chronic illnesses are positively associated with disabilities in Singapore’s older adult population42. Disparities in disability prevalence among ethnic groups are also found in other countries43,44,45.
Healthcare cost
We simulated the healthcare cost across 30 years by ethnicity under four inflation scenarios. According to the Department of Statistics46, the overall inflation rate was 2.31% and the healthcare inflation rate was 1.13% in 2021. Although the healthcare inflation rate ranged from around 1% to less than 5% (ref. 46), the national health expenditure increased by 11% per year on average from 2006 to 2016 (ref. 47), and the medical cost inflation of Singapore was reported to be 10% in 2018 (ref. 48). The increasing prevalence of chronic diseases and the development of more advanced treatments propel the demand for healthcare and healthcare infrastructure, potentially driving medical inflation and overall expenditure49. The increasing number of third-party health insurers and the growth of insurance coverage encourage people to select more advanced and expensive solutions, resulting in a higher demand for healthcare and higher healthcare inflation49.
The lifetime healthcare costs are the highest in Indians due to prevalent chronic diseases and the lowest in Malays due to a shorter life expectancy6. The connection between high chronic disease prevalence and increased healthcare costs is evident, as resources are required to manage diseases. By highlighting the economic burdens, we underscore the need for policies that address the root causes of chronic diseases.
Intervention scenarios
In light of these findings, we assessed the impacts of four upstream interventions designed to mitigate the rising chronic disease prevalence and to aid policy decisions better. The Ministry of Health has been pushing for the development of programs and policies to shift focus from disease treatment to disease prevention and health promotion through the Healthier SG program, which encourages residents to engage with family doctors for better health and lifestyle50. We assessed the long-term effects of four intervention scenarios: (1) improved BP management, (2) increased PA, (3) sodium reduction and (4) all interventions. The control groups’ disease prevalences differ across scenarios due to different eligibilities. Among these interventions, scenarios 1 and 4 are projected to produce the greatest reduction in stroke and heart disease prevalence, respectively, and scenario 4 is expected provide the highest healthcare cost savings due to its broad coverage of the cohort. However, much of the observed cost savings arise not from widespread improvements in health outcomes or life extension but rather from the fact that most individuals do not experience significant changes in chronic conditions due to population aging. Only a small subset, approximately 3% to 7% of older adults, experience meaningful improvements in chronic disease status. It is also within this subgroup that we observe gains in both total life years and disability-free life years. Similar findings on healthy lifestyles also tend to be concentrated in specific subpopulations in other studies11,13,15,51,52. People with healthier diets, better cardiovascular health and fewer chronic diseases can have more life years free of cardiovascular diseases17,53,54,55. Indians are projected to have the greatest reduction in disease prevalence in all scenarios and the highest individual healthcare savings in the last three scenarios. Chronic diseases are projected to be more prevalent among Indians and incur the highest lifetime healthcare costs. Thus, Indians would have greater savings with interventions. Having a relatively shorter life expectancy6 and the highest ADL disability prevalence, Malays would benefit more in life-year and ADL disability-free life-year extensions with interventions. The implementation of these interventions could lead to substantial savings in healthcare costs, better health outcomes and longer lives.
In conclusion, while Malay and Indian older adults are projected to have a higher prevalence of chronic diseases and disabilities than Chinese older adults in Singapore, they are expected to experience larger impacts from interventions. Lifestyle interventions are projected to moderate the rise of chronic disease burdens and healthcare costs, while marginally extending life and disability-free life years for a small proportion of individuals. Such interventions may produce more benefits for society if they are initiated at younger ages, providing a greater opportunity to delay or prevent hypertension and diabetes. Nevertheless, programs targeting high-risk groups may be more sustainable and cost-effective in the long run56. The costs of running such public health interventions may be partially offset by healthcare savings from delaying diseases. By prioritizing preventive strategies, ethnic disparities could be addressed more effectively. This study provides a concrete step toward a policy discussion on the ethnic disparities of healthcare financing, presents an assessment of the benefits of long-term lifestyle interventions in Singapore and contributes valuable insights to aging research in the broader region.
Implications
The implications of our study are relevant to policymakers. Our study emphasizes the necessity of planning for the growing disease burden due to population aging. Moreover, our study demonstrates disparities in trends and costs among different ethnic groups in Singapore and assesses the long-term impacts of interventions in preventing diseases and reducing healthcare costs. Healthcare policies could alter the trajectory of comorbidities and moderate the rise of future burdens. Actions are needed to address poor management of chronic diseases (such as hypertension), lack of PA or high-sodium diets and to reduce disparities. Our analysis showed that lifestyle interventions may moderate the increase in healthcare costs and extend both overall life years and disability-free life years, with minority ethnic groups benefiting more. Our results are not only relevant for older adults in Singapore but also offer broader insights that are applicable globally. By incorporating these preventive measures, our study shows a more compelling and actionable framework for managing chronic disease burden and healthcare spending in aging populations worldwide.
In Singapore, the government has been focusing more on health promotion and health programs, such as Healthier SG, to prioritize the prevention of diseases50. Promoting screening of chronic diseases, prohibiting smoking in designated public areas57, and introducing public policies to raise awareness of the prevention and management of diabetes have been enacted to delay chronic diseases and disabilities58. A workgroup was formed by the Ministry of Health59 in 2021 to help ethnic minority groups gain better health by designing culturally beneficial interventions60. The interventions targeted the cause of poor health among minorities and were recommended to reduce health disparities. The Health Promotion Board61 also organizes a PA initiative to encourage Singapore residents to be more physically active. Multifactorial, culturally tailored interventions may improve care for ethnic minorities62. In the United States, culturally tailored smoking cessation intervention was found to be more effective for Koreans63, suggesting that effective programs need to be sensitive to cultural differences. The policy scenarios discussed above, as well as other potential longer-term changes in financing and service delivery models, will be further investigated with our Singapore FEM as more data on specific financing mechanisms become available.
Limitations
The model assumes that the current healthcare delivery model and treatment patterns will stay the same in the future. The FEM does not incorporate possible future advancements, such as treatment innovation or extensive screening programs, which could alter health trajectories and expenditures. Moreover, migration was not modeled, as existing policies in Singapore largely support short-term instead of permanent migration. The transitional models were estimated with a 6-year follow-up based on the Singapore Multi-Ethnic Cohort (MEC) survey data, which may not capture short-term changes in health status. Our spending projection also excludes long-term care, which is expected to increase as lifespan increases and the population ages with more chronic diseases and disabilities. Hence, the actual total cost is likely underestimated. Furthermore, we did not account for indirect costs, such as productivity loss at work and reduction in quality of life due to disabilities64. Future models should consider a broader set of expenditures and incorporate empirical evidence when it becomes available. Routine model refinements and policy evaluation will help maintain the relevance and accuracy of the projections of Singapore’s evolving demographics.
Although we found no significant ethnic-specific patterns in missing data, we acknowledge that some degree of bias cannot be entirely ruled out.
Additionally, we assume full adherence to interventions, although real-world adherence is possibly affected by a lack of motivation, socioeconomic limitations, poor awareness and time constraints65. Hence, our assumption of full adherence likely overestimates the intervention impacts in practice. Future research should consider varying adherence rates to reflect real-world conditions better.
While we modeled ethnic-specific differences in disease prevalence, there was a lack of data on the differential impact of interventions and relative risk reductions by ethnic groups. This may lead to an underestimation of ethnic variations in intervention impacts, which could partly explain the lack of significant differences across ethnicities. Future research on the effectiveness of ethnic-specific interventions may help address this gap.
Conclusion
This study focused on modeling health status and healthcare costs for three major ethnic groups and simulated the impacts of upstream lifestyle interventions, providing an overall understanding of ethnic disparities and the impacts of population-level health-promoting programs, such as Healthier SG. The FEM’s approach allows for this multidimensional characterization of health status to project the chronic disease and disability prevalence and lifetime healthcare spending among older adults.
Methods
Ethical approval for this study was obtained from the Institutional Review Board of the National University of Singapore (NUS-IRB-2022-582).
Data
The Singapore MEC study was a population-based prospective cohort study that surveyed the demographics, health status and behaviors of 14,465 participants aged 21–94 years (mean age, 46 ± 13 years). Participants were recruited between January 2004 and November 2010 and followed up between January 2011 and December 2016. The cohort consisted of 47% Chinese, 26% Malay and 27% Indian participants66. The MEC is a good representation of ethnic groups in Singapore and was designed to study ethnic differences in chronic disease risk66. The MEC was then reweighted to reflect older adults in Singapore in 2020, allowing us to model long-term health trajectories and ethnic disparities in Singapore.
The Well-being of the Singapore Elderly (WiSE) survey was an epidemiological survey conducted nationwide to help understand the burden of dementia and mental illnesses in older adults in Singapore67,68. We used the WiSE dataset to estimate the healthcare costs of older adults, adjusting for age, sex, ethnicity, education level and chronic diseases.
The Singapore Longitudinal Aging Study (SLAS) interviewed participants aged 55 years and older from 2003 to 2005 (ref. 69). The SLAS included disability information, where functional disability data on ADL and IADL disability prevalence were used to supplement the MEC.
Microsimulation model
The FEM is a microsimulation model accounting for population aging based on population dynamics and disease transitions. Adapting the FEM, we projected future health conditions and healthcare costs (primary care and hospitalization) for the three main ethnic groups in Singapore: Chinese, Malays and Indians. Primary healthcare costs cover polyclinic (public clinic) and general practitioner (private clinic) costs. Total healthcare costs include both primary healthcare costs and hospitalization costs. Overall, Chinese individuals made up 74.3% of the resident population, followed by Malays at 13.5% and Indians at 9% (ref. 70). The FEM allowed heterogeneity by modeling individual-level data.
The core features of the microsimulation model to project future health status and healthcare expenditure for three ethnic groups in Singapore were as follows: (1) projecting ethnic-specific individual-level cohorts; (2) projecting individuals from a baseline cohort over time and evaluating ethnic disparities in outcomes; and (3) replenishing the baseline cohort with incoming populations aged 51–56 years. Individuals moved forward in time by transiting to new health states probabilistically, with their health status and healthcare utilization observed at the end of each simulation cycle. During the simulation, individuals exited the model at the time of death. Therefore, the model lost some older adults at each cycle due to death, while replenishing cohorts were added to the population at the same time.
The FEM simulation was implemented in C++ for computational efficiency. We assumed that there is no gain in population due to immigration among older adults. Bootstrapping processes were conducted to obtain different sets of transitional models based on each sample to obtain 95% credible intervals. In line with the RAND Corporation’s study of the Future Adult Model, a sister model of the FEM, 50 rounds of bootstrapping were applied, and each set of transitional models estimated using the bootstrap sample was simulated 100 times in our study71.
Basic covariates
All chronic disease transitional models were adjusted for variables that do not vary over time (that is, sex, ethnicity, marital status, highest attained education) and variables that vary over time (age, body mass index, income level and smoking status).
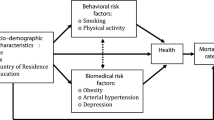
Health transition model
The FEM uses a discrete piecewise linear hazard model on longitudinal data to project health transitions. The hazard of acquiring a disease (hypertension, diabetes, heart disease and stroke), developing any disability, or dying was dependent on various risk factors. The transitional model covariates included the set of basic covariates and lagged chronic disease conditions determined using a mixed stepwise selection algorithm. We used probit regression to estimate the probability of transition to each health condition based on the outcome variable, controlling for demographics and comorbidities in the previous period. Probit regression is commonly used for chronic disease modeling in FEM studies72,73,74. The transitional models are listed in Supplementary Table 1. The questions asked in the MEC survey have the following format: “Have you ever been told by a doctor that you have … (for example, diabetes)?”. All independent variables were measured with a 6-year lag in the MEC. Diseases in our study were assumed to be absorbing states; thus, the transition probabilities were estimated in older adults who did not have a specific condition at the previous survey wave. We adopted the Asian body mass index cutoff (27.5 kg m−2) for obesity75.
Disability model
We used the SLAS to build disability models with sociodemographic covariates and the previous state’s chronic disease status. ADL disability status was defined as having any disability in tasks such as dressing, feeding, toileting, washing, mobility and transferring76. IADL disability was defined as having a disability in performing shopping tasks, making phone calls, managing money, taking transportation, preparing meals and doing household chores. Probit regression was used for any ADL or IADL disability, adjusting for risk factors.
Spending model
We used costs from the WiSE study to model the annual healthcare expenditure before government subsidy. We multiplied each service unit, such as the consultation minutes and number of visits, by the unit cost price for the healthcare costs over 3 months and multiplied the value by 4 to obtain the annual cost. Due to variations in local data, an extrapolation method in which UK unit cost data were used to estimate Singapore unit costs (primary and hospital doctors and hospital healthcare workers) was applied. Ratios between Singapore and the UK were generated from the WHO-CHOICE (World Health Organization Choosing Interventions that are Cost-Effective) database77. The Unit Cost of Health and Social Care 2013 (ref. 78) was used as a reliable source of UK unit costs. The cost ratio between the UK and Singapore remains unchanged. The average out-of-pocket expenditures were used when UK unit costs were unavailable. This method was applied by the Institute of Mental Health under the Ministry of Health to estimate the costs of dementia and depression for the Singapore government79,80.
Two-part models, with the first part being probit regression and the second part being a generalized linear model, were built to estimate the influence of multiple covariates on costs. We chose generalized linear models because they accept the non-normal distribution of the response variable. We converted the projected nominal expenditure (in Singapore dollars) to real spending based on the healthcare inflation rate from the consumer price index (CPI)46. With a 2% discount rate19, we subsequently assumed three inflation scenarios: (1) a mean annual inflation rate of 1%, close to the rate calculated from the CPI healthcare component of 2017–2021 (ref. 46); (2) a mean annual inflation rate of 3%; and (3) a mean annual inflation rate of 4.5%, similar to the highest rate (4.36%) from 2011 to 2021, calculated from the CPI healthcare component46. We applied the FEM to estimate the longitudinal expenditure based on an individual’s characteristics and chronic diseases. Projections of lifetime healthcare costs were obtained by tracking individual older adults from 2020 to 2050. All expenditures were in 2022 US dollar values, with an average exchange rate of Singapore $1 to US $0.7253 in 2022 (ref. 81).
Comorbidity
In our study, comorbidity was defined as having any of the following chronic diseases: diabetes, hypertension, stroke and heart disease.
Intervention scenarios
Healthier SG, a national program implemented by the Ministry of Health, started enrolling older adults in July 2023 to shift focus from treating diseases to providing preventative care50,82. Singapore residents are encouraged to see a family doctor for better chronic care and healthier lifestyles50. Specifically, social interventions, such as increased PA and a healthier diet, will be prescribed. We simulated four intervention scenarios from the Healthier SG50 program to bend the curves on chronic diseases and savings in healthcare costs. We incorporated the available ethnic differences where possible:
-
1.
Improved BP management intervention
-
2.
Increased PA intervention
-
3.
Sodium reduction intervention
-
4.
All of the above interventions
Improved BP management (intervention 1)
Intervention 1 focuses on better BP management among individuals with hypertension. Hypertension is a prevalent disease among Singapore’s older adults, and well-managed BP effectively reduces the risk of cardiovascular diseases83. In Healthier SG, residents are encouraged to engage with a family doctor who provides improved care for chronic diseases50. Hence, we designed this intervention to simulate the impact of better BP management on the long-term effects of stroke and heart disease risk among individuals with hypertension. According to a local study, 62.1% of Chinese, 80.0% of Malay and 71.9% of Indian individuals with treated hypertension had uncontrolled BP84. Applying ethnic-specific proportions, individuals with hypertension were considered eligible for this intervention. A 35% risk reduction in stroke incidence and a 20% risk reduction in heart disease incidence83 were applied. No mortality reduction was assumed for this intervention.
Increased PA (intervention 2)
Intervention 2 was used to investigate the effects of increasing PA in reducing chronic disease prevalence. In Healthier SG, family doctors can prescribe lifestyle interventions such as activities to encourage the residents to be more physically active. Muscle-strengthening exercises have been shown to improve cardiometabolic health, decrease feelings of depression, and increase bone density and skeletal muscle strength85. The National Health Survey 2022 (ref. 86) reports that 71.2% of Singapore residents aged 60–74 years engage in insufficient muscle-strengthening activities. The population with lower PA was considered eligible and assumed to perform no muscle-strengthening exercises. A 17% risk reduction in stroke, heart disease and diabetes incidence was applied to the eligible population based on a recent muscle-strengthening exercise study12. No mortality reduction was assumed for this intervention.
Sodium reduction (intervention 3)
Intervention 3 simulated the effects of reducing dietary sodium intake in preventing chronic diseases, with 90% of Singapore residents exceeding the recommended sodium intake87. In Healthier SG, digital technology such as Healthy 365 is used to provide further support on maintaining a healthy diet50, in addition to guidance from family doctors. Long-term dietary sodium intake reduction decreases the risk of hypertension by 18% and cardiovascular diseases by 30% (ref. 88). We applied a risk reduction of 18% in hypertension, 30% in stroke and 30% in heart disease to the eligible population (90% of Singapore residents)88. No mortality reduction was assumed for this intervention.
All interventions (intervention 4)
Intervention 4 simulated the effects of applying improved BP management, increased PA and sodium reduction together. In Healthier SG, residents are guided to be more physically active, to adopt healthier diets and to control chronic diseases better50. Hence, this scenario was used to investigate the health outcomes with multiple interventions applied concurrently. The inclusion criterion was being eligible for at least one intervention, which applies to around 98% of the entire population. The incidence risk reductions were assumed to be the largest effect of all interventions: 17% for diabetes, 18% for hypertension, 30% for stroke and 30% for heart disease. A lower relative risk for stroke was taken from sodium reduction (relative risk = 0.7) instead of improved BP management (relative risk = 0.65), as the sodium reduction intervention covers 90% of the population. No mortality reduction was assumed for this intervention.
In summary, the above four intervention scenarios target different groups of at-risk individuals based on their unique health profiles and lifestyle factors. Those with hypertension are prime candidates for improved BP management interventions, focusing on medication adherence and monitoring to prevent cardiovascular complications. Individuals leading sedentary lifestyles or at risk for obesity and type 2 diabetes would benefit the most from increased PA interventions, aimed at promoting regular exercise to improve overall health. For people with diets high in salt, a sodium reduction intervention is crucial in lowering sodium intake to manage BP. In a population setting, as there are different at-risk individuals, we applied all three interventions to different at-risk groups in the last scenario, where each group received relative risk reduction from one of the interventions. The combined approach covered the largest proportion of the population, with different at-risk groups benefiting accordingly.
Statistics and reproducibility
This study used MEC data. No statistical method was used to predetermine the sample size. Observations in individuals under the age of 51 years were excluded as this study focused on older adults. In the original MEC cohort, exclusions occurred in self-assessment during recruitment. Thus, the exact exclusion number was not recorded. No statistical software was used for data collection.
Transitional models were estimated using linear regression, probit regression, ordered probit regression and two-part models. Covariates included a set of basic variables and health conditions determined by the mixed stepwise algorithm, which conducted forward selection (P < 0.05) and backward elimination (P > 0.15) to select relevant risk factors. Analysis in this study was conducted using R version 4.3.3 and Stata 15.1. The distribution of continuous variables was assumed to be normal but was not formally tested.
As the MEC was a cohort study in which we observed individuals’ behaviors and disease trajectories over time, randomization and blinding do not apply. There were no experiments on MEC participants; thus, data collection and analysis were not blinded.
Informed consent was obtained from all participants at the time of the original data collection, and participants were compensated according to the protocols approved by the institutional review board. No new data were collected, and no direct contact with participants occurred in this study.
No statistical methods were used to predetermine sample sizes, but our sample sizes are similar to those reported in a previous publication using the Singapore MEC66.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
For confidentiality reasons, the datasets are not publicly available. The MEC dataset is available through the Saw Swee Hock School of Public Health (email: SSHSPHDataRequest@nus.edu.sg) upon reasonable request. Researchers interested in MEC data must submit a data request form. Data requests are reviewed by the Singapore Population Health Studies Scientific Committee, and ethics approval is required for research. An access fee may be applied to the data concierge. For WiSE (https://www.imh.com.sg/Research/Research-Programmes/Pages/Well-being-of-the-Singapore-Elderly-WiSE.aspx) and SLAS (https://www.cheba.unsw.edu.au/consortia/cosmic/studies/slas), requests for data access can be directed to the corresponding author, who can help facilitate the process with the data-owning institution upon reasonable request. The WHO-CHOICE (https://www.who.int/publications/m/item/who-choice-estimates-of-cost-for-inpatient-and-outpatient-health-service-delivery) is publicly available77. Source data are provided with this paper.
Code availability
The code used for estimating transitional models in this study is deposited on GitHub at https://github.com/GXueying/FEM-models/tree/main to share with the community.
References
World Population Prospects 2022: Summary of Results UN DESA/POP/2022/TR/NO. 3 (Population Division, Department of Economic and Social Affairs, United Nations, 2022).
Centers for Disease Control and Prevention. Trends in aging—United States and worldwide. MMWR Morb. Mortal. Wkly. Rep. 52, 101–104, 106 (2003).
Life Expectancy at Birth (Years) (World Health Organization, 2023); www.who.int/data/gho/data/indicators/indicator-details/GHO/life-expectancy-at-birth-(years)
Silva, A., Saiyed, N. S., Canty, E. & Benjamins, M. R. Pre-pandemic trends and Black:White inequities in life expectancy across the 30 most populous U.S. cities: a population-based study. BMC Public Health 23, 2310 (2023).
Juan, S.-C., Awerbuch-Friedlander, T. & Levins, R. Ethnic density and mortality: aboriginal population health in Taiwan. Public Health Rev. 37, 11 (2016).
Lim, R. B. T. et al. Ethnic and gender specific life expectancies of the Singapore population, 1965 to 2009—converging, or diverging? BMC Public Health 13, 1012 (2013).
National Population Health Survey 2020 (Household Interview and Health Examination) (Policy, Research & Surveillance Group, Epidemiology & Disease Control Division, Ministry of Health and Health Promotion Board of Singapore, 2020).
Government Health Expenditure and Healthcare Financing (Ministry of Health of Singapore, 2022).
Percentage of Spending on Mental Health, Diabetes and Ageing Versus Total Healthcare Spending in 2018 Against Amount Budgeted for 2019 (Ministry of Health of Singapore, 2019).
Tan, K. W., Dickens, B. S. L. & Cook, A. R. Projected burden of type 2 diabetes mellitus-related complications in Singapore until 2050: a Bayesian evidence synthesis. BMJ Open Diabetes Res. Care 8, e000928 (2020).
Reimers, C. D., Knapp, G. & Reimers, A. K. Does physical activity increase life expectancy? A review of the literature. J. Aging Res. 2012, 243958 (2012).
Momma, H., Kawakami, R., Honda, T. & Sawada, S. S. Muscle-strengthening activities are associated with lower risk and mortality in major non-communicable diseases: a systematic review and meta-analysis of cohort studies. Br. J. Sports Med. 56, 755–763 (2022).
Li, Y., Tang, Y., Xie, Y., Liu, H. & Wu, H. Association of healthy lifestyle with life expectancy free of five major disabilities in Chinese older adults. J. Glob. Health 14, 04034 (2024).
Messerli, F. H. et al. Sodium intake, life expectancy, and all-cause mortality. Eur. Heart J. 42, 2103–2112 (2021).
Mehta, N. & Myrskylä, M. The population health benefits of a healthy lifestyle: life expectancy increased and onset of disability delayed. Health Aff. https://doi.org/10.1377/hlthaff.2016.1569 (2017).
Li, Y. et al. Healthy lifestyle and life expectancy free of cancer, cardiovascular disease, and type 2 diabetes: prospective cohort study. BMJ 368, l6669 (2020).
Lagström, H. et al. Diet quality as a predictor of cardiometabolic disease-free life expectancy: the Whitehall II cohort study. Am. J. Clin. Nutr. 111, 787–794 (2020).
Population in Brief 2023 (Strategy Group, National Population and Talent Division, Prime Minister’s Office of Singapore, 2023).
Original Maturity: 30 Year or More (Monetary Authority of Singapore, 2020).
Gao, K., Shi, X. & Wang, W. The life-course impact of smoking on hypertension myocardial infarction and respiratory diseases. Sci. Rep. 7, 4330 (2017).
Salihu, H. M., Bonnema, S. M. & Alio, A. P. Obesity: what is an elderly population growing into? Maturitas 63, 7–12 (2009).
Fauziana, R. et al. Body mass index, waist–hip ratio and risk of chronic medical condition in the elderly population: results from the Well-being of the Singapore Elderly (WiSE) Study. BMC Geriatr. 16, 125 (2016).
Wong, L. Y., Toh, M. P. H. S. & Tham, L. W. C. Projection of prediabetes and diabetes population size in Singapore using a dynamic Markov model. J. Diabetes 9, 65–75 (2017).
Petrie, J. R., Guzik, T. J. & Touyz, R. M. Diabetes, hypertension, and cardiovascular disease: clinical insights and vascular mechanisms. Can. J. Cardiol. 34, 575–584 (2018).
Gress, T. W., Nieto, F. J., Shahar, E., Wofford, M. R. & Brancati, F. L. Hypertension and antihypertensive therapy as risk factors for type 2 diabetes mellitus. Atherosclerosis Risk in Communities Study. N. Engl. J. Med. 342, 905–912 (2000).
Seow, L. S. E., Subramaniam, M., Abdin, E., Vaingankar, J. A. & Chong, S. A. Hypertension and its associated risks among Singapore elderly residential population. J. Clin. Gerontol. Geriatr. 6, 125–132 (2015).
LaVeist, T. A., Thorpe, R. J. Jr, Galarraga, J. E., Bower, K. M. & Gary-Webb, T. L. Environmental and socio-economic factors as contributors to racial disparities in diabetes prevalence. J. Gen. Intern. Med. 24, 1144–1148 (2009).
Ojo, O. Diabetes in ethnic minorities in UK: the role of diet in glucose dysregulation and prevalence of diabetes. J. Food Nutr. Disord. https://doi.org/10.4172/2324-9323.1000110 (2013).
McBean, A. M., Li, S., Gilbertson, D. T. & Collins, A. J. Differences in diabetes prevalence, incidence, and mortality among the elderly of four racial/ethnic groups: whites, Blacks, Hispanics, and Asians. Diabetes Care 27, 2317–2324 (2004).
Yeo, K. K. et al. Ethnicity modifies the association between diabetes mellitus and ischaemic heart disease in Chinese, Malays and Asian Indians living in Singapore. Diabetologia 49, 2866–2873 (2006).
Mak, K.-H. et al. Ethnic differences in acute myocardial infarction in Singapore. Eur. Heart J. 24, 151–160 (2003).
Singapore Myocardial Infarction Registry Annual Report 2020 (National Registry of Diseases Office, Health Promotion Board of Singapore, 2020).
Lee, J. et al. Risk factors and incident coronary heart disease in Chinese, Malay and Asian Indian males: the Singapore Cardiovascular Cohort Study. Int. J. Epidemiol. 30, 983–988 (2001).
Hughes, K., Aw, T. C., Kuperan, P. & Choo, M. Central obesity, insulin resistance, syndrome X, lipoprotein(a), and cardiovascular risk in Indians, Malays, and Chinese in Singapore. J. Epidemiol. Community Health 51, 394–399 (1997).
Chong, S. A., Abdin, E., Nan, L., Vaingankar, J. A. & Subramaniam, M. Prevalence and impact of mental and physical comorbidity in the adult Singapore population. Ann. Acad. Med. Singap. 41, 105–114 (2012).
Abdin, E. et al. Changes in the prevalence of comorbidity of mental and physical disorders in Singapore between 2010 and 2016. Singapore Med. J. 63, 196–202 (2022).
Erving, C. L. Physical–psychiatric comorbidity: patterns and explanations for ethnic group differences. Ethn. Health 23, 583–610 (2018).
Erving, C. L. Physical–psychiatric comorbidity: implications for health measurement and the Hispanic epidemiological paradox. Soc. Sci. Res. 64, 197–213 (2017).
Maresova, P. et al. Consequences of chronic diseases and other limitations associated with old age—a scoping review. BMC Public Health 19, 1431 (2019).
Ng, T.-P., Niti, M., Chiam, P.-C. & Kua, E.-H. Prevalence and correlates of functional disability in multiethnic elderly Singaporeans. J. Am. Geriatr. Soc. 54, 21–29 (2006).
Ng, T.-P., Niti, M., Chiam, P.-C. & Kua, E.-H. Physical and cognitive domains of the instrumental activities of daily living: validation in a multiethnic population of Asian older adults. J. Gerontol. A 61, 726–735 (2006).
Mahesh, M. et al. Disability in Singapore’s elderly population. Ann. Acad. Med. Singap. 45, 284–296 (2016).
Ran, L. et al. Comparison of health-related quality of life between the Han and Yi ethnicity elderly in the Yi autonomous areas of Yunnan Province. BMC Geriatr. 19, 326 (2019).
Melvin, J., Hummer, R., Elo, I. & Mehta, N. Age patterns of racial/ethnic/nativity differences in disability and physical functioning in the United States. Demogr. Res. 31, 497–510 (2014).
Franse, C. B. et al. Ethnic differences in frailty: a cross-sectional study of pooled data from community-dwelling older persons in the Netherlands. BMJ Open 8, e022241 (2018).
Tables on CPI and Percentage Changes up to Class Level and Average Retail Prices of Selected Consumer Items (Department of Statistics of Singapore, 2023).
Healthcare Inflation (Ministry of Health of Singapore, 2018); moh.gov.sg/news-highlights/details/healthcare-inflation
Ng, R. J. Singapore 2018 healthcare cost inflation hits 10%, 10 times the economic inflation rate: Mercer report. The Business Times (10 June 2019); www.businesstimes.com.sg/international/singapore-2018-healthcare-cost-inflation-hits-10-10-times-economic-inflation-rate
Cheow, S.-A. Insurance linked to high medical inflation: experts. The Straits Times (28 June 2019); www.straitstimes.com/singapore/health/insurance-linked-to-high-medical-inflation
White Paper on Healthier SG (Ministry of Health of Singapore, 2022).
McPhee, J. S. et al. Physical activity in older age: perspectives for healthy ageing and frailty. Biogerontology 17, 567–580 (2016).
Gregg, E. W. et al. Impact of intensive lifestyle intervention on disability-free life expectancy: the Look AHEAD study. Diabetes Care 41, 1040–1048 (2018).
Rapsomaniki, E. et al. Blood pressure and incidence of twelve cardiovascular diseases: lifetime risks, healthy life-years lost, and age-specific associations in 1.25 million people. Lancet 383, 1899–1911 (2014).
Xia, X. et al. Cardiovascular health and life expectancy with and without cardiovascular disease in the middle-aged and elderly Chinese population. BMC Public Health 23, 2528 (2023).
Wilkins, J. T. et al. Lifetime risk and years lived free of total cardiovascular disease. JAMA 308, 1795–1801 (2012).
Bouchard, D. R., Baillargeon, J.-P. & Langlois, M.-F. The independent effect of age groups on the effectiveness of lifestyle intervention. Curr. Obes. Rep. 2, 107–119 (2013).
Smoking Prohibition (National Environment Agency of Singapore, 2025); www.nea.gov.sg/our-services/smoking-prohibition/overview
War on Diabetes (Ministry of Health of Singapore, 2024); www.moh.gov.sg/others/public-consultation/war-on-diabetes
Collection of Data by Working Group on Health for Ethnic Minorities to Examine Root Causes of Poor Health in Such Communities (Ministry of Health of Singapore, 2021).
Collection of Data by Working Group on Health for Ethnic Minorities to Examine Root Causes of Poor Health in Such Communities (Ministry of Health of Singapore, 2021); www.moh.gov.sg/newsroom/collection-of-data-by-working-group-on-health-for-ethnic-minorities-to-examine-root-causes-of-poor-health-in-such-communities
Tan, C. S., Lee, J. & Tan, J. National Steps Challenge, Singapore: a nationwide mHealth physical activity intervention. Br. J. Sports Med. 54, 1047–1048 (2020).
Chin, M. H., Walters, A. E., Cook, S. C. & Huang, E. S. Interventions to reduce racial and ethnic disparities in health care. Med. Care Res. Rev. 64, 7S–28S (2007).
Kim, S. S. et al. A culturally adapted smoking cessation intervention for Korean Americans: a mediating effect of perceived family norm toward quitting. J. Immigr. Minor. Health 17, 1120–1129 (2015).
Wilkinson-Meyers, L. et al. Estimating the additional cost of disability: beyond budget standards. Soc. Sci. Med. 71, 1882–1889 (2010).
Burgess, E., Hassmén, P. & Pumpa, K. L. Determinants of adherence to lifestyle intervention in adults with obesity: a systematic review. Clin. Obes. 7, 123–135 (2017).
Tan, K. H. X. et al. Cohort profile: the Singapore Multi-Ethnic Cohort (MEC) study. Int. J. Epidemiol. 47, 699–699j (2018).
Subramaniam, M. et al. Prevalence of dementia in people aged 60 years and above: results from the WiSE Study. J. Alzheimers Dis. 45, 1127–1138 (2015).
Satghare, P. et al. Prevalence and correlates of pain in people aged 60 years and above in Singapore: results from the WiSE study. Pain Res. Manag. 2016, 7852397 (2016).
Ng, T. P. et al. Mortality of older persons living alone: Singapore Longitudinal Ageing Studies. BMC Geriatr. 15, 126 (2015).
Singapore Census of Population 2020: Statistical Release 1 – Demographic Characteristics, Education, Language and Religion (Department of Statistics of Singapore, 2021).
Tysinger, B. Design, Validation, and an Application of the Future Adult Model: A Dynamic Microsimulation Model of Health-Related Outcomes in the United States (RAND School of Public Policy, RAND Corporation, 2021).
Leaf, D. E., Tysinger, B., Goldman, D. P. & Lakdawalla, D. N. Predicting quantity and quality of life with the Future Elderly Model. Health Econ. 30, 52–79 (2021).
Gonzalez-Gonzalez, C., Tysinger, B., Goldman, D. P. & Wong, R. Projecting diabetes prevalence among Mexicans aged 50 years and older: the Future Elderly Model-Mexico (FEM-Mexico). BMJ Open 7, e017330 (2017).
Chen, C. et al. Educational gradients in disability among Asia’s future elderly: projections for the Republic of Korea and Singapore. Asian Dev. Rev. 39, 51–89 (2022).
Obesity: HPB–MOH Clinical Practice Guidelines (1/2016) (Health Promotion Board, Ministry of Health of Singapore, 2016).
CareShield Life Claims (CareShield Life, 2020); www.careshieldlife.gov.sg/careshield-life/careshield-life-claims.html
WHO-CHOICE Estimates of Cost for Inpatient and Outpatient Health Service Delivery (World Health Organization, 2021); cdn.who.int/media/docs/default-source/health-economics/who-choice-estimates-of-cost-for-inpatient-and-outpatient-health-service-delivery.pdf?sfvrsn=b814d37e_3&download=true
Curtis, L. Unit Costs of Health and Social Care (Personal Social Services Research Unit, Univ. Kent, 2013).
Subramaniam, M. et al. Comorbid diabetes and depression among older adults—prevalence, correlates, disability and healthcare utilisation. Ann. Acad. Med. Singap. 46, 91–101 (2017).
Abdin, E. et al. The societal cost of dementia in Singapore: results from the WiSE study. J. Alzheimers Dis. 51, 439–449 (2016).
Singapore dollar to US dollar spot exchange rates for 2020 (Exchange Rates UK, 2023); www.exchangerates.org.uk/SGD-USD-spot-exchange-rates-history-2020.html
Promoting Healthier Living for All Ages and Families (Ministry of Health of Singapore, 2023); www.moh.gov.sg/news-highlights/details/promoting-healthier-living-for-all-ages-and-families#:~:text=Healthier%20SG%20benefits%20will%20commence,aged%2060%20years%20and%20above
Antonakoudis, G., Poulimenos, L., Kifnidis, K., Zouras, C. & Antonakoudis, H. Blood pressure control and cardiovascular risk reduction. Hippokratia 11, 114–119 (2007).
Malhotra, R., Chan, A., Malhotra, C. & Østbye, T. Prevalence, awareness, treatment and control of hypertension in the elderly population of Singapore. Hypertens. Res. 33, 1223–1231 (2010).
Bennie, J. A., De Cocker, K., Teychenne, M. J., Brown, W. J. & Biddle, S. J. H. The epidemiology of aerobic physical activity and muscle-strengthening activity guideline adherence among 383,928 U.S. adults. Int. J. Behav. Nutr. Phys. Act. 16, 34 (2019).
National Population Health Survey 2022 (Household Interview and Health Examination) (Epidemiology & Disease Control Division, Ministry of Health of Singapore, 2022).
National Health Surveys Highlight Need to Focus on Healthy Diets and Lifestyles (Ministry of Health of Singapore, 2023); www.moh.gov.sg/newsroom/national-health-surveys-highlight-need-to-focus-on-healthy-diets-and-lifestyles
Cook, N. R. et al. Long term effects of dietary sodium reduction on cardiovascular disease outcomes: observational follow-up of the trials of hypertension prevention (TOHP). BMJ 334, 885–888 (2007).
Acknowledgements
This study was supported by the Singapore Ministry of Health’s National Medical Research Council under its Population Health Research Grant (PHRGOC22Jul-0020, ID: MOH-001315) and the HPHSR Clinician Scientist Award (HCSAINV22jul-0005, ID: MOH-001304), awarded to C.C. X.G. was supported by the NUS Research Scholarship. The funders had no role in study design, data collection or analysis, preparation of the manuscript or decision to publish.
Author information
Authors and Affiliations
Contributions
C.C. designed this study. X.G. conducted the literature search, implemented this study, prepared the figures and wrote the paper. C.C. and X.G. analyzed and interpreted the data. H.L.W., S.M., M.S. and N.T.P. curated the data. H.L.W., T.P.N. and B.T. were involved in the discussion of results. All authors reviewed and approved the final paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Aging thanks Hui Shao and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
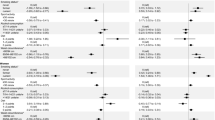
Extended Data Fig. 1 Individual cost-savings by intervention scenarios.
Intervention 1 targets 22.4% of the cohort (n = 366,649) with uncontrolled BP management, Intervention 2 targets 72.2% of the cohort (n = 1,180,774) with lower physical activity level, Intervention 3 targets 89.9% of the cohort (n = 1,470,382) with high sodium intake and Intervention 4 targets 98.1% of the cohort (n = 1,604,909) eligible for Intervention 1–3. The center point represents the mean and the black lines represent 95% credible interval with a significance level of 5% based on two-sided test.
Supplementary information
Supplementary Information
Supplementary technical documentation, Figs. 1–11 and Table 1.
Supplementary Data
Source data for Supplementary Figs. 1–11.
Source data
Source Data Fig. 1
Statistical source data.
Source Data Fig. 2
Statistical source data.
Source Data Fig. 3
Statistical source data.
Source Data Fig. 4
Statistical source data.
Source Data Fig. 5
Statistical source data.
Source Data Fig. 6
Statistical source data.
Source Data Extended Data Fig. 1
Statistical source data.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Guo, X., Tysinger, B., Wee, H.L. et al. Disease burden, lifetime healthcare cost and long-term intervention impact projections among older adults in Singapore. Nat Aging 5, 1358–1369 (2025). https://doi.org/10.1038/s43587-025-00915-0
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/s43587-025-00915-0