Abstract
Background
Efficacy of 2nd line treatment in advanced gastric or gastro-esophageal junction (GEJ) adenocarcinoma remains limited with no identified strong predictor of treatment efficacy. We evaluated the prognostic value of circulating tumor DNA (ctDNA) in predicting the efficacy of immune checkpoint inhibitors (ICI) plus chemotherapy in the randomized PRODIGE 59-FFCD 1707-DURIGAST trial.
Methods
ctDNA was evaluated before treatment (baseline) and at 4 weeks (before the third cycle of treatment, C3) using droplet-digital PCR assays based on the detection of CpG methylation.
Results
Progression-free survival (PFS) and overall survival (OS) were shorter in patients with a high (>1.1 ng/mL) versus low (<1.1 ng/mL) ctDNA concentration at baseline (2.3 vs. 5.8 months; HR = 2.19; 95% CI, 1.09–4.41; p = 0.03 and 4.5 vs. 12.9 months; HR = 2.73; 95% CI, 1.29–5.75; p < 0.01), respectively, after adjustment for identified prognostic variables. Patients with a ctDNA decrease ≤75% between baseline and C3 versus a ctDNA decrease >75% had a worse objective response rate (p = 0.007), shorter PFS (2.2 vs. 7.4 months, HR = 1.90; 95% CI, 1.03–3.51; p = 0.04) and OS (6.6 vs 16.0 months; HR = 2.18; 95% CI, 1.09–4.37; p = 0.03).
Conclusions
An early decrease in ctDNA concentration is a strong predictor of the therapeutic efficacy of ICI plus chemotherapy in advanced gastric/GEJ adenocarcinoma.
Clinical Trial Information NCT03959293 (DURIGAST).
Plain language summary
Some patients with advanced gastric cancer receive immunotherapy (treatments that help one’s own immune system recognize and attack cancer cells) in addition to other treatments. We measured circulating tumor DNA (ctDNA) in patient’s blood samples and looked at associations with treatment outcome. We found that survival was shorter in patients receiving immunotherapy plus chemotherapy, when the levels of ctDNA in the blood were high at the start of treatment and when they did not decrease over time. Our results suggest that ctDNA could be used as a predictor of how well this specific treatment will work in advanced gastric cancer patients.
Similar content being viewed by others
Introduction
The prognosis of advanced gastric and gastro-esophageal junction (GEJ) adenocarcinoma remains poor, with overall survival (OS) ranging from 10% to 15% at 5 years1. In Human Epidermal Growth Factor Receptor-2 (HER2) negative unresectable advanced/metastatic tumors, the most frequently used first-line palliative chemotherapy is a doublet of fluoropyrimidine (5-fluorouracil (5FU) or capecitabine) plus a platinum salt (cisplatin or oxaliplatin)2,3. Recently, the addition of docetaxel (TFOX regimen), immune checkpoint inhibitors (ICI, in PD-L1 positive tumors) and anti-claudin 18.2 (zolbetuximab, in claudin 18.2 positive tumors) to platinum/fluoropyrimidine regimens demonstrated increased OS4,5,6,7,8,9.
In the second-line, chemotherapies (docetaxel, paclitaxel, irinotecan or FOLFIRI) remain the standard of care, including the paclitaxel ramucirumab combination10,11,12,13,14,15. If a triplet regimen (TFOX/FLOT) is used as the first-line treatment, the FOLFIRI regimen is the most commonly used second-line regimen11,13,15. Thus, the PRODIGE 59-FFCD 1707-DURIGAST randomized phase 2 trial aimed to evaluate the efficacy and safety of FOLFIRI with durvalumab (anti-programmed cell death-ligand 1, anti-PD-L1) +/− tremelimumab (anti-cytotoxic T-lymphocyte antigen-4, CTLA-4) as the second-line treatment in patients with advanced gastric/GEJ adenocarcinoma. The regimen had an acceptable safety profile, but long-lasting antitumor activity (disease control beyond 1 year) was only observed in 20% of patients16.
Advances in molecular biology have revealed that malignant cells undergoing cellular turnover or death shed greater quantities of circulating tumor DNA (ctDNA), which is released into the bloodstream. ctDNA and circulating cell-free DNA (cfDNA), which includes DNA released by non-tumor cells and ctDNA, have been associated with prognosis in many cancers17,18,19. cfDNA is composed of both “normal” DNA from healthy cells and the tumor micro-environment as well as ctDNA from the tumor cells. cfDNA levels are significantly higher in patients with cancer than in healthy subjects and in other pathologic and non-pathologic conditions. In contrast, ctDNA is only released by tumor cells, and its detection and quantification using tumor-specific alterations are directly related to the evolution of the tumor. The ctDNA level provides an early prediction of treatment response, before the radiologic evaluation at 2 or 3 months using Response Evaluation Criteria in Solid Tumors 1.1 (RECIST) criteria, in many tumors, including digestive tumors17,20. ctDNA has thus emerged as a strong prognosis marker, in that it accurately reflects real-time tumor burden.
In advanced gastric/GEJ adenocarcinoma, the presence of ctDNA has been correlated with the detection of minimal residual disease (MRD) after curative surgery, and has been used to predict and monitor the response to systemic therapy in unresectable tumors21. Many studies demonstrated that postoperative positive ctDNA after resection of gastric/GEJ adenocarcinoma is associated with significantly worse outcomes22,23,24. By contrast, few series have evaluated ctDNA as an early biomarker of response to treatment in unresectable gastric/GEJ adenocarcinoma, especially concerning responsiveness to ICI. One study of 61 patients who received second- or third-line pembrolizumab alone demonstrated that a decrease in ctDNA from baseline to 6 weeks after starting pembrolizumab predicted an improved response rate (58% versus 0%, p = 0.049) and longer PFS (median 123 days versus 66 days, p = 0.029)25. Additional studies highlighting the usefulness of ctDNA as a biomarker for predicting immunotherapy response are expected to have a significant impact, especially given that the PD-L1 combined positive score (CPS) still falls short of being an accurate indicator of treatment response. Moreover, identifying a predictor of resistance to second-line treatment and beyond remains an unresolved and substantial challenge.
There are many methods to measure ctDNA. Most strategies rely on PCR-based techniques such as droplet digital PCR (ddPCR) that targets either mutations previously identified in the patient’s tumor tissue or very high frequency mutations in a small number of known hotspots, such as KRAS mutations in pancreatic cancers. However, such strategies cannot be applied to gastric/GEJ adenocarcinoma26,27. ctDNA monitoring by ddPCR targeting methylated cancer-specific biomarkers has recently been described as cost-effective and time-efficient17,28,29,30,31,32. Indeed, ctDNA detection based on hypermethylated genes using ddPCR could be used as a surrogate marker of mutations and as a potential universal biomarker of cancer28.
Herein, we tracked the kinetics of cfDNA/ctDNA in blood samples obtained from patients enrolled in the PRODIGE 59-FFCD 1707-DURIGAST trial. We used ddPCR to target methylated cancer-specific biomarkers (MSC-AS1, KCNA3, ZNF790-AS1), a method recently described as being cost-effective and time-efficient (patent WO2020254693-A1)33. Our findings underscore that cfDNA/ctDNA is an early predictor of the response to chemotherapy plus ICI in the second-line treatment of advanced gastric/GEJ adenocarcinoma.
Methods
Study design
PRODIGE 59-FFCD 1707-DURIGAST is a randomized, open-label, multicenter, non-comparative, phase 2 study designed to evaluate the safety and efficacy of FOLFIRI plus durvalumab (FD arm) and FOLFIRI plus durvalumab and tremelimumab (FDT arm) in the second-line treatment of patients with advanced gastric/GEJ adenocarcinoma34. The main inclusion criteria were patients aged 18 years or older, histologically proven advanced unresectable gastric/GEJ (Siewert 2 or 3) adenocarcinoma, with progression or intolerance after first-line chemotherapy with fluoropyrimidine plus platinum salt +/− taxane +/− anti-HER2 therapies in HER2-positive tumors, with an Eastern Cooperative Oncology Group (ECOG)—Performance Status (PS) 0 or 1 and adequate organ function16.
The primary endpoint was the percentage of FD or FDT-treated patients alive and without progression at 4 months (4-month PFS). Progression was based on RECIST 1.1 criteria and evaluated by the investigator. Secondary endpoints included OS, time to strategy failure (TTSF), objective response rate (ORR) and disease control rate (DCR)16,35.
This study was sponsored by the Fédération Francophone de Cancérologie Digestive (FFCD) and supported by the French PRODIGE intergroup. The PRODIGE 59-FFCD 1707-DURIGAST trial was approved by the French health authorities (Agence Nationale de Sécurité du Médicament et des Produits de Santé) and an independent ethics committee (Comité de Protection des Personnes Nord-Ouest II, number 2018-002014-13 on April 16, 2019). The study was conducted in accordance with the Declaration of Helsinki and International Conference on Harmonization Good Clinical Practice Guidelines. Written informed consent was obtained from all patients before treatment.
Patients and samples
Patients were evaluated every 8 weeks using clinical examinations, laboratory tests, and morphological assessments until progression16. Morphological assessments were based on thoracic-abdominal-pelvic CT scans according to RECIST 1.1 criteria. The treatment was repeated until documented disease progression, unacceptable toxicity, withdrawal of consent, or patient refusal.
Analyses of tumor biomarkers included the expression of DNA mismatch repair (MMR) protein by immunohistochemistry (IHC), microsatellite instability (MSI), and PD-L1 expression. PD-L1 IHC was done at a central laboratory using a PD-L1 primary antibody (QR-1, Diagomics, Blagnac, France), according to the manufacturer’s instructions, to calculate the PD-L1 tumor proportion score (TPS) and CPS. Carcinoembryonic antigen (CEA) and carbohydrate antigen 19.9 (CA19.9) levels were also collected at baseline and every 8 weeks.
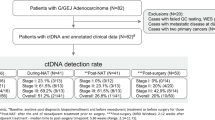
For ancillary studies, blood samples were prospectively collected before the first cycle at baseline (C0) and at 4 weeks just before the third cycle of treatment (C3). Among the 96 randomized patients, 70 (72.9%) participated in the ctDNA ancillary study. All 70 patients (100.0%) provided samples at baseline and 54 (77.1%) before cycle 3 (Fig. 1).
Circulating DNA measurement
Methods for sample preparation, plasma storage, DNA extraction, ddPCR detection and analysis have been previously reported17,28,30,31. Both ctDNA and cfDNA were detected and quantified by Met-ddPCR. Briefly, anonymized blood samples were collected before any second-line anti-cancer treatment in two 8.5-mL cfDNA tubes, and then sent to the EPIGENETEC central laboratory. Tubes were centrifuged for 20 min at 1600 g, and plasma was transferred into cryotubes and stored at −80 °C until ctDNA analysis. DNA extraction and Met-ddPCR were done with METHYS Dx using proprietary developed assays.
Before cfDNA extraction, the samples were defrosted at room temperature and centrifuged a second time (15 min, 2700 g). The cfDNA was extracted from plasma using the QIAamp® Circulating Nucleic Acid Kit (QIAGEN, #55114) according to the manufacturer’s instructions with an elution volume of 50 µL. Samples were incubated with proteinase K for 30 min at 60 °C. Each DNA extraction batch included a no-cfDNA sample consisting of phosphate-buffered saline 1× buffer (PBS) (Gibco, #14190-094). cfDNA was quantified with the Qubit™ dsDNA HS kit (Invitrogen™, #Q32854) using 2 μL of DNA and two reads. Samples were then immediately stored at −20 °C.
Bisulfite conversion of DNA samples was done with the EZ DNA Methylation-Gold Kit (Zymo Research, #ZD5006), as recommended by the manufacturer. M-elution buffer was used for elution. Bisulfite-converted DNA samples were either immediately tested by ddPCR or stored at −20 °C until ddPCR (no more than 5 days). For each conversion, we used three controls: the “no-DNA” PBS sample mentioned above, 10 ng human genomic DNA extracted from whole blood (pool from multiple donors, Promega, #G304A) as the negative control, and 10 ng enzymatically universally methylated human genomic DNA (Zymo Research, # D5011) as the positive control.
All plasma samples were screened for the presence of methylated markers by droplet-based digital PCR (Met-ddPCR) as previously described using Bio-Rad QX 200 assay (QX200 Generator, PX1 Sealer, Thermocycleurs C1000/S1000, QX200 Reader) (Supp Fig. 1)36. A sequential approach was used to determine the presence or absence of ctDNA in plasma and its quantity (ng/mL of plasma). The first analysis used a triplex assay to target two methylated cancer-specific genes (MSC Antisense RNA 1 (MSC-AS1) called « MSC » and (Potassium Voltage-Gated Channel Subfamily A Member 3 (KCNA3)) as well as a methylation-insensitive target on the albumin (ALB) gene used as the reference (assay called Triplex MSC/KCNA3/ALB in the manuscript). The number of copies of the ALB gene in each reaction was used to reflect the number of genome equivalents present. The concentration of DNA was then calculated assuming the presence of 3.3 pg DNA per genome equivalent. In the second step, for the negative or weakly positive samples, a new analysis was carried out, this time targeting the methylation of a sequence of the Zinc Finger Protein 790 Antisense RNA 1 (ZNF790-AS1) (assay referred to as Duplex ZNF790/ALB).
In addition, for each assay, Limit of blank (LOB) and Limit of detection (LOD) were calculated as previously described17,37. The LOB and LOD were calculated by repeating measurements of samples containing no biomarkers of interest (here bisulfite-converted negative control (genomic DNA, Promega®, #G304A). For both markers, LOB was 0, and LOD was 3. Samples with results (copies per uL) lower than the LOB were considered negative, while samples with results higher than the LOD were considered positive. For samples with results between the LOB and LOD, Met-ddPCR was repeated with more input DNA if sufficient DNA was available. If this was not feasible, samples were considered positive. Results were expressed as percentages (number of copies of the target/number of copies of the albumin X 100) and quantity of ctDNA in ng/mL of plasma. Data were processed with Quantasoft Analysis Pro (BIORAD) version 1.0 software. Patients with at least one copy of a methylated gene were considered positive for ctDNA testing, and patients with no methylated biomarker identified through ddPCR were considered negative for ctDNA testing.
For ctDNA, the methylated allelic frequency (MAF) was defined as the highest percentage of methylated genes found through ddPCR. ctDNA change between C3 and C0 was calculated as (ctDNA C3−ctDNA C0)/ctDNA C0.
Statistical considerations
We assessed the value of adding ctDNA to known prognostic factors for predicting PFS and OS in patients with advanced gastric/GEJ adenocarcinoma. Analyses were conducted on the modified intention-to-treat population (mITT population, defined as all patients who received at least one treatment dose in the study regardless of their eligibility criteria).
Quantitative variables are described with means, medians, standard deviations (SD), or interquartile ranges (IQR). Qualitative variables are described as frequencies and percentages. For quantitative variables, baseline characteristics of treatment arms were compared using a Student or Wilcoxon test, and for qualitative variables, a Chi2 test or a Fisher exact test was used.
The primary endpoint was the relationship between baseline ctDNA levels and PFS at 4 months based on RECIST 1.1 criteria as evaluated by the investigator. PFS was defined as the time from randomization to disease progression or death from any cause. Alive patients without progression were censored on the date of the last news. OS was defined as the time between randomization and death (all causes). Alive patients were censored at the last follow-up date. Survival curves were drawn using the Kaplan–Meier method and compared with the log-rank test. Follow-up time was estimated using the reverse Kaplan–Meier method.
The ctDNA concentration at baseline (C0) was evaluated as a prognostic factor for PFS and OS. The change in ctDNA concentration between C0 and C3 was evaluated as an early predictive marker of treatment efficacy (ORR, PFS, and OS). A Cox regression model was used to estimate hazard ratios (HR) with 95% confidence intervals (CI). Multivariate analyses were adjusted according to patient and tumor characteristics identified as prognostic factors.
We determined an optimal cut-off for baseline ctDNA using the maximally selected rank statistics from the ‘maxstat’ R package (Surv-cutpoint function) with OS as endpoint. The restricted cubic spline method was used to model the relationship between the change in ctDNA between baseline and C3 in its continuous form with PFS to define the optimal cut-off38. The relationship between baseline parameters and OS was first assessed using univariate Cox analyses, and then parameters with p-values of less than 0.05 were entered into a final multivariable Cox regression model, after considering collinearity among variables with a correlation matrix. The assumption of proportionality was checked by plotting log minus-log survival curves and by cumulative martingale process plots.
All analyses were carried out with a bilateral alpha type 1 error of 5% and all tests were two-sided. SAS software 9.4 (SAS Institute, Cary, NC) and R survival package (version 4.0.5) were used for statistical analyses.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Results
Population
Between August 27, 2020 and June 4, 2021, 96 patients in 37 centers were randomized in the DURIGAST trial, 92 patients received one or more doses of the treatment (mITT population) and 70 (72.9%) participated in the ctDNA ancillary study (34 patients in the FD arm and 36 patients in the FDT arm) (Fig. 1). There was no difference between the overall population and patients who participated in the ctDNA ancillary study (Supp Table 1).
Among the 70 patients participating in the present study the median age was 60 years. Twenty-two patients (31%) were women, and 46 (66%) had an ECOG PS at 1 (Table 1). Thirty-eight patients had GEJ tumors (54%), mostly with synchronous metastases (67%). The most frequent metastatic sites were the lymph nodes (44%), liver (40%), and peritoneum (31%). Most tumors were intestinal type (51%), and 24% were HER2 positive. The MMR status was determined for 67 tumors, of which three (4%) were classified as dMMR. A PD-L1 CPS ≥ 5 was observed in 35% of tumors, and a PD-L1-positive TPS ≥ 1 in 27% of tumors.
The median follow-up was 20.6 [95% CI 18.4–23.5] months. According to RECIST 1.1 criteria, 4-month PFS was 52.9% [90% CI 42.4%–63.1%]. Median PFS was 4.9 [95% CI 3.6–6.2] months, and median OS was 9.8 [95% CI 7.2–14.2] months.
ctDNA detection at baseline and prognostic value
Among the 70 patients analyzed, 64 (91%) had detectable ctDNA at baseline. Patients with baseline negative ctDNA were more frequently women, were more likely to have no lymph node metastasis, and had a higher neutrophil to lymphocyte ratio (LNR) (Table 1).
The median ctDNA level at baseline was 0.161 (IQR 0.0095-0.711) ng/mL. We found that higher ctDNA level at baseline was associated with male sex, liver metastasis, lymph node metastasis and synchronous metastatic disease, while there was no association with cfDNA (Supp Table 2). Baseline CEA and CA19.9 levels did not correlate with baseline ctDNA levels (p = 0.18 and p = 0.14, respectively). A positive versus negative ctDNA level at baseline was not associated with PFS (HR = 1.38; 95% CI 0.60–3.21; p = 0.45) or OS (HR = 1.40; 95% CI 0.51–3.89; p = 0.52) (Table 2). cfDNA as a continuous variable was associated with PFS, OS, and TTSF but not ctDNA (Supp Table 3). cfDNA and ctDNA dichotomized by median were associated with PFS, OS, and TTSF. Gastric primary tumor location, high lactate dehydrogenase (LDH), high alkaline phosphatase (ALP), peritoneal carcinomatosis and HER2 negative status were associated with worse PFS and OS (Table 2).
We found an association between ctDNA levels as a continuous variable and the primary endpoint, PFS at 4 months (p = 0.007) (Fig. 2). We defined the best cut-off for baseline ctDNA as 1.1 ng/mL. Patients on either side of this cut-off had similar personal and tumor characteristics (Supp Table 4). We found that a baseline ctDNA concentration higher than 1.1 ng/ml (n = 14) was significantly associated with shorter PFS both before (p = 0.012) and after adjustment for identified prognostic variables (HR = 2.19; 95% CI, 1.09–4.41; P = 0.028) (Fig. 3). Median PFS was 5.8 (95% CI, 3.9–8.1) and 2.3 (95% CI, 1.9–7.9) months for patients with a baseline ctDNA concentration below (n = 56) and above 1.1 ng/mL (n = 14), respectively. OS was significantly shorter in patients with high ctDNA (HR = 2.73; 95% CI, 1.29–5.75; p = 0.008) than in those with low ctDNA; median OS was 4.5 and 12.9 months, respectively (Fig. 3). cfDNA level at baseline was associated with DCR (p = 0.022) (Supp Table 2).
In addition, the best cut-off for baseline cfDNA was 2.44 ng/mL. Using this cut-off and after adjustment for identified prognostic variables, cfDNA was not associated with PFS (HR = 1.42; 95% CI, 0.80–2.49; p = 0.2) but was associated with OS (HR = 2.01; 95% CI, 1.03–3.92; p = 0.040) (Supp Fig. 2A and Supp Fig. 2B).
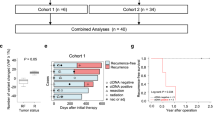
Prognostic impact of ctDNA kinetics
For 54 (77.1%) patients, ctDNA was measured at both C0 and C3. We found a decrease in ctDNA concentration for 38 (70.4%) patients and an increase in ctDNA concentration for 16 (29.6%) patients. The median ctDNA level at C3 was 0.054 ng/mL (0.0040–0.6895). Median ctDNA change between C0 and C3 was −75% (IQR −0.97%–+0.41%), while for cfDNA it was −9% (IQR −0.37%–+0.49%). The change in ctDNA between C0 and C3 was associated with ECOG PS and HER2 status (Supp Table 2). ctDNA kinetics did not correlate with CEA and CA19.9 kinetics (p = 0.35 and p = 0.26, respectively). A ctDNA increase was associated with poor outcomes, including DCR (p = 0.013), PFS (HR = 2.09; 95% CI, 1.19–3.67; p = 0.010), OS (HR = 2.51; 95% CI, 1.35–4.68; p = 0.004) and TTSF (HR = 1.88; 95% CI, 1.09–3.25; p = 0.023). No association was found for a cfDNA increase (Supp Table 3).
The restricted cubic spline method was employed to model the relationship between continuous ctDNA kinetics and PFS, and revealed a 75% decrease as the optimal cut-off, corresponding to the median ctDNA decrease between C0 and C3. Specifically, 27 (50%) patients exhibited a ctDNA decrease greater than 75%, while another 27 (50.0%) had a decrease of 75% or less. We found a strong correlation between a ctDNA decrease of 75% or less and PFS at 4 months (p = 0.006) (Supp Table 5). A ctDNA decrease of 75% or less was significantly associated with shorter PFS both before (p = 0.008) and after adjustment for identified prognostic variables (adjusted HR = 1.90; 95% CI, 1.03–3.51; p = 0.04) (Fig. 4). Median PFS was 7.4 months for patients with a ctDNA decrease greater than 75%, compared to 2.2 months for those with a decrease of 75% or less. After adjustment for identified prognostic variables, median OS in patients with a ctDNA decrease of 75% or less was significantly shorter (HR = 2.18; 95% CI, 1.09–4.37; p = 0.028) than that in patients with ctDNA decrease greater than 75% (6.6 versus 16.0 months, respectively) (Fig. 4).
Discussion
Our work is the first to demonstrate, to our knowledge, that ctDNA is a strong predictor of survival in patients treated with second-line chemotherapy plus ICI for gastric/GEJ adenocarcinoma. A high baseline level of ctDNA is associated with worse PFS and OS. Moreover, an early decrease, at week 4, in ctDNA concentration during treatment strongly predicts PFS and OS.
The randomized trials CheckMate 649 and KEYNOTE-859 showed that ICI plus chemotherapy was more effective than chemotherapy alone6,7. The survival increase was restricted to patients with tumor PD-L1 CPS ≥ 1, but no strong clinical/pathological factor, except for dMMR/MSI status, was associated with the survival benefit of this combination. Indeed, in pMMR/MSS PD-L1 CPS-positive tumors, the addition of ICI increased PFS by less than 2 months, but there are as yet no strong biomarkers to identify patients with prolonged survival. In the same way, in the PRODIGE 59-FFCD 1707-DURIGAST randomized phase 2 trial, no clinical/pathological factor was associated with PFS or OS. There was no correlation between CPS and survival16. Consequently, the identification of prognostic biomarkers in patients with advanced gastric/GEJ adenocarcinoma treated with ICI plus chemotherapy remains a challenge. However, ctDNA seems to fill this role.
In our series, most patients had positive ctDNA at baseline (91%). Previous studies in gastric/GEJ adenocarcinoma have already demonstrated that the ctDNA level is associated with disease stage and the number of involved metastatic disease sites, and that many “peritoneal-only” patients have undetectable ctDNA39. The proportion of patients with positive ctDNA ranges from 70 to 90%25,39,40,41. In our series, a higher ctDNA level at baseline was associated with male sex, liver metastasis, lymph node metastasis and synchronous metastatic disease. In many tumors, including gastric/GEJ adenocarcinoma, liver metastasis and/or synchronous metastatic disease have been associated with higher ctDNA levels17,31,34,40. Some studies have already shown higher ctDNA levels in patients with lymph node metastases in different tumor types, including gastric adenocarcinoma42[,43.
We found that baseline ctDNA above a cut-off at 1.1 ng/ml was significantly associated with shorter PFS after adjustment for known prognostic variables (HR = 2.19; 95% CI, 1.09–4.41; p = 0.028). It was difficult to identify any correlation between survival and positive versus negative ctDNA at baseline since most patients had positive ctDNA, thereby resulting in a lack of statistical power. By contrast, ctDNA as continuous variable was more strongly associated with PFS/OS. Indeed, median PFS was 5.8 months in patients with ctDNA below 1.1 ng/mL and 2.3 months for those above 1.1 ng/mL. A similar correlation was observed for OS, with median OS of 12.9 and 4.5 months, respectively. These results suggest that ctDNA is both a prognostic factor and a predictor of treatment efficacy. Until now, no other clinical/pathological factor has been so strongly associated with PFS and OS in advanced gastric/GEJ adenocarcinoma patients. Few series have evaluated ctDNA as an early biomarker of response to treatment in unresectable gastric/GEJ adenocarcinoma, especially with regard to responsiveness to ICI plus chemotherapy. One study involving 61 patients treated with second- or third-line pembrolizumab alone demonstrated good agreement between mutation burden, determined using ctDNA testing, and tumor tissue mutation burden. In the above study, the ctDNA mutation burden was associated with response to pembrolizumab25. In a series of 30 patients with advanced gastric/GEJ adenocarcinoma treated with first-line chemotherapy alone, ctDNA was associated with OS: 19.5 months in patients with low ctDNA versus 12.8 months in patients with high ctDNA40. In another series of 27 gastro-esophageal adenocarcinoma patients treated with ICI alone, those with low ctDNA-NGS maximum somatic variant allele frequency had a median OS of 8.8 versus 2.5 months for those with high ctDNA-NGS maximum somatic variant allele frequency39. In a recent meta-analysis that included patients with gastric cancer treated with chemotherapy, ctDNA was strongly associated with survival. The corresponding HR for OS, disease-free survival (DFS) and PFS were 2.74 (95% CI 2.24–3.35), 3.13 (95% CI 2.08–4.72) and 3.04 (95% CI 2.46–3.76), respectively44. It is worth noting that most of these series used a methylation (SOX17, WIF-1, RASSF1A or SFRP2 genes) or mutational approach to identify ctDNA. In our series, by contrast to ctDNA, cfDNA was not associated with PFS, and only associated with OS after adjustment for prognostic variables. These results highlight that ctDNA, by contrast to cfDNA, is more directly related to tumor burden and tumor DNA shedding and thus associated with treatment efficacy. By contrast cfDNA levels are also influenced by other factors like the cancer-related inflammatory response.
We also demonstrated that a decrease in ctDNA during treatment was associated with DCR, PFS, and OS. Median PFS was 7.4 months for patients with a decrease greater than 75% versus 2.2 months in those with a ctDNA decrease of 75% or less. One study evaluated ctDNA variation in only 18 patients, after 6 weeks of treatment with pembrolizumab alone and found that this decrease predicted an improved response rate (58% versus 0%, p = 0.049) and longer PFS (median 123 days versus 66 days, p = 0.029)25. In another series of 32 patients treated with chemotherapy, those with a more than 25% decline in maximal somatic variant allelic frequency had significantly longer PFS than did those without (7.3 months versus 3.6 months; p = 0.0011)41. All of these results suggest that ctDNA change is associated with treatment response and could be used as a predictor of treatment efficacy in advanced gastric/GEJ adenocarcinoma. The current gold standard for assessing tumor response and treatment efficacy in solid tumors is radiographic imaging interpreted using RECIST 1.1. Limitations to this method include evaluation after at least 2 months of treatment, poor interobserver reproducibility and difficulty to identify pseudo-progression in patients treated with ICI. The measurement of tumor biomarkers, like CEA and carbohydrate antigen 19-9 (CA19-9), has a prognostic value in gastric cancer, but variations in levels during treatment are not a strong predictor of treatment efficacy45. In contrast, changes in ctDNA levels during treatment appear to be a highly relevant biomarker of treatment efficacy in unresectable gastric/GEJ adenocarcinoma. In addition, ctDNA monitoring by ddPCR targeting methylated cancer-specific biomarkers is relevant in unresectable gastric/GEJ adenocarcinoma since there is no recurrent and frequent mutation in this type of cancer. Indeed, ctDNA monitoring by ddPCR targeting methylated cancer-specific biomarkers is easier, more cost-effective and time-efficient than tumor-informed ctDNA detection, given the need to identify frequent molecular alterations in the tumor of each patient in the latter.
The main limitation of this study is the small number of patients (n = 70). Nevertheless, to our knowledge, it is the largest series evaluating ctDNA in patients treated with ICI plus chemotherapy for gastric/GEJ adenocarcinoma. The other limitation of our study is that we were not able to determine the contribution of chemotherapy versus immunotherapy to ctDNA levels and kinetics and treatment response since all of the patients received the chemoimmunotherapy combination. Moreover, the second collection point for ctDNA was at 4 weeks, and most patients remained treated by a combination of chemotherapy and immunotherapy. In addition, we were not able to determine whether the ctDNA concentration was associated with the overall tumor burden, as in the crude RECIST 1.1 total measurement. We can however highlight many strengths, including a well-designed prospective phase II trial, the analysis of both cfDNA and ctDNA as well as ctDNA kinetics during treatment. Since many treatment options are now available for gastric/GEJ adenocarcinoma, ctDNA could help to guide the therapeutic strategy, including maintenance treatment and modifications of lines of treatment. For example, if ctDNA levels remain high after one or two cycles of first-line treatment with FOLFOX plus ICI, it is possible to start a second-line treatment with paclitaxel plus ramucirumab before radiological and clinical progression occurs. Recent results of the ARMANI trial suggest that changing the chemotherapy regimen despite the absence of radiological progression could improve survival, but a strategy using early ctDNA levels remains to be validated in a prospective trial. To our knowledge, there are no planned studies to evaluate the treatment strategy for gastric/GEJ adenocarcinoma based on the ctDNA level in a metastatic setting. By contrast ctDNA is used to detect MRD after radical resection and to evaluate adjuvant trastuzumab deruxtecan plus fluoropyrimidine versus standard chemotherapy in HER2-positive gastric/GEJ cancer patients with persistent MRD in the liquid biopsy after radical surgery (TRINITY trial).
To conclude, baseline ctDNA and early decreases in ctDNA levels during treatment with chemotherapy plus ICI were strongly associated with survival in patients with advanced gastric or GEJ adenocarcinoma. These results suggest that ctDNA can guide treatment strategies and could help physicians with treatment decision-making. ctDNA must be evaluated in a prospective trial to confirm that it is a robust and early predictor of treatment efficacy, earlier than a CT-scan, and can be used to guide treatment modifications in cases with no ctDNA decrease, thereby improving patients’ survival.
Data availability
The minimum datasets necessary to interpret this research (source data) have been provided within the article and supplementary data file. Detailed ctDNA results are available at dryad repository (https://doi.org/10.5061/dryad.fn2z34v47). ctDNA sequencing data are available at the FCCD under restricted access for ethical and privacy concerns. Applicants may also directly contact the corresponding author (D.T.). All other data are available from the corresponding author on reasonable request.
References
Jemal, A. et al. Global cancer statistics. CA Cancer J. Clin. 61, 69–90 (2011).
Kang, Y. K. et al. Capecitabine/cisplatin versus 5-fluorouracil/cisplatin as first-line therapy in patients with advanced gastric cancer: a randomised phase III non inferiority trial. Ann. Oncol. 20, 666–673 (2009).
Van Cutsem, E. et al. Phase III study of docetaxel and cisplatin plus fluorouracil compared with cisplatin and fluorouracil as first-line therapy for advanced gastric cancer: a report of the V325 study group. J. Clin Oncol. 24, 4991–4997 (2006).
Al-Batran, S. E. et al. Biweekly fluorouracil, leucovorin, oxaliplatin, and docetaxel (FLOT) for patients with metastatic adenocarcinoma of the stomach or esophagogastric junction: a phase II trial of the Arbeitsgemeinschaft Internistische Onkologie. Ann. Oncol. 19, 1882–1887 (2008).
Van Cutsem, E. et al. Docetaxel plus oxaliplatin with or without fluorouracil or capecitabine in metastatic or locally recurrent gastric cancer: a randomized phase II study. Ann. Oncol. 26, 149–156 (2015).
Janjigian, Y. Y. et al. First-line nivolumab plus chemotherapy versus chemotherapy alone for advanced gastric, gastro-oesophageal junction, and oesophageal adenocarcinoma (Check-Mate 649): a randomised, open-label, phase 3 trial. Lancet Oncol. 398, 27–40 (2021).
Shah, M. A. et al. Zolbetuximab plus CAPOX in CLDN18.2-positive gastric or gastroesophageal junction adenocarcinoma: the randomized, phase 3 GLOW trial. Nat. Med. 29, 2133–2141 (2023).
Shitara, K. et al. Zolbetuximab plus mFOLFOX6 in patients with CLDN18.2-positive, HER2-negative, untreated, locally advanced unresectable or metastatic gastric or gastro-oesophageal junction adenocarcinoma (SPOTLIGHT): a multicentre, randomised, double-blind, phase 3 trial. Lancet. 401, 1655–1668 (2023).
Rha, S. Y. et al. Pembrolizumab plus chemotherapy versus placebo plus chemotherapy for HER2-negative advanced gastric cancer (KEYNOTE-859): a multicentre, randomised, double-blind, phase 3 trial. Lancet Oncol. 24, 1181–1195 (2023).
Ford, H. E. et al. Docetaxel versus active symptom control for refractory oesophagogastric adenocarcinoma (COUGAR-02): an open-label, phase 3 randomised controlled trial. Lancet Oncol. 15, 78–86 (2014).
Thuss-Patience, P. C. et al. Survival advantage for irinotecan versus best supportive care as second-line chemotherapy in gastric cancer – A randomised phase III study of the Arbeitsgemeinschaft Internistische Onkologie (AIO). Eur. J. Cancer. 47, 2306–2314 (2011).
Hironaka, S. et al. Randomized, open-label, phase III study comparing irinotecan with paclitaxel in patients with advanced gastric cancer without severe peritoneal metastasis after failure of prior combination chemotherapy using fluoropyrimidine plus platinum: WJOG 4007 trial. J. Clin. Oncol. 31, 4438–4444 (2013).
Guimbaud, R. et al. Prospective, randomized, multicenter, phase III study of fluorouracil, leucovorin, and irinotecan versus epirubicin, cisplatin, and capecitabine in advanced gastric adenocarcinoma: a french intergroup (Fédération Francophone de Cancérologie Digestive, Fédération Nationale des Centres de Lutte Contre le Cancer, and Groupe Coopérateur Multidisciplinaire en Oncologie) study. J. Clin. Oncol. 32, 3520–3526 (2014).
Wilke, H. et al. Ramucirumab plus paclitaxel versus placebo plus paclitaxel in patients with previously treated advanced gastric or gastro-oesophageal junction adenocarcinoma (RAINBOW): a double-blind, randomised phase 3 trial. Lancet Oncol. 15, 1224–1235 (2014).
Maugeri-Saccà, M. et al. FOLFIRI as a second-line therapy in patients with docetaxel-pretreated gastric cancer: a historical cohort. J. Exp. Clin. Cancer Res. 32, 67 (2013).
Tougeron D. et al. FOLFIRI plus durvalumab with or without tremelimumab in second-line treatment of advanced gastric or gastroesophageal junction adenocarcinoma: the PRODIGE 59-FFCD 1707-DURIGAST randomized Clinical Trial. JAMA Oncol. 10, 709–717 (2024).
Garlan, F. et al. Early evaluation of circulating tumor DNA as marker of therapeutic efficacy in metastatic colorectal cancer patients (PLACOL study). Clin. Cancer Res. 23, 5416–5425 (2017).
Bettegowda, C. et al. Detection of circulating tumor DNA in early- and late-stage human malignancies. Sci. Transl. Med. 6, 224ra24 (2014).
Tie, J. et al. Circulating tumor DNA as an early marker of therapeutic response in patients with metastatic colorectal cancer. Ann. Oncol. 26, 1715–1722 (2015).
Evrard, C. et al. Circulating tumor DNA in unresectable pancreatic cancer is a strong predictor of first-line treatment efficacy: the KRASCIPANC prospective study. Dig. Liver Dis. 55, 1562–1572 (2023).
Lee, M. S., Kaseb, A. O. & Pant, S. The emerging role of circulating tumor DNA in non-colorectal gastrointestinal cancers. Clin. Cancer Res. 29, 3267–3274 (2023).
Ococks, E. et al. Longitudinal tracking of 97 esophageal adenocarcinomas using liquid biopsy sampling. Ann. Oncol. 32, 522–532 (2021).
Leal, A. et al. White blood cell and cell-free DNA analyses for detection of residual disease in gastric cancer. Nat. Commun. 11, 525 (2020).
Huffman, B. M. et al. 1415P—performance of a tumor-informed circulating tumor DNA assay from over 250 patients with over 600 plasma time points in esophageal and gastric cancer. Ann. Oncol. 32, S1040–S1075 (2021).
Kim, S. T. et al. Comprehensive molecular characterization of clinical responses to PD-1 inhibition in metastatic gastric cancer. Nat. Med. 24, 1449–1458 (2018).
Schwarzenbach, H., Hoon, D. S. & Pantel, K. Cell-free nucleic acids as biomarkers in cancer patients. Nat. Rev. Cancer. 11, 426–437 (2011).
Taly, V., Pekin, D., El Abed, A. & Laurent-Puig, P. Detecting biomarkers with microdroplet technology. Trends Mol. Med. 18, 405–416 (2012).
Garrigou, S. et al. A study of hypermethylated circulating tumor DNA as a universal colorectal cancer biomarker. Clin. Chem. 62, 1129–1139 (2016).
Boeckx, N. et al. Mutation andmethylation analysis of circulating tumor DNA can be used for follow-up of metastatic colorectal cancer patients. Clin. Colorectal. Cancer 17, e369e79 (2018).
Benhaim, L. et al. Circulating tumor DNA is a prognostic marker of tumor recurrence in stage II and III colorectal cancer: multicentric, prospective cohort study (ALGECOLS). Eur. J. Cancer. 159, 24–33 (2021).
Bachet, J. B. et al. Circulating tumour DNA at baseline for individualised prognostication in patients with chemotherapy-naïve metastatic colorectal cancer. An AGEO prospective study. Eur. J. Cancer. 189, 112934 (2023).
Pietrasz, D. et al. Prognostic value of circulating tumour DNA in metastatic pancreatic cancer patients: post-hoc analyses of two clinical trials. Br. J. Cancer. 126, 440–448 (2022).
Diagnosing gastric cancer, in vitro, comprises determining level of methylation of MSC antisense RNA 1 gene and gene comprising ZNF790 antisense RNA gene and potassium voltage-gated channel subfamily A member 3, in biological sample. Brevet. (2019): WO2020254693-A1, EP305811.
Evrard, C. et al. PRODIGE 59-DURIGAST trial: a randomised phase II study evaluating FOLFIRI+Durvalumab ± Tremelimumab in second-line of patients with advanced gastric cancer. Dig. Liver Dis. 53, 420–426 (2021).
Evrard, C. et al. Safety of FOLFIRI + Durvalumab +/- Tremelimumab in second line of patients with advanced gastric cancer: a safety run-in from the randomized phase II study DURIGAST PRODIGE 59. Biomedicines. 10, 1211 (2022).
Taieb, J. et al. Prognostic value and relation with adjuvant treatment duration of ctDNA in stage III colon cancer: a post hoc analysis of the PRODIGE-GERCOR IDEA-France trial. Clin. Cancer Res. 27, 5638–5646 (2021).
Milbury, C. A. et al. Determining lower limits of detection of digital PCR assays for cancer-related gene mutations. Biomol. Detect Quantif. 1, 8–22 (2014).
Perperoglou, A., Sauerbrei, W., Abrahamowicz, M. & Schmid, M. A review of spline function procedures in R. BMC Med. Res. Methodol. 19, 46 (2019).
Maron, S. B. et al. Circulating tumor DNA sequencing analysis of gastroesophageal adenocarcinoma. Clin. Cancer Res. 25, 7098–7112 (2019).
Davidson, M. et al. Detecting and tracking circulating tumour DNA copy number profiles during first line chemotherapy in oesophagogastric adenocarcinoma. Cancers 11, 736 (2019).
Jin, Y. et al. The predicting role of circulating tumor DNA landscape in gastric cancer patients treated with immune checkpoint inhibitors. Mol. Cancer 19, 154 (2020).
Bando, H. et al. Effects of metastatic sites on circulating tumor DNA in patients with metastatic colorectal cancer. JCO Precis Oncol. 6, e2100535 (2022).
Kung, C. Y. et al. Comparison of the mutation patterns between tumor tissue and cell-free DNA in stage IV gastric cancer. Aging 15, 777–790 (2023).
Min, L., Chen, J., Yu, M., Yang, K. & Liu, D. Utilizing circulating tumour DNA as a prognostic predictor of gastric cancer: a meta-analysis. Biomarkers 28, 427–436 (2023).
Ychou, M., Duffour, J., Kramar, A., Gourgou, S. & Grenier, J. Clinical significance and prognostic value of CA72-4 compared with CEA and CA19-9 in patients with gastric cancer. Dis. Markers 16, 105–110 (2000).
Acknowledgements
We thank all physicians participating in the PRODIGE 59-FFCD 1707-DURIGAST trial. We also thank all the cooperative PRODIGE group (FFCD—UNICANCER GI—GERCOR) for their contribution and participation in the present trial, especially Daniel Gonzalez, Lila Gaba, Meriem Guarssifi, and Charles Fuchey, the PRODIGE 59-FFCD 1707-DURIGAST FFCD team. We thank AstraZeneca for providing durvalumab and tremelimumab. Finally, we thank the “Ligue Nationale Contre le Cancer” for their support. The FFCD is the sponsor of the PRODIGE 59-FFCD 1707-DURIGAST trial. AstraZeneca provided financial support for the trial. FFCD funded a part the biobank and molecular analyses. AstraZeneca provided the study drug. AstraZeneca had no role in study design, data collection, data analysis, data interpretation, or writing of the report. D.T. prepared the first draft in collaboration with the FFCD and other co-authors. D.T. had full access to all patient-level study data and all authors approved the submission for publication.
Author information
Authors and Affiliations
Contributions
D.T., C.L., J.D., L.E., A.A., A.C., G.B., A.Z., N.E., M.B., L.K., C.P., B.C., T.A., A.B., and Y.R. participated in the trial. D.T. and P.L.P. wrote the first draft of the manuscript. All authors participated in reviewing, correcting, and editing the manuscript. D.T., K.L.M., V.T. and P.L.P. participated in conceptualisation of the study. K.L.M. and P.L.P. had access to the raw data and were involved in the formal analysis of the data. D.T., V.T., P.L.P., and K.L.M. accessed and verified all the data. D.T. sourced funding. A.B., H.D., V.T., and P.L.P. performed experiments and analysed ctDNA results. D.T. and P.L.P. directed the research and evolved the manuscript to the final draft.
Corresponding author
Ethics declarations
Competing interests
D.T. reports consultancy, advisory fees, honoraria from Servier, Pierre Fabre, Merck Serono, MSD, BMS, A.Z., Roche, Sanofi; research funding from Sandoz, AstraZenenca, Servier, MSD; travel grants from Pierre Fabre, MSD, Servier, Roche. P.L.P. reports consultancy, advisory fees, and honoraria from Servier, Pierre Fabre, and Biocartis. T.A. reports advisory fees, and honoraria from Pierre Fabre, Servier, MSD, BMS, Bayer. B.C. reports advisory fees from Bayer, MSD, BMS, Sanofi, and Roche, and honoraria from Amgen, Roche, Sanofi, Merck, BMS, SeqOne Genomics, and Pierre Fabre. A.Z. reported personal fees from Amgen, AbbVie, Astellas, Gilead, Merck, Sanofi, Roche, Servier, MSD, BMS, Pierre Fabre, Daiichi Sankyo, AstraZeneca, Zymeworks; grants from Amgen outside the submitted work. P.L.P. and V.T. are one of the founders of MethysDX. The other authors declare that there are no competing interests.
Peer review
Peer review information
Communications Medicine thanks Matthew Strickland and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Peer review reports are available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Tougeron, D., Louvet, C., Desramé, J. et al. Circulating tumor DNA strongly predicts efficacy of chemotherapy plus immune checkpoint inhibitors in patients with advanced gastro-esophageal adenocarcinoma. Commun Med 5, 136 (2025). https://doi.org/10.1038/s43856-025-00867-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s43856-025-00867-x