Abstract
Background
Laser keratotomy, a corneal incision technique for vision correction, has advanced with near-infrared (NIR) femtosecond (fs) lasers-ultrashort pulsed light sources in the near-infrared spectrum. However, NIR femtosecond lasers encounter challenges such as postoperative astigmatism due to scattering by edematous tissues, and endothelial cells distortion by mechanical impact.
Methods
The mid-infrared (MIR) femtosecond lasers at a central wavelength of 6.1 μm resonating with amide modes has an output power of 100 mW and a pulse width of ~200 fs. Systematic experiments of MIR fs laser keratotomy are performed on corneas of 8-week-old male C57BL/6J mice, with optical coherence tomography and fluorescein staining for evaluating corneal recovery in vivo. Electroretinography and visual cliff test are performed for evaluating potential adverse effects on retinal and visual function. Immunofluorescence and immunohistochemistry are carried out for accessing the density, morphology and function of endothelial cell, and the structure of incision and recovery condition of cornea after sacrificing the mice.
Results
Efficient deep keratotomy with minimal collateral damage is realized both in normal and edematous cornea, surpassing traditional NIR femtosecond lasers by experimental comparison. Histological imaging, fluorescein staining and immunofluorescence reveal that corneal incisions ablated by MIR fs laser can heal within 3 days by identifying optimal ablation parameters. Additionally, through the electrophysiology and visual cliff index evaluations, it is confirmed that no postoperative retinal and visual impairment caused, proving a good biological safety.
Conclusions
Keratotomy by MIR fs laser exhibits favorable ablative efficiency and biosafety in mice, which could serve as a new tool for ophthalmic surgery and extend the applications of femtosecond laser assisted keratotomy.
Plain language summary
In keratotomy, a cornea (eye structure) incision technique for vision correction, that requires deep or penetrating ablation, Near-infrared (NIR) femtosecond (fs) lasers are traditionally used. NIR fs lasers, however, encounter unwanted side effects such as postoperative astigmatism. Here, we report an in vivo keratotomy based on Mid-infrared (MIR) fs laser with a wavelength of 6.1 μm using mice. It is found that MIR fs laser penetrating keratotomy surpasses traditional NIR fs lasers in terms of ablation efficiency and undesired damage. Deep or penetrating cornea incisions ablated by MIR fs laser heal within 3 days with full restoration of the cornea cells highlighting its biological safety. It is therefore suggested that the 6.1 μm MIR fs laser is promising in addressing the current limitations of deep laser keratotomy.
Similar content being viewed by others
Introduction
Keratotomy and keratectomy are general ophthalmic surgical techniques that improve vision through incision creation and tissue removal, respectively. They have been used for refractive correction1, cataract treatment2, and corneal transplantation3. Since Trokel et al. demonstrated the potential value of laser in keratectomy in 19834, the surgical precision, procedure repeatability, treatment predictability, and minimal invasiveness haven been dramatically improved with better success rate, healing time and surgical prognosis. The boom of laser corneal surgery has subsequently been witnessed. Excessive collateral damage and rough incision are generally thought as main reasons of postoperative adverse reaction (astigmatism, dry eye and corneal haze etc.) in surgery5,6. Therefore, during the decades of long journey, abundant of research efforts have been made to seek for lasers that could generate the efficient incision with the minimal collateral damage. The argon-fluorine excimer laser emitting ultraviolet radiation at a wavelength of 193 nm and well absorbed by corneal tissues has been the dominant keratectomy tool. Ideally, excimer-based ablation could create clear surgical incision with smooth crater and little thermal damage to surrounding tissues7, however, it is difficult to achieve and preserve a good beam quality, together with the high operative cost, and the hazards of toxic gases in surgical environments8, which triggers a desire of a better keratotomy laser tool. In response, series of studies have been conducted on Er:YAG based mid-infrared (MIR) laser emitting a wavelength of 2940 nm coinciding with the peak absorption of water as an alternative source of corneal ablation9,10. Although Stojkovic et al. demonstrated that Q-switched Er:YAG laser with nanosecond-scale pulse duration can significantly reduce collateral damage in cornea compared to quasi-continuous modes11, corneal shrinkage appears to occur during penetrating keratoplasty with Er:YAG laser due to the excessive heat from relatively long pulses12. Therefore, further shortening the laser pulse width contributes to the improvement of the incision quality. Known that the relaxation time of the thermal diffusion in biological tissues is a few hundred picoseconds13, the femtosecond (fs) laser with an interaction duration much shorter than the thermal relaxation tightly confines the heat diffusion14, demonstrating immense potential in corneal surgery15. High-precision incision with minimal damage is achieved via the formation of cavitation bubbles at focus with high-power density of fs lasers with a common near-infrared (NIR) wavelength at ~1 μm16. However, there are some limiting factors that restrict NIR fs laser in deep or penetrating keratotomy17. Firstly, scattering of the NIR laser in cornea has severe impact on the surgical performance, especially in the edematous cornea which is the usual case in keratotomy. When NIR laser transmitting the deep pathological tissue, the scattering process not only depletes pulse energy but also distorts the focal spot and deteriorates the beam quality, which may lead to irregular or even failed incision18. In addition, the mechanical impact of high intensity fs pulse on cornea could cause tissue distortion and damage to endothelial cells19, leading to extended wound healing time and postoperative astigmatism20. Thirdly, corneas are transparent to radiation at the wavelength near 1 μm, hence the potential risk of damage to other ocular tissues caused by NIR pulses with high peak power pulses must be treated with caution. Therefore, new fs laser source with less scattering and mechanical impact, and higher absorption by ocular tissues are demanded fitting more rigorous acquirements of keratotomy.
MIR fs lasers resonating with amide and hydroxyl modes at a wavelength ranging from 6.1 to 6.5 μm present an attractive alternative for soft tissue ablation21,22, offering efficient and minimally invasive performance23,24. Laser at this wavelength can simultaneously excite the resonance of water and collagen protein. Different from the general ablative mechanism, heating of collagen in tissue causes it to preferentially transit from highly ordered arrays with high tensile strength to amorphous structure with less resilience, enabling easier decomposition through the explosive vaporization of the heated water. This facilitates an efficient ablation with less collateral damage25,26,27. The resonant absorption combined with fs cold processing could not only ensure a safe incision, but also help in preserving collagen fibers around incisions and reducing the endothelial cell damage. More importantly, MIR lasers with long wavelengths significantly mitigate optical scattering, making them well-suited for deep or penetrating keratotomy in edematous corneas28. At present, compact high-power MIR fs lasers have been realized by nonlinear frequency conversions29,30,31, which could provide a new path for the future development of laser-assisted keratotomy. However, the in vivo efficacy, healing process, biological safety, and postoperative complications as well as potential risks of MIR fs laser keratotomy have not yet been reported.
In this work, we demonstrate the in vivo keratotomy based on MIR fs laser for the first time, to the best of our knowledge. The MIR laser with a wavelength of 6.1 μm coinciding to the amide-I resonant mode, 200 fs pulse width and 100 mW output power from an optical parametric amplifier (OPA) is employed for corneal ablation in living mice. A superior ablation efficiency and collateral damage are demonstrated in MIR fs laser penetrating keratotomy compared to the counterpart traditional NIR fs lasers. Through the systematical investigation of the healing process by histological imaging, fluorescein staining imaging, OCT and immunofluorescence, it is revealed that deep corneal incisions ablated by MIR fs laser can heal in 3 days with structurally intact epithelium, stromal and endothelial layers by identifying the optimal ablation parameters. In addition, large-area laser ablation is performed, and rapid healing without adverse reactions is demonstrated. Postoperative retinal and visual function investigation through the visual cliff and electrophysiology index evaluations proves a good biological safety of the MIR fs laser keratotomy. It is therefore suggested that the 6.1 μm MIR fs laser is promising to serve as a new tool for future ophthalmological surgery, in addressing the limitations of deep or penetrating keratotomy.
Methods
MIR high-power fs laser source
MIR fs output was obtained from a two-stage OPA. A commercial pump source (Pharos, Light Conversion) can provide maximally a 20 W output centered at 1030 nm wavelength with 400 μJ per pulse and 250 fs pulse width at 50 kHz repetition rate. A portion of the pump laser with a power of 400 mW was focused by a lens with a focal length of 100 mm into a 10-mm thick YAG crystal. The residual pump was filtered by LPF (HT@1100–2000 nm), and the NIR supercontinuum spanning from 1100 to 1600 nm is generated through single filamentation. The NIR signal and the first-stage pump were focused to a LGS crystal (type Ι, θ = 51°, φ = 0°) with a thickness of 8 mm through lenses with focal length of 150 mm and 200 mm, respectively, passing through a dichroic mirror (HT@1100–1600 nm, HR@1030 nm). The signal at a wavelength of 1240 nm was subsequently amplified to 100 mW by tuning the phase-matching angle with a pump power of 2.5 W. Another pump beam with a power of 8 W was converged with the amplified signal to another LGS crystal (type Ι, θ = 51°, φ = 0°). Ge window was employed to remove the amplified signal while transmitting the MIR idler beam. The MIR output was subsequently transmitted through a hollow core MIR fiber (HF500MW, OptpKnowledge) to a scanning granting monochromator (Omini-λ500i, Zolix) with a MCT detector for the spectral measurement. The temporal profile was characterized by a homemade interference autocorrelator.
Modeling of photothermal corneal ablation by MIR fs pulses
The heat transfer model was established based on the finite element method through solving the bioheat balance equation:
Here, \(\rho\) is the density of corneal tissue, \(C\) indicates the specific heat, \(k\) represents the thermal conductivity, and \(T\) is the corneal local temperature32. The thermal parameters of cornea are obtained from Ref. 33 The heat source \(Q\) is dependent on MIR fs radiation absorbed by the cornea tissue, which was defined as a Gaussian spot of a 55 μm diameter, with a pulse energy of 2 μJ and a pulse duration of 200 fs at a repetition rate of 50 kHz, applied vertically on the corneal surface. The cross-section of the cornea was considered as a homogeneous layer with a thickness of 100 μm. The temperature rise of the corneal surface under MIR irradiation was calculated with a time step of 200 fs. According to the photothermal ablation theory of biological tissues irradiated by MIR laser25,34, when biological tissues deposit heat in a very short period of time and reach a temperature of 100 °C, the water molecules contained in the tissue begin to vaporize, leading to mechanical rupture and thermal decomposition of tissue fragments, achieving tissue removal and the formation of ablation crater35. Therefore, the critical temperature for corneal ablation was defined as 100 °C in this model.
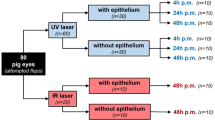
Preparation and characterization of tissue in vitro
The tissue used for FTIR spectral measurement is obtained from experimental pigs. Freshly enucleated pig globes were kept refrigerated and irrigated using 0.9% sodium chloride solution. Corneas were excised from the eyes by a trained preparator using a hand trepan. After lyophilization treatment, the spectrum was measured using a FTIR spectrometer (Nicolet IN10, Thermo Fisher Scientific). Thirty-two accumulative scans were taken with a resolution of 4 cm−1, and the data was collected using OMNIC software (Thermo Fisher Scientific). Mice were placed in an anesthesia tank and filled with isoflurane at a dose of 0.41 ml/min. After the mice entered the induced state of anesthesia, the mice were euthanized by rapid neck-breaking, and the eyeballs were subsequently dissected and obtained. Normal corneal tissues were ablated as soon as possible after harvest. As for edematous corneal ablation, eyeballs were harvested and immersed instantly in hypotonic solution for 20 h. Subsequently, the edematous corneas were ablated immediately. The MIR laser was focused on the surface of corneas through a lens with a focal length of 25 mm. The pulse energy was chosen as 2 μJ and the scanning speed is designed as 4 mm s−1 or 2 mm−1 for different corneas with 2 scanning times. As for the experiment of NIR fs keratotomy, different pulse energies emitted from the pump source (Pharos, Light Conversion) were adjusted according to the requirement of depth and ablation conducted with the same focusing and scanning parameters and conditions. Immediately after ablation, tissue samples were fixed in 4% formaldehyde solution and sent for embedding, sectioning and staining with hematoxylin and eosin. Histological examination was carried out using microscope to observe the defect of each layer of corneal tissue. Corneal injury was determined based on the hematoxylin staining and the structure of cells around the incision.
Animals
All animal care and protocols were approved by the Animal Research Committee of West China Hospital of Sichuan University (No. 20220224055). All procedures were conducted in accordance with the “National Research Council’s Guide for the Care and Use of Laboratory Animals, Eighth Edition”. The 8-week-old male C57BL/6J were obtained from GemPharmatech (Jiangsu, China). Mice were maintained a 12-h light/12-h dark cycle and had free access to food. Given that all the corneas of the mice were normal and had not received any intervention, the mice were randomly selected for the experiments and grouped based on the experimental parameters. The grouping of mice and data analysis were carried out by two blinded observers.
Corneal keratotomy in Vivo
The adult C57BL/6J mice housed under standard conditions, weighing 20–25 g, were used for the in vivo keratotomy experiment. Mice were anesthetized by intraperitoneal injection of 40 mg/ml tribromoethanol (Sigma-Aldrich Chemicals, St. Louis, MO, USA) and applied with 5% proparacaine hydrochloride eye drops (Unither Pharmaceuticals, China) for surface anesthesia. The pupil of the study eye was dilated with topical 5% tropicamide (Santen Pharmaceutical Co., LTD., Osaka, Japan) to expose the ablation area. After wiping the residual solution on the surface of eyes, the mice were then fixed on the electrically driven translation platform, with the position adjusted to allow the direct incident of the MIR laser on the cornea surface. The MIR laser with a pulse energy of 2 μJ was focused on the corneal surface with a spot diameter of ~55 μm. The mice were randomized into three groups (n = 24/group), with each study group receiving the MIR laser of different scanning speed. After ablation, the surface of eye was rinsed with 100 μL buffer, and the ocular surface was instilled by 3 μL of 0.1% liquid sodium fluorescein (Alcon Laboratories, Inc., Texas, USA), followed by rinsing by the fluorescein with 100 μL buffer again. Corneal epithelial damage was subsequently examined using a cobalt blue light. Tobramycin and dexamethasone ophthalmic ointment were applied to the left eye once a day. ImageJ software (National Institutes of Health) was used for image processing, measuring the area of fluorescent staining. At each time points postoperatively, incisions were examined by fluorescent staining, and mice from different groups were randomly selected to enucleate the eyeballs for histological examination (n = 3/group). For biosafety verification, the full eyeballs were sectioned and stained with hematoxylin and eosin 1 month after the large-scale MIR fs ablation (n = 3/group).
Optical coherence tomography (OCT) and immunofluorescence
OCT and immunofluorescence were carried out on 1, 3 and 7 days after MIR-fs laser keratotomy. A total of 27 mice were used in this study (n = 9/group). After anesthesia, an anterior segment OCT system equipped with 25 D lens is utilized. Corneas were harvested at different time points (n = 3/group) and fixed in 4% paraformaldehyde for 30 min, thoroughly washed with phosphate buffered saline (PBS), blocked with 5% normal goat serum and Triton X-100 for 1 h at room temperature. The corneas were incubated with primary antibodies Anti ZO-1 rabbit (1:500; Proteintech, China) and Anti Na/k-ATPase mouse (1:500; Sigma-Aldrich Chemicals, USA) at 4 °C overnight, and corneas were incubated with secondary antibodies Goat-rabbit 488 and Goat-mouse 555 (1:500; Jackson ImmunoResearch, USA) respectively at 4 °C overnight. Corneal tissues were mounted endothelial side up on a slide and were imaged using fluorescent microscope. Three regions were randomly selected from each biopsy specimen and ImageJ was used to measure the endothelial cells density and fluorescence intensity.
Electroretinography (ERG)
ERG was conducted in baseline, Day 4 and Day 8 after keratotomy to evaluate retinal function in response to full-field flash stimuli under scotopic condition with dim red light (n = 15/group). The mice were dark-adapted overnight and pupils were dilated with topical 5% tropicamide. Followed by anaesthetizing, the mice were placed on the ERG ganzfeld. Full-field ERG (ESPION, Diagnosys LLC) was performed putting a ground electrode on the tail and inserting a reference electrode from the scalp between two ears. A golden-ring electrode was then gently positioned on the cornea. The LED-based system provides flash stimuli over a stimulus intensity of 1.0 cd·m/s2. Responses to brief flashes were analyzed primarily by measuring the latency of a-wave and the amplitudes of b-wave. The amplitude of the a-wave was measured from the baseline to the maximum a-wave peak, and the latency of a-wave was characterized from 0 ms to the timepoint of a-wave peak. The b-wave was subsequently measured from the nadir of the a-wave to the apex of the b-wave peak.
Visual cliff test
The cliff device was consisted of two overlapped open-top acrylic boxes (84 cm × 53 cm × 41 cm/50 cm). The bottom of each box was divided into two equal sides. The upper left and bottom right were affixed with 3-cm black-and-white checked photographic paper, while the upper right area is transparent to form a visual cliff. The upper transparent area is considered as the cliff zone, while the left area with checked photographic paper is conceived as the safe zone. The test was conducted in a quiet and dark room with sufficient adaption time. The mouse was put on the midline of upper box platform, and two sides were explored freely within 300 s (n = 15/group). The recorded video results were analyzed manually to calculate the safe zone time, cliff zone time, the preference index (time in the safe zone /total test time) and the normalized ratio of safe side (the preference index /baseline index).
Statistical and reproducibility
Each experiment was repeated at least three times. The statistical analysis was performed using GraphPad Prism (GraphPad Software Inc), and the results were expressed as mean ± standard error of the mean (SEM). One-way ANOVA was used to analyze the differences between three groups at the same time points, and two-way ANOVA followed by Bonferroni’s multiple comparisons test was employed to analyze the differences between groups by considering scanning speed and postoperative duration simultaneously. P < 0.05 indicates a statistically significant difference.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Results
The MIR femtosecond keratotomy platform and corneal ablation modeling
The in vivo minimally invasive laser keratotomy is performed based on a MIR femtosecond OPA emitting a wavelength of 6.1 μm aided with an electrically driven translational platform, as shown in Fig. 1a. The MIR OPA consists of two amplifier stages based on LiGaS2 (LGS) crystals cut for Type-Ι phase-matching36,37, pumped at 1.03 μm with a power of 20 W and a pulse width of 250 fs at a repetition rate of 50 kHz. The MIR laser at a central wavelength of 6.1 μm as shown in Fig. 1b, with an output power of 100 mW (pulse energy of 2 μJ) is obtained. The inset of Fig. 1b presents the MIR output beam with a good Gaussian profile which ensures a tightly focused beam from the laser keratotomy system. A homemade interference autocorrelator is employed to characterize the temporal profile of the MIR pulse, indicating a pulse width of ~200 fs, with the measured and retrieved interference autocorrelation traces shown in Fig. 1c. The MIR femtosecond output with a diameter of 4 mm is focused to the ocular surface of experimental animal through a lens with a focal length of 25 mm. Dedicated ablation patterns with designed motion trace, incision size and ablation speed are generated through an electrically driven translation platform.
a The experimental schematic of corneal ablation by a MIR fs OPA. HWP half-wave plate, A aperture, YAG yttrium aluminum garnet, LPF long pass filter (HT@1100–2000 nm); DM1 dichroic mirror (HT@1100–1600 nm, HR@1030 nm); LGS, LiGaS2 crystal; DM2, dichroic mirror (HT@5–11 μm, HR@1030 nm); Ge, germanium window (3–12 μm anti-reflective coated); BD, beam dump; L, lens (5–11 μm anti-reflective coated). Inset shows the result of a deep corneal ablation in a living mouse. b The measured spectrum of MIR fs OPA with a central wavelength of 6.1 μm. Inset shows the beam profile of the MIR OPA. c The measured (black) and retrieved (red) interferometric autocorrelation traces of the MIR fs pulse, indicating a typical pulse duration of ~200 fs. d Simulations of corneal temperature distribution and ablation depth under MIR fs laser irradiation with different number of pulses. e The histological image of the corneal incision with 100 MIR fs pulses, which agrees well with the simulated incision size and shape in (d). f The temperature rise of corneal surface in keratotomy by MIR fs laser as the ablation time increasing is calculated by the heat balance equation.
To understand and thus control the laser ablation process of cornea tissue by MIR fs pulses, the heat transfer model is established based on finite element method by solving the bioheat balance equation. Figure 1f shows the temperature evolution on the corneal surface as the irradiation time increasing. The temperature of corneal surface rapidly exceeds the threshold of protein denaturation (~60 oC or 330 K) and explosive water vaporization (~100 oC or 370 K) ablated by MIR fs pulses, and exhibits cyclical increasement, which realizes efficient corneal ablation. Due to the limitation of computing power, the simulation is not conducted longer than 2 ms. Figure 1d presents the ablation depth and temperature distribution of cornea tissue with different ablation time. As the number of pulses increases, the ablation goes deeper, and an incision depth of 30 μm is obtained ablated by 100 MIR fs pulses, i.e., an ablation duration of 2 ms. As a proof of the modeling accuracy, in vitro corneal ablation is performed with 100 MIR fs pulses, and a crater of a depth of ~30 μm is formed as shown in the histological image in Fig. 1e, which demonstrates the precision and controllability of the MIR fs laser keratotomy through pulse counting with the aid of the ultrafast bioheat model. It is worth noting that the ablation depth in the range of mm-level is almost linearly proportional to the processing time, and 40 ms ablation period is enough for penetrating a 600 μm thickness which is the average central thickness of a human cornea.
Comparison of cornea ablation using NIR and MIR fs lasers
Femtosecond laser assisted in-situ keratomileusis (LASIK) has become a routing technique of corneal sculpting in an effort to correct refractive errors. In addition, femtosecond lasers are the most commonly used laser tools to assist various techniques of corneal transplantation surgery. To tell the difference of laser corneal ablation between the traditional NIR and resonating MIR fs lasers used in ophthalmic surgery, normal and edematous corneas of mice are ablated in vitro by lasers at different wavelengths as a comparison. The characteristic absorption spectrum of the cornea sample is firstly measured using a Fourier transform infrared (FTIR) spectrometer. As shown in Fig. 2a, absorption peaks of cornea sample at 3 μm, 6.1 μm and 6.45 μm are revealed, which correspond to resonances of hydroxyl, amide Ι and II modes, respectively. As reported by our recently work, MIR wavelength resonating with amide-I mode could provide efficient tissue ablation with cellular-scale collateral damage24, thus, 6.1 μm is chosen as the MIR fs laser wavelength. At wavelengths near 1 μm, in the contrary, the cornea sample is transmitting nearly all the radiation power. Figure 2b–e, j–m presents the photos of corneal incisions at different wavelengths, and Fig. 2f–i, n–q is the corresponding histological images. When corneal ablation is performed at a wavelength of 6.1 μm with a pulse energy of 2 μJ, a deep incision with an ablation depth of ~110 μm is formed, as shown in Fig. 2b, f. It is worth mentioning that there is slight collateral damage observed through the interaction of resonating MIR fs lasers, as presented in Fig. 2f. When the laser wavelength is switched to 1.03 μm, with 250 fs pulse width and 3 μJ pulse energy, at the same 50 kHz repetition rate (conventional parameters of keratotomy fs laser)38, only a shallow scratch is observed, and only corneal epithelia could be cut, with an ablation depth of ~20 μm, revealed in Fig. 2c, g. Further increasing the pulse energy of the 1.03 μm fs laser to 16 μJ deepens the incision, however, severe collateral damage with a rough incision and a large denaturation zone is caused, as presented in Fig. 2d, h, attributed to tissue ionization by the high laser intensity which is approximately 230 times higher than that used for MIR laser keratotomy. In addition, due to the high transparency of cornea at the wavelength of 1.03 μm, when the laser focus slightly drifts away from the corneal surface, thermal shrinkage of corneal epithelium is observed, and the residual energy results in irreversible damage to iris and lens, as shown in Fig. 2e, i. It is worth noting that the damage on the lens exhibits an enlarged and irregular crater, which may be attributed to the beam distortion while the NIR laser transmitting through the cornea tissue. In the case of edematous corneas, the accumulation of water enlarges the separation between collagen bundles in the matrix, leading to a disordered structure, a closer distance between lens and cornea, and decrease in corneal transparency, as shown in Fig. 2m, q. Notably, to investigate the effect of deep keratotomy, the laser scanning speed is reduced to extend the action time on deep tissue of cornea. A deep incision can still be formed at wavelength of 6.1 μm with 2 μJ pulse energy, and it almost penetrates the corneal layer due to the extension of action time, as shown in Fig. 2j, n. In contrast, the extended action time of 1.03 μm laser with 3 μJ energy fails to increase the incision depth, but only causes collateral thermal damage around the incision, as shown in Fig. 2k, o. Further increasing the pulse energy to 16 μJ resulting in a deeper incision while a much larger area of thermal damage than that in normal corneal keratotomy, which may be due to the scattering of 1.03 μm laser in watery cornea. In addition, severe deformation of lens is observed in Fig. 2l, p, which may be attributed to the extrusion between cornea and lens in turgid eyeball, as well as the mechanical shock induced by high intensity laser.
a The measured Fourier transform infrared (FTIR) absorption spectrum of corneal tissue. The resonance modes are marked above the absorption peaks. Photos (b–e), (j–m) and corresponding histological images (f–i), (n–q) of corneal incisions under different laser wavelengths and pulse energy. b, f When corneal ablation is performed at a wavelength of 6.1 μm with a pulse energy of 2 μJ, a sharp penetrating incision with a depth of ~110 μm is formed. c, g As the laser wavelength is switched to 1.03 μm, with 3 μJ pulse energy, only a shallow scratch with an epithelial ablation depth of ~20 μm is observed. d, h Further increasing the pulse energy of the 1.03 μm femtosecond laser to 16 μJ deepens the incision, however, severe collateral damage with a rough incision and a large denaturation zone is caused. e When the focus of 1.03 μm laser with 16 μJ pulse energy slightly drifts away from the corneal surface, thermal shrinkage of corneal epithelium is observed, and significant irreversible damage to iris and lens is caused. j, n Penetrating incision can still be formed in edematous cornea with 6.1 μm laser. k, o 1.03 μm laser with 3 μJ energy fails to create deep incision, but only causes collateral thermal damage around the incision. l, p Further increasing the pulse energy to 16 μJ resulting in a deeper incision while causing severe corneal collateral damage and deformation of lens. m, q Intact edematous cornea. The incisions are marked by white arrows.
MIR fs keratotomy and healing investigation
Systematic in vivo experiments of MIR fs laser keratotomy are performed on corneas of C57BL/6J mice with three randomized groups. The left eyes of mice receive MIR fs laser surgery and are classified into the study groups, while their counterparts (corresponding right eyes) belong to the control groups. Each study group is subjected to ablation by MIR fs laser at different scanning speed, namely 4, 6 and 8 mm s−1 for Group 1, 2 and 3, respectively. The corneas are stained with fluorescein and recorded four times which are preoperatively (baseline), immediately (0 h), 3 days and 7 days after surgery. In normal corneal tissues, the epithelial cells are tightly arranged, and fluorescein could barely adhere to the surface. While the tight junction between cells is disrupted as damages occurs on corneal epithelial tissues, the fluorescein could easily fill gaps of corneal defects, generating green fluorescence under illumination39. As shown in Fig. 3a–c, compared to the baseline, the central parts of corneas in all study groups at 0 h exhibit significant positive fluorescein plaque identical to ablation traces. The incisions are stretched by the tension of ocular surface after surgery. Fluorescent staining areas sharply decrease for 3 days postoperatively, with corneal haze are observable at incisions (marked by white dashed arrows). After 7 days, corneas further heal without staining around the incision, implying smooth surfaces. Notably, for corneas in Group 1, slight haze could still be observed as shown in Fig. 3a, while pupils of the other 2 groups are clearly visible. Moreover, there is no any sign of inflammation or edema observed in all groups, which indicates that the epithelium has fully healed.
a–c Corneas are stained with fluorescein and recorded four times: preoperatively (baseline), immediately (0 h), 3 days (3 d) and 7 days (7d) after surgery. The laser scanning speeds are a 4 mm s−1 (Group 1), b 6 mm s−1 (Group 2), and c 8 mm s−1 (Group 3). The haze areas at incisions are marked by white dashed arrows. It is observed that fluorescent staining areas sharply decrease for 3 days postoperatively. d As a quantitative assessment, the ratio of corneal fluorescent staining area (fluorescence area/total corneal area) at different time points after MIR fs laser ablation is evaluated for each group of mice by an image analysis software. The means of fluorescence are calculated here with error bars indicating the standard error of the mean. All groups exhibit an effective reduction in the fluorescence area after 3 days (statistically significant (P < 0.0001)), and no statistical differences are measured between 3 and 7 days postoperatively (n.s., not significant). This means that most corneal incisions by MIR fs laser ablation could heal within 3 days. The average fluorescence ratio of Group 1, 2 and 3 is 0.047, 0.008 and 0.021, respectively. The ratio of Group 2 is much smaller than that of Group 1 (P = 0.0257) and 3, indicating that the ablation speed of 6 mm s−1 generates the least collateral damage. In 7 days postoperatively, the fluorescent staining ratio further decreases slightly, and there becomes no statistically significant differences among the three study groups.
The ratio of corneal fluorescence region (fluorescence area/total corneal area) at different time points after MIR fs laser keratotomy is evaluated by an image analysis software, as a quantitative measure of corneal healing. The mean ± SEM of fluorescence ratios are subsequently calculated, as shown in Fig. 3d. Immediately after MIR fs laser ablation, the fluorescence area ratios of three groups are similar, namely 0.265 ± 0.022, 0.277 ± 0.024 and 0.288 ± 0.026 for Group 1, 2, and 3, respectively. All groups exhibit an effective reduction in the fluorescence area after 3 days (statistically significant (P < 0.0001)), and no statistical differences are measured between 3 and 7 days postoperatively. This demonstrates that most corneal incisions by MIR fs laser ablation could heal within 3 days. In addition, distinct fluorescence areas among study groups are observable in 3 days postoperatively. As shown in Fig. 3d, the average fluorescence ratio of Group 1, 2 and 3 is 0.047 ± 0.014, 0.008 ± 0.003 and 0.021 ± 0.008, respectively. Notably, the ratio of Group 2 is much smaller than that of Group 1 (statistically significant (P = 0.0257)). The average fluorescent staining area level in Group 2 is also lower than that in Group 3, indicating that the ablation speed of 6 mm s−1 generates the least collateral damage under the used laser parameters. It is worth mentioning that deeper incision could be achieved by choosing the optimal ablation speed and moving the focal point. In 7 days postoperatively, the fluorescent staining ratio further decreases slightly, and there becomes no statistically significant differences among the three study groups.
After the MIR fs laser keratotomy, different groups of mice are sacrificed at various observation time points and eyeballs are enucleated. Ocular tissues are sectioned and stained with hematoxylin and eosin (H&E), then corneal histomorphology is observed under the microscope. Figure 4 shows the representative histological images of different groups. In control groups, the histological structure of cornea is distinguishable as the epithelium (the uppermost with darker-colored area) consisting of multilayered cells in a regular arrangement (see inset), the stromal layer (the middle layer in lighter-colored area) with evenly distributed collagen fibers exhibiting significant layer structure, and the endothelial layer (the downmost with darker-colored area) showing single-layer cells. Immediate postoperative histological images reveal that larger crater and deeper ablation are achieved with slower scanning speed thus longer ablation time, which is consistent with the simulation result. For Group 1, the incision penetrates almost the entire corneal layer. The ablation time decreases with the speed. Thus, in Group 2, the depth of the incision could reach the center of stromal layer, while in Group 3, only the epithelial layer and the superficial stroma are ablated. Healing of corneal incision in 3 groups can be observed in histological images in 3 days postoperatively, namely, new epithelial cells begin to cover the incision areas. Compared to the control group, the proportion of epithelial layer in Group 2 and 3 decreases as a result of epithelial cells transferring towards to the incisions. For Group 1 samples with slow ablation speed, the disturbed cellular arrangement of epithelium and uneven epithelial thickness at corneal incision is observed. The boundary between epithelial and stromal layers in Group 1 and 3 is deformed, and there are nucleus-free areas in stroma (marked by blue dotted circles) with cloudy structures, in contrast to the flat boundary and clear layered structure exhibited in Group 2. It is suggested that Group 1 with a slower ablation speed (4 mm/s) deposits excessive heat; while Group 3 with faster scanning speed (8 mm/s) has the heat accumulated around the crater rather than dissipated through deeper tissue evaporation due to the low ablation efficiency. Thus, both Group 1 and 3 have greater collateral damage compared to Group 2, which is also consistent with the fluorescent staining results as shown in Fig. 3. After 7 days, the proportion of epithelium from Group 2 and 3 is recovered to normal with clear layered structures and regular arrangement, as shown in histological images in Fig. 4b, c. The epithelium adheres well to the stroma, which has rarely difference with the control group. Notably, hyperproliferation of cells and epithelial ingrowth are observed in Group 1, and the epithelial layer is thicker than surrounding tissues at the incision (see inset). This is attributed to the larger crater width and collateral damage caused by the slow ablation speed in Group 1. No defect in corneal epithelial layer is observed in all study groups, which is consistent with the results of fluorescent staining. Therefore, it is suggested that the optimal ablation parameters of MIR fs laser such as the ablation speed and the number of scans should be chosen to ensure an incision depth while minimizing the crater width and the tissue heating.
The scanning speeds are a 4 mm s−1 (Group 1), b 6 mm s−1 (Group 2), and c 8 mm s−1 (Group 3). Insets show images with higher magnifications of marked areas. In 3 days postoperatively, the disturbed cellular arrangement of epithelium and uneven epithelial thickness at corneal incision is observed for Group 1 samples (a). The boundary between epithelial and stromal layers in Group 1 and 3 is deformed, and nucleus-free areas with cloudy structures in stroma are revealed in Group 1 and 3 as marked by blue dotted circles in (a, c). In contrast, a flat boundary and clear layered structure are exhibited in Group 2 samples (b). After 7 days, the proportion of epithelium from Group 2 and 3 is recovered to normal with clear layered structures and regular arrangement (b, c). Hyperproliferation of cells and epithelial ingrowth are observed in Group 1, and the epithelial layer is thicker than surrounding tissues at the incision (see inset) (a).
To further conduct a comprehensive evaluation of corneal healing, optical coherence tomography (OCT) and immunofluorescence are carried out on 1, 3 and 7 days after surgery mentioned above. The depth of corneal incisions in each group is measured and the results are demonstrated in Fig. 5a, b. At the first day after surgery, the depths of incision in each group are distinctly visible (dark areas in the cornea). Moreover, there are significant differences in the depth of incisions producing by different ablative parameters. Lower laser scanning speed is found to achieve deeper ablation, which is consistent with previously described histological images. 3 days after surgery, as the corneal healing, the depth defect presented in OCT images of each group decreased significantly (P < 0.0001). 7 days later, corneal defect has further diminished, and there is no significant difference in depth among the groups.
a OCT images of cornea at different time points. The dark area in the central cornea represents the incision generated by MIR-fs laser. b Corneal incision depth in study groups. c The expression of ZO-1 (green) and Na/K-ATPase (red) in the mouse corneal endothelium. Analysis of corneal endothelial cells density based on ZO-1 staining (d) and quantization of Na/K-ATPase-related fluorescence intensity (e). All data are means ± SEM. *P < 0.05, **P < 0.01, ****P < 0.0001, n.s. not significant.
ZO-1 and Na/K-ATPase are used to conduct immunofluorescence staining on the corneal endothelium for evaluating the function of endothelium, which respectively characterizes the structural integrity and regulation ability of osmotic pressure. As shown in Fig. 5c–e, compared to the control groups, the endothelial cells in study groups exhibit irregular shapes instead of typical hexagons, and there are blurred cell boundaries in some areas. The density of endothelial cells decreased on the first day postoperatively, with the ratios of study groups to the control groups being 0.79 ± 0.09, 0.78 ± 0.03 and 0.86 ± 0.14, respectively. This may be attributed to endothelial cell barrier dysfunction. In addition, the expression levels of Na/K-ATPase in Group1 and Group2 are lower than those in control groups, with the fluorescence intensity ratios as 0.80 ± 0.07 and 0.70 ± 0.06, respectively. As the corneal incision heals, the function of endothelial cells gradually recuperates. 7 days after operation, the corneal endothelium exhibits a continuous and regular layered structure. The ratios of endothelial cells density in each study group to that in control group are 0.96 ± 0.03, 0.99 ± 0.03 and 0.98 ± 0.03, respectively. Notably, the density in Group2 increased significantly (P = 0.0476). The fluorescence intensity ratios are 1.15 ± 0.05, 1.11 ± 0.09 and 1.08 ± 0.09, respectively, with Group 2 showing a significant increasement (P = 0.0033). These results indicate that under the ablative parameters established above, the morphology and function of endothelial cells can be restored as the cornea heals.
Biological safety evaluation of MIR fs Laser keratotomy
Having known that the MIR fs laser keratotomy has a superior corneal ablation efficiency and decent healing rate, it is crucial to further validate the biological safety. Therefore, zigzag ablation patterns with large incision areas covering the entire pupil where visual axis locates is designed, so that any damage in the pathway would impact on visual acuity, visual function, and retinal electrophysiologic responses to visual stimulation. As shown in Fig. 6a–c, the ablation trace covers almost the entire part of exposed cornea and ensures the pupil fully obscured by incisions. In 3 days postoperatively, different degrees of fluorescent staining areas are observable at corneal incisions of all study groups. Group 2 again shows the smallest colored area, with fluorescence only measured at the intersection of scanning trace, while Group 1 and 3 exhibit larger areas of fluorescence (marked by yellow dotted circles). After 7 days, the stained region mostly vanishes, indicating that the epithelial defects are largely healed, although a small area of fluorescence can still be observed in Group 1. In addition, incisions in the three study groups reveal distinct degrees of haze and reduction of the cornea transparency (marked by white dotted circles). As shown in Fig. 6a–c, Group 2 has much smaller haze area than those in Group 1 and 3. Subsequently, the eyeballs are sectioned and stained with hematoxylin and eosin 1 month after the surgery to study the healing through observing the histomorphology of cornea. As presented in Fig. 6d, e, all study groups are structurally intact and homogeneously distributed. Compared to control groups, the stroma of corneas in all study groups become thinner with different degrees due to large-scale ablation of this layer. Residual craters can still be observed in Group 1, nevertheless, in Group 2 smooth cornea without noticeable ablation trace is exhibited, thanks to the best ablation parameter for the healing process.
Zigzag ablation patterns with large incision areas covering the entire pupil where visual axis exists is designed, so that any damage in the pathway would impact on visual acuity, visual function, and retinal electrophysiologic responses to visual stimulation. Corneas are stained with fluorescein and recorded four times: preoperatively (baseline), immediately (0 h), 3 days (3 d) and 7 days (7d) after surgery. The laser scanning speeds are a 4 mm s−1 (Group 1), b 6 mm s−1 (Group 2), and c 8 mm s−1 (Group 3). In 3 days postoperatively, Group 2 shows the smallest colored area, with fluorescence only measured at the intersection of scanning trace, while Group 1 and 3 exhibit larger areas of fluorescence (marked by yellow dotted circles). After 7 days, the stained region mostly vanishes, indicating that the epithelial defects are largely healed, although a small area of fluorescence can still be observed in Group 1. Incisions in the three study groups reveal distinct degrees of haze and reduction of the cornea transparency (marked by white dotted circles). As in (a–c), group 2 has much smaller haze area than those in group 2 and 3. d Histological images of eyeballs which are sectioned and stained with hematoxylin and eosin 1 month after the surgery with different scanning speed. e present the corresponding histological images of control groups. All study groups are structurally intact and homogeneously distributed. Compared to control groups, while residual craters can still be observed in Group 1, notably in Group 2, smooth cornea without noticeable ablation trace is exhibited, thanks to the best ablation speed and thus least collator damage.
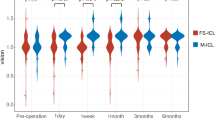
Knowing that the retina after injury has a limited repair capacity, any damage to the retina could lead to permanent visual acuity loss40. Furthermore, adverse reactions such as corneal opacity and cataract that obstruct the optical pathway may also influence the conversion and conduction of signals in eyes. Therefore, the assessment of postoperative retinal reaction is a critical gauge for evaluating the biological safety of MIR fs laser keratotomy, which is subsequently evaluated by electroretinography (ERG). The latency of a-wave in ERG waveforms reflects the time required for photoreceptor to receive light and begin converting it into electrical signal, while the amplitude of b-wave is the major component of ERG that reflects the strength of electrical signal converted and conducted by retinal cells. In previous researches, they have been used to evaluate the adverse events caused by retinal projection laser and ultraviolet radiation in collagen cross-linking for corneal diseases41,42. The influence of light transmission in cataract patients’ eyes can also be estimated by ERG43. Responses to brief flashes (shown in Fig. 7a) are analyzed primarily by measuring the latency of a-wave and the amplitudes of b-wave, where a-wave and b-wave is the first negative and first maximum positive wave reflecting outer and inner retinal function, respectively (shown in Fig. 7b). The impact of MIR fs laser keratotomy on retinal function and ocular pathway is thus evaluated by comparing the data between control and study groups at various observation time points, as shown in Fig. 7c. The mean interocular latency differences of a-wave are measured as 0.58 ± 0.35 ms, 0.01 ± 0.37 ms, 0.11 ± 0.62 ms (P > 0.05) before ablation, 0.53 ± 1.16 ms, 0.04 ± 0.48 ms, 0.00 ± 0.35 ms (P > 0.05) on Day 4 and -0.72 ± 0.86 ms, 0.02 ± 0.62 ms, 0.00 ± 0.73 ms (P > 0.05) on Day 8 for Group 1–3, respectively, as shown in Fig. 7d. The mean interocular amplitude of b-wave are 5.16 ± 21.21 μV, 16.10 ± 14.92 μV, −0.95 ± 16.88 μV (P > 0.05) before ablation, 61.44 ± 31.20 μV, 89.23 ± 35.00 μV, −7.16 ± 36.44 μV (P > 0.05) on Day 4 and −13.26 ± 43.89 μV, −36.48 ± 15.08 μV, −4.65 ± 17.23 μV (P > 0.05) on Day 8, for Group 1–3, respectively, as shown in Fig. 7e. No significant latency and amplitude differences are found in three groups after large-area ablation, which indicates the MIR fs laser keratotomy does not cause obvious retinal function abnormalities and obstruction to ocular optical pathway. Histological images of eyeballs in all groups also exhibit no damage to the structures of retina and other ocular tissues after large-area keratotomy, as shown in Supplementary Fig. S1.
a Experimental photo of in vivo retinal function evaluation by electroretinography (ERG). b Typical waveform of ERG under scotopic condition, where a-wave is the first negative wave which reflects outer retinal function and b-wave is the first maximum positive wave which reflects inner retinal function. c Representative measured waveforms of ERG before and 8 days after large-area keratotomy. The difference of latency and amplitude between control and study groups are shown in (d) and (e) respectively. No significant latency and amplitude differences are found in the three groups after large-area ablation, which indicates the MIR fs laser keratotomy does not cause obvious retinal function abnormalities and obstruction to ocular optical pathway. f Schematic diagram of the visual cliff tests. g The normalized ratio of safe side at different postoperative time points. It shows that there are almost no abnormalities in visual behavior caused by the large-area MIR fs laser keratotomy. All data are means ± SEM. n.s. not significant.
In addition, the visual cliff test is conducted to evaluate the visual function impairment caused by MIR stimulation. Visual cliff test is an objective method for evaluating visual function, which has been used in previous studies to detect gross abnormality in the optical pathway and retina44. As presented in Fig. 7g, on Day 3 after large-area keratotomy, the mean normalized ratios of choosing the safe side (left area in Fig. 7f) are measured as 1.18 ± 0.08, 1.06 ± 0.14, and 1.06 ± 0.09 contrast to the baseline (P > 0.05), which means there are almost no abnormalities in visual behavior test. On Day 7, the mean normalized ratio of safe side for all groups remains close to 1.0 showing 1.24 ± 0.18, 1.14 ± 0.11, and 1.07 ± 0.09 for Group 1, 2 and 3 respectively, which is consistent with the preoperational level.
Discussion
Efficient and precise corneal incisions are essential for laser-assisted keratotomy, particularly in corneal transplantation procedures requiring deep or penetrating cuts of diseased corneal tissue while minimizing collateral damage. This is especially important for endothelial cells to achieve a good adhesion of donor and recipient, improve postoperative astigmatism, and reduce the risk of adverse reactions. However, when the conventional NIR fs laser is used for corneal transplantation, the scattering caused by diseased tissue and low absorption at NIR wavelength may significantly reduce the incision accuracy and effective depth of penetration. Given the fact that corneal transplantations are mostly related to pathologies that cause edema28, perturbations of the fibrous structure thus causes a reduction of corneal transparency and exacerbation of scattering, which substantially depletes the laser energy and compromises the focused beam quality, resulting in an undesirable laser incision. Unfortunately, the loss caused by scattering could not be simply compensated by increasing the pulse energy, which could cause even stronger distortion of spot, resulting in unwanted side effects45. To address scattering limitations, which scales inversely proportional to λ4, keratotomy could be performed by shifting the wavelength to MIR region. At the laser wavelength of 6.1 μm resonating with amides and the OH-stretch mode of water, efficient penetrating corneal ablation could be realized with almost eliminated scattering. Results of edematous corneas ablation indicates that MIR-fs laser can achieve deep keratotomy with varying thicknesses by simply adjusting ablation duration and laser focus, enabling different types of keratoplasty, such as anterior lamellar, endothelial and penetrating keratoplasty. For precise ablation depth control, MIR fs laser corneal ablation can achieve micrometer-level precision using a fast laser beam shutter with sub-ms exposure time, as evidenced by simulation results. Additionally, MIR lasers deliver significantly lower intensity than NIR fs lasers, reducing stress on corneas, thereby avoiding damage to endothelial cells and high intraocular pressure, which ensures better donor-recipient matching and improves postoperative astigmatism in corneal transplants. Previous in vitro experiments and mice keratotomy studies demonstrate cellular-scale collateral damage by resonant MIR fs laser ablation, beneficial for reducing adverse complications in penetrating corneal surgery24. Thirdly, MIR lasers keratotomy is a cutting process from surface towards interior of the cornea, therefore, only an extremely small amount of energy can be directly transmitted to the deeper layers of the tissue, which offers enhanced safety for ophthalmic surgeries. Currently, the clinical translation of MIR-fs laser still encounters numerous challenges. Development of surgical platform entails the design of transmission system for femtosecond laser with special wavelength. Compared to those in the visible and NIR spectral ranges, the technologies related to MIR-fs laser are less mature nor optimized. Tremendous efforts have been made to achieve the efficient transmission of MIR-fs laser, such as the investigation of hollow-core fiber optics22,46, and we believe that MIR-fs laser would emerge as a promising tool for precise surgical procedures combine with these technologies.
In summary, deep keratotomy on living mice is performed based on a MIR fs laser tuned to the wavelength of 6.1 μm resonant with the amide-Ι vibrational mode. The penetrating incision with superior postoperative healing process is demonstrated to validate the high ablation efficiency and minimal collateral damage as a new technique for keratotomy. Histological imaging, fluorescein staining and immunofluorescence reveal that deep corneal incisions ablated by MIR fs laser can heal within 3 days by choosing optimal ablation parameters. Subsequent investigations into postoperative retinal and visual function following large-area laser ablation demonstrate the biological safety of MIR fs keratotomy. Visual cliff and electrophysiology indexes of mouse retina remain consistent with baseline levels post-surgery, indicating no abnormalities in gross visual function, optical signal transmission in mouse eyes, or retinal function damage. With the advancement in engineering and integration of the MIR fs OPA, deep corneal ablation and cornea transplantation could be pursued with a cellular-scale precision. Various ablation depths, according to the specific keratotomy requirements could be well controlled by counting the MIR fs pulse number. In addition, the resonant MIR fs laser keratotomy, devoid of ionization explosion processes and offering significantly lower intensity than conventional NIR fs lasers, eliminates damage to endothelial cells and improves postoperative astigmatism in corneal transplants. We anticipate that by leveraging existing beam control and guiding techniques in LASIK, keratotomy equipped with MIR fs OPA will emerge as a groundbreaking clinical tool in ophthalmic surgery and therapy.
Data availability
The source data for all figures can be found in Supplementary Data. The source data of MIR spectrum for Fig. 1 is in Supplementary Data Fig. 1b. The source data of MIR spectrum for Fig. 1 is in Supplementary Data Fig. 1b. The measured and retrieved MIR fs pulse for Fig. 1 is in Supplementary Data Fig. 1c. The source data of corneal temperature simulation for Fig. 1 is in Supplementary Data Fig. 1f. The source data of FTIR absorption spectrum for Fig. 2 is in Supplementary Data Fig. 2a. The ratio of corneal fluorescent staining area for Fig. 3 is in Supplementary Data Fig. 3d. The Corneal incision depth for Fig. 5 is in Supplementary Data Fig. 5b. The endothelial cells density and fluorescence intensity is in Supplementary Data Fig. 5d and Fig. 5e, respectively. The latency and amplitude of ERG for Fig. 7 is in Supplementary Data Fig. 7d and Fig. 7e, respectively. The source data of visual cliff is in Supplementary Data Fig. 7g. The data that support the findings of this study are available from the corresponding author upon request. Correspondence should be addressed to HouKun Liang: hkliang@scu.edu.cn
References
Aristeidou, A. et al. The evolution of corneal and refractive surgery with the femtosecond laser. Eye Vis. 2, 1–14 (2015).
Chee, S. P., Chan, N. S. W., Yang, Y. N. & Ti, S. E. Femtosecond laser-assisted cataract surgery for the white cataract. Br. J. Ophthalmol. 103, 544–550 (2019).
Tan, D. T. H., Dart, J. K. G., Holland, E. J. & Kinoshita, S. Ophthalmology 3 corneal transplantation. Lancet 379, 1749–1761 (2012).
Trokel, S. L., Srinivasan, R. & Braren, B. Excimer laser-surgery of the cornea. Am. J. Ophthalmol. 96, 710–715 (1983).
Erie, J. C., McLaren, J. W., Hodge, D. O. & Bourne, W. M. Recovery of corneal subbasal nerve density after PRK and LASIK. Am. J. Ophthalmol. 140, 1059–1064 (2005).
Fung, S. S. M., Aiello, F. & Maurino, V. Outcomes of femtosecond laser-assisted mushroom-configuration keratoplasty in advanced keratoconus. Eye 30, 553–561 (2016).
Lazare, S., Hoh, P. D., Baker, J. M. & Srinivasan, R. Controlled modification of organic polymer surfaces by continuous wave far-ultraviolet (185 nm) and pulsed-laser (193 nm) radiation-XPS studies. J. Am. Chem. Soc. 106, 4288–4290 (1984).
Mrochen, M., Semshichen, V., Funk, R. H. W. & Seiler, T. Limitations of erbium:YAG laser photorefractive keratectomy. J. Refract. Surg. 16, 51–59 (2000).
Peyman, G. A., Badaro, R. M. & Khoobehi, B. Corneal ablation in rabbits using an infrared (2.9-microns) erbium: YAG laser. Ophthalmology 96, 1160–1170 (1989).
Walsh, J. T., Flotte, T. J. & Deutsch, T. F. Er: YAG laser ablation of tissue - effect of pulse duration and tissue-type on thermal-damage. Lasers Surg. Med. 9, 314–326 (1989).
Stojkovic, B. et al. Q-switched erbium:YAG laser corneal trephination: thermal damage in corneal stroma and cut regularity of nonmechanical Q-switched erbium:YAG laser corneal trephination for penetrating keratoplasty. Cornea 23, 50–60 (2004).
Deshmukh, R., Stevenson, L. J. & Vajpayee, R. B. Laser-assisted corneal transplantation surgery. Surv. Ophthalmol. 66, 826–837 (2021).
Welch, A. J., & Van Gemert, M. J. Optical-thermal response of laser-irradiated tissue (Springer, 2011).
Gattass, R. R. & Mazur, E. Femtosecond laser micromachining in transparent materials. Nat. Photonics 2, 219–225 (2008).
Chung, S. H. & Mazur, E. Surgical applications of femtosecond lasers. J. Biophotonics 2, 557–572 (2009).
Sugioka, K. & Cheng, Y. Ultrafast lasers-reliable tools for advanced materials processing. Light Sci. Appl. 3, e149 (2014).
Chamberlain, W. D., Rush, S. W., Mathers, W. D., Cabezas, M. & Fraunfelder, F. W. Comparison of femtosecond laser-assisted keratoplasty versus conventional penetrating keratoplasty. Ophthalmology 118, 486–491 (2011).
Plamann, K. et al. Ultrashort pulse laser surgery of the cornea and the sclera. J. Opt. 12, 30 (2010).
Donner, R. & Schmidinger, G. Effects of femtosecond laser-assisted trephination on donor tissue in liquid interface as compared to applanated interface. Acta Ophthalmol. 100, e409–e413 (2022).
Birnbaum, F., Wiggermann, A., Maier, P. C., Böhringer, D. & Reinhard, T. Clinical results of 123 femtosecond laser-assisted penetrating keratoplasties. Graefes Arch. Clin. Exp. Ophthalmol. 251, 95–103 (2013).
Joos, K. M., Shen, J. H., Shetlar, D. J. & Casagrande, V. A. Optic nerve sheath fenestration with a novel wavelength produced by the free electron laser (FEL). Lasers Surg. Med. 27, 191–205 (2000).
Shen, J. H., Harrington, J. A., Edwards, G. S. & Joos, K. M. Hollow-glass waveguide delivery of an infrared free-electron laser for microsurgical applications. Appl. Opt. 40, 583–587 (2001).
Edwards, G. et al. Tissue ablation by a free-electron laser tuned to the amide-II band. Nature 371, 416–419 (1994).
Tian, K. et al. Tissue ablation with multi-millimeter depth and cellular-scale collateral damage by a femtosecond mid-Infrared laser tuned to the amide-I vibration. Laser Photonics Rev. 2, 2300421 (2024).
Edwards, G. S. Mechanisms for soft-tissue ablation and the development of alternative medical lasers based on investigations with mid-infrared free-electron lasers. Laser Photonics Rev. 3, 545–555 (2009).
Sun, W. S., Shen, J. H., Shetlar, D. J. & Joos, K. M. Endoscopic goniotomy with the free electron laser in congenital glaucoma rabbits. J. Glaucoma 9, 325–333 (2000).
Shah, R. J., Shen, J. H. & Joos, K. M. Endoscopic free electron laser technique development for minimally invasive optic nerve sheath fenestration. Lasers Surg. Med. 39, 589–596 (2007).
Peyrot, D. A. et al. Effect of incident light wavelength and corneal edema on light scattering and penetration: laboratory tudy of human corneas. J. Refract. Surg. 26, 786–795 (2010).
Pupeza, I. et al. High-power sub-two-cycle mid-infrared pulses at 100 MHz repetition rate. Nat. Photonics 9, 721–724 (2015).
Zou, X. et al. Flat-top pumped multi-millijoule mid-infrared parametric chirped-pulse amplifier at 10 kHz repetition rate. Laser Photonics Rev. 15, 9 (2021).
Zhang, J. W. et al. Multi-mW, few-cycle mid-infrared continuum spanning from 500 to 2250cm-1. Light Sci. Appl. 7, 17180 (2018).
Hutson, M. S., Hauger, S. A. & Edwards, G. Thermal diffusion and chemical kinetics in laminar biomaterial due to heating by a free-electron laser. Phys. Rev. E 65, 6 (2002).
McIntosh, R. L. & Anderson, V. A comprehensive tissue properties database provided for the thermal assessment of a human at rest. Biophys. Rev. Lett. 5, 129–151 (2010).
Vogel, A. & Venugopalan, V. Mechanisms of pulsed laser ablation of biological tissues. Chem. Rev. 103, 577–644 (2003).
Jacques, S. L. & Prahl, S. A. Modeling optical and thermal distributions in tissue during laser irradiation. Lasers Surg. Med. 6, 494–503 (1987).
Qu, S. Z. et al. 9 μm few-cycle optical parametric chirped-pulse amplifier based on LiGaS2. Opt. Lett. 44, 2422–2425 (2019).
He, L. et al. Dual-wavelength spectrum-shaped midInfrared pulses and steering high-harmonic generation in solids. Ultrafast Sci. 3, 0022 (2023).
Linke, S. J. et al. A new technology for applanation free corneal trephination: the picosecond infrared laser (PIRL). PLoS One 10, 12 (2015).
Guo, X. Y. et al. PPAR-α agonist fenofibrate ameliorates sjogren syndrome-like dacryoadenitis by modulating Th1/Th17 and treg cell responses in NOD mice. Invest. Ophthalmol. Vis. Sci. 63, 10 (2022).
Youssef, P. N., Sheibani, N. & Albert, D. M. Retinal light toxicity. Eye 25, 1–14 (2011).
Stohr, M., Dekowski, D., Bechrakis, N., Oeverhaus, M. & Eckstein, A. Evaluation of a retinal projection laser eyeware in patients with visual impairment caused by corneal diseases in a randomized trial. Ophthalmology 131, 545–556 (2023).
Lazaridis, A. et al. Revisiting the safety of the corneal collagen crosslinking procedure: evaluation of the effect of ultraviolet a radiation on retinal function and structure. Cornea 39, 237–244 (2020).
Yamauchi, Y., Mochizuki, J.-I., Hirakata, A. & Uda, S. Single flash electroretinograms of mature cataractous and fellow eyes. Clin. Ophthalmol. 10, 2031–2034 (2016).
Krishnamoorthy, V., Jain, V., Cherukuri, P., Baloni, S. & Dhingra, N. K. Intravitreal injection of fluorochrome-conjugated peanut agglutinin results in specific and reversible labeling of mammalian cones in vivo. Invest. Ophthalmol. Vis. Sci. 49, 2643–2650 (2008).
Nuzzo, V. et al. In situ monitoring of second-harmonic generation in human corneas to compensate for femtosecond laser pulse attenuation in keratoplasty. J. Biomed. Opt. 12, 11 (2007).
Deng A., et al. Microjoule-level mid-infrared femtosecond pulse generation in hollow-core fibers. Laser Photonics Rev. 17, 2370030 (2023).
Acknowledgements
This work was supported by National Natural Science Foundation of China (U22A2090, W2411056, 82101144, and 82070996), Sichuan Outstanding Youth Science and Technology Talents (2022JDJQ0031), Engineering Featured Team Fund of Sichuan University (2020SCUNG105), and Natural Science Foundation of Sichuan Province (2022NSFSC0824).
Author information
Authors and Affiliations
Contributions
J.G. and P.C. contributed equally to this work. H.L. and X.W. conceived and designed the experiment. J.G., M.X., K.T., L.H., W. L, Y. P. and Z.W. built the MIR OPA. J.G. and M.X. designed the keratotomy platform. H.L. and J.G. conducted the theoretical simulations. X.P. provided the ocular tissues. L.L. and P.C. designed the biology experiments. J.G. and P.C. performed the biology experiments and analyzed the data. H.L., J.G. and P.C. wrote the manuscript. H.L., W.L, Y.P., Q.J. Wang and Y.L. acquired the funding and resources. All authors discussed the results and contributed to the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Communications Medicine thanks Weiwei Liu and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. [Peer review reports are available].
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Guo, J., Chen, P., Xiang, M. et al. In vivo keratotomy by mid-infrared femtosecond laser resonant with amide vibrational mode. Commun Med 5, 207 (2025). https://doi.org/10.1038/s43856-025-00928-1
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s43856-025-00928-1