Abstract
Background
Iron deficiency, anemia, and infectious diseases contribute largely to the disease burden among children in Sub-Saharan Africa. Accurate assessment of iron status and its relationship with infections is essential for refining iron supplementation strategies.
Methods
We report retrospectively analyzed data from a cross-sectional study of children aged 2–17 years with acute febrile illness (fever ≤7 days) in Lambaréné, Gabon (NCT03047642). Symptom-based microbiological testing identified infection etiology. Blood count, C-reactive protein, iron parameters, and cytokines levels assessed iron deficiency, anemia, and immune activation.
Results
Among 415 screened children with acute febrile illness, hemoglobin and iron parameters are available in 197. Of those, 145 (73.6%) are anemic: 53 (36.6%) show anemia of inflammation (AI), 11 (7.6%) iron-deficiency anemia (IDA), and 29 (20.0%) combined AI/IDA. Others are categorized as multifactorial, with mostly microcytic anemia, transferrin saturation (TSAT) ≥ 20% and varying ferritin levels. TSAT is negatively associated with IL-10, IL-6, and IL-2 in the malaria-positive group, with IL-10 also showing a positive correlation with parasitemia counts. In malaria-negative children with undetermined pathogens, IFN-γ and IL-4 levels are positively associated with TSAT and ferritin.
Conclusions
These findings highlight iron dyshomeostasis in infectious diseases and confirm associations between iron availability and immune activation to causative pathogens.
Plain language summary
Iron deficiency and anemia are common in children living in Sub-Saharan Africa, especially during infections. The way the body reacts to infections affects how iron is used and stored, which can complicate diagnosis and treatment of these conditions. In this study, researchers looked at iron levels, immune system markers, and the causes of febrile illness in Gabonese children. The results show that many of these children had anemia caused by inflammation and disrupted iron balance, often linked to malaria and other infections. Different markers of immune activation during infection were related to how much iron was available in the blood. These findings can help improve iron supplementation strategies while reducing the risks associated with iron use during active infections.
Similar content being viewed by others
Introduction
Iron deficiency (ID) and anemia pose significant global health concerns, particularly affecting children in sub-Saharan Africa1,2. Nutritional iron deficiency anemia (IDA) accounted for an estimated 66.2% of total anemia cases worldwide in 20212. IDA adversely affects children’s mental and motor development and is associated with many social disadvantages3. Despite the significance of iron in this context, in 2019, the leading causes of death for children in this region were malaria, lower respiratory tract infections, and diarrheal diseases1.
A pivotal clinical trial in 2006 on dietary iron supplementation in children under five years of age on Pemba Island, Zanzibar, reported an increased incidence of malaria and infection related deaths in the iron-supplemented group4. This so-called Pemba trial raised concerns about the safety of systematic iron supplementation. Subsequent in vitro and animal studies supported these findings, indicating that iron supplementation increases susceptibility to and impairs control of various infectious diseases5,6. Since then, studies have also demonstrated a reduction in malaria incidence and severity among iron-deficient groups7,8,9. Recent studies have linked high iron stores to an increased risk of and worse outcomes from bacterial infections10,11.
Despite these findings, other research suggests that iron supplementation is safe and does not increase clinical malaria risk in children or anemic pregnant women when combined with insecticide-treated bed nets and antimalarial treatment12. Iron overload alters T helper 1 (Th1) cell-mediated immunity through changes in myeloid cell functions and interferon-γ (IFN-γ) signaling, whereas ID impairs lymphocyte proliferation due to their reliance on transferrin-bound iron uptake13. Given these complexities, it is evident that immune activation and iron metabolism are closely linked.
Here, we present data on the relationship between iron metabolism and immune activation in children aged 2–17 years with acute febrile illness (AFI) in Lambaréné, Gabon. Our findings reveal a high prevalence of anemia associated with inflammation and highlight the link between immune activation and iron availability in this population.
Materials and methods
Study design and population
This retrospective cross-sectional study was conducted in participants screened for the BFF-Dx study14 at the Centre de Recherches Médicales de Lambaréné (CERMEL) in Lambaréné, Gabon, from May through November 2019. The study site is located in Gabon’s Moyen-Ogooué Province and has moderate to high year-round malaria transmission. Children aged 2–17 years presenting at the outpatient clinic with ongoing fever, or a history of fever ≤7 days, were included. Patients with signs of severe illness were excluded. The analysis was conducted obeying the Declaration of Helsinki and following ICH-GCP. Approval from both institutional and national ethics committees (Comité National d’Ethique pour la Recherche, CNER, N°0078/2019PR/SG/CNER) as well as informed consent from parents or legal guardians was obtained, and written assent was acquired from participants aged 13–17 years. Detailed information on the study protocol of the BFF-Dx study has been published previously14.
Procedures
Fever at presentation was characterized by an axillary temperature > 37.5 °C. Extensive symptom-based testing was performed, and patients were stratified according to predefined case definitions as outlined in the published study protocol14. Established laboratory criteria, detailed by Escadafal et al.14, included positive PCR or antigen rapid diagnostic testing, a fourfold increase in antibody titers, or direct identification via microscopy. Malaria testing was performed by thick blood smear (TBS) technique, smears were assessed by up to three independent analyzers, and parasite counts were obtained using the WHO standard method.
Plasma ferritin, plasma transferrin, and serum iron (SI) levels were assessed using an automated analyzer (Cobas 311; Roche Diagnostics, Rotkreuz, Switzerland). Plasma concentrations of hepcidin and soluble transferrin receptor (sTfR) were analysed by ELISA kits with a detection range of 1.57–100 ng/ml and 31.25–2000 pg/ml, respectively (MyBioSource, San Diego, CA, USA; catalog numbers MBS8807155 and MBS8808159, respectively). Interleukin (IL) −2, −4, −6, −8, −10, tumor necrosis factor α (TNF-α), and IFN-γ were measured in serum using a multiplex bead array kit (Bio-Rad, Hercules, CA, USA; catalog number M50000007A) with a Luminex 200 system (ThermoFisher, Massachusetts, US). Data on full blood count (Yumizen H500 and H550, Horiba, Kyoto, Japan) and CRP (Nycocard CRP device, Abbott, Illinois, US) were available in most patients.
Transferrin saturation (TSAT) was calculated from SI concentrations using the following formula [(SI in µmol/L/transferrin g/L × 25.1) × 100]15. Reference values for hematological parameters specific to this study population have been published previously.16 Cohort-based reference values for ferritin and transferrin in European children aged 3–15 years were recently reported by Floegel et al.17.
Outcomes
Participants were stratified into age groups to match WHO guidelines for anemia diagnosis18.
Only laboratory-confirmed cases of AFI were used for the initial classification, which comprised non-bacterial infections, namely viral, fungal, protozoal, and helminth infections, bacterial infections, and AFI cases without an identified pathogen. These were subsequently grouped in TBS negative (M[−]) without identified pathogen (Undetermined), M[-] and confirmed bacterial or non-bacterial infection (B/NB), TBS positive (M[+]) without co-infection (Malaria) and M[+] with bacterial or non-bacterial co-infection (Malaria + B/NB). Anemia was defined according to WHO-guidelines18 and classified further according to ferritin levels and TSAT into those with anemia of inflammation (AI; TSAT < 20%, ferritin > 100 µg/L), iron deficiency anemia (IDA; TSAT < 20%, ferritin <30 µg/L), anemia of inflammation with possible iron deficiency anemia (AI/IDA; TSAT < 20%, Ferritin 30–100 µg/L) and multifactorial anemia (TSAT ≥ 20%). ID in general was defined as TSAT < 20%, consequently termed absolute ID (ferritin <100 µg/L) and functional ID (ferritin ≥ 100 µg/L); iron replete (IR) individuals were defined as TSAT ≥ 20%. Inflammation was specified as CRP > 5 mg/L. Malaria status was determined according to TBS.
Statistical analysis
The sample size was determined for the parent study based on a previously published formula19 and has been published elsewhere14.
Continuous variables are presented as medians with interquartile ranges (IQR; 25th–75th percentile) due to non-normal distributions, while categorical variables are reported as counts (n) and percentages.
Differences between two independent groups were assessed using the Mann–Whitney U test, while comparisons across three or more independent groups were performed using the Kruskal–Wallis test. Pairwise post hoc comparisons were conducted using the Mann–Whitney U test, with the Benjamini-Hochberg (BH) procedure applied to adjust for multiple testing. Effect sizes for the Mann–Whitney U test were calculated using the formula: r[U] = Z/√N. Categorical variables were compared using the Chi-squared test with Yates’ continuity correction. If > 20% of expected cell counts were <5, Fisher’s exact test was applied. Effect sizes were quantified using Cramér’s V (V) for Chi-squared tests and odds ratios (ORs) for contingency tables. Fisher’s exact test with BH adjustment was used for post hoc row-wise and pairwise comparisons. Wilson’s method was used to calculate 95% confidence intervals (CIs) for prevalence estimates.
The effect of malaria status on anemia was assessed by univariable logistic regression. Malaria exposure was determined by TBS and the outcome anemia according to previously mentioned age- and sex-adjusted cut-offs. Influences of sex and age on model performance were assessed via likelihood ratio test, opting for the unadjusted model. To explore the impact of body temperature, fever duration, inflammation, and malaria infection on ID (defined as TSAT < 20%), a separate multivariable logistic regression model was used. Exposure variables were selected based on clinical importance and dichotomized using predefined criteria (fever duration ≥ 3 days, CRP > 5 mg/L, and TBS pos status) except for body temperature, which was treated as a continuous variable. Linearity of the continuous variables with respect to the logit of the dependent variable was visually confirmed. Age and sex-adjusted analyses were performed separately, with the final model selected based on Tjur’s R² comparison. ORs and their corresponding 95% CI were calculated for both logistic regression analyses. Anemia severity and iron deficiency subtypes were analyzed using contingency tables to assess their association with malaria status, with ORs and corresponding 95% CIs reported.
Spearman’s rank correlation coefficient (ρ) was used to assess relationships between continuous variables, with 95% CIs calculated via Fisher's z-transformation.
All analyses were performed on complete cases. Missing data were predominantly due to procedural and technical constraints (e.g., insufficient sample volume for repeat assays) and were assumed to be missing at random. To ensure comparability of findings across analysis subsets resulting from complete case analysis (see Fig. 1), baseline characteristics were assessed, with detailed information provided for each subset in the Supplementary Material (Supplementary Table 1).
This flow diagram illustrates the number of patients from the eligible study population (N = 415) who had all the required parameters available for the respective analyses. The analysis subgroups represent the intersections of these groups where all parameters of interest are available. The flow diagram should be interpreted within the context of a complete case analysis. * Anemia analysis group, # Iron deficiency analysis group, § Cytokine analysis group; Abbreviations: FT ferritin, TF transferrin, SI serum iron, Hepc hepcidin, sTfR soluble transferrin receptor, B/NB bacterial or non-bacterial.
All reported p-values are two-sided and were adjusted using the BH procedure, controlling the false discovery rate at 5% per table or pairwise comparison. P-values remain unadjusted in tables reporting patient demographic and clinical information (Table 1) and exploratory correlation analyses (Fig. 3), with the significance level was set at α = 0.05.
Statistical analyses were performed using R statistical software (Version 4.2.1, R Core Team 2021) using the packages tidyverse20, stringdist, writexl, expss, ggpubr, ggsci, corrplot, ggflowchart, finalfit, UpsetR21, rstatix, epiR, Hmisc, DescTools, performance, gt, and gtsummary22.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Results
Overall, 417 participants with AFI presenting at the outpatient clinic were screened for eligibility and 415 children (227 female, 54.7%; 188 male, 45.3%) were included in this analysis (Fig. 1). Median (IQR) age was 6.0 (4.0–10.0) years and most children (n = 202, 48.7%) were in the age group between 5–11 years. 86 of 415 participants (20.7%) presented with fever, and the median (IQR) fever duration was 3.0 (2.0–4.0) days. In total, 174 of 415 (41.9%) participants tested positive for malaria by microscopy, of whom 9 (5.2%) had concomitant bacterial and 39 (22.4%) non-bacterial infections. Infection with Plasmodium falciparum (158, 90.8%) was most prevalent. Among 241 (58.1%) M[-] patients, 23 (9.5%) had bacterial and 54 (22.4%) non-bacterial infections. Overall, no etiologic cause of AFI was identified in 164/415 (39.5%) participants. Rapid diagnostic tests for Human Immunodeficiency Virus (HIV) yielded positive results in 6 of 416 (1.4%) children, equally distributed between both M[+] and M[−] children. Children diagnosed with malaria were significantly older (7.0 [4.0–11.0] years vs. 6.0 [4.0–10.0] years, p = 0.037) than M[−] peers (Table 1).
Demographic and clinical information on specific analysis groups shown in Fig. 1 can be found in the Supplementary Material (Supplementary Table 1).
Malaria is associated with increased odds for anemia
Among 297 of 415 participants (71.6%), in whom full blood count was available, anemia was highly prevalent. Of those, 222 were anemic, resulting in an estimated point prevalence of 74.7% (95% CI 69.5 –79.4) overall. Most anemic children presented with moderate (n = 146, 49.2%) followed by mild (n = 54, 18.2%) and severe (n = 15, 5.0%) anemia. The estimated point prevalence of anemia according to malaria status was 82.9% (92/111, 95% CI 74.6–89.4) in M[+] and 69.9% (130/186, 95% CI 62.8–76.4) in M[−] children.
M[+] children had a significantly higher odds of anemia compared to M[-] children (ORunadjusted 2.09, 95% CI 1.16–3.74). There were neither sex nor age specific differences regarding the odds of anemia with respect to malaria status. (Supplementary Table 2) Moreover, there was a moderate association between anemia severity and malaria status (V = 0.32, X2(3, N = 297) = 29.98, p < 0.001). Post-hoc comparison of malaria case proportions showed significant differences across all levels of anemia severity, with malaria prevalence increasing as anemia severity worsened. This trend was further supported by decreasing odds of a negative TBS with advancing anemia severity (no anemia: OR = 2.09, 95% CI 1.16–3.88; mild anemia: OR = 3.12, 95% CI 1.46–7.29; moderate anemia: OR = 0.46, 95% CI 0.27–0.76; severe anemia: OR = 0.14, 95% CI 0.02–0.52; Fig. 2a). Moreover, M[+] children had a significantly higher median red blood cell distribution width (RDW) compared to M[−] and, although not statistically significant, tended to be more microcytic and hypochromic (Supplementary Table 3).
Frequency distributions of (a) severity of anemia, (b) type of iron deficiency, and (c) anemia classified according to TSAT and ferritin concentrations in malaria positive (tbs pos) and malaria negative (tbs neg) patients. Graph (d) shows a matrix layout for number of patients that group according to different iron marker cut-offs. Black dots and connecting lines indicate possible combinations of biomarker cut-offs meeting the definitions of AI, AI/IDA, IDA or not. Abbreviation: ID iron deficiency, IR iron replete, tbs thick blood smear, TSAT transferrin saturation, AI anemia of inflammation, AI/IDA anemia of inflammation with possible iron-deficiency anemia, IDA iron-deficiency anemia.
Iron deficiency and fever
Overall, among 310 of 415 patients (74.7%) with available serum iron parameters, 72 (23.2%) had absolute ID (ferritin <100 µg/L), 107 (34.5%) functional ID (ferritin ≥ 100 µg/L), and 131 (42.3%) had normal iron status. When assessing the distribution of iron deficiency types according to malaria status, Chi-squared test results revealed a significant association (V = 0.15, X2(2, N = 310) = 7.27, p = 0.026). Post-hoc testing showed a significantly greater proportion of children having absolute ID in the M[−] compared to the M[+] group (28.5% vs. 16.5%, p = 0.046, Fig. 2b). In a multivariate logistic regression model for ID, defined as transferrin saturation (TSAT) < 20%, stratified for sex and adjusted for age, body temperature (OR 1.88, 95% CI 1.39–2.54) and a duration of fever ≥ 3 days (OR 0.57, 95% CI 0.35–0.93) were significantly associated with ID (Supplementary Table 4).
Anemia of inflammation
In 197 of 415 patients (47.5%), hemoglobin concentration and parameters of iron homeostasis were available, and among them, 145 (73.6%) were anemic. Among anemic patients 53 (36.6%) had AI, 29 (20.0%) AI/IDA, and 11 (7.6%) IDA irrespective of cause of AFI. Another 52 cases (35.9%) were attributed to multifactorial genesis and showed overall the picture of microcytic normochromic anemia (median [IQR] mean corpuscular volume, MCV 76 [68–78] fl; mean corpuscular hemoglobin concentration, MCHC 316.5 [307.0–325.3] g/L) with median (IQR) ferritin levels of 244 (103–470) µg/L, transferrin levels of 2.39 (2.01–2.57) g/L, and TSAT of 27 (23–33) %. The frequency of AI was highest in the M[+] group followed by multifactorial anemia (Fig. 2c). In this multifactorial group, 17/52 (32.7%) cases exhibited transferrin concentrations below the lower reference level (set at 2.2 g/L) and ferritin ≥100 µg/L, while 12/52 (23.1%) children had normal transferrin levels and ferritin concentrations <100 µg/L (Fig. 2d).
Median red blood cell (RBC) counts, MCV, mean corpuscular hemoglobin (MCH), MCHC, and RDW differed significantly between patients classified with AI, AI/IDA, and IDA, yet hemoglobin concentrations and hematocrit did not vary significantly. AI patients had significantly higher median c-reactive protein (CRP) levels compared to other groups except for multifactorial anemia. When comparing hepcidin and soluble transferrin receptor (sTfR) levels among classification of anemia groups, no statistically significant differences were observed. Moreover, no specific cytokine profiles were found to be associated with a specific type of anemia (Supplementary Table 5).
Iron metabolism and immune activation during malaria infection
Among children in the iron deficiency analysis group, significantly higher median plasma ferritin (244 [120–379] µg/L vs. 114 [60–230] µg/L, p < 0.001) and lower median plasma transferrin concentrations (2.45 [2.15–2.80] g/L vs. 2.65 [2.38–3.01] g/L, p < 0.001) were observed in M[+] compared to M[−] patients. A significant negative correlation between these iron parameters was observed within both groups (ρ(M[+]) = −0.55, 95% CI −0.67 to −0.39; ρ(M[−]) = −0.53, 95% CI −0.65 to −0.38).
When considering all participants with available hepcidin and sTfR levels, hepcidin concentrations were slightly higher in the M[+] group (36 ng/mL, IQR 29–79 ng/mL) compared to the M[−] group (33 ng/mL, IQR 27–45 ng/mL, p = 0.038). However, no statistically significant differences were observed in analyses limited to complete cases of iron markers or in subgroup analyses.
Malaria is not only associated with deranged iron metabolism but also alterations in circulating cytokine levels. Markers of immune activation were assessed in a subset of 54 children (iron status and cytokines analysis subgroup: n(M[ + ]) = 35, n(M[−] = 19) with either malaria infection or undetermined cause of AFI (Fig. 1), where both iron and cytokine levels were available. All evaluated parameters (interleukin (IL)−2, IL-6, IL-8, IL-10, tumor necrosis factor (TNF)-α, IFN-γ) were significantly higher in the M[+] group except for IL-4 (Supplementary Table 6). The cytokines exhibiting the most substantial differences between the M[+] and M[−] groups were IL-10 (r[U] = 0.71) and TNF-α (r[U] = 0.44), followed by IL-2 (r[U] = 0.34), IFN-γ (r[U] = 0.31), IL-8 (r[U] = 0.29) and IL-6 (r[U] = 0.28). The TNF-α: IL-10 ratio was significantly decreased in the M[+] compared to the M[−] group (r[U] = 0.56, p < 0.001).
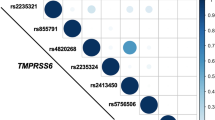
Malaria parasite counts were significantly correlated with various cytokine concentrations, listed here by descending order in strength of association: IL-10 (ρ = 0.72, 95% CI 0.51–0.85), IL-6 (ρ = 0.63, 95% CI 0.37–0.79), IL-8 (ρ = 0.39, 95% CI 0.06–0.64), and TNF-α (ρ = 0.39, 95% CI 0.06–0.64) (Fig. 3a). Moreover, ferritin and CRP levels were also positively associated with malaria parasitemia (Fig. 3a).
Graph (a) shows results of M[+] children (n = 35), and graph (b) for M [−] children with unidentified cause of AFI (n = 19) group. Associations between variables were calculated using Spearman’s correlation coefficient and only statistically significant associations (punadjusted < 0.05) are shown. Colors range from red (negative association) to white (no association) to blue (positive association), as indicated in the scale bar. Abbreviations: Hct hematocrit, CRP c-reactive protein, IL interleukin, IFN-γ interferon-γ, TNF-α tumor necrosis factor α.
In the M[+] group (N = 35), both SI and TSAT showed a significant negative correlation with levels of IL-2 (SI: ρ = −0.52, 95% CI −0.73 to −0.23; TSAT: ρ = −0.42, 95% CI −0.66 to −0.1), IL-6 (SI: ρ = −0.46, 95% CI −0.69 to −0.14; TSAT: ρ = −0.34, 95% CI −0.61 to −0.01), and IL-10 (SI: ρ = −0.49, 95% CI −0.7 to −0.18; TSAT: ρ = −0.34, 95% CI −0.61 to −0.01). Yet in the M[−] group (N = 19), TSAT levels were positively correlated with levels of IL-4 (ρ = 0.57, 95% CI 0.15–0.81), IFN-ɣ (ρ = 0.71, 95% CI 0.37–0.88). Moreover, ferritin concentrations correlated positively with IFN-ɣ (ρ = 0.69, 95% CI 0.34–0.87), while transferrin exhibited an inverse relationship with IFN-ɣ (ρ = −0.46, 95% CI −0.76 to −0.01). (Fig. 3b) Overall, IL-4 levels correlated positively with ferritin (M[+]: ρ = 0.43, 95% CI 0.11–0.67; M[-]: ρ = 0.68, 95% 0.32–0.87) and negatively with transferrin (M[+]: ρ = −0.38, 95% CI −0.63 to −0.05; M[−]: ρ = −0.52, 95%CI −0.79 to −0.09) in both groups.
Iron status and immune activation in coinfections
In children of the anemia analysis group, median RBC count (4.34, [3.80–4.79] × 1012/L vs. 4.61, [4.27–5.02] × 1012/L, p = 0.013), median hemoglobin concentration (94 [86–108] g/L vs. 106.0 [100–113] g/L, p = 0.009), and median hematocrit (30.5 [27.5–34.1] vs. 33.4 [31.4–35.2], p = 0.005) were significantly lower, while median RDW (14.90, [13.9 –16.40] % vs. 14.00 [13.08–15.50]%, p = 0.005) was higher in children with malaria infection compared to those with B/NB infections. Interestingly, children with B/NB infections exhibited no significant variations in RDW irrespective the malaria status (Supplementary Table 7).
Among children in the iron status and coinfections analysis subgroup (N = 230/415, 55.4%, Fig. 1), children with malaria + B/NB showed significantly higher median [IQR] ferritin levels (286 [178–409] vs. 190 [64–310], p = 0.037, Fig. 4a) and an increased median [IQR] ferritin: transferrin ratio (97 [40–169] vs. 67 [25–118], p = 0.045, Fig. 4c) compared to those with only B/NB infection. Apart from ferritin, no statistically significant variations in single iron parameters were observed between groups with identified pathogens (Fig. 4b, d–f) (Supplementary Table 8).
Plasma concentrations of (a) ferritin, (b) transferrin, c ferritin: transferrin ratio, (d) TSAT, (e) hepcidin, and (f) sTfR) were determined in children with bacterial or non-bacterial infection (B/NB, red), Malaria without co-infections (Malaria, light blue), Malaria with bacterial or non-bacterial co-infections (Malaria + B/NB, green), and Undetermined cause of infection (Undetermined, dark blue). Black dots and lines indicate group median and group interquartile range, respectively. P values were determined using Kruskal–Wallis test followed by Mann–Whitney post hoc testing with Benjamini–Hochberg adjustment for multiple comparisons. Significance levels were defined as follows, ns: padj > 0.05; *: padj ≤ 0.05; **: padj ≤ 0.01; ***: padj ≤ 0.001; ****: padj ≤ 0.0001. Only statistically significant differences from the post-hoc analysis are shown. Scales in a–f are adjusted to accurately display datapoints up to the 95th percentile. Cohort-based reference ranges for ferritin (10.9–81.1 µg/L) and transferrin (2.23 to 3.56 g/L) were recently assessed in European children and were found to be sex and age-dependent.17 There are no established reference values currently available for the hepcidin and sTfR assays. Abbreviations: AFI acute febrile illness, B/NB bacterial/non-bacterial, TSAT transferrin saturation.
Cytokine levels were assessed in 78 of 415 children (18.8%; cytokine analysis group) with different causes of AFI. Both TNF-α and IL-10 levels were significantly higher in the Malaria + B/NB compared to the B/NB infection group (Fig. 5a, b). IL-10 levels significantly differed between groups with an identified pathogen (Fig. 5b). These differences in immune activation patterns among different infection groups were best represented by the TNF-α: IL-10 ratio (Fig. 5c). Other cytokines exhibited no notable trends between disease entities (Fig. 5d–f and Supplementary Table 9). TNF-α, IL-10, and IL-6 levels were widely distributed in the Malaria group.
Serum concentrations of a TNF-α, (b) IL-10, (c) TNF-α:IL-10 ratio, (d) IL-6, (e) IFN-γ, and f IL-4 were measured children with bacterial or non-bacterial infection (B/NB, red), malaria without co-infections (Malaria, light blue), malaria with bacterial or non-bacterial co-infections (Malaria + B/NB, green), and undetermined cause of infection (Undetermined, dark blue). Black dots and lines indicate group median and group interquartile range, respectively. P values were determined using Kruskal–Wallis test followed by Mann–Whitney post hoc testing with Benjamini–Hochberg adjustment for multiple comparisons. Significance levels were defined as follows, ns: padj > 0.05; *: padj ≤ 0.05; **: padj ≤ 0.01; ***: padj ≤ 0.001; ****: padj ≤ 0.0001. Only statistically significant differences from the post-hoc analysis are shown. Scales in a–f are adjusted to accurately display datapoints up to the 95th percentile. There are no established reference values currently available for these cytokine assays. Abbreviations: AFI acute febrile illness, B/NB bacterial/non-bacterial, IL interleukin, IFN-γ interferon-γ, TNF-α tumor necrosis factor α.
Discussion
In this study, we examined iron homeostasis, hematologic and immunologic parameters, as well as causes of anemia in 415 Gabonese children with AFI. Our findings indicate a high prevalence of anemia 74.7% (95% CI 69.5–79.4) in these children, particularly in association with malaria. Large variations in anemia prevalence data were found for preschool-age children depending on sex, age, and geographical location, especially in Sub-Saharan Africa2. Past studies also showed higher anemia prevalence and severity in M[+] versus M[−] patients, consistent with our results23. This emphasizes the role of malaria and other infections in contributing to anemia development by disrupting iron homeostasis through immune activation24.
Our study found that most children with anemia had AI or AI/IDA. However, several children were classified as having multifactorial anemia because TSAT was ≥20%, despite appearing microcytic and hypochromic with ferritin levels >30 µg/L and signs of inflammation, all indicative of AI/IDA. This line of evidence diverges from data published by Engle-Stone et al.25, illustrating that 55% of anemic children in countries with a high burden of infectious disease had concomitant ID. However, concomitant hemolysis or low transferrin levels due to inflammation and/or malnutrition can result in pseudo-normal TSAT (≥20%), masking clinically evident ID. M[+] children exhibited elevated ferritin and hepcidin levels, decreased transferrin, and a high ferritin: transferrin ratio compared to M[−] children, thus emphasizing the limited use of ferritin to indicate ID.
Interestingly, malaria status did not significantly associate with ID in our multivariate analysis. Instead, higher body temperature and longer fever duration were significantly linked to increased odds of ID, suggesting that acute immune activation drives ID regardless of malaria infection13. Nonetheless, as ID is defined by TSAT < 20%, malaria and associated hemolysis may result in numerically higher relative TSAT, thus masking malaria infection as a known cause of ID26.
Moreover, the observed variations of hematological and iron parameters in this population may reflect the dynamics of iron markers during different stages of malaria infection, attributed to the inclusion criterion of fever <7 days. Castberg et al.27 suggest that the hemoglobin concentration remains significantly suppressed up to 24 days after radical cure of malaria infection. In Malaysian patients with Plasmodium falciparum infection, hepcidin levels dropped rapidly within 7 days after treatment, whereas ferritin declined gradually over the course of 28 days28. In the present study, samples were collected from children who had received on-site efficient anti-malarial therapy with no record of prior medication, making it unlikely that treatment timing significantly affected the proportion classified as ID or IDA.
Notably, we observed substantial variability in hepcidin concentrations, the central iron-regulatory hormone, across the different infection groups. Surprisingly, hepcidin levels did not differ significantly among the various types of anemia. This may be attributed, on one hand, to different factors affecting hepcidin expression29 and, on the other hand, to a hierarchy of signals affecting hepcidin expression with ID/IDA and/or hypoxia-driven inhibitory signals dominating over inflammation-inducible hepcidin induction, as observed in well-defined pre-clinical disease models30. However, factors such as nutritional status, hemolysis, kidney dysfunction, genetic hemoglobin polymorphisms, helminth infestations, and various immune activation pathways in response to viral, bacterial, or parasitic (co-)infections can further influence hepcidin formation in either way. While hepcidin has been shown to be a good indicator of iron needs and therapy guidance in non-febrile African children31, results of hepcidin tests are difficult to interpret in a setting of AFI. The interpretability of these findings could also be further affected by the choice of assay, as immunoassays, compared mass spectrometry, usually lack specificity for the bioactive isoform. Additionally, reference ranges of absolute hepcidin concentrations vary widely across different assay platforms.29
Strikingly, the ferritin: transferrin ratio and levels of TNF-α and IL-10 showed notable differences between M[+] and M[-] patients, regardless of the presence of additional infections, which concurs with previous findings32. Significant differences in IL-10, but not TNF-α, concentrations were observed between B/NB, Malaria + B/NB, and Malaria patients, suggesting a more pro-inflammatory response in B/NB infections. In contrast, malaria with or without co-infections resulted in blunted pro-inflammatory TNF-α and increased anti-inflammatory IL-10 formation, likely indicative of naturally acquired immunity due to repeated exposure to malaria33. Still, these findings should be interpreted with caution, as pooling children with B/NB infections into a single diagnostic group, despite increasing statistical power, also combined infectious diseases with distinct immune activation and cytokine patterns, as well as varying effects on iron homeostasis. High IL-10 levels were associated with higher parasite counts, and less effective parasite clearance, yet a reduced risk of severe malarial anemia in children34. Independent of malaria infection, elevated transcriptional levels of IL-10 were observed in anemic mice under iron supplementation when infected with Salmonella Typhimurium, suggestive of an association between iron supplementation and weakened immune control35. Moreover, IL-10 can induce anemia in inflammatory diseases dose-dependently by promoting macrophage iron retention, thereby reducing iron availability for erythroid progenitors36.
Contrasting immune responses were linked to iron parameters in children with malaria and undetermined AFI. In malaria patients, IL-2, IL-6, and IL-10 levels were negatively associated with SI and TSAT. Various cytokines, including IL-6, TNF-α, and IL-10, disrupt iron homeostasis and affect erythropoiesis, leading to AI24. IL-6 stimulates hepcidin production, resulting in ferroportin internalization37, while IL-10 regulates hepcidin in macrophages during Plasmodium falciparum infection in vitro38. Parasitemia also correlated with IL-6 and IL-10 levels in our study, while increased IL-6 levels were linked to the severity of malaria episodes in a recent meta-analysis39. In AFI cases with unidentified cause, IFN-γ and IL-4 levels were positively associated with TSAT and ferritin levels, suggesting a differentially regulated immune activation at higher TSAT. The prevalence of soil-transmitted helminth (STH) infections is estimated at 42% in rural Gabon40. Likewise, helminth infections might not be the acute cause of fever but could contribute to alterations in cytokine profiles in the undetermined infection group. Importantly, higher TSAT may also result from low transferrin levels or hemolysis, increasing circulating iron levels in that specific case.
One limitation of our study is the absence of baseline or follow-up data, which would have provided information on initial iron and immune status. This also prevented us from accounting for preexisting anemia or iron deficiency in our analyses. Consequently, the classification of AI relied primarily on inflammation-affected iron markers. Hemoglobin concentrations were not available for all participants, and not all samples could be analyzed for iron and cytokine levels. Furthermore, data on pathogens and conditions known to influence anemia and iron homeostasis—such as STH, schistosomiasis, or hereditary hemoglobin disorders—were lacking, as were markers of hemolysis. These limitations constrained our ability to predict relationships between iron status and immune activation. Similarly, marginally significant associations, such as those observed between cytokines and TSAT, should be interpreted with caution. The influence of multiple testing and inflammation-driven variations in iron parameters may affect the reliability of our findings in this case. Additionally, regional genetic and socio-economic factors, which may have impacted study outcomes, were not considered. As a result, these findings reflect the pediatric population of Lambaréné and may not be generalizable to other settings.
Our results emphasize the complex relationship between iron metabolism, infectious disease, and host immune activation. Potential implications of this study include tailoring iron interventions based on infection status and immune activation profile to improve iron deficiency and anemia management. This approach may involve withholding iron supplementation when absorption is impaired, thereby also reducing the risk of exacerbating infectious diseases. Additionally, investigating how iron- and pathogen-related mechanisms influence the function of different immune cell subsets is crucial, as it remains unclear how these interactions contribute to susceptibility to and severity of infections. Further prospective studies are needed to validate these associations and to inform evidence-based strategies for optimizing iron supplementation while mitigating infection risk in pediatric populations vulnerable to both anemia and infectious diseases.
Data availability
Underlying source data are provided with the manuscript. The source data for Figs. 1–5 in the main text are provided in Supplementary Data 1–9 file. Pseudonymized raw individual participant data supporting the results of this article will be made available to researchers upon sound request to the corresponding author. These data will be accessible immediately after publication.
Code availability
Custom code for all analyses is available on GitHub. The repository was uploaded on Zenodo to warrant long term access41.
References
Vos, T. et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 396, 1204–1222 (2020).
Collaborators, G. B. D. A. Prevalence, years lived with disability, and trends in anaemia burden by severity and cause, 1990-2021: findings from the Global Burden of Disease Study 2021. Lancet Haematol. 10, e713–e734 (2023).
Black, R. E. et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 382, 427–451 (2013).
Sazawal, S. et al. Effects of routine prophylactic supplementation with iron and folic acid on admission to hospital and mortality in preschool children in a high malaria transmission setting: community-based, randomised, placebo-controlled trial. Lancet 367, 133–143 (2006).
Clark, M. A. et al. Host iron status and iron supplementation mediate susceptibility to erythrocytic stage Plasmodium falciparum. Nat. Commun. 5, 4446 (2014).
Nairz, M. et al. Genetic and dietary iron overload differentially affect the course of Salmonella typhimurium infection. Front. Cell Infect. Microbiol 7, 110 (2017).
Gwamaka, M. et al. Iron deficiency protects against severe Plasmodium falciparum malaria and death in young children. Clin. Infect. Dis. 54, 1137–1144 (2012).
Barffour, M. A. et al. High iron stores in the low malaria season increase malaria risk in the high transmission season in a prospective cohort of rural Zambian children. J. Nutr. 147, 1531–1536 (2017).
Muriuki, J. M. et al. Iron status and associated malaria risk among African children. Clin. Infect. Dis. 68, 1807–1814 (2019).
Butler-Laporte, G. et al. Increasing serum iron levels and their role in the risk of infectious diseases: a Mendelian randomization approach. Int. J. Epidemiol. 52, 1163–1174 (2023).
Brandtner, A. et al. Linkage of alterations in systemic iron homeostasis to patients’ outcome in sepsis: a prospective study. J. Intensive Care 8, 76 (2020).
Neuberger, A., Okebe, J., Yahav, D. & Paul, M. Oral iron supplements for children in malaria‐endemic areas. Cochrane Database of Syst. Rev. 2, CD006589 (2016).
Nairz, M. & Weiss, G. Infections associated with iron administration. Met. Ions Life Sci. 14,19 (2019).
Escadafal, C. et al. Bacterial versus non-bacterial infections: a methodology to support use-case-driven product development of diagnostics. BMJ Glob. Health 5, e003141 (2020).
Yamanishi, H., Iyama, S., Yamaguchi, Y., Kanakura, Y. & Iwatani, Y. Total iron-binding capacity calculated from serum transferrin concentration or serum iron concentration and unsaturated iron-binding capacity. Clin. Chem. 49, 175–178 (2003).
Humberg, A., Kammer, J., Mordmuller, B., Kremsner, P. G. & Lell, B. Haematological and biochemical reference intervals for infants and children in Gabon. Trop. Med. Int. Health 16, 343–348 (2011).
Floegel, A. et al. Cohort-based reference values for serum ferritin and transferrin and longitudinal determinants of iron status in European children aged 3-15 years. J. Nutr. 154, 658–669 (2024).
Organization, W. H. Guideline on Haemoglobin Cutoffs to Define Anaemia in Individuals and Populations Vol. 2024 (World Health Organization, Geneva, 2024).
Aoshima, M. et al. A survey of high dimension low sample size asymptotics. Aust. N. Z. J. Stat. 60, 4–19 (2018).
Wickham, H. et al. Welcome to the tidyverse. J. Open Source Softw. 4, 1686 (2019).
Conway, J. R., Lex, A. & Gehlenborg, N. UpSetR: an R package for the visualization of intersecting sets and their properties. Bioinformatics 33, 2938–2940 (2017).
Sjoberg, D. D., Whiting, K., Curry, M., Lavery, J. A. & Larmarange, J. Reproducible summary tables with the gtsummary package. R. J. 13, 570–580 (2021).
Bouyou-Akotet, M. K. et al. Anaemia and severe malarial anaemia burden in febrile Gabonese children: a nine-year health facility based survey. J. Infect. Dev. Ctries 7, 983–989 (2013).
Weiss, G., Ganz, T. & Goodnough, L. T. Anemia of inflammation. Blood 133, 40–50 (2019).
Engle-Stone, R. et al. Predictors of anemia in preschool children: biomarkers reflecting inflammation and nutritional determinants of anemia (BRINDA) project. Am. J. Clin. Nutr. 106, 402S–415S (2017).
Muriuki, M. J. et al. Malaria is a cause of iron deficiency in African children. Nat. Med. 27, 653–658 (2021).
Castberg, F. C. et al. Malaria causes long-term effects on markers of iron status in children: a critical assessment of existing clinical and epidemiological tools. Malar. J. 17, 464 (2018).
Woolley, S. D. et al. Longitudinal changes in iron homeostasis in human experimental and clinical malaria. eBioMedicine 105, 105189 (2024).
Girelli, D., Nemeth, E. & Swinkels, D. W. Hepcidin in the diagnosis of iron disorders. Blood 127, 2809–2813 (2016).
Theurl, I. et al. Pathways for the regulation of hepcidin expression in anemia of chronic disease and iron deficiency anemia in vivo. Haematologica 96, 1761–1769 (2011).
Prentice, A. M. et al. Hepcidin is the major predictor of erythrocyte iron incorporation in anemic African children. Blood 119, 1922–1928 (2012).
Davenport, G. C. et al. Reduced parasite burden in children with falciparum malaria and bacteremia coinfections: role of mediators of inflammation. Mediat. Inflamm. 2016, 4286576 (2016).
Mooney, J. P. et al. Bouncing back’ from subclinical malaria: inflammation and erythrocytosis after resolution of P. falciparum infection in Gambian children. Front. Immunol. 13, 780525 (2022).
Thuma, P. E. et al. Distinct clinical and immunologic profiles in severe malarial anemia and cerebral malaria in Zambia. J. Infect. Dis. 203, 211–219 (2011).
Hoffmann, A. et al. Baseline iron status and presence of anaemia determine the course of systemic Salmonella infection following oral iron supplementation in mice. eBioMedicine 71, 103568 (2021).
Tilg, H., Ulmer, H., Kaser, A. & Weiss, G. Role of IL-10 for induction of anemia during inflammation. J. Immunol. 169, 2204–2209 (2002).
Nemeth, E. & Ganz, T. Hepcidin and Iron in health and disease. Annu. Rev. Med. 74, 261–277 (2023).
Huang, H. et al. Interleukin-10 regulates hepcidin in Plasmodium falciparum malaria. PLoS ONE 9, e88408 (2014).
Wilairatana, P. et al. Increased interleukin-6 levels associated with malaria infection and disease severity: a systematic review and meta-analysis. Sci. Rep. 12, 5982 (2022).
Edoa, J. R. et al. Epidemiology of soil-transmitted helminth infections and the differential effect of treatment on the distribution of helminth species in rural areas of Gabon. Trop. Med. Health 52, 3 (2024).
Mayr W. Source code for the manuscript entitled: Iron homeostasis and cytokine responses in Gabonese children with febrile illness. https://doi.org/10.5281/zenodo.15399607 (2025).
Acknowledgements
We gratefully acknowledge the assistance and support of the participating children, their parents, and the study team, including field workers, clinical investigators, data managers, and laboratory staff. The BFF-Dx study was funded by the governments of the Netherlands, United Kingdom, and Australia. The current retrospective analysis is funded by the Senior Fellowship Grant of Selidji Todagbe Agnandji: European Developing Countries Clinical Trial Partnership (EDCTP) senior fellow, grant no. TMA2017SF-1946. Additional funding was provided by the Christian Doppler Society (Laboratory for iron metabolism and anemia research). Additional support of the Verein zur Förderung von Forschung und Weiterbildung in Infektiologie und Immunologie an der Medizinischen Universität Innsbruck is gratefully acknowledged.
Author information
Authors and Affiliations
Contributions
W.M. contributed to the data curation, formal analysis, and writing of the original draft. P.E.N. contributed to the data curation, formal analysis, and validation. W.M. and P.E.N. contributed equally to this work. S.T.A. contributed to the conceptualization, design, supervision, and funding. G.W. contributed to the conceptualization, design, funding, formal analysis, and writing of the original draft. A.A. contributed to the data curation, investigation, and validation. L.K. contributed to the data curation and investigation. All authors had full access to the underlying data and contributed to reviewing and editing the original draft.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Communications Medicine thanks Carla Cerami and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Mayr, W., Ndong, P.E., Alabi, A. et al. Iron homeostasis and cytokine responses in Gabonese children with febrile illness. Commun Med 5, 305 (2025). https://doi.org/10.1038/s43856-025-00988-3
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s43856-025-00988-3