Abstract
Background
Ethiopia aims to eliminate local malaria transmission by 2030, but rising malaria cases, due to different factors, present a challenge. Understanding the prevalence and distribution of artemisinin partial resistance (ART-R) and other markers related to partner drugs as well as parasite connectivity in Ethiopia can greatly inform malaria control.
Methods
We analyzed 1199 clinical Plasmodium falciparum infections from 12 sentinel sites across five regions in Ethiopia, collected between 2019 and 2023. Using two molecular inversion probe (MIP) panels targeting key drug resistance genes and genome-wide SNPs, we assessed the prevalence of resistance-associated mutations, complexity of infection (COI), and parasite relatedness through identity-by-descent (IBD) and principal component analysis (PCA).
Results
The most prevalent k13 R622I mutation appears in 15.7% of samples, with marked regional variation. Three validated ART-R mutations (P441L, P574L, A675V) are detected in Ethiopia for the first time, as far as we are aware, with A675V found exclusively in a Gambella clinic serving refugees from Sudan and South Sudan. Additionally, polymorphisms associated with resistance to partner drugs, including those in crt, mdr1, dhps, and dhfr genes, are nearly fixed. Most samples (87.2%) consist of monogenomic infections (COI = 1), and mutant parasites show high local genetic relatedness at the health facility level, suggesting clonal transmission. PCA reveals regional clustering, particularly in Gambella, highlighting the influence of local drug pressure, regional transmission dynamics, and importation as drivers of the observed drug resistance patterns.
Conclusions
The increasing prevalence of k13 R622I and the emergence of additional ART-R mutations underscore the urgent need for enhanced ACT efficacy monitoring. Early detection of partner drug resistance and ACT failure will be essential to address malaria resurgence and support Ethiopia’s elimination goals.
Plain language summary
Ethiopia is aiming to eliminate the spread of malaria within the country by 2030. However, recent increases in malaria cases driven by several factors are making this goal more difficult to achieve. This study investigated whether malaria parasites in Ethiopia are becoming resistant to anti-malarial drugs. We analyzed blood samples collected between 2019 and 2023 from people infected with malaria at 12 health facilities across 5 regions. We focused on genetic changes in the parasites that are known to reduce the effectiveness of key malaria treatments, including artemisinin. We found that a previously reported genetic changes in the parasite, known as k13 R622I, is now widespread in Ethiopia but varies by location. We also identified three additional genetic changes linked to artemisinin resistance seen, as far as we are aware, for the first time in Ethiopia. The study shows that some drug-resistant parasites are spreading, particularly in certain areas. Our findings can be used to improve monitoring and strategies to eliminate malaria in Ethiopia.
Similar content being viewed by others
Introduction
Malaria remains a significant public health challenge in Africa, where approximately 95% of malaria cases and 96% of malaria deaths occur, predominantly among young children and pregnant women1. Despite notable progress in mitigating disease and transmission through the use of artemisinin-based combination therapies (ACTs), vector control measures, and vaccines like RTS,S, the path to eliminating malaria faces formidable obstacles2,3. These challenges include the emergence of drug- and diagnostic-resistant parasites4,5,6,7, insecticide-resistant mosquitoes8, new invasive mosquito species9, inadequate healthcare infrastructure, and funding gaps10. Since their introduction in the early 2000s, ACTs have become the cornerstone of malaria treatment across the continent11,12. Among the various ACTs, artemether-lumefantrine (AL) is the most widely used treatment for uncomplicated falciparum malaria in Africa13,14. However, the emergence of partial resistance to artemisinin (ART-R) poses a significant threat to the effectiveness of ACTs, undermining progress toward malaria elimination15,16. This highlights the urgent need for new strategies to better understand and mitigate the impact of antimalarial resistance.
ART-R was first reported in western Cambodia in Southeast Asia in 2006-200717,18 and has since spread or emerged independently across countries in the Greater Mekong Subregion19, South America20, and more recently in Eastern Africa21,22,23 and the Horn of Africa5,24. The emergence of ART-R WHO-validated markers has been confirmed in Ethiopia5, Eritrea24, Rwanda21, Uganda25, Tanzania6, and the Democratic Republic of the Congo (DRC)26. ART-R likely accelerates the emergence of resistance to partner drugs27, with the combination leading to clinical failure in Southeast Asia. Non-synonymous SNPs in the crt and mdr1 genes have been associated with susceptibility to amodiaquine28 and potentially lumefantrine29, though resistance markers for the latter are not well established30. The mdr1 N86 allele is associated with re-infection after artemether-lumefantrine (AL) treatment31. Given that lumefantrine and amodiaquine are the most widely used ACT partner drugs across Ethiopia and much of Africa, monitoring mutations in genes associated with susceptibility is important for surveillance4,6,32.
Therapeutic efficacy studies (TES) conducted in Ethiopia have consistently demonstrated high efficacy of AL and other ACTs across various sites33,34,35. Despite these positive results and Ethiopia’s progress in malaria control over the past two decades, the country is experiencing an increase in malaria cases across various regions. Malaria control efforts are facing several threats. One of the key threats is the presence of the K13 R622I mutation, a well-established marker of ART-R, which has been found at concerning frequencies, especially in northern Ethiopia5. While TES has not yet shown any impact on patient outcomes, the detection of validated ART-R markers raises concerns about the long-term efficacy of ACTs36. Another emerging challenge is the rise of Plasmodium falciparum strains with deletions in the hrp2 and hrp3 genes, which has led to the replacement of standard rapid diagnostic tests (RDTs) with alternative versions5,7. Additionally, the spread of urban-adapted mosquito species9,37, and increasing insecticide resistance38 pose further threats to malaria control efforts. Environmental and man-made factors such as climate change39, conflict, and population movement have also contributed to the spread of malaria transmission, fueling the recent resurgence. Moreover, weaknesses in surveillance systems hinder the effective monitoring of disease patterns, resistance trends, and the factors driving malaria’s resurgence. Dissecting and addressing these challenges requires enhanced surveillance, robust diagnostic tools, and innovative strategies to track and mitigate the spread of drug-resistant strains to achieve elimination goals40. Genomic surveillance of molecular markers of resistance and understanding the genomic diversity of the parasite will be critical41. Such surveillance helps identify resistance hotspots and informs targeted interventions, such as the deployment of sequential or triple ACT regimens, thus strengthening malaria control and elimination strategies42,43.
Integrating genomic data with routine surveillance systems for timely tracking of emerging and spreading resistance is crucial44,45. To this end, the Ethiopian Public Health Institute (EPHI), in collaboration with the national malaria control and elimination program, established a network of sentinel sites representative of the diverse malaria transmission ecologies across the country. These sites collect and analyze data on malaria transmission dynamics, treatment efficacy, and resistance patterns, providing opportunities for evidence-based decision-making in near real-time. These sentinel sites are integral to Ethiopia’s broader malaria control and elimination strategy, which aims to reduce the disease’s burden through early detection, targeted treatment, and prevention efforts. This study reports an in-depth analysis of the emergence and spread of drug resistance mutations and parasite relatedness using molecular inversion probe (MIP) sequencing of samples collected from 12 sentinel sites across the country.
Our analysis reveals that the k13 R622I mutation is the most prevalent artemisinin partial resistance (ART-R) marker, found in 15.7% of samples, with substantial regional variation. We also detect three validated ART-R mutations (P441L, P574L, A675V) in Ethiopia, as far as we are aware, for the first time, with A675V confined to a refugee clinic in Gambella. Resistance-associated polymorphisms in partner drug genes (crt, mdr1, dhps, and dhfr) are nearly fixed. Most infections are monogenomic, and identity-by-descent analysis shows high local genetic relatedness, suggesting clonal transmission. PCA reveals regional clustering, particularly in Gambella, underscores the role of local drug pressure, transmission dynamics, and importation in shaping resistance patterns. These findings highlight the urgent need for enhanced monitoring of artemisinin-based combination therapy (ACT) efficacy to support Ethiopia’s malaria elimination goals.
Methods
Study sites and sample collection
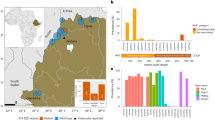
EPHI maintains 25 malaria sentinel sites, representing the variable eco-epidemiological zones across the country. A series of cross-sectional studies were conducted in 12 of these sites between 2019 and 2023 to assess the emergence and prevalence of antimalarial drug resistance markers. The selection of the 12 sites was necessitated by internal conflict in Ethiopia and other administrative issues. It was ensured that the study sentinel sites included at least one area where large-scale industry and irrigation, typically for sugar, is occurring and one location in a border area (Fig. 1a, Supplementary Data 1). From September to November of each year, patients attending the outpatient department with signs and symptoms of malaria were screened by microscopy. Microscopy occurred in the field and was reviewed by a second expert microscopist at EPHI. In cases of discordance, a third reader was used, blinded to previous reads. Inclusion criteria included P. falciparum positive by microscopy. Patients under 1 year of age or those with severe malaria were excluded. Informed consent was obtained from all adult participants and from the guardians of participating children. In addition, assent was obtained from children aged 12 to 17 years prior to sample collection. A brief questionnaire was performed (including patient age, sex, malaria signs and symptoms, travel history, and demography), and dried blood spot (DBS) samples were blotted onto Whatman 3 filter paper, air-dried, and placed individually in a plastic bag containing silica gel desiccant. These were stored at room temperature prior to transport to EPHI, and stored at −20 °C until used. Details of sample collection and processing are provided in Supplementary Fig. 1.
DNA extraction and MIP sequencing
DNA was extracted from DBS (one full DBS spot, typically involving 2 or 3 6 mm punches) using Chelex-Tween as previously described46. Five microliters of extracted DNA were used for each of the MIP captures using two panels: one covering key P. falciparum drug resistance genes and mutations47, including k13, mdr1, crt, dhfr, and dhps genes, and a newly designed panel of 305 MIPs targeting common SNPs (>5%) SNPs48. MIP capture and library preparation were performed as previously described5. Sequencing was conducted using an Illumina NextSeq 550 instrument (150 bp paired-end reads) at Brown University (RI, USA). For samples with newly detected K13 P441L, P574L and A675V, mutations in Ethiopia), an additional MIP capture was done using the same drug resistance MIP panel47 and resequenced to a high depth to confirm the mutations. Controls for each MIP capture and sequencing included genomic DNA from serial dilution of lab strain 3D7 as well as no template and no probe controls. We then assessed sequencing performance by calculating the mean coverage, standard deviation (SD), and coefficient of variation (CV) for probes targeting five key drug resistance genes: crt, dhfr, dhps, k13, and mdr1 (Supplementary Table 1). Probes were categorized into four coverage ranges based on their mean coverage: <10x, 10-50x, 50-100x, and >100x.
Variant calling and filtering
The sequencing reads generated for each MIP panel were demultiplexed separately using MIPtools software (https://github.com/bailey-lab/MIPTools) and further processed using MIP Wrangler software (https://github.com/bailey-lab/MIPWrangler), in which sequence reads sharing the same Unique Molecular Identifiers (UMIs) were collapsed to generate a single consensus. Each dataset was analyzed by mapping sequence reads to the P. falciparum 3D7 reference genome using Burrows-Wheeler Aligner (BWA)49. Then variant calling was performed using freebayes software50. To reduce false positives due to PCR and alignment errors, the alternative allele needed to be supported by more than one UMI within a sample, and the allele must have been represented by at least 10 UMIs across the entire population. For genome-wide SNPs, only biallelic variant SNP positions were retained for downstream analysis. Low-quality SNPs (mapping quality <30), were removed from the analysis using vcftools51; additionally, individual variant calls within each sample were set to missing if the site was not supported by at least five UMIs. After these steps, SNPs with more than 50% missing data across samples, and subsequently samples with more than 50% of SNPs missing, were removed from all downstream analyses5. We retained 855 samples and 508 informative high-quality biallelic SNPs distributed across 14 P. falciparum chromosomes used for downstream population genetic analysis. The distribution of retained samples and SNPs across the chromosomes can be found here (Supplementary Fig. 2)
Drug resistance prevalence estimation
For drug resistance analysis, variants were annotated using the Pf 3D7 v3 reference genome and gene features (version 3). Variants with a unique UMI count of 3 or greater were used to estimate the prevalence of key and known drug resistance mutations associated with different forms of antimalarial resistance, using the miplicorn package in R 4.2.1 (https://github.com/bailey-lab/miplicorn) and a custom R script. With the exception of the dhps 437 mutation (which is mutant in the reference genome), drug resistance prevalence was determined considering both heterozygous or homozygous variants as mutant alleles, while homozygous reference alleles considered as wild-type, and missing loci were not included for prevalence calculation (p = x/n*100), where p = prevalence, x = number of mutant alleles, n = number of successfully genotyped loci. n is different for each locus, as each locus had independent success rates for genotyping. Prevalence and frequency bar plots were generated using the ggplot2 package and spatial visualization of prevalence on maps of study areas was created using the sf package in R 4.2.1 software. Analysis of haplotypes included only samples where complete genotypes across all involved variant sites were available and was plotted and visualized using the UpSet package in R 4.2.1 software. Finally, the prevalence of each drug resistance marker was calculated at the health facility level.
Analysis of the complexity of infection, genetic diversity, and parasite population structure
The complexity of infection (COI) is the number of distinct parasite clones infecting a single host. To estimate the number of clones per sample, the VCF file containing SNP data was converted to THE REAL McCOIL categorical method format: heterozygous call as 0.5, homozygous reference allele as 0, homozygous alternative allele as 1 and no call as −1 and used as an input file for analysis of COI using THE REAL McCOIL R package52. To assess whether parasite populations within Ethiopia clustered per their health facilities, or by mutation status, we conducted principal component analysis (PCA) using SNPRelate53. We conducted additional population genetic analyses, including SNP π as measures of genetic diversity at the regional level, and calculated pairwise FST as a measure of genetic differentiation using vcftool,s and the result was visualized using ggplot2 in R 4.2.1 software.
Analysis of parasite relatedness using Identity-by-Descent (IBD)
We used identity-by-descent (IBD) to measure relatedness between parasites and identify regions of the genome shared with recent common ancestry using the inbreeding_mle function in MIPAnalyser software (v.1.0.1) (https://github.com/mrc-ide/MIPanalyzer) in R 4.2.1 software as previously described54. In brief, both monogenomic and polygenomic infections (major alleles used for heterozygous positions) were included in the IBD analysis. Inbreeding_mle uses a Markov chain Monte Carlo to detect genomic regions that are identical by descent (IBD) and aids simultaneous detection of parasite population clustering. Networks of highly related parasites per k13 mutation status or geographic origin (health facilities) were created using the igraph package in R 4.2.1 software. IBD sharing at the regional and local levels was assessed by calculating pairwise IBD values for each sample. Visualization was performed using the ggplot2 and sf libraries in R, along with additional spatial visualization tools such as rnaturalearth, ggspatial, and scatterpie. The map was generated using shapefiles from the Natural Earth database55, and IBD values were represented using color gradients. We focused on pairs with IBD ≥ 0.90 and visualized the mean IBD values for each site. We also fitted the linear mixed-effects model using the REML (Restricted Maximum Likelihood) method to assess the statistical significance of being mutant parasites for IBD sharing compared to wild-type. This model accounted for health facilities as a random effect, allowing for variability across different health facilities. We also conducted an ANOVA analysis to assess whether the variation in IBD-sharing is significant between health centers using R 4.2.1 software
Statistics and reproducibility
Statistical analyses were performed in R (v4.2.1). Sample sizes represent biologically independent patient-derived parasite samples from 12 sentinel sites (n values specified per analysis). Linear mixed-effects models with REML and ANOVA were used to assess differences in identity-by-descent (IBD) sharing, accounting for random effects of health facilities. Exact p-values, effect sizes, and confidence intervals are reported where applicable. Sequencing experiments included appropriate controls and quality filters to ensure reproducibility, with samples and variants with excessive missing data excluded from analyses.
Ethics
Before the commencement of the study, scientific and ethical approval was obtained from the Ethiopian Public Health Institute’s Institutional Review Board (EPHI-IRB), protocol number EPHI-IRB-398-2021. In addition, respective permissions and supporting letters were obtained from the health facilities administration. All the necessary precautionary and ethical methods were considered during the implementation of the study for the patients and investigators. All screening forms and case record forms are kept in a secured location, with access limited to authorized staff members. Unique numerical identifiers were used for the computer-based data entry and blood samples. Genotyping work conducted at Brown University was considered non-human subject research. Only aggregated clinical data and de-identified samples were used for reporting individual-level genotypes for publication.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Results
Study population and MIP genotyping
A total of 1199 P. falciparum-positive samples by microscopy were included in the study. All samples were sequenced using newly designed MIPs targeting informative SNPs across genome48, as well as previously optimized MIPs targeting key drug resistance genes including k13, mdr1, crt, dhfr, and dhps47. Details of sample collection, processing, and data analysis are provided in Supplementary Fig. 1 and the methods section. To ensure robust data quality for downstream analysis, we excluded SNPs with more than 50% missing data across samples, and subsequently excluded samples with more than 50% missing SNPs. This resulted in 855 samples and 508 informative, high-quality biallelic SNPs distributed across 14 P. falciparum chromosomes used for population genomic analysis. The MIP coverage of the retained samples and the distribution of SNPs across chromosomes are shown in Supplementary Fig. 2. In terms of probe coverage, the majority of probes also met or exceeded the 10x threshold (Supplementary Table 1). Most probes achieved coverage above 100x (Supplementary Fig. 3), with some variation in coverage across samples.
Samples came from participants enrolled at all 12 sentinel site health facilities (Fig. 1a, Supplementary Data 1) across five regions (Amhara = 270, Gambella = 131, Oromia = 193, SNNP = 221, Somali = 40) (Fig. 1b, Supplementary Data 2). The median parasite density of sequenced samples was 2,000 parasites/µL (range 48 to 61,000 parasites/µL) by microscopy, with better sequencing coverage in samples with higher parasitemia. Most samples (n = 767) were collected in 2022, 79.2% (n = 607) of which were successfully genotyped; 393 were collected in 2019 with 56.9% (n = 224) successfully genotyped, followed by 39 collected in 2023 with 61.5% (n = 24) successfully genotyped. Details of the number of samples attempted and successfully sequenced are summarized in Supplementary Table 2 for genome-wide SNPs and Supplementary Data 3 for drug resistance SNPs.
Prevalence and distribution of ART-R mutations
We assessed the prevalence of WHO-validated and candidate k13 ART-R mutations, revealing four WHO-validated k13 mutations (Fig. 2a, Supplementary Data 4). k13 R622I was the most prevalent (15.7% [95% CI 13.2–18.2%]). Its geospatial distribution was heterogeneous (prevalence range: 0 to 58.8%) at the health facility level (Supplementary Fig. 4), with the highest regional prevalence in the Amhara region (46.9% [95% CI 40.7–53.2%]) where it was first reported at a prevalence of 2.4% in one facility in 201456. k13 R622I was also prevalent in Erer (12.9%), a Somali region in the Eastern part of the country, and additionally observed at low frequency from health facilities in the Gambela and Oromia regions. However, k13 R622I was not observed in health facilities in the SNNP (Southern Nations, Nationalities, and Peoples) region. This suggests that the R622I mutation is dominant and more widely spread in the northern, northwestern, and eastern parts of the country.
a Spatial distribution of WHO-validated k13 mutations by health facility (pie charts). Colors indicate which mutation, and pie chart size is proportional to sample size per study site. b Pairwise IBD sharing within 622I mutant (n = 130) vs within wildtype (n = 725). The plot shows the probability that any two isolates are identical by descent, where the x-axis indicates IBD values and the y-axis indicates the frequency of isolates sharing IBD. c Network analysis showing highly related parasite pairs (IBD ≥ 0.99) for a total of 393 samples. Each node identifies a unique isolate, and an edge is drawn between two isolates if they meet the IBD threshold. Isolates that do not have an IBD pairwise connection above a threshold are not shown. Color codes correspond to k13 R622I mutants (pink) and wild parasites (blue-green). d Pairwise IBD sharing within k13 R622I mutant versus wild parasites, showing significant differences (***P = 0.0004, two-tailed, Mann-Whitney U-test). Boxes indicate the interquartile range, the line indicates the median, the whiskers show the 95% confidence intervals, and the dots show outlier values. WHO, World Health Organization; k13, kelch13 gene; IBD, identity by descent.
Of concern, we found three additional WHO-validated k13 mutations not previously observed in the Horn of Africa in the southern half of the country, where R622I is not as prevalent. We found 6 samples with A675V (Gambella Region), 4 samples with P441L (3 from the Southern Region, including 2 from Dilla and 1 from Secha health centers, and 1 from Oromia Region in the Metehara health center), and 5 samples with P574L (all from the Oromia Region in the Batu health center) (Supplementary Table 3). We also identified an additional 14 non-synonymous mutations within and outside the k13 propeller domain with variable frequencies (Supplementary Fig. 5). Other k13 variants not associated with ART-R were found, including K189T at a prevalence of 32% (CI, 27.1–38.3) across sites.
Genetic relatedness of the k13 mutant parasites
In order to better understand the spatial spread of mutant parasites, we analyzed Identity-By-Descent (IBD) relatedness between k13 R622I mutant and k13 wild-type isolates. Mutant parasites consistently showed higher IBD values compared to wild-type parasites (Fig. 2b, Supplementary Data 5). We then performed relatedness network analysis using an IBD threshold of ≥0.99 to detect clonal transmission and found clustering of mutant parasites distinct from the wildtype parasites (Fig. 2c) with an average IBD sharing estimate was significantly (p = 0.0008) higher for k13 R622I mutant isolates (mean IBD = 0.21) compared to the wild-type isolates (mean IBD = 0.14) (Fig. 2d). Notably, the majority of clonal mutant parasites were clustered at the regional (Supplementary Fig. 6a) or district (Supplementary Fig. 6b) levels, which suggests rapid spread of mutant parasites within specific areas of the region. Lower IBD threshold analysis (Supplementary Fig. 7) showed mutant parasites clustering with wild-type parasites, indicating shared genomic regions beyond the k13 gene. We fitted a linear mixed-effects model using REML (Restricted Maximum Likelihood) to assess the impact of mutations on IBD sharing and found mutation status significantly affect IBD, with both mutants-wildtypes (β = −0.24, t = −35.71, p = 0.0002) and wildtypes (β = −0.14, t = −18.60, p = 0.0006) showing lower IBD compared to the mutants. This pattern was consistent across health centers (Supplementary Fig. 8). Parasites with P574L mutations showed significant relatedness (p = 0.023) (Supplementary Fig. 9b), while those with A675V or P441L mutations showed no significant relatedness and were less related to wildtype (Supplementary Fig. 9a, c).
Prevalence of mutations associated with resistance to partner drugs
Mutations in the P. falciparum mdr1 gene, particularly isolates that carry the N86 (wild), 184F (mutant), and D1246 (wild) haplotype, have been associated with modest tolerance to lumefantrine (the first-line partner drug in Ethiopia, co-formulated as AL). Our analysis revealed that 99.1% ([95% CI 98.4–99.6%]) of sequenced samples carried N86 (wild type),98.1% ([95% CI 97.2–98.9%]) carried D1246 (wild type), and 94.8% ([95% CI 93.4–96.3%]) carried 184F (mutant) alleles. We then constructed haplotypes since combinations of mdr1 alleles determine tolerance to lumefantrine and found 6 haplotypes. The NFD haplotype is the most predominant in 94.8% ([95% CI 92.8-96.2%]) of isolates, followed by NYD in 3.2% ([95% CI 2.1-4.8%]) (Supplementary Fig. 10a). The overall high prevalence of NFD haplotype resulted in less spatial variation at regional level (Supplementary Fig. 10b). Nearly all parasites with the ART-R K13 R622I (Fig. 3a, Supplementary Data 6) and A567V (Fig. 3b, Supplementary Data 7) mutations also carry the NFD haplotype associated with lumefantrine tolerance. A Chi-squared test revealed a significant association between the K13 622I mutation and the mdr1 NFD haplotype (χ² = 5.5404, p = 0.0186).
a Co-occurrence of K13 622I and MDR1 N86 (wild), 184F (mutant) and D1246 (wild). b Co-occurrence of K13 675 V and MDR1 N86 (wild), 184F (mutant) and D1246 (wild). Only samples (n = 747) with calls across all four loci are shown. For polygenomic infections, the dominant haplotype (≥51% allele frequency) is shown. ART-R artemisinin resistance, k13, kelch13 gene, mdr1 multidrug resistance protein 1.
We also observed a high prevalence of mutations associated with resistance to sulfadoxine-pyrimethamine (SP) and chloroquine. SP was discontinued in 2004 and is not used for intermittent preventive treatment for pregnant women (IPTp) as in other African countries. Nonetheless, SP resistance mutations persist at high prevalence. In dhfr, 98.9% ([95% CI 98.6–99.4%]) of parasites had the S108N, 98.5% ([95% CI 97.8–99.3%]) had the N51I, and 65% ([95% CI 61.9–68.1%]) had the C59R mutations (Supplementary Fig. 11a) associated with pyrimethamine resistance. Overall, 61.6% ([95% CI 58.6–65.4%]) samples carry all three mutations (dhfr IRN, triple mutant) with equal distribution at the regional level across the country. None of the genotyped samples carried dhfr 164L, a mutation associated with higher levels of SP resistance. For sulfadoxine resistance, all isolates had dhps 437G, and 83.1% ([95% CI 80.6-85.4%]) had K540E (Supplementary Fig. 11a) The dhps A581G mutation, shown to increase SP resistance, when co-occurring with the above mutations occurred at low frequency, 3.4% ([95% CI 2.6–5.4%]) with some level of variation at regional level (Supplementary Table 4). Given the significance of combined mutations both dhps and dhfr for SP resistance, we determined the prevalence of the IRNGE quintuple mutation to be 58.6% ([95% CI 55.3, 61.9%]). Our analysis revealed significant regional variation in the prevalence of this quintuple mutation across Ethiopia, with the highest prevalence observed in the Southern (92.73%) and Oromia, (82.88%) regions, and the lowest in the Amhara and Gambela regions (19.53%) (Supplementary Table 4).
Chloroquine is widely used in Ethiopia for the treatment of Plasmodium vivax infections. Mutations in the P. falciparum chloroquine resistance transporter (CRT) were common; 896 (82.4%) parasites had the chloroquine-resistance marker 76T. All regions had high prevalence, with the exception of Gambela in the southwest, which had a prevalence of 7.6% ([95% CI 5.2–8.4%]) (Supplementary Fig. 11b). We estimated haplotype distribution and found that CVIET(C72/V73/74I/75E/76T) is the most dominant (77.2%) followed by CVMNK (17.7%), CVMNT (4.4%) and CVINT least prevalent (0.7%) haplotype in the country all regions except Gambella (Supplementary Fig. 11c) suggests less chloroquine pressure Gambella as P. vivax is less prevalent in this region. Additional mutations in crt gene are provided in Supplementary Data 1.
Complexity of infection, genetic diversity, and parasite population structure
The majority of sequenced samples were monogenomic 745 (87.1%) (Supplementary Fig. 12a), consistent with previous reports5,57, with some levelof variation in complexity of infection at the regional level (Fig. 4a, Supplementary Data 8). The maximum COI detected was 4 (from Gambella Region). We performed a genetic diversity analysis using SNP π (nucleotide diversity) and observed that the Gambella population exhibits the highest SNP π value (Fig. 4c), indicating greater genetic diversity compared to other regions. This finding is consistent with the higher number of clones detected from Gambella, likely reflecting relatively high malaria transmission during the study in the region. Principal components (PCs) 1 and 2 revealed distinct clustering of parasites from Gambella, supporting regional differentiation of the P. falciparum population within Ethiopia with some level parasite clustering by K13 622I status (Fig. 4a, Supplementary Fig. 12b). Pairwise population differentiation analysis (multilocus FST) showed that the parasite population from Gambella has a significantly higher degree of differentiation compared to other regions, which supports the PCA results, where parasites from Gambella formed a distinct cluster (Fig. 4d).
a Complexity of infections for P. falciparum at the regional level. Colors indicate regions, and black dots inside violin plots indicate median COI. b PCA plot of P. falciparum isolates (n = 855) at the regional level. Colors indicate the geography of sample origins, and shapes indicate k13 R622I mutation status. Each diamond or dot indicates individual parasites. The percentage of variance explained by each PCA is presented in each plot. c Nucleotide diversity (π) across different populations based on SNP minor allele frequency (MAF). Parasites from Gambella exhibit the highest SNP π values, indicating greater genetic diversity compared to other populations. Error bars represent the standard error of the mean nucleotide diversity for each population. d Pairwise differentiation of parasite populations across five regions: Amhara, Gambella, Oromia, SNNP, and Somali. The color intensity indicates the degree of differentiation, with darker shades representing higher differentiation. COI complexity of infection, PCA principal component analysis, k13 kelch13 gene, SNP single-nucleotide polymorphism, MAF minor allele frequency, π nucleotide diversity, SNNP Southern Nations, Nationalities, and Peoples’ Region.
Spatial patterns of parasite relatedness and connectivity
We conducted Identity-By-Descent (IBD) analysis of monogenomic infections to further elucidate the connectivity of the parasite population across different regions. Overall, we observed a tailed distribution of highly related parasite pairs (Fig. 5a, Supplementary Data 9) with some level of spatial heterogeneity of proportion of pairs IBD for parasite population at each health center (Fig. 5b). The proportion of IBD sharing was higher within health facilities compared to between health facilities. The lowest IBD sharing was observed between the Abol health center in the Gambella Region and other health facilities (Supplementary Fig. 13), which supports the distinct clustering of Gambella parasites in the PCA (Fig. 4b). We then conducted relatedness network analysis to assess where haplotypes sharing IBD above the specified threshold clustered by geographic region or sample origin. We found clear clustering of highly related parasite pairs (IBD ≥ 0.90) within health centers, suggesting inbreeding and clonal transmission at a local scale (Fig. 5c).
a Pairwise IBD sharing across 12 health facilities. The plot shows the probability that any two isolates are identical by descent, where the x-axis indicates IBD values and the y-axis indicates the frequency (%) of isolates sharing IBD. The inset highlights highly related parasite pairs with a heavy tail in the distribution, and some highly related pairs of samples having IBD ≥ 0.90. b Pairwise IBD sharing within a health facility. Boxes indicate the interquartile range, the line indicates the median, the whiskers show the 95% confidence intervals, and dots show outlier values. c Relatedness network of highly related parasite pairs (IBD ≥ 0.90) at study site. Each dot indicates a sample and colors correspond to health facilities across five regions in Ethiopia. Each node identifies a unique isolate, and an edge is drawn between two isolates if they share their genome above IBD ≥ 0.90. Only Isolates (n = 467) that share IBD ≥ 0.90 of their genomes with any other isolates are shown. d Spatial distribution of highly related parasite pairs with IBD ≥ 0.90. Color of circles or connecting lines represents the level of IBD sharing within and between sites, respectively. The within-site shading is based upon the most related pair of parasites at the site. IBD, identity by descent; P. falciparum, Plasmodium falciparum.
However, occasional sharing of nearly clonal parasites was seen between clinics, suggesting long range parasite sharing. ANOVA revealed significant differences in IBD-sharing between health centers (p = 0.0007), confirming spatial heterogeneity in IBD-sharing across the sites and it reflects variable malaria transmission. Visualization of the relatedness network on an Ethiopia map showed that most highly related pairs (IBD ≥ 0.90) were clustered within or near specific regions (Fig. 5d), with rare connections between Gambella and other areas, supporting limited gene flow between Gambella and other populations which supports PCA results (Fig. 4b). Additionally, we conducted an IBD network analysis using a lower IBD threshold (Supplementary Fig. 14), which revealed clustering of parasites from different regions and districts suggesting widespread genetic exchange across regions.
Discussion
Findings from our genomic analysis of parasites collected across 12 sentinel sites suggest a critical threat of ART-R in Ethiopia. Compared to previous reports in Ethiopia, we observed increased k13 R622I prevalence and evidence of spread. Specifically in 2022, we found a prevalence of R622I up to 53.7% in Andansa Health Centre within the Amhara region, compared to 2.4%56 in 2014 and 10%5 in 2018 at other health centers in the same region. The prevalence of R622I is much lower in other regions and is zero in the southern part of the country. This pattern remains consistent with a potential epicenter in Eritrea or along the border and outward spread. Parasites with the R622I mutation are more closely related and tend to cluster at the health facility or district level, in contrast to wild-type parasites. This suggests that mutant parasites spread rapidly within specific areas. The clustering of mutant parasites, alongside some wild-type variants, occurs prominently at a local scale, pointing to some level of connectivity between health facilities. This pattern indicates localized bursts of clonal spread. These findings align with our previous report of clonal transmission in three Ethiopian regions5. The clonal nature of k13 R622I mutant parasites, compared to wild-type parasites, points to inbreeding, especially in low transmission areas58,59.
This work at 12 sentinel sites across five regions provides a broader geographic understanding of parasite diversity and relatedness compared to previous work, which focused on fewer sites, mainly in the northern and northwestern regions regions5. It also highlights the value of establishing genomic surveillance at malaria sentinel sites, particularly how repeated surveillance can play a crucial role in tracking the emergence and spread of drug-resistant strains in different parts of Ethiopia. Integrating this infrastructure into malaria control programs and national laboratories, enabling them to detect early signals of resistance, monitor its geographic spread, and assess the effectiveness of current treatments60,61.
In addition to k13 R622I, three WHO-validated k13 mutations (A675V, P441L, and P574L) are reported, as far as we are aware, for the first time in Ethiopia. These k13 mutations are becoming more common in East Africa in East Africa22,23,62,63. The k13 P441L mutation was found in three health centers from different geographic areas with variable malaria transmission and a recent increase in malaria cases. The k13 P574L mutation was present in 5 samples from only one site, Batu Health Center in the Oromia region. k13 P574L mutations have each been shown to have multiple independent origins throughout SE Asia64 and have been reported in Africa65. However, whether this is an African or Asian origin of the k13 P574L mutation remains undetermined. Expanding genomic surveillance in endemic regions is critical to filling this knowledge gap and ensuring that appropriate interventions are put in place to monitor and mitigate the spread of resistance.
The k13 A675V mutation was only found in one health center from the Gambella Region of western Ethiopia, neighboring South Sudan. This mutation was reported in isolates collected in Uganda beginning in 2016. It has proven to enhance parasite survival in vitro and has been associated with resistance in vitro63,66. Importation of the A675V mutation seems probable given the IBD analysis showed lower relatedness and 4/6 of the participants with the mutation reported travel. However, we cannot confirm whether the haplotypes carrying this mutation are imported or locally emerged due lack of publicly available WGS data with k13 A675V mutations from East Africa. While microsatellite markers have been used in Southeast Asia to investigate the origin of similar mutations before WGS became widely accessible, our study does not utilize microsatellite data, and thus, such an analysis is not possible with our current dataset. Potentially supporting the impact of travel and importation on parasites in Ethiopia, the parasite population from Gambella did not cluster with other parasite populations in the country. While this differentiation could be seen for multiple reasons, Gambella shares a border with South Sudan and receives a large number of refugees from across the border. Recent studies of South Sudanese refugees entering and arriving at the Ugandan Adjumani refugee camp show a 15.4% prevalence of A675V67. Combined, this suggests that A675V may be spreading rapidly across South Sudan, thereby entering Ethiopia.
We also found a high prevalence of mutations associated with modestly reduced lumefantrine susceptibility, though direct evidence for a role in resistance remains limited68. Most of the genotyped samples carried the MDR1 NFD haplotype69,70,71,72, which fits with the evidence of their selection occurring earlier. Many parasites with WHO-validated ART-R markers also carried the MDR1 NFD haplotype, suggesting an increased risk of ACT failure. The co-occurrence of k13 mutations and MDR1 NFD may intensify drug selection pressure, prolonging exposure to lumefantrine and reducing its efficacy. The increasing prevalence of MDR1 NFD in East Africa suggests significant ACT selective pressure. With reports of declining ACT efficacy and rising treatment failures, close monitoring and alternative treatment strategies (e.g., sequential or triple ACT) are urgently needed in Ethiopia. Moreover, our findings highlight the persistent high prevalence of mutations associated with resistance to SP and chloroquine in Ethiopia, despite the withdrawal of SP as a first-line treatment in 2004 and its lack of use for intermittent preventive treatment in pregnant women. This persistence of SP-resistant mutations may be influenced by factors such as selective pressure from the use of co-trimoxazole in the country, or SP was fixed, and the absence of fitness costs for maintaining these mutations. On the other hand, chloroquine resistance, although no longer used as a first-line treatment for P. falciparum, remains prevalent, especially in regions where it continues to be used for P. vivax infections. The crt 76T, a key marker for chloroquine resistance, dominates, although regions like Gambela show lower prevalence, possibly due to lower P. vivax transmission. This indicates that local drug pressures and parasite population dynamics are crucial in shaping resistance patterns, with significant geographic variability across the country. These findings underscore the complexity of malaria drug resistance in Ethiopia and the ongoing challenges in managing both P. falciparum and P. vivax infections.
This study does have limitations. First, it does not address whether the mutations are directly emerging locally or are imported. This will be possible as more genomic information is produced from other areas of Africa and whole genome sequencing of these isolates is done, allowing for accurate tracking of K13 haplotypes. Second, it was cross-sectional and did not follow patients to assess for potential clinical measures of resistance (delayed clearance and recrudescence). Third, this study reflects the situation in Ethiopia from several years ago (2019–2023). The implementation of in-country sequencing would accelerate data generation and enable quicker action based on current trends in resistance. Fourth, 12 sentinel sites do not represent the entirety of malaria epidemiology or parasite populations circulating in Ethiopia. Nonetheless, sampling across most regions of the country provides valuable, generalizable information for the malaria control program. Despite these limitations, these data provide important findings about how ART-R is spreading in the Horn of Africa, which is critical information for malaria control programs. Lastly, our data suggests importation and population movement may play a role in the genetic patterns seen, but we do not have details on locations and duration of travel to test this.
In conclusion, this study highlights critical challenges for malaria control including: 1) the continued emergence and spread of the validated 622I mutation, 2) the detection of additional validated ART-R mutations in the Horn of Africa, and 3) the high rate of the co-occurrence of ART-R with the MDR1 NFD haplotype associated with reduced sensitivity to lumefantrine, the key partner drug in the region. It also raises additional questions about the impact of importation and travel on the spread of antimalarial resistance, questions that will be answered as more genomic data from Africa becomes available. We also demonstrate that sentinel surveillance systems can leverage genomics to provide critical information to control programs and potentially can help target where in vivo studies should be focused to determine the clinical impacts of antimalarial resistance polymorphisms, as was done for validated ART-R in Tanzania due to the 561H mutation15,23. All of East Africa and the Horn of Africa are going to face significant challenges in the years to come due to emerging antimalarial resistance, and malaria molecular surveillance will play a key role in fighting this emerging threat4,6,36.
Data availability
All sequencing data from the current study are available under accession numbers SAMN44118927–SAMN44119831 at the Sequence Read Archive (http://www.ncbi.nlm.nih.gov/sra). The associated BioProject can be found under accession number PRJNA1170993 (https:// www.ncbi.nlm.nih.gov/bioproject/). De-identified patient clinical information, a data dictionary, and drug resistance genotypes are provided in Supplementary Tables 1–4. Raw drug resistance genotypes are included in Supplementary Data 3. The source data for Fig. 1a is in Supplementary Data 1, the source data for Fig. 1b is in Supplementary Data 2, the source data for Fig. 2b is in Supplementary Data 4, the source data for Fig. 2c, d are in Supplementary Data 5, the source data for Fig. 3a is in Supplementary Data 6, the source data for Fig. 3b is in Supplementary Data 7, the source data for Fig. 4a–d are in Supplementary Data 8, and the source data for Fig. 5a–d are in Supplementary Data 9. All supplementary data and tables are available with the online version of the manuscript.
Code availability
Code used and respective input files to generate figures and tables in this paper re available on GitHub at https://github.com/Abefola/EPHI_SentinelSites_DR_project.git. Additional software packages and tools that are useful when working with MIP data are available at https://github.com/bailey-lab/MIPTools and https://github.com/Mrc-ide/mipanalyzer.
References
World Health Organization. World Malaria Report 2022. (World Health Organization, 2022).
Bhatt, S. et al. The effect of malaria control on Plasmodium falciparum in Africa between 2000 and 2015. Nature 526, 207–211 (2015).
Beeson, J. G. et al. The RTS, S malaria vaccine: Current impact and foundation for the future. Sci. Transl. Med. 14, eabo6646 (2022).
Rosenthal, P. J. et al. The emergence of artemisinin partial resistance in Africa: how do we respond? Lancet Infect. Dis. https://doi.org/10.1016/S1473-3099(24)00141-5 (2024).
Fola, A. A. et al. Plasmodium falciparum resistant to artemisinin and diagnostics have emerged in Ethiopia. Nat. Microbiol. 8, 1911–1919 (2023).
Ishengoma, D. S. et al. Urgent action is needed to confront artemisinin partial resistance in African malaria parasites. Nat. Med. https://doi.org/10.1038/d41591-024-00028-y (2024).
Feleke, S. M. et al. Plasmodium falciparum is evolving to escape malaria rapid diagnostic tests in Ethiopia. Nat. Microbiol. 6, 1289–1299 (2021).
Zinszer, K. & Talisuna, A. O. Fighting insecticide resistance in malaria control. Lancet Infect. Dis. 23, 138–139 (2023).
Emiru, T. et al. Evidence for a role of Anopheles stephensi in the spread of drug- and diagnosis-resistant malaria in Africa. Nat. Med. 29, 3203–3211 (2023).
Nkumama, I. N., O’Meara, W. P. & Osier, F. H. A. Changes in Malaria Epidemiology in Africa and new challenges for elimination. Trends Parasitol 33, 128–140 (2017).
Nosten, F. & White, N. J. Artemisinin-Based Combination Treatment of Falciparum Malaria. (American Society of Tropical Medicine and Hygiene, 2007).
Slater, H. C., Griffin, J. T., Ghani, A. C. & Okell, L. C. Assessing the potential impact of artemisinin and partner drug resistance in sub-Saharan Africa. Malar. J. 15, 10 (2016).
Halsey, E. S. & Plucinski, M. M. Out of Africa: Increasing reports of artemether-lumefantrine treatment failures of uncomplicated Plasmodium falciparum infection. J. Travel Med. 30, taad159 (2023)
Kokwaro, G., Mwai, L. & Nzila, A. Artemether/lumefantrine in the treatment of uncomplicated falciparum malaria. Expert Opin. Pharmacother. 8, 75–94 (2007).
Ishengoma, D. S. et al. Evidence of artemisinin partial resistance in North-western Tanzania: clinical and drug resistance markers study. Lancet Infect. Dis. https://doi.org/10.1016/S1473-3099(24)00362-1 (2024).
Tumwebaze, P. et al. Changing antimalarial drug resistance patterns identified by surveillance at three sites in Uganda. J. Infect. Dis. 215, 631–635 (2017).
Dondorp, A. M. et al. Artemisinin resistance in Plasmodium falciparum malaria. N. Engl. J. Med. 361, 455–467 (2009).
Noedl, H. et al. Evidence of Artemisinin-resistant malaria in Western Cambodia. N. Engl. J. Med. 359, 2619–2620.
Tun, K. M. et al. Spread of artemisinin-resistant Plasmodium falciparum in Myanmar: a cross-sectional survey of the K13 molecular marker. Lancet Infect. Dis. 15, 415–421 (2015).
Ashley Elizabeth, A. et al. Spread of Artemisinin Resistance in Plasmodium falciparum Malaria. N. Engl. J. Med. 371, 411–423.
Uwimana, A. et al. Author Correction: Emergence and clonal expansion of in vitro artemisinin-resistant Plasmodium falciparum kelch13 R561H mutant parasites in Rwanda. Nat. Med. 27, 1113–1115 (2021).
Young, N. W. et al. High frequency of artemisinin partial resistance mutations in the great lake region revealed through rapid pooled deep sequencing. medRxiv https://doi.org/10.1101/2024.04.29.24306442. (2024).
Juliano, J. J. et al. Prevalence of mutations associated with artemisinin partial resistance and sulfadoxine-pyrimethamine resistance in 13 regions in Tanzania in 2021: a cross-sectional survey. Lancet Microbe. 5,100920 (2024).
Mihreteab, S. et al. Increasing prevalence of Artemisinin-resistant HRP2-negative Malaria in Eritrea. N. Engl. J. Med. 389, 1191–1202 (2023).
Balikagala, B. et al. Evidence of Artemisinin-resistant malaria in Africa. N. Engl. J. Med. 385, 1163–1171 (2021).
van Loon, W. et al. Detection of Artemisinin Resistance Marker Kelch-13 469Y in Plasmodium falciparum, South Kivu, Democratic Republic of the Congo, 2022. Am. J. Trop. Med. Hyg. 110, 653–655 (2024).
Dhorda, M. et al. Artemisinin-resistant malaria in Africa demands urgent action. Science 385, 252–254 (2024).
Humphreys, G. S. et al. Amodiaquine and artemether-lumefantrine select distinct alleles of the Plasmodium falciparum mdr1 gene in Tanzanian children treated for uncomplicated malaria. Antimicrob. Agents Chemother. 51, 991–997 (2007).
Venkatesan, M. et al. Polymorphisms in Plasmodium falciparum chloroquine resistance transporter and multidrug resistance 1 genes: parasite risk factors that affect treatment outcomes for P. falciparum malaria after artemether-lumefantrine and artesunate-amodiaquine. Am. J. Trop. Med. Hyg. 91, 833–843 (2014).
Rosado, J. et al. Ex vivo susceptibility to antimalarial drugs and polymorphisms in drug resistance genes of African Plasmodium falciparum, 2016-2023: a genotype-phenotype association study. bioRxiv https://doi.org/10.1101/2024.07.17.24310448 (2024).
Sisowath, C. et al. In vivo selection of Plasmodium falciparum pfmdr1 86N coding alleles by artemether-lumefantrine (Coartem). J. Infect. Dis. 191, 1014–1017 (2005).
Björkman, A., Gil, P. & Alifrangis, M. Alarming Plasmodium falciparum resistance to artemisinin-based combination therapy in Africa: the critical role of the partner drug. Lancet Infect. Dis. 24, e540–e541 (2024).
Deressa, T., Seid, M. E., Birhan, W., Aleka, Y. & Tebeje, B. M. In vivo efficacy of artemether-lumefantrine against uncomplicated Plasmodium falciparum malaria in Dembia District, northwest Ethiopia. Ther. Clin. Risk Manag. 13, 201–206 (2017).
Nega, D. et al. Therapeutic efficacy of Artemether-Lumefantrine (Coartem®) in treating uncomplicated P. falciparum malaria in Metehara, Eastern Ethiopia: Regulatory clinical study. PLoS One 11, e0154618 (2016).
Daka, D. et al. Therapeutic efficacy of artemether-lumefantrine in the treatment of uncomplicated Plasmodium falciparum malaria in Arba Minch Zuria District, Gamo Zone, Southwest Ethiopia. Malar. J. 23, 282 (2024).
Assefa, A., Fola, A. A. & Tasew, G. Emergence of Plasmodium falciparum strains with artemisinin partial resistance in East Africa and the Horn of Africa: is there a need to panic? Malar. J. 23, 34 (2024).
Hamlet, A. et al. The potential impact of Anopheles stephensi establishment on the transmission of Plasmodium falciparum in Ethiopia and prospective control measures. BMC Med. 20, 135 (2022).
Messenger, L. A. et al. Insecticide resistance in Anopheles arabiensis from Ethiopia (2012-2016): a nationwide study for insecticide resistance monitoring. Malar. J. 16, 469 (2017).
Nigussie, T. Z., Zewotir, T. & Muluneh, E. K. Effects of climate variability and environmental factors on the spatiotemporal distribution of malaria incidence in the Amhara National Regional State, Ethiopia. Spat. Spatiotemporal Epidemiol. 40, 100475 (2022).
Tandoh, K. Z., Duah-Quashie, N. O., Raman, J. & Ochola-Oyier, L. I. Editorial: Malaria molecular epidemiology current situation in Africa. Front Epidemiol 4, 1400612 (2024).
Inzaule, S. C., Tessema, S. K., Kebede, Y., Ogwell Ouma, A. E. & Nkengasong, J. N. Genomic-informed pathogen surveillance in Africa: opportunities and challenges. Lancet Infect. Dis. 21, e281–e289 (2021).
Schaffner, S. F. et al. Malaria surveillance reveals parasite relatedness, signatures of selection, and correlates of transmission across Senegal. Nat. Commun. 14, 7268 (2023).
de Haan, F. et al. Strategies for deploying triple artemisinin-based combination therapy in the Greater Mekong Subregion. Malar. J. 22, 261 (2023).
Struelens, M. J. et al. Real-time genomic surveillance for enhanced control of infectious diseases and antimicrobial resistance. Front. Sci. Ser. 2, 1298248 (2024)
Golumbeanu, M., Edi, C. A. V., Hetzel, M. W., Koepfli, C. & Nsanzabana, C. Bridging the Gap from Molecular Surveillance to Programmatic Decisions for Malaria Control and Elimination. Am. J. Trop. Med. Hyg. https://doi.org/10.4269/ajtmh.22-0749 (2023).
Teyssier, N. B. et al. Optimization of whole-genome sequencing of Plasmodium falciparum from low-density dried blood spot samples. Malar. J. 20, 116 (2021).
Aydemir, O. et al. Drug-resistance and population structure of Plasmodium falciparum across the Democratic Republic of Congo using high-throughput molecular inversion probes. J. Infect. Dis. 218, 946–955 (2018).
Niaré, K. et al. Highly multiplex molecular inversion probe panel in Plasmodium falciparum targeting common SNPs approximates whole genome sequencing assessments for selection and relatedness. Front. Genet. 16, 1526049 (2025)
Li, H. Aligning sequence reads, clone sequences and assembly con*gs with BWA-MEM. https://doi.org/10.6084/M9.FIGSHARE.963153.V1 (2014).
Garrison, E. & Marth, G. Haplotype-based variant detection from short-read sequencing. arXiv 1207.3907 [q-bio.GN] https://doi.org/10.48550/arXiv.1207.3907 (2012).
Danecek, P. et al. The variant call format and VCFtools. Bioinformatics 27, 2156–2158 (2011).
Chang, H.-H. et al. THE REAL McCOIL: A method for the concurrent estimation of the complexity of infection and SNP allele frequency for malaria parasites. PLoS Comput. Biol. 13, e1005348 (2017).
Zheng, X. et al. A high-performance computing toolset for relatedness and principal component analysis of SNP data. Bioinformatics 28, 3326–3328 (2012).
Verity, R. et al. The impact of antimalarial resistance on the genetic structure of Plasmodium falciparum in the DRC. Nat. Commun. 11, 2107 (2020).
GISGeography. Natural Earth Data - Free GIS Public Domain Data. GIS Geography https://gisgeography.com/natural-earth-data-free-gis-public/ (2014).
Bayih, A. G. et al. A Unique Plasmodium falciparum K13 Gene Mutation in Northwest Ethiopia. Am. J. Trop. Med. Hyg. 94, 132–135 (2016).
Abera, D. et al. Genomic analysis reveals independent evolution of Plasmodium falciparum populations in Ethiopia. Malar. J. 20, 129 (2021).
Anderson, T. J. et al. Microsatellite markers reveal a spectrum of population structures in the malaria parasite Plasmodium falciparum. Mol. Biol. Evol. 17, 1467–1482 (2000).
Camponovo, F., Buckee, C. O. & Taylor, A. R. Measurably recombining malaria parasites. Trends Parasitol 39, 17–25 (2023).
Neafsey, D. E. & Volkman, S. K. Malaria genomics in the era of eradication. Cold Spring Harb. Perspect. Med. 7, a025544 (2017).
Auburn, S. & Barry, A. E. Dissecting malaria biology and epidemiology using population genetics and genomics. Int. J. Parasitol. 47, 77–85 (2017).
Meier-Scherling, C. P. G. et al. Selection of artemisinin partial resistance Kelch13 mutations in Uganda in 2016-22 was at a rate comparable to that seen previously in South-East Asia. medRxiv (2024) https://doi.org/10.1101/2024.02.03.24302209.
Conrad, M. D. et al. Evolution of partial resistance to Artemisinins in Malaria parasites in Uganda. N. Engl. J. Med. 389, 722–732 (2023).
Stokes, B. H. et al. Plasmodium falciparum K13 mutations in Africa and Asia impact artemisinin resistance and parasite fitness. Elife 10, e66277 (2021).
Uwimana, A. et al. Emergence and clonal expansion of in vitro artemisinin-resistant Plasmodium falciparum kelch13 R561H mutant parasites in Rwanda. Nat. Med. 26, 1602–1608 (2020).
Ikeda, M. et al. Artemisinin-resistant Plasmodium falciparum with high survival rates, Uganda, 2014-2016. Emerg. Infect. Dis. 24, 718–726 (2018).
Tukwasibwe, S. et al. Varied prevalence of antimalarial drug resistance markers in different populations of newly arrived refugees in Uganda. J. Infect. Dis. 230, 497–504 (2024).
Grais, R. F. et al. Molecular markers of resistance to amodiaquine plus sulfadoxine–pyrimethamine in an area with seasonal malaria chemoprevention in south central Niger. Malar. J. 17, 1–9 (2018).
Okell, L. C. et al. Emerging implications of policies on malaria treatment: genetic changes in the Pfmdr-1 gene affecting susceptibility to artemether-lumefantrine and artesunate-amodiaquine in Africa. BMJ Glob Health 3, e000999 (2018).
Veiga, M. I. et al. Globally prevalent PfMDR1 mutations modulate Plasmodium falciparum susceptibility to artemisinin-based combination therapies. Nat. Commun. 7, 11553 (2016).
Brhane, B. G. Rising prevalence of Plasmodium falciparum Artemisinin partial resistance mutations in Ethiopia. NCBI Sequence Read Archive. https://www.ncbi.nlm.nih.gov/bioproject/PRJNA1170993 (2025).
Fola, A. A. EPHI_SentinelSites_DR_project. Zenodo. https://doi.org/10.5281/zenodo.15707635 (2025).
Acknowledgements
The authors used an artificial intelligence language model to assist with English language editing during the writing process. The manuscript is original, and all authors take full responsibility for its content. This work was funded by the World Bank through the Africa CDC, with partial support from the National Institute of Allergy and Infectious Diseases (R01AI177791 to JBP, K24AI134990 to JJJ, and R01AI139520 to JAB).
Author information
Authors and Affiliations
Contributions
B.G.B., Ashenafi.A., A.A.F., JB.P., J.J.J., and J.A.B. conceived the study. B.G.B. led patient recruitment and sample collection with contributions from H.N., M.K., H.H., Y.W., G.T., Adugna.A, M.H., H.S., A.G., G.A., H.S., G.T. and A.A. B.G.B., A.L., and A.A.F. performed laboratory work. B.G.B. and A.A.F. led genetic data analysis and wrote the first draft of the manuscript. Ashenafi.A., J.B.P., J.J.J., and J.A.B. supported genetic data analysis and interpretations of results. All authors contributed to the writing of the manuscript and approved the final version before submission.
Corresponding authors
Ethics declarations
Competing interests
JBP reports research support from Gilead Sciences, non-financial support from Abbott Laboratories, and consulting for Zymeron Corporation, all outside the scope of the current manuscript. All other authors declare no competing interests.
Peer review
Peer review information
Communications Medicine thanks Eline Kattenberg, Craig Duffy and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. [ Peer reviewer reports are available].
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Brhane, B.G., Fola, A.A., Nigussie, H. et al. Rising prevalence of Plasmodium falciparum Artemisinin partial resistance mutations in Ethiopia. Commun Med 5, 297 (2025). https://doi.org/10.1038/s43856-025-01008-0
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s43856-025-01008-0