Abstract
Background
Sickle cell disease (SCD) is debilitating, with age-dependent complications such as stroke and liver disease, leading to significant morbidity and early mortality in young adults. Hematopoietic stem cell transplantation (HCT) is curative treatment for SCD, but transplantation-related risks often deter its use, especially in patients with severe comorbidities. A subset of severe SCD patients with significant end-organ dysfunction may benefit from a combined approach of HCT and solid organ transplantation (SOT).
Methods
To the best of our knowledge, this report presents, for the first time, the utilization of dual orthotopic liver transplantation and haploidentical HCT (haplo-HCT) for severe SCD with advanced liver cirrhosis. Employing nonmyeloablative conditioning regimen and post-transplantation cyclophosphamide (PTCy).
Results
Both patients undergo orthotopic liver transplantation followed by haplo-HCT from the same related donors, achieve stable allograft function, full donor engraftment, and successful immunosuppression withdrawal through immune tolerance induction.
Conclusions
Dual haplo-HCT and living donor liver transplantation (LDLT) is feasible in eligible SCD patients with end-stage liver disease.
Plain language summary
Sickle cell disease (SCD) affects the red blood cells resulting in pain and increased risk of infection. Transplant with bone marrow stem cells can cure SCD. Liver transplantation is also beneficial for people with liver failure. We combined transplant of liver and stem cells from the same donor in people with severe SCD and advanced liver disease. People benefited from this treatment, demonstrating this approach could be used for other people with SCD and liver disease.
Similar content being viewed by others
Introduction
Sickle cell disease (SCD) is an autosomal recessive inherited hemoglobin disorder characterized by the polymerization of abnormal sickle hemoglobin (HbS), a single nucleotide mutation in the β-globin gene that produces HbS, leading to red blood cell sickling, vaso-occlusion, hemolysis, and chronic end-organ damage. Clinically, SCD presents with anemia, pain crises, and age-dependent complications such as stroke, nephropathy, hepatopathy, and pulmonary disease. Improved therapies have increased survival, but end-organ dysfunction remains a leading cause of morbidity and mortality in adulthood, reaching >2.5 per 1,00,000 persons1,2,3,4,5,6,7. A 10-year survival probability dropped with age in patients with SCD8. Chronic organ damage caused by recurrent vascular obstruction, endothelial damage, and inflammation includes nephropathy, hepatopathy, stroke, and chronic lung disease9. Irreversible lung, kidney, and/or liver damage causes death rates of 56% and 13% in patients aged >20 and <20 years, respectively10. The prevalence of SCD is up to 2.6% and sickle-cell trait ranges from 2% to 27%11,12.
Hematopoietic stem cell transplantation (HCT) is the only curative option for SCD. HCT in SCD originated and evolved from the successful treatment of the first patient with both SCD and acute myeloid leukemia in 1984, leading to a successful cure13. Gene therapy also shows promise in curing SCD, but it has limitations, including the need for very selective criteria and high costs, which impact its accessibility and affordability, especially in low-income countries14,15,16. Recent advancements in haploidentical HCT and reduced-intensity conditioning regimens have expanded donor availability and reduced transplant-related risks, enabling the treatment of older patients with significant comorbidities11,17,18. However, patients with irreversible organ damage such as end-stage liver disease remain at high risk for transplantation-related complications19,20.
Sickle cell hepatopathy, caused by repeated sinusoidal sickling, leads to severe cholestasis, fibrosis, and ultimately cirrhosis, and it is often associated with significant liver dysfunction, including acute liver failure. Mortality is high despite supportive care and exchange blood transfusions. Chronic liver disease is also often a consequence of iron overload or transfusion-related viral hepatitis. Biliary cholelithiasis is also common in SCD and can lead to acute and chronic cholangitis21. Improved survival has been noted among recipients of single organ transplants with SCD and irreversible organ dysfunction22,23,24. Few reports have shown the feasibility of SOT as a therapeutic modality in patients with SCD with chronic organ failure25,26. Patients who receive a liver transplant can expect to gain an additional 13 to 17 years of life compared with those who never receive a transplant27. Although liver transplantation is lifesaving, it does not cure SCD itself, leaving patients vulnerable to disease recurrence. Combining liver transplantation with HCT offers a potential curative approach, using the same donor for both procedures to promote immune tolerance and facilitate immunosuppression withdrawal.
Thus, we hypothesized that a similar increase in post-transplantation survival would be observed among a more contemporary cohort of patients with severe SCD with irreversible organ damage using dual haploidentical bone marrow transplant and solid organ transplant (haplo-HCT/SOT). The lifelong immunosuppression received by SOT recipients exposes them to risks of opportunistic infections, malignancy, and other complications and even with full adherence to immunosuppression, does not eliminate the risk of chronic rejection and eventual allograft loss28. Stable mixed chimerism has been associated with immune tolerance in HLA-matched patients. A reduction of immunosuppression drugs to monotherapy was achieved in 10 of 22 HLA haplotype–matched patients with persistent mixed chimerism for at least 12 months. Withdrawal of monotherapy IST during the second year resulted in loss of detectable chimerism and subsequent rejection episodes29.
In an experimental mouse study, durable chimerism was achieved post-mismatched HCT with PTCy, and complete immune tolerance to subsequent donor-type skin grafts indicates that it could potentially serve as a platform for immune tolerance induction followed by solid organ transplantation or cell therapies30. Immune tolerance after sequential HCT followed by kidney transplant from the same donor resulted in long-term kidney-graft survival without long-term immunosuppression31.
In s study of HLA-mismatched kidney transplants combined with HCT from the same donors resulted in successfully weaned from immunosuppressants32. This appears feasible, with improvement in transplantation technology and supportive care.
As far as we are aware, no previous reports have described dual orthotopic liver transplantation and haploidentical HCT in patients with SCD-related advanced liver disease using the same donor. We report two cases demonstrating the feasibility, safety, and outcomes of this approach.
Methods
Study design and patients
Following a multidisciplinary team (MDT) meeting involving hematology, hepatology, and hepatobiliary surgery specialists, eligible patients with severe SCD and advanced liver disease were identified for sequential liver transplantation and haplo-HCT using the same related donor. The donor was selected based on optimal HLA matching, relationship to the recipient, age, sex, cytomegalovirus (CMV) status, and absence of donor-specific antibodies (DSAs).
Informed consent
Informed consent was obtained from both the patients and donors. For minors or patients unable to consent, consent was obtained from parents or legal guardians, as appropriate. Permission to publish identifiable information was also obtained from the patients and donors.
Pre-transplant management
Patients received monthly packed red blood cell (PRBC) exchanges to maintain hemoglobin S < 30% and intravenous deferoxamine chelation therapy to reduce iron overload.
Liver transplantation
On the day of liver transplantation, patients received intravenous methylprednisolone (250 mg) and basiliximab (20 mg) intraoperatively and on postoperative Day 1, followed by mycophenolate mofetil (MMF). Tacrolimus was initiated on Day 5 post liver transplantation.
Hematopoietic stem cell transplantation
Approximately 4–8 months after liver transplantation, patients underwent pre-HCT evaluation and clearance before admission to the hematopoietic cell transplant unit. A haploidentical conditioning regimen was administered, consisting of rabbit anti-thymocyte globulin (ATG), thiotepa, cyclophosphamide, fludarabine, and 200 cGy total body irradiation (TBI)33,34,35. The bone marrow was the stem cell graft source.
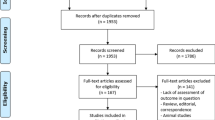
Primary graft-versus-host disease (GvHD) prophylaxis included post-transplantation cyclophosphamide, sirolimus, and MMF (Fig. 1). Ursodeoxycholic acid was given as veno-occlusive disease prophylaxis.
The regimen consisted of thymoglobulin 4.5 mg per kilogram of body weight day −9 to −7; thiotepa 10 mg per kilogram of body weight on day −7; cyclophosphamide 29 mg/kg total day −6 and day −5; fludarabine 30 mg/m2 from day −6 to day −2 or 150 mg/m2 total, and 200-cGy total-body irradiation on day −1. GVHD prophylaxis consisted of cyclophosphamide 50 mg per kilogram of body weight administered on days +3 and +4, mycophenolate mofetil 15 mg per kilogram of body weight commencing on day +5 through day +35, and sirolimus starting on day +5 through 1 year after BMT. All patients received unmanipulated, GCSF-mobilized bone marrow. BM bone marrow, BMT bone marrow transplantation, GCSF granulocyte colony-stimulating factor, GVHD graft-versus-host disease prophylaxis, MMF mycophenolate. mofetil; PO, given orally; PT post-transplantation cyclophosphamide, TBI total-body irradiation, TID three times a day.
Post-transplant monitoring
Patients were monitored regularly for toxicities and transplant outcomes, including chimerism and hemoglobin electrophoresis at Day 30, 60, 100, 180, 1 year, and as clinically indicated.
After completing 12 months of HCT, tapering immunosuppression therapy will commence once full chimerism is achieved, and no evidence of GvHD or liver allograft rejection.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Results
Patient #1
A 17-year-old male with sickle cell anemia (HbSS) complicated by frequent VOCs requiring multiple blood transfusions with secondary iron overload and SCD-related renal tubular acidosis with persistent hypokalemia. He developed liver cirrhosis—Child-Pugh class C, secondary to sickle cell hemosiderosis grade 3/4, leading to decompensated liver failure. Viral, autoimmune, and metabolic liver disease workups were negative. Multiple iron-chelating agents failed to reverse the liver damage. Ferritin level reached 6000 µg/L, and T2-weighted liver MRI showed evidence of severe iron overload. He had severe portal hypertension manifested by grade 2 esophageal varices and ascites requiring therapeutic fluid drainage.
He was referred to the HCT clinic for consideration for HCT. The ferritin level was 5698 µg/L (30–400). Hemoglobin was 80 g/L (135–180) with a normal WBC count and platelet count. Other laboratory test results were as follows: AST 175 U/L (10–45), ALT 42 U/L (10–45), ALP 349 U/L (64–115), total bilirubin 600 µmol/L (0–21), direct bilirubin 378 µmol/L, albumin 24 g/L (40–50), creatinine 19 mol/L (64–115), INR 1.7 (0.9–1.1), PT 16.2 (12.3–14.2), and PTT 46.8 (35.5–40.4). The calculated model for the end-stage liver disease (MELD) score was 28. A liver biopsy revealed severely congested sinusoids and was packed with clusters of sickle red cells. The liver parenchyma showed advanced fibrosis (cirrhosis) and cholestasis and severe iron hemosiderosis (grade ¾) consistent with sickle cell hepatopathy (Fig. 1, supplementary appendix).
After the optimal clearance and signing the consent, in December 2018, the patient underwent LDLT, i.e., partial lobe resection from the selected same donor for both liver and HCT. On the day of liver transplantation surgery, the patient received pulse steroids with methylprednisolone 250 mg intravenously and Basiliximab 20 mg intravenously (IV) in the operating room, and on Day 1 after liver transplantation, he was started on MMF. He received another dose of Basiliximab 10 mg IV on Day 4 after liver transplantation. Tacrolimus was started on Day 5 after liver transplantation. The course after liver transplantation was complicated by seizures with posterior reversible encephalopathy syndrome (PRES) secondary to Tacrolimus, as evident by brain MRI. Tacrolimus was changed to Sirolimus, and he was kept on levetiracetam; the seizures were controlled. The patient also had a brief period of elevated liver enzymes with suspicion of liver transplant rejection 20 days post-transplantation. He was started on pulse steroids of methylprednisolone 200 mg intravenously for 5 days, followed by a tapering course. In addition, he had one session of red blood cell (RBC) exchange as HbS reached 29%. Subsequently, his liver enzymes normalized. Sirolimus and MMF were continued, along with strict HbS monitoring, keeping HbS target <30% and hemoglobin at >80 g/L.
After 8 months following his liver transplantation, he was admitted to the HCT unit. He underwent a haplo-HCT using our haploidentical conditioning protocol for patients with SCD due to a lack of suitable fully matched sibling donors. The patient’s ferritin level pre-transplantation was 120 µg/L. The hematopoietic cell transplantation-specific comorbidity index (HCT-CI) was 3. The pre-allogeneic stem cell transplantation conditioning consisted of rabbit ATG, TT, Cy, Flu, and 200 cGy TBI. Bone marrow was the stem cell graft source. GvHD prophylaxis included PTCy, Sirolimus, and MMF (Fig. 1). Defibrotide was given as veno-occlusive disease (VOD) or sinusoidal obstruction syndrome (SOS) prophylaxis for 21 days in addition to ursodeoxycholic acid. The blood pressure was closely monitored and controlled with labetalol with a target blood pressure of 110-120/65-70 mmHg. The HCT course was uncomplicated, and engrafted neutrophils and platelets on Day +16 and Day +18, respectively; he did not develop signs or symptoms of VOD or acute or chronic GvHD. The peripheral blood chimerism at Day 30 after HCT was 100% donor cells for both myeloid and lymphoid cells using short tandem repeat (STR) molecular test, and the count remained within the normal range after engraftment. On Day +37 of haplo-HCT, he developed CMV viremia, which was managed with valganciclovir for approximately one month. Letermovir was not available for CMV prophylaxis. MMF was discontinued at 12 months after HCT with normal liver graft function and persistent full donor chimerism.
Sirolimus levels were kept between 3 and 8 ng/mL for another 6 months, following a slow taper; he was weaned off immunosuppression therapy (IST) at 24 months after HCT with normal liver function and blood counts with 100% donor cells on peripheral blood chimerism studies (Table 1). Chimerism analysis at different time points after HCT showed >95% donor-type chimerism in the myeloid and B-cell lineages throughout the 24 months of follow-up, at days 30, 90, 180, 1 year, and 2 years. At the time of Sirolimus discontinuation, chimerism in both myeloid and lymphoid lineages was 100%. The ferritin level after HCT is persistently within the normal values (range 30–400 µg/L), the last value at the time of weaning off Sirolimus was 137.0 µg/L. The liver function studies at the time of Sirolimus discontinuation; ALT of 24 U/L, AST of 21 U/L, Bilirubin of 6 µmol/L and albumin of 40 g/L. One year after Sirolimus discontinuation, ALT of 34 U/L, AST of 32 U/L, Bilirubin of 12 µmol/L, and albumin of 43 g/L. The coagulation profiles were consistently normal throughout 2 years post-HCT and 1 year after Sirolimus discontinuation.
Prompt lymphocyte recovery of CD4 T cells 792 mm3 (322–1750), CD8 T cells of 1199 mm3 (388–1086), and NK CD56 and CD16 cells 336 mm3 was exhibited (supplementary appendix Table S1).
Patient #2
A 25-year-old male was diagnosed with HbSS at the age of 6 months. His disease course had been complicated by frequent painful vaso-occlusive crises and frequent blood transfusions, and he required several RBC exchanges. He underwent left hip replacement at the age of 8 years due to avascular necrosis. Due to the lack of a matched sibling donor, he was on supportive care, including blood transfusion, hydroxyurea, and iron chelation therapy. In September 2019, he developed obstructive jaundice. Further investigation, including liver MRI, showed evidence of liver cirrhosis; MELD score was 25. He was referred for both liver and allogeneic stem cell transplantation. He was first evaluated in the HCT clinic in November 2019. At the time, he was jaundiced and had mild ascites. The ferritin level was 3961 µg/L. T2-weighted liver MRI indicated severe iron overload. Viral, autoimmune, and metabolic liver disease workups were negative. Laboratory test results were as follows: hemoglobin 80 g/L, normal WBC and platelet counts, AST 91 U/L, ALT 20 U/L, ALP 129 U/L, total bilirubin 604 µmol/L, direct bilirubin 472 µmol/L, albumin 30 g/L, creatinine 19 µmol/L, INR 1.2, PT 15.3, and PTT 43.5.
He was assessed in the hepatology clinic, then underwent liver biopsy, which showed features of severe sickle cell hepatopathy and advanced fibrosis (Fig. 2, supplementary appendix).
Following MTD evaluation, the best available donor was his sibling (brother) for both liver transplantation and HCT. We proceeded with LDLT first, followed by HCT after the successful outcome of the previous similar case. He was kept on monthly RBC exchange and iron chelation therapy, maintaining Hgb S < 30%. On 20 January 2021, he underwent LDLT from a living related donor, “the same donor selected for HCT,” after informed consent was signed by the patient. He received pulse steroids intraoperatively, followed by a tapering course of prednisone. Tacrolimus and MMF were also initiated as per the liver transplantation protocol. He was on a regular RBC exchange program to keep Hgb S ≤ 20% and hemoglobin ≥ 100 g/L.
Four months later, he underwent haplo-HCT from the same donor of liver transplant using the same haploidentical transplantation protocol used in case 1. Tacrolimus was replaced by sirolimus on Day 10 of HCT. His post-transplantation course was uneventful, except for asymptomatic CMV viremia that was treated with valganciclovir. Neutrophil and platelet engraftment occurred on Day +21 and Day +27, respectively. He was discharged on Day +27 of HCT. He achieved full peripheral blood chimerism (100%) for both myeloid and lymphoid lineages at Day +30 post-HCT. MMF was discontinued at 12 months after HCT with normal liver graft function and persistent full donor chimerism. At 12 months of HCT, sirolimus levels were kept between 3 and 8 ng/mL for another 8 months, following a slow taper; he was weaned off IST at 24 months after HCT with normal liver function, and blood counts and 100% donor cells on peripheral blood chimerism studies (Table 1). Chimerism analysis at different time points after HCT showed >95% donor-type chimerism in the myeloid and B-cell lineages throughout the 24 months of follow-up. At the time of Sirolimus discontinuation, chimerism in both myeloid and lymphoid lineages was 100%. The ferritin level after HCT is persistently within the normal values (range 30–400 µg/L), the last value at the time of weaning off Sirolimus was 98.4 µg/L. The liver function studies at the time of Sirolimus discontinuation; ALT of 22 U/L, AST of 32 U/L, Bilirubin of 19 µmol/L, and albumin of 49 g/L. One year after Sirolimus discontinuation, ALT of 12 U/L, AST of 27 U/L, Bilirubin of 19 µmol/L, and albumin of 46 g/L. The coagulation profiles were consistently normal throughout the 2 years post-HCT and 1 year after Sirolimus discontinuation.
He achieved prompt lymphocyte recovery of CD4 T cells 1049 mm3 (322–1750), CD8 T cells of 1253 mm3 (388–1086), and NK CD56 and CD16 cells 991 mm3 were exhibited (supplementary appendix Table S1).
In both cases, complete myeloid and lymphoid chimerism was attained without apparent risk of graft rejection or reduction in chimerism (supplementary appendix Table S1).
Discussion
To the best of our knowledge, we report, for the first time, the first two cases of patients with severe SCD who underwent sequential liver transplantation and haplo-HCT using the selected HLA haploidentical HCT donors as liver transplantation donors, then performing HCT from the same donors. This approach is a potential solution and curative option to cure SCD and to reverse preexisting end-organ dysfunction. The use of an HLA-mismatched bone marrow graft for transplantation and PTCy for GvHD prophylaxis induces durable lymphohematopoietic chimerism in recipients with a significant reduction in the risk of GvHD, allowing the withdrawal of immunosuppressants with immunotolerance and immune reconstitution with excellent lymphocyte recovery and no evidence of liver graft rejection.
Immune tolerance through donor hematopoietic stem cell infusion following kidney transplantation has been reported in two cases, both demonstrating stable mixed chimerism and no signs of graft rejection, allowing for the withdrawal of immunosuppressive therapy36,37.
Liver transplantation is the only life-saving treatment for acute and chronic sickle cell-induced liver damage. However, transplantation does not treat the disease but repairs the related end-organ damage; therefore, SCD can recur. SCD remains a very rare indication for liver transplantation worldwide. A systematic review revealed that until 2018, only 29 cases of liver transplantation for SCD were reported. The significantly low number of liver transplantations among SCD patients may be attributed to multiple factors, including limited access to liver transplantation among high-risk populations; comorbidities that make transplantation a high-risk procedure, thereby excluding SCD patients from listing; and many centers not considering SCD-related hepatopathy an acceptable indication for liver transplantation26.
Postoperative mortality is mainly due to sepsis, cerebrovascular accident, and recurrence of sickle cell liver disease. Re-transplantation rates in SCD are higher than those in other indications. Therefore, in many other centers worldwide, SCD is not an acceptable indication for liver transplantation 38,39.
Of 21 patients transplanted for SCD-induced liver failure, 57% had acute liver failure secondary to sickling, revealing 1- and 5-year survival rates of 58% and 41%, respectively. One- and 5-year survival rates in the other limited reported cases were 75% and 65%, respectively39.
An analysis of the Scientific Registry of Transplant Recipients identified 23 LDLT recipients with SCD. The median overall survival for liver transplantation in SCD was 67.7 months. The one-year graft and patient survival rates for SCD patients were 88.5% and 88.1%, respectively.
Three-year graft and patient survival rates were 72.1% and 70.5%, and five-year graft and patient survival rates were 48.1% and 58.8%, respectively. Morbidity was also higher in the peri-transplantation period. Patients with SCD were more likely to be admitted to the intensive care unit, require dialysis, and develop cardiovascular complications40.
Hosoya et al.9 reported 51 patients who underwent dual transplantation; only one patient with X-linked Hyper-IgM syndrome, who developed a potential liver toxicity, had cadaveric donor liver transplantation followed by allo-HCT from a matched unrelated donor41.
Our cases reported here show the feasibility and safety of performing liver transplantation followed by haplo-HCT for individuals with SCD and end-stage liver cirrhosis. We have demonstrated for the first time that individuals with severe SCD and end-stage liver disease can be considered for dual HCT/liver transplantation, especially with the availability of suitable related donors (fully matched or haploidentical). Our current approach was for affected patients to undergo liver transplantation first, followed by HCT. Significant supportive care before and after liver transplantation to control SCD, preserve the solid organ transplanted graft, and reduce peri- and postoperative sickle cell complications is crucial. This was achieved with the use of RBC exchange to keep HbS ≤ 30% and blood transfusion to keep Hgb ≥ 100 g/L, close monitoring of medication adverse effects (e.g., calcitonin inhibitor), and the use of judicious and effective antimicrobial screening and prophylaxis protocols.
SCD results in increased health care utilization, including chronic age-dependent end-organ dysfunction, severe morbidity, and early mortality. The limited application of HCT for individuals with SCD is traditionally related to a lack of donor availability, access, and socioeconomic barriers, comorbidities from the disease, and concern for HCT-related complications and mortality. A dual haplo-HCT/SOT approach has become more feasible because of improvements in transplantation technology and supportive care. The validation of a sequential dual SOT followed by HCT approach would require a prospective clinical trial and/or an international collaborative effort. The primary goal is to treat damaged vital organs, such as the liver and kidney, through SOT, followed by HCT to prevent further organ damage and cure SCD, using the same donor if HLA compatibility allows. A secondary goal is to eliminate the long-term use of immunosuppressive agents typically required for SOT alone by utilizing the same HLA-compatible donor for both procedures, SOT and HCT30,31,32. This will help establish clear guidelines for the dual transplantation approach, appropriate patient and donor selection, optimal conditioning, peri- and post-dual transplantation supportive care, and guidance of post-dual transplant immunosuppression therapy.
Data availability
Details of the cases are in Table 1. Additional data about the patients is available from the corresponding author upon reasonable request.
Change history
30 August 2025
A Correction to this paper has been published: https://doi.org/10.1038/s43856-025-01110-3
References
Kavanagh, P. L., Fasipe, T. A. & Wun, T. Sickle cell disease: a review. J. Am. Med. Assoc. 328, 57–68 (2022).
Piel, F. B., Steinberg, M. H. & Rees, D. C. Sickle cell disease. N. Engl. J. Med. 376, 1561–1573 (2017).
Brandow, A. M. & Liem, R. I. Advances in the diagnosis and treatment of sickle cell disease. J. Hematol. Oncol. 15, 20 (2022).
Piccin, A. et al. Autoimmune disease and sickle cell anaemia: intersecting pathways and differential diagnosis. Br. J. Haematol. 197, 518–528 (2022).
Yawn, B. P. et al. Management of sickle cell disease: summary of the 2014 evidence-based report by expert panel members. J. Am. Med. Assoc. 312, 1033–1048 (2014).
Kato, G. J. et al. Sickle cell disease. Nat. Rev. Dis. Prim. 4, 18010 (2018).
Lanzkron, S., Carroll, C. P. & Haywood, C. Jr Mortality rates and age at death from sickle cell disease: U.S., 1979-2005. Public Health Rep. 128, 110–116 (2013).
Platt, O. S. et al. Mortality in sickle cell disease. Life expectancy and risk factors for early death. N. Engl. J. Med. 330, 1639–1644 (1994).
Hosoya, H. et al. Toward dual hematopoietic stem-cell transplantation and solid-organ transplantation for sickle-cell disease. Blood Adv. 2, 575–585 (2018).
Powars, D. R., Chan, L. S., Hiti, A., Ramicone, E. & Johnson, C. Outcome of sickle cell anemia: a 4-decade observational study of 1056 patients. Medicines 84, 363–376 (2005).
Bolanos-Meade, J. & Brodsky, R. A. Blood and marrow transplantation for sickle cell disease: is less more?. Blood Rev. 28, 243–248 (2014).
Jastaniah, W. Epidemiology of sickle cell disease in Saudi Arabia. Ann. Saudi Med. 31, 289–293 (2011).
Johnson, F. L. et al. Bone-marrow transplantation in a patient with sickle-cell anemia. N. Engl. J. Med. 311, 780–783 (1984).
Frangoul, H. et al. CRISPR-Cas9 gene editing for sickle cell disease and beta-thalassemia. N. Engl. J. Med. 384, 252–260 (2021).
Basu, A. et al. Gene therapy versus common care for eligible individuals with sickle cell disease in the United States: a cost-effectiveness analysis. Ann. Intern. Med. 177, 155–164 (2024).
Morgan, G., Back, E., Besser, M., Hallett, T. B. & Guzauskas, G. F. The value-based price of transformative gene therapy for sickle cell disease: a modeling analysis. Sci. Rep. 14, 2739 (2024).
Kanter, J. et al. American Society of Hematology 2021 guidelines for sickle cell disease: stem cell transplantation. Blood Adv. 5, 3668–3689 (2021).
Bolanos-Meade, J. et al. HLA-haploidentical bone marrow transplantation with posttransplant cyclophosphamide expands the donor pool for patients with sickle cell disease. Blood 120, 4285–4291 (2012).
Klings, E. S. & Farber, H. W. Pulmonary hypertension as a risk factor for death in patients with sickle cell disease. N. Engl. J. Med. 350, 2521–2522 (2004).
Manci, E. A. et al. Causes of death in sickle cell disease: an autopsy study. Br. J. Haematol. 123, 359–365 (2003).
Praharaj, D. L. & Anand, A. C. Sickle hepatopathy. J. Clin. Exp. Hepatol. 11, 82–96 (2021).
Emre, S. et al. Liver transplantation in a patient with acute liver failure due to sickle cell intrahepatic cholestasis. Transplantation 69, 675–676 (2000).
Huang, E. et al. Improved survival among sickle cell kidney transplant recipients in the recent era. Nephrol. Dial. Transpl. 28, 1039–1046 (2013).
Kindscher, J. D., Laurin, J., Delcore, R. & Forster, J. Liver transplantation in a patient with sickle cell anemia. Transplantation 60, 762–764 (1995).
Blinder, M. A. et al. Successful orthotopic liver transplantation in an adult patient with sickle cell disease and review of the literature. Hematol. Rep. 5, 1–4 (2013).
Freedman, B. I. et al. APOL1 long-term kidney transplantation outcomes network (APOLLO): design and rationale. Kidney Int. Rep. 5, 278–288 (2020).
Jackson, W. E. et al. Survival Benefit of Living-Donor Liver Transplant. JAMA Surg. 157, 926–932 (2022).
Bertaina, A. et al. Sequential stem cell-kidney transplantation in schimke immuno-osseous dysplasia. N. Engl. J. Med. 386, 2295–2302 (2022).
Busque, S. et al. Mixed chimerism and acceptance of kidney transplants after immunosuppressive drug withdrawal. Sci. Transl. Med. 12, eaax8863 (2020).
Aversa, F. et al. Immune tolerance induction by nonmyeloablative haploidentical HSCT combining T-cell depletion and posttransplant cyclophosphamide. Blood Adv. 1, 2166–2175 (2017).
Eder, M. et al. Allograft and patient survival after sequential HSCT and kidney transplantation from the same donor-A multicenter analysis. Am. J. Transpl. 19, 475–487 (2019).
Leventhal, J. R. et al. Immune reconstitution/immunocompetence in recipients of kidney plus hematopoietic stem/facilitating cell transplants. Transplantation 99, 288–298 (2015).
de la Fuente, J. et al. Haploidentical bone marrow transplantation with post-transplantation cyclophosphamide plus thiotepa improves donor engraftment in patients with sickle cell anemia: results of an international learning collaborative. Biol. Blood Marrow Transpl. 25, 1197–1209 (2019).
Patel, D. A., Akinsete, A. M., de la Fuente, J. & Kassim, A. A. Haploidentical bone marrow transplant with posttransplant cyclophosphamide for sickle cell disease: an update. Hematol. Oncol. Stem Cell Ther. 13, 91–97 (2020).
Adetola, A. K. et al. Outcomes of non-myeloablative HLA-haploidentical bone marrow transplant with thiotepa and post-transplant cyclophosphamide in children and adults with sickle cell disease, a Phase II trial: vanderbilt global haploidentical transplant learning collaborative (VGC2). Blood 140, 2383–2385 (2022).
Nassiri, N. et al. Immune tolerance induction through haematopoietic chimerism after kidney donation. Lancet 400, e2 (2022).
Lum, E. L. et al. Delayed immune tolerance through donor haematopoietic stem cell infusion 14 months after kidney transplantation. Lancet 404, 1346 (2024).
Felli, E. et al. Liver transplantation for sickle cell disease: a systematic review. HPB ((Oxford)) 23, 994–999 (2021).
Levesque, E. et al. Liver transplantation in patients with sickle cell disease: possible but challenging-a cohort study. Transpl. Int. 33, 1220–1229 (2020).
Hogen, R. et al. Liver transplantation in patients with sickle cell disease in the United States. J. Surg. Res. 255, 23–32 (2020).
Hadzic, N. et al. Correction of the hyper-IgM syndrome after liver and bone marrow transplantation. N. Engl. J. Med. 342, 320–324 (2000).
Acknowledgements
Prof. Ghulam J. Mufti, Professor of hematology, King’s College Hospital, reviewed the paper. Prof. Josu de la Fuente, Professor of Pediatric Hematology, Imperial College London Healthcare NHS, provided the early draft of the haplo-HCT conditioning regimen protocol. Drs. Hussa Al Hussaini & Hadeel Almanea, pathologists, King Faisal Specialist Hospital & Research Center, provided the liver biopsies in the supplementary.
Author information
Authors and Affiliations
Contributions
A.A. wrote the initial draft of the paper; W.A. reviewed and edited the initial draft. Others reviewed the draft.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Communications Medicine thanks Tang-Her Jaing, Alan N. Langnas, and the other anonymous reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Alahmari, A.D., Alghamdi, S., Alasbali, R. et al. Haplo-stem cell transplant post liver transplantation to cure sickle cell disease with related liver dysfunction: a case series. Commun Med 5, 354 (2025). https://doi.org/10.1038/s43856-025-01040-0
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s43856-025-01040-0