Abstract
High-proportion spliced-in (hiPSI) titin truncating variant (TTNtv) carriers have a higher risk of atrial fibrillation and heart failure1. However, the role of cardiovascular risk factors in modifying the risk of atrial fibrillation and heart failure attributed to hiPSI TTNtv carriers is unknown. Here, we investigate the role of cardiovascular risk, quantified using the pooled cohort equations (PCEs), in influencing the hazard of outcomes attributed to hiPSI TTNtvs among UK Biobank participants without baseline cardiovascular disease. The cohort was stratified based on hiPSI TTNtv carrier status and cardiovascular risk (low: <5%, intermediate: 5.0–7.5% and high: >7.5%). The primary outcome was a composite of atrial fibrillation, heart failure or death. TTNtv noncarriers with low cardiovascular risk were used as the reference group for all analyses. Among 179,752 participants (median age: 56 (49, 62) years; 57.5% female), the risk of the primary outcome was lower in hiPSI TTNtv carriers with low cardiovascular risk (adjusted hazard ratio: 2.23 (95% confidence interval: 1.62–3.07)) than those with high cardiovascular risk (adjusted hazard ratio: 8.21 (95% confidence interval: 6.63–10.18)). A favorable cardiovascular risk factor profile may partially offset the risk of clinical outcomes among hiPSI TTNtv carriers.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
This study utilized data from the UK Biobank. UK Biobank data are available upon application to the UK Biobank (www.ukbiobank.ac.uk/). Source data are provided with this paper.
Code availability
Code utilized in this study has been deposited on GitHub (https://github.com/Arora-Translational-Lab/TTN_NCVR_2024_shetty_et_al/blob/main/Main_code).
References
Shetty, N. S. et al. High-proportion spliced-in titin truncating variants in African and European ancestry in the All of Us research program. Nat. Cardiovasc. Res. 3, 140–144 (2024)
LeWinter, M. M. & Granzier, H. L. Titin is a major human disease gene. Circulation 127, 938–944 (2013).
Fatkin, D. & Huttner, I. G. Titin-truncating mutations in dilated cardiomyopathy: the long and short of it. Curr. Opin. Cardiol. 32, 232–238 (2017).
Herman, D. S. et al. Truncations of titin causing dilated cardiomyopathy. N. Engl. J. Med. 366, 619–628 (2012).
Schafer, S. et al. Titin-truncating variants affect heart function in disease cohorts and the general population. Nat. Genet. 49, 46–53 (2017).
Schiabor Barrett, K. M. et al. Cardiomyopathy prevalence exceeds 30% in individuals with TTN variants and early atrial fibrillation. Genet. Med. 25, 100012 (2023).
Haggerty, C. M. et al. Genomics-first evaluation of heart disease associated with titin-truncating variants. Circulation 140, 42–54 (2019).
Roberts, A. M. et al. Integrated allelic, transcriptional, and phenomic dissection of the cardiac effects of titin truncations in health and disease. Sci. Transl. Med. 7, 270ra276 (2015).
Pirruccello, J. P. et al. Titin truncating variants in adults without known congestive heart failure. J. Am. Coll. Cardiol. 75, 1239–1241 (2020).
Ahlberg, G. et al. Rare truncating variants in the sarcomeric protein titin associate with familial and early-onset atrial fibrillation. Nat. Commun. 9, 4316 (2018).
Choi, S. H. et al. Association between titin loss-of-function variants and early-onset atrial fibrillation. JAMA 320, 2354–2364 (2018).
Tayal, U. et al. Truncating variants in titin independently predict early arrhythmias in patients with dilated cardiomyopathy. J. Am. Coll. Cardiol. 69, 2466–2468 (2017).
McAfee, Q. et al. Truncated titin proteins in dilated cardiomyopathy. Sci. Transl. Med. 13, eabd7287 (2021).
Akinrinade, O., Alastalo, T. P. & Koskenvuo, J. W. Relevance of truncating titin mutations in dilated cardiomyopathy. Clin. Genet. 90, 49–54 (2016).
Hershberger, R. E., Hedges, D. J. & Morales, A. Dilated cardiomyopathy: the complexity of a diverse genetic architecture. Nat. Rev. Cardiol. 10, 531–547 (2013).
Yusuf, S. et al. Modifiable risk factors, cardiovascular disease, and mortality in 155 722 individuals from 21 high-income, middle-income, and low-income countries (PURE): a prospective cohort study. Lancet 395, 795–808 (2020).
Lau, D. H., Nattel, S., Kalman, J. M. & Sanders, P. Modifiable risk factors and atrial fibrillation. Circulation 136, 583–596 (2017).
Ahmad, F. S. et al. Hypertension, obesity, diabetes, and heart failure-free survival: the cardiovascular disease lifetime risk pooling project. JACC. Heart Fail. 4, 911–919 (2016).
Khera, A. V. et al. Genetic risk, adherence to a healthy lifestyle, and coronary disease. N. Engl. J. Med. 375, 2349–2358 (2016).
Hasbani, N. R. et al. American heart association’s life’s simple 7: lifestyle recommendations, polygenic risk, and lifetime risk of coronary heart disease. Circulation 145, 808–818 (2022).
Parcha, V. et al. Association of a multiancestry genome-wide blood pressure polygenic risk score with adverse cardiovascular events. Circ. Genom. Precis. Med. 15, e003946 (2022).
Zhu, Z. et al. Association of lifestyle with incidence of heart failure according to metabolic and genetic risk status: a population-based prospective study. Circ. Heart Fail. 15, e009592 (2022).
Fomin, A. et al. Truncated titin proteins and titin haploinsufficiency are targets for functional recovery in human cardiomyopathy due to TTN mutations. Sci. Transl. Med. 13, eabd3079 (2021).
Hinson, J. T. et al. Heart disease. Titin mutations in iPS cells define sarcomere insufficiency as a cause of dilated cardiomyopathy. Science 349, 982–986 (2015).
Fomin, A. et al. Truncated titin proteins and titin haploinsufficiency are targets for functional recovery in human cardiomyopathy due to ml mutations. Sci. Transl. Med. 13, eabd3079 (2021).
McAfee, Q. et al. Truncated titin protein in dilated cardiomyopathy incorporates into the sarcomere and transmits force. J. Clin. Invest. 134, e170196 (2024).
Kellermayer, D. et al. Truncated titin is structurally integrated into the human dilated cardiomyopathic sarcomere. J. Clin. Invest. 134, e169753 (2024).
Choi, S. H. et al. Monogenic and polygenic contributions to atrial fibrillation risk: results from a national biobank. Circ. Res. 126, 200–209 (2020).
Yoneda, Z. T. et al. Early-onset atrial fibrillation and the prevalence of rare variants in cardiomyopathy and arrhythmia genes. JAMA Cardiol. 6, 1371–1379 (2021).
Platonov, P. G., Mitrofanova, L. B., Orshanskaya, V. & Ho, S. Y. Structural abnormalities in atrial walls are associated with presence and persistency of atrial fibrillation but not with age. J. Am. Coll. Cardiol. 58, 2225–2232 (2011).
Dzeshka, M. S., Lip, G. Y., Snezhitskiy, V. & Shantsila, E. Cardiac fibrosis in patients with atrial fibrillation: mechanisms and clinical implications. J. Am. Coll. Cardiol. 66, 943–959 (2015).
Burstein, B. & Nattel, S. Atrial fibrosis: mechanisms and clinical relevance in atrial fibrillation. J. Am. Coll. Cardiol. 51, 802–809 (2008).
Romano, R. et al. Reading frame repair of TTN truncation variants restores titin quantity and functions. Circulation 145, 194–205 (2022).
Sudlow, C. et al. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 12, e1001779 (2015).
Backman, J. D. et al. Exome sequencing and analysis of 454,787 UK Biobank participants. Nature 599, 628–634 (2021).
Van Hout, C. V. et al. Exome sequencing and characterization of 49,960 individuals in the UK Biobank. Nature 586, 749–756 (2020).
McLaren, W. et al. The ensembl variant effect predictor. Genome Biol. 17, 122 (2016).
Goff, D. C. Jr. et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on practice guidelines. J. Am. Coll. Cardiol. 63, 2935–2959 (2014).
Whelton, P. K. et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: executive summary: a report of the american college of cardiology/american heart association task force on clinical practice guidelines. J. Am. Coll. Cardiol. 71, 2199–2269 (2018).
ElSayed, N. A. et al. 2. Classification and diagnosis of diabetes: standards of care in diabetes-2023. Diabetes Care 46, S19–S40 (2023).
Acknowledgements
This research has been conducted using the UK Biobank Resource under application no. 58838. P.A. is supported by the National Heart, Lung and Blood Institute of the National Institutes of Health (NIH) awards (grant nos. R01HL160982, R01HL163852 and R01HL163081). N.P. is supported by the National Institutes of Health grant no. T32HL007457.
Author information
Authors and Affiliations
Contributions
P.A. conceptualized and designed the study. P.A., N.S.S., M.G., A.P., N.P., P.L. and G.A. acquired, analyzed or interpreted data. P.A., N.S.S., M.G., A.P., N.P., P.L. and G.A. drafted the manuscript. All authors performed critical revisions of the manuscript. M.G. and A.P. did the statistical analysis. P.A. and P.L. supervised and verified the data analysis.
Corresponding author
Ethics declarations
Competing interests
P.A. reports grant support from Merck Sharp & Dohme LLC and Bristol-Myers Squibb and consulting income from Bristol-Myers Squibb, which are all unrelated to this work. The other authors declare no competing interests.
Peer review
Peer review information
Nature Cardiovascular Research thanks N. Larson and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1
Study Population Flowchart.
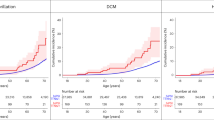
Extended Data Fig. 2 Cumulative Incidence of Study Outcomes Stratified by High Proportion Spliced-In Titin Truncating Variant Carrier Status.
This figure depicts the cumulative incidence of the primary outcome (Panel A), atrial fibrillation (Panel B), heart failure (Panel C), and all-cause mortality (Panel D) stratified by high-proportion spliced-in Titin truncating (hiPSI TTNtv) carrier status. hiPSI TTNtv carriers and non-carriers are depicted in red and blue, respectively. The x-axis represents the follow-up duration since enrollment. The at-risk table below each figure depicts the number of participants at a given age who are at risk of the outcome.
Extended Data Fig. 3 Cumulative Incidence of Study Outcomes Stratified by Cardiovascular Risk.
This figure depicts the cumulative incidence of primary outcome (Panel A), atrial fibrillation (Panel B), heart failure (Panel C), and all-cause mortality (Panel D) stratified by the cardiovascular risk. Low, intermediate, and high cardiovascular risk are presented in green, blue, and red, respectively. The x-axis represents the follow-up duration since enrollment. The at-risk table below each figure depicts the number of participants at a given age who are at risk of the outcome.
Extended Data Fig. 4 Risk of Study Outcomes According to Cardiovascular Risk Among High-Proportion Spliced-In Titin Truncating Variant Carriers.
This figure depicts the adjusted hazard ratio for study outcomes according to the cardiovascular risk profile among high-proportion spliced-in Titin truncating (hiPSI TTNtv) carriers. The cardiovascular risk was determined using the Pooled Cohort Equations and categorized into 3 groups [low (<5.0%), intermediate (5.0%-7.5%), and high (>7.5%)]. The low cardiovascular risk group was taken as the reference group. Data are presented as hazard ratio and 95% confidence interval. HR (95% CI) in the figure indicates the hazard ratio and 95% confidence interval. Panel A depicts the primary outcome. Panels B, C, and D depict the secondary outcomes of atrial fibrillation, heart failure, and all-cause mortality, respectively.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shetty, N.S., Gaonkar, M., Pampana, A. et al. Titin truncating variants, cardiovascular risk factors and the risk of atrial fibrillation and heart failure. Nat Cardiovasc Res 3, 899–906 (2024). https://doi.org/10.1038/s44161-024-00511-2
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s44161-024-00511-2