Abstract
Arterial pulsation is crucial for promoting neurofluid circulation. Most previous studies quantified pulsatility via blood velocity-based indices in large arteries. Here we propose an innovative method to quantify the microvascular volumetric pulsatility index (mvPI) across cortical layers and white matter (WM) using high-resolution four-dimensional (4D) vascular space occupancy (VASO) and arterial spin labeling (ASL) magnetic resonance imaging (MRI) at 7 T with simultaneous pulse recording. We assessed aging-related changes in mvPI in 11 young (28.4 ± 5.8 years) and 12 older (60.2 ± 6.8 years) participants and compared mvPI with large artery pulsatility assessed by 4D-flow MRI. mvPI peaked in the pial surface (0.18 ± 0.04). Deep WM mvPI was significantly higher in older participants (P = 0.006) than young ones. Deep WM mvPI correlated with large artery velocity PI (r = 0.56, P = 0.0099). We performed test–retest scans, non-parametric reliability test and simulations to demonstrate the reproducibility and accuracy of the method. In conclusion, our non-invasive method enables in vivo fine-grained measurement of mvPI, with implications for glymphatic function, aging and neurodegenerative diseases.
Similar content being viewed by others
Main
Cerebral arterial pulsation is the rhythmic dilation and constriction of brain arteries with the cardiac cycle, driven by the pressure wave from heart pumping. It was found that higher arterial pulsatility is generally associated with more severe small vessel disease (SVD)1,2,3,4 and Alzheimer’s disease as well as worse cognitive performance5,6,7,8, highlighting the role of cerebroarterial pulsatility in the pathogenesis and progression of cerebrovascular and neurodegenerative diseases.
Previous studies attempted to understand the function and underlying mechanisms of cerebroarterial pulsation within the brain. Iliff et al.9 proposed that arterial pulsatility is a key driver of cerebrospinal fluid (CSF) movement in the perivascular spaces (PVSs) into and through the brain parenchyma in mice, facilitating the clearance of interstitial solutes and wastes in the brain10,11,12. In general, arterial pulsation plays a crucial role in driving the glymphatic system13,14,15,16,17, a recently discovered waste clearance system in the brain. Mestre et al.18 directly observed that hypertension leads to an increase in arterial volumetric pulsatility, which subsequently results in a reduction in CSF flow. This finding underscores the potential influence of alterations in arterial volumetric pulsatility on the glymphatic system and provides a theoretical basis for understanding various cognitive disorders. Additionally, Jammal Salameh et al.19 found that arterial pulsation can modulate neuronal activity directly via mechanosensitive ion channels. These studies collectively support the role of arterial pulsatility in promoting fluid circulation in the glymphatic system and even directly influencing neuronal activity. However, all these studies were performed in animal models using invasive optical imaging and electrophysiological recording.
In humans, arterial pulsatility is typically measured using transcranial Doppler ultrasonography20 or phase-contrast MRI21,22 (PC-MRI), mostly in large vessels. Recently, high-resolution (submillilmeter) PC-MRI at 7 T has been applied for measuring the pulsatility of smaller lenticulostriate arteries23; however, it remains difficult to assess the pulsatility of cerebral microvasculature, including arterioles, capillaries and venules. In addition, existing methods largely quantify velocity rather than volumetric pulsatility, which more directly influences CSF movement.
Here we present a non-invasive approach to assess volumetric pulsatility of cerebral microvasculature across cortical layers in gray matter (GM) and WM, using high-resolution 4D VASO MRI24 with simultaneous recording of pulse signals at 7 T. Changes in mvPI and cerebral blood volume (CBV) across cardiac cycles are assessed through retrospective sorting of VASO signals into cardiac phases and estimating mean CBV in resting state (CBV0) by ASL MRI25 at 7 T (refer to Fig. 1 and Methods for details). We applied this method to 11 young and 12 older participants and compared mvPI results and pulsatility of large arteries assessed by 4D-flow PC-MRI. We found that mvPI was highest at the pial surface, decreasing toward deeper cortex and larger arteries. In deep WM, mvPI was substantially higher in older adults. Test–retest, non-parametric analyses and simulations confirmed the reproducibility and accuracy of our approach.
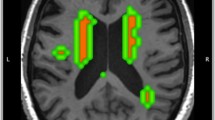
a, Cardiac phase definition: two complete cardiac cycles of pulse signals are shown. The time from one cycle’s systolic peak to the next systolic peak is divided into 10 equal phases, defined as phases 1–10. b, Retrospective sorting of images into 10 cardiac phases. The time and signal intensity curves of VASO (red) and BOLD (blue) signals are shown. The lower figure shows the trigger time corresponding to each image and its corresponding cardiac phase (black). c, CBF and CBV0 laminar profiles based on high-resolution (iso-1.25 mm) ASL scans and CBV0 were derived based on the listed equation. d, Variations of VASO signals across cardiac phases after retrospective sorting of VASO images; the mvPI was calculated based on the listed equations (details in Methods). Eq, equation; min, minutes; s, seconds.
Results
Microvascular volumetric pulsatility in pial mater, GM and WM
We first segmented the GM into six equi-volume layers (layers 1–6 from superficial to deep), one layer of superficial WM and an additional pial mater layer on the cortical surface. Due to its thinness, the pial mater layer here also includes adjacent subpial and subarachnoid spaces. Segmentation was derived from T1-weighted MRI (Extended Data Fig. 1a). The deep WM region of interest (ROI) was obtained by subtracting the superficial WM from the total WM. This enabled calculation of laminar profiles of VASO and ASL signals in pial mater, superficial and deep WM and six cortical layers (collectively referred to as cortical laminae). We calculated the laminar profile of cerebral blood flow (CBF) from ASL data for each participant. Extended Data Fig. 2a shows a representative CBF map, and Extended Data Fig. 2c shows a zoomed-in view of the superimposed segmentation, demonstrating the high quality of iso-1.25 mm CBF maps acquired using our three-dimensional turbo-FLASH (TFL) pseudo-continuous ASL (pCASL) at 7 T (ref. 25). Figure 2a illustrates the average laminar CBF and calculated CBV0 profiles of 11 young participants. A one-way repeated-measures ANOVA revealed a significant main effect of lamina (F8,80 = 12.34, P < 0.001, \({\eta }_{p}^{2}\) = 0.523 in CBF; F8,80 = 131.80, P < 0.001, \({\eta }_{p}^{2}\) = 0.921 in CBV0), indicating differences in resting CBF and CBV0 across cortical layers. The CBF profiles exhibit the highest values in the middle and superficial layers of the GM, aligning with the vascular density profiles reported by a previous study26. Based on equation (5) in Methods, we estimated the CBV changes across a cardiac cycle (ΔCBV = CBVmax − CBVmin) from VASO signals and plotted the laminar profile of ΔCBV in Fig. 2b. A one-way repeated-measures ANOVA revealed a significant main effect of lamina (F8,80 = 28.66, P < 0.001, \({\eta }_{p}^{2}\) = 0.718), indicating that ΔCBV progressively increases from the WM to superficial layers of the GM and pial mater. This observation aligns with the reported laminar profile of baseline CBV by Akbari et al.27. Using the method outlined in Fig. 1 (refer to Methods for details), we derived the laminar profile of the mvPI (Fig. 2c) in the whole imaging slab. A one-way repeated-measures ANOVA revealed a significant main effect of lamina (F8,80 = 19.66, P < 0.001, \({\eta }_{p}^{2}\) = 0.636), illustrating lamina-specific differences in mvPI. Extended Data Fig. 3a shows a matrix to quantify the differences in mvPI values across various cortical laminae. In conjunction with Fig. 2c, we found that mvPI has the highest value in cortical pial mater, which is significantly higher than all other laminae (Bonferroni correction, factor = 36, all corrected P < 0.001). In general, the cortical pial mater exhibits the highest mvPI value (0.18 ± 0.04), and the mvPI gradually decreases as the pial arteries enter the GM, reaching its lowest point in the deep WM.
Laminar profiles of CBF value (a), calculated CBV0 (a), ΔCBV (b) and mvPI (c) show the laminar changes of these parameters. The light blue shaded area indicates the WM area, and the light green shaded area indicates the pial mater area. WMd and WMs on the x axis represent the deep WM and superficial WM, respectively. The values on the x axis from 1 to 0 represent the GM from deep to superficial layers. Statistical significance was assessed by a two-sided bootstrap test (10,000 resamples) with Bonferroni correction (factor = 36). Exact P values are shown in the figure (n = 11 participants, biological replicates). Error bars indicate s.e.m. across participants. Extended Data Fig. 3a shows all comparison statistical results between laminae. d, Laminar mvPI profiles in ACA (blue), MCA (red) and PCA (green) vascular territories. The pink line shows the clustered permutation test P value between ACA and MCA. The yellow line shows the clustered permutation test P value between ACA and PCA. e, mvPI maps in a representative participant. f, Partially zoomed view of the mvPI map. NS, not significant.
Microvascular volumetric pulsatility in vascular territories
Given the different vascular compliance28 and supratentorial supply regions29 of the anterior cerebral artery (ACA), middle cerebral artery (MCA) and posterior cerebral artery (PCA), we compared average mvPI across these territories using a published vascular territory atlas30 (Extended Data Fig. 1b). Figure 2d shows laminar mvPI profiles for ACA, MCA and PCA. Two-way repeated-measures ANOVA revealed significant main effects of lamina (F8,80 = 53.14, P < 0.001, \({\eta }_{p}^{2}\) = 0.842) and territory (F2,20 = 9.84, P < 0.001, \({\eta }_{p}^{2}\) = 0.496), plus a significant interaction (F16,160 = 10.50, P < 0.001, \({\eta }_{p}^{2}\) = 0.512), indicating distinct mvPI distributions among territories. From WM to middle and superficial GM, mvPI in MCA was significantly higher than in ACA (Bonferroni factor = 9, layer 3 → superficial WM, P < 0.001; clustered permutation P = 0.006) and PCA (P < 0.001; permutation P = 0.010). Across all territories, cortical pial mater had the highest mvPI, with steeper declines in ACA and PCA than in MCA as arteries penetrated deeper.
Microvascular volumetric pulsatility maps
Voxel-wise mvPI maps were generated with the aforementioned method. Figure 2e displays the mvPI map of a representative participant. It indicates that mvPI is not uniformly distributed across the cortex, with regional high mvPI values observed in the WM. Figure 2f offers a detailed view of the mvPI map in a partially zoomed view of Fig. 2e, highlighting the distribution patterns within the GM. The arrows in this figure pinpoint areas with notably high mvPI values located in the superficial GM and pial mater. This observation aligns with the finding in the laminar profile, indicating obviously higher mvPI values in the pial mater and superficial GM compared to the deep and middle GM. Extended Data Fig. 4a shows the mvPI maps of other participants, demonstrating the high quality of mvPI maps calculated by our proposed method.
Reliability of mvPI measurements
The results presented above demonstrate a proof of concept of our method for mapping mvPI. We then investigated the reliability of our method through three distinct approaches. First, we conducted a test–retest study on six participants with a long interval (details in Extended Data Table 1; three are approximately 3 months, and another three are 5–8 months). Second, we employed a non-parametric reliability test to evaluate the robustness of our collected data. Lastly, we generated simulated data to analyze the influence of various parameters on the outcomes.
Figure 3a presents the mvPI maps from two scan sessions, conducted approximately 3 months apart, for three participants. Similarly, Extended Data Fig. 4a illustrates mvPI maps from two scans for an additional three participants, obtained over a longer interval. These images reveal that the mvPI distribution patterns remain highly consistent across the two scans for the same individual yet exhibit marked differences across different participants. To accurately quantify the differences between the images, we calculated the mean squared error (MSE) values for each pair within the six maps. The MSE value calculated between the two mvPI maps provides a comprehensive measure of the differences in both the amplitude and spatial distribution of mvPI. Figure 3b presents the MSE matrix, strengthening the observed patterns. Figure 3c further visualizes these values, demonstrating a significant distinction in the MSE distribution between maps of the same participant versus those from different participants (P = 0.0001). This finding underscores the reproducibility of the mvPI maps despite the relatively long interval between the two scans. Moreover, the capability to visualize individual mvPI maps in each participant enhances the potential for future clinical applications.
a, mvPI maps in three young participants and two different scans. b, MSE value matrix calculated by test and retest mvPI maps from six young participants. Red arrows highlight the MSE values from different scanning sessions of the same participant. c, Distribution of the MSE values in b. d, The results of the reliability test for three young participants with scan data from two sessions. The red line and red shading represent the mean laminar profile of ΔVASO and its 95% confidence interval, respectively, calculated from random data. The black line shows the laminar profile of the ΔVASO calculated for each participant. e, Average laminar profile of RI across the young participants. Statistical significance for all panels was assessed using a two-sided bootstrap test (10,000 resamples), with Bonferroni correction for multiple comparisons (factor = 9). Exact P values are shown in the figure (n = 11 participants, biological replicates). The top line shows the clustered permutation test result between RI and chance level. Error bars indicate s.e.m. across participants. f, Laminar RI profiles in ACA (blue), MCA (red) and PCA (green). The top lines show the clustered permutation test results between RI and chance level in ACA (blue), MCA (red) and PCA (green). g, Results of simulations. It shows the impact of various univariate changes (variations from left to right: tSNR, tissue volume, actual PI, CBV0 and breathing effect) on the calculated PI (blue) and RI (red). h, Baseline changes by breathing effect in simulation. It shows the chance level (blue) and 95% confidence interval upper (red).
As a second reliability check, we performed a non-parametric test by randomly shuffling the VASO time series to remove cardiac synchronization and computing ΔVASO for each shuffle. Repeating this 10,000 times produced a chance-level distribution. Figure 3d and Extended Data Fig. 5a show results for 11 young participants (six with test–retest). The measured ΔVASO (black line) exceeded the 95% confidence interval of the random distribution (red shading) at most layers, indicating high reliability and repeatability, with pial mater and superficial GM more reliable than deeper GM and WM. Reliability in WM was less stable. The temporal signal-to-noise ratio (tSNR) profile of VASO (Extended Data Fig. 5c) inversely matched the chance-level envelope, supporting the accuracy of the baseline estimation. We defined a reliability index (RI; equation (7)) to quantify detection above chance. RI > 1 indicates reliable results. Figure 3e shows that all laminae except deep WM had ΔVASO significantly above chance (Bonferroni corrected, P < 0.001; permutation P < 0.001). Deep WM pulsation was too weak for reliable mvPI estimation. Across vascular territories (Fig. 3f), ACA and PCA pulsatility was reliably detected only in pial mater and superficial GM, whereas MCA showed detectable pulsatility in all laminae except deep WM, consistent with mvPI being greater in MCA than ACA/PCA from middle GM to superficial WM. These results confirm that mvPI reflects genuine CBV changes from vascular pulsation, with clear laminar-specific and territory-specific differences. The RI metric can further serve as a quality control tool for clinical applications.
Considering multiple factors (tSNR, ROI size, breathing effect, CBV0, etc.) that may influence results, we generated simulated data based on parameters from our dataset (Extended Data Fig. 6a). Figure 3g shows the effects of univariate changes in voxel tSNR, tissue volume, actual mvPI, CBV0 and breathing effect on calculated mvPI and RI. When voxel tSNR was greater than 5, mvPI and RI remained stable, approximating the set value. In our ROIs, tSNR generally exceeded 7 (Extended Data Fig. 6e), indicating minimal impact. Tissue volumes of more than 2 ml also yielded stable estimates; actual ROI volumes generally exceeded 5 ml (Extended Data Fig. 6d). Varying the true mvPI confirmed accurate estimation: RI increased with mvPI and plateaued at mvPI of approximately 0.2, consistent with our observed maximum (Fig. 2c). CBV0 changes of more than 4% in GM/pial mater had little effect (Extended Data Fig. 6c), whereas 3–4% changes in WM influenced results (Extended Data Fig. 6b). Breathing effects did not affect mvPI, likely due to cardiac–respiratory independence, but reduced RI by raising the chance-level baseline (Fig. 3h). Overall, simulations support the reliability of our measurements and reveal genuine differences in microvascular pulsatility across vascular territories and laminae.
mvPI changes with aging
A decreasing CBF, lower metabolic rates of glucose and oxygen and a compromised structural integrity of the cerebral vasculature, especially the microvasculatures, are representative degenerative features of the vascular system of the aging brain31. To examine age effects on mvPI, we analyzed data from 12 older participants using the same procedures. The laminar mvPI profile (Fig. 4a, red) and inter-lamina difference matrix (Extended Data Fig. 3b) were compared with young participants (Fig. 4a, blue). Two-way ANOVA revealed significant main effects of laminae (F8,160 = 21.21, P < 0.001, \({\eta }_{p}^{2}\) = 0.485) and age (F1,20 = 24.06, P < 0.001, \({\eta }_{p}^{2}\) = 0.118). Older participants showed significantly higher mvPI in deep WM (Bonferroni, factor = 9, P = 0.006) and a markedly different distribution pattern (Fig. 4a and Extended Data Fig. 3a,b; Bonferroni, factor = 36). Young participants exhibited a monotonic mvPI decrease from pial mater to deep WM, whereas older participants showed a decline from pial mater to deep GM followed by a plateau. Extended Data Fig. 3d,e display CBV0 and ΔVASO profiles for both groups. No significant CBV0 difference was found in deep WM, but ΔVASO differed significantly (Bonferroni, factor = 9, P = 0.003), with a smaller P value than mvPI. Combined with the absence of CBV0 differences, this indicates that the deep WM mvPI increase in older adults mainly reflects VASO signal changes from microvascular pulsation rather than CBF differences.
a, Average laminar profile of mvPI in the young and older participants. Statistical significance for all panels was assessed using a two-sided bootstrap test (10,000 resamples). Bonferroni correction, factor = 36. Exact P values are shown in the figure (young n = 11 and older n = 11 independent biological replicates). Extended Data Fig. 3a,b shows all comparison statistical results between laminae in young and older. Error bars indicate s.e.m. across participants. b, Average laminar profile of RI in the young and older participants. Bonferroni correction, factor = 9; exact P values are shown in the figure; ***corrected P < 0.001, **corrected P < 0.01 and *corrected P < 0.05. The exact corrected P values for the comparison between young and older participants from deep WM to pia are as follows: <0.001, <0.001, 0.003, 0.017, 0.038, 0.004, 0.006, 0.004 and 0.088. c, MSE distribution in four groups: (1) between two scans of the same participant (red, six MSE points); (2) between different young participants (light blue, 130 MSE points); (3) between young and older participants (dark green, 187 MSE points); and (4) between different older participants (dark blue, 55 MSE points). The shape of each violin represents the kernel density estimation of the data. Embedded box plots indicate the interquartile range (IQR; box limits) and the median (center line). Whiskers represent the data range within 1.5× IQR from the box limits. Exact P values are shown in the figure. Bonferroni correction, factor = 6.
Figure 4b shows the laminar RI profiles for older (red) and young (blue) groups. In older participants, RI values in all laminae were significantly higher than 1 (Bonferroni factor = 9, all corrected P < 0.001; clustered permutation P < 0.001), indicating reliable detection of CBV changes from vascular pulsation across all laminae. Unlike the young group, where deep WM changes were not reliably detected, older participants showed significant CBV changes in deep WM. RI values were also significantly higher in older participants for both WM (deep and superficial WM, corrected P < 0.001) and GM (deep to superficial layers; corrected P = 0.003, 0.016, 0.034, 0.005, 0.009 and 0.006). Extended Data Fig. 7 shows mvPI and RI profiles by vascular territory, demonstrating that, across all territories, older participants had higher mvPI and RI in deep WM supplied by distal vasculature. In summary, older participants exhibited significantly higher mvPI and greater reliability in overall cortex, particularly in deep WM, compared to young participants. This observation aligns with previous studies that assessed the PI between age groups, whether based on blood flow velocity in larger arteries of humans32 or vascular volumetric changes in rats18.
Many studies identified hypertension, an age-associated chronic condition, as a major contributor to elevated cerebrovascular pulsatility18. In our cohort of older participants, half had a diagnosis of hypertension, whereas the other half did not (Extended Data Table 1). To investigate the potential contribution of hypertension to age-related changes in mvPI, we stratified the older participants into hypertensive and normotensive subgroups. As none of the young participants had hypertension, mvPI values in deep WM were compared across three groups: young adults, normotensive older adults and hypertensive older adults (Extended Data Fig. 8a). A one-way ANOVA revealed a significant group effect (F2,19 = 9.64, P = 0.001, \({\eta }_{p}^{2}\) = 0.504), indicating substantial differences in mvPI across groups. Post hoc comparisons showed that the hypertensive older group had significantly higher mvPI values than both the young group (uncorrected P < 0.001) and the normotensive older group (uncorrected P = 0.007). The normotensive older group also exhibited a trend toward increased mvPI relative to the young group (uncorrected P = 0.056), although this difference did not reach statistical significance. These findings suggest that both hypertension and aging may contribute to increased microvascular pulsatility in deep WM. Although the limited sample size constrains the statistical power of subgroup analyses and precludes definitive conclusions, the significant ANOVA results underscore the sensitivity of our method in detecting mvPI alterations associated with vascular risk factors.
Extended Data Fig. 4b shows mvPI maps of all older participants, which appear higher in WM compared to the young group (Extended Data Fig. 4a). This aligns with the greater laminar mvPI and RI values in older participants (Fig. 4a,b; two-way ANOVA, age main effect P < 0.001 for both mvPI and RI). Previous studies suggested that cerebral vascular variability may increase with age33,34, and mvPI changes may contribute. We calculated the MSE between all mvPI maps to quantify differences in amplitude and distribution, grouping results into (1) two scans of the same participant (0.072 ± 0.024), (2) different young participants (0.099 ± 0.023), (3) young versus older (0.155 ± 0.070) and (4) different older participants (0.195 ± 0.079) (Fig. 4c; Bonferroni factor = 6). MSE in group 1 was significantly lower than in other groups, indicating high repeatability and that WM mvPI heterogeneity reflects physiological, not technical, differences. Group 2 MSE was lower than group 4, supporting increased mvPI variability with age. Groups 3 and 4 had significantly higher mean and s.d. than group 2, and group 3 was lower than group 4, indicating that the variability increase is mainly due to growing differences among older participants rather than a uniform mvPI elevation.
Pulsatility of velocity and volume in the major cerebral arteries via 4D-flow PC-MRI
Finally, we used 4D-flow PC-MRI to examine the pulsations within the major cerebroarteries and their relationship with the mvPI. Previous studies demonstrated the feasibility of using 4D-flow to simultaneously measure the PI of velocity and volume at different locations of blood vessels35,36,37. As shown in Fig. 5a, we selected two ICA sites, one ACA site, three MCA sites and two PCA sites for pulsatility measurements. Figure 5b shows the cardiac phase profiles of velocity and cross-sectional area from ICA for a representative participant; similar profiles were obtained for each ROI. Using equations (8) and (9), we calculated velocity (vePI) and volumetric (voPI) PIs for both age groups (Fig. 5c and Extended Data Fig. 9b).
a, Schematic diagram of the ROI selection position of a typical subject in the circle of Willis. The lower left corner is the sagittal plane image within the black frame. b, The cardiac phase profile of velocity and cross-sectional area obtained by ICA from a random participant. c, The vePI and voPI results in both age groups within all MCA ROIs. The top image is the results of vePI, and the bottom one is the results of voPI. Red is for older participants, and blue is for young participants. The circles are the results for each participant, and the horizontal line is the average of this group of data. Statistical significance was assessed using a two-sided bootstrap test (10,000 resamples). Bonferroni correction, factor = 3. Exact P values are shown in the figure (young n = 9 and older n = 12 independent biological replicates). Error bars indicate s.e.m. across participants. d, Relationship between mvPI in deep WM and vePI in ICA and MCA1. The shading is the 95% confidence interval, and dots represent individual participants. n = 20 independent biological replicates. R2 indicates how much of the variance in the dependent variable is explained by the independent variable. e, Changes of vPI (including mvPI and voPI) as the cerebral vasculature in MCA territory. The blue and red curves represent the results for young and older participants, respectively. The light blue shaded area indicates the WM area, and the light green shaded area indicates the pial mater area. WMd and WMs on the x axis represent the deep WM and superficial WM. The values on the x axis from 1 to 0 represent the GM from deep to superficial. M1, M2 and M3 represent the MCA1, MCA2 and MCA3 segment. Young n = 9 and older n = 11 independent biological replicates. Error bars indicate s.e.m. across participants.
We focused on MCA results, as our field of view (FOV) primarily covered MCA regions, whereas coverage in other vascular territories was limited. The results for other regions are provided in Extended Data Fig. 9b. Figure 5c shows mean vePI and voPI for all MCA ROIs. For vePI, two-way ANOVA (vascular segment × age) revealed a main effect of segment (F2,56 = 25.74, P < 0.001, \({\eta }_{p}^{2}\) = 0.475), with M3 significantly lower than M1 (Bonferroni factor = 6, P < 0.001 in both groups), indicating decreased vePI in distal arteries, consistent with previous work36,37. For voPI, two-way ANOVA showed a main effect of segment (F2,56 = 15.81, P < 0.001, ηp2 = 0.357), with M3 significantly greater than M1 (Bonferroni factor = 6, P < 0.001 in both groups), opposite to the vePI trend and matching previous findings36. To investigate the age effects on vePI and voPI, we conducted a two-way ANOVA for vePI that revealed a significant main effect of age (F1,56 = 34.02, P < 0.001, \({\eta }_{p}^{2}\) = 0.374) in MCA ROIs, with vePI being significantly higher in the older group compared to the young group (Bonferroni factor = 9, as shown in Fig. 5c). This finding indicates that vePI increases with age, consistent with previous studies32,38,39 assessing vascular health. In contrast, voPI showed no significant age effect (F1,56 = 2.36, P = 0.130). Over the past several years, vePI in the ICA and M1 segment of MCA has frequently been used as an indicator to assess vascular health3,4,35,40, and vePI values have been shown to be associated with SVD1,2,3,4 and cognitive impairment in Alzheimer’s disease5,6,7,8. Next, we conducted a correlation analysis between the mvPI in deep WM calculated using the proposed method and the vePI in the ICA and M1 calculated using 4D-flow (Fig. 5d). Significant correlations exist between the mvPI in deep WM and vePI in the ICA and M1 (Pearson correlation: r = 0.5173, P = 0.0195 with ICA; r = 0.5618, P = 0.0099 with M1; n = 20, degrees of freedom = 18, two-sided test).
To characterize the dynamic changes in volumetric pulsatility along the cerebrovascular network, we combined the mvPI results in the MCA territory with voPI measurements from the MCA by 4D-flow (Fig. 5e). We found that the vPI (including both mvPI and voPI) gradually increased from proximal to distal segments in large arteries, reaching a maximum value in pial arteries within the pial mater on cortical surface. Subsequently, the mvPI decreased with increasing cortical depth, reaching a minimum in the deep WM. However, there was a significant overall increase in mvPI with aging (two-way ANOVA showed a significant main effect of age, F1,20 = 24.06, P < 0.001, \({\eta }_{p}^{2}\) = 0.118). In particular, there was a significant increase in mvPI with aging within the deep WM compared to other locations (Bonferroni factor = 9, corrected P = 0.018).
Discussion
Using our innovative method, we obtained the distribution of mvPI in both GM and WM. Simultaneously, we employed the conventional 4D-flow MRI to determine pulsatility of blood flow velocity and blood volume along the large arteries. By integrating these findings, we characterized the dynamic changes in volumetric pulsatility throughout the entire cerebrovascular tree from the large arteries to the arterial terminals of the WM. We found that arterial volumetric pulsatility peaks in the pial mater on the cortical surface, and the volumetric PI gradually decreases in both upstream arteries and downstream microvasculature. Compared to young participants, the mvPI in the GM and WM of the older participants was overall substantially increased, especially in the WM.
Several previous studies investigated the vascular origins of the VASO functional MRI (fMRI) signal41. VASO is thought to be sensitive primarily to CBV changes in pial arteries42, larger diving arterioles43, arterioles43 and capillaries44, whereas contributions from venules are expected to be weak45. Thereby, our method predominantly reflects the pulsatility of small arteries and capillaries, including pial arteries and the arteries smaller than them.
We produced a probability density distribution map of high mvPI (Extended Data Fig. 4c; details in Methods). We observed that regions with high mvPI frequently localize to watershed areas between different vascular territories in the WM. These regions are well known to be high-risk zones for various neurological disorders46. Anatomically, the vasculature in these areas primarily consists of distal arteries and capillaries, which supports the plausibility of elevated mvPI in these locations. Furthermore, the probability density map of high mvPI shows substantial overlap with WM hyperintensity probability density map47, suggesting a potential link. Notably, we also found that, in the frontal lobe, high mvPI tends to occur more frequently on the right side than on the left. This right-lateralized distribution is consistent with previous findings showing age-related reductions in CBF predominantly in the right frontal lobe48, suggesting a possible underlying relationship between these parameters.
The reliability of our method is strongly supported by rigorous validation processes. We employed non-parametric testing to confirm that our results are significantly higher than chance-level distributions, ensuring that they stem from genuine volumetric pulsatility changes rather than noise. Consistency across multiple scans of the same participants further demonstrates the stability of our method, with similar mvPI distribution patterns observed despite relatively long time gaps (3–8 months). The strong correlation between the mvPI results by our method and the vePI results obtained using 4D-flow further validates the reliability of our method. Additionally, our findings align with previous in vivo studies, particularly the high mvPI in pial mater9,14,15,18,49 and significantly increased mvPI in WM microvasculature with aging or disease in animal models18. These factors collectively affirm the reliability and potential of our method as a valuable imaging tool for assessing microvascular health in a living human brain. However, our method has a limitation in that we cannot determine a specific CBV0 value for each participant and must rely on an approximate value (0.055) derived from previous literature. We attempted to set a different CBV0 value (0.04) and found that the results remained largely consistent with those of the present study (Extended Data Fig. 8b). Although the calculated mvPI values differed, the statistical analysis and distribution patterns were essentially unchanged.
Our method shows strong potential for both research and clinical use, enabling accurate imaging of the cerebral microvascular system and capturing volumetric pulsatility in GM and WM. The mvPI proved sensitive to aging and vascular risk factors such as hypertension, consistent with a preclinical study in hypertensive mice18. This approach supports studies of neurodegenerative diseases and the cerebral glymphatic system, with implications for early diagnosis, monitoring and mechanistic exploration. For clinical applications, long scan times may be impractical. Because the deep WM mvPI could serve as a primary indicator, using lower-resolution sequences on 3 T or 7 T MRI to improve SNR may help shorten scans. Additionally, integrating a recent velocity selective ASL method50 for measuring CBF pulsatility with our approach could enable microvascular volume and blood flow pulsation maps within a clinically feasible session. In this study, we used the method to preliminarily investigate age effects on mvPI and its distribution. Next, combined with past research findings, we aim to propose a potential mechanism explaining the impact of age and vascular risks on microvascular pulsatility, thereby highlighting the feasibility and potential of our innovative method for advancing future research in this area.
Cerebral arterioles are key regulators of arterial pressure, showing a marked drop compared to large arteries51,52. Their small diameter greatly increases resistance, as described by the Poiseuille–Hagen formula (resistance ∝1 / r4), and their extensive branching further adds to this effect. As blood flows from large arteries into arterioles, the total cross-sectional area increases, lowering velocity and pressure (continuity equation A1v1 = A2v2). Smooth muscle cells in the arteriolar wall actively adjust diameter to regulate local blood flow and systemic pressure53,54. Large arteries, with their low resistance, cannot substantially reduce pulse pressure51, whereas arterioles dissipate it effectively through higher resistance and elastic wall expansion, distributing flow and protecting downstream capillaries51,55. On the brain’s surface, leptomeningeal and pial arteries possess an internal elastic lamina, basement membrane and smooth muscle layers14,56,57. Once they penetrate the cortex, they lose the elastic lamina and adventitia, becoming arterioles. Surface arterioles have densely arranged smooth muscle cells and abundant elastic fibers, enabling them to withstand higher pressures and dynamic changes58,59. By contrast, intracortical arterioles have fewer muscle cells, less dense arrangement and fewer elastic fibers, resulting in softer walls. Their main role is to supply neurons and glia within the GM, participate in local flow regulation and match metabolic demands. These anatomical differences have direct hemodynamic consequences. By the time blood reaches intracortical arterioles, much of the arterial and pulse pressure has been attenuated, reducing the need for further dissipation. Consequently, volumetric pulsatility is stronger in surface arterioles (Fig. 6). Unlike vPI, the Bernoulli equation (v2 ∝ P) shows that vePI depends on both pulse pressure and mean velocity; as both decrease distally, vePI correspondingly declines (Fig. 6). In summary, from hydromechanical and hemodynamic perspectives, cortical surface arteries exhibit the strongest volumetric pulsatility in the brain, in agreement with our observation of maximal pulsatility in the pial mater.
a, Potential physiological mechanisms of arterial pulsatility changes with laminae in normal or abnormal brain. The blue box at the top of the image illustrates the physiological mechanisms underlying the changes in vPI and vePI across arteries in young, healthy brains. Upward-pointing arrows indicate that these parameters increase along the arterial transmission pathway, whereas downward-pointing arrows signify a decrease. Conversely, the red box at the bottom of the image depicts the mechanisms of abnormal vPI and vePI in elderly or pathological brains. In this context, red arrows indicate an increase in parameters relative to healthy brains, whereas blue arrows denote a decrease. b, The laminar profiles distribution of arterial total volume, blood pressure, predicated vPI (including mvPI and voPI) and vePI in young and elderly individuals predicted by the hypothetical model.
In addition to reducing pulse pressure and protecting small vessels, cerebral arterial volumetric pulsation is a key driver of fluid circulation and waste clearance9,14,49,60,61. Experiments injecting molecules of various sizes into the rat caudate nucleus and cat CSF showed that interstitial solutes and CSF drain via the PVS and have identical half-lives, indicating bulk flow rather than diffusion10,62,63,64. Louveau et al.15 proposed that the PVS acts as a pseudo-lymphatic system, delivering fresh CSF to the interstitium and removing metabolic waste. Critically, cyclical vessel wall motion from arterial pulsation drives CSF movement18. Thus, the strong cortical surface arterial pulsation detected by our method can propel large volumes of fresh CSF into the brain parenchyma, enhancing fluid circulation and waste removal.
Aging brains show vascular degeneration, including reduced CBF, lower glucose and oxygen metabolism and structural compromise, especially in microvessels31. CBF reduction with aging likely reflects a shift toward constrictor responses, with impaired vasodilation or enhanced vasoconstriction65,66,67, compounded by age-related loss of perivascular innervation68,69. Microvascular density declines in both humans70 and animals71,72,73 with aging, accompanied by perivascular collagen deposition and basement membrane thickening74,75,76,77, reducing arteriole volume and branching and limiting their ability to dissipate arterial and pulse pressures78. Residual pressure propagates distally to distal arteries in WM, which cannot release it, mechanically increasing volumetric pulsation and producing strong wave reflections67,79. The effective reflection distance of the reflected wave increases in older participants compared to young participants79, indicating that the main reflection points of the reflected wave move distally (that is, the main source of wave reflection changed from various arterial branches to the reflection of the WM artery at the end of the artery) and support our inference according to fluid mechanics. Although wave reflection–pulsation interactions are complex, our data and rat studies18 suggest that this process enhances arterial volumetric pulsation, especially near terminal arteries. Because vascular volume changes are influenced by both direct cardiac input and reflections, the vascular wall’s time–change curve is altered, disrupting synchrony between pulsation and CSF flow. This can cause CSF reflux and markedly slow flow rate18. In summary, aging leads to markedly increased volumetric pulsation in WM arteries, with only slight increases in other arteries (Fig. 6).
In addition to aging, conditions such as hypertension and arteriosclerosis can abnormally increase arterial volumetric pulsation78,80. Prolonged exposure to elevated pulsation raises the risk of vascular degeneration, including fibrosis, particularly in small WM vessels81, leading to SVD and cerebral microbleeds81,82,83. If unchecked, these changes increase the likelihood of stroke, dementia, cognitive decline and related disorders82,83. High pulsatility also slows CSF flow18 and impairs waste clearance, promoting the accumulation of metabolic byproducts such as β-amyloid, which further obstruct clearance and may contribute to Alzheimer’s disease82,83,84. Therefore, detailed assessment of vascular volumetric pulsation can aid in evaluating vascular disorders such as SVD and cognitive diseases such as Alzheimer’s, providing broader insight into their underlying causes.
In summary, our method combining high-resolution VASO and three-dimensional TFL-pCASL MRI offers in vivo fine-grained measurement of microvascular volumetric pulsatility in the human brain. Our findings of the highest mvPI in the pial mater on the cortical surface and a significantly increased mvPI in the WM of older participants compared to younger ones have implications for cerebral microvascular health and its changes with aging and neurodegenerative diseases. Our technology offers a valuable imaging tool for understanding hydromechanical effects on cerebral microvasculature, fluid circulation and brain health.
Methods
Participants
Eleven young volunteers (mean age = 28.4 years, s.d. = 5.8 years, five females) and 12 older volunteers (mean age = 60.2 years, s.d. = 6.8 years, seven females) participated in this study. All participants in this study were healthy without known neurological or psychiatric disorders or major systemic diseases and refrained from caffeine 3 hours before the scan. All participants provided written informed consent according to a protocol approved by the institutional review board of the University of Southern California and were paid for attendance. Head motion was minimized by placing cushions on top and on two sides of the head. All participants underwent pCASL and VASO scans with recording photoplethysmogram (PPG) signals on the finger by BioPac. Six of the young participants underwent repeated VASO scans on two different days with long interval (details in Extended Data Table 1) for test and retest. Nine of the young participants and all the older participants were scanned with a 4D-flow sequence.
MRI data acquisition
MRI data were acquired on the investigational pTx part of a 7 T Terra system (Siemens Medical Systems) with an 8Tx/32Rx head coil (Nova Medical). Anatomical images were acquired with a T1-weighted MP2RAGE sequence (0.7-mm isotropic voxels, 224 sagittal slices, FOV = 224 × 224 mm2, TR = 4,500 ms, TE = 3.43 ms, TI1 = 1,000 ms, flip angle = 4°, TI2 = 3,200 ms, flip angle = 5°, bandwidth = 200 Hz/Px, slice partial Fourier = 6/8 and GRAPPA = 3).
Functional images were acquired for resting states with a slice-selective slab-inversion (SS-SI) VASO24,85,86,87 sequence (1-mm isotropic voxels, 24 axial slices, TI1/TI2/shotTR/TE = 1,367.4/2,512.2/47.7/16.2 ms, partial Fourier factor = 6/8, variable flip angle scheme with reference flip angle = 33°, three-fold GRAPPA acceleration in z direction with a CAIPIRINHA shift of 1, bandwidth = 1,644 Hz/Px, FOV = 160 mm, matrix size = 160 × 160 and acquisition time approximately 30 minutes), a three-dimensional TFL-pCASL25,88 sequence (1.25-mm isotropic voxels, 80 axial slices, FOV = 224 × 200 × 100 mm3, flip angle = 8°, TE = 2.5 ms, TR = 7 s, labeling duration = 1,500 ms, post-labeling delay = 1,500 ms, 10 segments, Poisson disc undersampling with R = 4, acquisition time approximately 12 minutes and Compressed Sensing reconstruction) and a 4D-flow PC-MRI sequence (0.8-mm isotropic voxels, 40 axial slices, FOV = 200 × 200 × 32 mm3, reconstructed cardiac phases: 12, flip angle = 15°, TR/TE = 64.32/2.87 ms, SENSE: 3, RL, AP and FH velocity encoding: 100 cm s−1, acquisition time approximately 8 minutes and Compressed Sensing reconstruction).
MRI data preprocessing
MRI data were analyzed using AFNI89, FreeSurfer90, ANTs91, SPM12 (ref. 92), the mripy package (https://github.com/herrlich10/mripy) and MATLAB (R2021a). The preprocessing of the VASO data includes removing spikes in time series, linear motion correction and T1-weighted anatomical image registration to functional volumes. ASL data were reconstructed, and CBF values were calculated using the method in previous studies25,88. We estimated a 12-parameter linear transformation from the anatomical volume to an MNI space template by nonlinear transformation with ANTs. Subsequently, we can use the vascular territory atlas30 in the standard brain template and transformed into the individual space of each participant using nonlinear transformation parameters. The 4D-flow MRI data preprocessing involved background phase correction and eddy current effects93. Velocity aliasing was corrected using phase unwrapping techniques94. Finally, the three-dimensional vector of blood flow velocity was computed for each voxel.
Cortical layers definition
VASO and ASL images were separately upsampled to a finer grid of 0.5 mm3 and 0.625 mm3 isotropic spatial resolution to avoid singularities at the edges in angular voxel space using the ‘3dresample’ program in AFNI with the nearest neighbor interpolation method. The T1-weighted MP2RAGE anatomical volume was segmented into WM, GM and CSF using FreeSurfer’s automated procedure and its high-resolution option. A boundary-based algorithm was separately used to co-register structural MP2RAGE images to VASO and ASL control images95. Eight cortical layers (one WM, six GM and one pial mater) were calculated using AFNI/SUMA and custom Python codes in the mripy package with the equi-volume layering approach96. Although the cortical depths of different brain regions vary (from approximately 4-mm thickness of the prefrontal cortex to approximately 2-mm thickness of the primary sensory cortex) and the voxel size is not large enough to clearly distinguish the cortical layers, a large number of voxels randomly sampled at different cortical depth allowed us to derive a reliable continuous laminar profile of neural activity24, as shown in Extended Data Fig. 1a.
PI calculation in VASO
Previous studies generally used (Vmax − Vmin) / Vmean (V is velocity or blood flow) as the PI calculation equation35,97. To estimate the volume change of microvasculature across the cardiac cycle, we used the following formula to calculate the mvPI:
where CBVmax, CBVmin and CBV0 are the CBV values when the blood vessels expand to their maximum volume, contract to their minimum volume and averaged over the entire cardiac cycle, respectively. ΔCBV is absolute CBV changes from CBVmin to CBVmax. According to the principle of VASO sequence98:
Equation (2) can be converted into the following:
According to equations (3) and (4), we can deduce:
where VASOmin is the VASO signal when it reaches CBVmin, and VASOmax is the VASO signal when it reaches CBVmax. Substituting equation (5) into equation (1), we can derive the equation for mvPI:
Figure 1 shows the calculation process of the mvPI using VASO and ASL data, including the following. (1) According to the recorded PPG signal, we defined 10 cardiac phases as shown in Fig. 1a. Then, we can get the cardiac phase at any timepoint like this black line in Fig. 1b, bottom. (2) Because the SS-SI VASO24,85,86,87 sequence recorded both VASO and blood oxygenation level dependent (BOLD) image series, we recorded the trigger time of all VASO images and BOLD images (blue and red bars in Fig. 1b, bottom). According to the cardiac phase corresponding to the trigger time, we can define the cardiac phase of every VASO/BOLD image (Fig. 1b, top). (3) We rebinned all the VASO and BOLD images with same cardiac phase and averaged it. Then, we got the cardiac phase profiles of both VASO and BOLD images. (4) We divided the VASO signal by the BOLD signal to obtain the cardiac phase profile of the corrected VASO signal (Fig. 1d). From this, we can calculate the value of (VASOmin − VASOmax) / VASO0 term in equation (6). (5) According to the ASL results, we can calculate the laminar profile of CBF value (Fig. 1c, left). (6) We assumed CBV0 ~ CBF0.38 according to the study by Grubb et al.99. Assuming average baseline CBV0 = 0.055 ml ml−1 in the GM100, we can get the laminar profile of CBV0 value (Fig. 1c, right). This is the 1 / CBV0 − 1 term in equation (6). Finally, we can calculate the mvPI value.
Voxel-wise mvPI maps were generated with the aforementioned method. To enhance the SNR, which may be insufficient in a single voxel, we applied intralayer spatial smoothing with a 6-mm full width at half maximum (FWHM) prior to calculation24,101. Due to the differing voxel sizes between the ASL and VASO sequences, as well as the relative low SNR of individual ASL voxels, we used an average CBF value within each laminar ROI to estimate mvPI.
We generated a high mvPI probability density distribution map by the mvPI maps of all participants projected onto the MNI template (Extended Data Fig. 4c). Due to slight variations in the FOV across participants, we first counted the number of participants covering each voxel, which was defined as the total counts of occurrences for that voxel. We then counted how often each voxel exhibited an mvPI value greater than 0.6—a subjectively defined high threshold based on the overall distribution of mvPI values—to determine the number of high mvPI occurrences at each voxel. The probability density value for each voxel was calculated by dividing the high mvPI counts by the total counts. To minimize the influence of sparse sampling and random variability, we excluded voxels with fewer than 10 total occurrences. This procedure yielded a high mvPI probability density distribution map.
Reliability test
We verified the reliability of the results using a non-parametric test. We selected an ROI to extract the average corrected VASO time series, and the ΔVASO of this ROI with cardiac cycle can be calculated using the calculation method described above equations (1)–(4). Then, we randomly shuffled the order of this time series and performed the calculation again using the same method to get a ΔVASO value. Repeating this step 10,000 times, we can get a ΔVASO value distribution of results representing no vascular pulsatility with a sample size of 10,000. We can get the mean and 95% confidence interval of this distribution, and we can also get the P value that our result satisfies the non-hypothesis that the measurement belongs to this distribution (the number of results in the distribution that are greater than the original ΔVASO divided by the sample size). We further defined an RI according to the following equation:
where ΔVASO is the calculated result from the original time series; Distributionave is the average value of the random distribution; and Distributionhigh-CI is the upper bound of the 95% confidence interval. RI is obtained by dividing the difference between the ΔVASO and the mean of the distribution by the difference between the upper level of the 95% confidence interval and the mean of the distribution. If the RI value is greater than 1, it means the result is reliable and vice versa. As shown in Extended Data Fig. 5, all participants showed reliable measurements (RI > 1) except for S15. Therefore, we used 11 older participants for mvPI analysis. The RI provided an objective and quantitative metric for quality control of our mvPI results.
PI calculation by 4D-flow
We drew several spherical masks with diameters larger than the diameter of the blood vessels at the locations of straight segments of major blood vessels. These included two ICAs, one ACA, three MCAs (M1, M2 and M3 segment) and two PCAs (P1 segment and P2 segment), shown in Fig. 5a. For more fine-grained analyses, we interpolated the resolution to 0.4 mm isotropic for subsequent calculations. Because the selected sites have small vascular curvature, we can calculate the equation of a three-dimensional plane perpendicular to the vessel based on the direction of the average blood flow velocity within the vessel. Using this plane equation, we extracted a cylindrical mask with a thickness of 1 mm, ensuring that the upper and lower planes of the cylinder were perpendicular to the vessel. By calculating the inner product of the blood flow velocity vector of each voxel within the mask and the unit blood flow velocity vector of the vessel, the velocity projection of each voxel in the blood flow direction can be determined. This approach yields a distribution of values across all voxels, comprising two components: (1) a distribution approximating a normal distribution with a mean close to 0, formed by voxels outside the vessel, and (2) a distribution with a higher mean value, formed by voxels within the vessel. To determine whether a voxel belongs to a blood vessel in a specific cardiac phase, we first sorted the distribution values less than 0 and selected the smallest 10% as the lower bound of the one-sided 95% confidence interval for the non-vascular distribution (for example, if there were 100 values less than 0, the 10th smallest value in the sorted list was chosen as the lower bound). The absolute value of this lower bound was then used as the upper limit of the one-sided 95% confidence interval for the non-vascular distribution. This value as a threshold was then applied to determine whether a voxel belongs to a blood vessel during a specific cardiac phase. All voxels with velocity values exceeding the threshold at all cardiac phases were considered part of the vascular mask. Using this mask, we can calculate the cardiac phase profile of blood flow velocity (Fig. 5b, blue line). Due to the laminar flow effect of blood, it is not possible to directly determine the volumetric proportion of the vascular component within a voxel at a given cardiac phase timepoint based solely on the velocity value of the voxel projected in the direction of blood flow. Consistent with a previous study36, for each cardiac phase, we applied half the value of the highest PC-MRI magnitude image as a threshold to identify vascular voxels—that is, a voxel was considered part of the vessel for that cardiac phase only if the vascular volume proportion within the voxel exceeded this threshold. Extended Data Fig. 9a illustrates the volume pulsatility of large and small arteries, respectively. The number of such voxels was then multiplied by the voxel volume (0.43 mm3) and divided by the cylinder height (1 mm) to calculate the cross-sectional area of the vessel for that cardiac phase. Then, we can get the cardiac phase profile of the arterial cross-sectional area (Fig. 5b, green line). Finally, we can calculate the PI values using the following equations:
where v means blood flow velocity, and S means vessel cross-sectional area. vePI and voPI present the PI values of the changes in blood flow velocity and arterial volume, respectively.
Calculation of MSE
Image stability assessment such as MSE102 and peak signal-to-noise ratio (PSNR)103 are widely used to measure the quality and stability of image processing. An mvPI map can be calculated based on the data from each visit of any participant. Then, we projected all vmPI maps into MNI space using the nonlinear projection parameters calculated by ANTs. Twelve mvPI maps from six participants, who underwent both test and retest sessions, were selected for analysis (for Fig. 3b,c). We used the common mask intersection of these 12 mvPI maps as the new mask, so all calculations used only the same batch of voxels. Then, we calculated the MSE value between each pair of maps using the following formula:
where I and K are two mvPI maps, and v is the number of voxels in the mask.
Additionally, we plan to extend this analysis to all participants, including both older and young participants, for the results presented in Fig. 4c. However, due to the small number of remaining voxels from the intersection mask of all mvPI maps, we calculated the MSE between two mvPI maps using just the intersection mask of these two mvPI maps instead of the intersection mask of all mvPI maps.
Simulations
Many previous studies showed that physiological factors, such as cardiac cycle and respiratory cycle, can affect CBV and fMRI signals104,105,106. Extended Data Fig. 6a displays the simulation process. We assumed that the factors that affect CBV changes are mainly the cardiac phase and respiratory phase and generated CBV time series using sine function. The heart rate was set to 80 ± 10 (mean ± s.d.) times per minute, and the respiratory rate was set to 12 ± 3 times per minute. The PI and RI were both set to 0.2 (based on the results in Fig. 2). In this way, we can obtain the time series of CBV changes with the cardiac phase and respiratory phase, respectively. Then, according to the repeated acquisition time of our sequence (approximately 3.1 s), we resampled and obtained the time series of CBV changes with a length of 600 TRs. We added these two time series together and calculated the time series of the VASO signal without noise according to equation (2). We then added Gaussian noise to the time series of the VASO signal to make the tSNR of a single voxel equal to 7 (the smallest tSNR in Extended Data Fig. 6e). We set the ROI size to 5 ml (that is, 5,000 voxels, the minimum value in Extended Data Fig. 6d) and then used the proposed method to calculate the PI and RI of the generated data. Finally, we can control a single variable to generate a curve showing the effect of a single variable change on PI and RI values, shown in Fig. 3g,h.
Statistical analysis
The statistical tests in this study were performed using MATLAB and JASP software (version 0.16.4). Given the relatively small sample size of our study, we used non-parametric bootstrapping method for the hypothesis tests of cortical laminae-dependent effect and age effect. Cluster-based permutation test was used for the clustered significance of a range of cortical laminae in vmPI and RI. One-way ANOVA and two-way ANOVA were performed for laminar effect or interaction effect of laminae and age or vascular territory. Prior to conducting the ANOVA test, each dataset was evaluated for normality using the Shapiro–Wilk test and for homogeneity of variance using Levene’s test.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Data availability
The raw data of VASO, MP2RAGE, ASL and 4D-flow MRI used in this study can be obtained from OpenNeuro (https://openneuro.org/datasets/ds006212). Source data are provided with this paper.
Code availability
The custom analysis code and the plotting code developed in this study are freely available at https://github.com/FanhuaGuo/VASO-microvascular-volumetric-pulsatility.git.
References
Shi, Y., Thrippleton, M. J., Marshall, I. & Wardlaw, J. M. Intracranial pulsatility in patients with cerebral small vessel disease: a systematic review. Clin. Sci. (Lond.) 132, 157–171 (2018).
Geurts, L. J., Zwanenburg, J. J. M., Klijn, C. J. M., Luijten, P. R. & Biessels, G. J. Higher pulsatility in cerebral perforating arteries in patients with small vessel disease related stroke, a 7T MRI study. Stroke 50, 62–68 (2019).
Birnefeld, J., Wahlin, A., Eklund, A. & Malm, J. Cerebral arterial pulsatility is associated with features of small vessel disease in patients with acute stroke and TIA: a 4D flow MRI study. J. Neurol. 267, 721–730 (2020).
Shi, Y. et al. Small vessel disease is associated with altered cerebrovascular pulsatility but not resting cerebral blood flow. J. Cereb. Blood Flow Metab. 40, 85–99 (2020).
Lim, J. S., Lee, J. Y., Kwon, H. M. & Lee, Y. S. The correlation between cerebral arterial pulsatility and cognitive dysfunction in Alzheimer’s disease patients. J. Neurol. Sci. 373, 285–288 (2017).
Roher, A. E. et al. Transcranial Doppler ultrasound blood flow velocity and pulsatility index as systemic indicators for Alzheimer’s disease. Alzheimers Dement. 7, 445–455 (2011).
Rivera-Rivera, L. A. et al. Changes in intracranial venous blood flow and pulsatility in Alzheimer’s disease: a 4D flow MRI study. J. Cereb. Blood Flow Metab. 37, 2149–2158 (2017).
Chung, C. P., Lee, H. Y., Lin, P. C. & Wang, P. N. Cerebral artery pulsatility is associated with cognitive impairment and predicts dementia in individuals with subjective memory decline or mild cognitive impairment. J. Alzheimers Dis. 60, 625–632 (2017).
Iliff, J. J. et al. Cerebral arterial pulsation drives paravascular CSF–interstitial fluid exchange in the murine brain. J. Neurosci. 33, 18190–18199 (2013).
Cserr, H. F. & Ostrach, L. H. Bulk flow of interstitial fluid after intracranial injection of Blue Dextran 2000. Exp. Neurol. 45, 50–60 (1974).
Ichimura, T., Fraser, P. A. & Cserr, H. F. Distribution of extracellular tracers in perivascular spaces of the rat brain. Brain Res. 545, 103–113 (1991).
Abbott, N. J. Evidence for bulk flow of brain interstitial fluid: significance for physiology and pathology. Neurochem. Int. 45, 545–552 (2004).
Jessen, N. A., Munk, A. S., Lundgaard, I. & Nedergaard, M. The glymphatic system: a beginner’s guide. Neurochem. Res. 40, 2583–2599 (2015).
Engelhardt, B. et al. Vascular, glial, and lymphatic immune gateways of the central nervous system. Acta Neuropathol. 132, 317–338 (2016).
Louveau, A. et al. Understanding the functions and relationships of the glymphatic system and meningeal lymphatics. J. Clin. Invest. 127, 3210–3219 (2017).
Rasmussen, M. K., Mestre, H. & Nedergaard, M. The glymphatic pathway in neurological disorders. Lancet Neurol. 17, 1016–1024 (2018).
McKnight, C. D., Rouleau, R. M., Donahue, M. J. & Claassen, D. O. The regulation of cerebral spinal fluid flow and its relevance to the glymphatic system. Curr. Neurol. Neurosci. Rep. 20, 58 (2020).
Mestre, H. et al. Flow of cerebrospinal fluid is driven by arterial pulsations and is reduced in hypertension. Nat. Commun. 9, 4878 (2018).
Jammal Salameh, L., Bitzenhofer, S. H., Hanganu-Opatz, I. L., Dutschmann, M. & Egger, V. Blood pressure pulsations modulate central neuronal activity via mechanosensitive ion channels. Science 383, eadk8511 (2024).
Thompson, R. S., Trudinger, B. J. & Cook, C. M. Doppler ultrasound waveform indices: A/B ratio, pulsatility index and Pourcelot ratio. Br. J. Obstet. Gynaecol. 95, 581–588 (1988).
Wahlin, A. et al. Measuring pulsatile flow in cerebral arteries using 4D phase-contrast MR imaging. AJNR Am. J. Neuroradiol. 34, 1740–1745 (2013).
Wahlin, A. et al. Assessment of craniospinal pressure-volume indices. AJNR Am. J. Neuroradiol. 31, 1645–1650 (2010).
van den Kerkhof, M., Jansen, J. F. A., van Oostenbrugge, R. J. & Backes, W. H. 1D versus 3D blood flow velocity and pulsatility measurements of lenticulostriate arteries at 7T MRI. Magn. Reson. Imaging 96, 144–150 (2023).
Huber, L. et al. High-resolution CBV-fMRI allows mapping of laminar activity and connectivity of cortical input and output in human M1. Neuron 96, 1253–1263 (2017).
Zhao, C. et al. Whole-cerebrum distortion-free three-dimensional pseudo-continuous arterial spin labeling at 7T. Neuroimage 277, 120251 (2023).
Duvernoy, H. M., Delon, S. & Vannson, J. L. Cortical blood vessels of the human brain. Brain Res. Bull. 7, 519–579 (1981).
Akbari, A., Bollmann, S., Ali, T. S. & Barth, M. Modelling the depth-dependent VASO and BOLD responses in human primary visual cortex. Hum. Brain Mapp. 44, 710–726 (2023).
Warnert, E. A., Murphy, K., Hall, J. E. & Wise, R. G. Noninvasive assessment of arterial compliance of human cerebral arteries with short inversion time arterial spin labeling. J. Cereb. Blood Flow Metab. 35, 461–468 (2015).
Kim, D. E. et al. Mapping the supratentorial cerebral arterial territories using 1160 large artery infarcts. JAMA Neurol. 76, 72–80 (2019).
Schirmer, M. D. et al. Spatial signature of white matter hyperintensities in stroke patients. Front. Neurol. 10, 208 (2019).
Farkas, E. & Luiten, P. G. Cerebral microvascular pathology in aging and Alzheimer’s disease. Prog. Neurobiol. 64, 575–611 (2001).
Kelly, R., Hayward, C., Avolio, A. & O’Rourke, M. Noninvasive determination of age-related changes in the human arterial pulse. Circulation 80, 1652–1659 (1989).
Garrett, D. D., Lindenberger, U., Hoge, R. D. & Gauthier, C. J. Age differences in brain signal variability are robust to multiple vascular controls. Sci. Rep. 7, 10149 (2017).
Kannurpatti, S. S., Motes, M. A., Rypma, B. & Biswal, B. B. Neural and vascular variability and the fMRI-BOLD response in normal aging. Magn. Reson. Imaging 28, 466–476 (2010).
Pahlavian, S. H. et al. Cerebroarterial pulsatility and resistivity indices are associated with cognitive impairment and white matter hyperintensity in elderly subjects: a phase-contrast MRI study. J. Cereb. Blood Flow Metab. 41, 670–683 (2021).
van Hespen, K. M., Kuijf, H. J., Hendrikse, J., Luijten, P. R. & Zwanenburg, J. J. M. Blood flow velocity pulsatility and arterial diameter pulsatility measurements of the intracranial arteries using 4D PC-MRI. Neuroinformatics 20, 317–326 (2022).
van Tuijl, R. J. et al. Does the internal carotid artery attenuate blood-flow pulsatility in small vessel disease? A 7 T 4D-flow MRI study. J. Magn. Reson. Imaging 56, 527–535 (2022).
Henry-Feugeas, M. C. & Koskas, P. Cerebral vascular aging: extending the concept of pulse wave encephalopathy through capillaries to the cerebral veins. Curr. Aging Sci. 5, 157–167 (2012).
Tang, J. et al. Assessment of arterial pulsatility of cerebral perforating arteries using 7T high-resolution dual-VENC phase-contrast MRI. Magn. Reson. Med. 92, 605–617 (2024).
Li, Y. et al. Three-dimensional assessment of brain arterial compliance: technical development, comparison with aortic pulse wave velocity, and age effect. Magn. Reson. Med. 86, 1917–1928 (2021).
Huber, L. et al. Cortical lamina-dependent blood volume changes in human brain at 7 T. Neuroimage 107, 23–33 (2015).
Kennerley, A. J. et al. Early and late stimulus-evoked cortical hemodynamic responses provide insight into the neurogenic nature of neurovascular coupling. J. Cereb. Blood Flow Metab. 32, 468–480 (2012).
Tian, P. et al. Cortical depth-specific microvascular dilation underlies laminar differences in blood oxygenation level-dependent functional MRI signal. Proc. Natl Acad. Sci. USA 107, 15246–15251 (2010).
Stefanovic, B. et al. Functional reactivity of cerebral capillaries. J. Cereb. Blood Flow Metab. 28, 961–972 (2008).
Hillman, E. M. et al. Depth-resolved optical imaging and microscopy of vascular compartment dynamics during somatosensory stimulation. Neuroimage 35, 89–104 (2007).
Toubasi, A. A. et al. Watershed regions are more susceptible to tissue microstructural injury in multiple sclerosis. Brain Commun. 6, fcae299 (2024).
Purkayastha, S. et al. Impaired cerebrovascular hemodynamics are associated with cerebral white matter damage. J. Cereb. Blood Flow Metab. 34, 228–234 (2014).
Lu, H. et al. Alterations in cerebral metabolic rate and blood supply across the adult lifespan. Cereb. Cortex 21, 1426–1434 (2011).
Iliff, J. J. et al. A paravascular pathway facilitates CSF flow through the brain parenchyma and the clearance of interstitial solutes, including amyloid beta. Sci. Transl. Med. 4, 147ra111 (2012).
Chen, C. et al. MVP‐VSASL: measuring MicroVascular Pulsatility using velocity‐selective arterial spin labeling. Magn. Reson. Med. 93, 1516–1534 (2025).
Richard, K. Cardiovascular Physiology Concepts (Lippincott Williams & Wilkins, 2011).
Faraci, F. M. & Heistad, D. D. Regulation of large cerebral arteries and cerebral microvascular pressure. Circ. Res. 66, 8–17 (1990).
Davis, M. J. & Hill, M. A. Signaling mechanisms underlying the vascular myogenic response. Physiol. Rev. 79, 387–423 (1999).
Lacolley, P., Regnault, V., Nicoletti, A., Li, Z. & Michel, J. B. The vascular smooth muscle cell in arterial pathology: a cell that can take on multiple roles. Cardiovasc. Res. 95, 194–204 (2012).
Safar, M. E., Levy, B. I. & Struijker-Boudier, H. Current perspectives on arterial stiffness and pulse pressure in hypertension and cardiovascular diseases. Circulation 107, 2864–2869 (2003).
Weller, R. O., Boche, D. & Nicoll, J. A. Microvasculature changes and cerebral amyloid angiopathy in Alzheimer’s disease and their potential impact on therapy. Acta Neuropathol. 118, 87–102 (2009).
Yousif, L. F., Di Russo, J. & Sorokin, L. Laminin isoforms in endothelial and perivascular basement membranes. Cell Adh. Migr. 7, 101–110 (2013).
Iadecola, C. Neurovascular regulation in the normal brain and in Alzheimer’s disease. Nat. Rev. Neurosci. 5, 347–360 (2004).
Cipolla, M. J. The Cerebral Circulation (Morgan & Claypool Life Sciences, 2016).
Schley, D., Carare-Nnadi, R., Please, C. P., Perry, V. H. & Weller, R. O. Mechanisms to explain the reverse perivascular transport of solutes out of the brain. J. Theor. Biol. 238, 962–974 (2006).
Iliff, J. J. et al. Brain-wide pathway for waste clearance captured by contrast-enhanced MRI. J. Clin. Invest. 123, 1299–1309 (2013).
Cserr, H. F., Cooper, D. N., Suri, P. K. & Patlak, C. S. Efflux of radiolabeled polyethylene glycols and albumin from rat brain. Am. J. Physiol. 240, F319–F328 (1981).
Rennels, M. L., Gregory, T. F., Blaumanis, O. R., Fujimoto, K. & Grady, P. A. Evidence for a ‘paravascular’ fluid circulation in the mammalian central nervous system, provided by the rapid distribution of tracer protein throughout the brain from the subarachnoid space. Brain Res. 326, 47–63 (1985).
Rennels, M. L., Blaumanis, O. R. & Grady, P. A. Rapid solute transport throughout the brain via paravascular fluid pathways. Adv. Neurol. 52, 431–439 (1990).
Hajdu, M. A., McElmurry, R. T., Heistad, D. D. & Baumbach, G. L. Effects of aging on cerebral vascular responses to serotonin in rats. Am. J. Physiol. 264, H2136–H2140 (1993).
Jiang, H. X., Chen, P. C., Sobin, S. S. & Giannotta, S. L. Age related alterations in the response of the pial arterioles to adenosine in the rat. Mech. Ageing Dev. 65, 257–276 (1992).
Tarumi, T. et al. Cerebral hemodynamics in normal aging: central artery stiffness, wave reflection, and pressure pulsatility. J. Cereb. Blood Flow Metab. 34, 971–978 (2014).
Linville, D. G. & Arneric, S. P. Cortical cerebral blood flow governed by the basal forebrain: age-related impairments. Neurobiol. Aging 12, 503–510 (1991).
Lacombe, P., Sercombe, R., Vaucher, E. & Seylaz, J. Reduced cortical vasodilatory response to stimulation of the nucleus basalis of Meynert in the aged rat and evidence for a control of the cerebral circulation. Ann. N. Y. Acad. Sci. 826, 410–415 (1997).
Abernethy, W. B., Bell, M. A., Morris, M. & Moody, D. M. Microvascular density of the human paraventricular nucleus decreases with aging but not hypertension. Exp. Neurol. 121, 270–274 (1993).
Amenta, F. et al. Age-related changes in brain microanatomy: sensitivity to treatment with the dihydropyridine calcium channel blocker darodipine (PY 108-068). Brain Res. Bull. 36, 453–460 (1995).
Amenta, F. et al. Effect of long-term treatment with the dihydropyridine-type calcium channel blocker darodipine (PY 108-068) on the cerebral capillary network in aged rats. Mech. Ageing Dev. 78, 27–37 (1995).
Sonntag, W. E., Lynch, C. D., Cooney, P. T. & Hutchins, P. M. Decreases in cerebral microvasculature with age are associated with the decline in growth hormone and insulin-like growth factor 1. Endocrinology 138, 3515–3520 (1997).
de Jong, G. I., de Weerd, H., Schuurman, T., Traber, J. & Luiten, P. G. Microvascular changes in aged rat forebrain. Effects of chronic nimodipine treatment. Neurobiol. Aging 11, 381–389 (1990).
de Jong, G. I., Jansen, A. S., Horvath, E., Gispen, W. H. & Luiten, P. G. Nimodipine effects on cerebral microvessels and sciatic nerve in aging rats. Neurobiol. Aging 13, 73–81 (1992).
Luiten, P. G., de Jong, G. I. & Schuurman, T. Cerebrovascular, neuronal, and behavioral effects of long-term Ca2+ channel blockade in aging normotensive and hypertensive rat strains. Ann. N. Y. Acad. Sci. 747, 431–451 (1994).
Keuker, J. I., Luiten, P. G. & Fuchs, E. Capillary changes in hippocampal CA1 and CA3 areas of the aging rhesus monkey. Acta Neuropathol. 100, 665–672 (2000).
Sun, Z. Aging, arterial stiffness, and hypertension. Hypertension 65, 252–256 (2015).
Mitchell, G. F. et al. Changes in arterial stiffness and wave reflection with advancing age in healthy men and women: the Framingham Heart Study. Hypertension 43, 1239–1245 (2004).
Gorelick, P. B. et al. Vascular contributions to cognitive impairment and dementia: a statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 42, 2672–2713 (2011).
Prins, N. D. et al. Cerebral white matter lesions and the risk of dementia. Arch. Neurol. 61, 1531–1534 (2004).
Pantoni, L. Cerebral small vessel disease: from pathogenesis and clinical characteristics to therapeutic challenges. Lancet Neurol. 9, 689–701 (2010).
Wardlaw, J. M., Smith, C. & Dichgans, M. Small vessel disease: mechanisms and clinical implications. Lancet Neurol. 18, 684–696 (2019).
Knopman, D. S. et al. Alzheimer disease. Nat. Rev. Dis. Primers 7, 33 (2021).
Talagala, S. L., Sarlls, J. E., Liu, S. & Inati, S. J. Improvement of temporal signal-to-noise ratio of GRAPPA accelerated echo planar imaging using a FLASH based calibration scan. Magn. Reson. Med. 75, 2362–2371 (2016).
Huber, L., Uludag, K. & Moller, H. E. Non-BOLD contrast for laminar fMRI in humans: CBF, CBV, and CMRO2. Neuroimage 197, 742–760 (2019).
Stirnberg, R. & Stocker, T. Segmented K-space blipped-controlled aliasing in parallel imaging for high spatiotemporal resolution EPI. Magn. Reson. Med. 85, 1540–1551 (2021).
Zhao, C. et al. Iso-1.25mm whole-cerebrum pCASL at 7T for mapping depth-dependent cortical gray matter and tract-specific white matter cerebral blood flow. In Proc. of the International Society for Magnetic Resonance in Medicine https://archive.ismrm.org/2024/1264_4qbpVIPnW.html (2024).
Cox, R. W. AFNI: software for analysis and visualization of functional magnetic resonance neuroimages. Comput. Biomed. Res. 29, 162–173 (1996).
Dale, A. M., Fischl, B. & Sereno, M. I. Cortical surface-based analysis. I. Segmentation and surface reconstruction. Neuroimage 9, 179–194 (1999).
Avants, B. B. et al. A reproducible evaluation of ANTs similarity metric performance in brain image registration. Neuroimage 54, 2033–2044 (2011).
Friston, K. J. et al. Statistical parametric maps in functional imaging: a general linear approach. Hum. Brain Mapp. 2, 189–210 (1995).
Schrauben, E. et al. Fast 4D flow MRI intracranial segmentation and quantification in tortuous arteries. J. Magn. Reson. Imaging 42, 1458–1464 (2015).
Loecher, M., Schrauben, E., Johnson, K. M. & Wieben, O. Phase unwrapping in 4D MR flow with a 4D single-step laplacian algorithm. J. Magn. Reson. Imaging 43, 833–842 (2016).
Saad, Z. S. et al. A new method for improving functional-to-structural MRI alignment using local Pearson correlation. Neuroimage 44, 839–848 (2009).
Waehnert, M. D. et al. Anatomically motivated modeling of cortical laminae. Neuroimage 93 Pt 2, 210–220 (2014).
van den Kerkhof, M. et al. Impaired damping of cerebral blood flow velocity pulsatility is associated with the number of perivascular spaces as measured with 7T MRI. J. Cereb. Blood Flow Metab. 43, 937–946 (2023).
Lu, H., Golay, X., Pekar, J. J. & Van Zijl, P. C. Functional magnetic resonance imaging based on changes in vascular space occupancy. Magn. Reson. Med. 50, 263–274 (2003).
Grubb, R. L. Jr, Raichle, M. E., Eichling, J. O. & Ter-Pogossian, M. M. The effects of changes in PaCO2 on cerebral blood volume, blood flow, and vascular mean transit time. Stroke 5, 630–639 (1974).
Lin, A. L. et al. Evaluation of MRI models in the measurement of CMRO2 and its relationship with CBF. Magn. Reson. Med. 60, 380–389 (2008).
Liu, C. et al. Layer-dependent multiplicative effects of spatial attention on contrast responses in human early visual cortex. Prog. Neurobiol. 207, 101897 (2021).
Qureshi, S. A., Mirza, S. M. & Arif, M. Fitness function evaluation for image reconstruction using binary genetic algorithm for parallel ray transmission tomography. In 2006 International Conference on Emerging Technologies 196–201 (IEEE, 2006).
Hore, A. & Ziou, D. Image quality metrics: PSNR vs. SSIM. In 2010 20th International Conference on Pattern Recognition 2366–2369 https://doi.org/10.1109/ICPR.2010.579 (IEEE, 2010).
Karemaker, J. M. An introduction into autonomic nervous function. Physiol. Meas. 38, R89 (2017).
Glover, G. H., Li, T. Q. & Ress, D. Image-based method for retrospective correction of physiological motion effects in fMRI: RETROICOR. Magn. Reson. Med. 44, 162–167 (2000).
van der Kleij, L. A., De Vis, J. B., de Bresser, J., Hendrikse, J. & Siero, J. C. W. Arterial CO2 pressure changes during hypercapnia are associated with changes in brain parenchymal volume. Eur. Radiol. Exp. 4, 17 (2020).
Acknowledgements
We thank L. Huber at Harvard Medical School Martinos Center for sharing the VASO sequence and J. Wen at Columbia University for guiding the writing. This work was supported by National Institutes of Health grants UF1-NS100614, S10-OD025312, R01-NS114382, R01-EB032169, RF1AG084072, R01-EB028297, R01-NS134712 and R01-NS121040.
Author information
Authors and Affiliations
Contributions
F.G. and D.J.W. conceived the study. F.G. and D.J.W. designed experiments. F.G. and C.Z. executed and analyzed experiments. F.G., C.Z., Q.S. and X.S. provided support to VASO. C.Z. provided support to ASL. C.Z. and N.J. provided support to 4D-flow. F.G. and D.J.W. drafted the paper. F.G., C.Z., Q.S., K.J., X.S. and D.J.W. interpreted the results, reviewed the paper and approved the decision to submit the paper for publication.
Corresponding author
Ethics declarations
Competing interests
N.J. is an employee of Siemens Healthineers, supporting the 4D-flow in this study. The other authors declare no competing interests.
Peer review
Peer review information
Nature Cardiovascular Research thanks Leif Ostergaard, Anders Wåhlin and Richard Wise for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Extended data
Extended Data Fig. 1 Schematic diagram of segmentation, estimated cortical depth, and arterial territories atlas.
a, Left image is the anatomical image from T1w MP2RAGE sequence. Right image is the results of the segmentation and estimated cortical depth. WMd: deep white matter; WMs: superficial white matter; CSF: cerebrospinal fluid. b, Schematic diagram of arterial territories atlas from previous study30.
Extended Data Fig. 2 CBF maps show the high-resolution in cortical laminar analysis.
a, CBF map of a young participant. b, CBF map of an older participant. c. CBF map zoomed with overlay segmentation. The high image quality and spatial specificity of the CBF map allow for accurate layer-specific analysis and precise display of the choroid plexus with high CBF distribution.
Extended Data Fig. 3 Compare mvPI, CBF, CBV0, ∆VASO and ∆CBV in whole FOV between young and older groups.
Matrix of the differences in mvPI values at different depths for young (a) and older (b) participants. Each element of the matrix represents the PI value of the depth corresponding to the row minus the PI value of the depth corresponding to the column. Bonferroni correction, factor = 36; *: corrected p < 0.05; +: uncorrected p < 0.05 but corrected p > 0.05. c, Laminar profile of CBF cross young (blue) and older (red) participants. d, Laminar profile of CBV0 calculated by CBF cross young (blue) and older (red) participants. No significant differences were observed between young and older participants across all laminae. e, Laminar profile of ∆VASO cross young (blue) and older (red) participants. Bonferroni correction, factor = 9, corrected p = 0.003 in deep white matter. Significant differences were observed between young and older participants in the deep white matter, with a p-value smaller than that obtained from the mvPI results. Combined with the previous finding that no significant difference was detected in CBV0, this suggests that the difference in mvPI in the deep white matter primarily arises from variations in VASO signals caused by microvascular pulsation, rather than differences in CBF. f, Laminar profile of ∆CBV cross young (blue) and older (red) participants. Statistical significance for all panels was assessed using a two-sided bootstrap test (10,000 resamples). Young n = 11 and older n = 11 independent biological replicates, representing individual human participants, each measured once. Error bars indicate SEM across participants.
Extended Data Fig. 4 mvPI maps and the high mvPI probability density distribution map of all other participants.
a, mvPI maps of all other young participants (besides S06, S07 and S08 shown in Fig. 3a), including 3 ones with retest session (green frame). Furthermore, these three subjects demonstrated relatively high repeatability in their results, despite the long intervals between scans (5–8 months). b, mvPI maps of all elder participants. As we can see, compared to young, the mvPI maps of older participants show the higher variability across participants. c, High mvPI probability density distribution map in white matter. The regions with high mvPI frequently seems localize to watershed areas between different vascular territories in the white matter.
Extended Data Fig. 5 The results of all other participants reliability test.
a, Reliability test results of all other young participants, including 3 ones with retest session (green frame). The red line and red shading represent the mean laminar profile of ∆VASO and its 95% confidence interval, respectively, calculated from random data. The black line shows the laminar profile of the ∆VASO calculated for each participants. b, Reliability test results of all elder participants. As we can see, S15 is an outlier that cannot be distinguished from variations caused by random noise. As a result, the VASO-related group analysis in this study excluded S15 from the final results. And compared with young participants, the ∆VASO of elder were generally significantly higher than chance-level, shown in the higher reliability index. c, Laminar tSNR profile. The distribution of tSNR and chance-level are exactly inversely proportional, which illustrates the accuracy of our chance-level calculation. n = 23 (included 11 young and 12 older participants) independent biological replicates, representing individual human participants, each measured once. Error bars indicate SEM across participants.
Extended Data Fig. 6 Some parameters in our data and the simulations in white, gray matter and CSF.
a, simulation progress. Details in Method. CBV0 was set to 3%~4% to simulate the conditions in white matter (b), and 5%~6% to simulate the conditions in gray matter and CSF (c), respectively. We found that when CBV0 was high (in gray matter or CSF), the PI value was calculated very accurately, and the RI value reached a plateau more quickly. However, when CBV0 was low (in white matter), the vPI value had to be above 0.05 to be accurately calculated. And when the PI value reached 0.1, the calculated RI value could be stable and significantly greater than 1, and it was difficult to reach a plateau. The simulation results explain why we can measure high PI and RI values in the elderly, but they are difficult to detect in young people because the true PI values are smaller. The tissue volume (d) and the average tSNR (e) were shown in each vascular territory and each laminar ROI, n = 23 (included 11 young and 12 older participants). Bars represent group means and dots represent individual participants.
Extended Data Fig. 7 laminar profile of mvPI and RI in ACA, MCA, and PCA.
Laminar profiles of mvPI (left) and RI (right) in ACA (a), MCA (b), and PCA (c). The blue and red curves represent the results for younger and elder participants, respectively. The light blue shaded area indicates the white matter area, and the light green shaded area indicates the CSF area. WMd and WMs in x axis represent the deep white matter and superficial white matter. The values on the x-axis from 1 to 0 represent the gray matter from deep to superficial. The blue and red statistical values represent the differences between young and old participants compared to chance levels, while the black values indicate the direct differences between young and old participants. Statistical significance for all panels was assessed using a two-sided bootstrap test (10,000 resamples). Bonferroni factor = 9. Young n = 11 and older n = 11 independent biological replicates, representing individual human participants, each measured once. Exact p values are shown in the figure. Error bars indicate SEM across participants. *: corrected p < 0.05; **: corrected p < 0.01; ***: corrected p < 0.001. The exact corrected p-values for the comparison between young and older from deep WM to pia are: 0.195, 0.003, 0.344, 0.371, 0.046, 0.312, 0.935, 9*0.162, 9*0.252 in ACA; <0.001, 0.005, 0.072, 0.136, 0.045, 0.012, 0.015, 0.011, 0.028 in MCA; 9*0.220, 0.057, 0.023, 0.024, 0.034, 0.014, 0.028, 0.083, 0.381 in PCA.
Extended Data Fig. 8 laminar profile of mvPI using another CBV0 value (0.04) and compare the effect of hypertension in mvPI of deep WM.
a, The mvPI in deep WM of three groups were compared: healthy young, normotensive older, and hypertensive older. The p-values marked in the figure have not been corrected for multiple testing. Error bars indicate SEM across participants. b, Laminar profile of mvPI cross young (blue) and older (red) participants using CBV0 = 0.04 (same method with Fig. 4a). Compared with the results in the paper, except for the calculated mvPI values, the distribution patterns and statistical results are the same as in the paper. It shows that setting the CBV0 value to a different value will not have a significant impact on our results. Statistical significance was assessed using a two-sided bootstrap test (10,000 resamples). Young n = 11 and older n = 11 independent biological replicates, representing individual human participants, each measured once. Error bars indicate SEM across participants. Bonferroni factor = 9.
Extended Data Fig. 9 Schematic diagram of arterial pulsation and results of other ROI sites in 4D-flow scan.
a, Schematic diagram of arterial pulsation in large (MCA1, upper row) and small (MCA3, lower row) arteries. The first and second columns display magnitude images captured at the systole and the end of diastole, respectively, with the arterial boundaries delineated using blue and red lines. The third column displays zoomed-in images comparing the arterial boundaries between these two cardiac phases. b, The velocity pulsatility index (vePI) and volumetric pulsatility index (voPI) results in both age groups in all ROI sites except MCA. The top image is the results of vePI, and the bottom one is the results of voPI. Red is for older subjects and blue is for young subjects. The circles are the results for each participant, and the horizontal line is the average of this group of data. Statistical significance was assessed using a two-sided bootstrap test (10,000 resamples). Young n = 9 and older n = 12 independent biological replicates, representing individual human participants, each measured once. Exact uncorrected p values are shown in the figure. Error bars indicate SEM across participants.
Supplementary information
Source data
Source Data Fig. 1
Numerical data.
Source Data Fig. 2
Included map image (jpg or eps) and numerical data (xlsx).
Source Data Fig. 3
Included map image (jpg or eps) and numerical data (xlsx).
Source Data Fig. 4
Numerical data.
Source Data Fig. 5
Included map image (jpg or eps) and numerical data (xlsx).
Source Data Fig. 6
Numerical data.
Source Data Extended Data Fig. 1
Included map image (jpg or eps).
Source Data Extended Data Fig. 2
Included map image (jpg or eps).
Source Data Extended Data Fig. 3
Numerical data.
Source Data Extended Data Fig. 4
Included map image (jpg or eps).
Source Data Extended Data Fig. 5
Numerical data.
Source Data Extended Data Fig. 6
Numerical data.
Source Data Extended Data Fig. 7
Numerical data.
Source Data Extended Data Fig. 8
Numerical data.
Source Data Extended Data Fig. 9
Included map image (jpg or eps) and numerical data (xlsx).
Source Data Extended Data Table 1
Numerical data
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Guo, F., Zhao, C., Shou, Q. et al. Assessing cerebral microvascular volumetric with high-resolution 4D cerebral blood volume MRI at 7 T. Nat Cardiovasc Res 4, 1424–1438 (2025). https://doi.org/10.1038/s44161-025-00722-1
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s44161-025-00722-1