Abstract
Minimizing antimicrobial use is a recommended strategy to reduce the evolution and spread of antibiotic resistance; however, efficacy is elusive to measure. Wastewater-based surveillance provides a promising means to relate trends in microbial community antibiotic resistance profiles as a function of interventions and other factors. We examined influent sewage metagenomes for two neighboring wastewater treatment plants (WWTPs) serving a university and a nearby community. We compared antibiotic resistance gene (ARG) profiles as a function of diagnoses of COVID-19 and other illnesses, antibiotic use, antibiotic/antimicrobial and disinfectant/quaternary ammonium compound concentrations, and COVID-19-related behavioral shifts. Diversity and abundances of ARGs unique to the corresponding sewage were consistently higher for the community WWTP, but converged in 2022 when antibiotic prescriptions surged in the university zip code. Decreases in ARG diversity/abundance were not apparent during periods of decreased antibiotic usage, indicating that extended times may be required for wastewater ARG signals to attenuate following interventions.

Similar content being viewed by others
Introduction
Wastewater-based surveillance (WBS) and wastewater-based epidemiology (WBE) entail monitoring targets reflective of human behavior, such as illicit drugs1 and alcohol2; they have been successfully implemented as an early warning system for polio3 and were rapidly adopted throughout the world for SARS-CoV-2 monitoring. WBS differs from WBE in that it involves continuous testing of wastewater over time to benefit public health, as defined by Larsen and colleagues4, while WBE entails relating these measurements to specific human disease outcomes and corresponding interventions. Now, many WBS programs, including the US National Wastewater Surveillance System5, are looking to expand to other public health targets, including antimicrobial resistance (AMR)6. However, AMR is associated with numerous pathogens and antimicrobial resistance genes (ARGs), and thus a key first step of advancing WBS of AMR is to fill key data gaps that are missed by very limited clinical testing and characterization of strains and to characterize overall trends across microbial communities and relate their abundances to interventions and other factors7,8.
AMR limits the effectiveness of antibiotics towards bacterial pathogens and is an urgent global health threat9. Excessive use and misuse of antibiotics can contribute to AMR by exerting selection pressures that result in elevated levels of antibiotic resistant bacteria (ARB) and ARGs in the human gut, excreta, and sewage10. There have been concerted efforts both nationally and internationally to improve antibiotic stewardship, including reducing and optimizing use of antibiotics and disinfectants whenever possible11. However, it is challenging to directly measure the benefits of such efforts. WBS could be a powerful tool in taking a step towards addressing this data gap8. Examination of WBS data collected during the COVID-19 pandemic provides a dynamic scenario to relate antimicrobial use data to AMR measures in sewage. Concerns raised during this period include decreased implementation of antibiotic stewardship programs12, overprescription and misuse of antibiotics for COVID-19 patients13, and greater use of disinfectants due to increased hygiene vigilance14. If antibiotic resistant infections in patients increased, then increased release of ARB and ARGs into the sewage would be expected14,15,16,17.
At the onset of the pandemic, there was uncertainty regarding appropriate COVID-19 treatment. Antibiotics were often prescribed to prevent secondary bacterial infections that might arise from respiratory distress or other co-morbidities. For US hospitals in February-March 2020, >70% of COVID-19 patients were administered at least one antibiotic, with 81% of prescriptions commencing immediately upon admission18. Such practices occurred even though coinfection rates were lower (~3–16%) than expected19,20,21. Areas with high COVID-19 burdens especially struggled to maintain antibiotic stewardship. For example, US hospital data (n = 716 hospitals) indicated that, on average, during March–October 2020, there were greater numbers of antibiotic days of therapy (DOT) per 1000 patient days than the years preceding the pandemic for cefepime (a beta-lactam), azithromycin (a macrolide), and doxycycline (a tetracycline)18. Despite increases in inpatient antibiotic prescription rates during the early stages of the pandemic, outpatient prescription rates appear to have drastically fallen in 2020. Between 2011 and 2018, outpatient prescriptions in the US decreased by 10%; while from 2019 to 2020, there was a 25% decline, primarily attributed to decreased outpatient visits and healthcare-seeking behavior11. Between 2019 and 2020, the rates of outpatient oral antibiotic prescriptions decreased. These rates increased in 2022, returning to levels observed prior to the pandemic22,23,24. Fewer respiratory illness diagnoses in young adults during the pandemic25 might have contributed to changes in antibiotic prescriptions, for example, from 2010 to 2018, influenza associated with antibiotic prescribing (e.g., misuse) was highest in a cohort study for adults aged 18–19 (compared with adults aged 18–59)26.
Increased hygiene vigilance was initially a logical intervention to mitigate COVID-19. The US Centers for Disease Control (CDC) recommended daily surface disinfection27, using one of the EPA List N of disinfectants28. Global disinfectant and sanitizer demand increased during the pandemic and remained higher than pre-pandemic levels through March 202129. Quaternary ammonium compounds (QACs) are the most common active ingredients in these EPA-approved products. QAC biocides are frequently used in solvents, cleaning products (soap and cleaning wipes), personal care products, and biomedical materials30,31,32. The presence of a positively-charged quaternary amine group and one or two long alkyl chains within the QAC structure30 enables QACs to sorb to negatively charged solids such as sludges, sediments, and soils. Correspondingly, QACs are widely found in the environment30. During the pandemic, wet disinfecting wipes, often containing QACs33, were flushed at such quantities that blockages were reported in many sewer systems34,35.
Concerns about the unanticipated negative consequences of disinfectant overuse with respect to AMR were raised early during the COVID-19 pandemic. Chen and colleagues29 noted that the lack of diversity in disinfectant types could potentially promote bacterial resistance since bacteria were repeatedly exposed to the same biocidal agent. Increasing tolerance to QACs has been shown to correspond with increases in antibiotic resistance, though further evidence is needed to show this same correlation in the environment36. Disinfectants can promote antibiotic resistance by imposing a selective advantage for bacteria carrying ARGs and may increase the tendency for horizontal gene transfer14. In particular, some Gram-negative bacteria, such as Pseudomonas aeruginosa, exhibit natural resistance to QACs due to their intrinsic carriage of efflux pumps. Other bacteria acquire QAC resistance by either increasing expression of existing efflux pumps, acquiring efflux pumps that remove QACs, reducing membrane permeability, or increasing membrane stability37. Importantly, the QAC resistance gene, qacE, is embedded in the class 1 integron intI1, which plays a critical role in the dissemination of multi-antibiotic resistance38. Prior research suggests an increase in co-resistance (different resistance determinants on the same genetic element) and cross-resistance (one genetic determinant responsible for antibiotic and QAC resistance39) between QACs and a range of clinically important antibiotics and disinfectants. Some efflux pumps mediate cross-resistance due to their ability to export both QACs and other antimicrobial agents. For example, qacH, detected in clinical isolates on an integron on a conjugative plasmid, also encodes resistance to aminoglycosides, chloramphenicol, tetracycline, trimethoprim, beta-lactams, and sulfonamides37,40.
Previous studies have examined the impact of the COVID-19 pandemic on AMR using WBS. Using a combination of qPCR and metagenomics, Harrington and colleagues6 observed increases in ARGs associated with fluoroquinolone and beta-lactam resistance during a surge of COVID-19 infections in Las Vegas, Nevada (US) in 2020. Similarly, early in the pandemic (June–December 2020) ARGs associated with macrolide resistance, along with resistance genes qacE, tet(G), and sul1 increased in New Jersey (US)41. In Southwest England, higher loads of beta-lactam, quinolone, and macrolide antimicrobial agents and intI1 and sul1 genes were observed later in the pandemic (2021-22) via LC-MS/MS and qPCR, respectively42. The objective of the present study was to comprehensively compare antibiotic and antimicrobial use data with metagenomic profiles of ARGs carried across microbial communities in the influents of two small WWTPs serving neighboring, but distinct, communities during a period of stark changes in antibiotic/antimicrobial use circa the COVID-19 pandemic. This study examined whether two different, but interconnected, communities with separate sewersheds would have wastewater AMR signals that corresponded to differences in antibiotic consumption. One WWTP primarily served a university town (university WWTP) of 52,500, and the other WWTP served a relatively smaller community of ~21,500 (community WWTP). We hypothesized that antimicrobials, QACs, and antibiotic prescriptions would be positively associated with wastewater AMR signals and that this trend would be consistent across both WWTPs. ARG profiles were related to data available on diagnoses of COVID-19 and other illnesses, clinical antibiotic use, disinfectant/QAC use, measured antibiotics/antimicrobials in the sewage, and differences in populations served. Shotgun metagenomic sequencing was applied to comprehensively profile ARGs, mobile genetic elements (MGEs), and QAC resistance genes in the sewage. The present study expands upon previous research by including not only antimicrobials, but QACs, measured in wastewater, as well as extensive inpatient and outpatient antibiotic prescription information from the region studied, coupled with deep metagenomic sequencing. The findings help to refine approaches for WBS of AMR and shed light on how behavior surrounding antibiotic and disinfectant use can be reflected in sewage AMR measurements and, more broadly, on how the COVID-19 pandemic may have influenced community-level antibiotic resistance carriage.
Results
Comparison of COVID-19 case loads and SARS-CoV-2 signal in wastewater
A positive correlation observed between COVID-19 cases and SARS-CoV-2 measurements in sewage verified this well-established relationship43 and generally validated the sample collection and analysis workflow, while revealing differences in infection patterns between the two communities (Fig. S1). The overall number of clinical cases per 10,000 people was not different between zip codes in 2020; however, in 2021, the number of clinical diagnoses was ~2× greater in the university town than the community town (Wilcox p < 0.05). There were two spikes in COVID-19 cases in the university town that corresponded with the semester start dates.
Social distancing mandates, infection rates, and health-seeking behavior
COVID-19 intervention policies were extensive in the university town (Table S1). In March 2020, students were forbidden from returning to campus after spring break, and all classes immediately switched to virtual mode. Classes remained primarily virtual during the fall 2020 semester and were held entirely virtually after November 21, 2020. The percentage of undergraduate classes held virtually increased from 4 to 66% between the 2019–2020 and 2020–2021 academic years. Subsequently, interventions eased and virtual class delivery declined to 11% during the 2021–2022 academic year. Both towns were served by the same K-12 public school district, which implemented virtual-only classes in March 2020, followed by hybrid classes with mask requirements and a 50% reduction in in-person attendance during the 2020–2021 academic year. Full capacity in-person classes resumed with mask mandates during the 2021–2022 academic year.
Immediately following the pronouncement of the COVID-19 pandemic, in April 2020, antibiotic prescriptions associated with upper respiratory infections (URIs) drastically decreased in both communities and remained low through April 2022 (Fig. S2). The beginning of this trend coincided with precipitous reductions in outpatient visits and health-seeking behavior in the months subsequent to the COVID-19 global lockdown (Fig. S3). The years and quarters with the most patients seen were 2019 (1st quarter), 2021 (3rd and 4th quarters), and 2022 (2nd and 4th quarters). On-campus health center diagnoses from March to April 2022 indicated fewer COVID-19 diagnoses relative to the same period in 2021 (Wilcox, p < 0.001), but more viral/URI diagnoses (Wilcox, p < 0.01) (Fig. S4).
Outpatient antibiotic use
Outpatient prescriptions for 159 medications, compiled from 151 ambulatory practices, revealed greater numbers of prescriptions (normalized to the population) each year from 2017 to 2022 in the community zip code relative to the university zip code (Figs. S5A, B and S6). Prescription rates dramatically decreased in both zip codes in April 2020 relative to prior years (Figs. 1A and S7). In 2019, the university zip code reported greater total and population-normalized prescriptions than in 2020 or 2021 (Fig. S5C, D). In the community zip code, tetracycline prescription rates were higher in 2022 (Fig. S8). There was a steady increase in total outpatient prescriptions in 2021 and 2022, following a seasonal pattern of trending highest in the 4th quarter. At the university health center, raw prescription counts and appointment-normalized prescriptions for penicillins, cephalosporins, and tetracyclines (the three most commonly prescribed antibiotic classes) increased from 2021 to 2022, when the months of March–April were compared (Table S2).
A Outpatient prescription counts/1000 people for zip codes corresponding to the university and community WWTPs compiled based on prescription order date (population data from https://datacommons.org/place/). Arrows indicate a sharp decline in prescriptions at the start of the COVID-19 pandemic. MLS indicates resistance to macrolide, lincosamide, and streptogramin. B Total inpatient prescriptions (in units of days of therapy (DOT)/1000 patients) for each month shown as yearly quarters as Q1 (circles): Jan–March, Q2 (triangles): April–June, Q3 (x-boxes): July–Sept, and Q4 (x-circles): Oct-Dec. Statistical comparisons were performed using Kruskal Wallis post hoc Dunn’s test revealed differences in total inpatient prescriptions for 2017 vs 2021 (p ≤ 0.0001) and 2022 (p ≤ 0.0001), 2018 vs 2021 (p ≤ 0.0001) and 2022 (p ≤ 0.001), 2019 vs 2021 (p ≤ 0.01) and 2022 (p ≤ 0.05) and 2020 vs 2021 (p ≤ 0.01) and 2022 (p ≤ 0.05).
Inpatient antibiotic use
Monthly prescriptions for 45 antibiotics at a regional medical facility from 2017 to 2022 provided insight into trends for inpatient prescription practices that were assumed to be representative of the hospital that discharges to the university WWTP (data for this hospital were not available). In 2020, inpatient prescriptions increased in March and April, at the onset of the pandemic (689 ± 18.6 days of therapy (DOT)/1000 patient days, Fig. 1B), and were lowest in November (473 DOT/1000 patient days) (Fig. S9B). Other than the noted increases in 2020, the mean total DOT/1000 patient days for the regional facility trended downward from 2017 to 2020, with a sharp decrease in 2021 that was maintained through 2022 (Kruskal–Wallis post hoc Dunn’s test, p < 0.05) (Fig. 1B). Prescriptions for aminoglycoside, beta-lactam, carbapenem, fluoroquinolone, glycopeptide, lincosamide, and nitroimidazoles displayed decreasing trends from 2017 to 2022, while prescriptions for folate pathway inhibitors, oxazolidinones, lipopeptides, and macrolides increased (Fig. S9). Prescriptions for monobactams (aztreonam antibiotic) stood out as increasing markedly in 2020 when compared with 2018, 2021, or 2022 (Kruskal–Wallis post hoc Dunn’s test, p < 0.05), but it is noted that there were far fewer prescriptions relative to other antibiotics (maximum 3.9 DOT/1000 patient days per year). Glycopeptide DOT/1000 patient days per year were greater in 2020 than in 2021 or 2022, while carbapenem trended higher in 2020, but not significantly.
Antibiotics, antifungals, and QACs measured in the sewage
Similar total numbers of antibiotics, antifungals, and other antimicrobials were detected at both WWTPs across all sampling dates (university: 16 ± 2; community: 15 ± 2) (Fig. 2A). Notably, vancomycin (glycopeptide) levels were elevated at the university WWTP relative to the community WWTP, which is consistent with this antibiotic mainly being used in hospitals and its intravenous administration and with the university WWTP receiving hospital wastewater. Tylosin (macrolide) was not expected to be detected, given that it is not administered to humans, but it was found to be elevated at the community WWTP (Table S3, Wilcox, p < 0.05). Azithromycin, clarithromycin, oxolinic acid, sulfamethazine, and thiabendazole were greater in 2022 in the university WWTP sewage than each previous year analyzed. Imipenem, a carbapenem administered intravenously in hospital settings, was the only antibiotic with greater levels in the university wastewater in 2020 than in 2022 (Wilcox, p < 0.05) (Table S4). Elevated levels of methylparaben were detected in the university WWTP sewage in late September of 2020 (Fig. 2A). In the community wastewater, the overall levels of antibiotics and antimicrobials measured in 2020 and 2022 were statistically similar (Table S4); however, high levels of trimethoprim were observed towards the end of 2020 (mid-September to December) (Fig. 2A). In April 2022, total antibiotic levels measured at the university WWTP were about double that of levels measured at the community WWTP. Measured antibiotics were not found to be correlated with either ARGs grouped by resistance class (Fig. S10) or with outpatient prescriptions (Fig. S11). This may be due to the limited number of antibiotic samples collected, variability in sample collection type and time point, and/or degradation of antibiotics in the sewer system prior to sample collection.
A Antimicrobial compounds measured in wastewater influent by non-target UPLC/MS/MS screening. The six antibiotic/antifungal compounds with the greatest peak areas for both WWTPs across all samples were: azithromycin (MLS), ciprofloxacin (quinolone), clarithromycin (MLS), methylparaben (anti-fungal), thiabendazole (anti-fungal and anti-parasitic), and trimethoprim (diaminopyrimidine). B Concentrations of quaternary ammonium compounds (QACs) in wastewater influent. QAC abbreviations: Benzyldimethyldodecylammonium chloride (C12-BAC), benzyldimethyltetradecylammonium chloride (C14-BAC), benzyldimethylhexadecylammonium chloride (C16-ABAC), octyl decyl dimethyl ammonium chloride (C20-DDAC), dioctyl dimethyl ammonium chloride (C18-DDAC), and dodecyl dimethyl ammonium chloride (C22-DDAC).
Among the six QACs quantified in samples collected in 2020 and 2022, C14-BAC (4.5 ± 6.6 vs. 13.9 ± 13.4 µg/L) and C16-BAC (1.0 ± 1.1 vs. 3.1 ± 2.8 µg/L) were greater in the community WWTP than the university WWTP for both years (square root transformed t-test, p < 0.05) (Fig. 2B).
Comparison of sewage resistomes with time and across WWTPs
ARGs were comprehensively profiled via metagenomics to assess patterns of enrichment or attenuation associated with antibiotic/antimicrobial use patterns as they differed between the communities and in response to the COVID-19 pandemic. ARGs were normalized to the bacterial 16S rRNA housekeeping gene44, in a manner analogous to the PMMoV-normalization of SARS-CoV-2 and indicative of the relative proportion of sewage microbial communities carrying ARGs. The WWTP influent resistomes formed two distinct NMDS clusters (Fig. 3A). In 2022, however, the university WWTP resistome composition and diversity (Fig. 3B) began to more closely resemble that of the community WWTP. Alpha diversity increased in the university WWTP from 2021 to 2022 (Wilcox, Holm adjusted p = 0.003), while in the community WWTP it increased from 2018 to 2020 (p = 0.011) and decreased from 2020 to 2021 (Wilcox, Holm adjusted p = 0.042).
A Beta diversity of ARGs via NMDS (stress = 0.1432995) categorized by wastewater treatment plant (WWTP; PERMANOVA: R2 = 0.28, p value = 0.001). B ARG Shannon diversity (university WWTP versus community WWTP, Wilcox, p < 0.0001). C NMDS of Family-level bacterial taxonomy (stress = 0.1136702) categorized by WWTP (PERMANOVA: R2 = 0.31, p value = 0.001). D Family-level Shannon diversity (university WWTP vs. community WWTP, Wilcox, p < 0.0001).
The two WWTPs shared 76% (n = 1409) of the same ARGs across all sampling dates (Figs. 4 and S10). ARGs unique to each sewage source were also compared, and a greater number were consistently found across all (313 vs. 131) and shared (232 vs. 178) sampling dates at the community WWTP than the university WWTP (Fig. 4A). Unique ARGs at both plants were primarily in the beta-lactam class, while at the community WWTP they also belonged to the aminoglycoside and quinolone classes (Fig. S11). A spike in unique ARGs was apparent in October 2020 for the community WWTP. The relative abundances of total unique ARGs were higher for the community WWTP until 2022 (Wilcox p = 0.7) (Fig. 4B). Taxa at the family level showed similar trends to ARGs with distinct clustering between WWTPs (PERMANOVA, R2 = 0.31, p = 0.001) (Fig. 3C, D).
A ARGs that were unique to the university (U-) or community (C-) wastewater treatment plants (WWTPs) compared across all sampling dates from 2020 to 2022 (left), from 2022 only (center), and for the university WWTP for 2020–2021 vs 2022 (right). B Unique ARGs compared across all dates, indicated by antibiotic class. Total relative abundances were higher in the community WWTPs in 2020 and 2021 (Wilcox p < 0.0001). Samples were not collected at the university WWTP prior to October 2020. MLS indicates resistance to macrolide, lincosamide, and streptogramin.
Few classes of prescribed antibiotics significantly correlated with ARGs detected in the wastewater influent. When comparing the two WWTPs together, the mean monthly ARG/16S rRNA gene copy abundance and mean monthly outpatient prescriptions/1000 people were significantly correlated for beta-lactam (Spearman’s R = 0.65, p < 0.0001), quinolone (R = 0.74, p < 0.0001), and trimethoprim (R = 0.54, p < 0.01) antibiotic classes. However, when considering each WWTP separately, only the quinolones correlated for the community WWTP (R = 0.5, p < 0.05) and the beta-lactams for the university WWTP (R = 0.68, p < 0.05) (Fig. S12).
QAC resistance genes
qacE, qacEdelta1, qacL, and qacH were detected at both WWTPs (Fig. S13A). For the university WWTP, the sum of total QAC resistance genes peaked one month before the biggest wave of COVID-19 cases (February 2021); while at the community WWTP, these genes peaked one month after the largest wave of COVID-19 cases (January 2020) (Fig. S13B). None of the QAC resistance genes significantly correlated with any of the measured QACs, or their sum, although a negative correlation was noted with C20-DDAC and qacE (Spearman R = −0.58, p = 0.047).
Network analysis carried out on assembled contigs revealed a broad array of potential qac gene hosts, primarily in the phylum Proteobacteria (Fig. 5A, B). The most frequently detected family harboring qacL was Burkholderiaceae, a family that comprises multiple species unlikely to be derived directly from human feces. For qac genes encoded on Burkholderiaceae contigs with higher-level taxonomic annotations available, the most common genera were Acidovorax, Thaurea, and Polaromonas, which are commonly detected in wastewater and not in feces. This result is consistent with QACs being used as cleaning agents and not passing through the human gut. Nevertheless, QAC genes were co-localized in assemblies with a remarkably diverse array of ARGs encoding resistance to beta-lactams, quinolones, phenicols, rifamycins, sulfonamides, trimethoprim, and aminoglycosides (Fig. 5C, D). Of note, aminoglycoside genes were frequent cargo despite low usage of aminoglycosides (one prescription count/month for a total of three different months for the university zip code and for nine different months in the community zip code). At least one qacL context displayed a structure with similarity to Tn2145 (Fig. S14) resembling a transposon-encoded class 1 integron that encoded a quinolone pentapeptide repeat resistance protein, a putative extended spectrum beta-lactamase, an aminoglycoside resistance gene, a bicyclomycin resistance gene, and a dihydrofolate reductase-encoding gene putatively conferring resistance to folate synthesis inhibitors (e.g., trimethoprim). Despite overall structural similarity to Tn21, qacL displayed about 63% identity to qacEdelta, the QAC gene of the canonical structure.
A University wastewater treatment plant (WWTP): Bipartite graph of quaternary ammonium compound (QAC) gene hosts (at the family level) colored by phylum. Edge weights highlight normalized counts (contigs with QAC gene per sample) of gene-host predictions. B Community WWTP: Bipartite graph of QAC gene hosts (at the family level) colored by phylum. Edge weights highlight normalized counts (contigs with QAC gene per sample) of gene-host predictions. C University WWTP: Bipartite graph of co-localized ARGs detected at least once with one of the QAC genes. D Community WWTP: Bipartite graph of co-localized ARGs detected at least once with one of the QAC genes.
A number of bacterial families (e.g., Enterobacteriaceae, Pasteurellaceae, Rhodocyclaceae, Vibrionaceae, and Rhizobiaceae) previously reported to harbor QAC resistance genes were positively correlated with at least two QAC resistance genes (Table S5). The families that best correlated varied for the different QAC resistance genes and between WWTPs.
Discussion
The WBS infrastructure that rapidly proliferated across the globe for the purpose of monitoring SARS-CoV-2 now provides an opportunity to facilitate monitoring other disease agents and public health indicators3. WBS of AMR could prove to be a very powerful tool as it can provide both the vital information required to assess the status of resistance in a given community and also contribute to the broader pool of data needed to compare disparate communities and assess the efficacy of local, national, and international interventions7,8. Such interventions are detailed in corresponding action plans and typically center around means to eliminate, minimize, or otherwise optimize the use of antibiotics when necessary in order to reduce selective pressure, which favors survival and dissemination of resistant pathogens46,47,48. WBS of AMR presents distinct challenges compared to traditional focus on a single pathogen, as has been successfully done for SARS-CoV-2 or polio, because there are hundreds of bacterial pathogens and thousands of ARGs of concern49; furthermore, concerns regarding privacy have been raised50. The metagenomic-based approach applied herein presents the advantage of comprehensively assessing whether changes in selective pressure associated with interventions are resulting in measurable reduction in carriage of ARGs across human-associated microbial communities and thus overall reduction in probability of evolution of resistant strains and their circulation among human populations7,8,46. Metagenomic-based WBS of AMR further provides advantages in terms of filling key data gaps that result from the minimal collection of isolates from individual patients8. Such data are difficult to obtain due to cost, patient privacy, and lack of reporting requirements. In addition to assessing community-scale interventions of interest, like improved stewardship of antibiotics or minimizing wastewater disposal of unused meds, metagenomic monitoring of AMR as applied here could provide a screening tool for follow-up on agents of concern with more targeted culture or PCR-based methods. Furthermore, in lower resource settings, such an approach could help to narrow in on the AMR determinants of concern.
This study takes a key step towards calibrating metagenomic-based WBS of AMR by comparing sewage measurements with available clinical data. To our knowledge, no other study has compared metagenomic WBS to their community prescription data, particularly at the resolution of this study. The COVID-19 pandemic provided a unique opportunity to achieve this goal through analysis of the sewage resistomes of two neighboring small towns experiencing distinct shifts in antibiotic and antimicrobial usage before, during, and in the later stages of the COVID-19 pandemic. The confirmed relationship observed between clinical COVID-19 cases and measurements of SARS-CoV-2 in sewage validated our general sampling and monitoring approach and also revealed different patterns of illness in the adjacent communities (Fig. S1). In particular, COVID-19 cases in the university town were largely driven by cyclical migration of student populations coincident with each Spring and Fall semester.
Through examination of regional and campus prescription data, it was found that outpatient antibiotic use dropped precipitously in both communities in the early stages of the pandemic (Fig. 1). This is consistent with a previous study that noted changes in behavior, such as masking or other non-pharmaceutical interventions, led to fewer antibiotic prescriptions across the US51. In January–May 2020, US antibiotic outpatient prescriptions decreased, most likely due to fewer ambulatory visits52. Prescriptions particularly decreased for agents typically prescribed for non-COVID-19 respiratory infections (e.g., common cold, flu)53.
We observed a steady increase in outpatient antibiotic prescriptions during the autumn and early winter each year, with peak antibiotic prescription rates in 2022 being comparable to pre-pandemic levels. Data from the university health center showed an increase in URI diagnoses in 2022 (Fig. S4), but as URIs are often viral, they do not routinely prescribe antibiotics. However, regional outpatient prescriptions of antibiotics related to URIs also increased towards the end of 2022 (Fig. S2). Still, a striking finding was that outpatient prescription rates in the zip code served by the community WWTP were consistently higher than for the zip code served by the university WWTP (Figs. S5B and S6). Measurements of antibiotics in sewage indicated markedly higher levels in the community WWTP from September to December 2020, comparable levels in March 2022, and lower levels in April 2022, relative to the university WWTP (Fig. 2A). The higher levels of antibiotics measured in the university sewage in April 2022 coincided with elevated URIs diagnoses at the student medical clinic and is consistent with the assumption that university students exert a strong influence on the wastewater composition. ARG resistance classes measured in sewage were more strongly correlated with outpatient prescription data when considering both WWTPs simultaneously (Fig. S12). These differences may be due to outpatient data being fixed to the patient’s home zip codes, whereas WWTPs may serve different zip code(s) and/or receive waste from people traveling through or working in the area. Follow-up study zooming in on trends seen between clinical prescription data and wastewater ARG measurements, while expanding to examine other hypothetical factors at play, such as wastewater variables, would be of value. Additional factors that may help explain differences between the WWTP resistomes are discussed further in supplementary information, including microbiome trends and physiochemical parameters (Fig. S15–17 and Table S6). It is noted both WWTPs had similar ammonia and COD levels; however, TSS, BOD, and pH were lower in the university WWTP (Table S6) and may help explain underlying differences shaping the WWTP resistome (Fig. S15). A temporal shift, as observed in 2022 for the university resistome and microbiome (Fig. 3), however, was not seen in the physiochemical parameters (Fig. S17).
Metagenomic sequencing provided a comprehensive comparison of the compositions of the resistomes between the two communities over time (Fig. 3). Notably, the diversity of ARGs measured in the community WWTP was significantly higher. There was also a greater magnitude of ARGs unique to the community WWTP sewage, relative to ARGs unique to the university WWTP sewage (Fig. 4). These observations are consistent with the understanding that elevated antibiotic use selects for elevated ARGs in human feces, making their way into sewage. Notably, both the alpha and beta diversities of ARGs in the two sewages converged in late 2022 as pandemic-related restrictions began to lift, and the two communities likely had more overlapping interactions through work, recreation, and commerce. Late 2022 was also a time when antibiotic prescription rates peaked at the university health center, and several antibiotics and an antifungal were found to be elevated (azithromycin, clarithromycin, oxolinic acid, sulfamethazine, and thiabendazole) in the university WWTP sewage (Table S6), perhaps also as a result of behavior returning to a pre-pandemic “normal”.
Deshpande and colleagues41 found that qacE was elevated in wastewater during early stages of the pandemic, likely due to changes in behavior regarding disinfectant use. While the present study did not find similar changes in QAC resistance gene abundance, it provided new insight into the potential role of QACs in shaping sewage resistomes. Interestingly, QACs, particularly C16-BAC and C14-BAC, were consistently higher in the sewage of the community WWTP (Fig. 2B). Use of QACs has the potential to co-select for a wide variety of mobile ARGs38 and thus reducing their use may also be an important strategy for reducing antibiotic resistance levels. Indeed, here we found QAC genes within multidrug encoding MGEs, confirming the possibility of co-selection (Fig. 5). With respect to WBS, it is important to consider that any selection exerted by QACs would be expected to reflect interactions in the sewage environment itself54, since QACs are surface-applied and are not ingested. Such selection is consistent with increases in QAC genes being linked to increases in specific bacterial families known to house QAC genes (Table S7). QAC measurements were only available to compare 2020 vs. 2022, and while there was not a significant year-to-year difference, the 2020 measurements tended to have higher peak areas (Fig. 2B). It is also a possibility that residual antibiotics in sewage select for QAC genes, rather than vice versa. For example, trimethoprim ARGs were frequently co-localized with QAC genes, and trimethoprim was notably persistent in sewage. It is also noted that antibiotics vary in their stability in wastewater and thus hypothetical potential to exert selective pressure within the sewer. Nonetheless, although beta-lactams are known to be amongst the least stable antibiotic classes, their prescription rates correlated the most strongly with ARGs (Fig. S12). The comparisons made herein would be strengthened in future studies examining QAC concentrations and resistance genes with more closely aligned sampling dates for both sample types, as some generalizations had to be made here for statistical testing.
This study provides general insight into how the COVID-19 pandemic may have affected AMR in human populations and in sewage. It appeared that, despite sharp declines in antibiotic prescriptions in 2020 for both zip codes (Fig. 1), the community WWTP sewage continued to be characterized by higher diversity and relative abundance of ARGs (Figs. 3 and 4). These results suggest a number of possible explanations: (1) it may take a significant period of time for ARGs to attenuate in sewage, even with drastic reductions in prescription practices (2) while metagenomics provides a comprehensive profile of ARGs, the detection limit is high, and a more sensitive approach (e.g., qPCR) might have detected more nuanced shifts in gene abundances, (3) if there was an immediate shift due to decreased antibiotic usage in April 2020, it would have been missed in this study, as weekly wastewater sampling began in August 2020, and (4) increased QAC use amplified associated ARGs in the sewage by the time it reached the WWTP. It was further remarkable how the increase in antibiotic prescriptions and measured antibiotics in the university sewage coincided with a shift in the university sewage resistome to resemble that of the community sewage (Figs. 1 and 3). This was likely due to behavioral changes, especially given the population having a large proportion of undergraduate students; however, microbial interactions and growth that may occur throughout the sewer system can also contribute to the observed differences55. The overall observations are consistent with the notion of ARGs being “easy to get, but hard to lose.” Accordingly, it may take extended periods of time for the benefits of antibiotic stewardship practices to be realized.
While this study was able to evaluate a wide array of hypothetical factors (e.g., outpatient and inpatient prescription of antibiotics, measurements of antibiotics and QACs in wastewater, wastewater quality), it is possible that a key driver of observed ARG patterns in sewage was overlooked. Findings of this study could help guide more focused, mechanistic studies, e.g., towards characterizing microbial ecological processes altering the resistome in the human gut versus the sewer and differentiating effects of selective pressure and HGT. Assembling the metagenomic data can also bring resolution regarding which bacteria are carrying which ARGs and their responses to changes at the sewershed scale that can be examined in further studies56. Finally, we note that making clinical data, such as prescription and infection rates, more publicly available would be extremely valuable towards assessing the generalizability of the approach and findings of this study in other locales.
This study took a key step in advancing metagenomic-based WBS as a viable approach for assessing temporal trends and filling key data gaps regarding ARG carriage across human populations and evaluating efficacy of potential interventions. Metagenomic sequencing was applied to the sewage from two neighboring towns to comprehensively profile sewage resistomes during a period when major shifts in antibiotic and antimicrobial use occurred as a result of the COVID-19 pandemic. This study was unique in its application of longitudinal, deep, metagenomic sequencing paired with acquisition of antibiotic prescription data in the region and direct testing of the sewage for antibiotics and QACs. Overall, it was found that the community with higher historical rates of outpatient prescriptions also carried a higher diversity of ARGs and had a greater number of unique ARGs, even when outpatient antibiotic use dropped during the peak of the COVID-19 pandemic. QAC genes were widely networked with ARGs and MGEs across multiple bacterial hosts, demonstrating potential for elevated QAC use to elevate ARGs in the sewage. This study suggests that stewardship practices should consider both antibiotics and antimicrobials/disinfectants used for hygiene purposes and that significant periods of time might be required for ARGs to attenuate across human-associated microbial communities following the implementation of stewardship practices46.
Methods
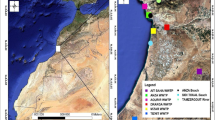
Site description and sampling
The university and community WWTPs (receiving 22,712 and 11,356 m3/day, respectively) are located <25 km apart in Southwest Virginia. The university WWTP received ~24% of its flow from the university, along with wastewater from a 146-bed hospital. Both WWTPs treat small volumes (0.4% and 0.05%, respectively) of pretreated industrial waste (from a lighting manufacturer/landfill and a vehicle parts manufacturer/household products manufacturer, respectively), and neither has combined stormwater sewers.
Starting August 28, 2020 (1 week after the semester began) through May 7, 2021 (last week of spring semester), 24-h flow proportional composite influent samples were collected from each WWTP after bar screening using an ISCO 5800 (Teledyne Inc., Louisville, KY) sampler maintained at 4 °C. Samples were collected twice weekly, such that one sample was representative of the weekend (7:00 a.m. Sunday–7:00 a.m. Monday) and one was representative of the workweek (7:00 a.m. Thursday–7:00 a.m. Friday). Grab samples from the community WWTP collected in 2017–201857, in 2019, and early 2020 (3/24/2020, 3/27/2020, 4/7/2020) were extensively described in Majeed et al.57 and are discussed herein for comparison to pre-pandemic conditions. Additional samples collected in 2022 allow for a late-pandemic comparison of both WWTPs. While previous samples were not collected in composite and were sequenced at a lower target sequencing depth, these factors are not expected to impact the major conclusions drawn in this study, as shown by Davis and colleagues58.
WWTP operational conditions (flow) and some wastewater physiochemical parameters (pH, total suspended solids (TSS), biochemical oxygen demand (BOD) were determined by the WWTP staff. Ammonia and chemical oxygen demand (COD) were measured at Virginia Tech using HACH methods 8000 and 8155 (Loveland, CO)59. TSS and volatile suspended solids (VSS) were measured according to Standard Method 254060.
Climate data were downloaded from the National Climatic Data Center’s archive61. Rainfall and daily temperature summaries were acquired from local weather stations. Mean weekly rainfall and temperature were calculated using data from the collection date and the six days prior.
SARS-CoV-2 RNA analysis
Sample concentration for RNA extraction followed previously described methods62,63. Briefly, MgCl2 was added to a 150–200 mL wastewater sample to achieve a final concentration of 25 mM, and the pH was adjusted to 3–4. After these adjustments, the samples were filtered through 0.45-µm mixed cellulose ester filters (Thermo Fisher Scientific, Waltham, MA). Filters were fragmented into 3–5-mm2 pieces using flame-sterilized tweezers and transferred into centrifuge tubes. Filters were stored at −80 °C until RNA extraction, which followed a mechanical procedure to release particles from the filters, after which a 300 µL aliquot of eluate was subjected to TRIzol/ethanol-based nucleic acid extraction64. Samples were neutralized in TRIzol/ethanol, then purified using a column-based system (Zymo Research, Irvine, CA). RNA was eluted in water and quantified via Nanodrop prior to storage at −80 °C.
SARS-CoV-2 genes (N and E) and pepper mild mottle virus (PMMoV) in RNA extracts were quantified at the Hampton Roads Sanitation District. Analysis was done using a one-step droplet digital PCR (ddPCR) multiplex protocol that included field blanks, no template controls, and synthetic SARS-CoV-2 RNA Control 4 positive standards (Twist Bioscience, San Francisco, CA), following the methods of Gonzalez et al.65.
Clinical data on COVID-19, other infections, and antibiotic use
COVID-19 clinical case data per zip code were shared by the Virginia Department of Health (VDH). Cases were documented as either the date that the case was reported to VDH, the date of illness onset, or the date that a test was conducted. Where available, symptom onset date was implemented in the analysis; otherwise, the test date followed by the date reported was used. Information regarding antibiotic use and positive COVID-19 infections was shared by the university health center. Information regarding inpatient and outpatient antibiotic prescriptions was shared by Carilion Clinic, which widely serves Southwest Virginia.
Wastewater samples were concentrated onto 0.22-µm filters for DNA extraction. Filtration was carried out until the filters clogged, and the final volume filtered was recorded (24–180 mL). DNA was extracted using the FastDNA™ SPIN Kit for Soil (MP Biomedicals, Solon, OH) following manufacturer’s instructions. DNA extracts were subjected to library preparation and sequencing at the Duke University Center for Genomic and Computational Biology using a NovaSeq 6000 (Illumina, San Diego, CA), targeting approximately 36 Gbp per sample of 2 × 150 paired-end reads.
Illumina short reads were processed together with previously sequenced samples57 (which were sequenced at a target depth of 7 Gbp per sample) using fastp to trim all adapters and filter reads. Reads that mapped to masked cow, dog, and human reference genomes were removed using bbduk66. Sequences were annotated against the Comprehensive Antibiotic Resistance Database (CARD v3.1.4; diamond blastx67: ≥80% identity and e-value < 10-10)68 and the Genome Taxonomy Database (GTDB v202 released April 27, 2021)69,70 using Kraken271. Samples were assembled using megahit v1.2.572 and open reading frames (orfs) predicted for the resulting contigs using prodigal73 -p meta. These orfs were then searched for MGEs from mobileOG-db74 v.beatrix-1.6 and ARGs from CARD v.3.1.4) using diamond (≥90% identity and e-value < 10−10). Contigs encoding QAC genes were classified according to the co-occurring mobileOGs into MGE-types. Contigs could belong to any combination of phage, plasmid, insertion sequence, integrative element, and/or conjugative element. Classifications were based on the R script https://github.com/clb21565/mobileOG-db/blob/main/scripts/getElementClassifications.R.
To identify known hosts of QAC resistance genes, the gene sequences for qacE, qacEdelta1, qacL, and qacH, as reported in CARD, were searched using BLASTN (megablast75) against the National Center for Biotechnology Information’s nucleotide collection (non-redundant protein and nucleotide sequences) database (searched on December 20th, 2022)76. Results were filtered and matches with >90% identity and 90% coverage were considered hits77, resulting in 5061, 5080, 952, and 23 total hits for qacE, qacEdelta1, qacL, and qacH, respectively (Table S7).
Antibiotics and QACs
To minimize external sources of contamination and preserve integrity for pharmaceutical and personal care product analysis, grab samples for analysis of antibiotics and antimicrobials were collected in acid-washed, methanol-rinsed glass amber bottles in 2020 (September, November, and December) and 2022 (March, April) for a total of eleven influent samples collected at each WWTP. Following solid phase extraction, ultra-performance liquid chromatography-tandem mass spectrometry (UPLC-MS/MS) was used for non-target analysis according to EPA method 169478. This method enabled screening of >140 compounds (Table S8) in a single run and semi-quantitative comparison of measurements as a function of peak area.
An additional nine influent samples were collected at both WWTPs for targeted quantification of six QACs: benzyldimethyldodecylammonium chloride (C12-BAC), benzyldimethyltetradecylammonium chloride (C14-BAC), benzyldimethylhexadecylammonium chloride (C16-ABAC), dioctyl dimethyl ammonium chloride (C18-DDAC), octyl decyl dimethyl ammonium chloride (C20-DDAC), and dodecyl dimethyl ammonium chloride (C22-DDAC) using LC/MS/MS as described in detail in the SI (Tables S9 and S10).
The study was deemed exempt by the Carilion Clinic Institutional Review Board (IRB-22-1775) as it is not categorized as human subjects research, as it included only de-identifiable prescription data.
Data analysis and statistics
All statistical tests were conducted in R (v 4.1.3)79. An α of 0.05 (p value < 0.05) was used as the level of significance, unless otherwise stated, with Bonferroni-Holm corrections for multiple comparisons. Metagenomic data were found to be non-normally distributed using the Anderson–Darling test; all other data were tested for normality using Shapiro–Wilks. Normally distributed data were compared using a t-test of log or square root transformed data. Non-normally distributed data were compared using Wilcoxon signed-rank test or Kruskal–Wallis post hoc Dunn’s test using the rstatix package80. Alpha diversity was determined using the Shannon diversity index; beta diversity was determined via Bray-Curtis dissimilarity matrices and visualized using non-metric multidimensional scaling (NMDS); significant differences between groups were calculated using Permutational Multivariate Analysis of Variance (PERMANOVA).
Spearman’s rank correlation coefficients were calculated to determine correlations between clinical cases and SARS-CoV-2 RNA, QAC resistance genes and bacterial families, antibiotic prescriptions and ARG classes, antibiotic prescriptions and antibiotic agents, and ARG classes and antibiotic agents. Multivariate regression analysis was applied to elucidate other factors hypothetically shaping the sewage resistomes further discussed in the SI. All ordination analyses were done using the R package vegan78. All figures were generated in R using ggplot279, cowplot80, and GGally81; color scales were generated using the viridis82 and pals83 packages.
Data availability
Observations and notes from this study may be found in the Supplementary File. The sequenced reads are available in the NCBI SRA repository (BioProject: PRJNA1083020). Additional data are available from the corresponding authors upon reasonable request.
References
Zuccato, E. et al. Cocaine in surface waters: a new evidence-based tool to monitor community drug abuse. Environ. Heal A Glob. Access Sci. Source 4, 14 (2005).
Thai, P. K. et al. Estimating alcohol consumption by wastewater-based epidemiology: an assessment of the correction factor for ethyl sulfate using large-scale national monitoring data. Environ. Sci. Technol. Lett. 8, 333–338 (2021).
Mao, K. et al. The potential of wastewater-based epidemiology as surveillance and early warning of infectious disease outbreaks. Curr. Opin. Environ. Sci. Heal 17, 1–7 (2020).
Larsen, D. A., Green, H., Collins, M. B. & Kmush, B. L. Wastewater monitoring, surveillance, and epidemiology: a review of terminology for a common understanding. FEMS Microbes. https://academic.oup.com/femsmicrobes/article/doi/10.1093/femsmc/xtab011/6354777. (2021).
CDC. National wastewater surveillance system. Centers for Disease Control and Prevention. https://www.cdc.gov/healthywater/surveillance/wastewater-surveillance/wastewater-surveillance.html. (2022).
Harrington, A. et al. Urban monitoring of antimicrobial resistance during a COVID-19 surge through wastewater surveillance. Sci. Total Environ. 853, 158577 (2022).
Pruden, A., Vikesland, P. J., Davis, B. C. & de Roda Husman, A. M. Seizing the moment: now is the time for integrated global surveillance of antimicrobial resistance in wastewater environments. Curr. Opin. Microbiol. 64, 91–99 (2021).
Aarestrup, F. M. & Woolhouse, M. E. J. Using sewage for surveillance of antimicrobial resistance. Science 367, 630–632 (2020).
WHO. Antimicrobial resistance. https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance (2021).
Pruden, A. Balancing water sustainability and public health goals in the face of growing concerns about antibiotic resistance. Environ. Sci. Technol. 48, 5–14 (2014).
CDC. Antibiotic use in the United States, 2021 update: progress and opportunities. US Department of Health and Human Services. https://www.cdc.gov/antibiotic-use/stewardship-report/current.html (2021).
Chibabhai, V., Duse, A. G., Perovic, O. & Richards, G. A. Collateral damage of the COVID-19 pandemic: Exacerbation of antimicrobial resistance and disruptions to antimicrobial stewardship programmes?. South Afr. Med. J. 110, 572–573 (2020).
Cong, W. et al. Antimicrobial Use in COVID-19 Patients in the First Phase of the SARS-CoV-2 Pandemic: A Scoping Review. Antibiotics. 10, 745 https://doi.org/10.3390/antibiotics10060745 (2021).
Rezasoltani, S., Yadegar, A., Hatami, B., Aghdaei, H. A. & Zali, M. R. Antimicrobial resistance as a hidden menace lurking behind the COVID-19 outbreak: the global impacts of too much hygiene on AMR. Front. Microbiol. 11, 590683 (2020).
Usman, M., Farooq, M. & Hanna, K. Environmental side effects of the injudicious use of antimicrobials in the era of COVID-19. Sci. Total Environ. 745, 141053 (2020).
Rawson, T. M., Ming, D., Ahmad, R., Moore, L. S. P. & Holmes, A. H. Antimicrobial use, drug-resistant infections and COVID-19. Nat. Rev. Microbiol. 18, 409–410 (2020).
Lu, J. & Guo, J. Disinfection spreads antimicrobial resistance. Science 371, 474 (2021).
Rose, A. N. et al. Trends in antibiotic use in United States hospitals during the coronavirus disease 2019 pandemic. Open Forum Infect. Dis. 8, ofab236 (2021).
Kubin, C. J. et al. Antimicrobial stewardship perspectives from a New York City hospital during the COVID-19 pandemic: challenges and opportunities. Am. J. Heal Pharm. 78, 743–750 (2021).
Musuuza, J. S. et al. Prevalence and outcomes of co-infection and superinfection with SARS-CoV-2 and other pathogens: a systematic review and metaanalysis. PLoS ONE 16, e0251170 (2021).
Alhumaid, S. et al. Coinfections with bacteria, fungi, and respiratory viruses in patients with sars-cov-2: a systematic review and meta-analysis. Pathogens 10, 809 (2021).
CDC. Outpatient antibiotic prescriptions — United States. https://www.cdc.gov/antibiotic-use/data/report-2019.html (2019).
CDC. Outpatient antibiotic prescriptions — United States. 2020. https://www.cdc.gov/antibiotic-use/data/report-2020.html (2020).
CDC. Outpatient antibiotic prescriptions-United States. 2022. https://www.cdc.gov/antibiotic-use/data/report-2022.html (2022).
Rodgers, L. et al. Changes in seasonal respiratory illnesses in the United States during the coronavirus disease 2019 (COVID-19) pandemic. Clin. Infect. Dis. 73, S110–S117 (2021).
Goldstein, E., Fireman, B. H., Klein, N. P., Lipsitch, M. & Ray, G. T. Antibiotic prescribing across age groups in the Kaiser Permanente Northern California population in association with different diagnoses, and with influenza incidence, 2010-2018. Epidemiol. Infect. 150, e85 (2022).
CDC. Cleaning and disinfecting your facility. Centers for Disease Control and Prevention. https://www.cdc.gov/coronavirus/2019-ncov/community/disinfecting-building-facility.html (2021).
EPA. EPA list N advanced search page: disinfectants for coronavirus (COVID-19). https://cfpub.epa.gov/wizards/disinfectants/ (2021).
Chen, B., Han, J., Dai, H. & Jia, P. Biocide-tolerance and antibiotic-resistance in community environments and risk of direct transfers to humans: unintended consequences of community-wide surface disinfecting during COVID-19?. Environ. Pollut. 283, 117074 (2021).
Pati, S. G. & Arnold, W. A. Comprehensive screening of quaternary ammonium surfactants and ionic liquids in wastewater effluents and lake sediments. Environ. Sci. Process Impacts 22, 430–441 (2020).
Schrank, C. L., Minbiole, K. P. C. & Wuest, W. M. Are quaternary ammonium compounds, the workhorse disinfectants, effective against severe acute respiratory syndrome-coronavirus-2?. ACS Infect. Dis. 6, 1553–1557 (2020).
Zheng, G., Filippelli, G. M. & Salamova, A. Increased indoor exposure to commonly used disinfectants during the COVID-19 pandemic. Environ. Sci. Technol. Lett. 7, 760–765 (2020).
Dear, K., Palmer, A. & Nixon, R. Contact allergy and allergic contact dermatitis from benzalkonium chloride in a tertiary dermatology center in Melbourne, Australia. Contact Dermatitis. 85, 146-153 https://doi.org/10.1111/cod.13826 (2021).
Alda-Vidal, C., Browne, A. L. & Hoolohan, C. Unflushables”: establishing a global agenda for action on everyday practices associated with sewer blockages, water quality, and plastic pollution. Wiley Interdiscip. Rev. Water 7, e1452 (2020).
Kaur, H. Disinfecting wipes are being flushed down toilets and causing major pipe problems. https://www.cnn.com/2020/03/20/us/wipes-flush-toilet-pipes-wellness-trnd/index.html (2020).
Boyce, J. M. Quaternary ammonium disinfectants and antiseptics: tolerance, resistance and potential impact on antibiotic resistance. Antimicrobial. Resist. Infect. Control 12, 32 (2023).
Hegstad, K. et al. Does the wide use of quaternary ammonium compounds enhance the selection and spread of antimicrobial resistance and thus threaten our health?. Micro. Drug Resist. 16, 91–104 (2010).
Gillings, M. R., Xuejun, D., Hardwick, S. A., Holley, M. P. & Stokes, H. W. Gene cassettes encoding resistance to quaternary ammonium compounds: a role in the origin of clinical class 1 integrons?. ISME J. 3, 209–215 (2009).
Baker-Austin, C., Wright, M. S., Stepanauskas, R. & McArthur, J. V. Co-selection of antibiotic and metal resistance. Trends Microbiol. 14, 176–82 (2006).
Ceccarelli, D., Salvia, A. M., Sami, J., Cappuccinelli, P. & Colombo, M. M. New cluster of plasmid-located class 1 integrons in Vibrio cholerae O1 and a dfrA15 cassette-containing integron in Vibrio parahaemolyticus isolated in Angola. Antimicrob. Agents Chemother. 50, 2493–2499 (2006).
Deshpande, A. S., Ehasz, G., Eramo, A. & Fahrenfeld, N. Changes in prevalence but not hosts of antibiotic resistance genes during the COVID-19 pandemic versus prepandemic in wastewater influent. ACS ES T Water. 3, 3626–3638 (2023).
Xu, L. et al. Antimicrobials and antimicrobial resistance genes in the shadow of COVID-19 pandemic: a wastewater-based epidemiology perspective. Water Res. 257, 121665 (2024).
Medema, G., Heijnen, L., Elsinga, G., Italiaander, R. & Brouwer, A. Presence of SARS-coronavirus-2 RNA in sewage and correlation with reported COVID-19 prevalence in the early stage of the epidemic in the Netherlands. Environ. Sci. Technol. Lett. 7, 511–516 (2020).
Li, B. et al. Metagenomic and network analysis reveal wide distribution and co-occurrence of environmental antibiotic resistance genes. ISME J. 9, 2490–2502 (2015).
Liebert, C. A., Hall, R. M. & Summers, A. O. Transposon Tn 21, flagship of the dloating genome. Microbiol. Mol. Biol. Rev. 63, 507–22 (1999).
UNEP. Bracing for Superbugs: strengthening environmental action in the One Health response to antimicrobial resistance (Newcastle University, 2023).
Federal Task Force on Combating Antibiotic-Resistant Bacteria. National Action Plan for Combating Antibiotic-Resistant Bacteria 2020–2025. U.S. Department of Health and Human Services (HHS) Office of the Assistant Secretary for Planning and Evaluation (ASPE) Office of Science and Data Policy, Washington, DC. https://aspe.hhs.gov/sites/default/files/migrated_legacy_files//196436/CARB-National-Action-Plan-2020-2025.pdf (2020).
WHO. Global Action Plan on Antimicrobial Resistance. 10, Microbe Magazine. Geneva, Switzerland: World Health Organization; 354–355 https://www.who.int/antimicrobial-resistance/publications/global-action-plan/en/ (2015).
Naghavi, M. et al. Global burden of bacterial antimicrobial resistance 1990–2021: a systematic analysis with forecasts to 2050. Lancet 404, 1199–1226 (2024).
Jacobs, D. et al. Wastewater monitoring raises privacy and ethical considerations. IEEE Trans. Technol. Soc. 2, lsaa039 (2021).
Buehrle, D. J., Wagener, M. M., Nguyen, M. H. & Clancy, C. J. Trends in outpatient antibiotic prescriptions in the United States during the COVID-19 pandemic in 2020. JAMA Netw. Open 4, e2126114 (2021).
CDC. Reduced access to care - Household pulse survey - COVID-19. https://www.cdc.gov/nchs/covid19/pulse/reduced-access-to-care.htm (2022).
King, L. M. et al. Trends in US outpatient antibiotic prescriptions during the coronavirus disease 2019 pandemic. Clin. Infect. Dis. 73, e652–e660 (2021).
McLellan, S. L. & Roguet, A. The unexpected habitat in sewer pipes for the propagation of microbial communities and their imprint on urban waters. Curr. Opinion Biotechnol. 57, 34–41 (2019).
Roguet, A., Newton, R. J., Eren, A. M. & McLellan, S. L. Guts of the urban ecosystem: microbial ecology of sewer infrastructure. mSystems 7, e0011822 (2022).
Brown, C. L. et al. Metagenomics disentangles epidemiological and microbial ecological associations between community antibiotic use and antibiotic resistance indicators measured in sewage. medRxiv. https://doi.org/10.1101/2024.12.11.24318846 (2024).
Majeed, H. J. et al. Evaluation of metagenomic-enabled antibiotic resistance surveillance at a conventional wastewater treatment plant. Front. Microbiol. 12, 1048 (2021).
Davis, B. C. Recommendations for the use of metagenomics for routine monitoring of antibiotic resistance in wastewater and impacted aquatic environments. Critical Rev. Environ. Sci. Technol. 53, 1731–1756 (2023).
Jirka, A. M. & Carter, M. J. Micro–semi-automated analysis of surface and wastewaters for chemical oxygen demand. Anal. Chem. 47, 1397–1402 (1975).
APHA-AWWA-WEF. Standard methods for the examination of water and wastewater. 23rd ed. Baird, R. & Bridgewater, L. (American Public Health Association, 2017).
Climate Data Online (CDO). https://www.ncei.noaa.gov/cdo-web/. (2022).
Ahmed, W. et al. Comparison of virus concentration methods for the RT-qPCR-based recovery of murine hepatitis virus, a surrogate for SARS-CoV-2 from untreated wastewater. Sci. Total Environ. 739, 139960 (2020).
Cohen, A. et al. Subsewershed SARS-CoV-2 wastewater surveillance and COVID-19 epidemiology using building-specific occupancy and case data. ACS EST Water 2, 2047–2059 (2022).
Ceci, A. et al. Development and implementation of a scalable and versatile test for COVID-19 diagnostics in rural communities. Nat. Commun. 12, 1–14 (2021).
Gonzalez, R., Larson, A., Thompson, H., Carter, E. & Cassi X. F. Redesigning SARS-CoV-2 clinical RT-qPCR assays for wastewater RT-ddPCR. medRxiv. https://www.medrxiv.org/content/10.1101/2021.03.02.21252754v2%0A, https://www.medrxiv.org/content/10.1101/2021.03.02.21252754v2.abstract (2022).
Clum, A. et al. DOE JGI metagenome workflow. mSystems 6, e00804–e00820 (2021).
Buchfink, B., Xie, C. & Huson, D. H. Fast and sensitive protein alignment using DIAMOND. Nat. Methods 12, 59–60 (2014).
Alcock, B. P. et al. CARD 2020: Antibiotic resistome surveillance with the comprehensive antibiotic resistance database. Nucleic Acids Res. 48, D517–D525 (2020).
Parks, D. H. et al. A complete domain-to-species taxonomy for Bacteria and Archaea. Nat. Biotechnol. 38, 1079–1086 (2020).
Parks, D. H. et al. A standardized bacterial taxonomy based on genome phylogeny substantially revises the tree of life. Nat. Biotechnol. 36, 996–1004 (2018).
Wood, D. E., Lu, J. & Langmead, B. Improved metagenomic analysis with Kraken 2. Genome Biol. 20, 257 (2019).
Li, D. et al. MEGAHIT v1.0: a fast and scalable metagenome assembler driven by advanced methodologies and community practices. Methods 102, 3–11 (2016).
Hyatt, D. et al. Prodigal: prokaryotic gene recognition and translation initiation site identification. BMC Bioinforma. 11, 119 (2010).
Brown, C. L. et al. mobileOG-db: a manually curated database of protein families mediating the life cycle of bacterial mobile genetic elements. Appl. Environ. Microbiol. 88, e0099122 (2022).
Morgulis, A. et al. Database indexing for production MegaBLAST searches. In: Bioinformatics. (2008).
Sayers, E. W. et al. Database resources of the National Center for Biotechnology Information. Nucleic Acids Res. 50, D20–D26 (2022).
Hutinel, M., Larsson, D. G. J. & Flach, C. F. Antibiotic resistance genes of emerging concern in municipal and hospital wastewater from a major Swedish city. Sci. Total Environ. 812, 151433 (2022).
EPA. Method 1694: Pharmaceuticals and personal care products in water, soil, sediment, and biosolids by HPLC/MS/MS. https://www.epa.gov/sites/default/files/2015-10/documents/method_1694_2007.pdf (2008).
R Core Team. R: a language and environment for statistical computing (R Foundation for Statistical Computing, 2021).
Kassambara, A. rstatix: Pipe-friendly framework for basic statistical tests. https://cran.r-project.org/package=rstatix (2021).
Schloerke, B. et al. Ggally: extension to ggplot2 R package version 2.1.2. https://cran.r-project.org/web/packages/GGally/index.html (2020).
Garnier, S. et al. Rvision - colorblind-friendly color maps for R. R package version 0.6.1. https://cran.r-project.org/web/packages/viridis/index.html (2021).
Wright K. pals: Color palettes, colormaps, and tools to evaluate them. R package version 1.7. https://cran.r-project.org/package=pals. (2021).
Acknowledgements
This study was initiated by an internal award from Virginia Tech and NSF CSSI Award 2004751, NSF NRT Award 2125798, and NSF PIRE Award 1545756. Additional funding was provided by CDC Award 5D30122C14707. The authors would like to extend their thanks to the WWTP operators who provided samples as well as data over the years. Additional thanks to Monica Gurung, Callen Barlik, Ana Haines, Minyoung Choi, Fadi Hindi, and James Mullet for help in the lab. Thank you to Jason Deese (VDH), Kanitta Charoensiri (VT), and Taylor Patterson (VT) for providing additional data. Thanks are extended to Virginia Tech’s Fralin Life Sciences Institute and Advanced Research Computing for computational resources and research support.
Author information
Authors and Affiliations
Contributions
A.M.M. collected and processed samples, analyzed the data, and wrote the manuscript. C.L.B. collected and processed samples, analyzed data, wrote sections of the manuscript, and edited the manuscript. M.A.R. and N.M. conducted the bioinformatics analyses with L.Z. supervising. H.M. collected and processed samples collected prior to 2019. C.V.F. and A.C. and the Molecular Diagnostics Laboratory at FBRI provided SARS-CoV-2 sample processing and data analysis, and R.G. conducted ddPCR, K.X. processed antibiotic and QAC samples. L.M., A.B.B., and J.R. provided summarized clinical data and insights into trends and results. P.J.V., A.P., and L.Z. supervised the research, analysis, writing, and editing. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Maile-Moskowitz, A., Brown, C.L., Rumi, M.A. et al. Relating antimicrobial use to wastewater resistance gene patterns via metagenomic analysis of two neighboring treatment plants circa the COVID-19 pandemic. npj Antimicrob Resist 3, 82 (2025). https://doi.org/10.1038/s44259-025-00153-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s44259-025-00153-9