Abstract
Adverse childhood experiences have been linked to psychopathology due to reduced social networks or social thinning. However, evidence of the temporal associations between adverse childhood experiences, social networks, and psychopathology was lacking, as few studies assessed social networks repeatedly. Further, their underlying neurocognitive and biological mechanisms related to hypervigilance and inflammation remain unclear. This study aimed to clarify these associations using a three-wave population-based cohort study during the COVID-19 pandemic (n = 465), where we leveraged repeated social network assessments. Self-reported questionnaires assessed adverse childhood experiences, social network size and diversity, psychological distress, and hypervigilance regarding COVID-19. Blood tests were conducted to measure inflammation markers. Individuals with more adverse childhood experiences demonstrated lesser increases in their social networks than those without adverse childhood experiences. Decreased network sizes were associated with severe psychological distress, but this association did not remain after adjusting for baseline distress. On the other hand, reduced network diversities were associated with increased psychological distress. We did not find any paths through hypervigilance regarding COVID-19 and inflammation that explain associations between adverse childhood experiences, social thinning, and psychological distress. These findings emphasize the significant social network changes in the associations between adverse childhood experiences and psychopathology.
Similar content being viewed by others
Introduction
Adverse childhood experiences (ACEs) encompass a wide array of challenging early-life experiences, ranging from child abuse, neglect, and household dysfunction1 to socio-environmental factors such as peer victimization and neighborhood dysfunction2,3. In the US, the most prevalent ACEs are economic hardship and parental divorce, which affect roughly 20% of children aged 0 to 17 years4. Approximately 50% of adults reported at least one ACE across countries such as the US5, European countries6, and Japan7. ACEs have been established as a significant contributor to various health outcomes, including depression1,8,9, with approximately 40% of cases attributed to ACEs6. Despite the consistent findings linking ACEs to later mental illness, the underlying mechanisms remain empirically unestablished.
Impaired social relationships could be a potential explanation for the associations between ACEs and psychopathology. Children who have experienced maltreatment tend to exhibit heightened mistrust of unfamiliar faces in experimental settings10, which may impede the development of healthy interpersonal bonds. In alignment with this, maltreated children reported higher levels of interpersonal relationship troubles such as peer victimization11. This social relationship problem pertains to adulthood. Associations between ACEs and smaller social networks have been demonstrated among older adults12,13. Adults with ACEs have reported lower levels of support from family and friends, which partially mediated the associations with psychopathology14. This body of literature aligns with the attachment theory15, suggesting that insecure early-life relationships with significant figures can lead to later insecure attachments, impaired social relationships, and, consequently, poor mental health16,17. The neurocognitive transactional model further supports the impacts of ACEs on social functioning from a neuroscience perspective11,18.
The neurocognitive social transactional model introduced an explanatory framework for the associations between ACEs, social relationships, and psychopathology. According to this model, individuals exposed to childhood adversities face an increased risk of stress generation—experiencing interpersonal stress throughout their lives, not just passively but also by actively initiating it19. Additionally, they experience social thinning—a reduction in the quantity and quality of social relationships from childhood to adulthood, which subsequently leads to later psychopathology19. Conceiving social functioning as a longitudinal process, which is relevant to the concept of social thinning or a reduction of social networks that can only be evaluated with multiple assessments, can provide deeper insights into the long-term impact of early childhood adversities on psychopathology by giving a potential underlying mechanism. However, previous studies have predominantly relied on a cross-sectional design and could not capture temporal dynamics20. Given that social relationships are inherently time-varying and reciprocal over time, adopting a temporal perspective is crucial to understanding the complexities of human social lives and health processes19. Therefore, there is a pressing need to examine changes in social networks in relation to ACEs. Further, recent studies reported that social thinning and mental illness were associated with higher levels of inflammation markers21,22, such as C-reactive protein (CRP), suggesting that these inflammation markers may explain the association between social thinning and psychopathology.
Social networks may be confounded by individual preferences for social integration. An individual’s social network characteristics can be influenced by their personality and innate characteristics23,24, static traits not affected by later life experiences. In response to the COVID-19 pandemic, the government issued social distancing policies to prevent infections, restricting social integration uniformly25. In the acute phase of the pandemic, social lives might be constrained for everyone, regardless of their past life experiences, due to stringent endorsement of social distancing. However, during the chronic phase, individuals gradually return to normal social lives, to which extent could vary by past experiences, such as ACEs. Thus, by using the COVID-19 pandemic as a challenge test, we aimed to capture changes in social networks and elucidate the link between ACEs and psychopathology via social thinning.
We particularly focused on social network size and diversity obtained from a self-reported questionnaire to examine social thinning. These measures asked the number of people and social roles individuals have on a daily basis. Our specific focus on these structural aspects of social networks was based on three reasons. First, maintaining social networks and having continuous relationships is more relevant to the social thinning concept hypothesized in the neurocognitive social transactional model than random interactions with strangers19. Second, structural social networks might be less influenced by reporting bias due to ACEs than social support, as ACEs would distort the perception of emotional social relationships26, while structural social networks are conceptually more objective. Third, from an interventional perspective, increasing structural social networks, i.e., sizes and diversities, is easier to implement by providing opportunities for people to gather and have activities together compared to increasing perceived social support27.
In the current study, we aimed (1) to examine the association between ACEs and social network changes, (2) to examine the association between ACEs and subsequent psychological distress, and (3) to identify the temporal association between ACEs, social network changes, and later psychological distress. We hypothesized that (1) individuals with more ACEs would demonstrate lesser increases in social networks during the chronic phase of the COVID-19 pandemic, (2) individuals with more ACEs would report more severe psychological distress, and (3) the association between ACEs and later psychological distress would be mediated by a reduction in social networks, i.e., social thinning. As a post-hoc analysis, we explored potential underlying mechanisms through neurocognitive measures and biomarkers. To achieve these objectives, we leveraged data from a prospective cohort with baseline data collected right after 1st wave of the COVID-19 outbreak and two follow-up assessments between the second and third waves and between the fifth and sixth waves.
Methods
This study analyzed data from the Utsunomiya COVID-19 seROprevalence Neighborhood Association (U-CORONA) study conducted in Utsunomiya City, Japan28. U-CORONA study was approved by the research ethics committee at Tokyo Medical and Dental University (M2019-357). The current study was not preregistered elsewhere. The custom code for the analyses is publicly available on the Zenodo29. The baseline survey took place from 14th June 2020 to 5th July 2020, immediately following the first wave of the COVID-19 outbreak in Japan and preceding the second wave. The study invited a total of 2290 participants in 1000 households, including 1973 adults aged equal to or over 18 years, selected randomly from the basic resident registry of Utsunomiya City. For the initial survey, 649 adults completed and returned the questionnaire filled at home with written informed consent. Two subsequent waves of data collection were carried out: the second wave was from 16th October 2020 to 25th October 2020, and the third wave was conducted in November 2021. While the first and second surveys were completed with a visit to the study venue (Kuramochi Clinic Interpark) to collect biological samples, the third survey consisted solely of a questionnaire-based survey via mail. Therefore, participants did not need to come to the venue. Results of physical and blood exams were returned so that participants could see doctors to follow up on any incidental findings. No urgent medical conditions were detected. For the current analysis, we included adult participants who provided questionnaire responses in both first and third waves (as ACEs were defined as adverse experiences before 18 years of age). We excluded participants lacking data on ACEs in wave 1 (a primary exposure variable), those without data on at least one measure of social network size and diversity across waves 1 to 3 (to examine changes in social networks), and those without data on psychological distress in wave 3 (a primary outcome variable). This resulted in a sample of 465 participants for analysis.
Timeline of COVID-19 waves in Japan
To contextualize the study within the COVID-19 landscape, it is crucial to understand the timing of waves of infection outbreaks in Japan. The first wave extended from 23rd March 2020 to 17th May 2020, while the second wave was from 22nd June 2020 to 6th September 2020. Subsequently, Japan experienced a series of waves: the third wave from 26th October 2020 to 28th February 2021; the fourth wave from 1st March 2021 to 20th June 2021; the fifth wave from 12th July 2021 to 26th September 2021; and the sixth wave from 20th December 2021 to 19th June 202230.
ACEs
Participants were queried about specific childhood experiences of the following items: (1) my parents had a mental illness, (2) my parents had alcohol abuse, (3) my father was violent toward my mother, (4) my parents severely beat and injured me, (5) parents did not take care of my needs, such as feeding and changing the clothes, (6) my parents said hurtful things or insults to me, (7) my parents divorced, (8) my parents died, (9) my family had financial hardship, (10) I was bullied at school, (11) an adult sexually touched me, (12) I was sick and hospitalized for an extended period, (13) I had a near-death experience in a natural disaster, such as a major earthquake or typhoon, which were the items from the Japanese ACEs scale, ACE-J7. Responses indicating “yes” were summed up to calculate the total number of ACEs experienced, subsequently categorized as “none”, “1 ACE”, or “2+ ACEs”. We censored the upper tails of ACEs given the small proportion of participants with three or more ACEs in this sample as well as in the other Japanese cohort31, which indicated that three or more ACEs might be an overreport.
Social network
Social network size was assessed by asking, “How many people do you usually meet or talk to?” Responses were recorded as specific numerical values. Social network diversity was measured by asking participants to identify the number of distinct social roles. Drawing from Cohen’s Social Network Index32, participants were asked to select from various predefined social roles. These roles included spouse, child, parent, relative, neighbor, colleague, group member (e.g., club, gym, lesson, religious organizations), friend, and other. The total number of roles ranged from 0 to 9.
Psychological distress
Psychological distress was evaluated using the Kessler Psychological Distress Scale (K6)33,34. Participants rated the frequency of experiences of negative affect on a 5-point Likert scale. The sum score was calculated by aggregating responses to six items, resulting in scores ranging from 0 to 24.
Hypervigilance score (hypervigilance regarding COVID-19)
In this study, we defined hypervigilance as a hypervigilance regarding the COVID-19 pandemic and infection, including stress associated with the COVID-19 pandemic and infection. This was assessed through a self-reported questionnaire. Participants responded to inquiries about their concerns and stress related to COVID-19, including potential infection to themselves and their friends and family members, effects on physical and mental health, stress related to staying indoors, difficulties complying with social distancing measures, and changes in family and friendship dynamics. Responses were measured on a 5-point Likert scale, and item scores were standardized and summed to generate a hypervigilance score, with higher scores indicating greater hypervigilance. The eight items used to calculate a hypervigilance score demonstrated good reliability (Cronbach’s alpha = 0.77).
Chronic inflammation markers
Based on prior research35,36, we selected several markers of chronic inflammation related to depression: CRP, neutrophil/lymphocyte ratio (NLR), monocyte/lymphocyte ratio (MLR), and systemic immune-inflammation index (SII; calculated as SII = platelets × neutrophils/lymphocytes). Blood samples were collected at the survey site, and the counts of neutrophils, lymphocytes, monocytes, and platelets were determined using an automatic hematology analyzer, Sysmex XN-1000 (Sysmex Corporation, Kobe, Japan)37. High-sensitivity CRP was measured using nephelometry on the Behring Nephelometer II analyzer (BN II; Siemens Healthcare Diagnostics, Tokyo, Japan). CRP levels less than 0.05 mg/L (a lower limit of detection) were treated as 0.05 mg/L, while values exceeding 10 mg/L were excluded from the analysis as they indicate acute inflammation, active infection, or active injury38. CRP values were log-transformed to achieve a normal distribution. Additionally, outliers were defined as values lying below the 25th percentile – 3IQR or above the 75th percentile + 3IQR for neutrophils, lymphocytes, monocytes, platelets, and log-transformed CRP and excluded from the analysis.
Covariates
Several potential confounders were considered, including participants’ age, sex, household income, household highest education, baseline psychological distress (K6), smoking status, weight, and height. These covariates were collected via self-reported questionnaires during wave 1. Sex information was obtained via a self-reported questionnaire. Although we did not explicitly ask about biological sex, we considered that sex was reported given the cultural background. Missing data in covariates (the highest missing proportion was 10.8% for household income) were imputed using multiple imputation by chained equation with R package “mice” using predictive mean matching39. With a maximum of 25 iterations, 30 imputed datasets were obtained.
Statistical methods
To investigate the associations between ACEs, social network changes, and psychological distress, mixed models were employed, accounting for the clustering structure of data. Social network size is known to follow a negative binomial distribution, and log transformation may work poorly as the distribution is overdispersed and the values could be 0. Thus, we examined the association between ACEs and social network size using negative binomial generalized linear mixed models (GLMMs). Linear mixed models (LMMs) were employed for associations with social network diversity. First, the associations between ACEs and social network changes were examined by regressing social network metrics measured at waves 1, 2, and 3 on ACE categories (none, 1, 2+) using mixed modeling with random intercepts for household and individual (individual clusters are nested in household clusters). To examine the differences in changes in social networks, ACE categories, time (a month from the baseline survey), and ACE categories × time interaction terms were included along with the below-mentioned potential confounders. The models were run separately for social network size and diversity. Second, the association between ACEs and psychological distress was examined by regressing psychological distress at wave 3 over ACE categories using LMMs with random intercepts for households. Third, the association between social network changes and psychological distress was assessed by regressing psychological distress at wave 3 over the changes in social networks using LMMs with random intercepts for households. Changes in social networks were obtained by applying negative binomial GLMMs or LMMs regressing social network size or diversity over time with the inclusion of random intercepts and random slopes and extracting coefficients of time for each individual. Therefore, social network changes are equal to individual changes in social network size or diversity by month. All the models were adjusted for age, sex, household income, and household education. The models for psychological distress were further adjusted for baseline psychological distress. In the analysis using mixed modeling, parameters were obtained from each imputed dataset and results were shown by aggregating the values across 30 imputed datasets following Rubin’s rule40. We conducted sensitivity analyses to check the robustness of findings irrespective of ACE operationalization in two ways. First, we repeated the analyses with the continuous ACE scores instead of categorized ACEs. Second, the social thinning hypothesis was tested with each subcategory of ACEs (family dysfunction, maltreatment, and other expanded items)7.
The associations between ACEs, social thinning, and psychological distress led us to conduct further post-hoc analyses. The post-hoc analyses were built upon two hypotheses: (1) bidirectional associations between ACEs, social networks, and psychological distress; and (2) the mediating role of social networks in the associations between ACEs and psychological distress via hypervigilance and inflammation.
Bidirectional associations were evaluated by using a cross-lagged panel model (CLPM) and a random-intercept cross-lagged panel model (RI-CLPM)41. Briefly, RI-CLPM better takes into consideration the influence of trait-like time-invariant constructs by decomposing between- and within-components of the variables of interests (i.e., social network size/diversity and psychological distress), while CLPM only controls for the stable nature of constructs with auto-regressive parameters. Therefore, while cross-lagged and auto-regressive associations in RI-CLPM reflect the within-individual effects, those in CLPM reflect both within- and between-individual effects, necessitating caution in the differences in interpretation. ACEs and potential confounders mentioned above were all included as time-invariant covariates. Social network size was log10-transformed after adding one to prevent zero-values when being entered into CLPM/RI-CLPM to achieve a normal distribution. We confirmed that the associations between ACEs and social network size over time were comparable between LMMs analyzing log10-transformed values and negative binomial GLMMs analyzing raw values.
The mediating role was explored with Structural Equation Models (SEM). To build the SEMs, we first obtained the multilevel partial correlations among ACEs, hypervigilance regarding COVID-19, inflammation markers, social networks, and psychological distress by calculating the correlations between residuals of the LMMs that regressed the variables of interests over age, sex, household income, and household education with random intercept. In the models for inflammation markers, smoking status and BMI (calculated with height and weight) were additionally included42. Any combinations of variables of interest (ACEs, hypervigilance regarding COVID-19, levels of inflammation markers (CRP, NLR, MLR, SII), baseline/change in social network size/diversity (obtained using negative binomial GLMMs/LMMs), and psychological distress) were tested. Further, hypothesized paths between ACEs, social networks, hypervigilance regarding COVID-19, inflammation, and psychological distress were explored with SEMs. Our examined paths were (1) ACEs → hypervigilance regarding COVID-19/CRP → social networks baseline/change → psychological distress at wave 3, and (2) ACEs → social networks baseline/change → Hypervigilance regarding COVID-19/CRP → psychological distress at wave 3. All the SEMs were fitted with maximum likelihood estimations, and missing was considered with full-information maximum likelihood estimations. Standardized coefficients were obtained. All statistical analyses were two-sided and assumed multivariate normality (the residuals were examined). The analyses were conducted using R version 4.2.343.
Reporting summary
Further information on research design is available in the Nature Portfolio Reporting Summary linked to this article.
Results
Characteristics of the analytical sample
Table 1 presents the characteristics of the analytical sample. The mean age of participants was 52.2 years (SD: 17.3), with 47.3% male and 52.7% female. Among the participants, 340 (73.1%) reported no ACEs, 80 (17.2%) reported 1 ACE, and 45 (9.7%) reported 2 or more ACEs. The prevalence of each type of ACEs is shown in Supplementary Table 1. Common ACEs were economic hardship (9.7%), parental divorce (6.2%), and peer victimization (6.2%). The distributions of social network size and diversity are shown in Supplementary Fig. 1, and the distribution of ACE scores is shown in Supplementary Fig. 2.
Social thinning hypothesis
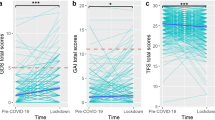
We examined the social thinning hypothesis, which hypothesized that individuals who experienced ACEs would demonstrate decreased social networks (Table 2). At baseline, there was no evidence of significant differences in social network size (1ACE: B = 0.205, 95%CI = −0.047 to 0.456, p = 0.110; 2+ ACEs: B = 0.161, 95%CI = −0.154 to 0.477, p = 0.316) and diversity (1ACE: B = 0.049, 95%CI = −0.254 to 0.352, p = 0.752; 2+ ACEs: B = 0.008, 95%CI = −0.380 to 0.396, p = 0.967) by the number of ACEs. However, over time, those without ACEs exhibited a steep increase in both social network size (B = 0.015, 95%CI = 0.007 to 0.023, p < 0.001) and diversity (B = 0.069, 95%CI = 0.058 to 0.080, p < 0.001). In contrast, individuals who experienced 2 or more adversities showed a decline in social network size (interaction term: B = −0.025, 95%CI = −0.048 to −0.002, p = 0.032) and a smaller increase in diversity (interaction term: B = −0.042, 95%CI = −0.074 to −0.010, p = 0.010) compared to those without ACEs. Figure 1 illustrates this longitudinal change in social networks. Results were comparable using continuous ACE scores and log10-transformed social network with linear mixed modeling (Supplementary Tables 2 and 3). Supplementary Table 4 shows the associations with each ACE subcategory, i.e., family dysfunction, maltreatment, and other expanded items. The result demonstrated the same patterns across subcategories, suggesting no significant differences in the associations between ACEs and changes in social networks by the types of ACEs.
Trajectories were generated using mixed models (n = 465) for (A) social network size and (B) social network diversity categorized by the number of ACEs. The axis for social network size was log10-transformed, and horizontal lines represent time from the baseline survey in months. Lines show marginal associations conditioning on age, sex, household income, and household education. Plots show individual observed values. Green lines represent the mean social network trajectories for those without ACEs, purple lines for those with 1 ACE, and yellow lines for those with 2 or more ACEs.
ACEs and psychological distress
We investigated the association between ACEs and psychological distress (Table 3). While individuals with 2 or more ACEs exhibited higher levels of psychological distress (B = 2.391, 95%CI = 0.966 to 3.815, p = 0.001), this association did not remain statistically significant after adjusting for baseline psychological distress (B = 0.877, 95%CI = −0.371 to 2.125, p = 0.168).
This lack of evidence of significant associations between ACEs and increases in psychological distress drove us to explore the possibility that the deteriorated psychological distress might be related to stress resulting from social thinning, based on the diathesis-stress model, as a secondary analysis. To test this hypothesis, moderation models were examined, including interaction terms between ACEs and the changes in social networks over time. However, the results did not support the diathesis-stress model (Table 4; 2+ ACEs × social network size change: B = −30.052, 95%CI = −118.514 to 58.409, p = 0.501; 2+ ACEs × social network diversity change: B = −11.151, 95%CI = −52.019 to 29.718, p = 0.592). We found that changes in social network diversity were associated with later psychological distress after adjusting for baseline psychological distress (B = −11.257, 95%CI = −21.600 to −0.915, p = 0.033), while no statistically significant association between changes in social network size and later psychological distress was observed (B = −3.821, 95%CI = −16.446 to 8.804, p = 0.553). After excluding ACEs from the models, the associations between changes in social networks and changes in psychological distress did not change (Table 5; social network size changes: B = −7.665, 95%CI = −19.749 to 4.419, p = 0.214; social network diversity changes: B = −11.939, 95%CI = −20.822 to −3.056, p = 0.008). To address the possibility of reverse causation, we also investigated the association between baseline psychological distress and changes in social networks (Table 6). Baseline psychological distress predicted the changes in social network size (interaction term: B = −0.002, 95%CI = −0.004 to −0.0004, p = 0.020) but not changes in social network diversity (interaction term: B = −0.002, 95%CI = −0.005 to 0.0002, p = 0.075). The results were similar using continuous ACE scores (Supplementary Tables 5 and 6). These nuanced associations led us to examine the secondary hypotheses: bidirectional associations and the mediating role.
Longitudinal associations of ACEs, social network changes, and psychological distress and their underlying mechanisms
Following the above results, the post-hoc analyses were conducted to test the following two hypotheses: 1) ACEs might lead to more psychological distress and small social networks, and through a bidirectional association between psychological distress and social networks, ending up with more severe psychological distress, and 2) ACEs could predict a decrease in social networks as well as heightened hypervigilance and inflammation, all of which might lead to later psychological distress. To confirm the first hypothesized association, a random-intercept cross-lagged panel model (RI-CLPM) and a cross-lagged panel model (CLPM) (shown in Supplementary Fig. 3) were analyzed. The fit indices are shown in Supplementary Table 7. Significant autoregressive and cross-lagged paths, as well as paths from ACEs in RI-CLPM, are depicted in Fig. 2. We found a path from social network size at wave 2 to psychological distress at wave 3 (β = 0.146, SE = 0.272, p = 0.049) and a path from psychological distress at wave 2 to social network size at wave 3 (β = −0.166, SE = 0.006, p = 0.027). Also, ACEs were associated with more psychological distress at wave 1 (β = 0.291, SE = 0.046, p < 0.001). We could not find any statistically significant cross-lagged paths in the RI-CLPM for social network diversity (Supplementary Fig. 4). ACEs were associated with more psychological distress at wave 1 (β = 0.286, SE = 0.046, p < 0.001) and less social network diversity at wave 3 (β = −0.168, SE = 0.064, p = 0.003). The results of CLPM are shown in Supplementary Fig. 5.
The arrows shown in the figure indicate the hypothesized paths between ACEs, social networks, and psychological distress. (A) Associations between ACEs, social network size, and psychological distress. (B) Associations between ACEs, social network diversity, and psychological distress. The RI-CLPM was analyzed for n = 436 participants. Thick lines show the paths with p < 0.05, thin lines show the paths with p < 0.10, and dashed lines show the paths with p > 0.10. †p < 0.10, *p < 0.05, **p < 0.001. Models were adjusted for age, sex, household income, and household education.
The second hypothesis on the mediating role of social thinning was explored with consideration of neurocognitive and biological mechanisms, i.e., hypervigilance and inflammation. As collectively represented by sickness behavior, smaller social networks, psychopathology, and inflammation can be considered as a sequential and reciprocal physical response21. Thus, inflammation was assumed to potentially mediate the associations. These higher levels of inflammatory markers, as well as alteration in brain systems due to ACEs, are also considered to lead to lasting effects on psychosocial functioning, such as heightened reactivity to social stimuli (hypervigilance)22, supporting our exploration of the mediating roles of hypervigilance and inflammation. As a preliminary post-hoc analysis, we first examined the multilevel partial correlations between ACEs, social network size and diversity, hypervigilance regarding COVID-19, inflammation markers, and psychological distress (Fig. 3). Hypervigilance regarding COVID-19 was correlated with ACEs (r = 0.103, 95%CI = 0.009 to 0.197, p = 0.033), inflammation markers (CRP: r = 0.121, 95%CI = 0.027 to 0.215, p = 0.012; NLR: r = 0.100, 95%CI = 0.006 to 0.194, p = 0.037; MLR: r = 0.099, 95%CI = 0.004 to 0.193, p = 0.040; SII: r = 0.106, 95%CI = 0.012 to 0.200, p = 0.028), baseline social network diversity (r = 0.105, 95%CI = 0.011 to 0.200, p = 0.029), change in social network size (r = −0.112, 95%CI = −0.206 to −0.018, p = 0.019), and psychological distress (baseline: r = 0.303, 95%CI = 0.212 to 0.394, p < 0.001; T3: r = 0.125, 95%CI = 0.031 to 0.218, p = 0.009). CRP was only correlated with hypervigilance regarding COVID-19 (r = 0.121, 95%CI = 0.027 to 0.215, p = 0.012) and baseline social network size (r = −0.092, 95%CI = −0.186 to 0.003, p = 0.057) except for other inflammation markers.
We further applied SEMs to explore the roles of social networks, hypervigilance regarding COVID-19, and CRP in the association between ACEs and psychological distress. The hypothesized paths and significant paths are depicted in Fig. 4. We found the potential paths from ACEs to psychological distress at T3 via change in social network and hypervigilance regarding COVID-19. ACEs were associated with a decrease in social network size (β = −0.127, SE = 0.044, p = 0.008), which in turn was associated with more hypervigilance (β = -0.103, SE = 0.052, p = 0.035), ending up with more psychological distress (β = 0.143, SE = 0.048, p = 0.002). Additionally, moderation models examining the role of hypervigilance regarding COVID-19 as an upper causal factor were explored as a follow-up analysis, hypothesizing that hypervigilance regarding COVID-19 as a personal characteristic might modify the association between ACEs and psychological distress. The results showed no statistically significant moderation effects on the association between ACEs and psychological distress or social networks (change in social network size: B = 0.078, 95%CI = −0.203 to 0.360, p = 0.585; change in social network diversity: B = 0.139, 95%CI = −0.166 to 0.443, p = 0.372; psychological distress: B = −0.079, 95%CI = −0.329 to 0.172, p = 0.540).
The hypothesized paths of (A) ACEs → hypervigilance regarding COVID-19/inflammation → baseline/changes in social networks → psychological distress and (B) ACEs → baseline/changes in social networks → hypervigilance regarding COVID-19/inflammation → psychological distress are shown. Thick lines show the paths with p < 0.05, thin lines show the paths with p < 0.10, and dashed lines show the paths with p > 0.10. †p < 0.10, *p < 0.05, **p < 0.001. Models were adjusted for age, sex, household income, and household education (n = 436 participants were included). The model for CRP was additionally adjusted for smoking and BMI. ACEs adverse childhood experiences, PD psychological distress, CRP C-reactive protein, SNS social network size, SND social network diversity.
Discussion
Our findings revealed distinct trajectories in social network size and diversity over time by the number of ACEs; individuals with two or more ACEs exhibited lesser increases in both social network size and diversity than those without ACEs, suggesting associations between more ACEs and social thinning. Furthermore, while more ACEs and decreased social networks were associated with severe psychological distress in the third wave, adjusting for baseline distress diminished these associations. Only decreases in social network diversities were associated with increased psychological distress. Associations between ACEs and psychological distress were partially explained by decreased social network size and hypervigilance regarding COVID-19. This study advanced our understanding of the associations between ACEs, social networks, and psychopathology in several important ways. First, we analyzed data from a three-wave survey of a population-based cohort to capture changes in social networks over time. This provided a more detailed view of how ACEs impact social network development. Second, our study capitalized on data collected during the COVID-19 pandemic, including a period marked by strict social distancing endorsement. This offered a unique opportunity to examine the effects of both ACEs and a shared external stressor on social networks and psychological distress and how these effects persist over time.
Our study builds upon a well-established association between ACEs and the quality and quantity of social networks. Previous studies have demonstrated the associations of retrospectively recalled childhood adversities with reduced social support14,44,45,46,47 and diminished social participation12,13,48 among adults. Our study advanced it by examining changes in social network size and diversity. During the acute phase of the COVID-19 pandemic, when strict social distancing policies were universally enforced, social interactions were constrained regardless of their ACE exposure. Interestingly, while individuals without ACEs gradually returned to their pre-pandemic levels of social interactions, those with more ACEs exhibited a significantly slower rate of increase (or even decrease) in social network size and diversity. This observation might be in line with the diathesis-stress hypothesis49,50. The traumatic nature of ACEs may have left these individuals more susceptible to fear and anxiety in the face of the COVID-19 pandemic, implied by the partial correlation between ACEs and hypervigilance regarding COVID-19. This heightened fear might have led them to continue social withdrawal even after the acute phase of the pandemic.
Our study introduced a temporal dimension to the associations between ACEs and psychopathology1,6,8,9 and between social networks and psychopathology51. Our findings demonstrated that ACEs and changes in social networks were associated with psychological distress, although the associations of only changes in social network diversity remained after adjusting for baseline distress. It is crucial to acknowledge the possible chance findings. Also, the time between baseline and follow-up surveys might be relatively short to capture changes in psychological distress. Yet, despite these nuances, our study did not pinpoint the elusive second hit in the context of the diathesis-stress model, as social network changes did not predict a significant increase in the severity of psychological distress among individuals with ACEs. This leaves room for longer follow-ups and exploring other aspects of social networks, such as social support.
We explored the paths through inflammation and hypervigilance in the association between ACEs, social network changes, and psychopathology. Associations between higher levels of inflammatory markers and psychopathology have been explained as sickness behavior, a bodily response to illness, including loss of appetite, fatigue, and social withdrawal through inflammatory signals to the brain21. Our exploration was guided by the hypothesis that ACEs impact the brain and immune system during sensitive periods, resulting in enduring effects on psychopathology22. However, our results did not support inflammation as a biological underpinning of the associations. A recent longitudinal study in young adults failed to find inflammation as a mediator while highlighting the consistent associations between ACE and depression52. Our study analyzed an older population and failed to find evidence to support inflammation as a mediator either.
We also investigated hypervigilance as a potential underlying mechanism and found no mediating and moderating roles. ACEs have been associated with heightened sensitivity to both positive and negative social stimuli in the studies of neuroscience11,18,19 as well as those of immunity or inflammation21. Hypervigilance refers to an excessive state of alertness and heightened sensitivity to potential threats or dangers in one’s environment, leading to social stress and social thinning19. We only found partial correlations between hypervigilance regarding COVID-19, psychological distress, and social networks. It is possible that our assessment of hypervigilance regarding COVID-19 did not fully capture its characteristics since it only assessed COVID-19-related situations. Therefore, the interpretation and generalization require caution.
Limitations
First, data on ACEs, social networks, and psychological distress were self-reports. This might introduce inflated correlations due to shared informants and a potential reporting bias, particularly among individuals predisposed to psychological distress. Further, individuals exposed to ACEs might report fewer social networks due to the biased perception of their social connections, given their experience of neglect and rejection. Therefore, this may lead to overestimating the associations between ACEs and reduced social networks. Note since we examined the change in social networks within individuals, this individual-level bias in assessments of social connections might be partially canceled out by a fixed effect in the analysis. Second, while our initial sample aimed to represent the population in the city, in-person participation in the first two surveys and remote questionnaire completion in the third may have introduced a sampling bias due to attrition. Our analytical sample reported lower income compared to the demographics of Utsunomiya City. Therefore, we need caution to generalize our results to the target population as well as other populations. Third, the assessment of social network size did not include concrete information on temporal reference (“usually”) and method (“meet or talk to”). Therefore, social network sizes might be differently assessed between individuals (i.e., some responded based on weekly face-to-face meetups while some included monthly virtual meetups). Given our main interest was to explore the change in social networks, which analyzed within-individual variability, our results may not be strongly affected by this between-individual variability in the interpretation of the questionnaire as this between-individual variability will be canceled out as a fixed effect. However, we should consider the potential measurement error. Moreover, we only assessed two components of social networks, i.e., size and diversity. We acknowledge that social support and casual social interactions that do not happen daily are also important social network aspects and call for future studies that examine other social networks in the associations with ACEs and psychopathology. Fourth, our models were constructed following the linearity assumption, although social networks can change in a non-linear manner (e.g., up-and-down trajectory). We used linear models as we have no strong hypothesis on the non-linearity within our short follow-up period and no motivation to capture such granular changes over time as it might reflect measurement errors rather than meaningful changes. However, we recommend other flexible models, such as the Latent Change Score Model, in future studies with a longer follow-up period.
Conclusion
Our study found that more ACEs were associated with a lesser extent of increase in social networks using repeated social network assessments as well as with psychological distress. We also found that reduced social networks were associated with psychological distress. Our findings underscore the significance of social network changes in the associations between ACEs and psychopathology and highlight the importance of repeated social network assessments. We introduced inflammation and hypervigilance as subjects for further research to extend our understanding of the long-term effects of ACEs on psychopathology. We also encourage future research that incorporates life course perspectives, follows up for longer periods, and integrates social, psychological, neurocognitive, and biological variables.
Data availability
The datasets presented in this article are not publicly available because the ethics committee did not approve data sharing. Requests to access the datasets should be directed to the corresponding author (koyama.yuna@tmd.ac.jp) and will be shared if it is aimed to interpret, replicate, and build upon the methods or findings in the article. The summary data underlying Figs. 1 and 4 and Supplementary Figs. 1 and 2 are available from https://doi.org/10.5281/zenodo.13786163.
Code availability
Custom computer codes used to generate results are publicly available from https://doi.org/10.5281/zenodo.13786163.
References
Petruccelli, K., Davis, J. & Berman, T. Adverse childhood experiences and associated health outcomes: A systematic review and meta-analysis. Child Abuse Negl 97, 104127 (2019).
Karatekin, C. & Hill, M. Expanding the Original Definition of Adverse Childhood Experiences (ACEs). J. Child Adolesc. Trauma 12, 289–306 (2019).
Kalmakis, K. A. & Chandler, G. E. Adverse childhood experiences: towards a clear conceptual meaning. J. Adv. Nurs. 70, 1489–1501 (2014).
Crouch, E., Probst, J. C., Radcliff, E., Bennett, K. J. & McKinney, S. H. Prevalence of adverse childhood experiences (ACEs) among US children. Child Abuse Negl 92, 209–218 (2019).
Giano, Z., Wheeler, D. L. & Hubach, R. D. The frequencies and disparities of adverse childhood experiences in the U.S. BMC Public Health 20, 1327 (2020).
Bellis, M. A. et al. Life course health consequences and associated annual costs of adverse childhood experiences across Europe and North America: a systematic review and meta-analysis. The Lancet. Public health 4, e517–e528 (2019).
Fujiwara, T. Impact of adverse childhood experience on physical and mental health: A life-course epidemiology perspective. Psychiatry Clin. Neurosci. 76, 544–551 (2022).
Herzog, J. I. & Schmahl, C. Adverse Childhood Experiences and the Consequences on Neurobiological, Psychosocial, and Somatic Conditions Across the Lifespan. Front. Psychiatry 9, 420 (2018).
Lipsky, R. K., McDonald, C. C., Souders, M. C., Carpio, C. C. & Teitelman, A. M. Adverse childhood experiences, the serotonergic system, and depressive and anxiety disorders in adulthood: A systematic literature review. Neurosci. Biobehav. Rev. 134, 104495 (2022).
Neil, L. et al. Trust and childhood maltreatment: evidence of bias in appraisal of unfamiliar faces. J. Child Psychol. Psychiatry 63, 655–662 (2022).
Goemans, A., Viding, E. & McCrory, E. Child Maltreatment, Peer Victimization, and Mental Health: Neurocognitive Perspectives on the Cycle of Victimization. Trauma Violence Abuse 24, 530–548 (2023).
Ashida, T., Fujiwara, T. & Kondo, K. Association between adverse childhood experiences and social integration among older people in Japan: Results from the JAGES study. Arch. Gerontol. Geriatr. 114, 105099 (2023).
Ashida, T., Fujiwara, T. & Kondo, K. Childhood socioeconomic status and social integration in later life: Results of the Japan Gerontological Evaluation Study. SSM - population health 18, 101090 (2022).
McLafferty, M., O’Neill, S., Armour, C., Murphy, S. & Bunting, B. The mediating role of various types of social networks on psychopathology following adverse childhood experiences. J. Affect. Disord. 238, 547–553 (2018).
Bowlby, J. The bowlby-ainsworth attachment theory. Behav. Brain Sci. 2, 637–638 (1979).
Briere, J., Runtz, M., Eadie, E., Bigras, N. & Godbout, N. Disengaged parenting: Structural equation modeling with child abuse, insecure attachment, and adult symptomatology. Child Abuse Negl 67, 260–270 (2017).
Sabaß, L. et al. Attachment mediates the link between childhood maltreatment and loneliness in persistent depressive disorder. J. Affect. Disord. 312, 61–68 (2022).
Miskolczi, C., Halász, J. & Mikics, É. Changes in neuroplasticity following early-life social adversities: the possible role of brain-derived neurotrophic factor. Pediatr. Res. 85, 225–233 (2019).
McCrory, E., Foulkes, L. & Viding, E. Social thinning and stress generation after childhood maltreatment: a neurocognitive social transactional model of psychiatric vulnerability. The lancet. Psychiatry 9, 828–837 (2022).
Worrell, C. Navigating a complex landscape - A review of the relationship between inflammation and childhood trauma and the potential roles in the expression of symptoms of depression. Brain, behavior, & immunity - health 20, 100418 (2022).
Tzouvara, V. et al. Adverse childhood experiences, mental health, and social functioning: A scoping review of the literature. Child Abuse Negl 139, 106092 (2023).
Eisenberger, N. I. & Moieni, M. Inflammation affects social experience: implications for mental health. World Psychiatry 19, 109–110 (2020).
Iveniuk, J. Social Networks, Role-Relationships, and Personality in Older Adulthood. J. Gerontol. B Psychol. Sci. Soc. Sci. 74, 815–826 (2019).
Rollings, J., Micheletta, J., Van Laar, D. & Waller, B. M. Personality Traits Predict Social Network Size in Older Adults. Pers. Soc. Psychol. Bull. 49, 925–938 (2023).
Sun, K. S. et al. Effectiveness of different types and levels of social distancing measures: a scoping review of global evidence from earlier stage of COVID-19 pandemic. BMJ Open 12, e053938 (2022).
Rokita, K. I., Dauvermann, M. R. & Donohoe, G. Early life experiences and social cognition in major psychiatric disorders: A systematic review. Eur. Psychiatry 53, 123–133 (2018).
Harada, K. et al. Three-year effects of neighborhood social network intervention on mental and physical health of older adults. Aging Ment. Health 25, 2235–2245 (2021).
Nawa, N. et al. Seroprevalence of SARS-CoV-2 in Utsunomiya City, Greater Tokyo, after the first pandemic in 2020. Journal of General and Family Medicine n/a, (2020).
ace-socialnetwork custom code. https://doi.org/10.5281/zenodo.13786163 (2024).
Infectious Agents Surveillance Report (IASR). (2022).
Koyama, Y. et al. Association between adverse childhood experiences and brain volumes among Japanese community-dwelling older people: Findings from the NEIGE study. Child Abuse Negl 124, 105456 (2022).
Cohen, S., Doyle, W. J., Skoner, D. P., Rabin, B. S. & Gwaltney, J. M. Social ties and susceptibility to the common cold. JAMA 277, 1940–1944 (1997).
Furukawa, T. A. et al. The performance of the Japanese version of the K6 and K10 in the World Mental Health Survey Japan. Int. J. Methods Psychiatr. Res. 17, 152–158 (2008).
Kessler, R. C. et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychol. Med. 32, 959–976 (2002).
Mazza, M. G. et al. Anxiety and depression in COVID-19 survivors: Role of inflammatory and clinical predictors. Brain Behav. Immun. 89, 594–600 (2020).
Feng, X. et al. Immune-Inflammatory Parameters in COVID-19 Cases: A Systematic Review and Meta-Analysis. Frontiers in medicine. 7, 301 (2020).
Aguadero, V., Cano-Corres, R., Berlanga, E. & Torra, M. Evaluation of biological fluid analysis using the sysmex XN automatic hematology analyzer. Cytometry B Clin. Cytom. 94, 836–844 (2018).
Pearson, T. A. et al. Markers of inflammation and cardiovascular disease: application to clinical and public health practice: A statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation 107, 499–511 (2003).
van Buuren, S. & Groothuis-Oudshoorn, K. mice: Multivariate imputation by chained equations in R. J. Stat. Softw. 1–68 (2010).
Rubin, D. B. Multiple Imputation for Nonresponse in Surveys. vol. 81 (John Wiley & Sons, 1987).
Mulder, J. D. & Hamaker, E. L. Three Extensions of the Random Intercept Cross-Lagged Panel Model. Struct. Equ. Modeling 28, 638–648 (2021).
Nedic Erjavec, G. et al. Depression: Biological markers and treatment. Prog. Neuropsychopharmacol. Biol. Psychiatry 105, 110139 (2021).
R: A language and environment for statistical computing. R Foundation for Statistical Computing. (2023).
Reed-Fitzke, K. et al. Identifying at-risk marines: A person-centered approach to adverse childhood experiences, mental health, and social support. J. Affect. Disord. 325, 721–731 (2023).
Nurius, P. S., Fleming, C. M. & Brindle, E. Life Course Pathways From Adverse Childhood Experiences to Adult Physical Health: A Structural Equation Model. J. Aging Health 31, 211–230 (2019).
Dorri, A. A., Stone, A. L., Salcido, R. Jr, Russell, S. T. & Schnarrs, P. W. Sexual and gender minority adverse childhood experiences (SGM-ACEs), perceived social support, and adult mental health. Child Abuse Negl 143, 106277 (2023).
Su, Y., Meng, X., Yang, G. & D’Arcy, C. The relationship between childhood maltreatment and mental health problems: coping strategies and social support act as mediators. BMC Psychiatry 22, 359 (2022).
Bürgin, D. et al. Adverse childhood experiences increase the risk for low perceived social participation and health-related quality of life in a large-scale population-based study in Germany. Child Abuse Negl 144, 106382 (2023).
Mosley-Johnson, E., Campbell, J. A., Garacci, E., Walker, R. J. & Egede, L. E. Stress that Endures: Influence of Adverse Childhood Experiences on Daily Life Stress and Physical Health in Adulthood. J. Affect. Disord. 284, 38–43 (2021).
Mc Elroy, S. & Hevey, D. Relationship between adverse early experiences, stressors, psychosocial resources and wellbeing. Child Abuse Negl 38, 65–75 (2014).
Wickramaratne, P. J. et al. Social connectedness as a determinant of mental health: A scoping review. PLoS One 17, e0275004 (2022).
Iob, E., Lacey, R., Giunchiglia, V. & Steptoe, A. Adverse childhood experiences and severity levels of inflammation and depression from childhood to young adulthood: a longitudinal cohort study. Mol. Psychiatry 27, 2255–2263 (2022).
Acknowledgements
We thank Euma Ishii, Yoshifumi Fukuya, Keitaro Miyamura, Yu Funakoshi, and medical students at TMDU who participated in the data collection, the medical staff in Kuramochi Clinic Interpark, and all the participants in this study. This research was supported by the Japan Agency for Medical Research and Development (AMED) under Grant Number 20he0722006. The funders had no role in study design, data collection, analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
Y.K., Y.Y., H.N., J.K., and T.F. conducted the surveys. Y.K., Y.Y., and H.N. curated the data. Y.K. conceived the research, analyzed the data, and wrote the first draft. T.F. aided the interpretation and proposed further analysis. Y.Y., H.N., J.K., and T.F. reviewed the manuscript and gave comments. All authors confirmed the finalized manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Communications psychology thanks Carl D’Arcy, Tasuku Igarashi and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Primary Handling Editors: Marike Schiffer. A peer review file is available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Koyama, Y., Yamaoka, Y., Nishimura, H. et al. More adverse childhood experiences are associated with increased social thinning and severe psychological distress. Commun Psychol 2, 94 (2024). https://doi.org/10.1038/s44271-024-00145-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s44271-024-00145-x