Abstract
Purpose
To examine potential overall survival (OS) differences between males and females with advanced gastric (GAC), gastroesophageal junction (GEJAC) and esophageal (EAC) adenocarcinoma.
Patients and methods
The study included patients from Kaiser Permanente Northern California with de novo metastatic or relapsed EAC, GEJAC and GAC. We used Cox regression modeling to examine association of sex with OS adjusting for demographics, performance status, Charlson comorbidity index, histology (Lauren’s classification), receipt of chemotherapy, and HER2 amplification or overexpression, p53, KRAS, CDKN2A, PIK3CA co-mutations and MYC amplification.
Results
Of 875 total eligible patients, 426 had GAC, of whom 224 were male and 202 were female. Among patients with GAC, males had better OS than females (HR = 0.73; [95% CI, 0.59–0.92]), and this OS difference was preserved across the molecular subgroups except mutKRAS. Intriguingly, among GAC patients with a p53 mutation, males versus females had better OS if tumor carried a non-gain-of-function mutation (non-GOF, HR = 0.59; [95% CI, 0.40–0.85]) but worse OS if tumor carried gain-of-function mutation (GOF, HR = 1.80; [95% CI, 0.83–3.99]). Sex was not associated with OS among patients with GEJAC (HR = 1.14); (95% [CI, 0.77–1.67]) or EAC (HR = 1.0; [95% CI, 0.57–1.74]). These results remained similar when separate analyses were performed among patients who received and among patients who did not receive chemotherapy.
Conclusions
Males had better OS than females among patients with advanced GAC. In addition, among GAC patients with a mutp53, sex and OS association was inversely driven by the presence of GOF versus non-GOF. Our data reveal a previously unappreciated sex disparity in survival outcomes among patients with advanced GAC. If confirmed, this finding could have important implications for clinical practice and for further understanding the biology of GAC.
Similar content being viewed by others
Introduction
Over the last four decades and across multiple countries, the incidence rates of esophageal (EAC) and gastroesophageal junction adenocarcinoma (GEJAC) have been rising while the incidence of gastric adenocarcinoma (GAC) has been falling [1,2,3,4]. Nonetheless, GAC remains the fifth most common malignancy worldwide [5,6,7]. The incidence rates of EAC and GEJAC are 5-to-9-fold higher among males than females [1, 8, 9]. While for GAC, the incidence rate in males is approximately twice that for females in most studies [5, 6, 10]. The etiology underlying these sex disparities in incidence rates is not completely understood, with some data suggesting that sex hormones and other biological factors may play important roles [3].
The mortality rates for EAC, GEJAC and GAC continue to be some of the worst among all malignancies [1]. Despite the recognized male-female difference in incidence of EAC, GEJAC and GAC, data on potential sex disparities in overall survival (OS) of these three anatomically linked malignancies remain limited. Most studies using data that included patients with all stages have shown similar mortality rates between male and female patients or that females had better OS than males [1, 11,12,13,14,15]. Few studies have assessed the potential sex disparity in OS in patients with relapsed and metastatic EAC, GEJAC and GAC independently.
The importance of the cancer risk and survival differences between male and female patients is being increasingly recognized [16, 17]. The investigation of sex-biased survival disparity could provide critical insights in improving the outcomes of both men and women with cancer [16, 17]. The aims of this study were to examine potential male-female differences in OS among patients with relapsed and metastatic GAC, EAC and GEJAC and whether sex differences in OS vary by molecular features. Since late 2017 next-generation sequencing (NGS) was routinely performed for patients with advanced malignancy within Kaiser Permanente Northern California (KPNC). The study was conducted in the cohort of patients with advanced upper gastrointestinal adenocarcinomas whose tumors underwent NGS between 2017 and 2023. We used Cox regressing modeling for analysis adjusting for six most common genomic alterations in this cohort of patients in addition to demographics, Lauren’s classification as well as other factors.
Methods
Study population
Beginning late 2017 next-generation sequencing (NGS) was routinely performed for patients with advanced malignancy within Kaiser Permanente Northern California (KPNC). This cohort included 875 eligible KPNC patients with relapsed or de novo metastatic GAC (n = 426), GEJAC (n = 276), and EAC (n = 173). We excluded patients with esophageal squamous cell carcinoma. The molecular profiling was performed using StrataNGS (Ann Arbor, Michigan) from November 2017 to December 2023. Patient data on demographics, Charlson comorbidity index (CCI), performance status (PS), histology (Lauren’s classification) and receipt of systemic therapy were obtained from the electronic medical record (Epic) and cancer registry databases. CCI was based on the 12 month-period prior to diagnosis of relapsed or de novo metastatic EAC, GEJAC and GAC. Approximately 80.1% of female and 45.2% of male stage 4 GAC patients within KPNC had NGS performed during the study period. This study was approved by the KPNC institutional review board with waiver of consent and was conducted according to International Ethical Guidelines for Biomedical Research Involving Human Subjects (CIOMS).
NGS
During the study period, StrataNGS was a 429-gene, pan-solid tumor, NGS assay for formalin-fixed paraffin-embedded (FFPE) tumor tissue, performed on co-isolated DNA and RNA [18]. For the full study cohort, alterations in more than 110 individual genes were identified. We identified the six most common genomic alterations in this study including HER2 overexpression or amplification (HER2 + ), TP53 (mutp53), CDKN2A (mutCDKN2A), KRAS (mutKRAS), PIK3CA (mutPIK3CA) mutation and MYC amplification.
HER2+ definition
HER2 overexpression or amplification was considered positive (HER2 + ) if HER2 expression was 3+ in 10% or more tumor cells by immunohistochemistry, or positive by fluorescent in situ hybridization (FISH), or positive with six copies of ERBB2 by NGS [19]. A total of 133 patients had HER2+ tumors, of these, 99 (74.4%) received trastuzumab.
Gastroesophageal junction (GEJ) definition
Tumors were classified as GEJ based on reports by gastroenterologists who performed diagnostic upper endoscopies with a tissue biopsy and was defined as the anatomic area that represents the junction between the distal esophagus and the proximal stomach (cardia) [20].
Histology
Lauren’s classification data in patients with advanced GAC were extracted from pathology reports and included diffuse type, intestinal type, mixed type and unknown.
Helicobacter Pylori and Epstein Barr Virus Tests
Among 875 patients, 265 patients (190 GAC and 75 EAC) had Helicobacter Pylori test performed, only 13 (11 GAC and 2 EAC) had a positive test. There were only 3 patients with Epstein Barr Virus (EBV) test performed and among them one had a positive test.
Chemotherapy
Chemotherapy use (yes, no) was based on whether agents were administered after the diagnosis of relapsed or de novo metastatic disease and consisted of primarily fluorouracil-based multiagent regimens with or without a checkpoint inhibitor, or with or without Trastuzumab (for HER2 positive patients).
PD-L1 expression and therapy with immune checkpoint inhibitor
There were 314 patients with PD-L1 expression test results available, among them 195 had positive PD-L1 expression and 119 patients had negative PD-L1 expression. Approximately 50% of all patients received treatment with either an immune checkpoint inhibitor (ICI) nivolumab or pembrolizumab as single agent or in combination with chemotherapy.
Definition of gain-of-function (GOF) and non-gain-of-function (non-GOF) TP53 mutation
The mutp53 GOF in our study was defined as R175H, R248Q, R248W, R249S, R273H, R273L, and R282W, all located at the DNA binding domain (DBD) and all the other p53 alterations were grouped as non-GOF, same as in our previous study [21].
Statistical analysis
OS was measured from the date of diagnosis of relapsed or metastatic EAC, GEJAC and GAC to the date of death or end of study follow-up (March 10th, 2024), whichever came first. Patients who were still alive at the end of the study period were censored at that time. Median follow-up time was 37.6 months for females and 31.4 months for males. We used Pearson’s chi squared test to assess differences in distributions of demographics and HER2 + , mutp53, mutKRAS, mutCDKN2A, mutPIK3CA and MYC amplification. We used the one-way ANOVA test to assess differences in continuous variables. We used the Kaplan-Meier estimator (log rank test) to generate unadjusted (univariate) OS curves and estimate median OS. The number of patients at risk in the Kaplan-Meier OS curves accounted for delayed entry into the cohort at the time of receipt of NGS results (i.e., left truncation, with median study entry of 0.7 months post-diagnosis) [22]. Cox proportional regression modeling was used to estimate hazard ratios (HRs) and 95% confidence intervals (CI) for the association between anatomic subgroups or sex and OS, adjusted for covariates. Time since diagnosis of advanced adenocarcinoma was the time scale used in the regression models, with allowance for delayed entry into the cohort. Covariates included in our main regression models (and unless otherwise stated) were age (continuous), sex (male, female), ethnicity (Non-Hispanic White, Black, Asian, Hispanic, other/unknown), PS (0 to 1, 2 to 4), CCI (continuous), histology (diffuse type, intestinal type, mixed type, unknown), treatment received (yes, no). We examined the effect of specific genomic alteration in a model that included all six alterations simultaneously: (HER2+ [yes, no]), mutp53 [yes, no], mutCDKN2A [yes, no], mutKRAS [yes, no], mutPIK3CA (yes, no), and MYC amplification (yes, no, unknown).
Because patients who did not receive chemotherapy had poorer OS, we performed independent analysis of both subgroups of patients who received and who did not receive chemotherapy. The statistical analysis was performed using SAS software version 9.4, R (R Core Team, 2020).
Results
Distributions of demographic and clinical characteristics among sex and anatomic subgroups
The distributions of clinical characteristics among male (n = 224) and female (n = 202) patients with GAC, the largest anatomic group (n = 426), are presented in Table 1. Male versus female GAC patients had fewer cases with diffuse type histology by Lauren’s classification and had higher CCI but were similar with respect to all other characteristics including receipt of chemotherapy and ICI as well as the distribution of the six most common genomic alterations (Table 1). For GEJAC (n = 276), male versus female patients also appeared to be older and had more patients of Asian and White decent but similar in all other characteristics (Supplementary Table 1). For EAC (n = 173), male versus female patients appeared to be older, had higher percent of Asian and Non-Hispanic White decent, higher CCI, but similar PS, receipt of chemotherapy, and percent of genomic alterations (Supplementary Table 2).
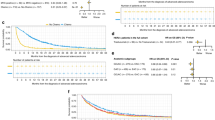
Association of sex and OS among the full cohort and anatomic subgroups
Among all GAC patients (full cohort), male versus female had better OS (hazardous ratio [HR] = 0.73, [95% confidence interval [CI], 0.59–0.92]) (Fig. 1a). The median OS was 8.9 versus 7.6 months by Kaplan-Meier curves (log-rank test, P = 0.07. Fig. 1b). The number of patients still at risk (alive) at 12 months was 69 (34.1%) for females and 83 (37.0%) for males, and the number of patients still at risk (alive) at 24 months was 27 (13.4%) for females and 43 (19.2%) for males (Fig. 1b). The results for the association of sex and OS were similar when GAC analyses were restricted to patients who received chemotherapy (HR = 0.75; [95% CI, 0.60–0.94]) and to patients who did not receive chemotherapy (HR = 0.52; [95% CI, 0.31–0.89]) (Fig. 1a). The HRs of OS between male versus female among the entire GAC cohort, the sub-cohort that received chemotherapy and the sub-cohort that did not receive chemotherapy remain significant when false discovery rate (FDR) was calculated (Fig. 1a). The median OS was 2.3 versus 1.3 months for male versus female GAC patients who did not receive chemotherapy (log-rank test, P = 0.10, Fig. 1c). In contrast, male and female patients with EAC or GEJAC had similar OS (Fig. 1a and Supplementary Figs. 1 and 2). Chemotherapy was strongly associated with better OS among both male (HR = 0.24; [95% CI, 0.16–0.38]) and female (HR = 0.18; [95% CI, 0.12–0.29]) GAC patients (Fig. 1d). Using cBioPortal (https://www.cbioportal.org/study/clinicalData?id=stad_tcga_gdc) we identified patients with stage 4 gastric adenocarcinoma in The Cancer Genome Atlas (TCGA) database. There were total of 44 patients with stage 4 gastric adenocarcinoma in this portal, among them 19 patients were females and 25 were males. The HR on OS was 0.62 (0.27–1.40) favoring male patients though the confidence interval was wide due to small sample size (Table 2).
Association of sex and OS among anatomic subgroups stratified by HER2 status
Approximately 9% of patients with GAC had HER2+ disease (Table 1). HER2+ disease was more common among patients with EAC (24.9%) or GEJAC (18.8%) (Supplemental Tables 1 and 2). Among GAC patients, males had better OS than females among both HER2+ (HR = 0.73; [95% CI, 0.58–0.92]) and HER2 negative (HR = 0.14; [95% CI, 0.02–0.93]) subgroups (Fig. 2). In contrast, there was no OS difference between male and female patients among EAC HER2 negative patients (there were only 3 EAC HER2+ female patients, sample size too small for meaningful comparison.), or among GEJAC HER2+ and HER2 negative patients (Supplementary Fig. 3).
Association of sex and OS among anatomic subgroups stratified by mutp53 status
Approximately 59% of male and 54% of female GAC patients had mutp53 (Table 1). Male versus female GAC patients with either wild-type p53 (wtp53, HR = 0.68; [95% CI, 0.47–0.98]) or mutp53 (HR = 0.78; [95% CI, 0.57–1.06]) had better OS (Fig. 3). Intriguingly, among GAC patients with mutp53 GOF, males appeared to have worse OS than females (HR, 1.80, [95% CI, 0.83–3.99]), while among GAC patients with mutp53 non-GOF, males versus females had better OS (HR = 0.59; [95% CI, 0.40–0.85]). In addition, this GOF versus non-GOF difference was confirmed with interaction analysis that shows significant statistical difference HR for interaction term = 2.54, [95% CI, 1.25–5.16] (Fig. 3). Nearly 90% of patients with EAC had mutp53 (Supplementary Table 1). Male versus female EAC patients with mutp53 had no OS difference (Supplementary Fig. 4). Approximately 79% of male and 68% of female patients with GEJAC had mutp53 (Supplementary Table 2), male versus female GEJAC patients with mutp53 also had no OS difference (Supplementary Fig. 4).
Association of sex and OS among anatomic subgroups stratified by mutKRAS status
Male versus female GAC patients with wild-type KRAS (wtKRAS) had substantially better OS (HR = 0.69, [95% CI, 0.54–0.88]), while male versus female GAC patients with mutKRAS had no OS difference (HR = 1.00, [95% CI, 0.40–2.22]) (Fig. 4a). Male versus female EAC and GEJAC patients with wtKRAS had no OS difference (Supplementary Fig. 5). Male versus female GEJAC patients with mutKRAS appeared to have worse OS but with wide confidence interval (CI) due to small sample size (HR = 2.04, [95% CI, 0.74–5.66]) (Supplementary Fig. 5).
Association of sex and OS among anatomic subgroups stratified by mutCDKN2A status
Male versus female GAC patients with either wild-type CDKN2A (wtCDKN2A) (HR = 0.75; [95% CI, 0.59–0.96]) or mutCDKN2A (HR = 0.67, [95% CI, 0.37–1.20]) had better OS (Fig. 4b). Male versus female EAC patients with wtCDKN2A had no OS difference (Supplementary Fig. 6). Male versus female GEJAC patients with wtCDKN2A or mutCDKN2A had no OS differences (Supplementary Fig. 6).
Association of sex and OS among anatomic subgroups stratified by mutPIK3CA status
Male versus female GAC patients with wild-type PIK3CA (wtPIK3CA) had better OS (HR = 0.69; [95% CI, 0.54–0.88]), while male versus female GAC patients with mutPIK3CA had no OS difference (Fig. 4c). Male versus female EAC or GEJAC patients with wtPIK3CA had no OS difference (Supplementary Fig. 7).
Association of sex and OS among anatomic subgroups stratified by MYC amplification status
Males had better OS than females among GAC patients with MYC amplification negative (HR = 0.72; [95% CI, 0.59–0.91]) (Fig. 5a). The sample size for the GAC patients with MYC amplification positive was too small (n = 12 for males and 11 for females) for meaningful analysis. Male versus female EAC or GEJAC patients with MYC amplification negative had no OS difference (Supplementary Fig. 8). There were too few female EAC or GEJAC patients with MYC amplification positive to allow meaningful comparison with male patients.
OS of male versus female GAC patients who did not receive chemotherapy by molecular subgroups
We performed an independent analysis of GAC patients who did not receive chemotherapy. The OS of male versus female GAC patients who did not receive chemotherapy was better across the molecular subgroups except that of mutKRAS (Fig. 5b), which is similar to the results with the full cohort.
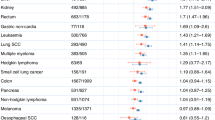
Summary of data
Fig. 5c summarizes the data. Males had better OS than females among patients with GAC but not among patients with EAC or GEJAC. Among GAC patients, male versus female had better OS across the molecular subgroups except mutKRAS. Male versus female GAC patients with mutp53 had substantially better OS if tumor carried non-GOF but worse OS if tumor carried GOF, and this was confirmed by interaction analysis. When analysis was performed independently for patients who received chemotherapy and for patients who did not receive chemotherapy, the results were similar.
Discussion
In this study with a large dataset from a community multi-center healthcare organization, we have shown that male versus female had better OS among advanced GAC but not among advanced EAC or GEJAC patients. This modest OS difference between male versus female GAC patients appeared preserved across the molecular subgroups except mutKRAS. Intriguingly, among GAC patients with mutp53, male versus female had better OS if tumor carried non-GOF but worse OS if tumor carried GOF. Both males and females showed similar OS association with chemotherapy and HER2 positivity, therefore suggesting that chemotherapy and HER2 expression were not associated with this sex disparity in survival outcomes in patients with advanced GAC.
This sex disparity in survival outcomes among advanced GAC patients was unexpected as previous epidemiology studies including all disease stages had suggested that female patients had similar or better survival outcomes compared to male patients with GAC [1, 12, 23]. More intriguingly, OS of male versus female GAC patients with mutp53 was inversely associated with the presence of non-GOF versus GOF. To our knowledge this is the first time that mutp53 is found to be associated with a prognostic sex dichotomy in a malignancy. The mechanism of this mutp53 non-GOF versus GOF association with sex dichotomy is not clear and will be interesting to investigate further. A bioinformatic study showed that among all malignancies male cancer patients carried higher rate of mutp53 than female cancer patients and patients with mutp53 had poorer OS than patients with wtp53 [23]. Our data with EAC, GEJAC and GAC all showed similar rate of mutp53 between male and female patients. The same bioinformatic study also showed that X-chromosome encodes many proteins that interact with wtp53 and that many cancers express inhibitors of wtp53 [24, 25]. Our current finding, together with the finding in our accompanying manuscript that shows that mutp53 GOF versus non-GOF was associated with worse OS among patients with GAC but not EAC or GEJAC, adds new dimensions to the complexity and versatility of mutp53 and expands upon our previous discoveries that mutp53 non-GOF was associated with worse OS of right-sided versus left-sided CRC while mutp53 GOF versus non-GOF was associated with worse OS in left-sided CRC and pancreatic ductal adenocarcinoma [21, 26].
Sex disparities in outcomes have been previously found in other malignancies. We recently reported that male versus female patients with advanced intermediate to high-grade soft tissue sarcoma had better OS, and that male versus female patients with SMARCA4-mutated advanced malignancies had worse OS [27, 28]. In a study of stage I and II melanoma patients it was found that females had superior outcomes than males [29]. Epidemiology studies have found that in general females appear to have better outcomes than males in majority of malignancies [12, 15, 23]. However, these studies included all stages of malignancies and lacked the comparative specificities presented in our work that restricted the analysis to advanced stage only and with the most common genomic alterations integrated into the statistical modeling. The factors and mechanism underlying such a disparity remain poorly understood and could include sex hormones, tumor biology and social factors. Our study suggests that tumor biology likely plays important roles. A recent study showed that loss of Y chromosome in bladder carcinoma was associated with poor OS, and with a suppressive tumor microenvironment characterized by exhaustion of CD8+ T cells which sensitizes the tumors to immune check point inhibitors [30]. Loss of Y chromosome has been reported to be associated with poor prognosis of patients with head and neck cancer and EAC [31, 32]. Loss of Y chromosome has also been found in GAC and GAC cell lines [33, 34]. It is not clear if loss of Y chromosome plays a role in the pathology and outcomes of patients with GEJAC and GAC. Recently biological mechanisms underlying predominant female incidence in systemic lupus was found to be related to Xist, a long non-coding RNA that is only expressed in females and the primary effector of X-inactivation, using a transgenic male mouse model [35]. Interestingly, p53 directly regulates the expression of Xist [36]. Studies using TCGA and other publicly available datasets have shown sex-dependent differences in the rate of certain mutations (e.g. STK11 mutation more common in men, DMD mutation more common in women, etc.), driver mutation signatures, copy number variations, and gene expression signatures, and tumor mutation burden, etc. [37, 38]. There are also evidences that males and females have different metabolism of cancer drugs, such as rituximab and fluoropyrimidine leading to different dosing of rituximab and higher toxicities of fluoropyrimidine-based regimens in women [39, 40].
Our study has limitations. It is a retrospective study and the number of patients with some of our subgroups was relatively small. In addition, the length of follow-up for some patients remained relatively short. Also, more than half of the GAC patients did not have histology type (Lauren’s classification) data available. Our study has several strengths. Our dataset is relatively large, with 426 GAC patients and nearly 900 total patients who received comprehensive primary and specialty services from a large integrated healthcare system that consists of 21 medical centers. In addition, the diverse membership is relatively stable, and electronic records capture virtually all encounters, diagnoses, and procedures. Furthermore, our study was restricted to advanced stage only and with molecular features integrated into the statistical modeling in addition to the other important factors.
In summary, our study suggests that males versus females had better OS among patients with advanced GAC but not among patients with advanced EAC or GEJAC. This sex disparity among advanced GAC patients was preserved across all molecular subgroups except mutKRAS. In addition, the sex and OS association among GAC patients with mutp53 was inversely driven by the presence of non-GOF versus GOF. To our knowledge our data for the first-time linked a sex-dependent cancer prognosis to mutp53. Our findings provide additional evidence illustrating the importance of sex disparities in cancer outcomes which may facilitate future studies on p53 biology, especially on its mechanistic interplay with sex and spatial biology.
Data availability
Kaiser Permanente Northern California (KPNC) Institutional Review Board has not provided approval for StrataNGS data on individual patients used in this study to be placed in a public access repository. However, researchers can request access to use this study data by contacting the DOR Data Sharing Workgroup at DOR-DataSharingWorkgroup@kp.org.
References
Siegel R, Giaquinto AN, Jemal A. Cancer statistics, 2024 - Siegel - 2024 - CA: A Cancer Journal for Clinicians - Wiley Online Library. Accessed April 18, 2024. https://acsjournals.onlinelibrary.wiley.com/doi/10.3322/caac.21820.
Edgren G, Adami H-O, Weiderpass E, Nyren O. A global assessment of the oesophageal adenocarcinoma epidemic | Gut. Accessed April 21, 2024. https://gut.bmj.com/content/62/10/1406.
Thrift AP, Whiteman DC. The incidence of esophageal adenocarcinoma continues to rise: analysis of period and birth cohort effects on recent trends. Ann Oncol. 2012;23:3155–62. https://doi.org/10.1093/annonc/mds181.
Bartel M, Brahmbhatt B, Bhurwal A. Incidence of gastroesophageal junction cancer continues to rise: Analysis of Surveillance, Epidemiology, and End Results (SEER) database. JCO. 2019;37:40–40. https://doi.org/10.1200/JCO.2019.37.4_suppl.40.
Wong MCS, Huang J, Chan PSF, Choi P, Lao XQ. Global Incidence and Mortality of Gastric Cancer, 1980-2018. JAMA Netw Open. 2021;4:e2118457. https://doi.org/10.1001/jamanetworkopen.2021.18457.
Morgan E, Arnold M, Camargo MC, Gini A, Kunzmann AT, Matsuda T. The current and future incidence and mortality of gastric cancer in 185 countries, 2020–40: A population-based modelling study. eClinicalMedicine. 2022;47. https://doi.org/10.1016/j.eclinm.2022.101404.
Fitzmaurice C, Allen C, Barber RM, Barregard L, Bhutta ZA, Hermann B, Global Burden of Disease Cancer Collaboration. Global, Regional, and National Cancer Incidence, Mortality, Years of Life Lost, Years Lived With Disability, and Disability-Adjusted Life-years for 32 Cancer Groups, 1990 to 2015: A Systematic Analysis for the Global Burden of Disease Study. JAMA Oncol. 2017;3:524–48. https://doi.org/10.1001/jamaoncol.2016.5688.
Xie SH, Lagergren J. The male predominance in esophageal adenocarcinoma. Clin Gastroenterol Hepatol. 2016;14:338–47.e1. https://doi.org/10.1016/j.cgh.2015.10.005.
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2019. CA: A Cancer J Clin. 2019;69:7–34. https://doi.org/10.3322/caac.21551.
Karimi P, Islami F, Anandasabapathy S, Freedman ND, Kamangar F. Gastric cancer: descriptive epidemiology, risk factors, screening, and prevention. Cancer Epidemiol Biomark Prevent. 2014;23:700–13. https://doi.org/10.1158/1055-9965.EPI-13-1057.
Agarwal S, Bell MG, Dhaliwal L, Codipilly DC, Dierkhisin RA, Lansing R. Population based time trends in the epidemiology and mortality of gastroesophageal junction and esophageal adenocarcinoma. Dig Dis Sci. 2024;69:246–53. https://doi.org/10.1007/s10620-023-08126-6.
He Y, Su Y, Zeng J, Chong W, Hu X, Zhang Y,et al. Cancer‐specific survival after diagnosis in men versus women: A pan‐cancer analysis - He - 2022 - MedComm - Wiley Online Library. Accessed April 16, 2024. https://onlinelibrary.wiley.com/doi/10.1002/mco2.145.
Nam SY, Jeon SW, Kwon YH, Kwon Okyung. Sex difference of mortality by age and body mass index in gastric cancer. Digest Liver Disease. 2021;53:1185–91. https://doi.org/10.1016/j.dld.2021.05.006.
Luan X, Niu P, Wang W, Zhao L, Zhang X, Zhao D, et al. Sex disparity in patients with gastric cancer: a systematic review and meta-analysis. J Oncol. 2022;2022:1269435 https://doi.org/10.1155/2022/1269435.
Micheli A, Ciampichini R, Oberaigner W, Ciccolallo L, de Vries E, Izarzugaza L, et al. The advantage of women in cancer survival: An analysis of EUROCARE-4 data. Eur J Cancer. 2009;45:1017–27. https://doi.org/10.1016/j.ejca.2008.11.008.
Özdemir BC, Oertelt-Prigione S, Adjei AA, Borchmann, Haanen SJB, Letschet A, et al. Investigation of sex and gender differences in oncology gains momentum: ESMO announces the launch of a Gender Medicine Task Force. Ann Oncol. 2022;33:126–8. https://doi.org/10.1016/j.annonc.2021.11.011.
Wagner AD, Oertelt-Prigione S, Adjei A, Moehler M, Peters S, Ozdemir BC, et al. Gender medicine and oncology: report and consensus of an ESMO workshop. Ann Oncol. 2019;30:1914–24. https://doi.org/10.1093/annonc/mdz414.
Miller TI, Zoumberos NA, Johnson B, Rhodes DR, Tomlins SA, Chan SA, et al. A genomic survey of sarcomas on sun-exposed skin reveals distinctive candidate drivers and potentially targetable mutations. Human Pathology. 2020;102:60–9. https://doi.org/10.1016/j.humpath.2020.06.003.
Bartley AN, Washington MK, Colasacco C, Venture CB, Ismaila N, Benson III, et al. HER2 Testing and Clinical Decision Making in Gastroesophageal Adenocarcinoma: Guideline From the College of American Pathologists, American Society for Clinical Pathology, and the American Society of Clinical Oncology. JCO. 2017;35:446–64. https://doi.org/10.1200/JCO.2016.69.4836.
Lin D, Khan U, Goetze TO, Reizine, N, Goodman, KA, Shah, MA, et al. Gastroesophageal junction adenocarcinoma: is there an optimal management? Am Soc Clin Oncol Educ Book. 2019;e88-95. https://doi.org/10.1200/EDBK_236827.
Pan M, Jiang C, Tse P, Achacoso N, Alexeeff S, Solorzano AV, et al. TP53 gain-of-function and non–gain-of-function mutations are differentially associated with sidedness-dependent prognosis in metastatic colorectal cancer. JCO. 2022;40:171–9. https://doi.org/10.1200/JCO.21.02014.
Hernán MA, Sauer BC, Hernández-Díaz S, Platt R, Shrier I. Specifying a target trial prevents immortal time bias and other self-inflicted injuries in observational analyses. J Clin Epidemiol. 2016;79:70–5. https://doi.org/10.1016/j.jclinepi.2016.04.014.
Jung KW, Park S, Shin A, Oh C-M, Kong H-J, Jun JK, et al. Do female cancer patients display better survival rates compared with males? Analysis of the Korean National Registry Data, 2005–2009. PLoS ONE. 2012;7:e52457 https://doi.org/10.1371/journal.pone.0052457.
Haupt S, Caramia F, Herschtal A, Soussi T, Lozano G, Chen, et al. Identification of cancer sex-disparity in the functional integrity of p53 and its X chromosome network. Nat Commun. 2019;10:5385. https://doi.org/10.1038/s41467-019-13266-3.
Haupt S, Haupt Y. Cancer and tumour suppressor p53 encounters at the juncture of sex disparity. Front Genet. 2021;12:632719. https://doi.org/10.3389/fgene.2021.632719.
Pan M, Jiang C, Zhang Z, Achacoso N, Alexeeff S, Solorzano AV, et al. TP53 Gain-of-Function and non–gain-of-function mutations are associated with differential prognosis in advanced pancreatic ductal adenocarcinoma. JCO Precision Oncol. 2023;:e2200570. https://doi.org/10.1200/PO.22.00570.
Pan M, Jiang C, Zhang Z, Achacoso N, Solorzano AV, Tse P, et al. Sex- and Co-Mutation-dependent prognosis in patients with SMARCA4-mutated malignancies. Cancers. 2023;15:2665. https://doi.org/10.3390/cancers15102665.
Pan M, Zhou MY, Jiang C, Zhang, Z, Bui, N, Bien, J, et al. Sex-dependent prognosis of patients with advanced soft tissue sarcoma. Clin Cancer Res. Published online October 13, 2023. https://doi.org/10.1158/1078-0432.CCR-23-1990.
Joosse A, Collette S, Suciu S, Nijsten T, Lejeune F, Kleeberg UR, et al. Superior Outcome of Women With Stage I/II Cutaneous Melanoma: Pooled Analysis of Four European Organisation for Research and Treatment of Cancer Phase III Trials. JCO. 2012;30:2240–7. https://doi.org/10.1200/JCO.2011.38.0584.
Abdel-Hafiz HA, Schafer JM, Chen X, Xiao T, Gauntner T, Li Z, et al. Y chromosome loss in cancer drives growth by evasion of adaptive immunity. Nature. 2023;619:624–31. https://doi.org/10.1038/s41586-023-06234-x.
Hollows R, Wei W, Cazier JB, Mehanna H, Parry G, Halford G, et al. Association between loss of Y chromosome and poor prognosis in male head and neck squamous cell carcinoma. Head & Neck. 2019;41:993–1006. https://doi.org/10.1002/hed.25537.
Loeser H, Wölwer CB, Alakus H, Chong S-H, Zander T, Buettner R, et al. Y chromosome loss is a frequent event in Barrett’s adenocarcinoma and associated with poor outcome. Cancers. 2020;12:1743. https://doi.org/10.3390/cancers12071743.
Oh S, Min K, Kim M, Lee SK. Sex chromosomes are severely disrupted in gastric cancer cell lines. Int J Mol Sci. 2020;21:4598 https://doi.org/10.3390/ijms21134598.
Ochi H, Douglass HO, Sandberg AA. Cytogenetic studies in primary gastric cancer. Cancer Genet Cytogenet. 1986;22:295–307. https://doi.org/10.1016/0165-4608(86)90022-1.
Dou DR, Zhao Y, Belk JA, Zhao Y, Casey KM, Chen DC, et al. Xist ribonucleoproteins promote female sex-biased autoimmunity. Cell. 2024;187:733–749.e16. https://doi.org/10.1016/j.cell.2023.12.037.
Delbridge ARD, Kueh AJ, Ke F, Zamudio NM, El-Safin F, Jasz N, et al. Loss of p53 Causes stochastic aberrant X-Chromosome inactivation and female-specific neural tube defects. Cell Rep. 2019;27:442-54.e5. https://doi.org/10.1016/j.celrep.2019.03.048.
Li CH, Prokopec SD, Sun RX, Yousif F, Schmitz N, Boutros PC. Sex differences in oncogenic mutational processes. Nat Commun. 2020;11:4330. https://doi.org/10.1038/s41467-020-17359-2.
Yuan Y, Liu L, Chen H, Wang Y, Xu Y, Mao H, et al. Comprehensive characterization of molecular differences in cancer between male and female patients. Cancer Cell. 2016;29:711–22. https://doi.org/10.1016/j.ccell.2016.04.001.
Wagner AD, Grothey A, Andre T, Dixon JG, Wolmark N, Haller DG, et al. Sex and adverse events of adjuvant chemotherapy in colon cancer: an analysis of 34,640 patients in the ACCENT database. JNCI: J Natl Cancer Inst. 2021;113:400–7. https://doi.org/10.1093/jnci/djaa124.
Müller C, Murawski N, Wiesen MHJ, Held G, Poeschek V, Zeynalova S, et al. The role of sex and weight on rituximab clearance and serum elimination half-life in elderly patients with DLBCL. Blood. 2012;119:3276–84. https://doi.org/10.1182/blood-2011-09-380949.
Acknowledgements
We thank Michael Oehrli for support in providing additional data during revision.
Funding
This study was supported by Kaiser Permanente Northern California and Stanford University. M.P. was partly supported by the Jiayin Foundation.
Author information
Authors and Affiliations
Contributions
MP and LB conceived, designed and supervised the study. MP wrote the manuscript. PT and EC provided administrative support. CJ, NA, MT, JS, TH, AD, PT, AVS, EC provide study materials. CJ, NA, MT, JS, TH, AD, PT, AVS, EC performed collection and assembly of the data. MP, LB, CJ, MT, JS, TH, AD performed data analysis and interpretation. MP, LB and GF wrote and revised the manuscript. All authors reviewed and approved the final manuscript. Final approval of manuscript: All authors. Accountable for all aspects of the work: All authors.
Corresponding author
Ethics declarations
Competing interests
Authors declare no conflict of interest. M. Pan reports personal fees from Aadi Bioscience, Boehringer Ingelheim and NewBay Pharma outside the submitted work. L.A. Habel reports grants from Strata Oncology outside the submitted work. No disclosures were reported by the other authors.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Pan, M., Tong, M.M., Stover, J. et al. Sex disparity in survival outcomes of advanced gastric adenocarcinoma. BJC Rep 3, 58 (2025). https://doi.org/10.1038/s44276-025-00173-y
Received:
Revised:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s44276-025-00173-y