Abstract
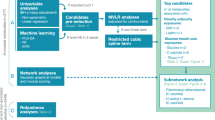
Metabolites influencing miscarriage outcomes remain understudied. We hypothesized that aberrant metabolism impacts threatened miscarriage outcomes and that understanding these pathways could offer new management strategies. This case-control study analyzed serum metabolomics from 80 women between 5 and 12 weeks’ gestation at KK Women’s and Children’s Hospital, Singapore, comparing three groups: women with threatened miscarriage who miscarried (TMMC), those with ongoing pregnancies (TMO), and women with normal pregnancies (NP). Using untargeted liquid chromatography-mass spectrometry and pathway analysis through MetaboAnalyst 5.0 and the Kyoto Encyclopedia of Genes and Genomes, 267 metabolites across 12 enriched pathways were identified. Dysregulations in steroid (AUC 0.82), folate (AUC 0.59), fatty acid (AUC 0.70), and glucosaminoglycan (AUC 0.64) pathways distinguished women who miscarried from those with ongoing pregnancies (TMMC vs TMO). We provide initial insights into the metabolic profile associated with miscarriage, highlighting disruptions in steroid hormone, fatty acid, folate, and glucosaminoglycan biosynthesis. Further validation may support biomarker development for prognostication.
Similar content being viewed by others
Introduction
Threatened miscarriage is characterized by per vaginal bleeding without cervical changes within the first 20 weeks of gestation1. It affects about 20% of pregnant women in their lifetime with a notable 25% of them progressing to an actual miscarriage2. In Singapore, similar prevalence rates have been observed, with an estimated 20% of pregnancies ending with miscarriage – most occurring within the first trimester3. Notably, Singapore faces unique demographic challenges, including an aging maternal population and the rising prevalence of metabolic disorders4, both of which are known risk factors for miscarriage. These factors underscore the pressing need for enhanced risk stratification and targeted management strategies tailored to the local context. This obstetric complication presents a prognostic challenge due to its multifactorial aetiology encompassing various maternal demographic and clinical factors, including advanced maternal age5, a history of miscarriage6, pre-existing medical conditions7, poor metabolic health8, and progesterone insufficiency3,9,10. Threatened miscarriage can be distressing, both physically and psychologically, and comes at significant cost to individuals, healthcare systems and society-at-large11. Individualized diagnosis, risk assessment and prevention of miscarriage continues to be challenging12. As of 2021, both the International Federation of Gynaecology and Obstetrics (FIGO) and National Institute for Health and Care Excellence (NICE) guidelines suggest a management approach for threatened miscarriage that hinges on the history of previous miscarriages. Progesterone supplementation is recommended for women experiencing early pregnancy bleeding who have a history of miscarriage, although the efficacy of this intervention remains a subject of ongoing debate and investigation13,14. Therefore, better prognostication methods that guide treatment strategies to preserve pregnancy or counselling of potential adverse outcomes are urgently needed.
Successful pregnancy involves multiple metabolic adaptations that are necessary in order to ensure a sufficient supply of essential nutrients and energy to support the growth and the development of the fetus. Throughout gestation, maternal basal metabolic rate increases which causes energy expenditure to increase to levels close to high performance endurance athletic activities15. The transformation to an ‘anabolic state’ of the first (and second) trimester of the pregnancy, where lipids are stored, and glucose homeostasis is regulated16,17, are known metabolic alterations in healthy pregnancies. Barring inborn errors, the converse inability for the maternal metabolic adaptations to occur can lead to insufficient support of fetal nutritional and developmental needs, and adverse outcomes such as early pregnancy loss. Emerging studies look to the use of metabolomics to identify potential prognostic biomarkers for assessing miscarriage risk by closely examining maternal metabolic health. This is driven by research that have found that women with poor metabolic health, like those with metabolic syndrome, are more likely to experience pregnancy complications compared to those without such conditions18,19. Metabolomics involves the comprehensive analysis of metabolites in cells, fluids, and tissues20. It offers a detailed snapshot of metabolic pathways and biochemical processes, thereby providing a nuanced understanding of an individual’s metabolic state at a given time point. Prior research has demonstrated significant urinary metabolomic disparities between patients with miscarriages and those with healthy pregnancies, suggesting dysfunctional placental mitochondrial β-oxidation of fatty acids as a possible etiology of spontaneous miscarriage21. Other serum metabolomic studies involving subjects with spontaneous miscarriage implicate a wide array of metabolic pathways from lipid to homocysteine metabolism22,23,24. These emerging evidence point towards the role of metabolic abnormalities in miscarriage25.
Building on this, our study aims to identify key serum metabolomic differences that distinguish women who experience miscarriage, providing novel insights into the metabolic signatures underpinning early pregnancy outcomes. We hypothesize that women with threatened miscarriage exhibit unique metabolic profiles in contrast to those with healthy pregnancies. Among women with threatened miscarriage, we ask what are the key metabolites and pathways that distinguishes those who eventually miscarry compared to those who go on to have an ongoing pregnancy. A thorough understanding of these metabolite variations may illuminate the underlying metabolic imbalances that interplay with miscarriage, opening new possibilities to guide upstream prognostication and downstream treatment interventions.
Results
Prospectively collected serum samples from 80 patients, including 70 patients identified with threatened miscarriage (TM group) and 10 control patients (NP group) with non-bleeding and normal pregnancy were collected for metabolomic analysis. Of the 70 TM patients, 38 had ongoing pregnancy beyond 16 weeks (TMO group); 32 eventually miscarried before 16 weeks’ gestation (TMMC group) (Table 1). TMO and TMMC patients were significantly older than NP patients (p < 0.001). There was no significant age difference between TMO and TMMC patients. Consistent with miscarriages being associated with lower levels of progesterone, TMMC patients had significantly lower progesterone levels than NP and TMO patients.
Metabolomic differences in women with Threatened Miscarriage (TM) as compared to Normal Pregnancies (NP)
Figure 1a presents the PLS-DA scores plot of the serum metabolome between the TM and NP groups. A critical task in PLS modelling is the selection of the number of PLS components to construct a pseudo inverse which is optimal for prediction. To assess the statistical robustness of the model, a 5-fold cross-validation using five principal components was performed, giving an R2 (explained variation) of 0.99, Q2 (predicted variation) of 0.65 and a classification accuracy of 0.99, indicating substantial predictive ability and good fitting of the PLS-DA model. The analysis demonstrates a clear separation of the samples into two distinct clusters. This separation highlights the distinct metabolic profiles between the TM and NP groups (Fig. 1a).
a The partial least squares-discriminant analysis (PLS-DA) of serum metabolites in patients with threatened miscarriage (TM) vs those with normal pregnancies (NP), with the PLSDA showing separation into 2 distinct clusters (5 fold cross-validation with 5 principal components – R2 = 0.99, Q2 = 0.65, classification accuracy = 0.99). b The PLS-DA of metabolites in patients with threatened miscarriage who eventually miscarried (TMMC) vs those who had ongoing pregnancies (TMO). PLSDA shows poor separation (5 fold cross-validation with 5 principal components – R2 = 0.98, Q2 = 0.22, classification accuracy = 0.66).
A total of 114 metabolites were found to be significantly different between the TM and NP samples, with FC ≥ 2 or ≤0.5, and raw p-value < 0.05. Figure 2a shows the volcano plot for these compounds. Eight metabolic pathways were found to be enriched and significantly different (p-value < 0.05) between the TM and NP samples. Table 2 summarises the identified pathways and metabolite hits, along with the FC and raw and false discovery rate (FDR)-adjusted p-values, as well as FC and p-values corrected for age, BMI and smoking status. Within these pathways, 16 unique metabolites were identified, of which five were significantly different (FC ≥ 2 or ≤0.5, and raw p-value < 0.05), most of which remained significant after correction and using FDR-adjusted p-values, with the exception of estrone sulfate, which fell slightly below the FC threshold, and leukotriene D4. Notably, products of steroid metabolism, namely estrone sulfate, dehydroepiandrosterone sulfate and cholesterol sulfate, key metabolites of associated with pregnancy were observed to be significantly enriched in the TM group26, thereby validating our results.
a Volcano plot for metabolites in patients with threatened miscarriage (TM) vs those with normal pregnancies (NP). Metabolites which were significantly different (Fold Change (FC) ≥ 2 or ≤0.5, and raw p-value < 0.05) are highlighted. FC is expressed with NP as reference. b Volcano plot for metabolites in patients with threatened miscarriage who eventually miscarried (TMMC) vs those who had ongoing pregnancies (TMO). Metabolites which were significantly different (Fold Change (FC) ≥ 2 or ≤0.5, and raw p-value < 0.05) are highlighted. (FC is expressed with NP as reference). Red hues indicate metabolites with increased abundance in the TM group compared to NP (positive fold change), while blue hues indicate metabolites with decreased abundance in the TM group compared to NP (negative fold change). Black/gray points represent metabolites that do not meet the statistical significance threshold.
Metabolomic differences in women with threatened miscarriage and different outcomes (TMMC vs TMO)
Figure 1b illustrates the results of the multivariate analysis between the TMMC and TMO groups using PLS-DA. Compared to the previous comparison (TM vs NP), this PLS-DA shows less distinct separation, with noticeable overlaps between the two clusters (Fig. 1b). Despite this overlap, the 5-fold cross-validation of the model yielded an R2 of 0.98, indicating strong fit, but a lower Q2 of 0.22, suggesting limited predictive ability. The model yielded a classification accuracy of 0.66. This result reflects the metabolic similarities between the two groups, both of which experienced a threatened miscarriage.
However, despite the overlapping profiles, 28 metabolites were found to be significantly different between the TMMC and TMO groups, with a FC of ≥2 or ≤0.5 and a raw p-value < 0.05, indicating statistical significance. Table 2 summarises the identified pathways and metabolite hits, along with the FC and raw and false discovery rate (FDR)-adjusted p-values, as well as FC and p-values corrected for age, BMI and smoking status. Five compounds (estrone sulfate, palmitic acid, 7,12-dimethylbenz[a]anthracene 5,6-oxide, 4a-Hydroxytetrahydrobiopterin, dermatan) were significantly different between the two groups based on raw p-value < 0.05 but not FC criteria, and they continue to be significant after correction for age, BMI and smoking status, but not when adjusted for FDR. Given the clinical similarities between the 2 groups and the strictness of the Bonferroni method, these compounds will be discussed below for their potential biological significance despite not meeting the FC criteria. Figure 2b provides a volcano plot highlighting these significantly altered compounds, with the FC and p-value thresholds clearly visualized.
The most significantly impacted pathway was steroid hormone biosynthesis (p < 0.001), characterized by a marked decrease in estrone sulfate (FC = 0.39). Additionally, unsaturated fatty acid biosynthesis (p < 0.05) showed notable alterations, with palmitic acid exhibiting the largest fold change (FC = 2.02). In the folate synthesis pathway (p < 0.05), 4α-hydroxytetrahydrobiopterin was significantly reduced (FC = 0.70). Interestingly, we also observed a significant reduction in dermatan (FC = 0.75), a glycosaminoglycan metabolite (p < 0.05) found in blood vessels and stroma of the placental villi that prevents placenta thrombosis27, in individuals who ultimately experienced miscarriage, suggesting a potential link between dermatan levels and pregnancy outcomes.
ROC analyses revealed that serum estrone sulfate demonstrated the strongest discriminatory performance between TMMC and TMO with an AUC of 0.81 (95% Cl 0.71–0.92), followed by palmitic acid (AUC 0.70, 95% Cl 0.57–0.82), dermatan (AUC 0.64, 95% Cl 0.51–0.77), and 4a-hydroxytetrahydrobiopterin (AUC 0.59, 95% Cl 0.45–0.73).
The metabolomic differences between TMO and NP, as well as between TMMC and NP, are detailed in Supplementary Tables 1 and 2, respectively.
Discussion
The staggering number of miscarriages coupled with recent calls for improved medical approaches to address this issue, underscores the urgency of advancing our understanding of the biological mechanisms and metabolic pathways involved in miscarriages11. This study compares the serum metabolomic profiles of three groups of women: those experiencing threatened miscarriage who subsequently miscarry (TMMC), those who experienced threatened miscarriages with ongoing pregnancies at 16 weeks (TMO), and those with normal pregnancies (NP).
Our study clearly indicates that the serum metabolomic profile of those who miscarried is clearly different from those with normal pregnancies, identifying a total of 267 metabolites belonging to 12 enriched pathways, and possessing predicative abilities. Importantly, among women with threatened miscarriage, TMMC had a distinct metabolomic profile from TMO with a total of 28 different metabolites. Specifically, we identified alterations in steroid, fatty acid, glycosaminoglycan and folate metabolic pathways, which mediates inflammation and mitochondrial dysfunction, in women who miscarried (Fig. 3; Table 3).
Box plots showing the normalized concentrations of (a) estrone sulfate, (b) dermatan, (c) 4α-hydroxytetrahydrobiopterin and (d) palmitic acid in the NP (red), TMMC (green), and TMO (blue) groups. The yellow diamonds represent the mean concentrations for each group, while the black dots indicate individual data points. NP normal pregnancies, TMMC patients with threatened miscarriage who eventually miscarried, TMO patients with threatened miscarriage who had ongoing pregnancies.
While several metabolic pathways were significantly altered in both the TM vs NP and TMO vs TMMC comparisons, their biological interpretations differ based on clinical context. The TM vs NP comparison reflects broader systemic alterations in response to early pregnancy bleeding, regardless of outcome. However, as a larger proportion of women in the TM group ultimately had ongoing pregnancies (TMO, 38 out of 70), the overall metabolomic profile of TM is skewed toward the metabolic signature of TMO, which is in turn more similar to NP. This may explain the observed overlap in enriched pathways between TM and NP groups, as well as the relatively modest group separation seen in multivariate analysis.
In contrast, the TMO vs TMMC comparison specifically isolates outcome-related differences among women who all presented with early bleeding. The metabolites that distinguished TMMC from TMO—such as estrone sulfate, palmitic acid, dermatan sulfate, and 4α-hydroxytetrahydrobiopterin—represent potential prognostic biomarkers for eventual miscarriage.
Steroid hormones are integral to the conception and maintenance of a healthy pregnancy, with progesterone promoting immune tolerance and endometrial preparation28, while androgens and estrogens facilitate vascular development, and myometrial preparation for labour29,30. Perturbation in the homeostasis of these hormones has been linked to the pathogenesis of threatened miscarriage26,31. In our study, we observed significant alterations in the metabolites involved in steroid hormone synthesis pathway across both comparisons (TM vs NP and TMMC vs TMO) (Table 3). Specifically, estrone sulfate levels were significantly decreased in TMMC as compared to TMO. Estrone sulfate, an important precursor to estradiol, can be used as a proxy for serum estradiol levels. These findings align with prior evidence indicating that low serum estradiol levels is associated with higher miscarriage rates32,33.
Reduced levels of dehydroepiandrosterone sulfate (DHEA-S), a precursor in the steroid hormone pathway, may contribute to lower levels of estrone sulfate, as DHEA-S acts as an intermediate substrate between cholesterol and sex steroids necessary for a healthy pregnancy. Low DHEA-S levels has been linked to impaired pregnancy viability26,34. Corroborating this hypothesis, a recent systematic review and meta-analysis found that DHEA-S supplementation was associated with significant improvements in clinical pregnancy rates, live birth outcomes, and endometrial receptivity in in-vitro fertilization procedures35. Furthermore, Boyle et al. (2024) demonstrated that estradiol restoration via DHEA-S supplementation significantly reduced in miscarriage rates36. These observations lend credence to the potential utility of DHEA-S as a therapeutic intervention in the prevention of miscarriage, encouraging additional research in this novel therapeutic modality35. The balance between these hormones is crucial in preventing the excessive inflammatory reactions that can lead to miscarriage, underscoring the hormone’s protective role in early gestation.
Tetrahydrobiopterin (BH4) is an essential cofactor for lipid ester metabolism and the synthesis of various neurotransmitters and nitric oxide, producing 4α-hydroxytetrahydrobiopterin (BH4 4α carbolamine) which will be recycled back to BH437,38. Our study observed BH4 4α-carbolamine to be significantly lower in TMMC compared to TMO. This suggests reduced BH4 levels and thus decreased synthesis of neurotransmitters which could affect neuronal functions and signaling during pregnancy and fetal neurodevelopment39,40. Reduced BH4 levels have also been reported to be associated with hypertensive pregnancies and impaired uteroplacental vascular remodeling that could be normalized with 5-methytetrahydrofolate supplementation in an animal model41. Taken together, adequacy of BH4 levels may be a key determinant of healthy pregnancy. To ensure BH4 adequacy going into pregnancy, folic acid supplementation may be recommended from preconception to pregnancy. Previous research had investigated the utility of folic acid supplementation as a potential treatment target in the context of threatened miscarriage. However, the evidence regarding the relationship between serum folic acid levels and the risk of threatened miscarriage remains inconclusive. Some studies found no association42,43 while other research has observed a link44,45. In terms of supplementation, Gindler et al. found that the miscarriage rate of primiparous women was not influenced by 400 µg of folic acid supplementation46. Beyond supplementation, as it is difficult to directly measure BH4 in the blood38, BH4 4α-carbolamine may also serve as an indirect method of measurement along with the potential to predict miscarriage in women with threatened miscarriage.
Fatty acids are crucial for foetal development and growth during pregnancy47, with palmitic acid being the predominant saturated free fatty acid observed in maternal serum48. Our study found significantly elevated levels of palmitic acid among patients with TMMC as compared to TMO. This increase in palmitic acid has been associated with placental inflammation via activation of the NLRP3 inflammasome, resulting in miscarriage and other adverse pregnancy outcomes in a murine study49. In another murine study, exposure to excess palmitic acid has also been shown to hinder embryonic development and growth50. The lipotoxic effect of excessive palmitic acid, through stress induction of the mitochondria and endoplasmic reticulum, can lead to embryo apoptosis50. These findings align with a human metabolomics study by Fei et al. who reported higher levels of the pro-inflammatory metabolite sphingosine and lower levels of the anti-inflammatory metabolite sphingosine 1-phosphate in individuals with missed miscarriages, pointing to an inflammatory mechanism at play51. Our study suggests that a similar inflammatory dysregulation via palmitic acid may apply to those with threatened miscarriage and hold the potential to predict the eventual outcome of the pregnancy.
Glycosaminoglycans (GAGs) are crucial components of the extracellular matrix (ECM) in uterine tissue52. They support cell signaling, tissue remodeling and hydration, essential for embryo implantation and placental development52,53. GAG levels increase during pregnancy to accommodate fetal growth and uterine expansion52. In our study, dermatan sulfate levels were significantly reduced in the TMMC group compared to the TMO group. Dermatan sulfate is a GAG that activates the anti-thrombin activity of heparin cofactor II found in maternal and fetal blood. Maternal-fetal exchange of blood gases and nutrients occurs at placental villi, which are covered by a layer of syncytiotrophoblasts. Heparin cofactor II come in contact with dermatan sulfate with injury to these syncytiotrophoblasts covering the surface of placental villi. Heparin cofactor II serve to limit fibrin coagulation and deposits at such sites of syncytiotrophoblast injury. Therefore, it is tempting to speculate that a reduction in dermatan sulfate might lead to thrombotic lesions, compromise placental function and lead to miscarriages54.
Maternal age is a major risk factor of miscarriage with the risk rising sharply in women of age of 35 years and above. Our study might reflect age-related metabolic aberrations associated with the exponential increase in chromosomal aberrations in oocytes and foetal tissues precipitating in miscarriage55. Clinically, the aetiology of threatened miscarriage is a highly heterogenous and there is no “one-size-fits” all management strategy56. At present, management ends at serum progesterone supplementation but accumulating evidence have shown that it is ineffective at improving pregnancy outcomes14,57. Suggestions have been made to incorporate individualised risk assessment, including metabolic profiles to tailor surveillance of women who are likely to experience recurrent miscarriages. Our study suggest that such an approach may be warranted in first-time miscarriages.
Our study utilized serum metabolomics to identify metabolites which may serve as screening biomarkers and therapeutic targets. From our findings, dysregulation in key metabolic pathways which converge on imbalanced inflammation may play a critical role in determining the eventual outcome of threatened miscarriage. This opens the possibility of screening and subsequent modulation of metabolite levels via oral supplementation of deficient metabolites such as DHEA-S, dermatan sulfate and folic acid, and concurrent suppression of palmitic acid.
This is the first study to identify distinguishing metabolomic features in women who experienced threatened miscarriage, paving the way for the identification of specific metabolites that could predict the progression towards either a successful pregnancy or a miscarriage. This enables early intervention and personalized management strategies. Our study crucially reports the gestational age of the sample, thus providing context for interpreting the metabolic changes that occur at different stages of pregnancy. By accounting for gestational age, our study provides valuable understanding of metabolic alterations associated with miscarriage risk at specific pregnancy stages, enhancing the ability to pinpoint time-sensitive changes that potentially be translated as biomarkers.
Our study is subject to certain limitations that should be considered when interpreting its findings. The primary limitation is the relatively small sample size, which may affect the generalizability of our results. The limited number of participants, particularly within the control group, reduces statistical power and increases the risk of false negatives—potentially overlooking subtle yet biologically meaningful metabolic differences associated with miscarriage. Moreover, the control group’s small size may not fully represent the metabolic diversity of the general population of women with normal pregnancies, limiting the comparability between groups. However, the most clinically relevant comparison lies between women with threatened miscarriage who subsequently miscarried (TMMC) and those who progressed to term (TMO), as these groups present similarly at baseline yet experience markedly different outcomes. This focus justifies the prioritization of case recruitment and partially mitigates concerns regarding the smaller control sample size. Additionally, the study cohort may not encompass the full spectrum of metabolic variability within the wider Asian population or across different ethnicities, which may limit the broader applicability of our findings58. Future studies should include larger and more ethnically diverse cohorts to validate our observations and capture a more representative range of metabolomic profiles.
While we performed multivariable adjustment for key potential confounders—including maternal age, BMI, and smoking status—during univariate differential analysis, the small sample size limits the robustness of these adjustments. Maternal age differed significantly between groups; however, the average age remained below the conventional threshold for advanced maternal age (≥35 years), which is more strongly associated with adverse pregnancy outcomes59. BMI did not significantly differ across groups, and smoking status was included where available. Although residual confounding cannot be entirely ruled out, we believe its impact on the observed metabolomic differences is likely limited.
To account for multiple hypothesis testing, we applied FDR correction during univariate analysis. As expected in high-dimensional datasets with limited sample sizes, several metabolite-level associations that were nominally significant did not remain so after correction. This attenuation is likely due to limited statistical power rather than the absence of true biological differences. Future studies with larger cohorts and complementary statistical methods may provide a more balanced approach to identifying meaningful metabolomic signals without excessively penalizing exploratory discovery. Future studies with larger cohorts and complementary statistical methods may offer a more balanced approach for identifying meaningful metabolomic signals without excessively penalizing exploratory discovery.
Finally, longitudinal data in our study would have provided time-course changes to the serum metabolomic profiles. Our research design is cross-sectional, capturing a single snapshot in time, which restricts our ability to establish causal relationships or to track the progression of metabolic changes over the course of pregnancy leading up to miscarriage. Longitudinal studies are essential to understand the dynamic changes in serum metabolites and their interaction with the risk of miscarriage. The absence of such data limits our ability to draw robust conclusions about the temporal nature of the metabolic alterations observed and their potential role in the pathophysiology of miscarriage.
As such, future research involving larger and more diverse cohorts and employing a longitudinal design is necessary to validate and extend our understanding of the metabolic pathways associated with miscarriage. Extending metabolomic studies to pre-pregnancy individuals would enlighten the plausibility and validity of metabolites and metabolic alterations found in this study as early predictive biomarkers of miscarriage. These alterations may also reflect and emphasize biologically entrenched interference in placenta formation in women with a higher risk of miscarriage60. The advent of endometrial and placenta organoids offers experimental models to dissect the metabolic and potentially age-related metabolic mechanisms in miscarriages61,62.
In conclusion, our study elucidates a detailed network of altered metabolic pathways linking inflammation to threatened miscarriage. We also present a key set of metabolites that distinguishes eventual outcome of threatened miscarriage. This research represents the first to delineate these distinct metabolic pathways in previously healthy women who have experienced threatened miscarriage, laying the foundations for predictive tools for more tailored management.
Methods
Patient characteristics
This is a case-control study, involving 80 patients recruited at the KK Women’s and Children’s Hospital. Recruitment for the negative control group took place from July 1 to July 29, 2019, while patients with threatened miscarriage were enrolled between October 26, 2020, and March 21, 2022. All selected patients were pregnant with a single intrauterine fetus confirmed by ultrasonography at 5–12 gestation weeks. Patients who were age 40 years and above, had two or more previous miscarriages, had a previous episode of pregnancy-related per vagina bleeding in the current pregnancy, underwent progesterone treatment for previous per vagina bleeding or for any other medical reasons in this current pregnancy, diagnosed with inevitable miscarriage, planning to terminate the pregnancy and those with uncontrolled medical conditions, were excluded.
Pregnancy outcomes were determined at 16 weeks gestation to be either that of miscarriage at or before 16 weeks, or ongoing pregnancy beyond 16 weeks gestation. Of the 70 patients identified with threatened miscarriage (TM group), 38 had normal pregnancy and delivery (TMO group); 32 eventually miscarried before 16-weeks gestation (TMMC group). 10 control patients (NP group) with non-bleeding and normal pregnancy were selected (Table 1).
Ethics approval
This study was conducted in accordance with the ethical principles outlined in the Declaration of Helsinki. Ethics approval was obtained from the SingHealth Centralised Institutional Review Board (CIRB 2019/2513 and CIRB 2016/2950) and all patients provided informed written consent.
Sample collection & data storage
Blood samples were collected at recruitment during the initial presentation. 20 ml of peripheral blood samples were collected and centrifuged at 3000 g for 10 min at 20 oC. Aliquoted serum was stored at −80 oC until analysis. Patient data is stored in REDCap and a password-encrypted laptop.
Serum metabolomics analyses: LC-MS
Serum metabolomic processing was conducted with the following protocol: 100 μL ice-cold extraction solvent (V methanol: V water=9:1) reconstitution was added to the sample. The sample solution (30 μL) was collected into a fresh 2 mL LC/MS glass vial for the UHPLC-QTOF-MS analysis. The supernatant fraction was analysed using Agilent 1290 ultrahigh pressure liquid chromatography system. The column used for the separation was an Agilent ZORBAX RRHD (1.8 μm*2.1*100 mm). The oven temperature was set at 50 °C. The gradient elution involved a mobile phase consisting of (A) 0.1% Acetonitrile in water and (B) 0.1% Acetonitrile in methanol. The initial condition was set at 5% B. A 7 min linear gradient to 70% B was applied, followed by a 12 min gradient to 100% B which was held for 3 min, then returned to starting conditions over 0.1 min. Flow rate was set at 0.4 ml/min, and 10 μL of samples was injected. The electrospray ionization mass spectra were acquired in negative ion mode, due to the lower background noise63. Mass data were collected between m/z 100 and 1000 at a rate of two scans per second. The ion spray voltage was set at 4000 V, and the heated capillary temperature was maintained at 350 °C. The drying gas and nebulizer nitrogen gas flow rates were 12.0 L/min and 35 psi, respectively. Washing samples were injected in between every 5 samples for maintaining stability and washing the needle. A rigorous quality assurance / quality control (QA/QC) pipeline was implemented. Pooled quality control (QC) samples were injected at regular intervals during the analytical sequence to monitor instrument stability, and features with a relative standard deviation (RSD) > 20% in QC samples were excluded. Missing values due to technical limitations were imputed using the half-minimum approach within QC samples; biological missing values (absent in >70% of samples within a group) were excluded. Features with low signal-to-noise ratio (S/N < 5) or detected in <50% of QC samples were removed to reduce noise. Combat algorithm (parametric adjustment) was applied to correct for intra-batch variability. Probabilistic quotient normalization (PQN) was performed using QC-based reference spectra to account for systematic variations.
For metabolomics analysis, raw spectrometric data were converted to CEF formats via Mass Hunter Profinder (Agilent, US) and input to Mass Profiler Professional (MPP) for peak finding, peak alignment and peak normalization across all samples. Molecular features were filtered by abundance, mass range, number of ions per feature, and charge state in the MS Experiment Creation Wizard. The minimum absolute abundance was set at 2000 counts for filtering. Significance Testing and Fold Change Wizard were employed to improve the quality of results and to create an initial differential expression from data. The steps are predetermined and based on the experiment type, experiment grouping, and conditions you entered when creating your project and setting up your experiment. The elemental compositions of the metabolites were first calculated based on the exact mass, the nitrogen rule and the isotope pattern by Mass Hunter software from Agilent. The elemental composition and exact mass were used for database searching. The identification of untargeted metabolites followed the Metabolomics Standards Initiative (MSI) guidelines, with 15% of annotated metabolites matched to in-house authentic chemical standards, 60% matched to public databases (HMDB, METLIN), and the remaining metabolites assigned based on mass-to-charge ratio (m/z) and fragmentation patterns consistent with a metabolite class, or retained as “unknowns” but excluded from downstream biological interpretation. All annotations were cross-validated using XCMS Online and MS-DIAL platforms, with manual curation to resolve ambiguities (e.g., isomer discrimination via collision energy-resolved fragmentation). A total of 1538 metabolites were detected and quantified in the dataset following peak alignment, deconvolution, and compound identification.
Statistical analysis
Maternal characteristics across the four study groups (TM, TMO, TMMC, and NP) were compared with Fisher’s exact tests for categorical variables and Kruskal-Wallis tests for continuous variables with a p < 0.05. Where overall differences were significant, pairwise comparisons were performed using the Mann-Whitney U test with Bonferroni correction applied (p < 0.0167 considered significant).
Metabolomic data from the negative ion mode LC-MS were analysed using Metaboanalyst 5.064. For every pairwise comparison between the four groups, data were normalized by median, log-transformed, and auto-scaled. Fold changes (FC) was calculated for each metabolite, and univariate differential analysis was conducted using the Student’s t-test. Metabolites were considered significant if they met both a fold change threshold (FC ≥ 2 or ≤ 0.5) and a raw p-value < 0.05. A total of 1538 unique metabolites were tested. To adjust for multiple hypothesis testing, the Benjamini-Hochberg false discovery rate (FDR) correction was applied65. However, raw p-values were ultimately used for feature selection to balance sensitivity with interpretability in downstream pathway analysis, given the exploratory nature of the study and the limited sample size. The univariate analysis was repeated with adjustments for potential confounders including age, BMI, and smoking status.
Multivariate analysis was performed using partial least squares-discriminant analysis (PLS-DA) to assess group separation. To evaluate model robustness and minimize the risk of overfitting, cross-validation metrics including the explained variance (R²) and cross-validated predictive ability (Q²) were reported.
Significant metabolites were subjected to pathway enrichment analysis was performed using Metaboanalyst 5.0 and the Kyoto Encyclopaedia of Genes and Genomes (KEGG) (http://www.Genome.jp/kegg/) to identify the key metabolic pathways involved in miscarriage. Statistically significant pathways were identified by p-value < 0.05.
To evaluate the discriminatory performance of each significant pathway, a pathway activity score was computed for each sample by calculating the average of the normalized intensities of all metabolites mapped to that pathway. These pathway scores were used as predictors in logistic regression models to classify between groups (e.g., TM vs NP). Receiver operating characteristic (ROC) curve analysis was performed, and the area under the curve (AUC) was calculated to quantify the discriminatory performance of each pathway. All ROC and AUC analyses were conducted using the PROC LOGISTIC procedure in SAS version 9.4 (SAS Institute Inc., Cary, NC).
Data Availability
The datasets used and/or analysed during the current study available from the corresponding author on reasonable request.
Code availability
The underlying code for this study is not publicly available but may be made available to qualified researchers on reasonable request from the corresponding author.
References
Mouri, M., Hall, H. & Rupp, T. J. Threatened Miscarriage. In StatPearls (StatPearls Publishing, 2025). Available at https://www.ncbi.nlm.nih.gov/books/NBK430747/.
Kuehn, B. M. More Comprehensive Care for Miscarriage Needed Worldwide. JAMA 325, 2335 (2021).
Tan, T. C. et al. Novel approach using serum progesterone as a triage to guide management of patients with threatened miscarriage: a prospective cohort study. Sci. Rep. 10, 9153 (2020).
Loy, S. L. et al. Metabolic health status and fecundability in a Singapore preconception cohort study. Am. J. Obstet. Gynecol. 226, 714.e1-–714.e16 (2022).
Smith, K. E. & Buyalos, R. P. The profound impact of patient age on pregnancy outcome after early detection of fetal cardiac activity. Fertil. Steril. 65, 35–40 (1996).
Stirrat, G. M. Recurrent miscarriage. Lancet 336, 673–675 (1990).
García-Enguídanos, A., Calle, M. E., Valero, J., Luna, S. & Domínguez-Rojas, V. Risk factors in miscarriage: a review. Eur. J. Obstet. Gynecol. Reprod. Biol. 102, 111–119 (2002).
Ng, K. Y. B. et al. Systematic review and meta-analysis of female lifestyle factors and risk of recurrent pregnancy loss. Sci. Rep. 11, 7081 (2021).
Lek, S. M. et al. Validation of serum progesterone <35nmol/L as a predictor of miscarriage among women with threatened miscarriage. BMC Pregnancy Childbirth 17, 78 (2017).
Ku, C. W. et al. How can we better predict the risk of spontaneous miscarriage among women experiencing threatened miscarriage?. Gynecol. Endocrinol. 31, 647–651 (2015).
Quenby, S. et al. Miscarriage matters: the epidemiological, physical, psychological, and economic costs of early pregnancy loss. Lancet 397, 1658–1667 (2021).
Coomarasamy, A. et al. Sporadic miscarriage: evidence to provide effective care. The Lancet 397, 1668–1674 (2021).
Coomarasamy, A. et al. Progesterone to prevent miscarriage in women with early pregnancy bleeding: the PRISM RCT. Health Technol. Assess. 24, 1–70 (2020).
Devall, A. J. et al. Progestogens for preventing miscarriage: a network meta-analysis. Cochrane Database Syst. Rev. 4, CD013792 (2021).
Thurber, C. et al. Extreme events reveal an alimentary limit on sustained maximal human energy expenditure. Sci. Adv. 5, eaaw0341 (2019).
Jebeile, H., Mijatovic, J., Louie, J. C. Y., Prvan, T. & Brand-Miller, J. C. A systematic review and metaanalysis of energy intake and weight gain in pregnancy. Am. J. Obstet. Gynecol. 214, 465–483 (2016).
Armistead, B. et al. Placental Regulation of Energy Homeostasis During Human Pregnancy. Endocrinology 161, bqaa076 (2020).
Hilali, N. G. et al. Recurrent pregnancy loss and metabolic syndrome. Ginekologia Polska 91, 320–323 (2020).
Grieger, J. A. et al. Metabolic syndrome in pregnancy and risk for adverse pregnancy outcomes: A prospective cohort of nulliparous women. PLoS Med 15, e1002710 (2018).
Cui, L., Lu, H. & Lee, Y. H. Challenges and emergent solutions for LC-MS/MS based untargeted metabolomics in diseases. Mass Spectrometry Reviews 37, 772–792 (2018).
Ku, C. W. et al. Spontaneous miscarriage in first trimester pregnancy is associated with altered urinary metabolite profile. BBA Clin 8, 48–55 (2017).
Li, X. et al. Metabolomic Profiling of Plasma Samples from Women with Recurrent Spontaneous Abortion. Med. Sci. Monit. 24, 4038–4045 (2018).
Craciunas, L., Chu, J., Pickering, O., Mohiyiddeen, L. & Coomarasamy, A. The metabolomic profile of endometrial receptivity in recurrent miscarriage. Minerva Obstet. Gynecol. 75, 526–534 (2023).
Chaudhry, S. H. et al. The role of maternal homocysteine concentration in placenta-mediated complications: findings from the Ottawa and Kingston birth cohort. BMC Pregnancy Childbirth 19, 75 (2019).
Liang, L. et al. Metabolic Dynamics and Prediction of Gestational Age and Time to Delivery in Pregnant Women. Cell 181, 1680–1692.e1615 (2020).
Noyola-Martinez, N., Halhali, A. & Barrera, D. Steroid hormones and pregnancy. Gynecol. Endocrinol. 35, 376–384 (2019).
Giri, T. K. & Tollefsen, D. M. Placental dermatan sulfate: isolation, anticoagulant activity, and association with heparin cofactor II. Blood 107, 2753–2758 (2006).
Kolatorova, L., Vitku, J., Suchopar, J., Hill, M. & Parizek, A. Progesterone: A Steroid with Wide Range of Effects in Physiology as Well as Human Medicine. Int. J. Mol. Sci. 23, https://doi.org/10.3390/ijms23147989 (2022).
Albrecht, E. D. & Pepe, G. J. Estrogen regulation of placental angiogenesis and fetal ovarian development during primate pregnancy. Int. J. Dev. Biol. 54, 397–408 (2010).
Makieva, S., Saunders, P. T. & Norman, J. E. Androgens in pregnancy: roles in parturition. Hum. Reprod. Update 20, 542–559 (2014).
Ku, C. W. et al. Serum progesterone distribution in normal pregnancies compared to pregnancies complicated by threatened miscarriage from 5 to 13 weeks gestation: a prospective cohort study. BMC Preg. Childbirth 18, https://doi.org/10.1186/s12884-018-2002-z (2018).
Deng, W. et al. Prediction of miscarriage in first trimester by serum estradiol, progesterone and β-human chorionic gonadotropin within 9 weeks of gestation. BMC Preg. Childbirth 22, https://doi.org/10.1186/s12884-021-04158-w (2022).
Check, J. H., Lurie, D., Davies, E. & Vetter, B. Comparison of First Trimester Serum Estradiol Levels in Aborters versus Nonaborters during Maintenance of Normal Progesterone Levels. Gynecologic and Obstetric Investigation 34, 206–210 (1992).
Ebeling, P. & Koivisto, V. A. Physiological importance of dehydroepiandrosterone. Lancet 343, 1479–1481 (1994).
Liu, Y., Hu, L., Fan, L. & Wang, F. Efficacy of dehydroepiandrosterone (DHEA) supplementation for in vitro fertilization and embryo transfer cycles: a systematic review and meta-analysis. Gynecol. Endocrinol. 34, 178–183 (2018).
Boyle, P. et al. Restoration of serum estradiol and reduced incidence of miscarriage in patients with low serum estradiol during pregnancy: a retrospective cohort study using a multifactorial protocol including DHEA. Front. Reprod. Health 5, https://doi.org/10.3389/frph.2023.1321284 (2024).
Desai, A., Sequeira, J. M. & Quadros, E. V. The metabolic basis for developmental disorders due to defective folate transport. Biochimie 126, 31–42 (2016).
Eichwald, T. et al. Tetrahydrobiopterin: Beyond Its Traditional Role as a Cofactor. Antioxidants (Basel) 12, https://doi.org/10.3390/antiox12051037 (2023).
Djukic, A. Folate-responsive neurologic diseases. Pediatr. Neurol. 37, 387–397 (2007).
Kronenberg, G. et al. Folate deficiency induces neurodegeneration and brain dysfunction in mice lacking uracil DNA glycosylase. J. Neurosci. 28, 7219–7230 (2008).
Chuaiphichai, S. et al. Endothelial GTPCH (GTP Cyclohydrolase 1) and Tetrahydrobiopterin Regulate Gestational Blood Pressure, Uteroplacental Remodeling, and Fetal Growth. Hypertension 78, 1871–1884 (2021).
Hoffman, M. L., Scoccia, B., Kurczynski, T. W., Shulman, L. P. & Gao, W. Abnormal folate metabolism as a risk factor for first-trimester spontaneous abortion. J. Reprod. Med. 53, 207–212 (2008).
Neiger, R., Wise, C., Contag, S., Tumber, M. & Canick, J. First Trimester Bleeding and Pregnancy Outcome in Gravidas with Normal and Low Folate Levels. American Journal of Perinatology 10, 460–462 (2008).
Ronnenberg, A. Preconception folate and vitamin B6 status and clinical spontaneous abortion in Chinese women. Obstetrics Gynecology 100, 107–113 (2002).
George, L. Plasma Folate Levels and Risk of Spontaneous Abortion. JAMA 288, 1867 (2002).
Gindler, J. et al. Folic acid supplements during pregnancy and risk of miscarriage. The Lancet 358, 796–800 (2001).
Duttaroy, A. K. & Basak, S. Maternal Fatty Acid Metabolism in Pregnancy and Its Consequences in the Feto-Placental Development. Front. Physiol. 12, 787848 (2021).
Broughton, D. E. & Moley, K. H. Obesity and female infertility: potential mediators of obesity’s impact. Fertil. Steril. 107, 840–847 (2017).
Sano, M. et al. Palmitic acid activates NLRP3 inflammasome and induces placental inflammation during pregnancy in mice. J. Reprod. Dev. 66, 241–248 (2020).
Jungheim, E. S. et al. Preimplantation exposure of mouse embryos to palmitic acid results in fetal growth restriction followed by catch-up growth in the offspring. Biol. Reprod. 85, 678–683 (2011).
Fei, H. et al. Plasma metabolomic profile and potential biomarkers for missed abortion. Biomed Chromatogr 30, 1942–1952 (2016).
Oliveira, G. B. D. et al. Composition and significance of glycosaminoglycans in the uterus and placenta of mammals. Brazilian Archives of Biology and Technology 58, 512–520 (2015).
Smock, R. G. & Meijers, R. Roles of glycosaminoglycans as regulators of ligand/receptor complexes. Open Biology 8, 180026 (2018).
Vossen, C. Y. et al. Hereditary thrombophilia and fetal loss: a prospective follow-up study. J Thromb. Haemost. 2, 592–596 (2004).
Brosens, J. J. et al. Maternal selection of human embryos in early gestation: Insights from recurrent miscarriage. Semin. Cell Dev. Biol. 131, 14–24 (2022).
Turesheva, A. et al. Recurrent Pregnancy Loss Etiology, Risk Factors, Diagnosis, and Management. Fresh Look into a Full Box. Journal of Clinical Medicine 12, 4074 (2023).
Coomarasamy, A. et al. Micronized vaginal progesterone to prevent miscarriage: a critical evaluation of randomized evidence. Am. J. Obstet. Gynecol. 223, 167–176 (2020).
Harb, H. M., Al-Rshoud, F., Dhillon, R., Harb, M. & Coomarasamy, A. Ethnicity and miscarriage: a large prospective observational study and meta-analysis. Fertility and Sterility 102, e81 (2014).
Ye, X., Baker, P. N. & Tong, C. The updated understanding of advanced maternal age. Fundamental Research 4, 1719–1728 (2024).
Kolte, A. M., Westergaard, D., Lidegaard, O., Brunak, S. & Nielsen, H. S. Chance of live birth: a nationwide, registry-based cohort study. Hum. Reprod. 36, 1065–1073 (2021).
Park, J. Y., Lim, H., Qin, J. & Lee, L. P. Creating mini-pregnancy models in vitro with clinical perspectives. eBioMedicine 95, 104780 (2023).
Turco, M. Y. et al. Trophoblast organoids as a model for maternal–fetal interactions during human placentation. Nature 564, 263–267 (2018).
Liigand, P. et al. Think Negative: Finding the Best Electrospray Ionization/MS Mode for Your Analyte. Analytical Chemistry 89, 5665–5668 (2017).
Pang, Z. et al. Using MetaboAnalyst 5.0 for LC–HRMS spectra processing, multi-omics integration and covariate adjustment of global metabolomics data. Nature Protocols 17, 1735–1761 (2022).
Xia, J., Mandal, R., Sinelnikov, I. V., Broadhurst, D. & Wishart, D. S. MetaboAnalyst 2.0–a comprehensive server for metabolomic data analysis. Nucleic Acids Research 40, W127–W133 (2012).
Acknowledgements
This study is funded by 01/DY2019/P1/12-A27 and 01/DY2019/P1/14-A29. C.W. Ku is supported by the National Medical Research Council, Ministry of Health, Singapore (NMRC/MOH-000596-00). We received partial funding from the Lien Foundation Optimizing Maternal and Child Health Program Fund and the SingHealth Duke-NUS Obstetrics and Gynecology Academic Clinical Program. The funders had no role in study design, data collection, data analysis, data interpretation, or writing of the manuscript. We thank the patients who participated in this study, the nurses for their logistical support and Miss Carol Seah for coordinating the study.
Author information
Authors and Affiliations
Contributions
C.W.K. and Y.H.L conceived this study. T.C.T. and Y.H.L. supervised the study. K.Y.C. performed the statistical analyses. C.W.K., Y.B.T., K.Y.C., C.O.K., S.T.C.N., and Y.H.L. drafted and revised the manuscript critically. All authors reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ku, C.W., Tan, Y.B., Chew, K.Y. et al. Untargeted metabolomics reveals key pathways in miscarriage: steroid, folate, fatty acid & glycosaminoglycan metabolism. npj Womens Health 3, 35 (2025). https://doi.org/10.1038/s44294-025-00085-9
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s44294-025-00085-9