Abstract
Whether light exposure during the day reduces non-visual light effects later in the evening has not been studied in adolescents. We investigate whether afternoon-early evening (AEE) light interventions (130 lx, 2500 lx, 4.5 h, compared to 6.5 lx illuminance) would increase melatonin levels during later evening light exposure (130 lx) in a counterbalanced crossover study with 22 adolescents (14-17 years, 11 female). Contrary to our hypothesis, evening melatonin levels decreased after AEE bright light exposure, while sleepiness and vigilance were unaffected, and skin temperature showed no clear changes. The AEE light had acute alerting effects and bright light exposure in the 32 h before laboratory entry was associated with higher evening melatonin and sleepiness. These findings suggest that bright AEE light increases alertness but may delay melatonin production by interfering with circadian rhythms. The study highlights the complex effects of light timing and its implications for managing adolescents’ light exposure.
Similar content being viewed by others
Introduction
Adolescents are highly susceptible to chronic sleep loss on school days1,2, with an international meta-analysis suggesting that 52% of 14–17-year-olds sleep less than recommended, compared to 25% of adults1. Extensive research has revealed numerous ramifications associated with adolescents’ sleep deprivation, including mental health issues3, increased risk behaviour4, and decreased cognitive functioning5. While adolescents’ sleep need remains stable across adolescence6 (Ø ~9 h7,8), data from several studies indicate that adolescents’ weekday sleep duration decreases as they age (between 10–18 years)9,10,11. This sleep loss is likely associated with a combination of early school/work start times and later bedtimes, often referred to as 'social jetlag'12, triggered by a delay-shift of the 'inner clock' during puberty (see reviews13,14,15). Physiologically, this delay has been linked to a slower build-up of sleep pressure in late compared to early puberty16,17, enabling older adolescents to stay up longer18. The physiological 'ability' to stay up longer tends to converge with greater bedtime autonomy in older adolescents19, facilitating nighttime activities which can have a multifaceted impact on sleep20,21. First, engaging content may prolong bedtime and sleep onset latency by increasing arousal22. Second, nighttime activities are likely to be combined with light exposure13 which can suppress adolescents’ melatonin release, increase alertness, and delay the circadian rhythm significantly23,24,25,26.
Light is the essential synchroniser for humans’ circadian timing system, entraining the inner clock to the environment and playing a significant role in immunological, cognitive, emotional, and sleep-wake regulation (see reviews27,28). Light exposure can delay or advance circadian rhythms profoundly, the direction depending on the individuals’ 'biological time' (e.g., time relative to their melatonin onset) at exposure25,29. The relationship between the timing of a given light exposure and the resulting direction and magnitude of the phase shift, at different points in the circadian cycle, is typically characterised by the phase response curve (PRC)29. Broadly speaking, early morning light advances the circadian phase, and late evening light delays it. The size of the light effect depends on the intensity and wavelength profile of the light30,31 and the individuals’ light sensitivity32 which in turn can be influenced by prior light history33. Brighter light and a higher short-wavelength proportion increase the strength of lights’ impact on the circadian system, particularly in individuals with a higher circadian sensitivity and a lower prior light exposure history. Additionally, light exposure has acute alerting physiological and behavioural effects: bright light can enhance alertness34,35, elevate heart rate31,36, increase core body temperature (CBT) while decreasing peripheral vasodilation37,38, and decrease melatonin release naturally occurring at night23,39,40,41. Converging evidence suggests that these non-visual effects of light in mammals are primarily driven by the intrinsically photosensitive retinal ganglion cells (ipRGCs), expressing the short-wavelength-sensitive photopigment melanopsin30,40,42,43,44. The ipRGCs relay the light information to the 'circadian master clock' located in the suprachiasmatic nuclei (SCN) of the hypothalamus via the retinohypothalamic tract (RHT)45.
Though triggered naturally during puberty, adolescents’ late sleep-wake rhythms are likely exacerbated by an increasing opportunity for ill-timed light exposure behaviour in older adolescents13,46, making light a viable target for circadian interventions. Firstly, a lack of morning light exposure is associated with a later circadian timing in adolescents47,48, likely due to reducing phase-advancing parts of light exposure. Consistent with these findings, bright light interventions in the morning have shown potential for circadian phase advancing in adolescents49,50,51,52, with the limitation that they often have to reduce morning sleep to apply light in the most sensitive phase-advancing hours50 or use special brief light flash devices during sleep49. Furthermore, several studies have demonstrated that night light exposure can acutely attenuate melatonin release, and have phase delaying effects in adolescents20,23,25,53 while electronic device use has been associated with decreased sleep quality54,55,56. However, evening restrictions for smartphone use were shown to be challenging to negotiate with adolescents56. While recent studies have explored dynamic evening lighting to attenuate non-visual responses to light57,58,59, excessively bright light in the home environment remains a widespread problem60,61. Thus, other ways of reducing the alerting and physiological effects of evening light exposure in adolescents should be explored, considering both evening and daylight.
There is a growing body of literature indicating that the circadian amplitude and circadian photosensitivity can adapt depending on the prior light history. Studies in animal models62,63 in vitro ipRGCs64,65 and adults33,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81 suggest that increasing prior daytime light exposure may increase the circadian amplitude and decrease the effects of subsequent light exposure at night. This has been demonstrated for the effects of night light exposure on phase-shifting66,74,75,77, melatonin secretion33,67,69,76,80, and alertness73 in adults. However, it is less clear what role the timing, duration and level of the prior light exposure play in modulating circadian responses, as many of these studies have applied high-contrast long-duration light conditions over multiple days33,66,67,68,70,73,75. Some studies have demonstrated circadian photosensitivity adaptation after morning light exposure77,78, after prior light in the evening81 and via light exposure at night69,79. However, there seems to be a lack of experimental studies investigating prior light exposure in the afternoon and early evening.
In general, only few studies have investigated the effects of afternoon light exposure or lack thereof on the circadian rhythms and sleep of adolescents25,47,48,82,83. Crowley and Eastman25 constructed a PRC based on N = 44 adolescents aged 14–17 years, which showed that two hours of bright light exposure (~5000 lx illuminance) in the afternoon had phase-advancing effects when it lasted up to ~9 h before midsleep time (i.e. up to ~6 pm for an adolescent who habitually goes to bed at ~10:30 pm and wakes up at ~7:30 am). Furthermore, data from field studies involving adolescents have shown an association between increased afternoon bright light exposure and earlier sleep onset83 or earlier sleep offset the next day48.
Although light history has been suggested to influence subsequent circadian photosensitivity67, no study to date has systematically characterised how afternoon and early evening light of different intensities might modulate physiological responses to subsequent late evening light exposure in adolescents. The aim of this study was to investigate whether increasing after-school light exposure could be a viable approach to mitigating the alerting effects of electric light around bedtime in adolescents. We used a counterbalanced crossover study design to test how adolescents’ physiological responses to late evening light exposure depend on prior afternoon to early evening (AEE) light exposure across 3 different light levels. To assess the amount of melatonin produced before sleep, the primary endpoint of this study was salivary melatonin concentration (area under the curve; AUC) during late evening light exposure. We tested the following hypotheses:
A-priori hypotheses
Evening salivary melatonin levels (AUC), subjective sleepiness (Karolinska Sleepiness Scale; KSS), and distal-to-proximal skin temperature gradient (DPG) are elevated, and response speed (Psychomotor Vigilance Task; PVT) is reduced when preceded by the 'moderate' or 'bright' AEE light intervention, compared to 'dim' light.
Post-hoc hypotheses
Subjective sleepiness (KSS) and the distal-to-proximal skin temperature gradient (DPG) are reduced, and response speed (PVT) is elevated during the 'moderate' or 'bright' AEE light intervention, compared to 'dim' light.
Results
22 healthy German-speaking adolescents (14–17 years, mean = 15.91, SD = 1.15 years, 50% female) completed the counterbalanced crossover protocol (see Fig. 1), which was adapted to each individual’s habitual bedtime (HBT). The agreed HBT ranged from 21:00 to 23:30 between individuals (mean = 22:15, SD = 31 min). Table 1 summarises the characteristics of the participants stratified by sex, and Supplementary Table S1 shows the applied inclusion and exclusion criteria. The AEE light intervention stimuli (see Fig. 2A, C) applied between 7.5 and 3 h before each individual’s HBT had approximately equivalent spectral distributions and differed by ~1.3 log10 units in terms of melanopic Equivalent Daylight Illuminance (see Fig. 2B and D). The later evening light exposure stimulus, applied in all sessions between 3 h before HBT and 1.5 h after HBT, was equivalent to the 'moderate' light intervention. The average time courses of the outcome measures per light condition are shown in Fig. 3, while Fig. 4 shows the average light history during the day prior to each experiment, expressed as the percentage above threshold per hour at different illuminance thresholds. For thresholds ≥ 500 lx illuminance, the curves show small peaks throughout the day, likely corresponding to increased access to daylight. Supplementary Table S2 shows the results of the linear mixed model analysis testing for differences in prior 'bright light history' between the experimental conditions.
Adolescent volunteers participated in a 21-day study schedule that included ≥ 5 days of sleep-wake stabilisation with sleep and light monitoring before each of the 3 experimental visits, which were individually scheduled to begin 8 h before HBT and last until 10.5 h after HBT. On average, HBT (0:00 in the protocol) corresponded to 22:15 (SD = 31 min). AEE light interventions lasted from 7.5 h to 3 h before HBT and varied between 'dim', 'moderate' and 'bright' light exposure in a counterbalanced order with illuminance levels of ~6.5 lx, ~130 lx, and ~2500 lx ( ~4 lx, ~80 lx, ~1400 lx mEDI). This was followed by later evening light exposure from 3 h before to 1.5 h after HBT (130 lx illuminance; ~80 lx mEDI). While awake, toilet breaks were scheduled every 1.5 h, and 4 equicaloric meals were provided every 2 h. We obtained half-hourly samples of subjective sleepiness (from 7 h before HBT) and saliva (from 6 h before HBT) until 1 h after HBT, plus a final evening sample taken 1 h and 20 min after HBT. 2 morning samples were taken 5 and 35 min after wake-up. PVT and VCS were administered on arrival as baseline, then 5 times during the protocol at 90 min intervals and the last time 1 h after HBT. Starting 7 h before HBT, skin temperatures were continuously monitored at 60 s intervals. PLR measurements, polysomnography (including KDTs), skin temperature after bedtime and sleep-related questionnaires taken in the morning were not included in this article. Abbreviations: AEE afternoon to early evening, exp. experimental sessions, HBT habitual bedtime (for home sleep), KDT Karolinska Drowsiness Test, KSS Karolinska Sleepiness Scale, mEDI melanopic Equivalent Daylight Illuminance, PLR pupillary light response, PVT Psychomotor Vigilance Task, VCS visual comfort and well-being scales.
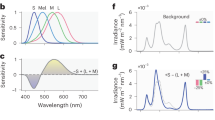
The individual depicted is author R.L., who has given written consent to the publication of this image. A Laboratory setup with the fluorescent ceiling lamp panel during task-free periods (curtains closed). B Spectral irradiance distribution of the 3 AEE light exposure interventions during task-free periods (curtains closed). The vertical light measurements were taken with a spectroradiometer placed at the eye level of the seated participants (115 cm from the floor, 85 cm from the overhead light source, 80 cm from the white curtain, Spectraval 1501, JETI Technische Instrumente GmbH, Jena, Germany, last calibration: 07.03.2023). C Laboratory setup during task performance using an LCD screen with black background and red lettering (curtains open). D Tabulated stimulus specifications per light intervention during the experiment, derived from vertical spectral irradiance measurements on the participants’ eye level with curtains closed and open, including alpha-opic Equivalent Daylight Illuminances (alpha-opic EDIs) and Correlated Colour Temperature (CCT).
A Salivary melatonin concentrations throughout the experimental evening based on data from 20 participants (n = 2 excluded). HBT (0 on the x-axis) on average corresponded to 22:15 (SD = 31 min). Coloured dots show the mean per condition (AEE light intervention), with error bars indicating the standard error. 2 single missing melatonin samples were estimated with linear interpolation (1 sample no. 9 and 13 after the dim and moderate light intervention, respectively). B Subjective sleepiness ratings throughout the experiment based on data from 18 participants (4 excluded). Coloured dots show the mean per condition, with error bars indicating the standard error. C Distal-proximal skin temperature gradient (DPG) throughout the experiment based on data from 21 participants (1 excluded). Coloured dots show the mean value in 30-min bins per condition, with error bars indicating the standard error. The first mean time bin (transition sample not used in LMM) is based on 19 single datapoints during the moderate light intervention,18 single datapoints for the 'bright' light intervention and 17 single datapoints for dim light. D PVT response speed (mean 1/RT) throughout the experiment based on data from 22 participants (0 excluded). Coloured dots show the mean value per condition, with error bars indicating the 95% confidence interval. Values at baseline (BL), not included in the LMM analysis, are based on 18 participants. Abbreviations: AEE afternoon to early evening, BL baseline before light intervention, DPG distal-proximal skin temperature gradient, mEDI melanopic Equivalent Daylight Illuminance, HBT habitual bedtime (for home sleep), KSS Karolinska Sleepiness Scale, PVT Psychomotor Vigilance Task, RT reaction time.
Distribution of light exposure history throughout the day before the experiment, averaged across all participants (n = 22). The y-axis shows the wrist-recorded time above threshold (TAT) in % as a function of the clock time in hours on the x-axis. The different colours code the different wrist-recorded illuminance thresholds. For thresholds ≥ 500 lx, several midday peaks of increased TAT are visible, likely representing school breaks with opportunity for daylight exposure.
Salivary melatonin
For our primary outcome, melatonin AUC during the later evening light exposure, n = 20 participants were included in the linear mixed model (LMM) analysis. Figure 5A shows the median and mean melatonin AUC values as a function of the preceding light intervention, together with the interquartile range (IQR) and individual data points, while Fig. 3A illustrates the average melatonin sample time course per light intervention relative to HBT. A full summary of the melatonin LMM estimates with covariates is given in Table 2, while the summary of the sparse models without covariates is presented in Table 3. Please note, that the intercepts of the sparse models represent the mean melatonin AUC and onset after the 'dim' afternoon-to-evening light condition. In contrast the intercepts of the covariate models (Table 2) represent the expected values when all covariates are set to their reference or zero levels. For the fixed effect estimates we refer to the full models with covariates.
A Evening melatonin AUC in pg/ml/h, across the 3 AEE light intervention conditions, based on data from 20 participants (n = 2 excluded). Single missing evening melatonin samples (n = 2) were estimated by linear interpolation. Coloured diamonds represent the mean melatonin AUC per condition. Coloured box plots show the interquartile range (IQR, box borders), the median (central horizontal line) and the range of minimum and maximum values within 1.5 times the IQR (whiskers). The grey dots mark the melatonin AUC of the individual participants in each condition. The significant difference (p < 0.05) in melatonin AUC between the bright light intervention and dim light in the linear mixed model analysis is indicated by the black asterisk. B Melatonin onset given in clock time, across the 3 AEE light intervention conditions, based on data from 20 participants (n = 2 excluded). Single missing evening melatonin samples (n = 2) were estimated by linear interpolation. Coloured diamonds represent the mean melatonin onset per condition. Coloured box plots show the interquartile range (IQR, box borders), the median (central horizontal line) and the range of minimum and maximum values within 1.5 times the IQR (whiskers). The grey dots mark the melatonin onset of the individual participants in each condition. The significant difference (p < 0.05) in melatonin onset between the bright light intervention and dim light in the linear mixed model analysis is indicated by the black asterisk. Abbreviations: AEE afternoon to early evening, AUC area under the curve, IQR interquartile range, MO melatonin onset.
There was no significant effect on evening melatonin AUC following the moderate AEE light intervention compared to following dim light (β = -7.37, p = 0.114). However, contrary to our hypothesis, there was a significant negative effect following the bright light intervention compared to following dim light (β = -11.29, p = 0.019), i.e. previous bright light until 3 hours before HBT was associated with lower later evening melatonin levels (−11.29 pg/ml/h) compared to previous dim light.
The covariate 'bright light history' (time above 1000 lx threshold; TAT 1000 lx) was a significant predictor in the model (β = 5.65, p = 0.009), indicating that a prolonged exposure to bright light ( > 1000 lx) from the previous day to laboratory entry was associated with an increase in evening melatonin AUC, i.e. 5.65 pg/ml/h per hour spent in above 1000 lx illuminance.
Following these findings, we performed an additional post-hoc analysis of the melatonin onset times (MO), which were determined with the hockey-stick method84, using the same LMM model approach without pre-specified hypotheses. A visualisation of the median and mean melatonin onset with individual data points and IQR, expressed in decimal hours (clock time), is shown in Fig. 5B. There was no significant effect on melatonin onset after the moderate AEE light intervention compared to after dim light (β = 0.30, p = 0.068). However, there was a significant positive effect after the bright light intervention compared to after dim light (β = 0.35, p = 0.037). The bright light intervention between 7.5 and 3 h before HBT was associated with a 21 min later melatonin onset on that evening compared to the previous dim light (summary of the LMM estimates, see Table 2).
The covariate 'bright light history' was a significant predictor in the model (β = −0.16, p = 0.020), indicating that a prolonged exposure to bright light ( > 1000 lx) from the previous day to laboratory entry (~32 h timespan) was associated with an earlier melatonin onset on the experimental evening, i.e. ~10 min (0.16 h) earlier for each hour recorded in above 1000 lx illuminance. These results for melatonin onset are in close alignment with those observed for melatonin AUC.
For completeness, the 2 melatonin values from the next morning were analysed with the same LMM structure and are summarised in the Supplementary Information (see Supplementary Table S3).
Subjective sleepiness
For subjective sleepiness during late evening light exposure, no significant effect was present following the moderate (β = 0.14, p = 0.265) or bright light intervention (β = -0.13, p = 0.320) compared to following dim light. The factor 'time' (median centred) showed a significant positive effect, with later time (1 h increments) being associated with higher reported sleepiness (β = 0.73, p < 0.001). Neither the interaction 'moderate light intervention * time' (β = 0.01, p = 0.958) nor the interaction 'bright light intervention * time' (β = -0.02, p = 0.830) showed a significant effect.
Bright light history was a significant covariate in the model (β = 0.24, p < 0.001), indicating that a prolonged exposure to bright light ( > 1000 lx) from the previous day to laboratory entry was associated with an increase in reported evening sleepiness (0.24 KSS units for every 60 minutes recorded in above 1000 lx illuminance).
As a post-hoc analysis, we further tested the acute light effects on sleepiness during the AEE light intervention, applying the same LMM structure. Significant negative effects were present both during the moderate (β = −0.63, p < 0.001) and bright intervention (β = −0.92, p < 0.001) compared to during the dim light. Factor 'time' showed a significant positive effect, with later time (1-hour increments) being associated with a higher sleepiness level (β = 0.29, p < 0.001). The 'moderate light intervention * time' interaction was not significant (β = 0.08, p = 0.477) compared to the interaction 'dim light * time'. However, the interaction 'bright light intervention * time' yielded a significant negative effect (β = −0.29, p = 0.008), showing that subjective sleepiness increased less over time during the bright light intervention than during dim light (cf. Fig. 3B).
There was no significant effect of the bright light history covariate on sleepiness during the AEE light condition (β = −0.04, p = 0.483).
A full summary of the subjective sleepiness LMM estimates is given in Supplementary Table S4 (sparse models in Supplementary Table S5).
Vigilant attention/response speed
For PVT response speed during the later evening light exposure, there was no significant effect following the moderate AEE light intervention (β = −0.06, p = 0.290) or the bright light intervention (β = −0.04, p = 0.461) compared to after dim light. Factor 'time' (median centred) did not show a significant effect (β = −0.07, p = 0.070). Neither the interaction 'moderate light intervention * time' (β = −0.01, p = 0.846) nor the interaction 'bright light intervention * time' (β = −0.05, p = 0.341) showed a significant effect compared to the interaction 'dim light * time'.
There was no significant effect of the bright light history covariate on response speed during the later evening light exposure (β = −0.04, p = 0.117).
As a post-hoc analysis, we further tested the acute light effects on PVT response speed during the AEE light interventions, applying the same model structure. No significant effect was detectable during the moderate light intervention (β = −0.10, p = 0.163) or bright light intervention (β = −0.09, p = 0.176) compared to during dim light. No significant effect for the factor 'time' (median centred) was detected (β = 0.02, p = 0.622). Neither the interaction 'moderate light intervention * time' (β = 0.01, p = 0.907) nor the interaction 'bright light intervention * time' (β = −0.03, p = 0.617) showed a significant effect compared to the interaction 'dim light * time'.
There was no significant effect of the bright light history covariate on response speed during the AEE light administration (β = −0.04, p = 0.201).
A full summary of the LMM estimates for PVT mean response speed is shown in Supplementary Table S6 (sparse models in Supplementary Table S7). Time courses of PVT measures other than mean response speed (see Fig. 3D) are shown in Supplementary Fig. S1.
Skin temperature (DPG)
Contrary to our hypothesis, there was a significant negative effect on later evening DPG following the moderate light intervention, showing a lower DPG compared to after dim light (β = −0.41, p < 0.001). In contrast to this finding, there was a significant positive effect after the bright light intervention, associated with a higher DPG compared to after dim light (β = 0.49, p < 0.001). Factor 'time' (median centred) did not yield a significant effect (β = 0.07, p = 0.388). Neither the interaction 'moderate light intervention * time' (β = 0.17, p = 0.136) nor the interaction 'bright light intervention * time' (β = 0.05, p = 0.665) showed a significant effect compared to the interaction 'dim light * time'.
There was no significant effect of the bright light history covariate on later evening DPG (β = 0.00, p = 0.994).
As a post-hoc analysis, we further tested the acute light effects on DPG during the AEE light intervention, applying the same LMM structure. A significant negative effect was observed during the moderate AEE light intervention compared to dim light (β = −0.27, p = 0.008). Contrary to those results we found a significant positive effect during the bright light intervention, showing a higher DPG compared to during dim light (β = 0.69, p < 0.001). Factor 'time' (median centred) showed a significant negative effect, with later time (1 h increments) being associated with a lower DPG during the light interventions (β = −0.26, p < 0.001). Neither the interaction 'moderate light intervention * time' (β = −0.09, p = 0.357), nor the interaction 'bright light intervention * time' was significant (β = 0.09, p = 0.374) compared to the interaction 'dim light * time'.
There was no significant effect of the bright light history covariate on DPG during the light interventions (β = −0.02, p = 0.652).
A full summary of the LMM estimates for DPG is given in Supplementary Table S8 (sparse models in Supplementary Table S9). More detailed skin temperature data showing the distal-proximal temperature bands and the distal temperatures in hands and feet are shown in Supplementary Fig. S2, panels A, B and C, while results for room temperature are described in the Supplementary Information and presented in Supplementary Fig. S2 D, E and F. The visual comfort and well-being ratings are shown in Supplementary Figs. S3 and S4).
Discussion
In the present study, we set out to investigate whether increasing after-school light exposure could be a potential strategy for increasing melatonin levels and mitigating the alerting effects of electric light around bedtime in adolescents.
Contrary to our hypothesis, we found evidence that later evening melatonin levels were reduced when preceded by the bright light intervention (7.5 and 3 hours before HBT). We found no effect on evening sleepiness or PVT response speed, but, contrary to our hypothesis, a lower DPG after the moderate light intervention. The bright light intervention resulted in a higher DPG (in line with our hypothesis), but this was confounded by an increased room temperature. Interestingly, the wrist-recorded bright light history of the previous day to the scheduled laboratory session was associated with an earlier melatonin onset, and increased evening melatonin and sleepiness levels.
The most striking finding of this study is that later evening melatonin levels were reduced when preceded by the bright light intervention (7.5 and 3 h before HBT). These results contrast with previous studies that reported increased melatonin levels and decreased alertness following bright light adaptation in adults.
One study based on a similar experimental design in young adult women (n = 12) found a significantly greater increase (pre-post difference) in melatonin during late evening light exposure (750 lx illuminance, 22:30–23:30) when preceded by bright (1200 lx, 18:30–21:00) than when preceded by dim light (5 lx) 81. However, when comparing melatonin AUC, DPG or subjective sleepiness, the authors only report a 'trend' and no statistically significant differences for these conditions81. The discrepancies with our findings may be due to the different samples, light characteristics, their inclusion of a dim light adaptation, or the use of the same clock schedule for all participants as opposed to the individualised times related to HBT in the present study.
Other studies in adults that have found decreased melatonin suppression after light adaptation have used a markedly different timing of prior light exposure. Two reports showed reduced nighttime salivary melatonin suppression after morning exposure to bright light (900 or 2700 lx illuminance)76 or blue light (79 lx)78 compared to dim ( <10 lx) or white (100 lx) light, respectively. Another study found reduced nocturnal plasma melatonin suppression under full-field monochromatic blue light exposure at 460 nm (3.1 and 7 μW/cm²) when preceded by dim light (18 lx, midnight to 2 am) compared to dark adaptation69. Additionally, several studies in adults used earlier and longer-term light exposure protocols over multiple days before testing for differences in melatonin levels33,66,67,68,70,73,75,85, compared with the 4.5 h AEE light intervention in the present study. They found that a day to a week of bright light exposure led to increased nighttime urinary melatonin secretion70,85, blunted melatonin suppression33, increased melatonin amplitude68 and AUC66,68, as well as decreased nocturnal CBT85. Others found a decrease in melatonin suppression after days of moderate light exposure67,73, and increased subjective sleepiness and PVT lapses73.
The discrepancies between these studies and the unexpected later evening melatonin reduction in the present trial may be explained by the timing of our AEE light intervention. It is plausible, that the AEE bright light until 3 h before HBT may have had an acute phase-delaying effect on melatonin release, overriding any potential increase of melatonin secretion amplitude or adaptation of circadian photosensitivity. Consistent with that notion, our post-hoc analysis showed that the preceding bright light intervention was associated with a 21 min later melatonin onset compared to the preceding dim light condition. The moderate light intervention, curiously, did not yield significant results, but indicated the same effect direction on melatonin as the bright light intervention, possibly because our study was underpowered to detect the smaller effect on melatonin after the moderate AEE light intervention.
Interestingly, Crowley and Eastman25 found that exposing adolescents to 2 h of bright light in the late afternoon for 3 consecutive days advanced their dim light melatonin onset by about 25 min. In our study, the late afternoon light exposure occurred around similar clock times on average, but later relative to our participants’ habitual sleep schedule. These differences in relative timing and their repetition across 3 days may explain why, contrary to their findings, we found an acute reduction in melatonin and some indications for an acute phase delay after the AEE bright light intervention. Although the largest proportion of the phase-delaying and melatonin-suppressing effects of light appear to occur within the first hour of exposure86, evidence from young adults29,87 suggests that bright light in the late afternoon may already cause phase delays, which is consistent with our findings.
Curiously, our data showed that the adolescents’ wrist-recorded bright light history from the morning of the previous day to the scheduled laboratory session ( ~32 h period) was positively associated with increased evening melatonin levels, an earlier melatonin onset, and increased subjective sleepiness on the experimental evenings, but not during the afternoon. Thus, in contrast to the very recent prior light history manipulated in the experiment, the bright light history from the day before may have been related to phase advances, paralleled by higher melatonin levels and evening sleepiness. Notably, the recorded ~32 h period of bright light history also covered 2 mornings. Higher levels in bright light history may therefore have contained a greater amount of light exposure in the phase advancing portion of the day. It is also possible that the increased exposure to daylight, which acts as a strong ‘zeitgeber’, synchronised individuals more closely with the natural light-dark cycle and increased the amplitude of their circadian oscillator, resulting in greater evening melatonin production and sleepiness68. These findings may also suggest that the adaptation of circadian photosensitivity in adolescents with regards to melatonin suppression and alertness may not manifest within a couple of hours, as some prior studies in adults have suggested69,81, but rather a couple of days.
Our wrist-recorded bright light history results are consistent with those observed in other studies using ambulatory light history data. This includes a report indicating an association between increased wrist-recorded light exposure in the previous 24 h and earlier sleep onset in adolescents83, a study in elderly people showing that time spent in daylight above 1000 lx illuminance within the previous 48 h was positively related to nocturnal urinary melatonin excretion88, and a study in adult indoor and outdoor workers showing that higher average 24 h wrist-recorded light exposure was associated with a lower percentage of melatonin suppression on experimental evenings80.
We did not observe any effect of the AEE light interventions on later evening sleepiness or PVT response speed. As expected, evening sleepiness increased over time, most likely due to decreasing circadian wake promotion and increasing sleep pressure89,90,91. Even though the adolescents remained awake until 90 min after their HBT and reported high levels of sleepiness, we found no significant effect of time on evening vigilance response speed (mean 1/RT), a measure shown to be sensitive to increasing sleep pressure92. Similarly, Agostini et al.20 only found an effect of time on morning PVT lapses compared to the rest of the day in late- and post-pubertal adolescents. These findings seem plausible in view of previous reports, suggesting that the accumulation of sleep pressure slows down during puberty such that pubertal and post pubertal adolescents have a higher tolerance for staying awake after their HBT16,17,18.
Our findings for evening skin temperature were mixed. We found a reduced DPG after the moderate light compared to dim light, contrary to our hypothesis. These results fall in line with Takasu et al.68 and may suggest that the moderate light intervention sustained sympathetic activation until later in the evening rather than reducing it. In contrast, we found an elevated DPG after the bright light intervention but this effect may have been influenced by a higher ambient room temperature, which has been shown to enhance heat loss through distal regions93,94. This raises uncertainty about whether the higher DPG was due to the light itself or the room temperature and warrants caution in interpreting this result.
In our study, we observed acute alerting responses of moderate and bright AEE light. During the bright light intervention, subjective sleepiness increased less over time compared with dim light, and both the moderate and bright light intervention acutely produced lower subjective sleepiness but did not affect PVT response speed. The light interventions also acutely affected DPG, with lower DPG during the moderate compared to dim light and higher DPG during the bright light intervention.
Several studies, meta-analyses, and reviews have examined the daytime alerting effects of light95,96,97,98,99. A recent mini-review100 summarizes these findings and concludes that different intensities and qualities of light can increase both objective and subjective alertness, increase activity levels, modulate brain responses, and potentially improve cognitive performance during the day100. Siraji et al.95 reported in their review that of the studies investigating bright light exposure, particularly in the afternoon, ~57% (8 out of 14) showed a reduction of subjective sleepiness and only ~17% (1 out of 6) demonstrated a decrease in reaction times. Our study accords with the majority of these studies in showing that the AEE light interventions were effective in acutely inducing subjective alertness but not in terms of PVT reaction time. The acute alerting effect of the moderate AEE light condition contrasts with the absence of its’ effect on later evening melatonin. Light-induced alertness and melatonin differences in the literature have been explained by the mediation via distinct mechanisms with differing spectral sensitivities101. Notably, exposure to short-wavelength light has been shown to enhance alertness without consistent concomitant melatonin suppression102, and vice versa—melatonin suppression may occur in the absence of subjective alerting effects103.
It remains unclear to what extent the reported sleepiness was psychologically influenced by the perception of brightness as participants also clearly perceived the light interventions as being of different brightness (see Supplementary Fig. S3 A, B).
In addition, previous research has indicated a close relationship between thermoregulation and sleepiness regulation104,105,106,107,108 where an increasing DPG reflects the body’s readiness for sleep through core cooling via peripheral vasodilation106. In our data, we found a very small, positive correlation between DPG and sleepiness ratings during the evening light condition. In contrast, sleepiness and DPG showed a small negative correlation during the AEE light intervention, again, likely masked by the higher ambient room temperature93,94. In general, increasing light levels have been shown to decrease DPG37,109 and increase CBT31,38,110 via sympathetic activation111, although these effects may be time-dependent and more pronounced when the circadian timing system promotes sleep37,109,110. Other studies showed contradictory effects of bright light on DPG and CBT93,112,113,114,115, rendering the effects of daytime light exposure on thermoregulation inconclusive.
Consensus lighting recommendations for circadian health in adults suggest that light levels should be dimmed at least 3 h before bedtime116. Conversely, the present findings suggest that reducing light 3 h before HBT may not be early enough for healthy adolescents and that reducing light exposure earlier may be beneficial. Taken together, our data indicate that afternoon exposure to bright light up to 3 h before habitual bedtime has acute alerting and possibly persistent thermoregulatory effects and reduces melatonin levels in adolescents during subsequent light exposure later in the evening, possibly via a circadian phase delay. It may therefore be inappropriate for mitigating the non-visual effects of light around bedtime on the same evening. Notably, while behavioural interventions117,118 and morning light exposure49,50,51,52 have shown some potential, a growing body of evidence indicates that delaying school start times for middle and high school students effectively improves sleep and circadian health119,120,121,122,123,124, suggesting that policy changes are needed to address the widespread problem of inadequate sleep in adolescents125,126.
Despite the insights that can be drawn from this study, we acknowledge several limitations. First, the lack of an evening dim light condition prevented us from determining a dim light melatonin onset (DLMO) and calculating the relative melatonin suppression under later evening moderate light. In addition, although we estimated melatonin onset under moderate light conditions, we did not record salivary melatonin levels over two consecutive evenings, which prevented us from reliably investigating circadian phase shifts in response to the different light conditions. Our primary outcome, melatonin AUC, does not allow us to determine whether the observed reduction in melatonin is due to a delayed onset, acute suppression, changes in amplitude, or a combination of these factors. The visible difference in brightness between the lighting interventions made it impossible to blind participants, despite counterbalancing the order of application. However, this should not have affected objective measures such as our primary outcome melatonin, skin temperature or PVT responses. Furthermore, the bright light intervention was confounded by differences in room temperature, which specifically affected the skin temperature for this condition and limited the interpretation of these results. Finally, our results were based on a rather small sample of healthy adolescents (aged 14–17 years), which limited our ability to test for sex differences and other demographic variations. The sample size and cohort studied, although sufficient to detect significant effects in the present study, may limit the generalisability of our findings to a wider population.
This study also has several strengths. To our knowledge, it is the first controlled experiment to examine the effects of afternoon light exposure on alertness and melatonin levels during subsequent evening light exposure in adolescents. The study was conducted in a well-controlled laboratory setting that allowed precise manipulation and measurement of light exposure, while multimodal monitoring allowed inclusion of relevant covariates such as pre-experimental bright light history. In addition, precise measurement of salivary melatonin with high temporal resolution using a sensitive radioimmunoassay provided accurate estimates of our primary outcome. The within-subject design minimised the confounding effects of individual variability, thereby increasing the accuracy of the results. In addition, the comprehensive multi-stage screening process, which included various health assessments, ensured the inclusion of a healthy sex-balanced sample. Realistic evening and afternoon light levels and after-school hours were used to ensure transferability to real-world contexts while maintaining a high level of experimental control.
Our study highlights the complex effects of differently timed light and emphasises the importance of considering light exposure history when assessing a particular light stimulus. The present data raise the possibility that light history-driven adaptations of circadian photosensitivity may take longer than a few hours to manifest in adolescents. The physiological mechanisms underlying these adaptations are not well understood and there is no consensus on light exposure history in terms of 'how long ago' is meaningful116,127. Further research is needed to clarify how circadian photosensitivity adapts to different patterns of light exposure, including differences in timing, duration and level, and how these effects may differ in different populations, such as age groups. Building on current models for predicting non-visual effects of light40,128,129,130,131,132,133, we propose that future work can then aim to develop complex models that consider the integration of light exposure beyond instantaneous light measurements to more accurately reflect the complex nature of non-visual responses to light.
Methods
Ethics information
This study was carried out in the Centre for Chronobiology in Basel (Switzerland), between September 2022 and July 2023. The experimental protocol, screening questionnaires and consent form were approved by the Ethics Committee northwest/central Switzerland (2022-00432) and pre-registered as a clinical trial (https://clinicaltrials.gov/study/NCT05483296). The study execution strictly adhered to the Declaration of Helsinki, and all the recruited participants and their legal representatives were fully informed with study details and consented in a written form. The individual depicted in the photographs in Fig. 2 and Supplementary Fig. S8 is author R.L., who has provided written consent for the publication of these images.
Participants
A total of 82 students initially expressed interest in participating in the study, of whom a sex-balanced sample (n = 22, 11 female) of healthy German-speaking teenagers (14–17 years) completed the study protocol (see demographics in Table 1). The selection criteria, screening instruments used, and corresponding cut-off points are shown in Supplementary Table S1, while the number of exclusions and withdrawals with their reasons are shown and described in Supplementary Fig. S5. Full participation in the study was compensated with 550 (CHF), or a partial amount in case of dropout. All questionnaires and instructions during the screening and study procedures were administered in German language. If an individual was excluded for non-adherence during the sleep-wake rhythm stabilisation period but had already completed one or more study visits, none of their data were used.
Of the 22 participants who completed the protocol, 5 (23%) were rated as post-pubertal, 11 (50%) as late pubertal, 5 (23%) as mid-pubertal and 1 (4.5%) as early pubertal on the basis of a self-report questionnaire2. 8 of 11 female participants reported a regular menstrual cycle with 2 of them taking hormonal contraception. 2 participants reported an irregular cycle, and 1 did not have a menarche yet.
Study protocol
The study procedure including study sampling and timing is illustrated in Fig. 1. Before each scheduled experimental session, the ambulatory part of the protocol consisted of ≥ 5 days of sleep-wake rhythm stabilisation, during which participants were instructed to adhere to individually agreed target habitual bedtimes (HBT, lights off) and habitual wake times (HWT) within 1 h (±30 min, ≥8 h sleep opportunity window), and to abstain from alcohol, caffeine, and other drugs/medications. The individualised target times were agreed with the adolescent participants and their legal representatives to ensure compatibility with daily life, school, and their habitual sleep-wake rhythm, while requiring 8–10 h sleep opportunity, corresponding to the National Sleep Foundation’s recommendations at that age134, to prevent large sleep debt during the experiment. Adherence was monitored starting ≥ 5 days before each in-lab session, using wrist actimetry (ActTrust 2; Condor Instruments, Brazil) and self-report sleep diaries135. Non-compliance (HBT or HWT deviation of ≥1 h) in more than one night per study week led to exclusion from study participation (see Supplementary Table S1).
During each of the 3 laboratory sessions, participants spent 18.5 h (including sleep) without external time cues such as watches, smartphones and daylight in the light-, temperature- and sound-controlled laboratory facilities of the Centre for Chronobiology, University Psychiatric Clinics in Basel, Switzerland. Baseline room temperature for the laboratories, corridor and toilets were 22 °C with ventilation provided by an automated integrated air conditioning system in the facility. The laboratory sessions were individually scheduled to begin 8 h before HBT and last until 10.5 h after HBT. On entering the laboratory, participants were asked to take a urine-based multi-panel drug test (Nal von Minden; Moers, Germany) and a breathalyser-based alcohol test (ACE X, ACE Instruments; Freilassing, Germany) under bathroom lighting (see Supplementary Table S10), while their previous sleep-wake pattern and caffeine consumption were checked. An in-lab 8-h sleep opportunity window in darkness was scheduled between 1.5 and 9.5 h after the agreed-upon at-home bedtime (HBT). 4 approximately equicaloric meals were provided in 2-h intervals (first meal: 6 h before HBT) with similar food content across participants. In task-free periods, participants were allowed to read and study, play games, or engage in other activities that do not require self-luminous displays (e.g., listening to music and podcasts on provided speakers), but were instructed to remain seated and monitored to keep their eyes open with their sitting posture directed forward. Participants were asked to keep their activities consistent across all 3 experimental sessions. While awake, participants were instructed to take toilet breaks and 3 min walking activity in the corridor, scheduled in 1.5 h intervals. More details on the instructions are given below.
After 8 h of sleep opportunity in darkness (1.5–9.5 h after HBT), participants were awakened in the morning and provided 2 more morning saliva samples, subjective ratings of sleepiness and completed a self-reported sleep quality questionnaire136 within a 30 min time window before showering, eating breakfast and leaving the laboratory.
Instructions for posture, gaze and activities
During the experimental sessions, participants were instructed to keep consistent activities and maintain a consistent seated posture and viewing angle across all conditions. Specifically, our instructions were the following:
-
1.
Seating posture: Sit upright in the designated chair in the marked area, with your back against the backrest and feet flat on the floor.
-
2.
Gaze: Maintain a forward-facing posture, looking straight ahead at the screen during the tasks and forward/downward on the table in the task-free periods.
-
3.
Activities:
-
When reading, writing or using other material, place the book or material on the table at a comfortable reading distance, avoiding excessive tilting or changes in posture. Avoid blocking any light with the material.
-
When using the screen for tasks and instructions, keep your head and eyes aligned with the screen at a natural angle.
-
Maintain consistent activities across all three experimental sessions as much as possible.
-
-
4.
Breaks and movement:
-
Follow scheduled breaks and remain seated during the experimental periods, except for designated walking and toilet breaks.
-
When leaving the room wear the provided red-orange tinted filter goggles to prevent unintended light exposure.
-
These instructions were reinforced throughout the sessions to maintain consistency while allowing for a degree of natural variation, ensuring a balance between experimental control and ecological validity.
Light conditions
During the experiment, the participants received overhead room light exposure from a large (119 cm by 119 cm) fluorescent ceiling lamp panel (Philips Lighting, Eindhoven, The Netherlands), which comprised 2700 K fluorescent tubes (Master TL5 HO 54 W/827) and 17,000 K fluorescent tubes (Master TL5 HO Activiva Active 54 W 1sl). These lamps have been successfully applied in previous studies with young adults in the Centre for Chronobiology137. Despite the increasing prevalence of LED technology, fluorescent lighting remains common in indoor environments. According to recent estimates, fluorescent light sources accounted for ~36.5% of lighting units in the US by the end of 2020138, suggesting that a substantial proportion of fluorescent lighting is still in use.
In the dim light condition, we used a neutral density filter (211, 0.9 ND, LEE Filters Worldwide, Andover, UK) covering the light source to achieve homogenous dim light from the same lamp. The study room was furnished with a white curtain and a white tablecloth directly in front of the participant’s seat to ensure homogeneous light reflection. All walls had a uniform, highly reflective white paint finish, and the floor adjacent to the participant was covered with white fleece (see Fig. 2, Panel A, C).
All three experimental light conditions were conducted with the same fluorescent light panel and had an approximately equivalent spectral composition, with a colour temperature between 4000 K and 4100 K (see Fig. 2, Panel D). Light characteristics were measured vertically with a spectroradiometer placed at the eye level of the seated participants (115 cm from the floor, 85 cm from the overhead light source, 80 cm from the white curtain, Spectraval 1501, JETI Technische Instrumente GmbH, Jena, Germany, last calibration: 07.03.2023). Over the course of an experimental lighting condition, the light level varied by ~5–9%.
Subjective sleepiness, visual comfort and well-being scales, as well as instructions for the auditory psychomotor vigilance test and the Karolinska drowsiness test, were displayed on a 22-inch LCD screen (Samsung SyncMaster 2243EW) with a black background and red lettering (red letters. luminance = 3.20 Cd/m², melanopic EDL = 1.87 Cd/m²) in order not to interfere with the lighting conditions. The screen was hidden behind a white curtain (see Fig. 2, Panel A), and only visible when the screen was in use (see Fig. 2, Panel C). Whenever participants left the study room after the experiment started (for bathroom breaks and pupil measurements), they were instructed to wear red-orange tinted filter goggles (see Supplementary Fig. S6), while all lights along their path were dimmed to avoid aberrant light exposure (illuminance ≤ 6 lx, mEDI ≤ 0.2 lx at eye level, see Supplementary Table S10).
AEE light intervention
The light exposure intervention started in the afternoon after conducting compliance checks, baseline sleepiness, vigilant attention, and pupil measurements (~20 min incl. 3 min dark adaptation, properties shown Supplementary Table S11). Light exposure was consistent in timing and duration across all 3 experimental sessions of a participant, ranging from 7.5 h to 3 h before each participant’s HBT (~3.75 h net light exposure over a 4.5 h period). The 3 experimental AEE light conditions 'dim' 'moderate' and 'bright' differed in light level by approx.1.3 log10-unit steps yielding photopic illuminance levels of ~6.5 lx, ~130 lx and ~2500 lx; (~4 lx, ~80 lx, ~1400 lx mEDI, vertical plane with curtains closed, see Fig. 2). For the conditions 'dim' and 'bright', we chose light exposure conditions that differed as much as possible in light level, while maintaining spectral and colour temperature similarity. The moderate AEE condition was set approximately equidistant in log-units (mEDI) between these two extremes, again while maintaining spectral similarity. To ensure a more stable spectral irradiance output during the AEE light intervention, the fluorescent light source was switched on for a 'warm-up' period 30 min earlier.
The full tabulated spectral power distributions in CSV format for the conditions, displayed in Fig. 2B and in Supplementary Fig. S7 in logarithmic scaling, are provided along with the datasets for analysis (see Code and data availability). Different light units derived from spectral irradiance and radiance values, measured at different angles, directions, and reflection scenarios, are given in Table 4 (irradiance), Supplementary Fig. S8 (radiance), as well as Supplementary Table S12 (radiance). 45 min before the end of the light intervention, a second pupil measurement session was conducted. A summary report about the light conditions using the ENLIGHT checklist139 is provided in Supplementary Table S13.
Later evening light condition
The later evening light exposure ranged from 3 h before HBT to 1.5 h after HBT ( ~4 h net light exposure over a 4.5 h period) and had the same spectrum and light level as the 'moderate' AEE light condition ( ~130 lx illuminance, ~80 lx mEDI, ~4010 K). According to prior literature, the chosen evening light level and duration were biologically effective in acutely suppressing melatonin according to previous research in adults40 and adolescents23. At the same time, although relatively bright, the condition was within a realistic range of common evening domestic lighting conditions60.
Morning light condition
Participants were awakened by switching on a dimmed warm white, fluorescent light source ( ~2800 K, 1.5 lx illuminance, 0.6 lx mEDI at eye level while lying in bed) and 5 min later were seated at a table where they remained for 30 min illuminated by the same light source (~2800 K, 3.9 lx illuminance, 1.6 lx mEDI at eye level while seated).
Salivary melatonin
Saliva samples ( >1 ml) were collected every 30 min from 6 h before HBT until 1 h after HBT, plus a final evening sample taken 1 h and 20 min after HBT (10 min before the experimental bedtime). Two samples were collected in the morning, 5 and 35 min after the experimental wake-up time. In total, 18 samples were collected per session, 7 during the AEE intervention, 9 during the later evening light condition that followed the AEE light intervention, and 2 in the morning.
Melatonin was measured using a direct double antibody radioimmunoassay (RIA, RK-DSM261) with a limit of quantification of 0.9 pg/mL, an analytical sensitivity of 0.2 pg/mL, an intra-assay precision of 7.9% and an inter-assay precision of 9.8%. Measurements were performed by an external service laboratory (NovoLytiX GmbH, Witterswil, Switzerland). The area under the curve (AUC) of salivary melatonin was calculated using the trapezoidal method (AUC function from the 'DescTools' package140) on samples taken during the evening light exposure, starting 3 h before HBT. Additionally, we visualised the time course of melatonin (t1, t2, …tn).
As a post-hoc analysis, the melatonin onset (MO) was determined based on the 16 samples from the afternoon to experiment bedtime and calculated with a piecewise linear-parabolic function using the hockey stick method (v2.5)84 with a default area of interest upper border of 5 pg/ml. When necessary, the default area of interest upper border was adapted based on an individual’s baseline melatonin values, following the procedure of Blume et al.141. R.L. and C.C. independently performed the MO analyses while blinded to the experimental conditions. Divergences were then resolved in a final discussion with F.F.
Subjective sleepiness
Subjective sleepiness was assessed every 30 min using the German version of the single-item 9-point Karolinska Sleepiness Scale (KSS) 142 plus a baseline value immediately after arrival.
Vigilant attention
Reaction time performance of vigilant attention was measured using a modified 5-min auditory version of the Psychomotor Vigilance Test (PVT)143,144. The cues were played at a sound pressure level of 60 dB and for task execution, participants used the space key with their dominant hand to respond. After a response, the next tone was played randomly after 2–9 s. False starts were coded for RTs < 100 ms145 and lapses were coded for RTs ≥ 500 ms. After removing false starts and lapses, response speed (mean 1/RT) was calculated as the outcome of interest, as it was shown to be most sensitive for slight deviations in sleep pressure92. The first test was taken on arrival as a baseline, then 5 times during the protocol at 90 min intervals and the last at a 60 min interval, 30 min before scheduled experimental bedtime (1 h after HBT).
Skin temperature
Starting 7 h before HBT, we continuously monitored skin temperature with 6 surface skin temperature thermocouples146 (BS 1922L Thermochron iButton®, Maxim, US) with 60-s intervals and a 0.0625°C sensitivity. Sensors were placed with air-permeable surgical tape (Fixomull®; Beiersdorf, Hamburg, Germany) on proximal (2 probes, subclavicular area) and distal (4 probes, hands and feet) regions of the body. Skin temperatures (distal & proximal) and the distal-proximal skin temperature gradient (DPG) were calculated accordingly by the author M.D. All raw recordings were visually inspected for each subject and segments where the sensors were either removed or malfunctioning were cleaned out manually. DPG computation during the cleaned periods thus relies on the remaining working probes. In contrast to raw skin temperature data, heat loss mechanisms reflected by the DPG have been shown to remain relatively stable across menstrual phases147,148.
Room temperature was monitored with 1 surface temperature thermocouple, also with 60-s intervals at a 0.0625°C sensitivity, placed in a small cotton sachet 10 cm below the right armrest of the participant’s chair. As for skin temperatures, these recordings were individually inspected to warrant any recording issues.
Ambulatory light history
Light levels at the wrist, expressed in photopic illuminance, were measured at 1-min intervals during the ambulatory monitoring part of the protocol, ≥ 5 days before each experimental session, using wrist-worn actimeters (ActTrust 2, Condor Instruments, Brazil).
Participants were instructed to wear the device continuously and on their non-dominant wrist without sleeves covering it, except when it might get wet or damaged. The recorded illuminance data were pre-processed using the Light Log R package149 in R and corrected by a factor of 1.22 to account for the average difference between the ActTrust 2 devices and a Jeti Spectraval 1501 spectroradiometer (JETI Technische Instrumente GmbH, last calibration: 07.03.2023) measured under the same illuminant as in the experiment at different intensities. Based on the procedure in ref.150, samples below 1 lx, likely due to sleeve covering as well as samples taken during the scheduled bedtime, were excluded from this analysis.
Bright light history was used as a covariate in the mixed linear models to account for participants’ light exposure prior to laboratory entry. It was quantified as the time above the 1000 lx illuminance threshold (TAT 1000 lx) from the previous day’s HWT to the scheduled laboratory session ( ~32 h period). Thus, it incorporated bright light exposure throughout the day before the experiment and from morning until afternoon on the day of the experiment. Similar periods (24–48 h) for prior light exposure have been used and reported to decrease melatonin suppression, increase melatonin secretion, and advance sleep onset in prior studies80,83,88. The average light history during the day prior to each experiment, expressed as time over threshold at different illuminance thresholds, is shown in Fig. 4. However, it is important to note that there are likely to be differences between light exposure at eye level and that measured at the wrist151,152.
Pubertal stage and chronotype
Self-reported pubertal stage153 and chronotype (mid-sleep time corrected for oversleeping)154,155 were assessed as part of the screening procedure and considered as passive stratification covariates in the LMM analyses. Previous reports have shown reduced light-induced melatonin suppression23 and lower melatonin amplitude and AUC156 in late compared to early pubertal stages. Self-reported chronotype has been shown to correlate with dim light melatonin onset and actigraphy-based sleep timing157,158.
Additional measures
Furthermore, a visual comfort and well-being scale (VCS) was employed. Adapted German versions of the first 6 items of a visual comfort scale159 were used to assess the participant’s visual comfort under the different lighting conditions. Additionally, participants rated the subjective room temperature and temperature preference with 2 custom questions, and their momentary affect and well-being in relation to mood, hunger, relaxation, and motivation with 4 questions based on the questionnaire used by Reichert et al.160. These self-reports were administered every 90 min together with the PVT and used to check on the well-being of the participants. Moreover, participants were asked to fill out a daily sleep and daytime diary135. At the end of the last experimental session, participants also filled in a questionnaire assessing their light exposure-related behaviour retrospectively161.
Further measured outcomes that were not included in the analysis of this particular study were pupillary light responses162, polysomnography, Karolinska Drowsiness Tests142, self-reported sleep quality136 and dream recall163.
Design, reproducibility, and statistics
In this within-subject design, all participants received the same 3 experimental conditions but in counterbalanced order. There was a washout period of ≥ 1 week (1 exception of 5 days) between the 3 in-lab sessions to minimise any carry-over effects of the previous sleep-wake behaviour and light condition. Experiments were typically scheduled on the same weekday for consistency. The counter-balanced random assignment to the condition sequence was conducted in separate strata for female and male participants with the 'blockrand' package164 in R. In case of dropouts, the respective 'new' participant was assigned to the same condition sequence as the participant who dropped out.
A total of 22 healthy adolescents (50% female, 50% male, target n = 18 complete data sets) were assigned to one of 6 possible condition sequences. The 4 additionally recruited participants had the same experimental condition order as the first 4, which had missing baseline data and only a third of the samples for subjective sleepiness and missing baseline data for the PVT. Consequently, these first 4 participants were excluded from the subjective sleepiness analysis (n = 18 complete datasets) but not the vigilant attention analysis (n = 22 complete datasets), because the baseline samples were not processed in the LMM analyses.
We excluded n = 2 participants from the melatonin analyses because their maximum evening melatonin levels were lower than their diurnal melatonin fluctuations and no clear onset could be detected (see melatonin profiles in Supplementary Fig. S9). The 9 samples taken during the late evening light condition formed the basis for the primary outcome analysis (melatonin AUC). Participants with single missing evening melatonin samples (n = 2) were included and for AUC calculation, these missing values were estimated by linear interpolation, resulting in a sample of n = 20 for evening melatonin analyses. In the melatonin onset (MO) analysis using the hockey stick method84 the default 'area of interest upper border' of 5 pg/ml had to be adjusted in n = 6 individuals, and in 3 cases, single outlier values before MO (diurnal fluctuations) had to be excluded from the 'hockey stick' fitting. These deviations from the default setting were discussed between R.L. and C.C. and agreed upon in discussion with F.F.
For skin and room temperature, 1 participant had erroneous thermocouple data (resolution = 0.5 instead of 0.0625 °C) and was hence excluded from the analysis. Otherwise, data from 12 single thermocouples (2 in dim light conditions, 1 in bright light condition, 8 in moderate light condition, and 1 room temperature) were compromised and therefore excluded from the analysis. For one participant, room temperature data was not recorded. The missing thermocouples were compensated by using the data from the corresponding sensor on the other side of the body, resulting in a total of n = 21 participants’ DPG datasets for the LMM analysis. The first hour recorded at the start and after the offset of the light intervention (transitional periods) was not included in the LMM analyses. Thus, each LMM, including data recorded during and after the light intervention, respectively, contained a total of 7 30-min DPG bins.
As described in the supplementary information, we found that the room temperature was considerably higher during and after the bright light intervention (see Supplementary Fig. S2 D) compared to the moderate and dim light conditions and was also subjectively rated as slightly but noticeably higher (see Supplementary Fig. S2 E, F). Thus, the DPG and skin temperature results of the bright light intervention need to be interpreted with caution, as the internal validity of the effect of the light level vs. temperature differences is not given.
Statistics
We conducted all statistical analyses in R (4.3.1, R Core Team, 2023)165, using the packages 'lme4'166 and 'lmerTest'167 to test our estimate-specific hypotheses with LMMs. Degrees of freedom for the fixed effects were estimated using Satterthwaite’s approximation and the model was fit using Restricted Maximum Likelihood (REML). As hypothesised a priori, we first tested whether our outcome measures during the later evening light exposure were significantly different (two-sided, p < 0.05) when preceded by the 'bright' or 'moderate' light interventions, compared to 'dim' light. Post-hoc hypotheses were analysed with the same model structure and procedure but—except for melatonin—were based on the data recorded during the AEE light interventions. LMM assumptions were visually inspected with the help of the 'performance' package168 (see Supplementary Figs. S10–S18), which indicated that they were largely met, with some slight violations of the 'normality of residuals' assumption. LMM analyses were nonetheless performed due to the robustness of LMMs to deviations in the distribution assumptions169. Two models were calculated for each of the different outcome variables: a 'covariate' model including the theoretically relevant covariates (see full models below), and a 'sparse' model including only the main effect(s) (see model variables in bold below). The LMMs had the following structure:
We report here, the estimates of the linear mixed model (LMM) analyses from the covariate models. Additional estimates for the sparse models without covariates are reported in Table 3, and Supplementary Tables S3, S5, S7, and S9. The covariate of primary interest was 'bright light history' (TAT 1000 lx) used as a secondary intervention variable, while the other covariates were used as passive stratification factors to control for additional variance. These estimates were not interpreted but are reported in the LMM result tables for completeness. The following variables were modelled as fixed effects: The light intervention conditions (categories 'moderate' and 'bright', relative to 'dim'), bright light history (numeric, 'TAT 1000 lx'), self-reported pubertal stage (categories 'late pubertal', 'midpubertal', and 'early pubertal', relative to 'post-pubertal' stage) and self-reported chronotype (numeric, midpoint of sleep corrected for oversleep, 'MSFSC'). Repeated measures per participant were included as a random factor. For subjective sleepiness, PVT response speed, and DPG, a (median centred) 'time' variable was additionally included in the linear models together with the 'time * AEE light intervention condition' interaction terms to account for the effects of the factor time during the protocol. Median centring for the 'time' variable was performed for each tested period separately (during the AEE light condition and late evening light condition, respectively), so that 'time = 0' refers to the middle of each tested period. This prevented high variance inflation factors (VIFs) between the factor 'time' and the 'time * AEE light intervention condition' interaction term.
Data availability
As part of this publication, the anonymised and de-identified datasets analysed in the current study (https://doi.org/10.6084/m9.figshare.27063514.v1), as well as a laboratory logfile (https://doi.org/10.6084/m9.figshare.27079828.v1), are made publicly available on Figshare under the CC BY-ND 4.0 licence.
Code availability
The statistical analysis code using these datasets is made publicly available on GitHub (https://doi.org/10.5281/zenodo.15551972) under the MIT licence.
References
Kocevska, D. et al. Sleep characteristics across the lifespan in 1.1 million people from the Netherlands, United Kingdom and United States: a systematic review and meta-analysis. Nat. Hum. Behav. 5, 113–122 (2021).
Gariepy, G. et al. How are adolescents sleeping? Adolescent sleep patterns and sociodemographic differences in 24 European and North American countries. J. Adolesc. Health 66, S81–S88 (2020).
Bacaro, V., Miletic, K. & Crocetti, E. A meta-analysis of longitudinal studies on the interplay between sleep, mental health, and positive well-being in adolescents. Int. J. Clin. Health Psychol. 24, 100424 (2024).
Short, M. A. & Weber, N. Sleep duration and risk-taking in adolescents: a systematic review and meta-analysis. Sleep. Med. Rev. 41, 185–196 (2018).
Short, M. A. et al. Cognition and objectively measured sleep duration in children: a systematic review and meta-analysis. Sleep. Health 4, 292–300 (2018).
Ohayon, M. M., Carskadon, M. A., Guilleminault, C. & Vitiello, M. V. Meta-analysis of quantitative sleep parameters from childhood to old age in healthy individuals: developing normative sleep values across the human lifespan. Sleep 27, 1255–73 (2004).
Fuligni, A. J., Bai, S., Krull, J. L. & Gonzales, N. A. Individual differences in optimum sleep for daily mood during adolescence. J. Clin. Child Adolesc. Psychol. 48, 469–479 (2017).
Mercer, P. W., Merritt, S. L. & Cowell, J. M. Differences in reported sleep need among adolescents. J. Adolesc. Health 23, 259–263 (1998).
Galland, B. C. et al. Establishing normal values for pediatric nighttime sleep measured by actigraphy: a systematic review and meta-analysis. Sleep 41, (2018).
Kalak, N., Lemola, S., Brand, S., Holsboer-Trachsler, E. & Grob, A. Sleep duration and subjective psychological well-being in adolescence: a longitudinal study in Switzerland and Norway. Neuropsychiatr. Dis. Treat. 10, 1199–207 (2014).
Iglowstein, I., Jenni, O. G., Molinari, L. & Largo, R. H. Sleep duration from infancy to adolescence: reference values and generational trends. Pediatrics 111, 302–7 (2003).
Wittmann, M., Dinich, J., Merrow, M. & Roenneberg, T. Social jetlag: misalignment of biological and social time. Chronobiol. Int. 23, 497–509 (2006).
Crowley, S. J., Wolfson, A. R., Tarokh, L. & Carskadon, M. A. An update on adolescent sleep: new evidence informing the perfect storm model. J. Adolesc. 67, 55–65 (2018).
Carskadon, M. A. Sleep in adolescents: the perfect storm. Pediatr. Clin. North Am. 58, 637–47 (2011).
Tarokh, L., Short, M., Crowley, S. J., Fontanellaz-Castiglione, C. E. G. & Carskadon, M. A. Sleep and circadian rhythms in adolescence. Curr. Sleep. Med. Rep. 5, 181–192 (2019).
Jenni, O. G., Achermann, P. & Carskadon, M. A. Homeostatic sleep regulation in adolescents. Sleep 28, 1446–54 (2005).
Taylor, D. J., Jenni, O. G., Acebo, C. & Carskadon, M. A. Sleep tendency during extended wakefulness: insights into adolescent sleep regulation and behavior. J. Sleep. Res. 14, 239–44 (2005).
Skeldon, A. C., Derks, G. & Dijk, D.-J. Modelling changes in sleep timing and duration across the lifespan: Changes in circadian rhythmicity or sleep homeostasis?. Sleep. Med. Rev. 28, 96–107 (2016).
Bartel, K. A., Gradisar, M. & Williamson, P. Protective and risk factors for adolescent sleep: a meta-analytic review. Sleep. Med. Rev. 21, 72–85 (2015).
Agostini, A., Carskadon, M. A., Dorrian, J., Coussens, S. & Short, M. A. An experimental study of adolescent sleep restriction during a simulated school week: changes in phase, sleep staging, performance and sleepiness. J. Sleep. Res. 26, 227–235 (2017).
Crowley, S. J. & Carskadon, M. A. Modifications to weekend recovery sleep delay circadian phase in older adolescents. Chronobiol. Int. 27, 1469–92 (2010).
Dworak, M., Schierl, T., Bruns, T. & Strüder, H. K. Impact of singular excessive computer game and television exposure on sleep patterns and memory performance of school-aged children. Pediatrics 120, 978–85 (2007).
Crowley, S. J., Cain, S. W., Burns, A. C., Acebo, C. & Carskadon, M. A. Increased sensitivity of the circadian system to light in early/mid-puberty. J. Clin. Endocrinol. Metab. 100, 4067–73 (2015).
Nagare, R., Rea, M. S., Plitnick, B. & Figueiro, M. G. Nocturnal melatonin suppression by adolescents and adults for different levels, spectra, and durations of light exposure. J. Biol. Rhythms 34, 178–194 (2019).
Crowley, S. J. & Eastman, C. I. Human adolescent phase response curves to bright white light. J. Biol. Rhythms 32, 334–344 (2017).
Höhn, C. et al. Effects of evening smartphone use on sleep and declarative memory consolidation in male adolescents and young adults. Brain Commun. 6, fcae173 (2024).
Golombek, D. A. et al. The times they’re a-changing: effects of circadian desynchronization on physiology and disease. J. Physiol. Paris 107, 310–22 (2013).
Blume, C., Garbazza, C. & Spitschan, M. Effects of light on human circadian rhythms, sleep and mood. Somnologie 23, 147–156 (2019).
Khalsa, S. B. S., Jewett, M. E., Cajochen, C. & Czeisler, C. A. A phase response curve to single bright light pulses in human subjects. J. Physiol. 549, 945–52 (2003).
Brown, T. M. Melanopic illuminance defines the magnitude of human circadian light responses under a wide range of conditions. J. Pineal Res. 69, 12655 (2020).
Cajochen, C. et al. High sensitivity of human melatonin, alertness, thermoregulation, and heart rate to short wavelength light. J. Clin. Endocrinol. Metab. 90, 1311–6 (2005).
Chellappa, S. L. Individual differences in light sensitivity affect sleep and circadian rhythms. Sleep 44, zsaa214 (2021).
Hébert, M., Martin, S. K., Lee, C. & Eastman, C. I. The effects of prior light history on the suppression of melatonin by light in humans. J. Pineal Res. 33, 198–203 (2002).
Lockley, S. W. et al. Short-wavelength sensitivity for the direct effects of light on alertness, vigilance, and the waking electroencephalogram in humans. Sleep 29, 161–8 (2006).
Cajochen, C., Zeitzer, J. M., Czeisler, C. A. & Dijk, D.-J. Dose-response relationship for light intensity and ocular and electroencephalographic correlates of human alertness. Behav. Brain Res. 115, 75–83 (2000).
Scheer, F. A. J. L., van Doornen, L. J. P. & Buijs, R. M. Light and diurnal cycle affect human heart rate: Possible role for the circadian pacemaker. J. Biol. Rhythms 14, 202–212 (1999).
Lok, R. et al. Bright light decreases peripheral skin temperature in healthy men: A forced desynchrony study under dim and bright light (II). J. Biol. Rhythms 37, 417–428 (2022).
Dijk, D.-J., Cajochen, C. & Borbély, A. A. Effect of a single 3-hour exposure to bright light on core body temperature and sleep in humans. Neurosci. Lett. 121, 59–62 (1991).
Lewy, A. J., Wehr, T. A., Goodwin, F. K., Newsome, D. A. & Markey, S. P. Light suppresses melatonin secretion in humans. Science 210, 1267–9 (1980).
Giménez, M. et al. Predicting melatonin suppression by light in humans: unifying photoreceptor-based equivalent daylight illuminances, spectral composition, timing and duration of light exposure. J. Pineal Res. 12786 https://doi.org/10.1111/jpi.12786 (2022).
Gooley, J. J. et al. Exposure to room light before bedtime suppresses melatonin onset and shortens melatonin duration in humans. J. Clin. Endocrinol. Metab. 96, E463–E472 (2011).
Spitschan, M. Melanopsin contributions to non-visual and visual function. Curr. Opin. Behav. Sci. 30, 67–72 (2019).
Berson, D. M., Dunn, F. A. & Takao, M. Phototransduction by retinal ganglion cells that set the circadian clock. Science 295, 1070–1073 (2002).
Cajochen, C., Stefani, O., Schöllhorn, I., Lang, D. & Chellappa, S. L. Influence of evening light exposure on polysomnographically assessed night-time sleep: a systematic review with meta-analysis. Light. Res. Technol. 147715352210787 https://doi.org/10.1177/14771535221078765 (2022).
Baver, S. B., Pickard, G. E., Sollars, P. J. & Pickard, G. E. Two types of melanopsin retinal ganglion cell differentially innervate the hypothalamic suprachiasmatic nucleus and the olivary pretectal nucleus. Eur. J. Neurosci. 27, 1763–1770 (2008).
Roenneberg, T. & Merrow, M. Entrainment of the human circadian clock. Cold Spring Harb. Symposia Quant. Biol. 72, 293–299 (2007).
Figueiro, M. G. et al. Measuring circadian light and its impact on adolescents. Light Res. Technol. 43, 201–215 (2011).
Gasperetti, C. E., Dolsen, M. R. & Harvey, A. G. The influence of intensity and timing of daily light exposure on subjective and objective sleep in adolescents with an evening circadian preference. Sleep. Med. 79, 166–174 (2021).
Kaplan, K. A. et al. Effect of light flashes vs sham therapy during sleep with adjunct cognitive behavioral therapy on sleep quality among adolescents: a randomized clinical trial. JAMA Netw. Open 2, e1911944 (2019).
Misiunaite, I., Eastman, C. I. & Crowley, S. J. Circadian phase advances in response to weekend morning light in adolescents with short sleep and late bedtimes on school nights. Front. Neurosci. 14, 99 (2020).
Crowley, S. J., Fournier, C. L. & Eastman, C. I. Late bedtimes prevent circadian phase advances to morning bright light in adolescents. Chronobiol. Int. 35, 1748–1752 (2018).
Crowley, S. J., Poole, E., Adams, J. & Eastman, C. I. Extending weeknight sleep duration in late-sleeping adolescents using morning bright light on weekends: a 3-week maintenance study. SLEEP Adv. zpae065 https://doi.org/10.1093/sleepadvances/zpae065 (2024).
van der Lely, S. et al. Blue blocker glasses as a countermeasure for alerting effects of evening light-emitting diode screen exposure in male teenagers. J. Adolesc. Health 56, 113–9 (2015).
Carter, B., Rees, P., Hale, L., Bhattacharjee, D. & Paradkar, M. S. Association between portable screen-based media device access or use and sleep outcomes: a systematic review and meta-analysis. JAMA Pediatr. 170, 1202–1208 (2016).
Perrault, A. A. et al. Reducing the use of screen electronic devices in the evening is associated with improved sleep and daytime vigilance in adolescents. Sleep 42 (2019).
Bartel, K. A., Scheeren, R. & Gradisar, M. Altering adolescents’ pre-bedtime phone use to achieve better sleep health. Health Commun. 34, 456–462 (2019).
Wen, P. et al. Optimizing residential light environments in simulated youth olympic village for improving young athletes’ sleep quality and reducing next-morning drowsiness. Build. Environ. 261, 111749 (2024).
Rahman, S. A., St Hilaire, M. A. & Lockley, S. W. The effects of spectral tuning of evening ambient light on melatonin suppression, alertness and sleep. Physiol. Behav. 177, 221–229 (2017).
Stefani, O. et al. Changing color and intensity of LED lighting across the day impacts on circadian melatonin rhythms and sleep in healthy men. J. Pineal Res. 12714 https://doi.org/10.1111/jpi.12714 (2020).
Cain, S. W. et al. Evening home lighting adversely impacts the circadian system and sleep. Sci. Rep. 10, 19110 (2020).
Higuchi, S., Nagafuchi, Y., Lee, S.-I. & Harada, T. Influence of light at night on melatonin suppression in children. J. Clin. Endocrinol. Metab. 99, 3298–303 (2014).
Bano-Otalora, B. et al. Bright daytime light enhances circadian amplitude in a diurnal mammal. Proc. Natl. Acad. Sci. USA 118, 2100094118 (2021).
Hannibal, J., Georg, B., Hindersson, P. & Fahrenkrug, J. Light and darkness regulate melanopsin in the retinal ganglion cells of the Albino Wistar Rat. J. Mol. Neurosci. 27, 147–156 (2005).
Wong, K. Y., Dunn, F. A. & Berson, D. M. Photoreceptor adaptation in intrinsically photosensitive retinal ganglion cells. Neuron 48, 1001–10 (2005).
Do, M. T. H. & Yau, K.-W. Adaptation to steady light by intrinsically photosensitive retinal ganglion cells. Proc. Natl. Acad. Sci. USA 110, 7470–5 (2013).
Hashimoto, S. et al. Midday exposure to bright light changes the circadian organization of plasma melatonin rhythm in humans. Neurosci. Lett. 221, 89–92 (1997).
Smith, K. A., Schoen, M. W. & Czeisler, C. A. Adaptation of human pineal melatonin suppression by recent photic history. J. Clin. Endocrinol. Metab. 89, 3610–3614 (2004).
Takasu, N. N. et al. Repeated exposures to daytime bright light increase nocturnal melatonin rise and maintain circadian phase in young subjects under fixed sleep schedule. Am. J. Physiol. Regul. Integr. Comp. Physiol. 291, 1799–807 (2006).
Jasser, S. A., Hanifin, J. P., Rollag, M. D. & Brainard, G. C. Dim light adaptation attenuates acute melatonin suppression in humans. J. Biol. Rhythms 21, 394–404 (2006).
Park, S. J. & Tokura, H. Bright light exposure during the daytime affects circadian rhythms of urinary melatonin and salivary immunoglobulin A. Chronobiol. Int. 16, 359–71 (1999).
Higuchi, S., Motohashi, Y., Ishibashi, K. & Maeda, T. Less exposure to daily ambient light in winter increases sensitivity of melatonin to light suppression. Chronobiol. Int. 24, 31–43 (2007).
Danilenko, K. V., Plisov, I. L., Wirz-Justice, A. & Hebert, M. Human retinal light sensitivity and melatonin rhythms following four days in near darkness. Chronobiol. Int. 26, 93–107 (2009).
Chang, A.-M., Scheer, F. A. J. L., Czeisler, C. A. & Aeschbach, D. Direct effects of light on alertness, vigilance, and the waking electroencephalogram in humans depend on prior light history. Sleep 36, 1239–46 (2013).
Dijk, D.-J. et al. Amplitude reduction and phase shifts of melatonin, cortisol and other circadian rhythms after a gradual advance of sleep and light exposure in humans. PLoS One7, 30037 (2012).
Chang, A.-M., Scheer, F. A. J. L. & Czeisler, C. A. The human circadian system adapts to prior photic history. J. Physiol. 589, 1095–102 (2011).
Kozaki, T., Kubokawa, A., Taketomi, R. & Hatae, K. Effects of day-time exposure to different light intensities on light-induced melatonin suppression at night. J. Physiol. Anthropol. 34, 27 (2015).
Münch, M. et al. Blue-enriched morning light as a countermeasure to light at the wrong time: effects on cognition, sleepiness, sleep, and circadian phase. NPS 74, 207–218 (2016).
Kozaki, T., Kubokawa, A., Taketomi, R. & Hatae, K. Light-induced melatonin suppression at night after exposure to different wavelength composition of morning light. Neurosci. Lett. 616, 1–4 (2016).
Lee, S.-I. et al. Melatonin suppression during a simulated night shift in medium intensity light is increased by 10-minute breaks in dim light and decreased by 10-minute breaks in bright light. Chronobiol. Int. 37, 897–909 (2020).
Rufiange, M., Beaulieu, C., Lachapelle, P. & Dumont, M. Circadian light sensitivity and rate of retinal dark adaptation in indoor and outdoor workers. J. Biol. Rhythms 22, 454–457 (2007).
te Kulve, M., Schlangen, L. J. M. & van Marken Lichtenbelt, W. D. Early evening light mitigates sleep compromising physiological and alerting responses to subsequent late evening light. Sci. Rep. 9, 16064 (2019).
Galina, S. D., Souza, J. C., Valdez, P. & Azevedo, C. V. M. Daily light exposure, sleep-wake cycle and attention in adolescents from different urban contexts. Sleep. Med. 81, 410–417 (2021).
da Costa Lopes, L., Ribeiro da Silva Vallim, J., Tufik, S., Louzada, F. & D’Almeida, V. Associations between real-life light exposure patterns and sleep behaviour in adolescents. J. Sleep Res. e14315 https://doi.org/10.1111/jsr.14315 (2024).
Danilenko, K. V., Verevkin, E. G., Antyufeev, V. S., Wirz-Justice, A. & Cajochen, C. The hockey-stick method to estimate evening dim light melatonin onset (DLMO) in humans. Chronobiol. Int. 31, 349–55 (2014).
Kanikowska, D., Hirata, Y., Hyun, K. & Tokura, H. Acute phase proteins, body temperature and urinary melatonin under the influence of bright and dim light intensities during the daytime. J. Physiol. Anthropol. 20, 333–338 (2001).
Chang, A.-M. et al. Human responses to bright light of different durations. J. Physiol. 590, 3103–3112 (2012).
St Hilaire, M. A. et al. Human phase response curve to a 1 h pulse of bright white light. J. Physiol. 590, 3035–45 (2012).
Obayashi, K. et al. Positive effect of daylight exposure on nocturnal urinary melatonin excretion in the elderly: a cross-sectional analysis of the HEIJO-KYO study. J. Clin. Endocrinol. Metab. 97, 4166–4173 (2012).
Silva, E. J., Wang, W., Ronda, J. M., Wyatt, J. K. & Duffy, J. F. Circadian and wake-dependent influences on subjective sleepiness, cognitive throughput, and reaction time performance in older and young adults. Sleep 33, 481–490 (2010).
Åkerstedt, T., Anund, A., Axelsson, J. & Kecklund, G. Subjective sleepiness is a sensitive indicator of insufficient sleep and impaired waking function. J. Sleep. Res. 23, 242–254 (2014).
Monk, T. H. Subjective ratings of sleepiness—the underlying circadian mechanisms. Sleep 10, 343–353 (1987).
Basner, M. & Dinges, D. F. Maximizing sensitivity of the psychomotor vigilance test (PVT) to sleep loss. Sleep 34, 581–91 (2011).
te Kulve, M., Schlangen, L. J. M., Schellen, L., Frijns, A. J. H. & van Marken Lichtenbelt, W. D. The impact of morning light intensity and environmental temperature on body temperatures and alertness. Physiol. Behav. 175, 72–81 (2017).
Martinez-Nicolas, A. et al. Daytime variation in ambient temperature affects skin temperatures and blood pressure: ambulatory winter/summer comparison in healthy young women. Physiol. Behav. 149, 203–211 (2015).
Siraji, M. A., Kalavally, V., Schaefer, A. & Haque, S. Effects of daytime electric light exposure on human alertness and higher cognitive functions: a systematic review. Front. Psychol. 12, 765750 (2022).
Lok, R., Smolders, K. C. H. J., Beersma, D. G. M. & Kort, Y. A. W. Light, alertness, and alerting effects of white light: a literature overview. J. Biol. Rhythms 33, 589–601 (2018).
Cajochen, C. Alerting effects of light. Sleep. Med. Rev. 11, 453–464 (2007).
Souman, J. L., Tinga, A. M., Te Pas, S. F., van Ee, R. & Vlaskamp, B. N. S. Acute alerting effects of light: a systematic literature review. Behav. Brain Res. 337, 228–239 (2018).
Xu, Q. & Lang, C. P. Revisiting the alerting effect of light: a systematic review. Sleep. Med Rev. 41, 39–49 (2018).
Stefani, O., Schöllhorn, I. & Münch, M. Towards an evidence-based integrative lighting score: a proposed multi-level approach. Ann. Med. 56, 2381220 (2024).
Revell, V. L., Arendt, J., Fogg, L. F. & Skene, D. J. Alerting effects of light are sensitive to very short wavelengths. Neurosci. Lett. 399, 96–100 (2006).
Figueiro, M. G., Sahin, L., Wood, B. & Plitnick, B. Light at night and measures of alertness and performance: implications for shift workers. Biol. Res. Nurs. 18, 90–100 (2016).
Blume, C. et al. Melatonin suppression does not automatically alter sleepiness, vigilance, sensory processing, or sleep. Sleep 45, zsac199 (2022).
Kräuchi, K., Cajochen, C., Pache, M., Flammer, J. & Wirz-Justice, A. Thermoregulatory effects of melatonin in relation to sleepiness. Chronobiol. Int. 23, 475–484 (2006).
Lok, R., van Koningsveld, M. J., Gordijn, M. C. M., Beersma, D. G. M. & Hut, R. A. Daytime melatonin and light independently affect human alertness and body temperature. J. Pineal Res. 67, 12583 (2019).
Kräuchi, K. The thermophysiological cascade leading to sleep initiation in relation to phase of entrainment. Sleep. Med. Rev. 11, 439–451 (2007).
Kräuchi, K., Cajochen, C., Möri, D., Graw, P. & Wirz-Justice, A. Early evening melatonin and S-20098 advance circadian phase and nocturnal regulation of core body temperature. Am. J. Physiol. 272, 1178–88 (1997).
Kräuchi, K., Cajochen, C. & Wirz-Justice, A. Thermophysiologic aspects of the three-process-model of sleepiness regulation. Clin. Sports Med. 24, 287–300 (2005).
Harmsen, J.-F. et al. The influence of bright and dim light on substrate metabolism, energy expenditure and thermoregulation in insulin-resistant individuals depends on time of day. Diabetologia https://doi.org/10.1007/s00125-021-05643-9 (2022).
Rüger, M., Gordijn, M. C. M., Beersma, D. G. M., Vries, B. & Daan, S. Time-of-day-dependent effects of bright light exposure on human psychophysiology: comparison of daytime and nighttime exposure. 290, R1413–20 (2006).
Saito, Y. et al. Effect of bright light exposure on muscle sympathetic nerve activity in human. Neurosci. Lett. 219, 135–137 (1996).
Zhang, P. & Tokura, H. Thermoregulatory responses in humans during exercise after exposure to two different light intensities. Eur. J. Appl. Physiol. 79, 285–289 (1999).
Foret, J., Aguirre, A., Touitou, Y., Clodoré, M. & Benoit, O. Effect of morning bright light on body temperature, plasma cortisol and wrist motility measured during 24 h of constant conditions. Neurosci. Lett. 155, 155–158 (1993).
Seika, A. & Hiromi, T. The influence of bright light exposure for several hours during daytime on tympanic temperature level at sweating onset. J. Therm. Biol. 23, 99–106 (1998).
Aizawa, S. & Tokura, H. Influence of bright light exposure for several hours during the daytime on cutaneous vasodilatation and local sweating induced by an exercise heat load. Eur. J. Appl. Physiol. 78, 303–307 (1998).
Brown, T. M. et al. Recommendations for daytime, evening, and nighttime indoor light exposure to best support physiology, sleep, and wakefulness in healthy adults. PLoS Biol. 20, 3001571 (2022).
Gadam, S. et al. Interventions to increase sleep duration in young people: a systematic review. Sleep Med. Rev. 101807 https://doi.org/10.1016/j.smrv.2023.101807 (2023).
Griggs, S., Conley, S., Batten, J. & Grey, M. A systematic review and meta-analysis of behavioral sleep interventions for adolescents and emerging adults. Sleep. Med. Rev. 54, 101356 (2020).
Meltzer, L. J., Wahlstrom, K. L., Plog, A. E. & Strand, M. J. Changing school start times: impact on sleep in primary and secondary school students. Sleep 44, zsab048 (2021).
Berry, K. M. et al. Association of delaying school start time with sleep-wake behaviors among adolescents. J. Adolesc. Health 69, 831–837 (2021).
Borisenkov, M. F. et al. Later school start time is associated with better academic performance, sleep-wake rhythm characteristics, and eating behavior. Chronobiol. Int. 39, 1444–1453 (2022).
de Araújo, L. B. G., Bianchin, S., Pedrazzoli, M., Louzada, F. M. & Beijamini, F. Multiple positive outcomes of a later school starting time for adolescents. Sleep. Health 8, 451–457 (2022).
Yip, T. et al. School start times, sleep, and youth outcomes: a meta-analysis. Pediatrics 149, e2021054068 (2022).
Chan, C. S., Tang, M. C., Leung, J. C. Y., Poon, C. Y. S. & Lau, E. Y. Y. Delayed school start time is associated with better sleep, mental health, and life satisfaction among residential high-school students: a prospective study. Sleep zsae171 https://doi.org/10.1093/sleep/zsae171 (2024).
Watson, N. F. et al. Delaying middle school and high School start times promotes student health and performance: An American Academy of Sleep Medicine position statement. J. Clin. Sleep. Med. 13, 623–625 (2017).
Johnson, K. G. & Malow, B. A. Implications of sleep health policy: daylight saving and school start times. Continuum: Lifelong Learn. Neurol. 29, 1253 (2023).
Münch, M. et al. The role of daylight for humans: gaps in current knowledge. Clocks Sleep. 2, 61–85 (2020).
St. Hilaire, M. A., Lammers-van der Holst, H. M., Chinoy, E. D., Isherwood, C. M. & Duffy, J. F. Prediction of individual differences in circadian adaptation to night work among older adults: application of a mathematical model using individual sleep-wake and light exposure data. Chronobiol. Int. 37, 1404–1411 (2020).
Mayer, C., Walch, O., Forger, D. B. & Hannay, K. Impact of light schedules and model parameters on the circadian outcomes of individuals. J. Biol. Rhythms 38, 379–391 (2023).
Huang, Y. et al. Predicting circadian phase across populations: a comparison of mathematical models and wearable devices. Sleep 44, zsab126 (2021).
Murray, J. M. et al. Light-based methods for predicting circadian phase in delayed sleep-wake phase disorder. Sci. Rep. 11, 10878 (2021).
Cheng, P. et al. Predicting circadian misalignment with wearable technology: validation of wrist-worn actigraphy and photometry in night shift workers. Sleep 44, (2021).
Usmani, I. M., Dijk, D.-J. & Skeldon, A. C. Mathematical analysis of light-sensitivity related challenges in assessment of the intrinsic period of the human circadian pacemaker. J. Biol. Rhythms 39, 166–182 (2024).
Hirshkowitz, M. et al. National Sleep Foundation’s updated sleep duration recommendations: final report. Sleep. Health 1, 233–243 (2015).
Carney, C. E. et al. The consensus sleep diary: standardizing prospective sleep self-monitoring. Sleep 35, 287–302 (2012).
Parrott, A. C. & Hindmarch, I. The Leeds Sleep Evaluation Questionnaire in psychopharmacological investigations—a review. Psychopharmacology 71, 173–179 (1980).
Gabel, V. et al. Differential impact in young and older individuals of blue-enriched white light on circadian physiology and alertness during sustained wakefulness. Sci. Rep. 7, 7620 (2017).
Lee, K., Donnelly, S. & Phillips, G. 2020 US Lighting Market Characterization. (2024).
Spitschan, M., Kervezee, L., Lok, R., McGlashan, E. & Najjar, R. P. ENLIGHT: A consensus checklist for reporting laboratory-based studies on the non-visual effects of light in humans. EBioMedicine 98, 104889 (2023).
Signorell, A. DescTools: Tools for descriptive statistics. (2024).
Blume, C., Cajochen, C., Schöllhorn, I., Slawik, H. C. & Spitschan, M. Effects of calibrated blue-yellow changes in light on the human circadian clock. Nat. Hum. Behav. https://doi.org/10.1038/s41562-023-01791-7 (2023).
Akerstedt, T. & Gillberg, M. Subjective and objective sleepiness in the active individual. Int J. Neurosci. 52, 29–37 (1990).
Dinges, D. F. & Powell, J. W. Microcomputer analyses of performance on a portable, simple visual RT task during sustained operations. Behav. Res. Methods Instrum. Comput. 17, 652–655 (1985).
Chellappa, S. L. et al. Non-visual effects of light on melatonin, alertness and cognitive performance: Can blue-enriched light keep us alert?. PLOS ONE 6, 16429 (2011).
Sinclair, K. L., Ponsford, J. L., Rajaratnam, S. M. W. & Anderson, C. Sustained attention following traumatic brain injury: use of the psychomotor vigilance task. J. Clin. Exp. Neuropsychol. 35, 210–24 (2013).
van Marken Lichtenbelt, W. D. et al. Evaluation of wireless determination of skin temperature using iButtons. Physiol. Behav. 88, 489–497 (2006).
Kräuchi, K. et al. Diurnal and menstrual cycles in body temperature are regulated differently: A 28-day ambulatory study in healthy women with thermal discomfort of cold extremities and controls. Chronobiol. Int. 31, 102–113 (2014).
Shechter, A., Boudreau, P., Varin, F. & Boivin, D. B. Predominance of Distal Skin Temperature Changes at Sleep Onset across Menstrual and Circadian Phases. J. Biol. Rhythms 26, 260–270 (2011).
Zauner et al. LightLogR: Working with wearable light logger data. (2023).
Hand, A. J. et al. Measuring light regularity: Sleep regularity is associated with regularity of light exposure in adolescents. Sleep 46, zsad001 (2023).
Aarts, M. P. J., van Duijnhoven, J., Aries, M. B. C. & Rosemann, A. L. P. Performance of personally worn dosimeters to study non-image forming effects of light: Assessment methods. Build. Environ. 117, 60–72 (2017).
Stampfli et al. The light-dosimeter: a new device to help advance research on the non-visual responses to light. Light. Res. Technol. 147715352211471 https://doi.org/10.1177/14771535221147140 (2023).
Carskadon, M. A. & Acebo, C. A self-administered rating scale for pubertal development. J. Adolesc. Health 14, 190–195 (1993).
Roenneberg, T., Wirz-Justice, A. & Merrow, M. Life between clocks: daily temporal patterns of human chronotypes. J. Biol. Rhythms 18, 80–90 (2003).
Ghotbi, N. et al. The µMCTQ: an ultra-short version of the Munich ChronoType Questionnaire. J. Biol. Rhythms 35, 98–110 (2020).
Crowley, S. J., Acebo, C. & Carskadon, M. A. Human puberty: salivary melatonin profiles in constant conditions. Dev. Psychobiol. 54, 468–73 (2012).
Reiter, A. M., Sargent, C. & Roach, G. D. Finding DLMO: estimating dim light melatonin onset from sleep markers derived from questionnaires, diaries and actigraphy. Chronobiol. Int. 37, 1412–1424 (2020).
McHill, A. W. et al. Robust stability of melatonin circadian phase, sleep metrics, and chronotype across months in young adults living in real-world settings. J. Pineal Res. 70, e12720 (2021).
Spitschan, M., Lazar, R., Yetik, E. & Cajochen, C. No evidence for an S cone contribution to acute neuroendocrine and alerting responses to light. Curr. Biol. 29, 1297–1298 (2019).
Reichert, C. F. et al. Wide awake at bedtime? Effects of caffeine on sleep and circadian timing in male adolescents—a randomized crossover trial. Biochem. Pharmacol. 191, 114283 (2021).
Siraji, M. A. et al. An inventory of human light exposure behaviour. Sci. Rep. 13, 22151 (2023).
Spitschan, M. & Woelders, T. The method of silent substitution for examining melanopsin contributions to pupil control. Front. Neurol. 9, 941 (2018).
Chellappa, S. L., Münch, M., Blatter, K., Knoblauch, V. & Cajochen, C. Does the circadian modulation of dream recall modify with age?. Sleep 32, 1201–1209 (2009).
Snow, G. & Snow, M. G. Package ‘blockrand’. The Comprehensive R Archive Network (2013).
R Core Team. R: A Language and Environment for Statistical Computing. (R Foundation for Statistical Computing, 2023).
Bates, D., Mächler, M., Bolker, B. & Walker, S. Fitting linear mixed-effects models using lme4. J. Stat. Soft. 67 (2015).
Kuznetsova, A., Brockhoff, P. B. & Christensen, R. H. B. lmerTest package: Tests in linear mixed effects models. J. Stat. Softw. 82, 1–26 (2017).
Lüdecke, D., Ben-Shachar, M. S., Patil, I., Waggoner, P. & Makowski, D. performance: An R package for assessment, comparison and testing of statistical models. J. Open Source Softw. 6, 3139 (2021).
Schielzeth, H. et al. Robustness of linear mixed-effects models to violations of distributional assumptions. Methods Ecol. Evolut. 11, 1141–1152 (2020).
Buysse, D. J., Reynolds, C. F., Monk, T. H., Berman, S. R. & Kupfer, D. J. The Pittsburgh sleep quality index: A new instrument for psychiatric practice and research. Psychiatry Res. 28, 193–213 (1989).
Westreich, D. & Greenland, S. The Table 2 fallacy: Presenting and interpreting confounder and modifier coefficients. Am. J. Epidemiol. 177, 292–298 (2013).
Spitschan, M. et al. Luox: Validated reference open-access and open-source web platform for calculating and sharing physiologically relevant quantities for light and lighting. Wellcome Open Res. 6, 69 (2022).
Acknowledgements
During this work, R.L. received funding from the European Training Network LIGHTCAP (project number 860613) under the Marie Skłodowska-Curie actions framework H2020-MSCA-ITN-2019 and by the Nikolaus and Bertha Burckhardt-Bürgin Foundation. We would like to thank Johannes Zauner for his assistance in computing the wrist-worn bright light history using the LightLogR package, and Christine Blume for her support and providing code for the PVT analysis. Furthermore, we are grateful to Kurt Kräuchi for his valuable comments on skin temperature regulation and to Deborah Vogt for her support with the linear mixed model implementation. We also extend our gratitude to all the study helpers and interns for their contributions to data collection.
Author information
Authors and Affiliations
Contributions
The authors made the following contributions. R. L.: Conceptualization, Data curation, Formal Analysis, Investigation, Methodology, Project administration, Supervision, Validation, Visualization, Writing—original draft, Writing—review & editing; F.F.: Conceptualization, Formal Analysis, Methodology, Writing—review & editing; M. D.: Formal Analysis, Writing—review & editing; C. E.: Investigation, Writing—review & editing; O. S.: Conceptualization, Methodology, Supervision, Writing—review & editing; M.S.: Conceptualization, Formal Analysis, Methodology, Supervision, Writing—review & editing; C. C.: Conceptualization, Formal Analysis, Funding acquisition, Methodology, Project administration, Resources, Supervision, Visualization, Writing—review & editing.
Corresponding author
Ethics declarations
Competing interests
R.L., F.F., M.D. and C.E. do not report any competing interests. O.S. is listed as an inventor on the following patents: ('Display system having a circadian effect on humans', US8646939B2; 'Projection system and method for projecting image content', DE102010047207B4; 'Adaptive lighting system', US8994292B2; 'Projection device and filter therefor', WO2006013041A1; 'Method for the selective adjustment of a desired brightness and/or colour of a specific spatial area, and data processing device', WO2016092112A1). O.S. is a member of the Daylight Academy, Good Light Group and Swiss Lighting Society. O.S. has had the following commercial interests in the last two years (2023–2025) related to lighting: Investigator-initiated research grants from SBB and DFS. M.S. declares the following potential conflicts of interest in the past five years (2021–2025). Academic roles: Member of the Board of Directors, Society of Light, Rhythms, and Circadian Health (SLRCH); Chair of Joint Technical Committee 20 (JTC20) of the International Commission on Illumination (CIE); Member of the Daylight Academy; Chair of Research Data Alliance Working Group Optical Radiation and Visual Experience Data. Remunerated roles: Speaker of the Steering Committee of the Daylight Academy; Ad-hoc reviewer for the Health and Digital Executive Agency of the European Commission; Ad-hoc reviewer for the Swedish Research Council; Associate Editor for LEUKOS, journal of the Illuminating Engineering Society; Examiner, University of Manchester; Examiner, Flinders University; Examiner, University of Southern Norway. Funding: Received research funding and support from the Max Planck Society, Max Planck Foundation, Max Planck Innovation, Technical University of Munich, Wellcome Trust, National Research Foundation Singapore, European Partnership on Metrology, VELUX Foundation, Bayerisch-Tschechische Hochschulagentur (BTHA), BayFrance (Bayerisch-Französisches Hochschulzentrum), BayFOR (Bayerische Forschungsallianz), and Reality Labs Research. Honoraria for talks: Received honoraria from the ISGlobal, Research Foundation of the City University of New York and the Stadt Ebersberg, Museum Wald und Umwelt. Travel reimbursements: Daimler und Benz Stiftung. Patents: Named on European Patent Application EP23159999.4A ('System and method for corneal-plane physiologically-relevant light logging with an application to personalized light interventions related to health and well-being'). C.C. has had the following commercial interests in the last two years (2022–2024) related to lighting: honoraria, travel, accommodation and/or meals for invited keynote lectures, conference presentations or teaching from Toshiba Materials, Velux, Firalux, Lighting Europe, Electrosuisse, Novartis, Roche, Elite, Servier, and WIR Bank. With the exception of the funding source supporting this work, O.S., M.S. and C.C. declare no influence of the disclosed roles or relationships on the work presented herein. The funders had no role in study design, data collection and analysis, decision to publish or preparation of the manuscript.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lazar, R., Fazlali, F., Dourte, M. et al. Afternoon to early evening bright light exposure reduces later melatonin production in adolescents. npj Biol Timing Sleep 2, 25 (2025). https://doi.org/10.1038/s44323-025-00040-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s44323-025-00040-6