Abstract
Patients with Becker muscular dystrophy (BMD) often experience forefoot overload due to abnormal gait patterns, resulting in chronic pain, instability, and ulceration. Conventional orthotic devices frequently fail to accommodate the complex and individualized biomechanical needs of these patients. Here, we introduce a computational framework that integrates finite element analysis, machine learning, and Bayesian optimization to design dual-layer lattice pads adapted to gait-induced pressure distribution. A Gaussian Process Regression model accurately predicted structure–function relationships, enabling efficient multi-objective optimization within a high-dimensional design space. The optimized lattice configuration reduced peak plantar pressure by 51.36% during simulated gait, outperforming previous solutions. Unlike conventional uniform-stiffness insoles, the dual-layer architecture allows gradient mechanical tuning through parametric control, providing enhanced pressure offloading and structural adaptability. This work proposes a computationally scalable and theoretically generalizable framework for precision orthotic design and outlines a pathway for integrating computational biomechanics with AI-informed material engineering in future personalized rehabilitation technologies.
Similar content being viewed by others
Introduction
Becker Muscular Dystrophy (BMD) is an X-linked recessive genetic disorder caused by mutations in the Duchenne muscular dystrophy gene, primarily characterized by progressive muscle degeneration1,2. Although substantial advancements in modern medicine have significantly improved the life expectancy of individuals with BMD3, the progressive decline in muscle function severely compromises the biomechanical function of the foot and gait performance4. Due to dorsiflexor muscle weakness and ankle joint contracture, patients with BMD exhibit reduced activation of the dorsiflexor muscle group during gait5. As a result, these individuals often adopt a forefoot initial contact gait pattern, leading to concentrated plantar pressure in the metatarsal region, which may cause pain and ulceration. Shock-absorbing interventions can mitigate excessive mechanical stress in high-pressure areas, thereby alleviating foot pain and reducing the risk of ulcer formation6. One of the classic strategies for such interventions is the use of metatarsal pads. These pads are typically implemented as supplementary components positioned proximally to the metatarsal heads on the base layer of supportive footwear7,8,9. While a recently published meta-analysis has confirmed the effectiveness of custom-designed metatarsal pads in redistributing plantar pressure10, conventional products are generally constrained by limitations in manufacturing and design approaches, resulting in uniform structural stiffness and suboptimal mechanical adaptability.
In recent years, with advancements in materials engineering and computational mechanics, additive manufacturing (AM) technologies have demonstrated unique advantages in the development of customized medical devices11,12,13. Lattice structures based on computer-aided design (CAD) offer programmable mechanical property gradients, enabling the tuning of macroscopic mechanical responses by adjusting unit cell parameters14, thus providing more targeted cushioning and support effects15,16,17,18. However, current research has predominantly focused on predicting and optimizing structural and material properties using single or discrete parameters19,20,21,22. These approaches typically rely on predefined parameter spaces and seek local optima under specific experimental or simulation conditions. Due to their lack of adaptability, they often fall short in achieving rapid and efficient multi-objective optimization when confronted with unknown or complex personalized requirements. Data-driven approaches enable the development of efficient computational models that can uncover latent patterns within complex structures23. In previous work, we proposed a single-layer parametrized lattice insole that integrates finite element (FE) analysis with machine learning (ML) techniques, demonstrating its potential to reduce peak plantar pressure24. However, the single-layer lattice design did not account for the unique gait characteristics and mechanical demands of patients with neuromuscular disorders.
In this study, a parameter-adjustable, dual-layer lattice-structured metatarsal pad was developed within an FE simulation environment to address the plantar pressure unloading needs in the metatarsal region of patients with BMD. ML techniques were first employed to establish the underlying relationships between structural parameters and their corresponding physical properties, enabling the prediction of unknown data beyond the original dataset. A global optimization of the structural parameters was then performed with the objective of minimizing plantar pressure. To the best of the authors’ knowledge, few existing studies have utilized data-driven approaches for the optimal design of lattice-structured metatarsal pads. This study introduces an innovative design framework that incorporates a dual-layer parametrized lattice architecture. By constructing a response surface model between unit cell geometric parameters and mechanical performance, and integrating FE analysis, ML, and optimization algorithms, the proposed method enables precise control over structural characteristics. Compared to conventional trial-and-error methods, this approach translates patient-specific biomechanical features into quantifiable lattice parameters, thus not only fulfilling targeted shock-absorption requirements for metatarsal unloading but also offering a dynamically adaptive and long-term reliable personalized solution for individuals with other neuromuscular disorders or at high risk of diabetic foot ulceration.
Results
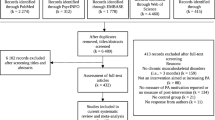
Validation results
As shown in Fig. 1A, no visible local damage was observed on the sample surface when compressed by 5 mm, indicating that the deformation remained within the elastic range. The deformation pattern of the printed samples was consistent with the trends predicted by FE analysis. Furthermore, for the randomly generated parameter samples, the differences between the experimental and simulated reaction forces during compression were 3.2% and 0.4%, respectively, demonstrating the high reliability of the structural FE model. As illustrated in Fig. 1B, the overall Mean Squared Error (MSE) of the Gaussian Process Regression (GPR) model was 1029.96, with an overall coefficient of determination R2 of 0.97, indicating that the model accurately captured the trend of performance variation. A detailed analysis of each output variable revealed that the R² values for F1–F5 and D all exceeded 0.96, confirming the model’s excellent fitting accuracy and robustness. Supplementary materials present residual histograms for the six target variables (F1–F5 and D) on the test set (Fig. S3). The error distributions are centered near zero and approximately follow a normal distribution, indicating that the GPR model exhibits stable and unbiased predictive performance across all outputs. Fig. 1C compares plantar pressure data collected by the PEDAR system under barefoot conditions with those obtained from the FE analysis. The distributions were highly similar, with only a 3.3% difference in peak forefoot pressure, indicating the strong reliability of the foot FE model.
A Comparison between compression test results of randomly generated parameter samples and FE simulation results. At 5 mm compression, the reaction forces of samples A and B in the FE simulations differed from the actual tests by only 3.2% and 0.4%, respectively. B The GPR model achieved an overall MSE of 1029.96 and R2 of 0.97 in predicting parameters and structural properties, with all individual R2 values exceeding 0.96. C Plantar pressure data collected using insole sensors under barefoot conditions closely matched the FE simulation results.
Relationship between unit cell parameters and mechanical properties
As shown in Fig. 2A, all force values (F1–F5) exhibited an overall increasing trend with increasing structural thickness T; that is, as T increased, the corresponding force values also increased. However, the rate of increase varied with different combinations of parameters A and B, indicating that these parameters modulate the mechanical response of the material. For instance, when A = 5 and B = 1, the growth rate of F5 with increasing T was the highest. In contrast, the distribution of deformation D was more complex and showed potentially nonlinear behavior under different A, B configurations.
A Relationship between structural and physical properties: parameters A, B, and T influence the reaction force and deformation during compression. B Plantar pressure gradually decreases and stabilizes with an increasing number of iterations. C Peak metatarsal stress in the control group (left) versus when using the metatarsal pad with optimized parameters (right).
Plantar pressure and metatarsal stress
As shown in Fig. 2B, during the Bayesian optimization (BO) process, the peak plantar pressure progressively decreased as parameter combinations were iteratively updated. The model began to converge after approximately 88 iterations. At this point, the optimizer identified the following optimal structural parameters: upper layer — A = 1.55, B = 4.99, T = 3.13; lower layer — A = 4.88, B = 1.99, T = 3.98. Under this parameter configuration, FE analysis revealed that the metatarsal pad most effectively reduced the peak pressure in the forefoot region during the toe-off phase of gait, decreasing from 0.47 MPa to 0.23 MPa—a reduction of 51.36%. This result indicates a significant alleviation of excessive pressure concentration in the anterior plantar region.
A comparative analysis of the maximum principal stress across the five metatarsals revealed that the optimized insole also provided a cushioning effect on metatarsal stress distribution (Fig. 2C). Notably, the first metatarsal exhibited the most significant reduction, with its maximum principal stress decreasing by approximately 18.35%, suggesting that the geometric parameters of the pad offered more effective offloading support in the medial forefoot region (i.e., the first metatarsal support zone). Although the reductions in stress for the second and third metatarsals were relatively modest, the results still demonstrate the positive impact of the optimized structure on overall metatarsal load distribution.
To evaluate the structural response under forefoot loading, we recorded the deformation of the dual-layer pad configuration (Supplementary Fig. S4). In the “optimized” parameter combination, the upper metatarsal pad exhibited a maximum vertical deformation of 16.047 mm under peak load, which exceeded its original thickness of 15 mm. In contrast, the lower pad with a negative Poisson’s ratio configuration demonstrated only 3.342 mm vertical displacement under the same loading condition.
Discussion
In this study, a dual-layer parametrized lattice-structured cushioning metatarsal pad was developed specifically for addressing forefoot pressure issues in patients with BMD by integrating FE analysis, ML-based modeling, and BO. The GPR-based model (R² = 0.97) effectively captured the nonlinear relationships between unit cell parameters and mechanical performance, thereby overcoming the efficiency limitations of conventional trial-and-error methods in complex multi-objective optimization problems. The BO framework facilitated efficient exploration of the design space through a surrogate model-guided search process, achieving convergence within 88 iterations. Compared to single-cell optimization approaches—such as the 37% ± 17% reduction reported by Chatzistergos et al.25 and a previously published 44.45% reduction in shock-absorbing insoles24—the proposed design achieved a significant 51.36% reduction in peak forefoot pressure. Relative to previous studies25, the present work further demonstrates the applicability of data-driven methods for the customized design of foot orthotic devices, particularly showing enhanced adaptability to individual biomechanical differences. This offers a viable strategy for improving plantar biomechanics in BMD patients and other individuals affected by chronic lower-limb conditions.
The optimization strategy of the proposed dual-layer structure enabled gradient-based unloading of plantar pressure through dynamic coupling of parameters between the upper and lower layers. This design concept mirrors the natural “layered energy dissipation” mechanisms found in biological tissues, such as the multi-layered fibrous architecture of the heel fat pad26,27. However, this study further advances the concept by utilizing parametrized unit cells to achieve precise control over mechanical properties. The results demonstrated that the optimized metatarsal pad achieved more than a 50% reduction in peak forefoot pressure in the simulated environment, thereby effectively mitigating stress concentration in the metatarsophalangeal joint region.
Notably, in the final optimized structure, the lower layer of the metatarsal pad adopted a typical re-entrant unit cell configuration with parameter values A = 4.88 and B = 1.99. This type of structure is well known for exhibiting negative Poisson’s ratio (NPR) behavior—characterized by lateral contraction under compression28—which has been shown to enhance energy dissipation and structural stability under loading20,29. In this study, the dual-layer design significantly expanded the degrees of freedom in parameter selection. Through the Bayesian optimization process, the identified parameter combination led to an effective reduction in peak forefoot pressure during the toe-off phase. Given the repetitive high-impact loading observed in the forefoot region during BMD gait, we speculate that the inclusion of an NPR structure was a key factor in achieving high-efficiency pressure unloading. In the optimized structure, the lower layer exhibited a maximum vertical displacement of only 3.34 mm under peak loading, whereas the upper layer deformed by 16.05 mm—exceeding its original thickness. This asymmetry in deformation indicates that the NPR design contributed to maintaining vertical stiffness and redirecting compressive forces laterally, thereby enhancing its role in energy dissipation. While not the central focus of this study, this observation suggests that controllable Poisson’s ratio behavior may be considered as a complementary design factor in future orthotic optimization efforts, particularly for improving load distribution and structural resilience in targeted applications.
In this study, dynamic biplanar fluoroscopic registration was employed to provide physiologically accurate kinematic boundary conditions for the model, enabling the optimized metatarsal pad to closely match the patient’s specific gait characteristics (e.g., internal rotation and flatfoot posture). This calibration approach, based on real motion data, substantially enhances the alignment between the design model and the patient’s biomechanical requirements. However, several limitations remain:
Although the present study was conducted on a single individual with BMD, further validation across a broader spectrum of neuromuscular and structural foot pathologies is essential to assess the generalizability of the proposed framework. Notwithstanding this limitation, the dual-layer lattice architecture developed herein demonstrates strong theoretical adaptability across diverse patient presentations. For instance, in individuals with foot drop, muscular insufficiency often results in delayed heel strike and premature mid-forefoot loading. To accommodate this altered loading pattern, the optimized pad design could be anteriorly repositioned, with parameter configurations tailored to enhance mid-forefoot cushioning. In patients with spastic paraplegia, where asymmetric muscle tone and rotational gait deviations are commonly observed, notable mediolateral loading asymmetries may arise30. Such cases may benefit from directionally tuned stiffness distributions within the lattice structure to augment lateral stability while preserving plantar conformity. From an anatomical standpoint, flatfoot and pes cavus represent two ends of the arch morphology spectrum, each associated with distinct ground contact mechanics31,32. Flatfoot often coincides with excessive pronation and midfoot pressure concentration, necessitating reinforced medial support. Conversely, high-arched feet typically exhibit localized peak pressures on the lateral forefoot and heel, indicating a need for enhanced compliance in peripheral regions to facilitate pressure redistribution. In principle, these condition-specific demands can be addressed within the existing optimization framework by adjusting cell thickness, re-entrant geometry, and local stiffness gradients. However, the generalizability of these adaptations remains to be validated through future large-scale empirical studies.
In addition, the current optimization focused exclusively on the forefoot loading phase within the gait cycle, without incorporating the full spatiotemporal plantar load progression across heel strike, midstance, and push-off. This simplification was deliberate, as the primary objective of the present study was to address localized forefoot stress concentrations in a BMD patient. Simulating the full stance-phase dynamics would have significantly increased computational complexity and run time, which was deemed disproportionate to the clinical question in this proof-of-concept stage. Nevertheless, we acknowledge that integrating full-stance loading trajectories into future iterations—potentially through multi-objective Bayesian optimization—could improve generalizability and enhance structural performance in patients with complex or multi-phase gait pathologies.
For safety considerations, due to the elevated fall risk associated with BMD patients, the participant was not permitted to wear the metatarsal pad prototype during walking trials. As a result, real-world wear testing and gait-based performance evaluation were not conducted at this stage. Nevertheless, comprehensive validation of the material properties and structural behavior has been completed, including mechanical testing under quasi-static loading and comparative analysis with finite element predictions, as presented in the main text and supplementary materials. We acknowledge that the absence of in-situ functional testing remains a limitation of the current study. In future work, we plan to develop a full-scale footwear system and recruit a larger cohort of participants for experimental testing in a controlled gait laboratory environment, including evaluations of long-term durability, mechanical stability under repeated loading, and usability metrics based on patient-reported outcomes. Prior studies have demonstrated the clinical value of such real-world validation strategies in orthotic insole research, including CAD-assisted insole development for diabetic patients33, vibro-sensitive insole testing in neuropathic populations34, and mechanical verification of FDM-printed lattice insoles35, all of which inform the direction of our planned translational work.
Methods
Participant
A male patient diagnosed with BMD (European shoe size 42, age 25, height 175 cm, weight 60 kg) voluntarily participated in this study. Due to progressive skeletal muscle weakness and degeneration, the patient exhibited an internally rotated and flat foot posture. The Foot Posture Index (FPI) was measured at 1036, and the Arch Index was calculated as 0.337. The patient reported:
“According to my attending physician, although my condition has a relatively good prognosis and is not expected to affect my life, I have felt a gradual weakening in my lower limbs in recent years, particularly in the calves. I can no longer move my ankles on my own, and my gait has been significantly affected. Nowadays, even simple daily activities like walking require footwear with strong shock-absorbing capabilities to reduce impact.”
With the assistance of experienced research personnel, the patient underwent a computed tomography (CT) scan to capture the geometric structure of the foot skeleton, which was subsequently used for anatomical modeling. Additionally, gait analysis was conducted in a motion capture laboratory to acquire data necessary for defining boundary conditions in FE analysis and for model validation38. This study was approved by the Institutional Review Board for Human Subjects Research at the university (Approval No. RAGH202409140901), and informed consent was obtained from the patient prior to participation.
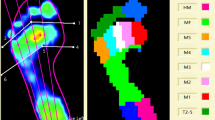
Metatarsal pad design
As shown in Fig. 3A, a dual-layer parametrized lattice-structured metatarsal pad was designed using nTopology 4.1.3 (New York, USA). Each layer of the pad was designed with a thickness (height) of 15 mm, resulting in a total pad height of 30 mm. The radius was set at 90 mm, which is substantially larger than the forefoot contact area to ensure sufficient coverage and interface between the foot and the metatarsal pad (right side of Fig. 3A). The internal 3D lattice structure was generated by revolving a 2D profile, with parameters (A, B) representing the inflection points of the structural lines in the 2D plane. As illustrated in Fig. 3B, by adjusting these parameters, the internal lattice could form three different configurations: re-entrant (A > B), honeycomb (A < B), and rectangular (A = B). To ensure that the pad could withstand loads equivalent to the peak ground reaction force encountered during walking—while remaining within the tensile strength limit of the material and maintaining controlled deformation—the internal structural thickness (T) was constrained within the range of 3.5 to 5 mm, with increments of 0.5 mm. The material used for the pad was flexible eSUN TPU 95 A (eSun Industrial Co., Ltd.), with a density of 1.21 g/cm³ and a tensile strength at break of 35 MPa. As shown in Fig. 3C, tensile tests were conducted on four type V specimens in accordance with ASTM D638 standards, and the resulting data were recorded for FE analysis to evaluate the structural response under load (details provided in Appendix A).
A Schematic illustration of the working principle of the metatarsal pad and a cross-sectional view of its internal structure. B Structural parameters and corresponding structural types. When the relative sizes of parameters A and B vary, the internal structure exhibits different configurations. The right panel shows a 2D cross-sectional view under specific parameter settings. C Tensile test samples and recorded data for material property evaluation, along with FE analysis of compression tests on cylindrical samples.
Dynamic biplanar fluoroscopy registration of the foot-metatarsal pad model
The participant, while wearing a foot positioning brace, underwent clinical CT scanning of the foot and ankle in the prone position (Siemens, Munich, Germany), with a slice interval of 0.75 mm. The grayscale thresholding tool in Mimics 21.0 (Materialize, Leuven, Belgium) was used to delineate the boundaries between skin and bone in the foot and ankle (Fig. 4A), and the resulting anatomical model was exported in STL format. The STL file was subsequently smoothed using Geomagic Studio 2014 (Geomagic, Inc., Research Triangle Park, NC, USA). The foot–ankle model was then assembled with the metatarsal pad in SolidWorks 2021 (SolidWorks Corporation, MA, USA). To reduce computational complexity and simplify contact calculations, all phalanges (distal, middle, and proximal) were modeled as a single rigid body, thereby minimizing degrees of freedom in the model. Other bones were connected via 2 mm thick solid elements to simulate cartilage and connective tissues39. The anatomical positions of foot ligaments and fascia were based on previously published studies40,41, with attachment sites adjusted according to the CT data.
Dynamic biplanar fluoroscopy is widely regarded as the gold standard for tracking in vivo skeletal motion42. As shown in Fig. 4A, a Dual Fluoroscopic Imaging System (DFIS, Taoimage, Shanghai, China) was used to capture dynamic images of the participant’s foot bones during walking. Through image segmentation and edge detection, the spatial positions of key anatomical structures were extracted. The 3D model of the metatarsal pad was then registered to the captured fluoroscopic images in both coronal and sagittal planes by manually adjusting the positions and shapes of the foot bones and soft tissues, thereby establishing spatial consistency within a unified world coordinate system.
Material properties and mesh generation
Tetrahedral meshing was performed using Ansys Workbench (developed by ANSYS, Inc., Canonsburg, Pennsylvania, USA). Given that the stiffness of bone is significantly higher than that of other soft tissues, its influence in this study was considered minimal; thus, no distinction was made between cortical and cancellous bone. For each simulation, the overall mesh size was reduced incrementally by 10% until the variation in results fell within 5%43. The final material properties are summarized in Table 1.
Boundary conditions and loading
Finite element analysis was performed using the Transient Structural solver in Ansys Workbench. During simulation, the proximal ends of the tibia, fibula, and selected soft tissue structures were fixed. The primary joints—namely the ankle and metatarsophalangeal (MTP) joints—were assigned full degrees of freedom, with contact surfaces defined as frictionless to allow relative sliding between articulating bones. Secondary joint movements were neglected by modeling the interfaces as bonded contacts mediated by cartilage, significantly reducing model complexity and computational cost. This approach is particularly suitable for studies focusing on the overall dynamic behavior of the foot. The coefficient of friction between the skin and the metatarsal pad, as well as between the pad and the ground, was set to 0.544.
To simulate external loading, time-varying vertical forces were applied to the bottom surface of the ground and the heel region, representing ground reaction forces and toe flexor muscle forces, respectively. These force values were derived from laboratory-based gait testing. Following the guidelines of the Gait 2392 musculoskeletal model in OpenSim (version 4.5, National Center for Simulation in Rehabilitation Research, Stanford, USA), experienced researchers placed retroreflective markers on the participant’s skin and tight-fitting clothing (Fig. 4B). Plantar pressure data were collected using the PEDAR in-shoe pressure measurement system (Novel GmbH, Munich, Germany), secured with socks in a barefoot condition. After a 5-min warm-up and familiarization period at a self-selected comfortable pace45, the participant began walking from the side onto a walkway instrumented with two force plates (sampling frequency 1000 Hz, AMTI, Watertown, MA, USA). Since the participant’s stride length was shorter than the long edge of the force plates, walking trials were conducted from the lateral side rather than aligned with the runway. Simultaneously, 10 optical motion capture cameras (Vicon Metrics Ltd., Oxford, UK) recorded marker trajectories at 200 Hz, while the PEDAR system sampled plantar pressure data at 100 Hz. Walking speed was self-selected and monitored using photoelectric gates positioned on either side of the walkway.
Gait trials were repeated until a set of valid experimental data was obtained. Adequate rest was provided between every 10 trials to prevent fatigue. Only trials in which the participant reported a normal gait pattern and both feet landed fully on separate force plates during the stance phase were considered valid. A total of 30 valid trials were collected, from which 80% (excluding the 3 fastest and 3 slowest trials) were retained for further processing in OpenSim, following previously published protocols32,46,47. First, the musculoskeletal model was scaled to match the participant’s anthropometric data based on the marker set, ensuring that the maximum positional error between experimental and virtual markers was less than 0.01 m. Subsequently, inverse kinematics and inverse dynamics analyses were performed, followed by static optimization using a cost function that minimized the sum of squared muscle activations to estimate muscle forces. The ground reaction forces and calf muscle forces from the impact loading phase were time-normalized (0–100%) across 24 gait trials, and their average profiles were used as external loading inputs in the FE simulation. The duration of load application in the FE model was set to match the average duration of the impact loading phase.
Data-driven cell performance modeling and optimization strategy
This study employed a data-driven modeling and optimization strategy implemented in Python. A multi-objective prediction framework based on GPR was developed to construct an ML model capable of capturing the relationship between the lattice structural parameters (A, B, T) and their corresponding performance metrics. BO was then applied to explore the multi-parameter design space and identify optimal structural combinations with the goal of reducing peak plantar pressure.
Construction of Gaussian process regression model for cell performance prediction
From the FE analysis results of 125 lattice structure samples with varying parameters, three key design parameters of each unit cell were extracted, along with the corresponding reaction forces under compressive displacement (F1–F5, representing reaction forces at different stages of compression) and the deformation at the midsection of the structure (D).
An input–output dataset was constructed and randomly divided into a training set (100 samples) and a test set (25 samples). Given the sensitivity of Gaussian Processes to input distributions, both the input features and output targets were standardized to improve model stability and generalization performance. GPR is a non-parametric Bayesian regression approach. The Matern kernel, known for its suitability in capturing physical behaviors in lattice-structured problems, was selected for this study to model the multi-output regression task. Accordingly, GPR with a Matern kernel was applied to learn the functional mapping between structural parameters and mechanical performance indicators:
Here, r = ∥x−x′∥ denotes the Euclidean distance; ν = 1.5 controls the smoothness of the kernel function; l is the length-scale hyperparameter; Kν is the modified Bessel function of order ν; and σ2 is the constant kernel weight. The model was trained and predicted in a column-wise manner for multi-output regression tasks, which is supported by the scikit-learn library. Predictions on the test set were subsequently inverse-transformed (de-standardized). Model performance was evaluated using the MSE and the coefficient of determination (R2).
Bayesian optimization of metatarsal pad structural parameters
In this study, a BO strategy was employed to search for optimal combinations of structural parameters for the metatarsal pad. An initial exploratory phase was conducted to build a surrogate model of the objective function, followed by iterative selection of the most promising sampling points on this model to progressively minimize peak plantar pressure. The optimization process assigned a separate set of parameters to the upper and lower layers of the pad, forming a combined input space. For each candidate combination, the corresponding pressure unloading performance was evaluated using simulations in Workbench, and an efficient parameter search was carried out using the Bayesian optimizer implemented in the scikit-optimize (skopt) library.
During the initial exploration phase, the optimizer randomly sampled 15 sets of parameter combinations from unexplored regions. Each combination was subjected to FE analysis of the metatarsal pad, and the corresponding peak plantar pressure was returned to the optimizer. The process then entered a model-guided optimization stage, where the optimizer continuously updated the posterior distribution of the objective function based on the accumulated data and selected the next parameter set expected to yield the greatest improvement. In each iteration, one candidate parameter set was proposed by the optimizer based on the current surrogate model. Throughout the optimization process, the trend of peak pressure reduction was monitored. To avoid unnecessary computational cost, the optimization was terminated either when the peak plantar pressure no longer decreased over the most recent 10 iterations or when a maximum of 200 iterations was reached. Finally, the combination that yielded the lowest peak pressure among all evaluated samples was selected, and the corresponding upper and lower layer parameter sets were identified as the optimal design solution.
Model validation
As shown in Fig. 4C, two sets of structural parameters were randomly generated outside the original dataset and fabricated using 3D printing for compression testing. These tests were used to evaluate the robustness and generalizability of both the structural FE model and the GPR-based predictive model. In addition, after training the Gaussian Process Regression model, its predictive performance was validated using the test dataset and assessed by calculating the MSE and the coefficient of determination (R²). The validity of the foot model was further evaluated by comparing plantar pressure distributions obtained from the PEDAR system with those predicted by the FE analysis.
Data availability
The raw data have been published on the Zenodo platform and are available for public use, https://doi.org/10.5281/zenodo.15377993.
References
Hoffman, E. P. & Kunkel, L. M. Dystrophin abnormalities in Duchenne/Becker muscular dystrophy. Neuron 2, 1019–1029 (1989).
Flanigan, K. M. Duchenne and Becker muscular dystrophies. Neurol. Clin. 32, 671–688 (2014).
Andrews, J. G. & Wahl, R. A. Duchenne and Becker muscular dystrophy in adolescents: current perspectives. Adolesce. Health Med.Ther. 9, 53–63 (2018).
Fischer, D. et al. The 6-minute walk test, motor function measure and quantitative thigh muscle MRI in Becker muscular dystrophy: A cross-sectional study. Neuromusc. Disord. 26, 414–422 (2016).
Barp, A. et al. Muscle MRI and functional outcome measures in Becker muscular dystrophy. Sci. Rep. 7, 16060 (2017).
Bellomo, T. R. et al. Management of the diabetic foot. Semin. Vasc. Surg. 35, 219–227 (2022).
Landorf, K. B., Ackland, C. A., Bonanno, D. R., Menz, H. B. & Forghany, S. Effects of metatarsal domes on plantar pressures in older people with a history of forefoot pain. J. Foot Ankle Res. 13, 18 (2020).
Lee, P. Y., Landorf, K. B., Bonanno, D. R. & Menz, H. B. Comparison of the pressure-relieving properties of various types of forefoot pads in older people with forefoot pain. J. Foot Ankle Res. 7, 18 (2014).
Chang, B.-C., Liu, D.-H., Chang, J. L., Lee, S.-H. & Wang, J.-Y. Plantar pressure analysis of accommodative insole in older people with metatarsalgia. Gait Posture 39, 449–454 (2014).
Ruiz-Ramos, M. et al. Effectiveness of bespoke or customised orthotic treatment in plantar pressure reduction of the central metatarsals: A systematic review and meta-analysis. J. Orthop. 59, 111–118 (2025).
Ng, W. L., Chua, C. K. & Shen, Y.-F. Print me an organ! Why we are not there yet. Prog. Polym. Sci. 97, 101145 (2019).
Askari, M. et al. Recent progress in extrusion 3D bioprinting of hydrogel biomaterials for tissue regeneration: a comprehensive review with focus on advanced fabrication techniques. Biomater. Sci. 9, 535–573 (2021).
Lu, Z. et al. Will this be the next step? A systematic review of 3D printing in footwear biomechanics. Footwear Sci. 1–16 https://doi.org/10.1080/19424280.2025.2472251.
Novak, J. I. & Novak, A. R. Is additive manufacturing improving performance in Sports? A systematic review. Proceedings of the Institution of Mechanical Engineers. Part P: J. Sports Eng. Technol. 235, 163–175 (2021).
Danko, M., Sekac, J., Dzivakova, E., Zivcak, J. & Hudak, R. 3D Printing of Individual Running Insoles – A Case Study. ORR 15, 105–118 (2023).
Jandova, S. & Mendricky, R. Benefits of 3D printed and customized anatomical footwear insoles for plantar pressure distribution. 3D Print. Addit. Manuf. 9, 547–556 (2022).
Muir, B. C. et al. Evaluation of novel plantar pressure-based 3-dimensional printed accommodative insoles - A feasibility study. Clin. Biomech. 98, 105739 (2022).
Salles, A. S. & Gyi, D. E. An evaluation of personalised insoles developed using additive manufacturing. J. Sports Sci. 31, 442–450 (2013).
Chansoda, K., Chookaew, W. & Suvanjumrat, C. Optimizing laser 3D printing parameters for customized rubber latex health shoe insoles. Prog. Addit. Manuf. https://doi.org/10.1007/s40964-024-00870-z. (2024).
Sun, Y. et al. 3D printed sports shoe Midsoles: Enhancing comfort and performance through finite element analysis of negative Poisson’s ratio structures. Mater. Des. 245, 113292 (2024).
Telfer, S., Woodburn, J., Collier, A. & Cavanagh, P. R. Virtually optimized insoles for offloading the diabetic foot: A randomized crossover study. J. Biomech. 60, 157–161 (2017).
Nickerson, K. A., Li, E. Y., Telfer, S., Ledoux, W. R. & Muir, B. C. Exploring the mechanical properties of 3D-printed multilayer lattice structures for use in accommodative insoles. J. Mech. Behav. Biomed. Mater. 150, 106309 (2024).
Liu, H., Hou, F., Li, A., Lei, Y. & Wang, H. High-efficient and reversible intelligent design for perforated auxetic metamaterials with peanut-shaped pores. Int J. Mech. Mater. Des. 19, 553–566 (2023).
Lu, Z. et al. Parametric cushioning lattice insole based on finite element method and machine learning: A preliminary computational analysis. J. Biomech. 184, 112674 (2025).
Chatzistergos, P. E., Gatt, A., Formosa, C., Farrugia, K. & Chockalingam, N. Optimised cushioning in diabetic footwear can significantly enhance their capacity to reduce plantar pressure. Gait Posture 79, 244–250 (2020).
Kimani, J. K. The structural and functional organization of the connective tissue in the human foot with reference to the histomorphology of the elastic fibre system. Acta Morphol. Neerl. Scand. 22, 313–323 (1984).
Maemichi, T., Matsumoto, M., Okunuki, T. & Kumai, T. Changes in functional characteristics of heel fat pad with age. Clin. Biomech. 118, 106294 (2024).
Li, T., Chen, Y., Hu, X., Li, Y. & Wang, L. Exploiting negative Poisson’s ratio to design 3D-printed composites with enhanced mechanical properties. Mater. Des. 142, 247–258 (2018).
Leung, M. S., Yick, K., Sun, Y., Chow, L. & Ng, S. 3D printed auxetic heel pads for patients with diabetic mellitus. Comput. Biol. Med. 146, 105582 (2022).
Klebe, S. et al. Gait analysis of sporadic and hereditary spastic paraplegia. J. Neurol. 251, 571–578 (2004).
Buldt, A. K. et al. Foot posture is associated with plantar pressure during gait: A comparison of normal, planus and cavus feet. Gait Posture 62, 235–240 (2018).
Lu, Z., Li, X., Rong, M., Baker, J. S. & Gu, Y. Effect of rearfoot valgus on biomechanics during barbell squatting: A study based on OpenSim musculoskeletal modeling. Front. Neurorobot 16, 832005 (2022).
Anggoro, P. W. et al. Computer-aided reverse engineering system in the design and production of orthotic insole shoes for patients with diabetes. Cogent. Eng. 5, 1470916 (2018).
Bagherzadeh Cham, M. et al. Effects of vibro-medical insoles with and without vibrations on balance control in diabetic patients with mild-to-moderate peripheral neuropathy. J. Biomech. 103, 109656 (2020).
Jonnala, U. K., sankineni, R. & Ravi Kumar, Y. Design and development of fused deposition modeling (FDM) 3D-Printed Orthotic Insole by using gyroid structure. J. Mech. Behav. Biomed. Mater. 145, 106005 (2023).
Evans, A. M., Copper, A. W., Scharfbillig, R. W., Scutter, S. D. & Williams, M. T. Reliability of the foot posture index and traditional measures of foot position. J. Am. Podiatr. Med. Assoc. 93, 203–213 (2003).
Cavanagh, P. R. & Rodgers, M. M. The arch index: a useful measure from footprints. J. Biomech. 20, 547–551 (1987).
Song, Y. et al. The influence of simulated worn shoe and foot inversion on heel internal biomechanics during running impact: A subject-specific finite element analysis. J. Biomech. 180, 112517 (2025).
Cheung, J. T.-M., Zhang, M., Leung, A. K.-L. & Fan, Y.-B. Three-dimensional finite element analysis of the foot during standing—a material sensitivity study. J. Biomech. 38, 1045–1054 (2005).
Ramlee, M. H., Abdul Kadir, M. R., Murali, M. R. & Kamarul, T. Biomechanical evaluation of two commonly used external fixators in the treatment of open subtalar dislocation—A finite element analysis. Med. Eng. Phys. 36, 1358–1366 (2014).
Golanó, P. et al. Anatomy of the ankle ligaments: a pictorial essay. Knee Surg. Sports Traumatol. Arthrosc. 24, 944–956 (2016).
Chen, T. L.-W. et al. Dynamic finite element analyses to compare the influences of customised total talar replacement and total ankle arthroplasty on foot biomechanics during gait. J. Orthop. Transl. 38, 32–43 (2023).
Henninger, H. B., Reese, S. P., Anderson, A. E. & Weiss, J. A. Validation of Computational Models in Biomechanics. Proc. Inst. Mech. Eng. H. 224, 801–812 (2010).
Cheung, J. T.-M. & Zhang, M. A 3-dimensional finite element model of the human foot and ankle for insole design. Arch. Phys. Med. Rehab. 86, 353–358 (2005).
Paquette, M. R., Melaro, J. A., Smith, R. & Moore, I. S. Time to stability of treadmill running kinematics in novel footwear with different midsole thickness. J. Biomech. 164, 111984 (2024).
Lu, Z. et al. Effect of heel lift insoles on lower extremity muscle activation and joint work during Barbell squats. Bioengineering 9, 301 (2022).
Lu, Z., Sun, D., Kovács, B., Radák, Z. & Gu, Y. Case study: The influence of Achilles tendon rupture on knee joint stress during counter-movement jump–Combining musculoskeletal modeling and finite element analysis. Heliyon 9, (2023).
Chen, T. L.-W., Wong, D. W.-C., Peng, Y. & Zhang, M. Prediction on the plantar fascia strain offload upon Fascia taping and Low-Dye taping during running. J. Orthop. Transl.20, 113–121 (2020).
Hsu, C.-Y. et al. Biomechanical analysis of the flatfoot with different 3D-printed insoles on the lower extremities. Bioengineering 9, 563 (2022).
Nie, B. et al. Determination of the in situ mechanical behavior of ankle ligaments. J. Mech. Behav. Biomed. Mater. 65, 502–512 (2017).
Siegler, S., Block, J. & Schneck, C. D. The mechanical characteristics of the collateral ligaments of the human ankle joint. Foot Ankle 8, 234–242 (1988).
Acknowledgements
We gratefully acknowledge the faculty and staff of the Research Academy of Grand Health at Ningbo University for their assistance with imaging and experimental equipment, the staff of the Doctoral School of Chemical Engineering and Material Sciences at the University of Pannonia for their support in 3D printing, and the Audi Hungaria Faculty of Automotive Engineering at Széchenyi István University for their technical support and in-depth discussions on material testing. This study was sponsored by the National Key R&D Program of China (2024YFC3607305; 2024YFC3607603).
Author information
Authors and Affiliations
Contributions
Conceptualization: Z.L., Y.G. Methodology: X.L., Y.S., G.F., A.K. Investigation: Z.L., X.L., Z.G., J.Z. Visualization: Z.L., Z.G. Supervision: D.S., Y.G. Writing—original draft: Z.L., X.L. Writing—review & editing: L.X., D.S., Y.G.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Lu, Z., Li, X., Sun, D. et al. Computationally tuned dual-layer lattice pads adapted to gait-induced pressure distribution. npj Adv. Manuf. 2, 43 (2025). https://doi.org/10.1038/s44334-025-00055-8
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s44334-025-00055-8