Abstract
This study aimed to estimate the burden of digestive disorders in Asia from 1990 to 2019 using Global Burden of Disease Study (GBD) 2019 data. We calculated disability-adjusted life-years (DALYs), prevalence, incidence, deaths, and estimated annual percentage changes (EAPCs). We also examined the burden rankings, future projections for six selected countries, the association with Sociodemographic Index (SDI), and risk factors. Digestive diseases showed a downward trend in age-standardized DALY rates over the past 30 years, which was predicted to continue in the future among selected countries, except for Turkmenistan. DALYs for digestive diseases were higher in males than females, peaking at 50–54 years. Alcohol use was the most attributable risk factor for digestive diseases DALYs. There was a negative correlation between the burden of digestive diseases and SDI, with some exceptions. Despite reduced age-standardized DALYs rates, digestive diseases remained prevalent, necessitating effective prevention and treatment programs by Asian governments.
Similar content being viewed by others
Introduction
Digestive diseases, as a significant contributor to morbidity and mortality globally, represent a wide range of conditions and place a substantial burden on healthcare systems. These diseases could not only impact the quality of life and productivity of patients but also could be fatal1,2. It has been reported that digestive diseases were the significant cause of DALYs and one of the leading causes of death in nearly all countries worldwide3,4. Meanwhile, studies have demonstrated that smoking, alcohol consumption, drug use, and high body–mass index exerted negative effects on the incidence, progression, and prognosis of digestive diseases5,6,7. Comprehending the disease burden attributable to risk factors is essential for implementing effective prevention measures to mitigate their adverse effects5.
Presently, there have been no previous studies assessing the burden of digestive diseases in Asian countries and territories. Based on the Global Burden of Disease Study 2019 (GBD 2019), our study was aimed to analyze and predict the trends and changes in the disability-adjusted life of years (DALYs), prevalence, incidence, and death of digestive diseases in Asia from 1990 to 2019. We also estimated the association between digestive disease burden and the Sociodemographic Index (SDI) and attributable risk factors.
Results
Estimates and trends of digestive diseases burden in Asia
Ranking as the 13th leading cause of disease burden, the burden of digestive diseases was significant in Asia in 2019. Digestive diseases accounted for 48.05 million (95% UI: 43.85–52.87) DALYs, 1373.22 million (95% UI: 1296.29–1454.29) estimated prevalent cases, 245.18 million (95% UI: 224.51–268.21) estimated incident cases and 1.32 million (95% UI: 1.22–1.42) deaths in 2019, which increased by 12.33%, 70.47%, 89.77%, 26.92% (Table 1, Supplementary Tables 1–3) from 1990, respectively. In the past 3 decades, the age-standardized rate of DALYs decreased from 1669.69 (95% UI: 1545.22–1791.27) per 100,000 population in 1990 to 992.97 (95% UI: 906.02–1092.05) in 2019, by an average of −1.91 (95% UI: −1.96 to −1.86) (Table 1). The same downward trend was observed in the age-standardized rate of deaths due to digestive diseases from 51.17 (95% UI: 47.42–54.51) per 100,000 population in 1990 to 28.85 (95% UI: 26.65–31.2) in 2019, with the EAPC being −2.1 (95% UI: −2.17 to −2.03) (Supplementary Table 3). Meanwhile, as shown in Fig. 1, an increasing trend was observed in the age-standardized rate of prevalence and incidence from 2005 to 2019.
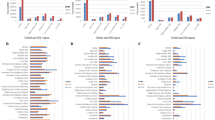
Digestive diseases contributed to 3.49% (3.27–3.73%) of total DALYs in Asia in 2019, ranked from 11th in 1990 to 13th in 2019. As shown in Table 2, there was a downward trend among the ranking of digestive diseases. Among all level 3 causes in GBD 2019, cirrhosis and other chronic liver diseases were ranked 13th in 1990 and 17th in 2019, both within the top 20. Cirrhosis and other chronic liver diseases (52.25%) were the major components of digestive diseases DALYs, followed by upper digestive system diseases (18.15%) (Fig. 2). Cirrhosis and other chronic liver diseases also had the highest age-standardized rate of prevalence and deaths in digestive diseases, while upper digestive system diseases had the highest age-standardized incidence rate (Supplementary Tables 1–3). Each subtype of cirrhosis and other chronic liver diseases exhibited a general downward trend in the age-standardized rate of DALYs, with cirrhosis due to alcohol showing some fluctuations in recent years, while the age-standardized prevalence rate of nonalcoholic fatty liver disease including cirrhosis increased, particularly after 2005 (Supplementary Figs. 2 and 3). Chronic hepatitis B, including cirrhosis, followed by chronic hepatitis C including cirrhosis, remained the leading causes of cirrhosis and other chronic liver diseases in 2019 when ranked by the age-standardized rate of DALYs, while cirrhosis due to alcohol experienced a rise in its ranking from 1990 to 2019 (Supplementary Fig. 4).
Digestive diseases burden by age and sex
As shown in Fig. 3, the number of DALYs gradually increased from adolescence, peaked at the age of 50–54 years, and then gradually decreased after the age of 55 years. The same trend was also observed in the prevalence and incidence for males, females, and both sexes combined, while the number of deaths for females peaked at the age of 80–84 years (Fig. 4). Among almost all age groups in our analysis, cirrhosis and other chronic liver diseases had the greatest contribution to digestive diseases burden, except for paralytic ileus and intestinal obstruction, which had the greatest contribution in individuals below the age of 5 years (Figs. 4 and 5).
In 2019, the number of DALYs [29.57 million (95% UI: 26.72–32.71) in males vs 18.48 million (95% UI: 16.29–20.98)], prevalence [721.86 million (95% UI: 679.78–763.05) in males vs 651.36 million (95% UI: 614.99–690.21)] and deaths [0.8 million (95% UI: 0.73–0.88) in males vs 0.52 million (95% UI: 0.46–0.58)] were higher in males than in females, while the numbers of incidence [127.98 million (95% UI: 117.30–140.01) in females vs 117.21 million (95% UI: 107–128.62)] were slightly higher in males (Fig. 4). Cirrhosis and other chronic liver diseases, pancreatitis, and inguinal, femoral, and abdominal hernia were more common in males than in females, while appendicitis, gallbladder and biliary diseases and vascular intestinal disorders were more common in females.
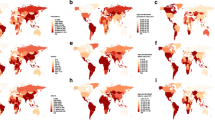
Digestive diseases burden by countries and territories
As shown in Fig. 6, the age-standardized prevalence rates of digestive diseases were significant in West Asia, where the age-standardized DALY rates were relatively low. In 2019, the highest age-standardized rates of DALYs due to digestive diseases were observed in Cambodia [2937.01 (95% UI: 2391.93–3500.65) per 100,000 population], Mongolia [2731.15 (95% UI: 2202.64–3420.59) per 100,000 population], Turkmenistan [2368.94 (95% UI: 1961.34–2903.24) per 100,000 population], Uzbekistan [2133.56 (95% UI: 1834.73–2488.83) per 100,000 population], Myanmar [1881.87 (95% UI: 1508.08–2329.64) per 100,000 population], Kyrgyzstan [1756.86 (95% UI: 1556.82–1977.68) per 100,000 population]. Conversely, the lowest age-standardized rates of DALYs of digestive diseases were found in Singapore, followed by Israel and Kuwait (Supplementary Table 4). Ranks of digestive diseases DALYs among the Level 3 causes of the GBD 2019 in Asia countries and territories were shown in Fig. 7. In almost all countries and territories in Asia, cirrhosis and other chronic liver diseases followed by upper digestive system diseases ranked as the primary cause of digestive diseases burden, except gallbladder and biliary diseases were the leading cause in Singapore. Cirrhosis and other chronic liver diseases were the major components of digestive diseases DALYs, accounting for more than 50% in most countries and territories in Asia, especially in Turkmenistan (79%) and Uzbekistan (78%) (Fig. 8).
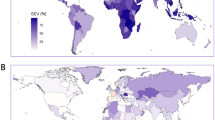
The relationship between country-level age-standardized DALYs rate of digestive diseases and SDI was shown in Fig. 9. The burden of digestive diseases showed a negative correlation with SDI, with a few exceptions.
Prediction of digestive disease burden
An upward trend was predicted in the number of DALYs for digestive diseases in the top six ranked countries, namely Cambodia, Mongolia, Turkmenistan, Uzbekistan, Myanmar, Kyrgyzstan, with age-standardized DALY rates decreasing in the future 25 years, except in Turkmenistan. The burden of digestive diseases was higher in males than in females historically, and this trend was predicted to continue over the next 25 years (Fig. 10).
Attributable risk factors for digestive disease burden
The percentage contribution of four risk factors to digestive diseases DALYs and deaths in 2019 was shown in Fig. 11. The findings reveal that in Asia, alcohol use contributed to 24.7% and 27.2% of DALYs and deaths, while drug use accounted for 9.3% of DALYs and 9.9% of deaths, respectively. Although alcohol use had the most significant impact in Asia, it accounted for only 2.2% of DALYs and 3.3% of deaths, similar to the contribution of drug use. Meanwhile, High body–mass index was responsible for 1.8% of DALYs and 0.9% of deaths, while smoking accounted for 1.9% of DALYs and 2.4% of deaths. The impact of high body–mass index was highest in Singapore (7.2% of DALYs) and Israel (5.4% of deaths), while the contribution of smoking was highest in the Philippines (5.4% of DALYs and 7.4% of deaths).
Discussion
Over the past 30 years, a declining trend in the ranking of DALYs and the age-standardized rates of DALYs due to digestive diseases were observed, while the absolute number of DALYs showed an increasing trend in Asia. Among all level 3 causes in GBD 2019, a decreasing trend in the ranking of DALYs was also found. Cirrhosis and other chronic liver diseases, which ranked 13th in 1990 and 17th in 2019, were the primary contributors to the burden. DALYs of digestive diseases were negatively related to SDI, with a few exceptions. Among the four risk factors in our study, alcohol use was most attributable. In addition to DALYs, there was an observed upward trend in the numbers of prevalence, incidence, and deaths. Demographic changes, population growth, as well as aging may be the primary factors driving and sustaining this trend, emphasizing the need for healthcare systems to provide essential treatment and care for the expanding demographic8.
The burden of digestive diseases in Asians varied by sex and age. The age group of 45–59 years had the most significant contribution to the burden of digestive diseases measured in DALYs. The high burden of digestive diseases among the working-age population caused enormous economic costs to societies, highlighting the imperative need for measures to reduce the prevalence and mortality from digestive diseases. Notably, there were higher deaths and DALYs burden observed in children aged 1–4 compared to those aged 5–20, which could be attributed to paralytic ileus and intestinal obstruction in children primarily. Compared with females, males bear a higher burden of digestive diseases. The Griswold’s study showed that alcohol use, associated with greater health loss in males compared to females, could be one of the driving factors9. It was reported that cirrhosis and other chronic liver diseases were higher in males. Moreover, male gender is an important risk factor of Hepatocellular Carcinoma among metabolic dysfunction-associated steatotic liver disease (MASLD) patients10. Chronic pancreatitis is also influenced by gender. Xiao’s study showed that although there was no gender disparity observed for acute pancreatitis or pancreatic cancer, the occurrence of chronic pancreatitis was twice as prevalent in males as in females11. This could be attributed to the genotype in chronic pancreatitis partly12.
The burden of digestive diseases in Asian also showed geographical variations, with a lower burden observed in countries with higher levels of SDI, except in middle-SDI countries. This trend could be attributed to differences in lifestyle and access to healthcare resources, emphasizing the importance of reducing healthcare disparities among ethnic and social groups13,14.
Our data suggested that cirrhosis and other chronic liver diseases not only contribute to 52.25% of DALYs associated with digestive diseases but also account for more than half of deaths due to digestive diseases in Asia. As a significant contributor to mortality and morbidity among individuals with digestive diseases, the burden and epidemiology of cirrhosis and other chronic liver diseases are undergoing changes. The most common causes of cirrhosis and other chronic liver diseases worldwide are MASLD, alcohol-related liver disease, and hepatitis B virus and hepatitis C virus15. However, the etiologies of cirrhosis and other chronic liver diseases are transitioning from viral to non-viral risk factors10,15,16,17. This could be attributed to heightened alcohol consumption, the increasing prevalence of obesity, and the pandemic of diabetes on the one hand, and advancements in the management of infections caused by hepatitis B virus and hepatitis C virus on the other hand16. In line with previous studies, chronic hepatitis B and C, including cirrhosis, showed a downward trend, particularly in China and India, both of which have played a significant role in reducing HBV incidence in Asia. China, as the first developing country to introduce a universal hepatitis B vaccination program for newborns and infants in 1992, achieved a reported three-dose hepatitis B (HepB3) coverage of 99.6% and a timely birth-dose coverage (HepB-TBD) of 95.6% by 2015, while India reported a HepB3 coverage of 91%, and this has significantly contributed to the reduction of HBV infection incidence in these regions18,19. Noteworthy, MASLD has evolved into a significant public health issue globally, with Asia leading the rise in its prevalence. With the epidemic of obesity and type 2 diabetes (T2DM), It is anticipated that the incidence of MASLD, which is not only found in adults but also in children and adolescents, will keep rising, leading to an immense clinical and economic burden10,20,21. Moreover, the increase in alcohol consumption, driven by economic growth, may have played a significant role in the escalating burden of alcohol-related liver disease, with the relative deficiency of aldehyde dehydrogenase 2 in Asian populations, compared to Western populations, potentially exacerbating liver damage induced by alcohol toxicity22.
Although the burden of cirrhosis and other chronic liver diseases has improved when adjusted for aging and population growth, the absolute number of DALYs has continued to rise. The increase in metabolic syndrome, alcohol abuse, and injection drug use in recent years could potentially exacerbate the future burden of cirrhosis. Patients with cirrhosis and other chronic liver diseases experienced higher healthcare expenses, lower employment rates, reduced income, elevated rates of comorbidities, more disability, and a lower quality of life23. While treatment of decompensated forms of cirrhosis may not result in a significant improvement in survival, it is essential to prioritize greater efforts in promoting primary prevention, identifying and treating liver disease at an early stage, and enhancing access to healthcare. Inexpensive and cost-effective preventive measures, such as administering HBV vaccinations, conducting screenings, ensuring safe blood transfusions, maintaining hygienic health facilities, and providing general education, are crucial in this regard4.
Followed by cirrhosis and other chronic liver diseases, upper digestive system diseases were another primary contributor to digestive disease burden in Asia. Among upper digestive system diseases, peptic ulcer disease was observed a significant decrease, due to the reduced prevalence of Helicobacter pylori (H. pylori) infection and the extensive usage of potent anti-secretory drugs. However, the increasing use of non-steroidal anti-inflammatory drugs (NSAIDs) and aspirin could take a heavy toll on the aged population, and ulcers not associated with H. pylori infection and NSAIDs were imposing great challenges to the diagnosis and therapy24,25. Dumic’s study revealed that besides being linked to peptic ulcer disease, H. pylori infection may be associated with extra intestinal diseases (neurologic, dermatological, cardiovascular, and hematologic)26. Another study conducted by Sbeit showed that both upper digestive system diseases and cardiovascular diseases were common and could affect each other through systemic inflammation, disturbed hemodynamics, interactions, and adverse effects of medications, as well as bacterial overgrowth27. Taking into account the combined effects of multiple etiologies could be beneficial for optimizing patient management and improving patient prognosis.
Alcohol use, smoking, drug use, and high body-mass index were included in the GBD database as risk factors for digestive diseases, the deleterious impacts of which have been well established9,28,29. In our study, alcohol consumption was observed to be the most attributable risk factor for digestive diseases in Asia. The harmful use of alcohol, recognized as a global issue, was estimated to be the world’s third-largest risk factor for disease and disability, with the liver considered the major victim30. Meanwhile, the various risk factors do not only act independently. For example, as an independent risk factor for pancreatitis, smoking could synergize with alcohol-related risks31. In the past few decades, urbanized lifestyles and dietary changes in many Asian countries, characterized by increased consumption of added fats and reduced physical activity, led to a higher prevalence of obesity. This obesity epidemic may significantly impact the health trajectory of future generations22,32. These four risk factors in our study were modifiable, and their impact on the burden of digestive diseases demonstrates the necessity of implementing ambitious prevention strategies in public health regulations and policies.
In recent years, increasing attention has been given to metabolic syndrome (MetS), which includes visceral obesity, dyslipidemia, diabetes mellitus, and hypertension, with MASLD emerging as the primary hepatic disorder in patients with this syndrome33. MASLD, MetS, and atherosclerosis share overlapping risk factors and similar pathophysiological mechanisms. MASLD is considered an emerging risk enhancer for atherosclerotic cardiovascular diseases, and the relationship between MASLD and type 2 diabetes is bidirectional34,35,36. Digestive diseases, cardiovascular diseases, and endocrinological disorders all significantly contribute to the global disease burden and escalating healthcare costs13,37,38. These interconnected conditions underscore the need for integrated prevention and management strategies. Moreover, the global burden of cancer is substantial and growing, with digestive system cancers constituting a significant proportion of human cancers, and effectively managing digestive diseases could potentially contribute to the reduction of these cancers39,40. Additionally, other generalized diseases, such as comorbid malnutrition, could worsen outcomes for patients with digestive diseases41. Therefore, it is essential to analyze these additional risk factors and comorbidities after their inclusion in the GBD database.
Our study investigated the burden of digestive diseases over the past 3 decades in Asian countries. However, there were some limitations in this study. Firstly, several digestive diseases, such as Barrett’s esophagus and eosinophilic esophagitis, may not be present in the GBD 2019 database. Secondly, The GBD 2019 contains only pre-COVID-19 pandemic data. Studies showed that, in addition to affecting the respiratory system, the novel coronavirus can also lead to a range of digestive system diseases. Lockdowns and restricted vaccine availability during this stage also had a negative impact on digestive diseases42,43. Lastly, this study only concentrated on the impact of individual etiologies and did not include the combined effects of multiple causes, as well as the synergistic interactions among risk factors.
Methods
Data sources
The GBD 2019, as a globally comprehensive effort, estimated the burden of 369 diseases, injuries, and risk factors covering 204 countries and territories from 1990 to 2019, with details of the general methods described on the official website (Global Burden of Disease (GBD) | Institute for Health Metrics and Evaluation (healthdata.org)). The burden of digestive diseases, including cirrhosis and other chronic liver diseases, upper digestive system diseases, appendicitis, paralytic ileus and intestinal obstruction, inguinal, femoral, and abdominal hernia, inflammatory bowel disease, vascular intestinal disorders, gallbladder and biliary diseases, pancreatitis, other digestive diseases, were quantified by DALYs, prevalence, incidence and death with metrics of rate, percent and number stratified by sex, age, countries and territories, which obtained from the Global Health Data Exchange query tool (VizHub - GBD Results (healthdata.org)). The 95% uncertainty intervals (UI) were calculated based on the GBD 2019 global age-standard population and the population predictions were obtained from the World Population Prospects 2017 Revision.
Statistical analysis
The estimated annual percentage changes (EAPCs) were calculated to depict the secular trends in the digestive disease burden. Regression analysis was performed using the equation y = α + βx + ε, where x = calendar year and y = ln (rate). The EAPC was then calculated as EAPC = 100 × [exp(β) − 1], with its 95% UI acquired from the regression model. EAPC > 0 and 95% UI > 0 indicated an upward trend, while EAPC < 0 and 95% UI < 0 indicated a downward trend. Disability-adjusted life-years (DALYs) were defined as the summation of years of life lost (YLLs) and years lived with disability (YLDs), representing the gap between the population’s actual health status and an ideal state of full health. A log-linear age–period–cohort model, implemented in R using the NORDPRED package, was fitted to recent trends to predict the burden of digestive diseases in the next 25 years.
The sociodemographic index (SDI) served as a composite measure of development status. In this study, we utilized the SDI for each of the 49 countries and territories in Asia, which were classified into five geographic sub-regions by the United Nations: South Asia, Central Asia, Southeast Asia, East Asia, and West Asia.
These analyses were conducted with the R program (version 4.1.3, R core team). We established a threshold of statistical significance as P-value < 0.05.
Case definition and risk factors
In the GBD 2019 cause list, which was organized as a four-level hierarchy, digestive diseases were grouped within one Level 2 cause, with cirrhosis and other chronic liver diseases, upper digestive system diseases, appendicitis, paralytic ileus and intestinal obstruction, inguinal, femoral, and abdominal hernia, inflammatory bowel disease, vascular intestinal disorders, gallbladder and biliary diseases, pancreatitis and other digestive diseases grouped on Level 3 cause. This hierarchy for digestive diseases is presented in Supplementary Fig. 1. Case definitions in this study primarily followed the 10th edition of the International Classification of Diseases (ICD-10).
The four attributable risk factors for digestive diseases were high body–mass index smoking, drug use, and alcohol use. We calculated the percentage contribution of these factors to DALYs and deaths of digestive diseases in 2019 according to GBD 2019.
Data availability
The data used in this study were obtained from the Global Health Data Exchange query tool.
Code availability
The codes used for the analysis are available from the corresponding author upon reasonable request.
References
Peery, A. F. et al. Burden and cost of gastrointestinal, liver, and pancreatic diseases in the United States: update 2018. Gastroenterology 156, 254–272.e11 (2019).
Peery, A. F. et al. Burden and cost of gastrointestinal, liver, and pancreatic diseases in the United States: update 2021. Gastroenterology 162, 621–644 (2022).
Chen, Y., Chen, T. & Fang, J.-Y. Burden of gastrointestinal cancers in China from 1990 to 2019 and projection through 2029. Cancer Lett. 560, 216127 (2023).
Sepanlou, S. G. et al. Burden of gastrointestinal and liver diseases in Middle East and North Africa: results of Global Burden of Diseases Study from 1990 to 2010. Middle East J. Dig. Dis. 7, 201–215 (2015).
Zhang, G., Cao, F., Shi, L., Ma, T. & Zhang, L. Contribution of high body mass index and alcohol use to liver cancer-related mortality: á study based on 195 countries or territories. Dig. Liver Dis. 52, 221–231 (2020).
Yuan, S. et al. Smoking, alcohol consumption, and 24 gastrointestinal diseases: Mendelian randomization analysis. eLife 12, e84051 (2023).
Malekzadeh, M. M. et al. Opium use and risk of mortality from digestive diseases: a prospective cohort study. Am. J. Gastroenterol. 108, 1757–1765 (2013).
Wang, R., Li, Z., Liu, S. & Zhang, D. Global, regional, and national burden of 10 digestive diseases in 204 countries and territories from 1990 to 2019. Front. Public Health 11, 1061453 (2023).
Griswold, M. G. et al. Alcohol use and burden for 195 countries and territories, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet 392, 1015–1035 (2018).
Yip, T. C.-F., Lee, H. W., Chan, W. K., Wong, G. L.-H. & Wong, V. W.-S. Asian perspective on NAFLD-associated HCC. J. Hepatol. 76, 726–734 (2022).
Xiao, A. Y. et al. Global incidence and mortality of pancreatic diseases: a systematic review, meta-analysis, and meta-regression of population-based cohort studies. Lancet Gastroenterol. Hepatol. 1, 45–55 (2016).
Whitcomb, D. C. Genetic risk factors for pancreatic disorders. Gastroenterology 144, 1292–1302 (2013).
Wang, Y. et al. Global burden of digestive diseases: a systematic analysis of the Global Burden of Diseases Study, 1990 to 2019. Gastroenterology 165, 773–783.e15 (2023).
Hanauer, S. B. The burdens of digestive diseases. Nat. Rev. Gastroenterol. Hepatol. 6, 377–377 (2009).
Moon, A. M., Singal, A. G. & Tapper, E. B. Contemporary epidemiology of chronic liver disease and cirrhosis. Clin. Gastroenterol. Hepatol. 18, 2650–2666 (2020).
Huang, D. Q. et al. Global epidemiology of cirrhosis—aetiology, trends and predictions. Nat. Rev. Gastroenterol. Hepatol. 20, 388–398 (2023).
Younossi, Z. M. et al. Changes in the prevalence of the most common causes of chronic liver diseases in the United States From 1988 to 2008. Clin. Gastroenterol. Hepatol. 9, 524–530.e1 (2011).
Liu, J., Liang, W., Jing, W. & Liu, M. Countdown to 2030: eliminating hepatitis B disease, China. Bull. World Health Organ. 97, 230–238 (2019).
Le, L. V. et al. Progress towards achieving viral hepatitis B and C elimination in the Asia and Pacific region: results from modelling and global reporting. Liver Int. 42, 1930–1934 (2022).
Younossi, Z. et al. Global perspectives on nonalcoholic fatty liver disease and nonalcoholic steatohepatitis. Hepatology 69, 2672–2682 (2019).
Perumpail, B. J. et al. Clinical epidemiology and disease burden of nonalcoholic fatty liver disease. World J. Gastroenterol. 23, 8263–8276 (2017).
Wong, M. C. S. et al. The changing epidemiology of liver diseases in the Asia–Pacific region. Nat. Rev. Gastroenterol. Hepatol. 16, 57–73 (2019).
Stepanova, M. et al. Direct and indirect economic burden of chronic liver disease in the United States. Clin. Gastroenterol. Hepatol. 15, 759–766.e5 (2017).
Shim, Y. K. & Kim, N. Nonsteroidal anti-inflammatory drug and aspirin-induced peptic ulcer disease. Korean J. Gastroenterol. 67, 300 (2016).
Lanas, A. & Chan, F. K. L. Peptic ulcer disease. Lancet 390, 613–624 (2017).
Dumic, I. et al. Gastrointestinal tract disorders in older age. Can. J. Gastroenterol. Hepatol. 2019, 1–19 (2019).
Sbeit, W., Kadah, A., Mahamid, M., Mari, A. & Khoury, T. The interplay between gastrointestinal and cardiovascular diseases: a narrative review focusing on the clinical perspective. Eur. J. Gastroenterol. Hepatol. 32, 132–139 (2021).
Ma, C. et al. Factors associated with geographic disparities in gastrointestinal cancer mortality in the United States. Gastroenterology 163, 437–448.e1 (2022).
Koh, J. C. et al. Asian consensus on the relationship between obesity and gastrointestinal and liver diseases. J. Gastroenterol. Hepatol. 31, 1405–1413 (2016).
Rocco, A. Alcoholic disease: liver and beyond. World J. Gastroenterol. 20, 14652 (2014).
Yadav, D. & Lowenfels, A. B. The epidemiology of pancreatitis and pancreatic cancer. Gastroenterology 144, 1252–1261 (2013).
Murray, C. J. L. Findings from the Global Burden of Disease Study 2021. Lancet 403, 2259–2262 (2024).
Watanabe, S., Yaginuma, R., Ikejima, K. & Miyazaki, A. Liver diseases and metabolic syndrome. J. Gastroenterol. 43, 509–518 (2008).
Danpanichkul, P. et al. Disparities in metabolic dysfunction-associated steatotic liver disease and cardiometabolic conditions in low and lower middle-income countries: a systematic analysis from the global burden of disease study 2019. Metabolism 158, 155958 (2024).
Zhang, D. et al. Nonalcoholic fatty liver disease as an emerging risk factor and potential intervention target for atherosclerotic cardiovascular diseases. J. Cardiovasc. Pharmacol. 81, 327–335 (2023).
Sheka, A. C. et al. Nonalcoholic steatohepatitis: a review. J. Am. Med. Assoc. 323, 1175–1183 (2020).
Roth, G. A. et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990-2019: update from the GBD 2019 Study. J. Am. Coll. Cardiol. 76, 2982–3021 (2020).
Zhang, H. et al. Global burden of metabolic diseases, 1990-2021. Metabolism 160, 155999 (2024).
Global Burden of Disease. 2019 Cancer Collaboration et al. cancer incidence, mortality, years of life lost, years lived with disability, and disability-adjusted life years for 29 cancer groups from 2010 to 2019: a systematic analysis for the Global Burden of Disease Study 2019. JAMA Oncol. 8, 420–444 (2022).
Jin, W. et al. Global, regional, and national cancer burdens of respiratory and digestive tracts in 1990–2044: a cross-sectional and age-period-cohort forecast study. Cancer Epidemiol. 91, 102583 (2024).
Malnutrition and liver disease in a developing country—PubMed. https://pubmed.ncbi.nlm.nih.gov/34497430/.
Sanz Segura, P., Arguedas Lázaro, Y., Mostacero Tapia, S., Cabrera Chaves, T. & Sebastián Domingo, J. J. Afectación del aparato digestivo en la covid-19. Una revisión sobre el tema. Gastroenterol. Hepatol. 43, 464–471 (2020).
Zhan, G.-F., Wang, Y., Yang, N., Luo, A.-L. & Li, S.-Y. Digestive system involvement of infections with SARS-CoV-2 and other coronaviruses: clinical manifestations and potential mechanisms. World J. Gastroenterol. 27, 561–575 (2021).
Acknowledgements
We deeply appreciate the contributions made by the 2019 GBD collaborators. This study received no specific funding.
Author information
Authors and Affiliations
Contributions
Study conception and design: Q.C. and X.W.T. Drafting of the paper: Q.C. and X.W.T. Data acquisition and critical revision: S.H., J.Y.P., R.L., S.Q.L., J.X.Z., X.M.S., H.X., P.W., W.Z., L.S., Y.P. Revision of paper, and final approval of paper: X.W.T., Q.C., and X.H.W.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Chen, Q., Wang, X., Peng, J. et al. The burden of digestive diseases in Asian countries and territories from 1990 to 2019: an analysis for the Global Burden of Disease 2019 study. npj Gut Liver 2, 6 (2025). https://doi.org/10.1038/s44355-025-00019-x
Received:
Accepted:
Published:
Version of record:
DOI: https://doi.org/10.1038/s44355-025-00019-x