Abstract
Exposure to fine particulate matter (PM2.5), a primary component of wildfire smoke, and exposure to high temperatures both independently increase the risk of mortality, with evidence of synergistic effects. These environmental stressors often co-occur during wildfire season, and their synergistic effects are expected to worsen with climate change. However, the combined health risks of wildfire-related PM2.5 and temperature remain poorly understood, limiting the effectiveness of public health interventions. This study investigated the joint effects of PM2.5 and temperature on community all-cause mortality across 13 wildfire seasons (2010–2022) in southwest British Columbia, Canada. Daily estimates of ambient PM2.5 and temperature exposure were assigned from a machine learning-based prediction model and satellite data, respectively. Using a case-crossover design and conditional logistic regression, we examined non-linear associations between co-exposures and mortality across deciles and absolute exposure ranges. We found significant, non-linear interactions, with the highest mortality risk observed on days with PM2.5 levels of 12–14 µg/m³ and temperatures ≥ 26 °C (OR = 7.31, 95% CI: [5.34, 10.0]). Co-exposures exceeding the 90th percentile showed synergistic effects, contributing an excess mortality risk of 7.9% (95% CI: 6.1, 9.1). Moderate co-exposure levels posed substantial risks, underscoring the need for greater attention to their public health impacts. Our findings highlight the urgent need to understand and address the compounding effects of PM2.5 and temperature to mitigate risks in a changing climate.
Similar content being viewed by others
Introduction
Climate change is causing warmer and drier conditions across many regions, including North America, increasing the risk of more frequent and intense wildfires1. Recent increases in wildfire occurrence have led to more episodic, short-term exposures to high concentrations of ambient fine particulate matter (PM2.5), a primary component of wildfire smoke (WFS)2. Given the large body of evidence on the adverse health effects of short-term PM2.5 exposure, including during WFS events3,4, it is imperative to better understand the risks associated with air pollution due to climate-related events, especially when exposure co-occurs with other climate-related hazards.
Concurrent with increasing exposures to WFS, climate change is leading to hotter weather and increasing the frequency of extreme heat events (EHEs). The detrimental health effects of heat exposure are well-documented in the scientific literature, particularly concerning all-cause mortality and cardio-respiratory outcomes5,6. Recent research in the western region of North America has demonstrated the substantial overlap between WFS and EHEs7,8,9. Epidemiological evidence further shows that elevated temperatures amplify the adverse health effects of PM2.5 exposure, and vice versa9,10,11,12,13.
Existing research on the health effects of PM2.5 and temperature also suggests plausible non-linear relationships and interactions that pose challenges for offering clear public health guidance when the exposures are co-occurring. Specifically, evidence suggests that the impact of short-term PM2.5 on mortality exhibits a log-linear relationship4,14,15,16,17, indicating that the health risks of PM2.5 on days with moderate WFS do not differ significantly from those on days with severe WFS (Fig. 1). In contrast, the relationship between temperature and mortality is exponential, with a marked increase in health risks from moderate to extreme heat days18,19,20,21,22(Fig. 1). Differences in how PM2.5 and temperature individually relate to mortality suggests a potentially complex interplay when the exposures co-occur, which may result in different magnitudes of co-exposure interactions along the range of each exposure. Most public health advice to date has focused on potential interaction at high levels of each exposure23.
Previous methods of studying the combined effects of PM2.5 and temperature on mortality have often simplified this interaction by categorizing levels of exposure into quantiles10,11,12. This approach has demonstrated how higher quantiles of temperature can amplify the mortality risks within higher quantiles of PM2.5, and vice versa. However, such an approach might not fully capture the nuanced, non-linear dynamics of their potential interaction. Therefore, a more detailed understanding of the precise nature of this interaction is needed to identify specific combinations of short-term ambient PM2.5 and temperature exposure levels that result in joint effects on population health. Such insights would benefit the development of public health policies and communication strategies by providing a clearer picture of when and how these co-exposures to environmental stressors pose human health risks23.
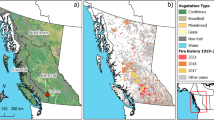
Our study aimed to elucidate these complex interactions by estimating the combined effects of daily ambient PM2.5 and temperature on community all-cause mortality over 13 wildfire seasons in the southwest region of mainland British Columbia (BC), Canada (Fig. 2a). By employing a time-stratified case-crossover design, we investigated the joint impacts of co-exposure across multiple categories of ambient PM2.5 and temperature exposure. Rather than limiting the analysis of co-exposures to quantile categories, we also defined both the temperature and PM2.5 exposure categories using specific ranges. Concentration-based categories align with existing air quality communication tools, such as the Canadian Air Quality Health Index (AQHI)24 and the American Air Quality Index (AQI)25, which are familiar to both the public and policymakers. Though quite nuanced regionally, temperature-based measures also inform when heat alerts are issued, such as Canada’s public weather alerts26 and the Heat Warning system in the US27. Fixed ranges thus potentially offer a direct and understandable way to assess co-exposure to PM2.5 and temperature, facilitating clearer public health advice and enabling individuals and communities to make informed decisions about their exposure and protective measures. This approach should advance the translation of complex air pollution epidemiological findings into practical, actionable guidance, enhancing the effectiveness of public health messages regarding the risks of PM2.5 exposure, particularly during periods of elevated temperatures.
a Map of the study area which includes residential postal codes (purple dots) within the Local Health Authority (LHA) boundaries (polygons) that intersect with the mainland southwestern region of the BC Heat Alert and Response System58,60. The map lines delineate study areas and do not necessarily depict accepted national boundaries. b Time series plots of average calendar week PM2.5 concentrations for the study area stratified by year, with the overall daily mean PM2.5 and average WFS day threshold indicated with the horizontal blue and red lines, respectively. c Time series plots of average weekly temperature for the study area stratified by year, with the overall daily mean temperature and average EHE day threshold indicated with the horizontal green and dark red lines, respectively.
Results
Exposure and outcome summary
The study included 21,220 community deaths. Of these decedents, 57% were 65 years or older and 63.5% were male. The average age at death was lower for males (63 years) than females (71 years). On average, each death had 3.4 control days.
Less than half (44%) of all case and control days had a low PM2.5 exposure ( < 6 µg/m3), and approximately one third (34%) were between 6 µg/m3 and 8 µg/m3 (Table 1). PM2.5 exposure as a continuous measure differed significantly (p < 0.001) between case and control days. While the percentage of days impacted by WFS did not differ significantly between case (9%) and control days (8%), categories of PM2.5 did (Table 1). There were also significant differences in temperature, temperature categories, and EHE days between the case and control days. The algorithm used in this study to define a WFS day confirmed the occurrence of such events in each month of our study period.
There was considerable overlap in the PM2.5 concentrations and temperatures on days impacted by WFS and EHEs (Fig. 3). On days classified as having WFS impacts, the median [interquartile range, IQR] PM2.5 concentration was 13.6 µg/m3 [11.1, 19.6] and the median temperature was 19.7 oC [16.5, 22.3]. Days without WFS impacts had a median PM2.5 concentration of 6.1 µg/m3 [5.0, 7.2] and a lower median temperature of 14.2 oC [11.2, 17.2]. EHE days had a median PM2.5 concentration of 12.1 µg/m3 [8.9, 15.8], with more than half (52%) of EHE days also having evidence of WFS impacts. Days without an EHE had a PM2.5 concentration of 6.2 µg/m3 [5.0, 7.5], with only 6.0% of days without an EHE also exhibiting WFS impacts.
There was notable overlap between days with moderate-to-high PM2.5 and warmer temperatures (Fig. S1, Supplemental Materials). Specifically, on days when PM2.5 was 16 µg/m³ or higher, the majority ( ~ 53%) had daily mean temperatures ranging between 20 °C and 26 °C (Fig. 2B). However, the most extreme temperature and PM2.5 categories rarely co-occurred (e.g., 1.2% for ≥26 °C and ≥16 µg/m³ co-occurrence). Notably, 18% of days in the 12–14 µg/m3 PM2.5 category had temperatures ≥26 °C. The lowest PM2.5 days predominantly occurred during cooler periods (Fig. S1, Supplemental Materials).
Associations between continuous PM2.5, temperature, and mortality
In crude models for community all-cause mortality, a 1-unit increase in PM2.5 (µg/m3) was associated an odds ratio (OR) of 1.004 [1.001, 1.006] and a 1-unit increase in temperature (°C) was associated with an OR of 1.027 [1.023, 1.032]. After mutual adjustment, only temperature remained significantly associated with community all-cause mortality, and the OR for PM2.5 was attenuated to the null. There was no evidence of a significant interaction between PM2.5 and temperature on a continuous scale (Table 2).
Associations between WFS, EHEs, and mortality
In models unadjusted for EHE days (Table 3), WFS days had a crude OR of 1.05 [0.98, 1.11] and EHE days had a crude OR of 1.50 [1.40, 1.60] when not adjusted for WFS days. In the mutually adjusted model, EHE days had an OR of 1.56 [1.45, 1.67], whereas the OR for WFS days was attenuated to 0.91 [0.85, 0.97]. Notably, there was a significant negative interaction between WFS and EHE days (Table 4).
Associations between PM2.5 and temperature deciles and mortality
In adjusted models using deciles of PM2.5, the highest decile of PM2.5 exposure, ranging from 10.1–121.0 µg/m³, was associated with an OR of 1.15 [1.08, 1.22], compared with PM2.5 below the 50th percentile. Odds of mortality was significantly elevated for all temperature categories over the 60th percentile category, with the highest ORs for the highest percentiles (Table 5).
There were significant interactions between the > 90th decile category of the PM2.5 and the three highest temperature decile categories, with the highest interaction effects observed for the > 90th decile of PM2.5 when the temperature was in the > 90th decile (OR = 1.66 [1.37, 2.00]) (Fig. 4a and Table S1, Supplemental Materials). Notably, the > 90th decile for PM2.5 exhibited its largest overlap with the > 90th decile for temperature (4% of days) compared with all other PM2.5 decile groups (Fig. 4b), suggesting that the interaction effects are concentrated within the > 90th decile exposure combination. The stratified models were consistent with the interaction modeling results, with the highest ORs observed in the > 90th decile for PM2.5 when temperatures were also in the > 90th decile (Fig. 5a, Table S2, Supplemental Materials).
Associations between absolute PM2.5 and temperature categories and mortality
Relative to PM2.5 < 6 µg/m³, only the 10–12 µg/m3 and 12–14 µg/m³ exposure categories were significantly associated with increased mortality, with crude ORs of 1.19 (1.10, 1.29) and 1.62 (1.48, 1.78), respectively (Table 6). After adjusting for temperature categories, only the 12–14 µg/m3 PM2.5 exposure category remained significantly associated with mortality, and the effect was attenuated. In contrast, temperature exposure categories were significantly associated with all-cause mortality in both crude models and models adjusted for PM2.5 categories (Table 6). In contrast to the PM2.5 exposure-response, the temperature exposure-response suggested an exponential relationship with mortality, with a very large upward shift in ORs when temperature was ≥26 oC.
Examination of joint effects between the absolute PM2.5 and temperature categories also indicated non-linear effect modification. Specifically, the multiplicative interaction model (Fig. 6a) indicated the largest interaction occurred between the 12–14 µg/m3 PM2.5 and ≥ 26 oC temperature categories. However, the wide 95% confidence intervals indicate substantial uncertainty in this interaction effect estimate, suggesting caution in its interpretation
In the stratified models (Fig. 7a), the ORs for the PM2.5 categories from 10 to 16 µg/m3 became substantially larger when stratified by the highest temperature category ( ≥ 26 oC, Fig. 7a). The exposure-response relationship across temperature categories also varied by the PM2.5 categories (Fig. 7b), and these joint effects exhibited a non-linear pattern. Notably, the largest ORs were estimated for PM2.5 exposure categories that were only moderately elevated.
a Absolute PM2.5 categories, estimated from models stratified by absolute temperature categories, and (b) absolute temperature categories, estimated from models stratified by absolute PM2.5 categories. Because of limited overlap between certain categories, OR estimates were excluded for co-exposures that had fewer than 10 days within any cell of a stratified model because these represent unstable estimates.
Supplemental analysis
Days with extreme PM2.5 and extreme temperature ( > 90th percentile) were associated with the highest odds of mortality compared with days without extreme PM2.5 or temperature ( < 50th percentile) (Table 7). The REOI and AP values above 0 indicate significant additive interaction, meaning the combined effect of extreme PM2.5 and extreme temperature exceeds the sum of their individual effects. The synergy index (S) is further suggestive of a significant synergistic effect. Additionally, there is a large increase in excess risk (ER) of community mortality, changing from 0.11% [−1.1, 1.4] and 1.3% [0.14, 2.3] for extreme PM2.5 only and extreme temperature only, respectively, up to 7.9% [6.1, 9.1] for the extreme co-exposure category. Such a pattern of a significant increase in the exposure-response due to high co-exposure is generally consistent with the above co-exposure models (Figs. 4a, 5, 6a, and 7).
Sensitivity analyses focused exclusively on the EHE and WFS definitions to explore whether varying the respective criteria influenced our inferential conclusions for these binary exposure variables. Varying the EHE definition based on different averaging days (2- versus 3-days) and percentile thresholds (95th versus 98th) did not change any of the overall observation that EHE exposure is associated with higher odds of mortality (Table S7, Supplemental Materials). Importantly, the EHE definition used for inference in our study (3-day average using 98th percentile threshold) resulted in the largest exposure-response relationship. For the WFS definition, using the HMS plume only to indicate a WFS day resulted in a much more attenuated exposure-response relationship.
Discussion
The findings from this time-stratified case-crossover study highlight the significant and complex relationships between PM2.5, temperature, and community all-cause mortality during wildfire seasons in the greater Vancouver area over a 13-year period. The results emphasize the combined effects of these environmental stressors, which have profound public health implications, particularly in the context of increasing frequency and severity with climate change. Most notably, the community mortality effects of PM2.5—which were temperature-dependent—are concentrated within a narrow range of moderately elevated concentrations, suggesting that such acute exposure may be under-appreciated in terms of our understanding of PM2.5 associated mortality risks.
Our study demonstrates a clear and strong association between hotter temperatures and higher community mortality during the greater Vancouver area’s warmest months. As expected, the exposure-response relationship between temperature and mortality appeared to be exponential, with a pronounced increase in the odds of death as mean daily temperatures exceeded 26 °C. When using EHE days to define exposure, effects on mortality were also significantly elevated. These findings align with the broader literature on the health effects of elevated daily temperature and extreme heat, which consistently shows up across multiple cities and countries as a critical risk factor for daily mortality22,28,29.
The relationships between PM2.5 exposure and community mortality were more nuanced compared with temperature, and therefore deserving of greater discussion. Specifically, same-day PM2.5 exposure did not consistently demonstrate a strong association with mortality across all PM2.5 exposure categories, particularly when adjusting for temperature. Another recent study from China also found that the exposure response relationship between PM2.5 categories on all-cause mortality resulted in stronger effect estimates at lower PM2.5 exposure categories compared with higher PM2.5 exposure categories. Specifically, PM2.5 exposure categories of 0–35 μg/m3, 35–75 μg/m3, and 115–150 μg/m3 were associated with a mortality increase of 1.07 (1.01, 1.13), 1.03 (1.00, 1.05), and 1.05 (1.01, 1.08), respectively30. A much larger study conducted across 652 cities in 24 countries found that the exposure-response relationship between acute PM2.5 exposure and mortality was steepest in cities with lower levels of PM2.5, lending further evidence of possible non-linear effects on mortality with effects concentrated in the lower spectrum of exposure31.
A pattern of PM2.5 exposure-response attenuation was observed with all other PM2.5 exposure metrics (continuous, WFS day, deciles, absolute ranges) after controlling for temperature or EHE exposure metrics. While other research has found attenuation in the health effect of PM2.5 after adjustment for heat exposure32, a possible explanation of these findings are that adjusting for hotter temperatures, to isolate the independent effect of increasing PM2.5 exposure, may constitute over-adjustment. Because we observed evidence of additive interaction between extreme PM2.5 and temperature exposures (Table 3), controlling for temperatures as a confounding factor might obscure the true combined effect of these co-exposures on mortality. This could contribute to biased estimation of the association of PM2.5 with mortality.
Our results suggested a non-linear relationship between PM2.5 and mortality. Only one of the exposure categories (12–14 µg/m³) was significantly associated with higher mortality after adjustment for temperature (Table 7), with the ORs diminishing or becoming null at the highest PM2.5 categories. Although less pronounced, there was also evidence of non-linearity with the decile-based exposure metrics. This paradoxical finding may have multiple explanations, such as biological saturation, where the cellular response to PM2.5 reaches a limit (59), or behavioral changes during high PM2.5 events, such as staying indoors and keeping windows and doors closed on high WFS days, which would reduce ambient PM2.5 exposure and likely contributes to exposure misclassification in our study33. Additionally, it is important to note that extremely high temperatures ( ≥ 26 °C) rarely coincided with days where PM2.5 concentrations exceeded 16 µg/m³. If we assume that the effect of PM2.5 is amplified by more extreme high temperatures, the lack of such heat occurrences during extreme high PM2.5 events could lead to a muted overall effect of PM2.5 on mortality. This suggests that the full impact of PM2.5 on mortality might be underestimated in situations where extreme heat is absent or infrequent, and that it would be valuable to repeat similar analyses in locations where both PM2.5 and temperature conditions are more extreme.
An important implication of the apparent non-linearity in the effects of PM2.5 on mortality is that current public health guidelines, such as the 24 h PM2.5 BC Air Quality Objective (AQO) of 25 µg/m³, may not adequately protect public health. In our study, most mortality impacts appear to have occurred at levels well below this threshold, a finding also reported by others15,34,35,36. The data from this study, along with findings from other research37,38, suggest significant WFS impacts beginning at PM2.5 levels much lower than the AQO. Taken together, moderately smoky conditions—rather than strictly extreme smoky conditions—tend to be the driver of mortality impacts. This indicates that the current AQO may need to be re-evaluated and potentially lowered to better account for the non-linear relationship between PM2.5 exposure and mortality risk in regions like greater Vancouver, especially during wildfire season when elevated PM2.5 concentrations are more frequent (Fig. 1).
The key finding from this study is the significant joint effects between PM2.5 and temperature on community mortality. Combined exposure to high levels of PM2.5 and temperature significantly increased the odds of mortality, but these joint effects were complex. The combined effects were most evident when PM2.5 exposure exceeded typical (i.e., median) background PM2.5 levels, where the odds of mortality increased substantially with increasing temperatures. This joint effect was markedly higher when mean daily temperatures exceeded 26 °C. Analyses of percentile-based exposure categories were generally consistent with this finding. Moreover, the influence of increasing PM2.5 levels on the magnitude of temperature effects also appeared to be non-linear, highlighting the complexities of this interaction.
Our results also suggest that a binary exposure classification (e.g., WFS or EHE) may be too crude when characterizing joint exposure-response relationships for WFS-derived PM2.5 and extreme heat. For instance, an apparent negative interaction was observed between WFS and EHEs on community mortality. This paradoxical result may be partially explained by the observed non-linear interaction associated with joint PM2.5 and temperature exposure. Moreover, our use of a binary exposure classification—especially for WFS—is subject to misclassification. Consistent with other studies from North America32,39,40,41, our WFS definition relied heavily on HMS satellite data from NOAA, an imperfect measure of actual surface-level smoky conditions. The sensitivity analyses showed that the exposure-response was even more attenuated when relying on the simpler metric of HMS plume only.
The uncertainty of HMS plume data as an indicator of WFS exposure stems from inherent limitations in spatial and temporal measurements of the satellite product. First, they do not delineate the vertical location of smoke in the atmospheric column, adding uncertainty as to whether the smoke is aloft at high altitudes or at the surface, especially for regions far afield from wildfire activity. There is added uncertainty spatially for the smoke plume edges, driven by the coarse spatial resolution of the satellite imagery and imagery displacement effects that are spatially dependent. Finally, HMS plume data are a snapshot in time, thus incapable of capturing the dynamic nature of smoke plume dispersion over hours or days. Even within an HMS polygon, there can be variations in the density (low, moderate, high) of smoke levels, adding to uncertainty in assigning PM2.5 to wildfires and defining WFS days42.
Our post hoc analysis suggested a greater-than-additive effect of same-day extreme PM2.5 and temperature exposure. This finding aligns with recent case-crossover studies employing time-stratified analyses, which also estimated significant greater-than-additive effects of extreme PM2.5 and temperature co-exposures9,13. Rahman et al. 9 reported a 5.4% (95% CI: 2.3, 7.8) excess mortality risk attributable to same-day co-exposure to > 90th percentile average PM2.5 and maximum temperature. Similarly, Xu et al. 13 estimated a 2.8% increase in the excess mortality risk from myocardial infarction was attributable to co-exposure to extreme temperature (2-day > 95th percentile) and PM2.5 (> 95th percentile) in Jiangsu province, China. Here, we estimated an excess community all-cause mortality risk of 7.9% (95% CI: 6.1, 9.1) attributable to same-day co-exposure to extreme ( > 90th percentile) average daily PM2.5 and temperature.
While the synergistic effects on excess mortality in our study are notably larger than those observed in the two case-crossover studies described above, this discrepancy may be explained by our focus on deaths that occurred outside of healthcare settings. People in the community, as opposed to those under care, may be more vulnerable due to several key factors. Firstly, although individuals in care settings such as long-term care facilities or hospitals may be biologically more susceptible to adverse health effects from environmental stressors, this susceptibility is often mitigated by factors like central air conditioning systems43, which can significantly reduce exposure to extreme PM2.5 and temperatures. For instance, one study in a Vancouver in-patient care facility during wildfire smoke episodes found indoor PM2.5 levels to be substantially lower than outdoor levels (29.6 ug/m3 vs. 72.0 ug/m3 respectively)44. Similarly, during the 2021 heat dome, the same facility reported indoor temperatures that were considerably cooler than those outdoors (23.6 °C vs. 27.2 °C), demonstrating the protective effect of such environments45.
In contrast, individuals in the Vancouver community typically lack access to central AC46 and reside in older buildings that exacerbate their exposure to environmental extremes. Recent data indicate that AC ownership in the Vancouver metropolitan area is significantly lower ( ~ 20%) compared to the national average in Canada (61%)46. This disparity is particularly problematic at night, when sustained warmer temperatures limit the body’s ability to cool down.
Moreover, while individuals in care settings benefit from proximal access to health monitoring and immediate medical interventions, those in the community must often travel to emergency rooms for medical assistance, which can be critical during emergencies. The lack of constant health monitoring and ready access to transportation exacerbates their vulnerability, especially during extreme events like heatwaves when emergency medical services are strained47. The 2021 BC coroner’s report highlights that most fatalities during BC’s 2021 EHE were among older adults with chronic diseases, living alone without adequate cooling or ventilation and resided in socially vulnerable communities48.
There are significant public health implications regarding the synergistic effects of co-exposure to PM2.5 and temperature on community mortality risk. However, fully understanding these implications requires a more refined and comprehensive analysis of when these synergistic effects are likely to occur in communities across differing levels of PM2.5 and temperature exposures. To date, only a few studies, including two in California9,49, one in Jiangsu province, China13, and this one have employed a time-stratified case-crossover design to investigate the joint effects of PM2.5 and temperature on individual-level mortality, yielding largely consistent results. These individual-level studies align with a broader body of ecological research that also demonstrates synergistic effects and additive excess risk of all-cause and cause-specific mortality from environmental co-exposures12,50,51,52,53. The consistent finding of an additive interaction between PM2.5 and temperatures over the 90th percentile suggests a possible temperature threshold where the combined effects begin to significantly exceed the independent effects9,50.
We observed a marked increase in the impact of PM2.5 on community mortality when temperatures reached and exceeded 26 °C. While this specific temperature threshold may not be generalizable to populations beyond greater Vancouver, it indicates that using absolute temperature categories, rather than only quantiles, can elucidate the daily temperatures at which PM2.5-related mortality risks are most severe. As noted earlier, the largest mortality effects for PM2.5 occurred far below the provincial 24 h AQO in BC and within a limited exposure range. This range also had extensive overlap with elevated temperature days. We note that one limitation of our PM2.5 and temperature categorization approach is that it may be less objective compared with quantile-based parameterizations. However, our analyses using quantile-based groupings showed a similarly complex interaction between PM2.5 and temperature.
As climate change continues to drive more frequent and severe wildfires and heatwaves, population exposure to these environmental hazards is expected to increase and complicate conventional public health approaches1. Our findings underscore the need for integrated public health strategies that address the combined risks of air pollution and extreme heat. Such strategies could include the development and implementation of early warning systems for combined PM2.5 and temperature, public education campaigns, and targeted interventions for susceptible populations to mitigate the adverse health effects when these environmental stressors co-occur23.
While this study provides valuable insights into the health effects of extreme heat and wildfire-related PM2.5 co-exposure, there are several limitations. First, exposure misclassification is a potential concern, as we relied on ML-based PM2.5 exposure estimation and satellite-based temperature measurements rather than measuring individual-level exposures. However, any misclassification is likely to be non-differential, which would bias results toward the null rather than create spurious associations, particularly when population exposure is common54. Second, although the time-stratified case-crossover design inherently controls for time-invariant confounders at the individual level, unmeasured time-varying confounders cannot be ruled out. We tested for potential confounding by holiday status and found no meaningful or significant impact on effect estimates. Additionally, while the COVID-19 pandemic occurred during our study period, its influence on exposure to wildfire-related PM2.5 and extreme heat is unlikely to introduce bias, as there is no strong evidence linking the pandemic to these environmental stressors. Lastly, given the relatively wide confidence intervals for some interaction effect estimates, caution is warranted when interpreting findings for specific exposure categories with lower precision. Despite these limitations, our study design and analytical approach help minimize bias, and our findings contribute to the understanding of the health risks associated with heat and wildfire smoke co-exposure.
This study provides timely insights into the all-cause community mortality risks associated with PM2.5 and temperature co-exposures in the greater Vancouver area. Our findings indicate significant, non-linear, and potentially synergistic interactions between these combined environmental stressors, underscoring the need for a comprehensive public health approach that addresses their combined effects under climate change. The evidence also suggests that current air quality standards may not fully protect public health, because significant mortality impacts occurred at PM2.5 levels well below existing thresholds. Additionally, the interaction between PM2.5 and heat appear to be more pronounced at specific temperature thresholds, emphasizing the importance of tailoring public health interventions to account for local contexts and susceptibilities, including the integration of early warning systems and targeted interventions for at-risk populations.
Methods
This study was conducted in the greater Vancouver region of British Columbia (BC), Canada between 2010 and 2022, during the warmer months (May-October) when wildfire activity is typical in BC (“wildfire season”) (Fig. 2b)55. This study area includes BC’s largest metropolitan regions, with a 2016 population (mid-point of study period) of approximately 2.46 million people, or approximately 53% of the provincial population56. The summer climate in the study area is typically temperate with excellent air quality. Over the study period, the mean temperature was 14.7 oC and the mean PM2.5 concentration was 7.4 µg/m3. Even so, this region experienced catastrophic EHEs in 2009 and 202157, and had prolonged periods of WFS exposure in 2010, 2014, 2015, 2017, 2018, 2020, 2021, and 2022 (Fig. 2b)55.
We selected this sub-region of BC because we aimed to study an area with relatively uniform exposures to hot temperatures and WFS impacts over a geographically dense urban population. This approach is crucial, given the regional differences in how populations adapt to hot temperatures, which can influence sensitivity for various health outcomes, including mortality.
Analyses were restricted to all 6-digit postal codes within Local Health Authorities (LHAs) in the southwestern mainland region of the BC Provincial Heat Alert and Response System (BC HARS). The BC HARS comprises five geographic regions each with its own temperature threshold criteria for issuing heat alerts to protect public health58. Postal codes were used to define the study area because they represent the smallest geographic unit recorded in the BC vital statistics records, which are described in more detail below. Six-digit postal codes are expressed as geographic points and linked to Canadian census geographies using the national Postal Code Conversion File. These are called single link indicators (SLIs) and they represent the geographic area with the majority of dwellings assigned to a particular postal code (analogous to population centroid)59.
Mortality and exposure data
Death records between 2010 and 2022 were extracted from the BC Vital Statistics Agency database, consistent with our previous work on the relationship between temperature and mortality in BC58,60. In this dataset, each death record includes the date of death, primary cause of death classified according to the International Classification of Diseases, 10th revision (ICD-10), age, sex, setting of death (e.g., acute care, private home, etc.), and the 6-digit postal code of the location where the death occurred60. We included all recorded community deaths of individuals with a BC residential postal code in the study area. Community deaths are defined as those that occurred outside of a care-providing facility, such as a hospital or long-term care home. We focused on community deaths based on our prior internal work showing they are more strongly associated with PM2.5 and temperature than mortality in all locations61. The weaker association with all deaths is likely due in part to people in care-providing facilities having protection from exposures due to air filtration and air conditioning requirements, as well as receiving medical or supportive care.
To provide a comprehensive assessment of the relationships between PM2.5, temperature, and all-cause community mortality we generated multiple exposure metrics (Table 8). These ranged from conventional measures such as continuous and binary exposures, to metrics with multiple exposure categories. The specific metrics are described in more detail below, and all exposure metrics were linked with the mortality data using the 6-digit residential postal code of each decedent.
Daily PM2.5 concentrations were assigned to all 6-digit postal codes in the study area by intersecting the geographic points of postal codes with predicted daily grid cell PM2.5 concentrations from the Canadian Optimized Statistical Smoke Exposure Model (CanOSSEM). CanOSSEM is a comprehensive machine learning model that combines satellite remote sensing data to optimize the estimation of PM2.5 concentrations from WFS and residential wood burning. CanOSSEM predictions of PM2.5 were generated at a spatial resolution of 5 km x 5 km grid cells, covering all populated areas of Canada, with high reported accuracy62.
To estimate the effect of PM2.5 pollution on all-cause community mortality and its interactive effects with different temperatures, we analyzed PM2.5 as a continuous exposure and alternatively classified PM2.5 into distinct exposure categories (Table 8). Specifically, we categorized the daily PM2.5 concentrations values into deciles and used values at or below the 50th percentile as the reference group to compare against each of the decile-based exposure group above the 50th percentile. As an alternative to using deciles, we also grouped PM2.5 concentrations as <6 µg/m3, ≥6–8 µg/m3, ≥8–10 µg/m3, ≥10–12 µg/m3, ≥12–14 µg/m3, ≥14–16 µg/m3, ≥16 µg/m3. The reference category of <6 µg/m3 was selected because it approximates the overall PM2.5 median during the study period (median = 6.1 µg/m3) and reflects periods where ambient air quality is not impacted by WFS in the study area (Fig. 2B). Establishing categories in 2 µg/m3 bins allows flexibility to explore how specific co-exposures to PM2.5 and temperature categories are associated with mortality in a potentially non-linear relationship.
We also derived a binary indicator of WFS exposure by identifying days impacted and not impacted by WFS, using the approach described by O’Dell and colleagues (28). First, we identified grid cells in CanOSSEM that intersected with a smoke plume, indicated by the daily Hazard Mapping System (HMS) smoke plume polygons provided by the US National Oceanic and Atmospheric Administration (NOAA)63. Based on assessment of satellite remote sensing data, HMS data provide an indication whether a plume was present in the atmospheric column (i.e., overhead) for an observed area. For each grid cell, we then calculated the long-term mean (meanno_plume) and standard deviation (SDno_plume) of CanOSSEM PM2.5 concentrations on days that did not intersect with an HMS polygon. Next, we added the meanno_plume and 1.5*SDno_plume, which represents a grid cell specific threshold for WFS impacts. For a grid cell to be defined as impacted by WFS on any given day, two criteria had to be met: (1) the grid cell intersected with an HMS plume and (2) the PM2.5 concentration exceeded the meanno_plume + 1.5* SDno_plume threshold. If these criteria were not met, the grid cell and intersecting postal code point(s) were classified as having no WFS impact on that day.
For temperature exposure assessment we used the average daily (24 h) value for each CanOSSEM grid cell and the overlapping postal code point(s), which were derived from the Modern-Era Retrospective Analysis for Research and Applications, Version 2 (MERRA-2)64. The MERRA-2 has a spatial resolution of 0.5° × 0.625°.
Temperature exposure metrics were then derived using continuous exposure and the same type of decile and absolute categorical exposure classifications used for PM2.5. The absolute temperature categories were: <14 °C, ≥ 14–17 °C, ≥17–20 °C, ≥20–23 °C, ≥23–26 °C, ≥26 °C. We chose < 14 °C as the reference category because it approximates the median temperature during the study period (median temperature = 14.5 °C).
Deciles of temperature exposure were calculated using the daily temperature values across the defined study area. Days with a mean temperature below the regional median ( < 50th percentile) of mean daily temperature were assigned as a reference group, with increasing increments of deciles assigned for all other days (50th–60th, 60th–70th, 70th–80th, 80th–90th, >90th).
Because EHEs typically involve consecutive days of exposure, we derived an EHE metric that accounts for this “heat wave” effect65,66. Specifically, for each day, we calculated the consecutive 3-day average temperatures (2-days prior, 1-day prior, and same day) for each CanOSSEM grid cell. Next, we calculated the month-specific 98th percentile of 3-day average temperatures by grid cell for the entire study period66,67,68,69,70. This 98th percentile was then used as a threshold to derive an indicator variable for extreme heat event (EHE) days within each postal code.
To facilitate comparison of our results with existing literature, we defined a co-exposure metric using mutually exclusive extreme exposure groups, similar to Rahman et al. 9 and Xu et al. 13. These two studies also used a case-crossover design to investigate the effects of co-exposure to PM2.5 and temperature extremes on mortality. Like these studies, we classified days as having extreme PM2.5 (>90th region-wide percentile) and/or extreme temperature ( > 90th location-specific percentile) and fit a model, using days without extreme PM2.5 or temperature as the reference group, to estimate the effect of the following mutually exclusive exposure groups: extreme PM2.5 days only, extreme temperature days only, and days with both extreme PM2.5 and extreme temperature.
Study design
The study employed a time-stratified case-crossover design, in which every case acts as its own control. The case-crossover design is useful for examining specific individual-level acute health outcomes (i.e., all-cause mortality) associated with short-term exposures (i.e., PM2.5 or temperature). By comparing exposure levels on the day of the event (case days) with those on similar days when the event did not occur (control days), the effect of the exposure on the event can be assessed. This approach helps adjust for unmeasured long-term and seasonal variable trends. Furthermore, it automatically adjusts for all individual-level time invariant (or slowly varying) characteristics (e.g., age, sex, lifestyle, comorbidities) as the comparisons are conducted within subject. We applied the time-stratified method, which selects control days from the same calendar month and weekday as the case day, minimizing biases related to time trends, seasonal exposures, and health event variations71.
Statistical analyses
Multivariable conditional logistic regression models were used to estimate the independent and joint associations between the exposure metrics and all-cause mortality. We fit several different models to provide a comprehensive view of the complex associations. All models were fit with decedents as their own stratum. For the stratified modeling, we subset the data to individuals who had a case or control day that fit the respective criteria. For example, a death was selected for a stratified analysis if any of its case or control days fell into the stratum of interest (e.g., ≥26 °C). Multiplicative interaction terms using most of the PM2.5 and temperature exposure metrics were fit to test for statistical interactions on mortality. We conducted the analyses using the clogit function from the survival package (version 3.4-0) in R (version 4.2.2). The full modeling results are provided in the Supplemental Materials (Tables S1–S6).
We performed post hoc analyses evaluating additive interaction effects of extreme PM2.5 and temperature by using the mutually exclusive extreme exposure groups9,13. To test additive interaction, we estimated relative excess odds due to interaction (REOI), proportion attributable to interaction (AP), and synergy index (S)13,72. We calculated confidence intervals (CIs) for these measures using the delta method, which approximates standard errors based on the regression estimates and their variances, following the approach recommended by Hosmer and Lemeshow73. We also adapted the approach in Rahman et al. 9 to estimate all-cause excess risk (ER) of mortality due to co-exposure. Here, a bootstrapping procedure with 1,000 iterations was applied, resampling from the data with replacement to generate an empirical distribution of ER estimates. The 95% CIs for ER were obtain using the percentile method, taking the 2.5th and 97.5th percentiles of the bootstrap distribution.
Sensitivity analyses were conducted to address certain assumptions in our analyses. Specifically, other analyses explored the sensitivity of mortality models to varying the EHE definition based on the number of averaging days (2-days, 3-days) and the percentile used for deriving the EHE temperature thresholds (95th percentile, 98th percentile). Finally, we also tested the sensitivity of mortality models using an alternate WFS day binary definition by defining a day impacted by WFS where there was an HMS smoke plume detected without any PM2.5 concentration threshold criterion.
Data availability
The data that support the findings of this study are not openly available but can be made available from the corresponding author upon reasonable request. Air quality and meteorological data are located in controlled access data storage at the British Columbia Centre for Disease Control. Data tables used for analysis include vital statistics records that can be accessed in the public domain, available through the BC Vital Statistics Agency.
Code availability
R code of conditional logistic regression analyses can be made available by the authors upon request.
References
Intergovernmental Panel on Climate Change. Climate Change 2021 – The Physical Science Basis: Working Group I Contribution to the Sixth Assessment Report of the Intergovernmental Panel on Climate Change. (Cambridge University Press, 2023). https://doi.org/10.1017/9781009157896.
Burke, M. et al. The contribution of wildfire to PM2.5 trends in the USA. Nature 1–6 https://doi.org/10.1038/s41586-023-06522-6 (2023).
Liu, J. C., Pereira, G., Uhl, S. A., Bravo, M. A. & Bell, M. L. A systematic review of the physical health impacts from non-occupational exposure to wildfire smoke. Environ. Res. 136, 120–132 (2015).
Chen, G. et al. Mortality risk attributable to wildfire-related PM2·5 pollution: a global time series study in 749 locations. Lancet Planet. Health 5, e579–e587 (2021).
Khatana, S. A. M., Werner, R. M. & Groeneveld, P. W. Association of Extreme Heat With All-Cause Mortality in the Contiguous US, 2008-2017. JAMA Netw. Open 5, e2212957 (2022).
Liu, J. et al. Heat exposure and cardiovascular health outcomes: a systematic review and meta-analysis. Lancet Planet. Health 6, e484–e495 (2022).
Rosenthal, N., Benmarhnia, T., Ahmadov, R., James, E. & Marlier, M. E. Population co-exposure to extreme heat and wildfire smoke pollution in California during 2020. Environ. Res. Clim. 1, 025004 (2022).
Austin, E., Kasner, E., Seto, E. & Spector, J. Combined Burden of Heat and Particulate Matter Air Quality in WA Agriculture. J. Agromedicine 26, 18–27 (2021).
Rahman, M. M. et al. The Effects of Coexposure to Extremes of Heat and Particulate Air Pollution on Mortality in California: Implications for Climate Change. Am. J. Respir. Crit. Care Med. 206, 1117–1127 (2022).
Heaney, A. et al. Impacts of Fine Particulate Matter From Wildfire Smoke on Respiratory and Cardiovascular Health in California. GeoHealth 6, e2021GH000578 (2022).
Grigorieva, E. & Lukyanets, A. Combined Effect of Hot Weather and Outdoor Air Pollution on Respiratory Health: Literature Review. Atmosphere 12, 790 (2021).
Anenberg, S. C., Haines, S., Wang, E., Nassikas, N. & Kinney, P. L. Synergistic health effects of air pollution, temperature, and pollen exposure: a systematic review of epidemiological evidence. Environ. Health Glob. Access Sci. Source 19, 130 (2020).
Xu, R. et al. Extreme Temperature Events, Fine Particulate Matter, and Myocardial Infarction Mortality. Circulation 148, 312–323 (2023).
Bowe, B., Xie, Y., Yan, Y. & Al-Aly, Z. Burden of Cause-Specific Mortality Associated With PM2.5 Air Pollution in the United States. JAMA Netw. Open 2, e1915834 (2019).
Weichenthal, S. et al. How low can you go? Air pollution affects mortality at very low levels. Sci. Adv. 8, eabo3381 (2022).
Dai, L., Zanobetti, A., Koutrakis, P. & Schwartz, J. D. Associations of Fine Particulate Matter Species with Mortality in the United States: A Multicity Time-Series Analysis. Environ. Health Perspect. 122, 837–842 (2014).
Krishna, B. et al. Daily nonaccidental mortality associated with short-term PM2.5 exposures in Delhi, India. Environ. Epidemiol. 5, e167 (2021).
Achebak, H., Devolder, D. & Ballester, J. Heat-related mortality trends under recent climate warming in Spain: A 36-year observational study. PLOS Med. 15, e1002617 (2018).
Zhang, Y. et al. The Short-Term Effect of Ambient Temperature on Mortality in Wuhan, China: A Time-Series Study Using a Distributed Lag Non-Linear Model. Int. J. Environ. Res. Public. Health 13, 722 (2016).
Gasparrini, A. et al. Small-area assessment of temperature-related mortality risks in England and Wales: a case time series analysis. Lancet Planet. Health 6, e557–e564 (2022).
Masselot, P. et al. Excess mortality attributed to heat and cold: a health impact assessment study in 854 cities in Europe. Lancet Planet. Health 7, e271–e281 (2023).
Shindell, D. et al. The Effects of Heat Exposure on Human Mortality Throughout the United States. GeoHealth 4, e2019GH000234 (2020).
Coker, E. S. et al. Climate change and health: rethinking public health messaging for wildfire smoke and extreme heat co-exposures. Front. Public Health 12, 1324662 (2024).
Canada, E. and C. C. About the Air Quality Health Index. https://www.canada.ca/en/environment-climate-change/services/air-quality-health-index/about.html (2007).
US Environmental Protection Agency. AQI Basics | AirNow.gov. https://www.airnow.gov/aqi/aqi-basics.
Canada, E. and C. C. Criteria for public weather alerts. https://www.canada.ca/en/environment-climate-change/services/types-weather-forecasts-use/public/criteria-alerts.html (2010).
US Department of Commerce, N. Heat Watch vs. Warning. https://www.weather.gov/safety/heat-ww.
Yu, W. et al. Daily average temperature and mortality among the elderly: a meta-analysis and systematic review of epidemiological evidence. Int. J. Biometeorol. 56, 569–581 (2012).
Luo, Q., Li, S., Guo, Y., Han, X. & Jaakkola, J. J. K. A systematic review and meta-analysis of the association between daily mean temperature and mortality in China. Environ. Res. 173, 281–299 (2019).
Ma, Z. et al. Short-term effects of different PM2.5 ranges on daily all-cause mortality in Jinan. China. Sci. Rep. 12, 5665 (2022).
Liu, C. et al. Ambient Particulate Air Pollution and Daily Mortality in 652 Cities. N. Engl. J. Med. 381, 705–715 (2019).
Evoy, R., Hystad, P., Bae, H. & Kincl, L. The impact of wildfire smoke and temperature on traumatic worker injury claims, Oregon 2009–2018. Health Sci. Rep. 5, 1–11 (2022).
Coker, E. S. et al. Enhancing Wildfire Smoke Exposure Assessment: A Machine Learning Approach to Predict Indoor PM2.5 in British Columbia, Canada. ACS EST Air https://doi.org/10.1021/acsestair.4c00204 (2024).
Henderson, S. B., Nguyen, P. D. M., Yao, J. A., & M. Lee. The public health paradox of wildfire smoke. BC Med. J. 66, 93, 95 (2024).
Christidis, T. et al. Low concentrations of fine particle air pollution and mortality in the Canadian Community Health Survey cohort. Environ. Health Glob. Access Sci. Source 18, 84 (2019).
Brauer, M. et al. Mortality–Air Pollution Associations in Low Exposure Environments (MAPLE): Phase 2. Res. Rep. Health Eff. Inst. 2022, 212 (2022).
Schneider, S. R., Lee, K., Santos, G. & Abbatt, J. P. D. Air Quality Data Approach for Defining Wildfire Influence: Impacts on PM2.5, NO2, CO, and O3 in Western Canadian Cities. Environ. Sci. Technol. 55, 13709–13717 (2021).
Lee, M. J. et al. Using low-cost air quality sensors to estimate wildfire smoke infiltration into childcare facilities in British Columbia, Canada. Environ. Res. Health 2, 025002 (2024).
Aguilera, R., Corringham, T., Gershunov, A. & Benmarhnia, T. Wildfire smoke impacts respiratory health more than fine particles from other sources: observational evidence from Southern California. Nat. Commun. 12, 1493 (2021).
O’Dell, K. et al. Estimated Mortality and Morbidity Attributable to Smoke Plumes in the United States: Not Just a Western US Problem. GeoHealth 5, e2021GH000457 (2021).
Zhou, X. et al. Excess of COVID-19 cases and deaths due to fine particulate matter exposure during the 2020 wildfires in the United States. Sci. Adv. 7, eabi8789 (2021).
Liu, T. et al. Is the smoke aloft? Caveats regarding the use of the Hazard Mapping System (HMS) smoke product as a proxy for surface smoke presence across the United States. Int. J. Wildland Fire 33, 1–31 (2024).
ASHRAE. Chapter 9: Health Care Facilities. (2019).
Nguyen, P. D. M. et al. Using Low-Cost Sensors to Assess Fine Particulate Matter Infiltration (PM2.5) during a Wildfire Smoke Episode at a Large Inpatient Healthcare Facility. Int. J. Environ. Res. Public. Health 18, 9811 (2021).
Dickson, J. M., Lee, M. J., Jones, K., Ebrahimi, G. & Henderson, S. B. Monitoring temperature variability inside a healthcare facility during an extreme heat event using low-cost sensors. J. Hosp. Manag. Health Policy 7, (2023).
Government of Canada, S. C. The prevalence of household air conditioning in Canada. https://www150.statcan.gc.ca/n1/pub/82-003-x/2023007/article/00002-eng.htm (2023).
Wettstein, Z. S., Hall, J., Buck, C., Mitchell, S. H. & Hess, J. J. Impacts of the 2021 heat dome on emergency department visits, hospitalizations, and health system operations in three hospitals in Seattle, Washington. J. Am. Coll. Emerg. Physicians Open 5, e13098 (2024).
Government of British Columbia. Extreme Heat and Human Mortality: A Review of Heat-Related Deaths in B.C. in Summer 2021: Report to the Chief Coroner of British Columbia. (2022).
Azzouz, M. et al. Does socioeconomic and environmental burden affect vulnerability to extreme air pollution and heat? A case-crossover study of mortality in California. J. Expo. Sci. Environ. Epidemiol. 1–9 https://doi.org/10.1038/s41370-024-00676-9 (2024).
Lee, W. et al. Synergic effect between high temperature and air pollution on mortality in Northeast Asia. Environ. Res. 178, 108735 (2019).
Hu, X. et al. Does air pollution modify temperature-related mortality? A systematic review and meta-analysis. Environ. Res. 210, 112898 (2022).
Li, J. et al. Modification of the effects of air pollutants on mortality by temperature: A systematic review and meta-analysis. Sci. Total Environ. 575, 1556–1570 (2017).
Areal, A. T., Zhao, Q., Wigmann, C., Schneider, A. & Schikowski, T. The effect of air pollution when modified by temperature on respiratory health outcomes: A systematic review and meta-analysis. Sci. Total Environ. 811, 152336 (2022).
Jurek, A. M., Greenland, S., Maldonado, G. & Church, T. R. Proper interpretation of non-differential misclassification effects: expectations vs observations. Int. J. Epidemiol. 34, 680–687 (2005).
Matz, C. J. et al. Health impact analysis of PM2.5 from wildfire smoke in Canada (2013–2015, 2017–2018). Sci. Total Environ. 725, 138506 (2020).
Government of Canada, S. C. Census Profile, 2016 Census - British Columbia [Province] and Canada [Country]. https://www12.statcan.gc.ca/census-recensement/2016/dp-pd/prof/details/page.cfm?Lang=E&Geo1=PR&Code1=59&Geo2=PR&Code2=01&SearchText=Canada&SearchType=Begins&SearchPR=01&B1=All&type=0 (2017).
https://www.canada.ca/en/health-canada/services/climate-change-health/extreme-heat.html Canada, H. Extreme heat events: Overview (2024).
BCCDC. Provincial-Heat-Alerting-Response-System.pdf. http://www.bccdc.ca/resource-gallery/Documents/Guidelines%20and%20Forms/Guidelines%20and%20Manuals/Health-Environment/Provincial-Heat-Alerting-Response-System.pdf (2023).
Canada, S. Postal Code Conversion File, March 2022 Postal Codes, 2022. Abacus Data Network (2022).
McLean, K. E. et al. Establishing Heat Alert Thresholds for the Varied Climatic Regions of British Columbia, Canada. Int. J. Environ. Res. Public. Health 15, 2048 (2018).
McLean, K. E., Lee, M. J., Coker, E. S. & Henderson, S. B. A population-based case-control analysis of risk factors associated with mortality during the 2021 western North American heat dome: focus on chronic conditions and social vulnerability. Environ. Res. Health 2, 035010 (2024).
Paul, N., Yao, J., McLean, K. E., Stieb, D. M. & Henderson, S. B. The Canadian Optimized Statistical Smoke Exposure Model (CanOSSEM): A machine learning approach to estimate national daily fine particulate matter (PM2.5) exposure. Sci. Total Environ. 850, 157956 (2022).
Operations, U. D. of C. N. N. E. S. D. and I. S. O. of S. and P. NOAA’s Office of Satellite and Product Operations. https://www.ospo.noaa.gov/Products/land/hms.html.
NASA. MERRA-2. https://gmao.gsfc.nasa.gov/reanalysis/MERRA-2/.
Khan, L. et al. The association of extreme environmental heat with incidence and outcomes of out-of-hospital cardiac arrest in British Columbia: A time series analysis. Resusc. Plus 17, 100560 (2024).
Xu, Z., FitzGerald, G., Guo, Y., Jalaludin, B. & Tong, S. Impact of heatwave on mortality under different heatwave definitions: A systematic review and meta-analysis. Environ. Int. 89–90, 193–203 (2016).
Toloo, G. S. et al. Socio-demographic vulnerability to heatwave impacts in Brisbane, Australia: a time series analysis. Aust. N. Z. J. Public Health 38, 430–435 (2014).
Kang, S.-H. et al. Heat, heat waves, and out-of-hospital cardiac arrest. Int. J. Cardiol. 221, 232–237 (2016).
Yin, P. et al. The added effects of heatwaves on cause-specific mortality: A nationwide analysis in 272 Chinese cities. Environ. Int. 121, 898–905 (2018).
Huang, C. et al. Mortality burden attributable to heatwaves in Thailand: A systematic assessment incorporating evidence-based lag structure. Environ. Int. 121, 41–50 (2018).
Wu, Y., Li, S. & Guo, Y. Space-Time-Stratified Case-Crossover Design in Environmental Epidemiology Study. Health Data Sci. 2021, 9870798 (2021).
Knol, M. J. & VanderWeele, T. J. Recommendations for presenting analyses of effect modification and interaction. Int. J. Epidemiol. 41, 514–520 (2012).
Hosmer, D. W. & Lemeshow, S. Confidence interval estimation of interaction. Epidemiol. Camb. Mass 3, 452–456 (1992).
Richardson, D. B. & Kaufman, J. S. Estimation of the Relative Excess Risk Due to Interaction and Associated Confidence Bounds. Am. J. Epidemiol. 169, 756–760 (2009).
Acknowledgements
This research took place on the traditional, ancestral, unceded territory of the xwməθkwəýəm (Musqueam), Skwxwú7mesh (Squamish), and səlilwətaɬ (Tsleil-Waututh) Nations. The authors acknowledge our own positions as uninvited guests on these lands.No external funding was used for this study.
Author information
Authors and Affiliations
Contributions
E.C. conceived of the study, wrote the manuscript and performed the statistical analysis. S.C. helped plan the statistical analysis and reviewed and edited the manuscript. D.M. reviewed and edited the manuscript. M.S. reviewed and edited the manuscript. S.H. conceived of the study, helped plan the statistical analysis, and reviewed and edited the manuscript. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Coker, E.S., Cleland, S.E., McVea, D. et al. The synergistic effects of PM2.5 and high temperature on community mortality in British Columbia. npj Clean Air 1, 15 (2025). https://doi.org/10.1038/s44407-025-00014-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s44407-025-00014-9