Abstract
Insulin-like growth factor binding protein 1 (IGFBP-1) is a potentially interesting marker for liver fat in NAFLD as it is exclusively produced by the liver and insulin is its main regulator. We determined whether measurement of fasting serum phosphorylated IGFBP-1 (fS-pIGFBP-1) helps to predict liver fat compared to routinely available clinical parameters and PNPLA3 genotype at rs738409. Liver fat content (proton magnetic resonance spectroscopy) was measured in 378 subjects (62% women, age 43 [30–54] years, BMI 32.7 [28.1–39.7] kg/m2, 46% with NAFLD). Subjects were randomized to discovery and validation groups, which were matched for clinical and biochemical parameters and PNPLA3 genotype. Multiple linear regression and Random Forest modeling were used to identify predictors of liver fat. The final model, % Liver Fat Equation’, included age, fS-pIGFBP-1, S-ALT, waist-to-hip ratio, fP-Glucose and fS-Insulin (adjusted R2 = 0.44 in the discovery group, 0.49 in the validation group, 0.47 in all subjects). The model was significantly better than a model without fS-pIGFBP-1 or S-ALT or S-AST alone. Random Forest modeling identified fS-p-IGFBP-1 as one of the top five predictors of liver fat (adjusted R2 = 0.39). Therefore, measurement of fS-pIGFBP-1 may help in non-invasive prediction of liver fat content.
Similar content being viewed by others
Introduction
NAFLD is closely associated with the metabolic syndrome (MetS) and predicts T2D independent of obesity1. Simple steatosis has recently been show to progress to non-alcoholic steatohepatitis (NASH) and clinically significant fibrosis2. Regarding diagnosis of NAFLD, a recent US Practice Guideline3 stated: “As liver biochemistries can be within normal ranges in patients with NAFLD, they may not be sufficiently sensitive to serve as screening tests… screening for NAFLD in adults attending primary care clinics or high-risk groups attending diabetes or obesity clinics is not advised at this time due to uncertainties surrounding diagnostic tests”. There is thus a need to develop such tests for NAFLD.
Insulin-like growth factor binding protein-1 (IGFBP-1) is one of six IGFBPs, which bind to and regulate bioavailability of insulin-like growth factor-1 (IGF-1)4. The liver exclusively produces IGFBP-1 in non-pregnant adults5. Insulin acutely decreases serum IGFBP-1 concentrations and is its major regulator in vivo in humans6. In addition to insulin, insulin sensitivity regulates serum IGFBP-1 concentrations7. fS-IGFBP-1 is lower in subjects with hepatic insulin resistance (IR) and high liver fat content than in subjects with preserved hepatic insulin sensitivity and low liver fat content7.
In NAFLD, fS-IGFBP-1 has been shown to be decreased in studies involving 142 Japanese subjects8, 48 Italian women9 and 49 African American and 77 Latino adolescents10. These studies did not compare models measuring IGFBP-1 alone or in combination with routinely available parameters associated with NAFLD such as age, gender, measures of obesity, glucose, insulin, lipids, liver enzymes to models without IGFBP-1.
Human hepatoma cells produce predominantly phosphorylated IGFBP-1 (pIGFBP-1)11. The majority of circulating IGFBP-1 is in a phosphorylated form12, which has the highest affinity for IGF-I11. These pIGFBP-1 assays utilize the antibodies and kits developed by one laboratory13,14 and thus avoid problems of standardization between laboratories unlike for measurement of e.g. insulin concentrations15. The concentration of phosphorylated but not other forms of IGFBP-1 associates with macrovascular complications in patients with T2D16 and pIGFBP-1 correlates better with cardiovascular risk factors than lesser-phosphorylated IGFBP-117. These data provide a rationale for measuring specifically pIGFBP-1 rather than IGFBP-1 as a marker of liver fat content and associated metabolic abnormalities.
There are no data on the relationship between pIGFBP-1 and liver fat content or comparing pIGFBP-1 to routinely available markers in prediction of liver fat content. Furthermore, a common (30% to 50% of all subjects) variant in the patatin-like phospholipase domain-containing protein 3 (PNPLA3) gene at rs738409 (encoding I148M) increases liver fat content and risk of NASH but is not associated with features of IR1. Studies developing tools for non-invasive diagnosis NAFLD might thus benefit of genotyping for this gene variant. Previous studies have not considered this gene variant and have been performed in relatively small cohorts (48 to 142 subjects8,9,10). In the present study, we determined whether measurement of fS-pIGFBP-1 concentrations helps in non-invasive prediction of liver fat content, when features known to be associated with liver fat content1 such as age, gender, liver function tests, measures of obesity and the PNPLA3 genotype at rs738409 are taken into account. To this end, we measured these parameters, fS-pIGFBP-1 and liver fat content (proton magnetic resonance spectroscopy [1H-MRS]) in 378 subjects.
Results
Subject characteristics
Characteristics of the study subjects are shown in Table 1. Of all subjects, 46% had NAFLD. The discovery (n = 252) and validation (n = 126) groups were comparable with respect to clinical and biochemical parameters and PNPLA3 genotype at rs739409 (Table 1).
Univariate analysis
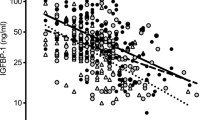
In univariate analysis in the discovery group, liver fat content was significantly inversely correlated with fS-pIGFBP-1 concentrations and significantly positively correlated with age, male gender, body mass index (BMI), waist circumference, increased liver enzyme, triglyceride, insulin and glucose concentrations and the PNPLA3 genotype at rs738409 (Table 2). The correlation coefficient between fS-Insulin and fS-pIGFBP-1 in all subjects was −0.51, P < 0.0001.
The variables were divided into groups measuring the same biological phenomenon such as measures of body composition or glycemia as shown in Table 2. The variables with best predictive value within each group in the discovery group, along with age, gender, fS-pIGFBP-1 and PNPLA3 genotype at rs738409, were used in development of an equation for prediction of liver fat and in Random Forest analyses.
Prediction of liver fat
The variables that had the best predictive value in the discovery group in univariate analysis were entered in multivariate linear regression analysis to create an equation for prediction of liver fat. The significant variables and their possible interactions were examined. The final variables for multiple linear regression analysis were derived using backward stepwise regression method based on Akaike Information Criteria (AIC). These variables were age, fS-pIGFBP-1, an interaction term (age times fS-pIGFBP-1), fS-alanine aminotransferase (ALT), waist-to-hip ratio, fasting plasma (fP)-Glucose and fS-Insulin. The final multiple linear regression model (‘% Liver fat equation’) in the discovery group (adjusted R2 = 0.44, P < 0.0001) is shown in Table 3. For calculation, Supplementary Table 1 can be used. The adjusted R2 was 0.49 in the validation group and 0.47 in all subjects. The adjusted R2 was 0.44 in all subjects, if fS-Insulin was omitted from the model (P < 0.0001 vs. the best model) and 0.46 if fS-pIGFBP-1 was omitted (P < 0.05 vs. the best model). The ‘% Liver fat equation’ also predicted liver fat significantly better than liver enzymes alone: aspartate aminotransferase (AST) only (adjusted R2 = 0.15), ALT only (adjusted R2 = 0.25), or both (adjusted R2 = 0.25, P < 0.0001 for all comparisons). The correlation coefficient between predicted liver fat content using ‘% Liver fat equation’ and liver fat measured using 1H-MRS was ρ = 0.62, P < 0.0001 (Fig. 1). The area under the receiver operator characteristic (AUROC) to predict NAFLD by ‘%Liver fat equation’ was 0.84 (0.80–0.88) which was significantly greater than that predicted by the Fatty Liver Index18 (0.72 [0.67–0.77], p < 0.0001) or the Hepatic Steatosis Index19 (0.62 [0.57–0.68], p < 0.0001).
The best predictors in univariate analysis within each group were also subjected to Random Forest modeling for prediction of liver fat (Fig. 2). This approach identified S-ALT, waist-to-hip ratio, fS-insulin, fS-triglycerides and fS-pIGFBP-1 as the top five variables explaining variation in liver fat content. The adjusted R2 was 0.39 in all subjects.
Discussion
We determined whether measurement of fS-pIGFBP-1 might help in the prediction of liver fat content in the face of other correlates of liver fat. The final model predicting liver fat included age, fS-pIGFBP-1, an interaction term (age times fS-pIGFBP-1), S-ALT, waist-to-hip ratio, fP-Glucose and fS-Insulin. The present data are novel in that we i) measured pIGFBP-1 rather than IGFBP-1, ii) did not study pIGFBP-1 in isolation but rather in combination with other markers of liver fat content including for the first time PNPLA3 genotype. The present dataset is also the hitherto largest in which IGFBP-1 or pIGFBP-1 and liver fat content have been quantitated.
Early studies measuring IGFBP-1 did not specify to what extent the assay measured phosphorylated forms of IGFBP-18,9,10,20,21. The median fS-pIGFBP-1 in the present study was 58 μg/l. This is in line with previously reported pIGFBP-1 concentrations ranging from 29 to 10012,16,17, which are markedly higher than concentrations of lesser-phosphorylated IGFPB-1 that range from 4 to 12 μg/l16,17. The phosphorylation status of IGFBP-1 alters its antigenicity22. Therefore immunoassays may grossly underestimate changes in IGFBP-1 concentrations23. In keeping with this, previous RIAs yielded mean fS-IGFBP-1 concentrations ranging from 16 to 20 μg/l7,24,25 and detected only a fraction of total IGFBP-1. Consistent with these data, in the subset of 23 subjects in the present study where we measured both IGFBP-1 using RIA and pIGFBP-1 using immunoenzymometric assay (IEMA), the mean concentration of fS-IGFBP-1 measured using RIA (18 μg/l) was much lower than that of fS-pIGFBP-1 measured using IEMA (58 μg/l).
The inverse relationship between liver fat content and pIGFBP-1 is consistent with previous data in diverse groups measuring IGFBP-1 using RIA or an immunoradiometric assay7,8,9,10. In the studies by Savastano et al. in 48 subjects9 and Kotronen et al. in 113 subjects7, the correlation coefficients between fS-IGFBP-1 and hepatic steatosis score (ultrasound) or liver fat (1H-MRS) were in both studies −0.38 (P < 0.01 or less). In the present study, the correlation coefficient between fS-pIGFBP-1 and liver fat (1H-MRS) in 378 subjects was −0.29 (P < 0.0001) and thus statistically comparable to the previous data in smaller groups of subjects (P = 0.5 for r = −0.29 in 378 subjects vs. r = −0.38 in 48 subjects9 and P = 0.3 for r = −0.29 in 378 subjects vs. r = −0.38 in 113 subjects7).
Multiple causes (measures of obesity, aging) and consequences (hypertriglyceridemia, hyperinsulinemia, hyperglycemia, increased liver enzymes) of IR are known to be significantly associated with increased liver fat1. This was also true in the present study and emphasizes the need to consider several parameters rather than one parameter in isolation when developing tools for non-invasive prediction of liver fat (Table 2). In addition, carriers of the I148M variant in the PNPLA3 gene at rs738409 have increased liver fat and liver enzyme concentrations but no features of IR26. We found the PNPLA3 I148M gene variant to be significantly associated with liver fat in univariate (Table 2) but not in multiple linear regression (Table 3) analyses. This could be because the PNPLA3 gene variant signals its influence via ALT, which remained a significant independent predictor in multiple linear regression analysis (Table 3). In addition to these established markers, fS-pIGFBP-1 was significantly associated with liver fat content in both univariate and multiple linear analyses.
In line with the significant interaction between age and fS-pIGFBP-1, IGFBP-1 has been shown to correlate with age independent of BMI27. Aging also associates with decreased suppression of IGFBP-1 by insulin27. Regarding mechanisms underlying the observed inverse relationship between fS-Insulin and fS-pIGFBP-1, the subjects with increased liver fat content also were hyperinsulinemic (Table 2). Thus the relationship could reflect insulin inhibition of production of IGFBP-1 in the liver5. Hepatic IR could also influence the slope of the relationship between fS-Insulin and fS-IGFBP-1. A fixed increment in serum insulin suppresses serum IGFBP-1 less in insulin-resistant than -sensitive subjects7. Of these two factors, i.e., insulin per se and hepatic insulin sensitivity, insulin may be the most important regulator of fS-IGFBP-1, as type 1 diabetic patients who lack the portal-peripheral insulin gradient have markedly higher fS-IGFBP-1 concentrations than matched non-diabetic subjects despite enhanced hepatic insulin sensitivity28,29.
We acknowledge limitations in our study. First, the study was cross-sectional and hence fails to prove cause and effect. Second, even when a multitude of factors known to be either causes or consequences of liver fat content were considered, a large proportion of the variation in liver fat remains unexplained. Direct measurement of liver fat content by ultrasound therefore would seem to be a more attractive tool, as it is widely available. This method has, however, the limitation that it lacks sensitivity in subjects with low liver fat content30 and accuracy in obese subjects31. 1H-MRS is considered to be the most accurate non-invasive method for assessing hepatic steatosis32 and it also does not expose to radiation but it is expensive and requires MRI and hence is not widely available. Compared to measurement of e.g. liver enzymes alone, the ‘%Liver fat equation’ was much better in capturing information of liver fat. The AUROC of the ‘%Liver fat equation’ (0.84) was significantly better than that of the Fatty liver Index (0.72) or the Hepatic Steatosis Index (0.62).
The variables included in equations predicting liver fat should be standardized to enable comparison between different laboratories and centers. Although fS-Insulin is perhaps the most popular laboratory test to assess insulin sensitivity, assay procedures are highly variable and measure various forms of insulin using divergent procedures15. In this context it is noteworthy that measurement of pIGFBP-1 for predicting pre-term delivery13,14 and lesser-phosphorylated IGFBP-1 for diagnosis of premature rupture of fetal membranes33 produced by a single manufacturer have become a worldwide standard. We thus conclude that measurement of fS-pIGFPB1 independently contributes to prediction of liver fat even when the known associates are considered and may thus be helpful in non-invasive estimation of liver fat content.
Materials and Methods
Subjects
The subjects (n = 378) were recruited for metabolic studies34 by newspaper advertisements, by contacting occupational health services, or amongst subjects referred to the Department of Gastroenterology because of chronically elevated serum transaminase concentrations using the following inclusion criteria: (i) age 18 to 75 years; (ii) no known acute or chronic disease except obesity or T2D based on medical history, physical examination, standard laboratory tests and electrocardiogram; (iii) alcohol consumption of less that 20 g per day. Study physicians assessed alcohol intake by using the same questionnaire addressing the quantity of different alcoholic drinks consumed during an average week. Exclusion criteria included pregnancy, serologic evidence of hepatitis B or C, autoimmune hepatitis, clinical signs or symptoms of inborn errors of metabolism, or a history of use of toxins or drugs associated with liver steatosis, antihypertensives possibly influencing glucose metabolism or thiazolidinediones. The study protocol was approved by the ethics committee of the Helsinki University Central Hospital and was carried out in accordance with the Declaration of Helsinki. Each participant provided written informed consent.
Metabolic study
The subjects were studied after an overnight fast. Body composition was measured as detailed below. Blood was withdrawn for measurement of plasma glucose concentration and serum total, HDL and low-density lipoprotein (LDL) cholesterol, triglyceride, glycosylated hemoglobin A1c (HbA1c), insulin, C-peptide, pIGFBP-1, ALT and AST concentrations. Blood samples were also taken for genotyping PNPLA3 at rs73840935.
Measurement of body composition
Waist circumference was measured midway between spina iliaca superior and the lower rib margin and hip circumference at the level of the greater trochanters. Body weight was recorded to the nearest 0.1 kg using a calibrated digital scale (Soehnle, Monilaite-Dayton, Finland) with subject barefoot and wearing light indoor clothing. Height was recorded to the nearest 0.5cm using a non-stretchable tape. BMI was defined as [weight (kg)/(height (m))2]. Body fat percentage was determined using a bioelectric impedance analysis (BioElectrical Impedance Analyzer System model #BIA-101A; RJL Systems, Detroit, MI).
Liver fat content measured using 1H-MRS
Liver fat was measured using 1H-MRS34. In 1H-MRS studies, the intensity differences arising from various acquisition parameters and localization techniques were normalized as previously described and liver fat content was expressed as mass fraction34. We have previously validated this measurement against histologically determined liver fat content36. NAFLD was defined as in the Dallas Heart Study (liver fat ≥5.56% by 1H-MRS)37.
Analytical procedures
Plasma glucose was measured using a hexokinase method on an autoanalyser (Roche Diagnostics Hitachi 917, Hitachi Ltd., Tokyo, Japan). Serum insulin and C-peptide concentrations were measured using time-resolved fluoroimmunoassay with respective Auto-DELFIA kits (Wallac, Turku, Finland). Serum HbA1c was measured using high-pressure liquid chromatography using the fully automated analyzer system (Bio-Rad, Richmond, CA). Serum triglyceride, total and HDL cholesterol concentrations were measured using the enzymatic kits from Roche Diagnostics using an autoanalyzer (Roche Diagnostics Hitachi, Hitachi Ltd., Tokyo, Japan). Serum LDL cholesterol concentrations were calculated using the Friedewald formula38. Serum ALT and AST activities were determined as recommended by the European Committee for Clinical Laboratory Standards using the Roche Diagnostics Hitachi 917.
Serum pIGFBP-1 concentrations were determined with an IEMA with a monoclonal antibody as the detecting antibody (Medix Biochemica, Kauniainen, Finland) according to the manufacturer’s instructions, as described before39. The assay uses a monoclonal antibody specific to human pIGFBP-1, which is immobilized on microwell plates and a monoclonal antibody specific to IGFBP-1, which is conjugated with horse-radish peroxidase. The intra- and interassay coefficients of variation were 2.7% to 7.8% and 3.9% to 10%, respectively. Each sample was assayed as a duplicate and the mean value was used. The detection limit the assay was 0.3 μg/l and the measuring range 1 to 200 μg/l. No cross-reactivity between other IGFBPs was seen. All sera were analyzed after storage at −80 C until analysis. The present series included 23 samples, which had been collected 5 years ago and in which fS-IGFBP-1 had been measured using a radioimmunoassay (RIA)7. These samples were re-assayed with the IEMA detecting fS-pIGFBP-1. The mean concentrations were 18 ± 2 μg/l with the RIA and 57 ± 8 μg/l with the IEMA (P < 0.001). The correlation coefficient between the two measurements was 0.64, P < 0.001 (Suppl. Fig. 1). In these samples, the correlation coefficient between liver fat and pIGFBP-1 was −0.45 (P = 0.029) and IGFBP-1 −0.45 (P = 0.033).
Statistical analyses
The subjects were randomly divided using bootstrap randomization into discovery (2/3 of the subjects) and validation (1/3 of the subjects) groups. All subjects were used as the second validation group. Normality of distribution of continuous variables was tested using Kolmogorov-Smirnov test. The Mann-Whitney U and Chi-square tests were used to compare the validation and discovery groups. Spearman’s rank correlation coefficient was used for univariate analysis. Liver fat content and circulating parameters were used as continuous variables and non-normally distributed data after logarithmic (base 10) transformation.
We used linear regression and Random Forest prediction models to estimate the liver fat content. For both models, we entered variables that significantly correlated with liver fat in univariate analyses in the discovery group. To avoid multi-collinearity, we entered one variable from a group of variables reflecting the same biological phenomenon (body composition, liver enzymes, glycemia, insulinemia and lipids) as shown in Results in Table 2. The final variables for multiple linear regression analysis were derived using backward stepwise regression method based on AIC. We applied multiple linear regression analyses to create an equation to estimate liver fat content and evaluated the model using adjusted coefficient of determination (R2). Predictive models were compared using the F-test based on the residual sum of squares adjusted for the total number of variables in each model. To compare the accuracy of the equation with the Fatty Liver Index18 and the Hepatic Steatosis Index19, we used their respective reference values and for the created equation the 5.56% reference value37 as a cut-off for NAFLD and compared the AUROCs using the DeLong method40. In the Random Forest modeling, the optimal number of variables on each tree was defined based on the estimation of out-of-Bag error. By using the predictors described above, 500 regression trees were trained in the discovery group. The predictability of each variable was estimated by cross-validating its relationship with the outcome in the validation group and all subjects. A variable importance plot based on the importance score summarized the importance of each predictor. Correlation coefficients were compared statistically using the Fisher r-to-z transformation41.
We considered a P-value of less than 0.05 statistically significant. Using a sample size of 378 subjects, a power of 80% and a P-value of 0.05, a linear correlation coefficient of 0.144 or over can be detected. Calculations were made using R Project for Statistical Computing version 3.1.1 (www.r-project.org/, Vienna, Austria) and GraphPad Prism version 6.00 for Windows (GraphPad Software, San Diego, CA).
Additional Information
How to cite this article: Petäjä, E. M. et al. Phosphorylated IGFBP-1 as a non-invasive predictor of liver fat in NAFLD. Sci. Rep. 6, 24740; doi: 10.1038/srep24740 (2016).
References
Yki-Järvinen, H. Non-alcoholic fatty liver disease as a cause and a consequence of metabolic syndrome. Lancet Diabetes Endocrinol 2, 901–910 (2014).
McPherson, S. et al. Evidence of NAFLD progression from steatosis to fibrosing-steatohepatitis using paired biopsies: Implications for prognosis and clinical management. J. Hepatol. 62, 1148–1155 (2015).
Chalasani, N. et al. The diagnosis and management of non-alcoholic fatty liver disease: Practice guideline by the American Association for the Study of Liver Diseases, American College of Gastroenterology and the American Gastroenterological Association. The American journal of gastroenterology 107, 811–826 (2012).
Firth, S. M. & Baxter, R. C. Cellular actions of the insulin-like growth factor binding proteins. Endocr. Rev. 23, 824–854 (2002).
Brismar, K., Fernqvist-Forbes, E., Wahren, J. & Hall, K. Effect of insulin on the hepatic production of insulin-like growth factor-binding protein-1 (IGFBP-1), IGFBP-3 and IGF-I in insulin-dependent diabetes. J. Clin. Endocrinol. Metab. 79, 872–878 (1994).
Suikkari, A. M., Koivisto, V. A., Koistinen, R., Seppälä, M. & Yki-Järvinen, H. Dose-response characteristics for suppression of low molecular weight plasma insulin-like growth factor-binding protein by insulin. J. Clin. Endocrinol. Metab. 68, 135–140 (1989).
Kotronen, A., Lewitt, M., Hall, K., Brismar, K. & Yki-Järvinen, H. Insulin-like growth factor binding protein 1 as a novel specific marker of hepatic insulin sensitivity. J. Clin. Endocrinol. Metab. 93, 4867–4872 (2008).
Wasada, T. et al. Hepatic steatosis rather than visceral adiposity is more closely associated with insulin resistance in the early stage of obesity. Metab. Clin. Exp. 57, 980–985 (2008).
Savastano, S. et al. Liver-spleen axis, insulin-like growth factor-(IGF)-I axis and fat mass in overweight/obese females. J Transl Med 9, 136 (2011).
Alderete, T. L. et al. Relationships between IGF-1 and IGFBP-1 and adiposity in obese African-American and Latino adolescents. Obesity (Silver Spring) 19, 933–938 (2011).
Jones, J. I., D’Ercole, A. J., Camacho-Hubner, C. & Clemmons, D. R. Phosphorylation of insulin-like growth factor (IGF)-binding protein 1 in cell culture and in vivo: effects on affinity for IGF-I. Proc. Natl. Acad. Sci. USA 88, 7481–7485 (1991).
Coverley, J. A. & Baxter, R. C. Phosphorylation of insulin-like growth factor binding proteins. Mol. Cell. Endocrinol. 128, 1–5 (1997).
Riboni, F. et al. Biochemical markers predicting pre-term delivery in symptomatic patients: phosphorylated insulin-like growth factor binding protein-1 and fetal fibronectin. Arch. Gynecol. Obstet. 284, 1325–1329 (2011).
Rahkonen, L. et al. Cervical length measurement and cervical phosphorylated insulin-like growth factor binding protein-1 testing in prediction of preterm birth in patients reporting uterine contractions. Acta Obstet Gynecol Scand 88, 901–908 (2009).
Singh, B. & Saxena, A. Surrogate markers of insulin resistance: A review. World J Diabetes 1, 36–47 (2010).
Heald, A. H. et al. Low circulating levels of insulin-like growth factor binding protein-1 (IGFBP-1) are closely associated with the presence of macrovascular disease and hypertension in type 2 diabetes. Diabetes 51, 2629–2636 (2002).
Borai, A. et al. Serum insulin-like growth factor binding protein-1 (IGFBP-1) phosphorylation status in subjects with and without ischaemic heart disease. Atherosclerosis 208, 593–598 (2010).
Bedogni, G. et al. The Fatty Liver Index: a simple and accurate predictor of hepatic steatosis in the general population. BMC Gastroenterol 6, 33 (2006).
Lee, J.-H. et al. Hepatic steatosis index: a simple screening tool reflecting nonalcoholic fatty liver disease. Dig Liver Dis 42, 503–508 (2010).
Maddux, B. A., Chan, A., De Filippis, E. A., Mandarino, L. J. & Goldfine, I. D. IGF-binding protein-1 levels are related to insulin-mediated glucose disposal and are a potential serum marker of insulin resistance. 29, 1535–1537 (2006).
Rajpathak, S. N. et al. Insulin-like growth factor axis and risk of type 2 diabetes in women. Diabetes 61, 2248–2254 (2012).
Westwood, M., Gibson, J. M., Davies, A. J., Young, R. J. & White, A. The phosphorylation pattern of insulin-like growth factor-binding protein-1 in normal plasma is different from that in amniotic fluid and changes during pregnancy. J. Clin. Endocrinol. Metab. 79, 1735–1741 (1994).
Mehta, S., Livingstone, C., Borai, A. & Ferns, G. Insulin-like growth factor binding protein-1 in insulin resistance and cardiovascular disease. British Journal of Diabetes & Vascular Disease 12, 17–25 (2012).
Lewitt, M. S. et al. Insulin-like growth factor-binding protein-1 in the prediction and development of type 2 diabetes in middle-aged Swedish men. Diabetologia 51, 1135–1145 (2008).
Mohamed-Ali, V. et al. Insulin-like growth factor binding protein-1 in NIDDM: relationship with the insulin resistance syndrome. Clinical Endocrinology 50, 221–228 (1999).
Sookoian, S. & Pirola, C. J. Meta-analysis of the influence of I148M variant of patatin-like phospholipase domain containing 3 gene (PNPLA3) on the susceptibility and histological severity of nonalcoholic fatty liver disease. Hepatology 53, 1883–1894 (2011).
Rutanen, E. M., Kärkkäinen, T., Stenman, U. H. & Yki-Järvinen, H. Aging is associated with decreased suppression of insulin-like growth factor binding protein-1 by insulin. J. Clin. Endocrinol. Metab. 77, 1152–1155 (1993).
Yki-Järvinen, H., Mäkimattila, S., Utriainen, T. & Rutanen, E. M. Portal insulin concentrations rather than insulin sensitivity regulate serum sex hormone-binding globulin and insulin-like growth factor binding protein 1 in vivo. J. Clin. Endocrinol. Metab. 80, 3227–3232 (1995).
Llauradó, G. et al. Liver fat content and hepatic insulin sensitivity in overweight patients with type 1 diabetes. J. Clin. Endocrinol. Metab. 100, 607–616 (2015).
Ryan, C. K., Johnson, L. A., Germin, B. I. & Marcos, A. One hundred consecutive hepatic biopsies in the workup of living donors for right lobe liver transplantation. Liver Transpl. 8, 1114–1122 (2002).
Mottin, C. C. et al. The role of ultrasound in the diagnosis of hepatic steatosis in morbidly obese patients. Obes Surg 14, 635–637 (2004).
Bohte, A. E., van Werven, J. R., Bipat, S. & Stoker, J. The diagnostic accuracy of US, CT, MRI and 1H-MRS for the evaluation of hepatic steatosis compared with liver biopsy: a meta-analysis. Eur Radiol 21, 87–97 (2011).
Rutanen, E. M. et al. Evaluation of a rapid strip test for insulin-like growth factor binding protein-1 in the diagnosis of ruptured fetal membranes. Clin. Chim. Acta 253, 91–101 (1996).
Kotronen, A. et al. Prediction of non-alcoholic fatty liver disease and liver fat using metabolic and genetic factors. Gastroenterology 137, 865–872 (2009).
Kotronen, A. et al. A common variant in PNPLA3, which encodes adiponutrin, is associated with liver fat content in humans. Diabetologia 52, 1056–1060 (2009).
Kotronen, A., Vehkavaara, S., Seppälä-Lindroos, A., Bergholm, R. & Yki-Järvinen, H. Effect of liver fat on insulin clearance. Am. J. Physiol. Endocrinol. Metab. 293, E1709–15 (2007).
Szczepaniak, L. S. et al. Magnetic resonance spectroscopy to measure hepatic triglyceride content: prevalence of hepatic steatosis in the general population. Am. J. Physiol. Endocrinol. Metab. 288, E462–8 (2005).
Friedewald, W. T., Levy, R. I. & Fredrickson, D. S. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin. Chem. 18, 499–502 (1972).
Nuutila, M., Hiilesmaa, V., Kärkkäinen, T., Ylikorkala, O. & Rutanen, E. M. Phosphorylated isoforms of insulin-like growth factor binding protein-1 in the cervix as a predictor of cervical ripeness. Obstet Gynecol 94, 243–249 (1999).
DeLong, E. R., DeLong, D. M. & Clarke-Pearson, D. L. Comparing the Areas under Two or More Correlated Receiver Operating Characteristic Curves: A Nonparametric Approach. Biometrics 44, 837 (1988).
Fisher, R. A. On the “Probable Error” of a Coefficient of Correlation Deduced from a Small Sample. Metron 1, 3–32 (1921).
Acknowledgements
We gratefully acknowledge Katja Sohlo, Mia Urjansson, Anne Salo and Aila Karioja-Kallio (Helsinki University Central Hospital, Department of Medicine), Pentti Pölönen (Helsinki University Central Hospital, HUS Medical Imaging Center, Radiology), Marja-Leena Lehtiniemi and Tea Rostela (United Medix Laboratories) for skillful technical assistance; Satu Vehkavaara, M.D., Ph.D. and Robert Bergholm, M.D., Ph.D. for their contributions; and volunteers for their help. This study was supported by research grants from the Academy of Finland (HY), EU/EFPIA Innovative Medicines Initiative Joint Undertaking (EMIF grant no. 115372, HY), the Sigrid Juselius (HY), the Novo Nordisk (HY) Foundations and EVO (HY, NL). The authors (HY) are members of the EPoS (Elucidating Pathways of Steatohepatitis) consortium funded by the Horizon 2020 Framework Program of the European Union under Grant Agreement 634413.
Author information
Authors and Affiliations
Contributions
E.P. and Y.Z. analyzed the data. E.P. and H.Y.-J. interpreted the data and wrote the main text. M.H. and J.I. supervised the pIGFBP-1 assays. A.H. and N.L. performed and interpreted the 1H-MRS studies. H.Y.-J. designed and supervised the project. All authors reviewed the manuscript.
Ethics declarations
Competing interests
E.M.P., Y.Z., M.H., A.H., N.L. and H.Y.J. have nothing to declare. J.I. has worked as a consultant for Medix Biochemica.
Electronic supplementary material
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Petäjä, E., Zhou, Y., Havana, M. et al. Phosphorylated IGFBP-1 as a non-invasive predictor of liver fat in NAFLD. Sci Rep 6, 24740 (2016). https://doi.org/10.1038/srep24740
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep24740