Abstract
Many drugs and xenobiotics are lipophilic and they should be transformed into more polar water soluble compounds to be excreted. Cimetidine inhibits cytochrome P450. The aim of this study was to investigate the preventive and/or reversal action of cimetidine on cytochrome P450 induction and other metabolic alterations provoked by the carcinogen p-dimethylaminoazobenzene. A group of male CF1 mice received a standard laboratory diet and another group was placed on dietary p-dimethylaminoazobenzene (0.5% w w−1). After 40 days of treatment, animals of both groups received p-dimethylaminoazobenzene and two weekly doses of cimetidine (120 mg kg−1, i.p.) during a following period of 35 days. Cimetidine prevented and reversed δ-aminolevulinate synthetase induction and cytochrome P450 enhancement provoked by p-dimethylaminoazobenzene. However, cimetidine did not restore haem oxygenase activity decreased by p-dimethylaminoazobenzene. Enhancement in glutathione S-transferase activity provoked by p-dimethylaminoazobenzene, persisted in those animals then treated with cimetidine. This drug did not modify either increased lipid peroxidation or diminution of the natural antioxidant defence system (inferred by catalase activity) induced by p-dimethylaminoazobenzene. In conclusion, although cimetidine treatment partially prevented and reversed cytochrome P450 induction, and alteration on haem metabolism provoked by p-dimethylaminoazobenzene AB, it did not reverse liver damage or lipid peroxidation. These results further support our hypothesis on the necessary existence of a multiple biochemical pathway disturbance for the onset of hepatocarcinogenesis initiation.
Similar content being viewed by others
Main
Cytochrome P450 (P450) plays a key role in the oxidative metabolism of drugs and xenobiotics, many of which are lipophilic and to be excreted they should be transformed into more polar water soluble molecules by the system of hepatic mono-oxygenases (Lim and Lu, 1998).
P450 can be influenced by a number of exogenous and endogenous factors (Whitlock and Denison, 1995) and its induction and inhibition is of the utmost interest in carcinogenesis (Toussaint et al, 1993).
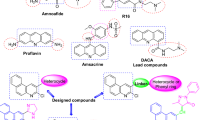
We have earlier proposed a mechanism for the onset of hepatocarcinogenesis involving an activating status of the whole liver which reflected an important and sustained increase in P450 levels, leading to biochemical aberrations in haem metabolism which in turn would lead to the tumorigenic process (Gerez et al, 1997). We have also suggested that reactive oxygen species (ROS), produced during carcinogenesis chemically induced by p-dimethylaminoazobenzene (DAB), would be involved in the generation of hepatic lesions (Gerez et al, 1998a, b) and the so triggered peroxidative damage would be implicated in the initiation step of hepatocarcinogenesis.
The development of cancer is a dynamic process of de-regulation of gene function. Accumulation of damage alters gene function and clonal expansion of mutated cells (Cerutti, 1994). During drug metabolism, generated reactive oxygen species (ROS) play a key role in several stages of carcinogenesis (Halliwell, 1999; Caballero et al, 2001).
Cimetidine (CIM) is a H2-histamine receptor antagonist clinically used in the treatment of peptic ulcers and other gastric acid-related disorders (Chang et al, 1992a). It inhibits hepatic mixed-function oxidase activity (Baird et al, 1987) and it appears that CIM is a more potent inhibitor of hepatic P450 when administered in vivo than when it is added to microsomes in vitro (Chang et al, 1992b).
The presence of a high affinity binding site for CIM on P450 in liver microsomes, with both the imidazole and cyano positions of CIM interacting with the hemin iron is well documented. Ranitidine, a structurally dissimilar H2-histamine antagonist, not inhibiting hepatic mixed-function oxidases, has not a binding site on P450, suggesting therefore that CIM would alter the oxidative metabolism of some compounds by having a direct inhibitory effect on P450. If CIM exerts a significant general effect upon haem biosynthetic and/or degradative pathway, we would expect these effects to be manifest in both P450 and in other haem containing proteins when animals are treated with CIM (Baird et al, 1987).
Since elucidation of a specific form of microsomal P450 exclusively associated with azoreduction remains elusive (Zbaida, 1995), we have shown that administration of DAB to mice, remarkably increases total P450 and that these changes are associated with hepatoxicity and lipid peroxidation, leading to the carcinogenesis onset. Considering that in our experimental model, the sustained P450 induction provoked as a consequence of the carcinogen metabolism, is responsible for the liver injury and the peroxidative damage, our aim was to investigate if diminution of P450 caused by CIM could avoid the biochemical aberrations associated with the initiation stage of hepatocarcinogenesis (Gerez et al, 1998a, 1998b; Caballero et al, 2001).
Materials and methods
Chemicals
Chemicals were reagent grade and purchased from Sigma Chemical Co. (St. Louis, MO, USA).
Animals and treatment
Male CF1 mice (30 g) received a standard laboratory diet (SLD, Purina 3, Asociación de Cooperativas Argentinas, San Nicolás, Buenos Aires) (groups A, n=16) or were placed on dietary p-dimethylaminoazobenzene (DAB, 0.5%, w/w) (groups B, n=16). After 40 days, animals of both groups (A and B) received DAB and two weekly doses of CIM (120 mg kg−1 i.p.) (ACIM; BCIM) or saline (AS, BS) for a following period of 35 days (Mera et al, 1994). Other group (CIM) of animals (n=6) received SLD along the whole period of assay and were injected with CIM under the same scheduled protocol than the DAB treated groups. Animals of control group (n=6) were fed with the SLD and received saline i.p. twice a week for the same period. The treatment protocol is shown in Figure 1. All animals were given food and water ad libitum.
All animals were inspected at least twice daily. Body weight and food consumption were measured at intervals throughout the study. Food was removed from animals 16 h before sacrifice. Mice were killed (at least six animals per group) under ether anaesthesia at the indicated times and liver samples were processed immediately as previously described (Gerez et al, 1998a). All animals received human care and were treated in accordance with guidelines established by the Animal Care and Use Committee of the Argentine Association of Specialists in Laboratory Animals (AADEALC) and in accordance with the UK Guidelines for the Welfare of Animals in Experimental Neoplasia (UKCCCR, 1998).
Assays
δ-Aminolevulinic acid synthetase (ALA-S) activity was measured as described by Marver et al (1966) and microsomal haem oxygenase (HO) activity according to Yoshida and Kikuchi (1978).
Cytochrome P450 (P450) content was determined in the microsomal fraction according to Omura and Sato (1964). Glutathione S transferase (GST) was determined by the method of Habig et al (1974). Catalase was measured as described by Chance and Maehly (1955).
The lipid peroxidation (LP) index was evaluated by the formation of malondialdehyde and determined as thiobarbituric acid reactive species (TBARS) by the method of Niehaus and Samuelson (1968). Protein concentration was determined by the method of Lowry et al (1951). Enzyme units (U) were defined as the amount of enzyme producing 1 nmol of product or consuming 1 nmol of substrate (catalase) under the standard incubation conditions. Specific activity (Sp. Act.) was expressed as U mg−1 protein.
Statistical analysis
Newman-Keuls test was used to assess the degree of significance. A probability level of 0.05 was used in testing for significant differences between controls and treated animals.
Results
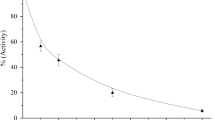
As already shown, DAB induced a significant increase in P450 content (Gerez et al, 1997) and as expected CIM provoked 40% reduction in P450 levels (Nanji et al, 1994). Simultaneous administration of CIM and DAB (ACIM) partially prevented the enhancement of P450 content. When animals were pre-treated with DAB and then received CIM (BCIM) induction of P450 was also partially reversed. In both cases, after CIM treatment P450 levels were still 50% above basal levels (Figure 2).
Effect of CIM on hepatic P450 levels. Animals were treated under the experimental protocol, described in Figure 1. Open bar CIM, hatched bars Treatment groups A, solid bars Treatment groups B. The data represent mean values±s.d. and are expressed as percentage of the corresponding mean control values of SLD fed animals without any other treatment, for each time point. Saline control group (mean±s.d.): P450=0.34±0.03 nmol mg−1 protein. Significantly different (P<0.05) from saline treated group * and the corresponding DAB group (AS or BS) **.
It has already been reported that CIM could reduce the activity of hepatic ALA-S induced by allylisopropylacetamide (AIA) in porphyric adult rats (Marcus et al, 1990) and that CIM could also be used in the prophylaxis of human acute intermittent porphyria by maintaining a baseline suppression of ALA-S activity (Horie et al, 1995; Rogers, 1997). In this study, CIM itself inhibited 40% ALA-S activity. CIM also prevented ALA-S induction provoked by DAB restoring basal levels at the end of the treatment (ACIM) and even partially reversed this induction in animals pre-treated with DAB (BCIM), achieving a 43% diminution respect to the BS group (Figure 3a).
Effect of CIM on hepatic ALA-S (A) and HO (B) activities. Saline control group (mean±s.d.): ALA-S=1.4 × 10−4±0.3 × 10−4 U mg−1 protein; HO=2.25±0.11 U mg−1 protein. Other experimental conditions and symbols are as indicated in Materials and Methods and legends to Figures 1 and 2. Significantly different (P<0.05) from saline treated group * and the corresponding DAB group (AS or BS) **.
CIM was found to inhibit both in vivo and in vitro the rate limiting enzymes of haem degradation, and it was suggested that the drug itself or a metabolite would inhibit HO (Marcus et al, 1984). In our experimental system, CIM given alone inhibited 25% HO activity and no effect was detected on the reduction of HO activity already provoked by DAB (Figure 3b).
Catalase is a haem protein present in high concentration in mammalian liver. Although administration of CIM to mice affects the synthesis and degradation of haem, no alteration in catalase activity had been described so far (Baird et al, 1987). In this study, CIM did not modify catalase activity in either controls or in DAB treated animals. Instead, as previously reported (Caballero et al, 2001) a significant inhibition has been observed in animals receiving only the carcinogen (AS: 50%; BS: 74%) (Figure 4a).
Effect of CIM on hepatic catalase activity (A) and LP (TBARS content, B). Saline control group (mean±s.d.): TBARS=135 × 10−3± 24 × 10−3 nmol mg−1 protein; Catalase=1.9 × 103±0.2 × 103 U mg−1 protein. Other experimental conditions and symbols are as indicated in Materials and Methods and legends to Figures 1 and 2. Significantly different (P<0.05) from * saline treated group and the ** corresponding DAB group (AS or BS) .
It was demonstrated that CIM could not prevent CCl4-induced LP in vivo (Cluet et al, 1986). Johnston and Kroening (1998) have observed that CIM inhibited LP in primary rats hepatocytes in culture but it did not reduce hepatocyte death induced by CCl4. We have found here that CIM alone did not produce any alteration in the LP index. Co-treatment (DAB+CIM) did not modify increased LP produced by DAB (ACIM: 110%; BCIM: 220%) (Figure 4b).
As expected CIM produced only 25% increase in GST activity. The significant enhancement (110%) in GST activity provoked by DAB (Gerez et al, 1998b) persisted in those animals also receiving CIM (Figure 5).
Effect of CIM on hepatic GST activity. The data represent mean values±s.d. and are expressed as percentage of the corresponding mean control values of SLD fed animals without any other treatment, for each time point. Saline control group (mean±s.d.): GST=1.45±0.25 U mg−1 protein. Other experimental conditions and symbols are as indicated in Materials and Methods and legends to Figures 1 and 2. Significantly different (P<0.05) from * saline treated group and the ** corresponding DAB group (AS or BS).
Discussion
CIM a substituted imidazole, has been well documented to inhibit hepatic P450 mediated drug metabolism in rats and humans (Chang et al, 1992b). Numerous drug-drug interactions involving CIM have been identified, in most cases, due to inhibition of hepatic drug metabolism by CIM occurring at very low serum concentrations (Chang et al, 1992b). In vitro addition of CIM to hepatic microsomes has been shown to inhibit the P450 catalysed oxidation of many substrates, considering CIM as a general inhibitor of P450 enzymes, although Reilly et al (1988) have suggested that there is in fact a more selective action for CIM. It was also proposed, that the varying effects of CIM on P450 enzymes could be attributed to different CIM binding affinities for these mixed function oxidases (Faux and Combes, 1993). The inhibitory effect of CIM on the metabolic activity of CYP2C9, 2C19, 2D6 y 3A was recently demonstrated in human liver microsomes (Furuta et al, 2001).
P450 induction is important in the pathogenesis of alcoholic hepatic diseases and it has been demonstrated that CIM can prevent alcoholic hepatic injury by reducing LP (Nanji et al, 1994). Mera et al (1994) have also investigated whether CIM might prevent CCl4 induced liver cirrhosis by preventing the increase in hepatic collagen content and/or LP. They did found a protective effect of CIM, which was attributed to a reduction in P450. They have also observed that CIM stimulated the regenerative process.
Quantitative ultrastructural studies of CIM treated rat liver showed a significant proliferation of smooth endoplasmic reticulum, changes which were qualitatively similar to those produced by phenobarbital (Wright et al, 1991).
We have demonstrated here that CIM partially prevented and reversed the induction of P450 levels produced by the carcinogenic agent DAB. Because DAB metabolism through the mono-oxygenase system is responsible for liver damage, decrease in P450 could ameliorate or delay this process (Yan et al, 1998). However, the significant increase in GST activity provoked by DAB still persisted in animals also receiving CIM, indicating that reduction in P450 by CIM is not enough to completely overcome DAB toxicity and suggesting that other mechanisms would be participating in the whole process.
CIM restored ALA-S basal levels induced by DAB, but it did not reverse HO inhibition. If administration of CIM to mice would affect haem synthesis, changes in the activity of any haem protein such as catalase, would be expected. However, we did not observe any changes in either DAB treated or control animals. It has been previously demonstrated that neither acute nor chronic treatment of mice with CIM produced any effect on catalase or had any action on haem metabolism, or it did interact with any haem containing protein (Baird et al, 1987). Thus, both our evidence and that of others is consistent with the hypothesis proposing that CIM alters the metabolism of some compounds through its specific interaction with P450.
Therefore, as a result of DAB metabolism, ROS and reactive nitrogen species (RNS) are generated. Free radicals induced LP and the role of free radicals in carcinogenesis is also well known (Cerutti, 1994). LP index, greatly enhanced in animals fed with DAB, was not modified by CIM, consequently liver cytotoxicity should be ascribed to oxidative stress and it was here demonstrated by the persistent increase in GST activity.
We have also shown that free radicals excess was not modified by CIM in animals subjected to the carcinogenic diet, and as a consequence catalase inhibition was not affected by co-treatment of DAB and CIM. This irreversible autocatalytic process produces then a continuous increase in ROS and RNS generation leading to a desbalance between radicals and the antioxidant defence system (Pigeolet et al, 1990).
It is noteworthy, that increased GST, diminished catalase, and enhanced LP reflecting initiation of carcinogenesis (Gerez et al, 1998a, b; Caballero et al, 2001), were not modified by CIM, in spite of its partial reversal in the increased P450 levels.
These results further support our hypothesis about the necessary multiple biochemical pathway disturbances for the onset of hepatocarcinogenesis initiation (Figure 6).
These findings also provide evidence for the importance of animal experiments in studying the multiple action and crosstalk among different biochemical pathways provoked by the administration of xenobiotics.
Change history
16 November 2011
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Baird MB, Sfeir GT, Slade-Pacini CD (1987) Lack of inhibition of mouse catalase activity by cimetidine: an argument against a relevant general effect of cimetidine upon heme metabolic pathways. Biochem Pharmacol 36: 4366–4369
Caballero F, Gerez E, Olveri L, Falcoff N, Batlle A, Vazquez E (2001) On the promoting action of tamoxifen in a model of hepatocarcinogenesis induced by p-dimethylaminoazobenzene in CF1 mice. Int J Biochem Cell Biol 33: 681–690
Cerutti P (1994) Oxy-radicals, cancer. Lancet 344: 862–863
Chance B, Maehly A (1955) Assay of catalases and peroxidases. In Methods Enzymology Vol 2: Chance E, Maehly A (eds) pp. 764–768, New York: Academic Press
Chang T, Levine M, Bandiera SM, Bellward GD (1992a) Selective inhibition of rat hepatic microsomal cytochrome P-450. I. Effect of the in vivo administration of cimetidine. J Pharmacol Exp Ther 260: 1441–1449
Chang T, Levine M, Bellward GD (1992b) Selective inhibition of rat hepatic microsomal cytochrome P-450. II. Effect of the in vitro administration of cimetidine. J Pharmacol Exp Ther 260: 1450–1455
Cluet JL, Boisset M, Boudene C (1986) Effect of pretreatment with cimetidine or phenobarbital on lipoperoxidation in carbon tetrachloride- and trichloroethylene-dosed rats. Toxicology 38: 91–102
Faux SP, Combes RD (1993) Interaction of cimetidine with cytochrome P450 and effect on mixed-function oxidase activities of liver microsomes. Hum Exp Toxicol 12: 147–152
Furuta S, Kamada E, Suzuki T, Sugimoto T, Kawabata Y, Shinozaki Y, Sano H (2001) Inhibition of drug metabolism in human liver microsomes by nizatidine, cimetidine and omeprazole. Xenobiotica 31: 1–10
Gerez E, Vazquez E, Caballero F, Polo C, Batlle A (1997) Altered heme pathway regulation and drug metabolizing enzyme system in a mouse model of hepatocarcinogenesis. Effect of veronal. Gen Pharmac 29: 569–573
Gerez E, Caballero F, Vazquez E, Polo C, Batlle A (1998a) Hepatic enzymatic metabolism alterations oxidative stress during the onset of carcinogenesis: protective role of α-tocopherol. Eur J Cancer Prevention 7: 69–76
Gerez E, Vazquez E, Caballero F, Batlle A (1998b) Beta-carotene partially prevents the damage induced by 1,4-dimethylaminoazobenzene. Eur J Cancer Prevention 7: 337–342
Habig W, Pabst M, Jakoby W (1974) Glutathione S-transferases. The first enzymatic step in mercapturic acid formation. J Biol Chem 249: 7130–7139
Halliwell B (1999) Oxygen and nitrogen are pro-carcinogens. Damage to DNA by reactive oxygen, chlorine and nitrogen species: measurement, mechanism and the effects of nutrition. Mutat Res 443: 37–52
Horie Y, Norimoto M, Tajima F, Sasaki H, Nanba E, Kawasaki H (1995) Clinical usefulness of cimetidine treatment of acute relapse in intermittent porphyria. Clin Chim Acta 234: 171–175
Johnston DE, Kroening C (1998) Mechanism of early carbon tetrachloride toxicity in cultured rat hepatocytes. Pharmacol Toxicol 83: 231–239
Lim JH, Lu AYH (1998) Inhibition and induction of cytochrome P450 and the clinical implications. Clin Pharmacokinet 35: 361–390
Lowry O, Rosebrough N, Farr A, Randall R (1951) Protein measurement with -the Folin- phenol reagent. J Biol Chem 193: 265–275
Marcus DL, Halbrech JL, Bourque AL, Lew G, Nadel H, Freedman ML (1984) Effect of cimetidine on delta-aminolevulinic acid synthase and microsomal heme oxygenase in rat liver. Biochem Pharmacol 33: 2005–2008
Marcus DL, Nadel H, Lew G, Freedman ML (1990) Cimetidine suppresses chemically induced experimental hepatic porphyria. Am J Med Sci 300: 214–217
Marver H, Tschudy D, Perlroth M, Collins A (1966) δ-aminolevulinic acid synthetase. I. Studies in liver homogenates. J Biol Chem 241: 2803–2809
Mera E, Muriel P, Castillo C, Mourelle L (1994) Cimetidine prevents and partially reverses CCl4-induced liver cirrhosis. J Appl Toxicol 14: 87–90
Nanji AA, Zhao S, Khwaja S, Sadrzadeh SM, Waxman DJ (1994) Cimetidine prevents alcoholic hepatic injury in the intragastric feeding rat model. J Pharmacol Exp Ther 269: 832–837
Niehaus W, Samuelson B (1968) Formation of malonaldehyde from phospholipids arachidonate during microsomal lipid peroxidation. Eur J Biochem 6: 126–130
Omura T, Sato R (1964) The carbon monoxide binding pigment of liver microsomes. J Biol Chem 239: 2370–2378
Pigeolet E, Corbisier P, Houbion A, Lambert B, Michiels C, Raes M, Zachary M, Remacle J (1990) Glutathione peroxidase, superoxide dismutase and catalase inactivation by peroxides and oxygen derived free radicals. Mech Ageing Dev 51: 283–297
Reilly PE, Mason SR, Gilliam EM (1988) Differential inhibition of human liver phenacetim O-deethylation by histamine and for histamine H2-receptor antagonists. Xenobiotica 18: 381–387
Rogers PD (1997) Cimetidine in the treatment of acute intermittent porphyria. Ann Pharmacother 31: 365–367
Toussaint C, Albin N, Massaad L, Grunenwald D, Parise O, Morizet J, Gouyette A, Chaot G (1993) Main drugs and carcinogen-metabolizing enzyme systems in human non-small cell lung cancer and peritumoral tissues. Cancer Res 53: 4608–4612
UKCCCR-UK Coordinating Committee on Cancer Research (1998) Guidelines for the Welfare of Animals in Experimental Neoplasia: London.
Whitlock J, Denison M (1995) Induction of cytochrome P450 enzymes that metabolize xenobiotics. In Cytochrome P450: Structure, mechanisms and biochemistry 2nd edition, Ortiz de Montellano P (ed) pp 367–390, New York: Plenum Press
Wright AW, Winzor DJ, Reilly PE (1991) Cimetidine: an inhibitor and an inducer of rat liver microsomal cytochrome P-450. Xenobiotica 21: 193–203
Yan Y, Higashi K, Yamamura K, Fukamachi Y, Abe T, Gotoh S, Sugiura T, Hirano T, Higashi T, Ichiba M (1998) Different responses other than the formation of DNA-adducts between the livers of carcinogen-resistant rats (DRH) and carcinogen-sensitive rats (Donryu) to 3′-methyl-4-dimethylaminoazobenzene administration. Jpn J Cancer Res 89: 806–813
Yoshida T, Kikuchi G (1978) Purification and properties of heme oxygenase from pig spleen microsomes. J Biol Chem 253: 4224–4229
Zbaida S (1995) The mechanism of microsomal azoreduction: predictions based on electronic aspects of structure-activity relationships. Drug Metab Rev 27: 497–516
Acknowledgements
A Batlle and E Vazquez are members of the Career of Scientific Researcher at the Argentine National Research Council (CONICET). F Caballero and E Gerez hold the post of Research Assistants at the CONICET. This work has been supported by grants from the CONICET (105508/99 and 4108/96), the Agencia de Promoción Científica y Tecnológica (No 5-00000-01861) and the University of Buenos Aires (N° TW 065), Argentina. This work was presented in part at the 17th International Congress of Biochemistry and Molecular Biology, May 1999, San Francisco, CA, USA. Its Abstract was published in FASEB J 13 (7): A1564, 1999.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Caballero, F., Gerez, E., Batlle, A. et al. Interaction of cimetidine with P450 in a mouse model of hepatocarcinogenesis initiation. Br J Cancer 86, 630–635 (2002). https://doi.org/10.1038/sj.bjc.6600102
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/sj.bjc.6600102
Keywords
This article is cited by
-
Ex vivo carbon monoxide prevents cytochrome P450 degradation and ischemia/reperfusion injury of kidney grafts
Kidney International (2008)