Abstract
Purpose
The objective of this study is to assess whether baseline optic nerve head (ONH) topography and retinal nerve fiber layer thickness (RNFLT) are predictive of glaucomatous visual-field progression in glaucoma suspect (GS) and glaucomatous eyes, and to calculate the level of risk associated with each of these parameters.
Methods
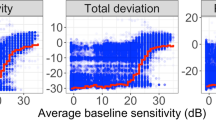
Participants with ≥28 months of follow-up were recruited from the longitudinal Advanced Imaging for Glaucoma Study. All eyes underwent standard automated perimetry (SAP), confocal scanning laser ophthalmoscopy (CSLO), time-domain optical coherence tomography (TDOCT), and scanning laser polarimetry using enhanced corneal compensation (SLPECC) every 6 months. Visual-field progression was assessed using pointwise linear-regression analysis of SAP sensitivity values (progressor) and defined as significant sensitivity loss of >1 dB/year at ≥2 adjacent test locations in the same hemifield at P<0.01. Cox proportional hazard ratios (HR) were calculated to determine the predictive ability of baseline ONH and RNFL parameters for SAP progression using univariate and multivariate models.
Results
Seventy-three eyes of 73 patients (43 GS and 30 glaucoma, mean age 63.2±9.5 years) were enrolled (mean follow-up 51.5±11.3 months). Four of 43 GS (9.3%) and 6 of 30 (20%) glaucomatous eyes demonstrated progression. Mean time to progression was 50.8±11.4 months. Using multivariate models, abnormal CSLO temporal-inferior Moorfields classification (HR=3.76, 95% confidence interval (CI): 1.02–6.80, P=0.04), SLPECC inferior RNFLT (per −1 μm, HR=1.38, 95% CI: 1.02–2.2, P=0.02), and TDOCT inferior RNFLT (per −1 μm, HR=1.11, 95% CI: 1.04–1.2, P=0.001) had significant HRs for SAP progression.
Conclusion
Abnormal baseline ONH topography and reduced inferior RNFL are predictive of SAP progression in GS and glaucomatous eyes.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Weinreb RN, Khaw PT . Primary open-angle glaucoma. Lancet 2004; 363: 1711–1720.
Zangwill LM, Bowd C, Berry CC, Williams J, Blumenthal EZ, Sanchez-Galeana CA et al. Discriminating between normal and glaucomatous eyes using the Heidelberg Retina Tomograph, GDx Nerve Fiber Analyzer, and Optical Coherence Tomograph. Arch Ophthalmol 2001; 119: 985–993.
Medeiros FA, Zangwill LM, Bowd C, Weinreb RN . Comparison of the GDx VCC scanning laser polarimeter, HRT II confocal scanning laser ophthalmoscope, and stratus OCT optical coherence tomograph for the detection of glaucoma. Arch Ophthalmol 2004; 122: 827–837.
Sehi M, Grewal DS, Sheets CW, Greenfield DS . Diagnostic ability of Fourier-domain vs time-domain optical coherence tomography for glaucoma detection. Am J Ophthalmol 2009; 148: 597–605.
Zangwill LM, Weinreb RN, Berry CC, Smith AR, Dirkes KA, Liebmann JM . The confocal scanning laser ophthalmoscopy ancillary study to the ocular hypertension treatment study: study design and baseline factors. Am J Ophthalmol 2004; 137: 219–227.
Zangwill LM, Weinreb RN, Beiser JA, Berry CC, Cioffi GA, Coleman AL et al. Baseline topographic optic disc measurements are associated with the development of primary open-angle glaucoma: the Confocal Scanning Laser Ophthalmoscopy Ancillary Study to the Ocular Hypertension Treatment Study. Arch Ophthalmol 2005; 123: 1188–1197.
Weinreb RN, Zangwill LM, Jain S, Becerra LM, Dirkes K, Piltz-Seymour JR et al. Predicting the onset of glaucoma: the confocal scanning laser ophthalmoscopy ancillary study to theOcular Hypertension Treatment Study. Ophthalmology 2010; 117: 1674–1683.
Strouthidis NG, Gardiner SK, Owen VM, Zuniga C, Garway-Heath DF . Predicting progression to glaucoma in ocular hypertensive patients. J Glaucoma 2010; 19: 304–309.
Medeiros FA, Alencar LM, Zangwill LM, Bowd C, Sample PA, Weinreb RN . Prediction of functional loss in glaucoma from progressive optic disc damage. Arch Ophthalmol 2009; 127: 1250–1256.
Vizzeri G, Weinreb RN, Martinez de la Casa JM, Alencar LM, Bowd C, Balasubramanian M et al. Clinicians agreement in establishing glaucomatous progression using the Heidelberg retina tomograph. Ophthalmology 2009; 116: 14–24.
Mohammadi K, Bowd C, Weinreb RN, Medeiros FA, Sample PA, Zangwill LM . Retinal nerve fiber layer thickness measurements with scanning laser polarimetry predict glaucomatous visual field loss. Am J Ophthalmol 2004; 138: 592–601.
Lalezary M, Medeiros FA, Weinreb RN, Bowd C, Sample PA, Tavares IM et al. Baseline optical coherence tomography predicts the development of glaucomatous change in glaucoma suspects. Am J Ophthalmol 2006; 142: 576–582.
Gardiner SK, Johnson CA, Demirel S . Cup size predicts subsequent functional change in early glaucoma. Optom Vis Sci 2011; 88: 1470–1476.
Sehi M, Guaqueta DC, Greenfield DS . An enhancement module to improve the atypical birefringence pattern using scanning laser polarimetry with variable corneal compensation. Br J Ophthalmol 2006; 90: 749–753.
Lemij HG, Reus NJ . New developments in scanning laser polarimetry for glaucoma. Curr Opin Ophthalmol 2008; 19: 136–140.
Zhou Q . Retinal scanning laser polarimetry and methods to compensate for corneal birefringence. Bull Soc Belge Ophtalmol 2006; 302: 89–106.
Zhou Q, Weinreb RN . Individualized compensation of anterior segment birefringence during scanning laser polarimetry. Invest Ophthalmol Vis Sci 2002; 43: 2221–2228.
Greenfield DS, Knighton RW, Huang XR . Effect of corneal polarization axis on assessment of retinal nerve fiber layer thickness by scanning laser polarimetry. Am J Ophthalmol 2000; 129: 715–722.
Alencar LM, Bowd C, Weinreb RN, Zangwill LM, Sample PA, Medeiros FA . Comparison of HRT-3 glaucoma probability score and subjective stereophotograph assessment for prediction of progression in glaucoma. Invest Ophthalmol Vis Sci 2008; 49: 1898–1906.
Hitchings RA, Migdal CS, Wormald R, Poinooswamy D, Fitzke F . The primary treatment trial: changes in the visual field analysis by computer-assisted perimetry. Eye 1994; 8: 117–120.
De Moraes CG, Juthani VJ, Liebmann JM, Teng CC, Tello C, Susanna Jr R et al. Risk factors for visual field progression in treated glaucoma. Arch Ophthalmol 2011; 129: 562–568.
Gordon MO, Beiser JA, Brandt JD, Heuer DK, Higginbotham EJ, Johnson CA et al. The Ocular Hypertension Treatment Study: baseline factors that predict the onset of primary open-angle glaucoma. Arch Ophthalmol 2002; 120: 714–720.
Jonas JB, Dichtl A . Evaluation of the retinal nerve fiber layer. Surv Ophthalmol 1996; 40: 369–378.
De Moraes CG, Demirel S, Gardiner SK, Liebmann JM, Cioffi GA, Ritch R et al. Effect of treatment on the rate of visual field change in the ocular hypertension treatment study observation group. Invest Ophthalmol Vis Sci 2012; 53: 1704–1709.
Sung KR, Kim S, Lee Y, Yun SC, Na JH . Retinal nerve fiber layer normative classification by optical coherence tomography for prediction of future visual field loss. Invest Ophthalmol Vis Sci 2011; 52: 2634–2639.
Jonas JB, Gusek GC, Naumann GO . Optic disc, cup and neuroretinal rim size, configuration and correlations in normal eyes. Invest Ophthalmol Vis Sci 1988; 29: 1151–1158.
Acknowledgements
This study was supported by NIH Grant R01-EY013516, Bethesda, MD, USA; P30EY014801 University of Miami Core Grant; unrestricted grant from Research to Prevent Blindness, New York, NY, USA; and Department of Defense Grant to University of Miami (DOD-Grant number W81XWH-09-1-0675). Dr Greenfield has received research support from Carl Zeiss Meditec Inc.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Presented in part at the Annual Meeting of American Glaucoma Society, Dana Port, CA, USA, on 5 March 2011
Appendix A
Appendix A
Advanced Imaging for Glaucoma (AIG) Study Group: (1) Bascom Palmer Eye Institute, University of Miami, Palm Beach Gardens, FL, USA: DS Greenfield, M Sehi, CD Quinn, K Kishor; (2) University of Pittsburgh Medical Center, Pittsburgh, PA, USA: JS Schuman, G Wollstein, H Ishikawa, RJ Noecker, Larry Kagemann; (3) Doheny Eye Institute, University of Southern California, Los Angeles, CA, USA: R Varma, V Chopra, B Francis; (4) Casey Eye Institute, Oregon Health and Science University, Portland, OR, USA: D Huang, J Morrison, P Francis, B Edmunds, M Parikh, D Gatty, R Armour, L Lombardi, O Tan, Xinbo Zhang, Yimin Wang. See www.AIGStudy.net for the full list of authors.
Rights and permissions
About this article
Cite this article
Sehi, M., Bhardwaj, N., Chung, Y. et al. Evaluation of baseline structural factors for predicting glaucomatous visual-field progression using optical coherence tomography, scanning laser polarimetry and confocal scanning laser ophthalmoscopy. Eye 26, 1527–1535 (2012). https://doi.org/10.1038/eye.2012.203
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/eye.2012.203
Keywords
This article is cited by
-
Prediction of Visual Field Progression in Patients with Primary Open-Angle Glaucoma, Mainly Including Normal Tension Glaucoma
Scientific Reports (2017)
-
Baseline thickness of macular ganglion cell complex predicts progression of visual field loss
Graefe's Archive for Clinical and Experimental Ophthalmology (2014)