Abstract
Purpose
To evaluate the clinical outcome of Descemet stripping automated endothelial keratoplasty (DSAEK) in eyes with iridocorneal endothelial (ICE) syndrome.
Patients and methods
A retrospective case series study was conducted. Eighteen consecutive Chinese patients with 20 DSAEK grafts were enrolled. Participants were evaluated by anterior segment optical coherence tomography and confocal microscopy. Postoperative complications, graft survival, endothelial cell counts, corneal thickness, and anterior chamber depth were analysed. A Log-rank test in a Kaplan–Meier analysis and a Cox proportional hazard regression were used to analyse potential risk factors of graft failure.
Results
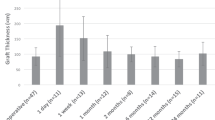
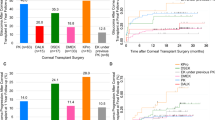
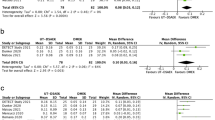
The mean follow-up duration was 19.0±8.6 months. The donors’ endothelial cell density (ECD) (cells/mm2) values at 1, 3, 6, 12, 18, and 24 months were 3342.2±287.0, 1897.6±745.4, 1793.6±755.7, 1618.1±604.3, 1421.9±650.8, 1265.1±844.1, and 1148.2±1217.8, respectively. Eleven of the 20 grafts exhibited secondary graft failure, with a mean estimated graft survival of 23.4 months. Immediate postoperative complications (air bubble ventilation for elevated intraocular pressure or rebubbling for graft detachment) were more common in eyes exhibiting graft failure (P=0.040). Postkeratoplasty glaucoma surgery emerged as a risk factor of graft failure, with a hazard ratio of 5.174. Eyes with a poor prognosis showed statistically greater central corneal thickness at 1 month, greater graft thickness at 3 months, and a shallower anterior chamber at 6 and 12 months.
Conclusions
The long-term outcome of DSAEK in eyes with ICE syndrome is relatively poor. Immediate postoperative complications, postkeratoplasty glaucoma surgery, thicker corneal parameters, and a shallow anterior chamber were all associated with graft failure.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Sacchetti M, Mantelli F, Marenco M, Macchi I, Ambrosio O, Rama P . Diagnosis and management of iridocorneal endothelial syndrome. BioMed Res Int 2015; 2015: 763093.
Hirst LW, Bancroft J, Yamauchi K, Green WR . Immunohistochemical pathology of the corneal endothelium in iridocorneal endothelial syndrome. Invest Ophthalmol Vis Sci 1995; 36: 820–827.
Malhotra C, Pandav SS, Gupta A, Jain AK . Phenotypic heterogeneity of corneal endothelium in iridocorneal endothelial syndrome by in vivo confocal microscopy. Cornea 2014; 33: 634–637.
Buxton JN, Lash RS . Results of penetrating keratoplasty in the iridocorneal endothelial syndrome. Am J Ophthalmol 1984; 98: 297–301.
Crawford GJ, Stulting RD, Cavanagh HD, Waring GO 3rd . Penetrating keratoplasty in the management of iridocorneal endothelial syndrome. Cornea 1989; 8: 34–40.
Chang PC, Soong HK, Couto MF, Meyer RF, Sugar A . Prognosis for penetrating keratoplasty in iridocorneal endothelial syndrome. Refract Corneal Surg 1993; 9: 129–132.
DeBroff BM, Thoft RA . Surgical results of penetrating keratoplasty in essential iris atrophy. J Refract Corneal Surg 1994; 10: 428–432.
Alvim PT, Cohen EJ, Rapuano CJ, Chung CW, Pereira ML, Eagle RC Jr et al. Penetrating keratoplasty in iridocorneal endothelial syndrome. Cornea 2001; 20: 134–140.
Quek DT, Wong CW, Wong TT, Han SB, Htoon HM, Ho CL et al. Graft failure and intraocular pressure control after keratoplasty in iridocorneal endothelial syndrome. Am J Ophthalmol 2015; 160: 422–429.e1.
Anshu A, Price MO, Tan DT, Price FW Jr . Endothelial keratoplasty: a revolution in evolution. Surv Ophthalmol 2012; 57: 236–252.
Ple-Plakon PA, Shtein RM . Trends in corneal transplantation: indications and techniques. Curr Opin Ophthalmol 2014; 25: 300–305.
Park CY, Lee JK, Gore PK, Lim CY, Chuck RS . Keratoplasty in the United States: a 10-year review from 2005 through 2014. Ophthalmology 2015; 122: 2432–2442.
Wacker K, Baratz KH, Maguire LJ, McLaren JW, Patel SV . Descemet stripping endothelial keratoplasty for Fuchs’ endothelial corneal dystrophy: five-year results of a prospective study. Ophthalmology 2016; 123: 154–160.
Price MO, Calhoun P, Kollman C, Price Jr FW, Lass JH . Descemet stripping endothelial keratoplasty: ten-year endothelial cell loss compared with penetrating keratoplasty. Ophthalmology 2016; 123: 1421–1427.
Price MO, Price FW Jr . Descemet stripping with endothelial keratoplasty for treatment of iridocorneal endothelial syndrome. Cornea 2007; 26: 493–497.
Huang T, Wang Y, Ji J, Gao N, Chen J . Deep lamellar endothelial keratoplasty for iridocorneal endothelial syndrome in phakic eyes. Arch Ophthalmol 2009; 127: 33–36.
Fajgenbaum MA, Hollick EJ . Descemet stripping endothelial keratoplasty in iridocorneal endothelial syndrome: postoperative complications and long-term outcomes. Cornea 2015; 34: 1252–1258.
Chaurasia S, Ramappa M, Garg P, Murthy SI, Senthil S, Sangwan VS . Endothelial keratoplasty in the management of irido-corneal endothelial syndrome. Eye 2013; 27: 564–566.
Hong Y, Peng RM, Wang M, Qu HQ, Hong J . Suture pull-through insertion techniques for descemet stripping automated endothelial keratoplasty in Chinese phakic eyes: outcomes and complications(4). PLoS One 2013; 8: e61929.
Wu EI, Ritterband DC, Yu G, Shields RA, Seedor JA . Graft rejection following descemet stripping automated endothelial keratoplasty: features, risk factors, and outcomes. Am J Ophthalmol 2012; 153: 949–957.e1.
Di Pascuale MA, Prasher P, Schlecte C, Arey M, Bowman RW, Cavanagh HD et al. Corneal deturgescence after descemet stripping automated endothelial keratoplasty evaluated by Visante anterior segment optical coherence tomography. Am J Ophthalmol 2009; 148: 32–7 e1.
Peng RM, Hao YS, Chen HJ, Sun YX, Hong J . Endothelial keratoplasty: the use of viscoelastic as an aid in reattaching the dislocated graft in abnormally structured eyes. Ophthalmology 2009; 116: 1897–1900.
Yuen LH, He M, Aung T, Htoon HM, Tan DT, Mehta JS . Biometry of the cornea and anterior chamber in Chinese eyes: an anterior segment optical coherence tomography study. Invest Ophthalmol Vis Sci 2010; 51: 3433–3440.
Nahum Y, Mimouni M, Busin M . Risk factors predicting the need for graft exchange after descemet stripping automated endothelial keratoplasty. Cornea 2015; 34: 876–879.
Anshu A, Price MO, Price FW . Descemet’s stripping endothelial keratoplasty: long-term graft survival and risk factors for failure in eyes with preexisting glaucoma. Ophthalmology 2012; 119: 1982–1987.
Decroos FC, Delmonte DW, Chow JH, Stinnett SS, Kim T, Carlson AN et al. Increased rates of descemet’s stripping automated endothelial keratoplasty (DSAEK) graft failure and dislocation in glaucomatous eyes with aqueous shunts. J Ophthal Vis Res 2012; 7: 203–213.
Ang M, Htoon HM, Cajucom-Uy HY, Tan D, Mehta JS . Donor and surgical risk factors for primary graft failure following descemet's stripping automated endothelial keratoplasty in Asian eyes. Clin Ophthalmol 2011; 5: 1503–1508.
Ishii N, Yamaguchi T, Yazu H, Satake Y, Yoshida A, Shimazaki J . Factors associated with graft survival and endothelial cell density after descemet's stripping automated endothelial keratoplasty. Sci Rep 2016; 6: 25276.
Suh LH, Yoo SH, Deobhakta A, Donaldson KE, Alfonso EC, Culbertson WW et al. Complications of descemet’s stripping with automated endothelial keratoplasty: survey of 118 eyes at one institute. Ophthalmology 2008; 115: 1517–1524.
Price MO, Price FW Jr . Endothelial cell loss after descemet stripping with endothelial keratoplasty influencing factors and 2-year trend. Ophthalmology 2008; 115: 857–865.
Suh LH, Dawson DG, Mutapcic L, Rosenfeld SI, Culbertson WW, Yoo SH et al. Histopathologic examination of failed grafts in descemet’s stripping with automated endothelial keratoplasty. Ophthalmology 2009; 116: 603–608.
Goldich Y, Artornsombidth P, Avni-Zauberman N, Perez M, Ulate R, Elbaz U et al. Fellow eye comparison of corneal thickness and curvature in descemet membrane endothelial keratoplasty and descemet stripping automated endothelial keratoplasty. Cornea 2014; 33: 547–550.
Price MO, Giebel AW, Fairchild KM, Price FW Jr . Descemet’s membrane endothelial keratoplasty: prospective multicenter study of visual and refractive outcomes and endothelial survival. Ophthalmology 2009; 116: 2361–2368.
Terry MA . Endothelial keratoplasty: why aren’t we all doing descemet membrane endothelial keratoplasty? Cornea 2012; 31: 469–471.
Hamzaoglu EC, Straiko MD, Mayko ZM, Sáles CS, Terry MA . The first 100 eyes of standardized descemet stripping automated endothelial keratoplasty versus standardized descemet membrane endothelial keratoplasty. Ophthalmology 2015; 122: 2193–2199.
Busin M, Madi S, Santorum P, Scorcia V, Beltz J . Ultrathin descemet's stripping automated endothelial keratoplasty with the microkeratome double-pass technique: two-year outcomes. Ophthalmology 2013; 120: 1186–1194.
Dickman MM, Kruit PJ, Remeijer L, van Rooij J, Van der Lelij A, Wijdh RH et al. A randomized multicenter clinical trial of ultrathin descemet stripping automated endothelial keratoplasty (DSAEK) versus DSAEK. Ophthalmology 2016; 123: 2276–2284.
Acknowledgements
This study was supported by the National Natural Science Foundation of China, No. 31271045.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on Eye website
Supplementary information
Rights and permissions
About this article
Cite this article
Ao, M., Feng, Y., Xiao, G. et al. Clinical outcome of Descemet stripping automated endothelial keratoplasty in 18 cases with iridocorneal endothelial syndrome. Eye 32, 679–686 (2018). https://doi.org/10.1038/eye.2017.282
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/eye.2017.282
This article is cited by
-
The clinical outcomes of keratoplasty in irreversible corneal decompensation secondary to Axenfeld–Rieger syndrome
International Ophthalmology (2022)
-
Clinical Factors for Rapid Endothelial Cell Loss After Corneal Transplantation: Novel Findings From the Aqueous Humor
Current Ophthalmology Reports (2019)