Abstract
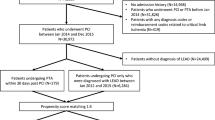
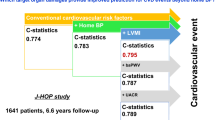
The effects of percutaneous transluminal angioplasty (PTA) on hemodynamic parameters are not established. We tested the hypothesis that PTA would achieve reductions in hemodynamic and target organ damage (TOD) measures in patients with peripheral artery disease (PAD). We enrolled 56 consecutive PAD patients who were scheduled to undergo elective PTA procedures. Brachial blood pressure (BP), central BP, left ventricular mass index (LVMI) and urinary microalbumin excretion ratio (UACR) were assessed at baseline and follow-up. The ankle–brachial index in the diseased leg significantly improved after the PTA (P<0.001). Compared with the pretreatment levels, brachial and central BPs, the carotid augmentation index (AI) and central augmentation pressure (AP) were significantly reduced after the PTA, as were LVMI and UACR. The change in AI in the PTA group was significantly associated with the extent of change in LVMI (P=0.002) and marginally associated with the change in UACR (P=0.07), independently of other covariates. In conclusion, in patients with PAD, significant reductions in carotid AI were observed by PTA treatment; these changes may be attributable to improvements in measures of cardiac and renal target organ damage.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$119.00 per year
only $9.92 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Hirsch AT, Haskal ZJ, Hertzer NR, Bakal CW, Creager MA, Halperin JL et al. ACC/AHA 2005 Practice Guidelines for the management of patients with peripheral arterial disease (lower extremity, renal, mesenteric, and abdominal aortic): a collaborative report from the American Association for Vascular Surgery/Society for Vascular Surgery, Society for Cardiovascular Angiography and Interventions, Society for Vascular Medicine and Biology, Society of Interventional Radiology, and the ACC/AHA Task Force on Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Peripheral Arterial Disease): endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation; National Heart, Lung, and Blood Institute; Society for Vascular Nursing; TransAtlantic Inter-Society Consensus; and Vascular Disease Foundation. Circulation 2006; 113 (11): e463–e465.
Welten GM, Schouten O, Hoeks SE, Chonchol M, Vidakovic R, van Domburg RT et al. Long-term prognosis of patients with peripheral arterial disease: a comparison in patients with coronary artery disease. J Am Coll Cardiol 2008; 51 (16): 1588–1596.
Meves SH, Diehm C, Berger K, Pittrow D, Trampisch HJ, Burghaus I et al. Peripheral arterial disease as an independent predictor for excess stroke morbidity and mortality in primary-care patients: 5-year results of the getABI study. Cerebrovasc Dis 2010; 29 (6): 546–554.
Leng GC, Lee AJ, Fowkes FG, Whiteman M, Dunbar J, Housley E et al. Incidence, natural history and cardiovascular events in symptomatic and asymptomatic peripheral arterial disease in the general population. Int J Epidemiol 1996; 25 (6): 1172–1181.
Zheng ZJ, Sharrett AR, Chambless LE, Rosamond WD, Nieto FJ, Sheps DS et al. Associations of ankle-brachial index with clinical coronary heart disease, stroke and preclinical carotid and popliteal atherosclerosis: the Atherosclerosis Risk in Communities (ARIC) Study. Atherosclerosis 1997; 131 (1): 115–125.
Ankle Brachial Index Collaboration. Ankle brachial index combined with Framingham Risk Score to predict cardiovascular events and mortality: a meta-analysis. JAMA 2008; 300 (2): 197–208.
Verdecchia P, Schillaci G, Borgioni C, Ciucci A, Gattobigio R, Zampi I et al. Prognostic significance of serial changes in left ventricular mass in essential hypertension. Circulation 1998; 97 (1): 48–54.
Ibsen H, Olsen MH, Wachtell K, Borch-Johnsen K, Lindholm LH, Mogensen CE et al. Reduction in albuminuria translates to reduction in cardiovascular events in hypertensive patients: losartan intervention for endpoint reduction in hypertension study. Hypertension 2005; 45 (2): 198–202.
O’Rourke MF, Hashimoto J . Mechanical factors in arterial aging: a clinical perspective. J Am Coll Cardiol 2007; 50 (1): 1–13.
Fu W, Ye C, Mei C, Rong S, Wang W . Reverse correlation between ankle-brachial index and left ventricular hypertrophy in patients on maintenance haemodialysis. Nephrology 2006; 11 (1): 9–14.
Matsushita M, Nishikimi N, Sakurai T, Yano T, Nimura Y . Urinary microalbumin as a marker for intermittent claudication. Eur J Vasc Endovasc Surg 1996; 11 (4): 421–424.
Matsui Y, Eguchi K, Shibasaki S, Ishikawa J, Hoshide S, Pickering TG et al. Monitoring of the central pulse pressure is useful for detecting cardiac overload during antiadrenergic treatment: the Japan Morning Surge 1 study. J Hypertens 2008; 26 (10): 1928–1934.
Devereux RB, Alonso DR, Lutas EM, Gottlieb GJ, Campo E, Sachs I et al. Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol 1986; 57: 450–458.
Sarnak MJ, Levey AS, Schoolwerth AC, Coresh J, Culleton B, Hamm LL et al. kidney disease as a risk factor for development of cardiovascular disease: a statement from the American Heart Association Councils on Kidney in Cardiovascular Disease, High Blood Pressure Research, Clinical Cardiology, and Epidemiology and Prevention. Circulation 2003; 108 (17): 2154–2169.
Association AD. Standards of medical care in diabetes—2011. Diabetes Care 2011; 34 (Suppl 1): S11–S61.
Ogihara T, Kikuchi K, Matsuoka H, Fujita T, Higaki J, Horiuchi M et al. The Japanese Society of Hypertension Guidelines for the Management of Hypertension (JSH 2009). Hypertens Res 2009; 32 (1): 3–107.
Price DD, McGrath PA, Rafii A, Buckingham B . The validation of visual analogue scales as ratio scale measures for chronic and experimental pain. Pain 1983; 17 (1): 45–56.
Miyazaki M, Higashi Y, Goto C, Chayama K, Yoshizumi M, Sanada H et al. Sarpogrelate hydrochloride, a selective 5-HT2A antagonist, improves vascular function in patients with peripheral arterial disease. J Cardiovasc Pharmacol 2007; 49 (4): 221–227.
Saba PS, Roman MJ, Pini R, Spitzer M, Ganau A, Devereux RB . Relation of arterial pressure waveform to left ventricular and carotid anatomy in normotensive subjects. J Am Coll Cardiol 1993; 22 (7): 1873–1880.
Segers P, Rietzschel ER, De Buyzere ML, De Bacquer D, Van Bortel LM, De Backer G et al. Assessment of pressure wave reflection: getting the timing right!. Physiol Meas 2007; 28 9: 1045–56.
O’Rourke MF, Nichols WW, Mitchell GF, Parise H, Benjamin EJ, Larson MG et al. Changes in wave reflection with advancing age in normal subjects * response. Hypertension 2004; 44 (6): e10–e11.
Westerhof BE, van den Wijngaard JP, Murgo JP, Westerhof N . Location of a reflection site is elusive: consequences for the calculation of aortic pulse wave velocity. Hypertension 2008; 52 (3): 478–483.
Hashimoto J, Westerhof BE, Westerhof N, Imai Y, O’Rourke MF . Different role of wave reflection magnitude and timing on left ventricular mass reduction during antihypertensive treatment. J Hypertens 2008; 26 (5): 1017–1024.
Dunn FG, Ventura HO, Messerli FH, Kobrin I, Frohlich ED . Time course of regression of left ventricular hypertrophy in hypertensive patients treated with atenolol. Circulation 1987; 76 (2): 254–258.
Mayet J, Ariff B, Wasan B, Chapman N, Shahi M, Poulter NR et al. Improvement in midwall myocardial shortening with regression of left ventricular hypertrophy. Hypertension 2000; 36 (5): 755–759.
O’Rourke MF, Safar ME . Relationship between aortic stiffening and microvascular disease in brain and kidney: cause and logic of therapy. Hypertension 2005; 46 (1): 200–204.
Fesler P, du Cailar G, Ribstein J, Mimran A . Glomerular hemodynamics and arterial function in normal individuals. J Hypertens 2010; 28 (12): 2462–2467.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on the Journal of Human Hypertension website
Supplementary information
Rights and permissions
About this article
Cite this article
Eguchi, K., Murakami, A., Horaguchi, T. et al. Percutaneous transluminal angioplasty for peripheral artery disease confers cardiorenal protection. J Hum Hypertens 28, 51–55 (2014). https://doi.org/10.1038/jhh.2013.37
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/jhh.2013.37