Abstract
Patients with germline mutations in BRCA1 or BRCA2 genes are predisposed to breast cancer. The BRCA1-associated breast cancers have distinct morphology, being more often medullary-like, triple negative and showing a ‘basal’ phenotype. On the other hand, BRCA2 and BRCAX cancers are a heterogeneous group without a specific phenotype. When incorporated into risk assessment models, pathology data improves prediction of carrier status. The role of BRCA1 and BRCA2 in DNA repair is being exploited to develop novel therapies, for example, using the poly-ADP-ribose polymerase inhibitors. A number of low-to-moderate-penetrant genes/loci have also been identified, but their role and contribution in breast cancer development is still under investigation.
Similar content being viewed by others
Main
Breast cancer is the commonest malignancy in women and it is estimated that a million women worldwide will develop breast cancer each year. A number of risk factors have been identified including early menarche, late menopause, nulliparity and a positive family history.1 First-degree relatives have an approximately twofold increase in risk of developing the disease. A number of highly penetrant breast cancer susceptibility genes have been identified and include BRCA1 and BRCA2.2, 3 These genes confer a high risk of breast and ovarian carcinoma. Two genes associated with rare cancer syndromes, P53 (Li–Fraumeni syndrome)4 and PTEN (Cowden syndrome)5 also confer a very high risk of breast cancer. Although all these genes confer a very high risk, they account for a relatively small proportion of inherited breast cancers. It has become increasingly clear that overall susceptibility to breast cancer is likely to be mediated through variants in many genes, each conferring a small-to-moderate risk of the disease. A number of such genes have been reported in the literature and include CHEK2, ATM, NBS1, RAD51, BRIP1 and PALB2.6, 7, 8, 9, 10 It is not known how many more genes that confer a small risk are yet to be identified or how these genes come together or interact with each other or with environmental factors to increase the breast cancer risk.
BRCA1, BRCA2 and BRCAX
The first high-penetrance gene, BRCA1, was isolated in the year 19942, 11 and a year later, BRCA2 was localised and cloned.3, 12 Over the last decade, it has been shown that breast cancer arising in patients harbouring a germline mutation in BRCA1 and BRCA2 genes differs from age-matched sporadic breast cancer cases and from familial breast cancers arising in non-BRCA1/2 patients. These differences are in morphology, immunophenotype and molecular characteristics.3, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29 These differences tell us something about the biology of familial breast cancer, but could also potentially be used in cancer clinics to predict which patients may harbour BRCA1 germline mutation.
Cellular Functions of BRCA1 and BRCA2
BRCA1 has several cellular roles. It has been implicated in DNA repair, cell-cycle regulation, transcriptional regulation and chromatin remodelling. On the contrary, functions attributed to BRCA2 have mainly been restricted to DNA recombination and repair processes. BRCA2 has a role in the regulation of RAD51 activity. RAD51 is a highly conserved DNA recombinase, involved in the repair of double-strand breaks and arrested replication forks.30
Loss of BRCA1 or BRCA2 leads to a deficiency in the repair of DNA double-strand breaks by the conservative mechanism of homologous recombination (HR). This mechanism is an error-free mechanism when the exchange is between identical sister chromatids (or homologous chromosomes). Such a deficiency leads to non-conservative/error-prone, and potentially mutagenic, repair of DNA lesions by mechanisms such as non-homologous end joining and single-strand annealing. The ultimate genomic instability developed is then likely to contribute to the cancer predisposition generated by loss-of-function mutations in BRCA1 or BRCA2.30
Histological types
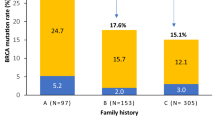
Histopathological analysis of hereditary breast cancers shows that the majority are ductal carcinomas of no-special type (IDC-NST); however, medullary carcinomas are overrepresented in patients with germline mutations in BRCA1.22, 23 Not surprisingly, these tumours have also been reported to have pushing margins and lymphocytic infiltrates more often than sporadic breast cancers (Figure 1a). Two papers with small number of cases suggested that lobular carcinoma, tubular carcinoma, tubulolobular carcinomas (collectively called the tubulolobular group)27 and pleomorphic lobular carcinomas13 were associated with BRCA2. This was not substantiated in a much larger study carried out on behalf of the Breast Cancer Linkage Consortium23 that found an association of lobular carcinoma with non-BRCA1/2 (that is, BRCAX).22 Bane et al16 also did not find this association. However, there is some evidence showing that BRCA2 may have a role in the aetiology of some sporadic lobular carcinomas, as LOH at the BRCA2 locus has been identified by our group in a subset of pleomorphic lobular carcinomas.31 Hence, unlike BRCA1, currently no specific morphological type has been associated with either BRCA2 or BRCAX, which seem to be morphologically heterogeneous.
Example of a BRCA1 basal-like cancer: (a) Low power ( × 40) view depicting the pushing border (arrows). (b) High magnification of tumour A ( × 400) showing high-grade nuclei and mitotic figures (arrows); (c–f) cores of a single tumour from a tissue microarray of basal-like cancers showing negativity for oestrogen receptor (ER, c), progesterone receptor (PR, d) and HER2 (e) and positivity for Cytokeratin 14 (CK14, f).
Histological grade
Both BRCA1 and BRCA2 tumours are overall higher grade than sporadic breast cancers. BRCA1 tumours tend to have a higher score for all parameters of grade (tubule formation, pleomorphism, mitotic counts) (Figure 1b), whereas BRCA2 tumours appear to lack tubules and are not more pleomorphic or have high mitotic counts. BRCAX tumours are very similar to sporadic breast cancers.
Multivariate analysis of morphological features
Many of the morphological features described are associated with each other. Multivariate analysis has shown that features predictive of BRCA1 phenotype include pushing margins, lymphocytic infiltrate and high mitotic counts, but not the medullary phenotype per se; hence BRCA1 tumours are high-grade, medullary-like cancers. Note that not all BRCA1 tumours have this morphology, just that there is a higher frequency of such cancers in this group. In contrast, the only features found to be significant for BRCA2 were pushing margins and lack of tubule formation;23 hence, BRCA2 does not have a specific phenotype.
Steroid receptors
BRCA1-associated breast cancers are more likely to be oestrogen (ER) and progesterone receptor (PgR) negative (∼90%) compared with sporadic breast cancers (∼30%) (Figure 1c and d). In contrast, the frequency of ER and PgR for BRCA2- and BRCAX-associated cancers is not significantly different to sporadic cancers.14, 19, 24, 25, 28
Other biological markers
BRCA1-associated cancers are often ER negative, and as would be expected, they are also usually negative for bcl232 and cyclinD1 (ER-associated genes), and do not show amplification of CCND1.33 They do, however, overexpress p27 and cyclinE134 as other high-grade and ‘basal’-like cancers. In a series of patients, amplification of the c-myc gene has been shown to be present in 18.2% of 20 tumours from BRCA1 mutation carriers and in 62.5% of 18 tumours from BRCA2 mutation carriers.28 BRCA1-associated carcinomas have also been associated with the cell cycle proteins, namely, E2F6, cyclins A and B1, SKP2 and Topo-II-α. BRCA2 tumours were shown to have higher expression of the cell cycle proteins cyclin D1, cyclin D3, p27, p16, p21, CDK4, CDK2 and CDK1.35
Association with ‘basal’ phenotype
As BRCA1-associated cancers are often triple negative (ER−, PgR−, HER2−), it is not surprising that a high proportion show a ‘basal’ phenotype (expression of basal/myoepithelial markers such as CK5/6, CK14, SMA, EGFR, P-cadherin and caveolin 1)17, 22, 36, 37 (Figure 1f). This is not a significant feature of BRCA2/BRCAX-related breast cancers, in that, the frequency is not higher than in sporadic cancers. Conversely, the BRCA1 pathway seems to be altered in sporadic breast cancers with a ‘basal’ phenotype.38 The trend of basal-like cancers to metastasise to brain,39, 40 which was also shown in patients with BRCA1 mutations, is also noteworthy.41
Can pathology aid clinical decision making?
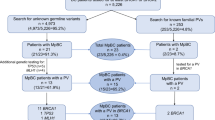
Unlike BRCA2/BRCAX, the morphology of tumours associated with BRCA1 is fairly distinct, and it has been postulated that this may help to identify potential carriers of germline mutation and hence triage patients towards testing. Current risk estimation models are not very specific and accurate, and new parameters that aid this process would be advantageous. Although a recent paper suggested that the use of basal markers was not predictive of BRCA1 status,42 this study had a very small data set and there are several studies that do show a role of morphology and immunohistochemistry in improving risk estimations for BRCA status, particularly in young women <40 years of age.24, 43, 44
Other predisposition genes
TP53, PTEN, CHEK2 and ATM
Hereditary breast cancers are also a part of a number of cancer syndromes including the Li–Fraumeni syndrome (TP53) and Cowden's syndrome (PTEN), which are caused by high-penetrant genes, but overall make a small contribution to familial breast cancer.45, 46 In contrast, CHEK2 and ATM are low-to-moderate-risk genes. Overall, there is little significant data relating pathology to these predisposition genes.47, 48
SNP Polymorphisms
Recently, a number of polymorphisms at genetic loci have been identified through large-scale genome-wide association studies.49 These include FGFR2, TNRC9, MAP3K1 and LSP1. It is not clear what the role of these genes is in breast cancer development, and hence nothing is currently known about the pathology or biology associated with these loci.
Unclassified BRCA1 and BRCA2 mutation variants
The BRCA1 and BRCA2 genes are frequently sequenced in kindred from families presenting with multiple cases of breast cancer, and as a consequence, pathogenic mutations are identified in some families. On the other hand, many rare sequence variants of unknown clinical significance are also reported. These rare missense substitutions and in-frame deletions of BRCA1 and BRCA2 genes pose a challenge for genetic counselling of individuals carrying such unclassified variants. Notwithstanding, variant classification has been shown to be improved by parallel analysis of oestrogen receptor, cytokeratin 5/6 and cytokeratin 14 tumour expression and use of updated methods that are able to estimate the clinical relevance of amino acid evolutionary conservation and position. This combination may assist genetic counselling of individuals with unclassified sequence variants.50, 51
Therapeutic potential
It has become increasingly clear that BRCA1 and BRCA2, as well as a number of other predisposition genes, such as CHEK2 and ATM, have a role in DNA repair. In particular, BRCA1 and BRCA2 are involved in an error-free type of repair called HR.
Cells with loss of HR have been shown to be sensitive to DNA crosslinking agents such as the mitomycin-C and platinum-based drugs.52 Further damage caused by these drugs in the absence of error-free repair leads to cell death. Data that these drugs may have an important role in managing patients harbouring these mutations are beginning to accumulate.
When HR is compromised, other error-prone repair mechanisms kick in—these include base excision and single-strand break repair. Counter intuitively, blocking these pathways in cells that have lost the BRCA function seems to be a good thing, as further damage caused by loss of the repair mechanisms leads to cell death. Poly-ADP ribose polymerase (PARP) is an enzyme involved in these pathways and PARP inhibitors look set to provide a novel way of targeting BRCA1 and BRCA2-associated breast cancers.53, 54
Disclosure/conflict of interest
The authors declare no conflict of interest.
References
Claus EB, Risch NJ, Thompson WD . Age at onset as an indicator of familial risk of breast cancer. Am J Epidemiol 1990;131:961–972.
Miki Y, Swensen J, Shattuck-Eidens D, et al. A strong candidate for the breast and ovarian cancer susceptibility gene BRCA1. Science 1994;266:66–71.
Wooster R, Bignell G, Lancaster J, et al. Identification of the breast cancer susceptibility gene BRCA2. Nature 1995;378:789–792.
Easton D, Ford D, Peto J . Inherited susceptibility to breast cancer. Cancer Surv 1993;18:95–113.
Lynch ED, Ostermeyer EA, Lee MK, et al. Inherited mutations in PTEN that are associated with breast cancer, cowden disease, and juvenile polyposis. Am J Hum Genet 1997;61:1254–1260.
McKinnon PJ . ATM and ataxia telangiectasia. EMBO Rep 2004;5:772–776.
Nevanlinna H, Bartek J . The CHEK2 gene and inherited breast cancer susceptibility. Oncogene 2006;25:5912–5919.
Rahman N, Scott RH . Cancer genes associated with phenotypes in monoallelic and biallelic mutation carriers: new lessons from old players. Hum Mol Genet 2007;16 (Spec No. 1):R60–R66.
Rahman N, Seal S, Thompson D, et al. PALB2, which encodes a BRCA2-interacting protein, is a breast cancer susceptibility gene. Nat Genet 2007;39:165–167.
Stratton MR, Rahman N . The emerging landscape of breast cancer susceptibility. Nat Genet 2008;40:17–22.
Hall JM, Lee MK, Newman B, et al. Linkage of early-onset familial breast cancer to chromosome 17q21. Science 1990;250:1684–1689.
Wooster R, Neuhausen SL, Mangion J, et al. Localization of a breast cancer susceptibility gene, BRCA2, to chromosome 13q12-13. Science 1994;265:2088–2090.
Armes JE, Egan AJ, Southey MC, et al. The histologic phenotypes of breast carcinoma occurring before age 40 years in women with and without BRCA1 or BRCA2 germline mutations: a population-based study. Cancer 1998;83:2335–2345.
Armes JE, Trute L, White D, et al. Distinct molecular pathogeneses of early-onset breast cancers in BRCA1 and BRCA2 mutation carriers: a population-based study. Cancer Res 1999;59:2011–2017.
Armes JE, Venter DJ . The pathology of inherited breast cancer. Pathology 2002;34:309–314.
Bane AL, Beck JC, Bleiweiss I, et al. BRCA2 mutation-associated breast cancers exhibit a distinguishing phenotype based on morphology and molecular profiles from tissue microarrays. Am J Surg Pathol 2007;31:121–128.
Foulkes WD, Stefansson IM, Chappuis PO, et al. Germline BRCA1 mutations and a basal epithelial phenotype in breast cancer. J Natl Cancer Inst 2003;95:1482–1485.
Honrado E, Benitez J, Palacios J . The molecular pathology of hereditary breast cancer: genetic testing and therapeutic implications. Mod Pathol 2005;18:1305–1320.
Honrado E, Osorio A, Milne RL, et al. Immunohistochemical classification of non-BRCA1/2 tumors identifies different groups that demonstrate the heterogeneity of BRCAX families. Mod Pathol 2007;20:1298–1306.
Honrado E, Osorio A, Palacios J, et al. Pathology and gene expression of hereditary breast tumors associated with BRCA1, BRCA2 and CHEK2 gene mutations. Oncogene 2006;25:5837–5845.
Honrado E, Osorio A, Palacios J, et al. Immunohistochemical expression of DNA repair proteins in familial breast cancer differentiate BRCA2-associated tumors. J Clin Oncol 2005;23:7503–7511.
Lakhani SR, Gusterson BA, Jacquemier J, et al. The pathology of familial breast cancer: histological features of cancers in families not attributable to mutations in BRCA1 or BRCA2. Clin Cancer Res 2000;6:782–789.
Lakhani SR, Jacquemier J, Sloane JP, et al. Multifactorial analysis of differences between sporadic breast cancers and cancers involving BRCA1 and BRCA2 mutations. J Natl Cancer Inst 1998;90:1138–1145.
Lakhani SR, Reis-Filho JS, Fulford L, et al. Prediction of BRCA1 status in patients with breast cancer using estrogen receptor and basal phenotype. Clin Cancer Res 2005;11:5175–5180.
Lakhani SR, Van De Vijver MJ, Jacquemier J, et al. The pathology of familial breast cancer: predictive value of immunohistochemical markers estrogen receptor, progesterone receptor, HER-2, and p53 in patients with mutations in BRCA1 and BRCA2. J Clin Oncol 2002;20:2310–2318.
Marcus JN, Watson P, Page DL, et al. Pathology and heredity of breast cancer in younger women. J Natl Cancer Inst Monogr 1994;86:23–34.
Marcus JN, Watson P, Page DL, et al. Hereditary breast cancer: pathobiology, prognosis, and BRCA1 and BRCA2 gene linkage. Cancer 1996;77:697–709.
Palacios J, Honrado E, Osorio A, et al. Immunohistochemical characteristics defined by tissue microarray of hereditary breast cancer not attributable to BRCA1 or BRCA2 mutations: differences from breast carcinomas arising in BRCA1 and BRCA2 mutation carriers. Clin Cancer Res 2003;9 (10 Part 1):3606–3614.
Quenneville LA, Phillips KA, Ozcelik H, et al. HER-2/neu status and tumor morphology of invasive breast carcinomas in Ashkenazi women with known BRCA1 mutation status in the Ontario Familial Breast Cancer Registry. Cancer 2002;95:2068–2075.
Venkitaraman AR . Cancer susceptibility and the functions of BRCA1 and BRCA2. Cell 2002;108:171–182.
Simpson PT, Reis-Filho JS, Lambros MB, et al. Molecular profiling pleomorphic lobular carcinomas of the breast: evidence for a common molecular genetic pathway with classic lobular carcinomas. J Pathol 2008;215:231–244.
Freneaux P, Stoppa-Lyonnet D, Mouret E, et al. Low expression of bcl-2 in Brca1-associated breast cancers. Br J Cancer 2000;83:1318–1322.
Vaziri SA, Tubbs RR, Darlington G, et al. Absence of CCND1 gene amplification in breast tumours of BRCA1 mutation carriers. Mol Pathol 2001;54:259–263.
Foulkes WD, Brunet JS, Stefansson IM, et al. The prognostic implication of the basal-like (cyclin E high/p27 low/p53+/glomeruloid-microvascular-proliferation+) phenotype of BRCA1-related breast cancer. Cancer Res 2004;64:830–835.
Palacios J, Honrado E, Osorio A, et al. Phenotypic characterization of BRCA1 and BRCA2 tumors based in a tissue microarray study with 37 immunohistochemical markers. Breast Cancer Res Treat 2005;90:5–14.
Arnes JB, Brunet JS, Stefansson I, et al. Placental cadherin and the basal epithelial phenotype of BRCA1-related breast cancer. Clin Cancer Res 2005;11:4003–4011.
Pinilla SM, Honrado E, Hardisson D, et al. Caveolin-1 expression is associated with a basal-like phenotype in sporadic and hereditary breast cancer. Breast Cancer Res Treat 2006;99:85–90.
Turner NC, Reis-Filho JS, Russell AM, et al. BRCA1 dysfunction in sporadic basal-like breast cancer. Oncogene 2007;26:2126–2132.
Fulford LG, Reis-Filho JS, Ryder K, et al. Basal-like grade III invasive ductal carcinoma of the breast: patterns of metastasis and long-term survival. Breast Cancer Res 2007;9:R4.
Gaedcke J, Traub F, Milde S, et al. Predominance of the basal type and HER-2/neu type in brain metastasis from breast cancer. Mod Pathol 2007;20:864–870.
Albiges L, Andre F, Balleyguier C, et al. Spectrum of breast cancer metastasis in BRCA1 mutation carriers: highly increased incidence of brain metastases. Ann Oncol 2005;16:1846–1847.
Collins LC, Martyniak AJ, Kandel MJ, et al. Basal cytokeratin and epidermal growth factor receptor expression are not predictive of BRCA1 mutation status in women with triple-negative breast cancers. Am J Surg Pathol 2009;33:1093–1097.
Farshid G, Balleine RL, Cummings M, et al. Morphology of breast cancer as a means of triage of patients for BRCA1 genetic testing. Am J Surg Pathol 2006;30:1357–1366.
James PA, Doherty R, Harris M, et al. Optimal selection of individuals for BRCA mutation testing: a comparison of available methods. J Clin Oncol 2006;24:707–715.
Walsh T, Casadei S, Coats KH, et al. Spectrum of mutations in BRCA1, BRCA2, CHEK2, and TP53 in families at high risk of breast cancer. JAMA 2006;295:1379–1388.
Lauge A, Lefebvre C, Laurent-Puig P, et al. No evidence for germline PTEN mutations in families with breast and brain tumours. Int J Cancer 1999;84:216–219.
Balleine RL, Murali R, Bilous AM, et al. Histopathological features of breast cancer in carriers of ATM gene variants. Histopathology 2006;49:523–532.
Cybulski C, Huzarski T, Byrski T, et al. Estrogen receptor status in CHEK2-positive breast cancers: implications for chemoprevention. Clin Genet 2009;75:72–78.
Easton DF, Pooley KA, Dunning AM, et al. Genome-wide association study identifies novel breast cancer susceptibility loci. Nature 2007;447:1087–1093.
Lovelock PK, Healey S, Au W, et al. Genetic, functional, and histopathological evaluation of two C-terminal BRCA1 missense variants. J Med Genet 2006;43:74–83.
Spurdle AB, Lakhani SR, Healey S, et al. Clinical classification of BRCA1 and BRCA2 DNA sequence variants: the value of cytokeratin profiles and evolutionary analysis--a report from the kConFab Investigators. J Clin Oncol 2008;26:1657–1663.
Turner N, Tutt A, Ashworth A . Targeting the DNA repair defect of BRCA tumours. Curr Opin Pharmacol 2005;5:388–393.
Bryant HE, Schultz N, Thomas HD, et al. Specific killing of BRCA2-deficient tumours with inhibitors of poly(ADP-ribose) polymerase. Nature 2005;434:913–917.
Farmer H, McCabe N, Lord CJ, et al. Targeting the DNA repair defect in BRCA mutant cells as a therapeutic strategy. Nature 2005;434:917–921.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Da Silva, L., Lakhani, S. Pathology of hereditary breast cancer. Mod Pathol 23 (Suppl 2), S46–S51 (2010). https://doi.org/10.1038/modpathol.2010.37
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/modpathol.2010.37
Keywords
This article is cited by
-
Microenvironmental niche divergence shapes BRCA1-dysregulated ovarian cancer morphological plasticity
Nature Communications (2018)
-
Can we prevent BRCA1-associated breast cancer by RANKL inhibition?
Breast Cancer Research and Treatment (2017)
-
The role of body size and physical activity on the risk of breast cancer in BRCA mutation carriers
Cancer Causes & Control (2015)
-
Epigenetic silencing of ARRDC3 expression in basal-like breast cancer cells
Scientific Reports (2014)
-
BRCA1 mRNA levels following a 4–6-week intervention with oral 3,3′-diindolylmethane
British Journal of Cancer (2014)