Abstract
Combination antiretroviral therapy is highly effective in HIV infection, leading to decreased incidences of AIDS-defining neoplasms. However, HIV patients still have a 10-fold increased risk of developing classical Hodgkin lymphoma compared with the general population. As Hodgkin- and Reed–Sternberg cells represent only a minority in the tumor infiltrate, the aim of the present study was to characterize the microenvironment of HIV-related classical Hodgkin lymphoma and compare it with classical Hodgkin lymphoma cases of immunocompetent individuals. The major morphologic differences were the presence of necrotic foci and the absence of epithelioid cell formation in HIV-related Hodgkin lymphoma. We observed a significantly decreased number of CD4+ T-cells and a significantly increased number of CD163+ macrophages in HIV-related Hodgkin lymphoma. Cases exhibiting a ‘sarcomatoid’ pattern of the reactive infiltrate exhibited significantly greater numbers of macrophages, associating the ‘sarcomatoid’ pattern to the presence of spindle-shaped macrophages. Whereas, rosetting of CD4+ T-cells around Hodgkin- and Reed–Sternberg cells was frequently observed in classical Hodgkin lymphoma in immunocompetent persons; rosetting in a subset of HIV-related Hodgkin lymphoma cases appeared to involve cytoplasmic protrusions of spindle-shaped macrophages. HIV-related Hodgkin lymphoma, therefore, is characterized by unique morphologic features, which should be recognized by pathologists.
Similar content being viewed by others
Main
In the era of combination antiretroviral therapy for HIV, incidences of AIDS-defining neoplasms like Kaposi sarcoma or non-Hodgkin lymphoma have markedly decreased. However, classical Hodgkin lymphoma is observed more frequently1 and HIV patients have a 9.4-fold increased risk of developing classical Hodgkin lymphoma compared with the general population.2, 3 Although HIV-related classical Hodgkin lymphoma occurs at any CD4 blood count, it is most frequently observed in patients with a moderate immune deficiency and CD4 blood counts of 150–249 cells/μl.2, 4
As Hodgkin- and Reed–Sternberg cells, the tumor cells in classical Hodgkin lymphoma, usually constitute a small subpopulation of the cells in affected lymph nodes; it is likely that the microenvironment, largely composed of CD4+ T regulatory 1 cells, has an essential role in the pathophysiology of the disease.5 As HIV infection usually involves decreased CD4+ T-cell counts in the peripheral blood, several studies have addressed the issue of the microenvironment in HIV-associated Hodgkin lymphoma and have found the CD4/CD8 T-cell ratio to be inverted.6, 7, 8, 9 However, the number of cases examined was very small in the majority of the studies6, 8, 9 (<10 HIV-positive classical Hodgkin lymphoma cases each). Thompson et al7 analyzed 47 HIV-positive Hodgkin lymphoma cases and found a ‘sarcomatoid’ pattern of the reactive microenvironment to be significantly associated with an adverse clinical outcome.
In recent studies, an increased number of tumor-associated macrophages in classical Hodgkin lymphoma was strongly associated with shortened survival of the patients.10, 11, 12 However, other studies could not confirm this finding.13, 14 In the present study, we aimed to further characterize the morphologic and immunohistochemical characteristics of HIV-associated Hodgkin lymphoma in comparison to classical Hodgkin lymphoma in non-HIV infected individuals with respect to the composition of the microenvironment and the tumor cell content. The objective of this study was also to evaluate if HIV-associated Hodgkin lymphoma presents a particularly high content of macrophages and if this is related to a ‘sarcomatoid’ appearance of the infiltrate.
Materials and methods
Tissue Samples
All Hodgkin lymphoma cases with known HIV-1 infection of the patients diagnosed between 1986 and 2012 at the Senckenberg Institute of Pathology (n=54) were included in the study. Of the original 54 patients, paraffin blocks with representative Hodgkin infiltrates could be retrieved in 25 patients (24 lymph nodes, 1 bone marrow). As a control group, lymph nodes from 15 non-HIV infected patients with classical Hodgkin lymphoma (EBV-associated mixed cellularity type) were selected. All cases were reviewed by histologic analysis applying a basic immune marker panel (CD30, CD15, PAX5, LMP1, CD20, CD3), and diagnoses were confirmed in all cases. 15 cases of nonspecific lymphadenitis were additionally stained for CD8. Informed consent was obtained in accordance with the Declaration of Helsinki, and approval of the ethics committee of the University Hospital of Frankfurt was obtained (No. 254/12).
Immunohistochemistry, Quantification and Statistics
Immunohistochemical stainings (CD4, CD8, CD163, CD30 and S100) were performed using the Alkaline Phosphatase-Real Detection Kit (DAKO, Glostrup, Denmark) as described previously.15 The antibodies used, dilutions and providers are listed in Supplementary Table 1. Antigen unmasking was performed for 2 min in a pressure cooker in TRIS-EDTA at pH 8.0. Immunohistochemical stainings were quantified using a light microscope equipped with a camera system (Microdissection Axiovert 200 M microscope, PALM, Bernried, Germany). For each slide, three representative counting frames (12 2824 μm2) were chosen, and the number of positively stained cells was point-counted using PALM software. All lymph node biopsies were also assessed for morphologic features including the presence of germinal centers (GC), epithelioid cell clusters, necrosis, a ‘sarcomatoid’ pattern and hyalinization in HE-staining. T-cell rosetting was evaluated by CD4-immunostaining and macrophage rosetting by CD163-immunostaining. Cell counting and assessment of histological parameters were carried out in each case without knowledge of the clinical parameters. The data were tested for the presence of a Gaussian distribution (Shapiro–Wilk test). If present, groups were compared using the unpaired t-test; otherwise, the Mann–Whitney test was applied.
Cocultures
CD4+ T-cells and CD14+ monocytes were isolated from peripheral blood of two healthy donors by magnetic cell separation (magnetic-activated cell sorting) with CD4- and CD14-microbeads (Miltenyi Biotec, Cologne, Germany). Isolation of monocytes was performed prior to CD4+ T-cell isolation to avoid contamination of the CD4+ T-cell fraction with CD4+ monocytes. High purity of the magnetic cell separation was confirmed by FACS analysis. The classical Hodgkin lymphoma cell lines KM-H2, L-428 and L-1236 as well as the Burkitt cell line Ramos were cocultured with CD4+ T-cells, monocytes or a 1:1 mixture of both for 5 days. The ratio of cell line to primary cells was 1:20. Cocultures were set up in triplicate. As negative controls, CD4+ T-cells, monocytes and the cell lines were cultured alone. Cultures were assessed under a Nikon ECLIPSE TE 300 microscope and sizes of cell clusters were evaluated using ImageJ 1.46 software (http://rsbweb.nih.gov/ij/). Smears obtained from the cultures were immunostained for CD4 and CD14.
Results
Clinicopathologic Features
The mean patient age of the HIV-positive Hodgkin lymphoma cohort was 47 years (range 28–73 years). Twenty patients were male and five patients were female. Clinical data were available for 15 classical Hodgkin lymphoma patients: Three patients presented with stage IIA/B, three patients with stage IIIB and nine cases with stage IVA/B; 10 patients had received combination antiretroviral therapy prior to therapy and five patients had not received previous antiviral therapy. CD4+ T-cell counts at diagnosis of Hodgkin lymphoma were 27–526/μl (mean 152/μl). The Hodgkin lymphoma subtypes were mixed cellularity in 19 cases, not otherwise specified in three cases, nodular sclerosis in two cases, and lymphocyte-depleted in one case. In all cases, the Hodgkin- and Reed–Sternberg cells were positive for the EBV-coded latent membrane protein 1. The mean patient age of the control group (HIV-negative classical Hodgkin lymphoma) was 39 years (range 6–76 years). All cases in the control group were classified as EBV-positive mixed cellularity.
Histological and Immunohistochemical Findings
The most striking differences observed between HIV-associated Hodgkin lymphoma and HIV-negative classical Hodgkin lymphoma were the presence of small to large confluent necrotic foci (11 of 23 cases) and the absence of CD163-negative epithelioid cell clusters (0 of 23 cases) in HIV-associated classical Hodgkin lymphoma (Table 1, Figure 1). In the control group of HIV-negative classical Hodgkin lymphoma, all of which were of mixed cellularity, necrosis was never observed, whereas 9 of 15 cases presented epithelioid cell clusters. A ‘sarcomatoid’ pattern7 was more frequently observed in HIV-associated Hodgkin lymphoma cases than in HIV-negative Hodgkin lymphoma (13/23 vs 4/15 cases), but was not specific for HIV-associated disease. Large hyalinized areas of the lymph node were observed in 8 HIV-related Hodgkin lymphoma cases, whereas such areas were present in only one HIV-negative case. Residual germinal centers were rarely observed either in HIV-associated Hodgkin lymphoma or HIV-negative Hodgkin lymphoma (2 of 24 cases and 5 of 15 cases, respectively).
(a) ‘Sarcomatoid’ pattern due to high content of spindle-shaped macrophages, frequently observed in HIV-associated classical Hodgkin lymphoma; HE (100 × ). (b) Small focus of necrosis, typically found in HIV-associated classical Hodgkin lymphoma; HE (100 × ). (c) Hyalinization of the lymph node structure, another typical feature of HIV-associated classical Hodgkin lymphoma; HE (100 × ). (d) Groups of epithelioid cells usually found in HIV-negative classical Hodgkin lymphoma; HE (200 × ). (e) CD163-immunostaining showing high numbers of macrophages in the HIV classical Hodgkin lymphoma infiltrate; rosetting of macrophage cytoplasmic protrusions around Hodgkin- and Reed–Sternberg cells highlighted by arrows (100 × ). The inset shows macrophage rosetting at higher magnification (400 × ). (f) CD163-immunostaining of a typical HIV-negative classical Hodgkin lymphoma with groups of CD163-negative epithelioid cells and a low number of CD163-positive macrophages (100 × ). (g) Typical CD4-immunostaining of HIV classical Hodgkin lymphoma with a low CD4 blood count. CD4 rosetting is not observed (100 × ). (h) CD4 immunostaining of a HIV-negative classical Hodgkin lymphoma with high numbers of CD4+ T-cells and rosetting around Hodgkin- and Reed–Sternberg cells (arrows, 100 × ).
Composition of the Microenvironment
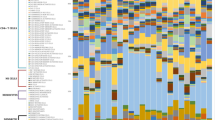
As expected, CD4 numbers were significantly lower in HIV-related Hodgkin lymphoma than in the HIV-negative cases (876 vs 3465 cells/mm2, P<0.001, unpaired t-test, Figure 2). CD8 numbers were stable between the two groups (2699 vs 2835 cells/mm2) and were comparable with CD8 numbers in nonspecific lymphadenitis (2947 cells/mm2). The number of CD163+ macrophages was significantly increased in HIV-associated Hodgkin lymphoma compared with HIV-negative Hodgkin cases (2836 vs 1430 cells/mm2, P=0.0025, unpaired t-test, Figure 2). The number of S100+ dendritic cells and Hodgkin- and Reed–Sternberg cells did not differ between HIV-related Hodgkin lymphoma and HIV-negative Hodgkin lymphoma cases (284 vs 331 and 267 vs 285 cells/mm2).
(a) Significantly lower number of CD4+ T-cells/mm2 in the lymph node in HIV classical Hodgkin lymphoma (n=24) compared with HIV-negative classical Hodgkin lymphoma (n=15) (P<0.001, unpaired t-test). (b) No differences were observed in the number of CD8-positive T-cells/mm2 in the lymph node in HIV-associated classical Hodgkin lymphoma (n=24) compared with HIV-negative classical Hodgkin lymphoma (n=15). (c) Significantly higher number of CD163-positive macrophages/mm2 in the lymph node in HIV-associated classical Hodgkin lymphoma (n=24) compared with HIV-negative classical Hodgkin lymphoma (n=15) (P=0.0025, unpaired t-test). (d) No differences were observed in the number of CD30-positive Hodgkin- and Reed–Sternberg cells/mm2 in the lymph node in HIV-associated classical Hodgkin lymphoma (n=24) compared with HIV-negative classical Hodgkin lymphoma (n=15). (e) Significantly higher number of CD163-positive macrophages/mm2 in the lymph node in HIV-associated Hodgkin lymphoma with necrosis (n=11) compared with HIV-associated Hodgkin lymphoma without necrosis (n=12) (P=0.0392, Mann–Whitney test). (f) Significantly higher number of CD163-positive macrophages/mm2 in the lymph node in classical Hodgkin lymphoma with a ‘sarcomatoid’ pattern (n=17) compared with classical Hodgkin lymphoma without sarcomatoid pattern (n=21) (P=0.027, unpaired t-test).
Among the HIV-associated Hodgkin lymphoma cases for which clinical data were available, we also determined if the number of CD163+ macrophages and CD4+ T-cells in the lymph node was dependent on previous combination antiretroviral therapy, the virus load or the CD4 blood count at diagnosis. There was no difference in the number of CD163+ macrophages between the groups with and without combination antiretroviral therapy (2943 vs 2905 cells/mm2). The difference in CD4+ T-cells in the HIV-associated Hodgkin lymphoma microenvironment between the group receiving (n=10) and not receiving combination antiretroviral therapy (n=6) was not significant (1327 vs 554 cells/mm2). Neither were the differences in the number of CD4+ T-cells or macrophages significant between cases with a high (≥340 copies/ml, n=7) or a low virus load (<20 copies/ml, n=5, 698 vs 2238 CD4+ cells/mm2 and 3753 vs 2028 CD163 cells/mm2). However, three of the HIV-associated Hodgkin lymphoma cases had a CD4 blood count >250/μl at diagnosis, and these cases also showed significantly higher CD4+ T-cell numbers and lower macrophage counts in the tissue than the other cases with CD4 blood counts <250/μl (n=11; 3756 vs 465 CD4+ cells/mm2, P=0.0127 and 1389 vs 3458 CD163 cells/mm2, P=0.0293, both Mann–Whitney test). As necrosis was an important feature in HIV-associated Hodgkin lymphoma, we also investigated if there was a relationship between the presence of necrosis and the numbers of CD4+ T-cells, CD8+ T-cells or CD163+ macrophages. There was a significantly higher number of CD163+ macrophages in the HIV-related Hodgkin lymphoma cases with necrosis (n=11; 3248 cells/mm2) compared with HIV-related Hodgkin lymphoma cases without necrosis (n=12; 2125 cells/mm2, P=0.0392, Mann–Whitey test, Figure 2). The differences in the numbers of CD4+ T-cells and CD8+ T-cells were not significant (376 vs 1357 CD4+ cells/mm2 and 2273 vs 3065 CD8+ cells/mm2). We also wanted to determine if the ‘sarcomatoid’ appearance observed in some cases was related to a high macrophage content. As a ‘sarcomatoid’ pattern was not specific for the HIV-associated Hodgkin lymphoma group and was also found in 4 HIV-negative classical Hodgkin lymphoma cases, we grouped all ‘sarcomatoid’ cases for the analysis. This revealed that the number of CD163+ macrophages was significantly higher in all cases with a ‘sarcomatoid’ pattern (2681 vs 1767 cells/mm2, P=0.027, unpaired t-test).
Rosetting around Hodgkin- and Reed–Sternberg Cells
As Hodgkin- and Reed–Sternberg cells are often surrounded by CD4+ T-cell rosettes, we also determined if CD4+ T-cell rosetting was present in the HIV-associated Hodgkin lymphoma cases. T-cell rosetting of Hodgkin- and Reed–Sternberg cells was observed in the HIV-related Hodgkin lymphoma group, but was less frequent than in the HIV-negative Hodgkin lymphoma group (3/23 vs 10/15 cases). In contrast, the HIV-associated Hodgkin lymphoma cases showed more frequent rosetting of cytoplasmic protrusions of CD163+ macrophages around the Hodgkin- and Reed–Sternberg cells (14/23 vs 3/15 cases). All three HIV-negative classical Hodgkin lymphoma cases showing macrophage rosetting also showed T-cell rosetting, whereas only one of the 14 HIV-associated Hodgkin lymphoma cases exhibiting macrophage rosetting additionally presented T-cell rosetting. To further corroborate this finding, we performed an in vitro cluster formation assay. The classical Hodgkin lymphoma cell lines L-428, KM-H2 and L-1236 were cocultured with CD4+ T-cells and/or monocytes purified from peripheral blood of healthy donors. After 5 days, cluster formation around the Hodgkin- and Reed–Sternberg cells could be observed in cocultures of all Hodgkin cell lines and CD4+ T-cells, monocytes or the mixture of both. No cluster formation was observed, if the Hodgkin cell lines were cultured without bystander cells. Coculture of the Burkitt cell line Ramos with CD4+ T-cells, monocytes or the mixture of both did not lead to cluster formation. Cocultures of all Hodgkin cell lines with CD4+ T-cells showed formation of massive non-adherent clusters (Supplementary Figure 1, median diameter 378.9 μm per cluster). In contrast, clusters induced by cocultures with monocytes were adherent and smaller in size, but the number of clusters was increased (Supplementary Figure 1, median diameter 300.3 μm per cluster). Interestingly, the cocultures of Hodgkin cell lines with both CD4+ T-cells and monocytes showed a similar pattern as the cocultures with monocytes lacking CD4+ T-cells: clusters were adherent with an intermediate cluster size (Supplementary Figure 1, 335.1 μm per cluster). Rosetting around Hodgkin- and Reed–Sternberg cells by CD4+ T-cells and monocytes was verified by immunostaining smears obtained from the cocultures for CD4 and CD14 (Figure 3). Importantly, cocultures that included both CD4+ T-cells and monocytes showed heterogeneous rosettes with CD4+ T-cells and monocytes surrounding the Hodgkin- and Reed-Sternberg cells simultaneously.
Smears from cocultures of L-428 and bystander cells: (a) L-428 with rosetting T-cells in coculture with CD4+ T-cells (Pappenheim). (b) L-428 with rosetting T-cells in coculture with CD4+ T-cells (CD4-immunostaining). (c) L-428 with rosetting monocytes in coculture with CD14+ monocytes (Pappenheim). (d) L-428 with rosetting monocytes in coculture with CD14+ monocytes (CD14-immunostaining). (e) L-428 with rosetting T-cells and monocytes in coculture with CD4+ T-cells and CD14+ monocytes (Pappenheim). (f) L-428 with rosetting T-cells and monocytes in coculture with CD4+ T-cells and CD4-negative/weakly positive monocytes (arrows, CD4-immunostaining).(g) L-428 with rosetting T-cells and monocytes in coculture with CD4+ T-cells and CD14+ monocytes (Pappenheim). (h) L-428 with rosetting T-cells and monocytes in coculture with CD4+ T-cells (CD14-negative) and CD14+ monocytes (CD14-immunostaining).
Discussion
In the present study, we compared 24 HIV-associated Hodgkin lymphoma cases with 15 HIV-negative classical Hodgkin lymphoma cases. We confirmed previous findings of a severely altered microenvironment in HIV-associated Hodgkin lymphoma with decreased CD4 numbers in the tissue.6, 7, 8, 9 Although previous studies observed an inverted CD4/CD8 T-cell ratio, we showed that this is merely due to decreased CD4 numbers, whereas the absolute number of CD8+ T-cells was stable in HIV-positive and HIV-negative cases. Interestingly, this study showed significantly increased numbers of CD163+ macrophages in HIV-related Hodgkin lymphoma, whereas the numbers of S100+ dendritic cells and Hodgkin- and Reed–Sternberg cells were similar between HIV-positive and HIV-negative cases. This is surprising, as one could suspect that HIV-associated Hodgkin lymphoma cases would present a higher content of Hodgkin- and Reed–Sternberg cells due to impaired surveillance by the immune system. A high number of macrophages has been correlated with frequent treatment failure in classical Hodgkin lymphoma.10, 11, 12 As the cases in the present series were collected over a long period of time, treatment protocols were heterogeneous and clinical data were not available in all cases. Therefore, the prognostic impact of macrophages in HIV-associated Hodgkin lymphoma should be assessed in future studies.
In a clinical study of a large cohort of HIV-patients, it was shown that patients with and without combination antiretroviral therapy experienced a decrease in CD4+ T-cell counts in the peripheral blood in the year preceding the diagnosis of classical Hodgkin lymphoma.4 This observation was possible because CD4+ T-cell blood counts in HIV-patients are usually well documented. It can be expected that HIV-negative individuals will react in the same manner, although this has not been documented. In our view, CD4+ T-cells are likely to be recruited from the peripheral blood to lymph nodes infiltrated by classical Hodgkin lymphoma via cytokines such as TARC and RANTES/CCL5 secreted by the Hodgkin- and Reed–Sternberg cells.16 Interestingly, although only CD4+ T-cells express CCR4,17 both CD4+ T-cells and macrophages express CD4 and CCR5. Although HIV-infected CD4+ T-cells are eliminated in high numbers, macrophages usually persist as viral reservoirs.18 As CCR5 not only represents the HIV fusion coreceptor, but also the ligand for RANTES, macrophages become increasingly attracted to the affected lymph nodes in the absence of CD4+ T-cells. Thus, in more severely immunocompromised HIV-patients with low CD4 blood counts, monocytes/macrophages may take over the role of CD4+ T-cells. We also found in cell culture experiments that monocytes are equally good at forming clusters and rosettes with Hodgkin cell lines, in line with a previous study.19 Macrophage rosetting is, therefore, likely to occur in the absence of CD4+ T-cells, but is not hampered by the presence of T-cells.
Thompson et al7 found a ‘sarcomatoid’ pattern of the reactive microenvironment associated with a worse clinical outcome in HIV-related Hodgkin lymphoma. In the present study, we also observed the ‘sarcomatoid’ pattern more frequently in HIV-related Hodgkin lymphoma than in HIV-negative classical Hodgkin lymphoma. However, this was not a specific finding in HIV patients. We associated the ‘sarcomatoid’ pattern with a spindle-shaped appearance of the macrophages in the microenvironment and found also a significantly higher content of macrophages in cases with the ‘sarcomatoid’ pattern. As epithelioid cell clusters were virtually absent in all cases with a ‘sarcomatoid’ pattern, the spindle-shaped appearance of macrophages in this pattern may reflect a functional differentiation state distinct from the epithelioid cell state and indicative of poor prognosis. Previous studies have suggested that CD4+ T-cells are required for epithelioid cell formation.20, 21, 22 Macrophage activation is a multistep process and has been divided into proinflammatory/M1 or regulatory/M2 polarization.23, 24 Although epithelioid cell formation in sarcoidosis and tuberculosis was shown to be associated with an M1 phenotype of macrophages,25, 26 tumor-associated macrophages were usually found to have an M2-like phenotype.24, 27 Data on macrophage polarization in HIV are contradictory, and a switch from M1 to M2 polarization of macrophages during the disease course has been proposed.28 Whereas HIV-infection of macrophages was shown to induce an M1-like phenotype with a hypersensitivity to Toll-like receptor agonists shortly after the infection,29 the fraction of CD163+ and CD16+ double-positive monocytes, which are precursors of alternatively activated macrophages, were increased in HIV-patients with low CD4+ T-cell blood counts,30 as was soluble CD163 in serum.31 CD163, usually known as a typical M2 marker and strongly expressed in the spindle-shaped macrophages of HIV-related Hodgkin lymphoma, was recently found to be expressed on a subset of M1-polarized macrophages.32 The presence of necrotic foci, a unique feature in the HIV-related Hodgkin lymphoma cases in the present study, may point to a proinflammatory activity. Cassol et al33 observed a significant increase in spindle-shaped cells after differentiation of monocytes into M1 compared with M2a differentiated macrophages. Interestingly, one patient of the four HIV-negative Hodgkin lymphoma cases with a ‘sarcomatoid’ pattern was suffering from chronic hepatitis C virus (HCV) infection and another patient had a severe concurrent infection resulting in a CD4+ T-cell blood count <500/μl, as frequently observed in sepsis.34 HCV, cytomegalovirus and influenza virus have also been shown to induce an M1 phenotype in macrophages.35, 36 Thus, other conditions concomitant with classical Hodgkin lymphoma can induce changes resembling the spindle cell macrophages observed in HIV-associated Hodgkin lymphoma. The spindle shape appearance of macrophages in HIV-associated Hodgkin lymphoma may be an abortive attempt of epithelioid cell formation in the absence of CD4+ T-cells.
All cases available in our registry were EBV-positive, in line with previous studies.37, 38 Thus, the clonal expansion of Hodgkin- and Reed–Sternberg cells in HIV-associated Hodgkin lymphoma probably shares several features of transformation with EBV-infected Hodgkin- and Reed–Sternberg cells arising in different conditions of immunosuppression like peripheral T-cell lymphomas,39 B-chronic lymphocytic leukemia,40, 41 or EBV-positive diffuse large B-cell lymphoma of the elderly.42 In concert with the particular composition of the microenvironment, we propose that HIV-related Hodgkin lymphoma associated with a high content of spindle-shaped macrophages and low CD4+ T-cell content represents a unique subtype of classical Hodgkin lymphoma, which should be recognized by pathologists.
References
Yotsumoto M, Hagiwara S, Ajisawa A et al. Clinical characteristics of human immunodeficiency virus-associated Hodgkin lymphoma patients in Japan. Int J Hematol 2012;96:247–253.
Biggar RJ, Jaffe ES, Goedert JJ et al. Hodgkin lymphoma and immunodeficiency in persons with HIV/AIDS. Blood 2006;108:3786–3791.
Clifford GM, Rickenbach M, Lise M et al. Hodgkin lymphoma in the Swiss HIV Cohort Study. Blood 2009;113:5737–5742.
Bohlius J, Schmidlin K, Boue F et al. HIV-1-related Hodgkin lymphoma in the era of combination antiretroviral therapy: incidence and evolution of CD4(+) T-cell lymphocytes. Blood 2011;117:6100–6108.
Marshall NA, Christie LE, Munro LR et al. Immunosuppressive regulatory T cells are abundant in the reactive lymphocytes of Hodgkin lymphoma. Blood 2004;103:1755–1762.
Bosch Princep R, Lejeune M, Salvado Usach MT et al. Decreased number of granzyme B+ activated CD8+ cytotoxic T lymphocytes in the inflammatory background of HIV-associated Hodgkin’s lymphoma. Ann Hematol 2005;84:661–666.
Thompson LD, Fisher SI, Chu WS et al. HIV-associated Hodgkin lymphoma: a clinicopathologic and immunophenotypic study of 45 cases. Am J Clin Pathol 2004;121:727–738.
Pelstring RJ, Zellmer RB, Sulak LE et al. Hodgkin’s disease in association with human immunodeficiency virus infection. Pathologic and immunologic features. Cancer 1991;67:1865–1873.
Kiyasu J, Aoki R, Tanaka PY et al. FOXP3(+) regulatory and TIA-1(+) cytotoxic T lymphocytes in HIV-associated Hodgkin lymphoma. Pathol Int 2012;62:77–83.
Steidl C, Lee T, Shah SP et al. Tumor-associated macrophages and survival in classic Hodgkin’s lymphoma. N Engl J Med 2010;362:875–885.
Kamper P, Bendix K, Hamilton-Dutoit S et al. Tumor-infiltrating macrophages correlate with adverse prognosis and Epstein-Barr virus status in classical Hodgkin’s lymphoma. Haematologica 2011;96:269–276.
Tzankov A, Matter MS, Dirnhofer S . Refined prognostic role of CD68-positive tumor macrophages in the context of the cellular micromilieu of classical Hodgkin lymphoma. Pathobiology 2010;77:301–308.
Azambuja D, Natkunam Y, Biasoli I et al. Lack of association of tumor-associated macrophages with clinical outcome in patients with classical Hodgkin’s lymphoma. Ann Oncol 2012;23:736–742.
Harris JA, Jain S, Ren Q et al. CD163 versus CD68 in tumor associated macrophages of classical Hodgkin lymphoma. Diagn Pathol 2012;7:12.
Renné C, Willenbrock K, Küppers R et al. Autocrine- and paracrine-activated receptor tyrosine kinases in classic Hodgkin lymphoma. Blood 2005;105:4051–4059.
Ma Y, Visser L, Roelofsen H et al. Proteomics analysis of Hodgkin lymphoma: identification of new players involved in the cross-talk between HRS cells and infiltrating lymphocytes. Blood 2008;111:2339–2346.
Imai T, Baba M, Nishimura M et al. The T cell-directed CC chemokine TARC is a highly specific biological ligand for CC chemokine receptor 4. J Biol Chem 1997;272:15036–15042.
Goodenow MM, Rose SL, Tuttle DL et al. HIV-1 fitness and macrophages. J Leukoc Biol 2003;74:657–666.
Flavell DJ, Wright DH . The Reed-Sternberg cell/lymphocyte rosette. I. Properties of rosettes formed between Hodgkin’s cell lines and allogeneic lymphocytes. Br J Cancer 1989;59:165–173.
Hansch HC, Smith DA, Mielke ME et al. Mechanisms of granuloma formation in murine Mycobacterium avium infection: the contribution of CD4+ T cells. Int Immunol 1996;8:1299–1310.
Muller H, Takeshita M . In situ immunophenotype of macrophages and lymphocytes in granuloma formation of tuberculous lymphadenitis in HIV-infected and immunocompetent patients. Res Virol 1991;142:159–172.
Muller-Hermelink HK, Kaiserling E, Sonntag HG . Modulation of epithelioid cell granuloma formation to apathogenic mycobacteria by cyclosporin A. Pathol Res Pract 1982;175:80–96.
Mantovani A, Sozzani S, Locati M et al. Macrophage polarization: tumor-associated macrophages as a paradigm for polarized M2 mononuclear phagocytes. Trends Immunol 2002;23:549–555.
Qian BZ, Pollard JW . Macrophage diversity enhances tumor progression and metastasis. Cell 2010;141:39–51.
Crouser ED, Culver DA, Knox KS et al. Gene expression profiling identifies MMP-12 and ADAMDEC1 as potential pathogenic mediators of pulmonary sarcoidosis. Am J Respir Crit Care Med 2009;179:929–938.
Ehrt S, Schnappinger D, Bekiranov S et al. Reprogramming of the macrophage transcriptome in response to interferon-gamma and Mycobacterium tuberculosis: signaling roles of nitric oxide synthase-2 and phagocyte oxidase. J Exp Med 2001;194:1123–1140.
Mantovani A, Allavena P, Sica A . Tumour-associated macrophages as a prototypic type II polarised phagocyte population: role in tumour progression. Eur J Cancer 2004;40:1660–1667.
Lugo-Villarino G, Verollet C, Maridonneau-Parini I et al. Macrophage polarization: convergence point targeted by Mycobacterium tuberculosis and HIV. Front Immunol 2011;2:43.
Brown JN, Kohler JJ, Coberley CR et al. HIV-1 activates macrophages independent of Toll-like receptors. PLoS One 2008;3:e3664.
Fischer-Smith T, Tedaldi EM, Rappaport J . CD163/CD16 coexpression by circulating monocytes/macrophages in HIV: potential biomarkers for HIV infection and AIDS progression. AIDS Res Hum Retroviruses 2008;24:417–421.
Burdo TH, Lentz MR, Autissier P et al. Soluble CD163 made by monocyte/macrophages is a novel marker of HIV activity in early and chronic infection prior to and after anti-retroviral therapy. J Infect Dis 2011;204:154–163.
Fuentes-Duculan J, Suarez-Farinas M, Zaba LC et al. A subpopulation of CD163-positive macrophages is classically activated in psoriasis. J Invest Dermatol 2010;130:2412–2422.
Cassol E, Cassetta L, Rizzi C et al. M1 and M2a polarization of human monocyte-derived macrophages inhibits HIV-1 replication by distinct mechanisms. J Immunol 2009;182:6237–6246.
Chen X, Ye J . Analysis of peripheral blood lymphocyte subsets and prognosis in patients with septic shock. Microbiol Immunol 2011;55:736–742.
Hiscott J, Nguyen TL, Arguello M et al. Manipulation of the nuclear factor-kappaB pathway and the innate immune response by viruses. Oncogene 2006;25:6844–6867.
Haller O, Kochs G, Weber F . Interferon, Mx, and viral countermeasures. Cytokine Growth Factor Rev 2007;18:425–433.
Audouin J, Diebold J, Pallesen G . Frequent expression of Epstein-Barr virus latent membrane protein-1 in tumour cells of Hodgkin’s disease in HIV-positive patients. J Pathol 1992;167:381–384.
Guidoboni M, Ponzoni M, Caggiari L et al. Latent membrane protein 1 deletion mutants accumulate in reed-sternberg cells of human immunodeficiency virus-related Hodgkin’s lymphoma. J Virol 2005;79:2643–2649.
Quintanilla-Martinez L, Fend F, Moguel LR et al. Peripheral T-cell lymphoma with Reed-Sternberg-like cells of B-cell phenotype and genotype associated with Epstein-Barr virus infection. Am J Surg Pathol 1999;23:1233–1240.
Kanzler H, Küppers R, Helmes S et al. Hodgkin and Reed-Sternberg-like cells in B-cell chronic lymphocytic leukemia represent the outgrowth of single germinal-center B-cell-derived clones: potential precursors of Hodgkin and Reed-Sternberg cells in Hodgkin’s disease. Blood 2000;95:1023–1031.
Mao Z, Quintanilla-Martinez L, Raffeld M et al. IgVH mutational status and clonality analysis of Richter’s transformation: diffuse large B-cell lymphoma and Hodgkin lymphoma in association with B-cell chronic lymphocytic leukemia (B-CLL) represent 2 different pathways of disease evolution. Am J Surg Pathol 2007;31:1605–1614.
Oyama T, Yamamoto K, Asano N et al. Age-related EBV-associated B-cell lymphoproliferative disorders constitute a distinct clinicopathologic group: a study of 96 patients. Clin Cancer Res 2007;13:5124–5132.
Acknowledgements
We would like to thank Ralf Lieberz, Yvonne Michel and Monica Mörtel for excellent technical assistance. This project was supported by DFG grant HA 6145/1-1.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on Modern Pathology website
Rights and permissions
About this article
Cite this article
Hartmann, S., Jakobus, C., Rengstl, B. et al. Spindle-shaped CD163+ rosetting macrophages replace CD4+ T-cells in HIV-related classical Hodgkin lymphoma. Mod Pathol 26, 648–657 (2013). https://doi.org/10.1038/modpathol.2012.217
Received:
Revised:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/modpathol.2012.217