Abstract
Background
To validate the Feverkidstool, a prediction model consisting of clinical signs and symptoms and C-reactive protein (CRP) to identify serious bacterial infections (SBIs) in febrile children, and to determine the incremental diagnostic value of procalcitonin.
Methods
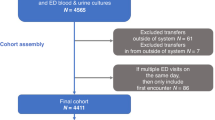
This prospective observational study that was carried out at two Dutch emergency departments included children with fever, aged 1 month to 16 years. The prediction models were developed with polytomous logistic regression differentiating “pneumonia” and “other SBIs” from “non-SBIs” using standardized, routinely collected data on clinical signs and symptoms, CRP, and procalcitonin.
Results
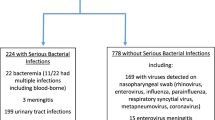
A total of 1,085 children were included with a median age of 1.6 years (interquartile range 0.8–3.4); 73 children (7%) had pneumonia and 98 children (9%) had other SBIs. The Feverkidstool showed good discriminative ability in this new population. After adding procalcitonin to the Feverkidstool, c-statistic for “pneumonia” increased from 0.85 (95% confidence interval (CI) 0.76–0.94) to 0.86 (0.77–0.94) and for “other SBI” from 0.81 (0.73–0.90) to 0.83 (0.75– 0.91). A model with clinical features and procalcitonin performed similar to the Feverkidstool.
Conclusion
This study confirms the external validity of the Feverkidstool, with CRP and procalcitonin being equally valuable for predicting SBI in our population of febrile children. Our findings do not support routine dual use of CRP and procalcitonin.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Alpern ER, Stanley RM, Gorelick MH et al, Epidemiology of a pediatric emergency medicine research network: the PECARN Core Data Project. Pediatr Emerg Care 2006; 22: 689–99.
Van den Bruel A, Haj-Hassan T, Thompson M, Buntinx F, Mant D . Diagnostic value of clinical features at presentation to identify serious infection in children in developed countries: a systematic review. Lancet 2010; 375: 834–45.
Van den Bruel A, Thompson MJ, Haj-Hassan T et al, Diagnostic value of laboratory tests in identifying serious infections in febrile children: systematic review. Br Med J 2011; 342: d3082.
Yo CH, Hsieh PS, Lee SH et al, Comparison of the test characteristics of procalcitonin to c-reactive protein and leukocytosis for the detection of serious bacterial infections in children presenting with fever without source: a systematic review and meta-analysis. Ann Emerg Med 2012; 60: 591–600.
Thompson M, Van den Bruel A, Verbakel J et al, Systematic review and validation of prediction rules for identifying children with serious infections in emergency departments and urgent-access primary care. Health Technol Assess 2012; 16: 1–100.
Craig JC, Williams GJ, Jones M et al, The accuracy of clinical symptoms and signs for the diagnosis of serious bacterial infection in young febrile children: prospective cohort study of 15 781 febrile illnesses. Br Med J 2010; 340: c1594.
Irwin AD, Wickenden J, Le Doare K, Ladhani S, Sharland M . Supporting decisions to increase the safe discharge of children with febrile illness from the emergency department: a systematic review and meta-analysis. Arch Dis Child 2015; 101: 259–66.
Nijman RG, Vergouwe Y, Thompson M et al, Clinical prediction model to aid emergency doctors managing febrile children at risk of serious bacterial infections: diagnostic study. Br Med J 2013; 346: f1706.
Maguire JL, Kulik DM, Laupacis A, Kuppermann N, Uleryk EM, Parkin PC . Clinical prediction rules for children: a systematic review. Pediatrics 2011; 128: e666–77.
Gomez B, Bressan S, Mintegi S et al, Diagnostic value of procalcitonin in well-appearing young febrile infants. Pediatrics 2012; 130: 815–22.
Luaces-Cubells C, Mintegi S, Garcia-Garcia JJ et al, Procalcitonin to detect invasive bacterial infection in non-toxic-appearing infants with fever without apparent source in the emergency department. Pediatr Infect Dis J 2012; 31: 645–7.
van Rossum AM, Wulkan RW, Oudesluys-Murphy AM . Procalcitonin as an early marker of infection in neonates and children. Lancet Infect Dis 2004; 4: 620–30.
Nijman RG, Moll HA, Smit FJ et al, C-reactive protein, procalcitonin and the lab-score for detecting serious bacterial infections in febrile children at the emergency department: a prospective observational study. Pediatr Infect Dis J 2014; 33: e273–9.
Bouwhuis CB, Kromhout MM, Twijnstra MJ, Buller HA, Moll HA . Few ethnic differences in acute pediatric problems: 10 years of acute care in the Sophia Children's Hospital in Rotterdam. Ned Tijdschr Geneeskd 2001; 145: 1847–51.
Hardelid P, Dattani N, Gilbert R, . Programme Board of the Royal College of P, Child H, Child Death Overview Working G. Estimating the prevalence of chronic conditions in children who die in England, Scotland and Wales: a data linkage cohort studyBr Med J Open 2014; 4: e005331.
van Veen M, Steyerberg EW, Ruige M et al, Manchester triage system in paediatric emergency care: prospective observational study. Br Med J 2008; 337: a1501.
Turner NM. Advanced Paediatric Life Support (APLS), 2nd edn. Maarsen, the Netherlands: Reed Business, 2006.
Bonadio WA, Hennes H, Smith D et al, Reliability of observation variables in distinguishing infectious outcome of febrile young infants. Pediatr Infect Dis J 1993; 12: 111–4.
McCarthy PL, Sharpe MR, Spiesel SZ et al, Observation scales to identify serious illness in febrile children. Pediatrics 1982; 70: 802–9.
Bleeker SE, Derksen-Lubsen G, Grobbee DE, Donders AR, Moons KG, Moll HA . Validating and updating a prediction rule for serious bacterial infection in patients with fever without source. Acta Paediatr 2007; 96: 100–4.
Reitsma JB, Rutjes AW, Khan KS, Coomarasamy A, Bossuyt PM . A review of solutions for diagnostic accuracy studies with an imperfect or missing reference standard. J Clin Epidemiol 2009; 62: 797–806.
R Foundation for Statistical Computing. R: a language and environment for statistical computing Vienna (Austria), 2006 (30-04-2014). http://www.R-project.org/.
Steyerberg EW. In: M Gail KK, J Samet, A Tsiatis, W Wong, eds. Clinical Prediction Models: A Practical Approach to Development, Validation, and Updating, 1st edn. Chapter 7. New York, NY, USA: Springer, 2009, pp113–138.
Moons KG, Donders RA, Stijnen T, Harrell FE Jr. . Using the outcome for imputation of missing predictor values was preferred. J Clin Epidemiol 2006; 59: 1092–101.
Marshall A, Altman DG, Holder RL, Royston P . Combining estimates of interest in prognostic modelling studies after multiple imputation: current practice and guidelines. BMC Med Res Methodol 2009; 9: 57.
Van Calster B, Van Belle V, Vergouwe Y, Timmerman D, Van Huffel S, Steyerberg EW . Extending the c-statistic to nominal polytomous outcomes: the Polytomous Discrimination Index. Stat Med 2012; 31: 2610–2626.
Vickers AJ, Cronin AM, Begg CB . One statistical test is sufficient for assessing new predictive markers. BMC Med Res Methodol 2011; 11: 13.
Van Calster B, Vergouwe Y, Looman CW, Van Belle V, Timmerman D, Steyerberg EW . Assessing the discriminative ability of risk models for more than two outcome categories. Eur J Epidemiol 2012; 27: 761–770.
Van Hoorde K, Vergouwe Y, Timmerman D, Van Huffel S, Steyerberg EW, Van Calster B . Simple dichotomous updating methods improved the validity of polytomous prediction models. J Clin Epidemiol 2013; 66: 1158–65.
Milcent K, Faesch S, Gras-Le Guen C et al, Use of procalcitonin assays to predict serious bacterial infection in young febrile Infants. JAMA Pediatrics 2016; 170: 62–9.
Galetto-Lacour A, Zamora SA, Andreola B et al, Validation of a laboratory risk index score for the identification of severe bacterial infection in children with fever without source. Arch Dis Child 2010; 95: 968–73.
Lacour AG, Zamora SA, Gervaix A . A score identifying serious bacterial infections in children with fever without source. Pediatr Infect Dis J 2008; 27: 654–656.
Bressan S, Gomez B, Mintegi S et al, Diagnostic performance of the lab-score in predicting severe and invasive bacterial infections in well-appearing young febrile infants. Pediatr Infect Dis J 2012; 31: 1239–44.
Mallett S, Halligan S, Thompson M, Collins GS, Altman DG . Interpreting diagnostic accuracy studies for patient care. Br Med J 2012; 345: e3999.
Thayyil S, Shenoy M, Hamaluba M, Gupta A, Frater J, Verber IG . Is procalcitonin useful in early diagnosis of serious bacterial infections in children? Acta Paediatr 2005; 94: 155–8.
Manzano S, Bailey B, Gervaix A, Cousineau J, Delvin E, Girodias JB . Markers for bacterial infection in children with fever without source. Arch Dis Child 2011; 96: 440–6.
Yu CW, Juan LI, Wu MH, Shen CJ, Wu JY, Lee CC . Systematic review and meta-analysis of the diagnostic accuracy of procalcitonin, C-reactive protein and white blood cell count for suspected acute appendicitis. Br J Surg 2013; 100: 322–9.
Verbakel JY, Van den Bruel A, Thompson M et al, How well do clinical prediction rules perform in identifying serious infections in acutely ill children across an international network of ambulatory care datasets? BMC Med 2013; 11: 10.
Vergouwe Y, Royston P, Moons KG, Altman DG . Development and validation of a prediction model with missing predictor data: a practical approach. J Clin Epidemiol 2010;2:205–14.
McIntosh K . Community-acquired pneumonia in children. N Engl J Med 2002; 346: 429–37.
Wilkins TR, Wilkins RL . Clinical and radiographic evidence of pneumonia. Radiol Technol 2005; 77: 106–110.
Lynch T, Bialy L, Kellner JD et al, A systematic review on the diagnosis of pediatric bacterial pneumonia: when gold is bronze. PLoS ONE 2010; 5: e11989.
Nijman RG, Thompson M, van Veen M, Perera R, Moll HA, Oostenbrink R . Derivation and validation of age and temperature specific reference values and centile charts to predict lower respiratory tract infection in children with fever: prospective observational study. Br Med J 2012; 345: e4224.
Elshout G, van Ierland Y, Bohnen AM et al, Alarm signs and antibiotic prescription in febrile children in primary care: an observational cohort study. Br J Gen Pract 2013; 63: e437–44.
Acknowledgements
We thank Barry Koelewijn, Sascha Smit, members of the point of care testing team of the Erasmus MC—Sophia Children’s Hospital, and all nurses at both study sites for their valuable contributions to the study. Moreover, we acknowledge Marjolein Neele for contributing to the data collection and for analyzing the laboratory samples at the Maasstad hospital. We thank Evelien Kerkhof for supporting data collection and defining final diagnoses. Finally, we acknowledge Marcel de Wilde for designing the electronic data entry forms at the Erasmus MC. None had access to the data or received additional financial compensation. The Afinion AS100 analyzer and Afinion AS100 C-Reactive Protein bedside kits were provided by Axis-Shield PoC AS, Norway, and were distributed by Clindia Benelux BV. The procalcitonin kits were supplied by Brahms.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Author contributions
All authors substantially contributed to the writing (i.e., drafting and/or critical revision) of the manuscript. R.G.N. is the main author of the paper and was involved in development and implementation of the study’s protocol, data acquisition, patient inclusion, and data analysis. H.A.M. contributed to obtaining funding for the study, protocol development, and data collection and monitoring. Y.V. was responsible for statistical analyses and interpretation of the results. F.J.S. was responsible for protocol development, data collection, and study implementation. F.W. was responsible for analyzing laboratory samples and data collection. E.W.S. contributed to obtaining funding, protocol development, statistical analyses, and interpretation of the results. J.v.d.L. contributed to obtaining funding and protocol development, supervising the data collection and monitoring, and providing technical support. Y.B.d.R. was involved in protocol development, laboratory analysis, and data collection. R.O. was mainly responsible for obtaining funding for the study, supervised the research project, and was responsible for protocol development, data collection, and interpretation of the results. All authors have read and approved the final version of the manuscript; R.G.N. and R.O. had full access to all data and take responsibility for the integrity of the data and accuracy of the data analysis.
Statement of financial support
R.G.N. is supported by ZonMW, a Dutch organization for health research and development, and Erasmus MC Doelmatigheid; Y.V. is funded by the Netherlands Organization for Scientific Research (Grant 917.11.383); and R.O. is supported by a fellowship grant of the European Society of Pediatric Infectious Diseases in 2010.
Disclaimer
Neither funding sources, nor Axis-Shield PoC AS, Clindia Benelux BV, or Brahms were involved in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Supplementary material is linked to the online version of the paper at
Supplementary information
Rights and permissions
About this article
Cite this article
Nijman, R., Vergouwe, Y., Moll, H. et al. Validation of the Feverkidstool and procalcitonin for detecting serious bacterial infections in febrile children. Pediatr Res 83, 466–476 (2018). https://doi.org/10.1038/pr.2017.216
Received:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/pr.2017.216
This article is cited by
-
Procalcitonin use in febrile children attending European emergency departments: a prospective multicenter study
BMC Pediatrics (2025)
-
Antibiotika in klinischen pädiatrischen Notfallambulanzen. Antibiotic Stewardship oder Suche nach dem „Schatz der nie gelungen“?
Monatsschrift Kinderheilkunde (2024)
-
Clinical prediction models for serious infections in children: external validation in ambulatory care
BMC Medicine (2023)
-
Diagnostic value of biomarkers for paediatric urinary tract infections in primary care: systematic review and meta-analysis
BMC Family Practice (2021)
-
Incidence, clinical profile, and risk factors for serious bacterial infections in children hospitalized with fever in Ujjain, India
BMC Infectious Diseases (2020)