Abstract
Background
Prenatal maternal obesity has been associated with an increased risk of neurocognitive problems in childhood, but there are fewer studies on executive functioning.
Methods
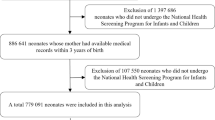
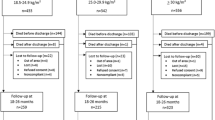
Tests and questionnaires to assess neurodevelopment, executive functioning, and the ability to delay gratification were conducted in 113 children (mean (SD)=4.24 (0.63) years of age) born to mothers with very severe obesity (SO, body mass index (BMI)⩾40 kg/m2, n=51) or to lean mothers (BMI⩽25 kg/m2, n=62).
Results
Prenatal maternal SO predicted poorer neurodevelopment (unstandardized regression coefficient (B)=−0.42, 95% confidence interval (CI) (−0.82; −0.02)), worse problem-solving (odd ratio (OR)=0.60, 95% CI (1.13; 0.07)), and fine motor skills (OR=4.91, 95% CI (1.27; 19.04)), poorer executive functioning in areas of attention, inhibitory control, and working memory (standardized B=3.75, 95% CI (1.01; 13.93)) but not in self-gratification delay. The effects were independent of maternal concurrent psychological well-being and child’s BMI, but not independent of maternal education.
Conclusion
Future studies should investigate whether perinatal management of maternal obesity could prevent adverse outcomes in child neurodevelopment.
Similar content being viewed by others
Log in or create a free account to read this content
Gain free access to this article, as well as selected content from this journal and more on nature.com
or
References
Heslehurst N, Rankin J, Wilkinson JR, Summerbell CD . A nationally representative study of maternal obesity in England, UK: trends in incidence and demographic inequalities in 619 323 Births, 1989-2007. Int J Obes 2010;34:420–8.
Weng SF, Redsell Sa, Swift Ja, Yang M, Glazebrook CP . Systematic review and meta-analyses of risk factors for childhood overweight identifiable during infancy. Arch Dis Child 2012;97:1019–26.
Casey B, Somerville L, Gotlib I et al, Behavioral and neural correlates of delay of gratification 40 years later. Proc Natl Acad Sci USA 2011;108:14998–15003.
Kilgour A, Starr J, Whalley L . Associations between childhood intelligence (IQ), adult morbidity and mortality. Maturitas 2010;65:98–105.
Heikura U, Taanila A, Hartikainen A et al, Variations in prenatal sociodemographic factors associated with intellectual disability: a study of the 20-year interval between two birth cohorts in Northern Finland. Am J Epidemiol 2008;167:169–77.
Mann J, McDermott S, Hardin J, Pan C, Zhang Z . Pre-pregnancy body mass index, weight change during pregnancy, and risk of intellectual disability in children. BJOG 2013;120:309–19.
Neggers Y, Goldenberg R, Ramey S, Cliver S . Maternal prepregnancy body mass index and psychomotor development in children. Acta Obstet Gynecol Scand 2003;82:235–40.
Gage S, Lawlor D, Tilling K, Fraser A . Associations of maternal weight gain in pregnancy with offspring cognition in childhood and adolescence: findings from the avon longitudinal study of parents and children. Am J Epidemiol 2013;177:402–10.
Huang L, Yu X, Keim S, Li L, Zhang L, Zhang J . Maternal prepregnancy obesity and child neurodevelopment in the Collaborative Perinatal Project. Int J Epidemiol 2014;43:783–92.
Pugh S, Richardson G, Hutcheon J et al, Maternal obesity and excessive gestational weight gain are associated with components of child cognition. J Nutr 2015;145:2562–9.
Hinkle S, Schieve L, Stein A, Swan D, Ramakrishnan U, Sharma A . Associations between maternal prepregnancy body mass index and child neurodevelopment at 2 years of age. Int J Obes 2012;36:1312–9.
Krakowiak P, Walker CK, Bremer AA et al, Maternal metabolic conditions and risk for autism and other neurodevelopmental disorders. Pediatrics 2012;129:e1121–8.
Craig W, Palomaki G, Neveux L, Haddow J . Maternal body mass index during pregnancy and offspring neurocognitive development. Obstet Med 2013;6:20–25.
Casas M, Chatzi L, Carsin A et al, Maternal pre-pregnancy overweight and obesity, and child neuropsychological development: two southern european birth cohort studies. Int J Epidemiol 2013;42:506–17.
O’Connor Duffany K, McVeigh K, Kershaw T, Lipkind H, Ickovics J . Maternal obesity: risks for developmental delays in early childhood. Matern Child Health J 2016;20:219–30.
Basatemur E, Gardiner J, Williams C, Melhuish E, Barnes J, Sutcliffe A . Maternal prepregnancy BMI and child cognition: A longitudinal cohort study. Pediatrics 2013;131:56–63.
Tanda R, Salsberry P, Reagan P, Fang M . The impact of prepregnancy obesity on children’s cognitive test scores. Matern Child Health J 2013;17:222–9.
Hinkle S, Sharma A, Kim S, Schieve L . Maternal prepregnancy weight status and associations with children’s development and disabilities at kindergarten. Int J Obes 2013;37:1344–51.
Brion M, Zeegers M, Jaddoe V et al, Intrauterine effects of maternal prepregnancy overweight on child cognition and behavior in 2 cohorts. Pediatrics 2011;127:e202–11.
Buss C, Entringer S, Davis E et al, Impaired executive function mediates the association between maternal pre-pregnancy body mass index and child ADHD symptoms. PLoS ONE 2012;7:e37758.
Seeyave D, Coleman S, Appugliese D et al, Ability to delay gratification at age 4 years and risk of overweight at age 11 years. Arch Pediatr Adolesc Med 2009;163:303–8.
Molyneaux E, Poston L, Ashurst-Williams S, Howard LM . Obesity and mental disorders during pregnancy and postpartum. Obstet Gynecol 2014;123:857–67.
Mina T, Denison F, Forbes S, Stirrat L, Norman J, Reynolds R . Associations of mood symptoms with ante- and postnatal weight change in obese pregnancy are not mediated by cortisol. Psychol Med 2015;45:3133–3146.
Buss C, Davis E, Hobel C, Sandman C . Maternal pregnancy-specific anxiety is associated with child executive function at 6-9 years age. Stress 2011;14:665–76.
Pearson R, Bornstein M, Cordero M et al, Maternal perinatal mental health and offspring academic achievement at age 16: the mediating role of childhood executive function. J Child Psychol Psychiatry 2016;57:491–501.
Ibanez G, Bernard J, Rondet C et al, Effects of antenatal maternal depression and anxiety on children’s early cognitive development: A prospective cohort study. PLoS ONE 2015;10:e0135849.
Liang J, Matheson B, Kaye W, Boutelle K . Neurocognitive correlates of obesity and obesity-related behaviors in children and adolescents. Int J Obes 2014;38:494–506.
Eriksen H, Kesmodel U, Underbjerg M, Kilburn T, Bertrand J, Mortensen E . Predictors of intelligence at the age of 5: Family, pregnancy and birth characteristics, postnatal influences, and postnatal growth. PLoS One 2013;8:1–8.
Mischel W, Shoda Y, Rodriguez MI . Delay of Gratification in Children. Science 1989;244:933–8.
Kidd C, Palmeri H, Aslin R . Rational snacking: Young children’s decision-making on the marshmallow task is moderated by beliefs about environmental reliability. Cognition 2013;126:109–14.
McClelland M, Cameron C, Duncan R et al, Predictors of early growth in academic achievement: The head-toes-knees-shoulders task. Front Psychol 2014;5:1–14.
Hornman J, Kertjens JM, de Winter AF, Arend BF, Reijneveld SA . Validity and internal consistency of the Ages and Stages Questionnaire 60-month version and the effect of three scoring methods. 2013 Early Human Dev 89:1011–5.
Jo H, Schieve L, Sharma A, Hinkle S, Li R, Lind J . Maternal prepregnancy body mass index and child psychosocial development at 6 years of age. Pediatrics 2015;135:e1198–209.
Wylie A, Sundaram R, Kus C, Ghassabian A, Yeung E . Maternal prepregnancy obesity and achievement of infant motor developmental milestones in the upstate KIDS study. Obesity 2015;23:907–13.
Whitehouse A, Shelton W, Ing C, Newham J . Prenatal, perinatal, and neonatal risk factors for specific language impairment: a prospective pregnancy cohort study. J Speech Lang Hear Res 2014;57:1418–27.
Bonato P, Boland FJ . Delay of gratification in obese children. Addict Behav 1983;8:71–4.
Bourget V, White DR . Performance of overweight and normal-weight girls on Delay of gratification Tasks. Int J Eat Disord 1984;3:63–71.
Francis L, Susman E . Self-regulation and rapid weight gain in children from age 3 to 12 years. Arch Pediatr Adolesc Med 2009;163:297–302.
Keim S, Daniels J, Dole N, Herring A, Siega-Riz A, Scheidt P . A prospective study of maternal anxiety, perceived stress, and depressive symptoms in relation to infant cognitive development. Early Hum Dev 2011;87:373–80.
Cordner Z, Tamashiro K . Effects of high-fat diet exposure on learning & memory. Physiol Behav 2015;152:363–71.
Lam L, Lawlis T . Feeding the brain - The effects of micronutrient interventions on cognitive performance among school-aged children: a systematic review of randomized controlled trials. Clin Nutr 2016. (doi:10.1016/j.clnu.2016.06.013).
Mohd-Shukri N, Duncan A, Denison F et al, Health behaviours during pregnancy in women with very severe obesity. Nutrients 2015;7:8431–43.
Bernard J, de Agostini M, Forhan A et al, The dietary n6:n3 fatty acid ratio during pregnancy is inversely associated with child neurodevelopment in the EDEN mother-child cohort. J. Nutrition 2013;143:1481–8.
Bilbo S, Schwarz J . The immune system and developmental programming of brain and behavior. Front. Neuroendocrinol 2012;33:267–86.
Brown AS, Sourander A, Hinkka-Yli-Soumaki S, McKeague IW, Sundvall J, Surcel HM . Elevated maternal C-reactive protein and autism in a national birth cohort. Mol Psychiatry 2014;19:259–64.
Acknowledgements
We thank the mother-and-baby participants and the pediatric nurse team especially Joan Thomson in the Clinical Research Facility, The Royal Hospital for Sick Children, NHS Lothian).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Statement of Financial Support
We thank Tommy’s the Baby Charity for the generous funding. THM received a Principal Development Scholarship, a Charles Darwin Scholarship, and a Global Research Scholarship, University of Edinburgh, Scotland. ML is supported by the Academy of Finland and University of Helsinki Funds. AJD received a Scottish Senior Clinical Fellowship (SCD/09). THM, AJD, and RMR acknowledge the support of the British Heart Foundation.
Supplementary material is linked to the online version of the paper at http://www.nature.com/pr
Supplementary information
Rights and permissions
About this article
Cite this article
Mina, T., Lahti, M., Drake, A. et al. Prenatal exposure to maternal very severe obesity is associated with impaired neurodevelopment and executive functioning in children. Pediatr Res 82, 47–54 (2017). https://doi.org/10.1038/pr.2017.43
Received:
Accepted:
Published:
Issue date:
DOI: https://doi.org/10.1038/pr.2017.43
This article is cited by
-
Current states in understanding oligodendroglia-mediated neurological issues in neurofibromatosis type 1 (NF1)
Acta Neuropathologica Communications (2025)
-
Impact of healthy pregnancy and lifestyle in mothers on developmental delay in their offspring: a strength-based analysis of a longitudinal study among indigenous children in Australia
BMC Pregnancy and Childbirth (2024)
-
Maternal metabolic syndrome in pregnancy and child development at age 5: exploring mediating mechanisms using cord blood markers
BMC Medicine (2023)
-
Maternal pre-pregnancy BMI and offspring hyperactivity–inattention trajectories from 3 to 8 years in the EDEN birth cohort study
European Child & Adolescent Psychiatry (2023)
-
Maternal pre-pregnancy body mass index and mental health problems in early adolescents from the 2004 Pelotas birth cohort
Scientific Reports (2022)