Abstract
Background and objectives
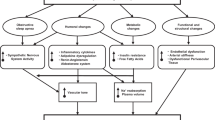
Individuals with obesity often face obesity bias, which may influence the delivery of appropriate medical care. Our aim is to evaluate the adequacy of therapeutic decisions regarding the pharmacological treatment for hypertension in patients with diabetes, both with and without obesity.
Methods
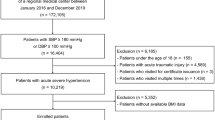
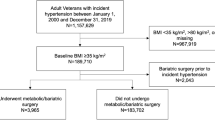
This is a multicentric cross-sectional study of patients with type 2 diabetes and arterial hypertension who received outpatient care in Southern Brazil. Participants were stratified into two groups according to their body mass index (BMI): lower weight (BMI < 25.0 kg/m2) and with obesity (BMI ≥ 30.0 kg/m2). The primary outcome evaluated was the difference in pharmacological treatment decisions for hypertension between groups, considering individualized hypertension targets from American Diabetes Association (ADA), European Society of Hypertension (ESH), and European Society of Cardiology (ESC) guidelines. Data were analyzed as a binary endpoint (failure to receive treatment intensification vs. receiving treatment intensification when necessary) and groups were compared using multivariable logistic regression.
Results
This study included 204 participants, of which 53 were at a lower weight and 151 had obesity. Patients with obesity more frequently failed to receive appropriate treatment intensification when compared to individuals with lower weight. The differences between the study groups were observed when considering the blood pressure target of three societies: ESH (adjusted OR 2.28 [95% CI 1.12–4.63], p = 0.022), ESC (adjusted OR 2.13 [95% CI 1.05–4.31], p = 0.035), and ADA (adjusted OR 2.33 [95% CI 1.13–4.77], p = 0.021).
Conclusion
These findings suggest that patients with obesity may face potential disparities in hypertension management, and obesity status may be related to therapeutic inertia in the management of arterial hypertension in this group.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on SpringerLink
- Instant access to the full article PDF.
USD 39.95
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
Data availability
The data collected for the study will be available for one year after publication of the article upon justified request to the email address of the main researcher and with a signed data access agreement.
References
Olenski AR, Zimerman A, Coussens S, Jena AB. Behavioral heuristics in coronary-artery bypass graft surgery. N Engl J Med. 2020;382:778–9.
Avorn J. The psychology of clinical decision making — implications for medication use. N Engl J Med. 2018;378:689–91.
Andreyeva T, Puhl RM, Brownell KD. Changes in perceived weight discrimination among Americans, 1995–1996 through 2004–2006. Obesity. 2008;16:1129–34.
Schwartz MB, Chambliss HO, Brownell KD, Blair SN, Billington C. Weight bias among health professionals specializing in obesity. Obes Res. 2003;11:1033–9.
Puhl RM, Latner JD, King KM, Luedicke J. Weight bias among professionals treating eating disorders: Attitudes about treatment and perceived patient outcomes. Int J Eating Disorders. 2014;47:65–75.
Brown I. Nurses’ attitudes towards adult patients who are obese: literature review. J Adv Nurs. 2006;53:221–32.
Sabin JA, Marini M, Nosek BA. Implicit and explicit anti-fat bias among a large sample of medical doctors by BMI, Race/Ethnicity and gender. PLoS ONE. 2012;7:e48448.
Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity. 2009;17:941–64.
Telo GH, Friedrich Fontoura L, Avila GO, Gheno V, Bertuzzo Brum MA, Teixeira JB, et al. Obesity bias: How can this underestimated problem affect medical decisions in healthcare? A systematic review. Obes Rev. 2024;25:e13696.
Alessi J, de Oliveira GB, Erthal IN, Teixeira JB, Scherer GDLG, Jaeger EH, et al. Diabetes and obesity bias: are we intensifying the pharmacological treatment in patients with and without obesity with equity? Diabetes Care. 2021;44:e206–8.
Tsimihodimos V, Gonzalez-Villalpando C, Meigs JB, Ferrannini E. Hypertension and diabetes mellitus. Hypertension. 2018;71:422–8.
Vargas-Uricoechea H, Cáceres-Acosta MF. Control of blood pressure and cardiovascular outcomes in type 2 diabetes. Open Med. 2018;13:304–23.
Marx N, Federici M, Schütt K, Müller-Wieland D, Ajjan RA, Antunes MJ, et al. ESC Guidelines for the management of cardiovascular disease in patients with diabetes. Eur Heart J. 2023;44:4043–140.
Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: guidelines for reporting observational studies. J Clin Epidemiol. 2008;61:344–9.
Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:1–253. i–xii
ElSayed NA, Aleppo G, Bannuru RR, Bruemmer D, Collins BS, Das SR, et al. 10. Cardiovascular disease and risk management: standards of care in diabetes—2024. Diabetes Care. 2024;47:S179–218.
Mancia G, Kreutz R, Brunstr M, Burnier M, Grassi G, Januszewicz A, et al. 2023 ESH Guidelines for the management of arterial hypertension [Internet]. 2023. Available from: www.jhypertension.com.
Maggio CA, Pi-Sunyer FX. Obesity and type 2 diabetes. Endocrinol Metab Clin North Am. 2003;32:805–22.
Seravalle G, Grassi G. Obesity and hypertension. Pharmacol Res. 2017;122:1–7.
Kim MS, Kim WJ, Khera AV, Kim JY, Yon DK, Lee SW, et al. Association between adiposity and cardiovascular outcomes: an umbrella review and meta-analysis of observational and Mendelian randomization studies. Eur Heart J. 2021;42:3388–403.
Brunström M, Carlberg B. Effect of antihypertensive treatment at different blood pressure levels in patients with diabetes mellitus: systematic review and meta-analyses. BMJ. 2016;352:i717.
Rosen AB, Schneider EC. Colorectal cancer screening disparities related to obesity and gender. J Gen Intern Med. 2004;19:332–8.
Østbye T, Taylor DH, Yancy WS, Krause KM. Associations between obesity and receipt of screening mammography, Papanicolaou tests, and influenza vaccination: results from the Health and Retirement Study (HRS) and the Asset and Health Dynamics Among the Oldest Old (AHEAD) Study. Am J Public Health. 2005;95:1623–30.
Puhl RM, Brownell KD. Confronting and coping with weight stigma: an investigation of overweight and obese adults. Obesity. 2006;14:1802–15.
Bocquier A, Verger P, Basdevant A, Andreotti G, Baretge J, Villani P, et al. Overweight and obesity: knowledge, attitudes, and practices of general practitioners in France. Obes Res. 2005;13:787–95.
Sutin AR, Stephan Y, Terracciano A. Weight discrimination and risk of mortality. Psychol Sci. 2015;26:1803–11. https://doi.org/10.1177/0956797615601103.
Funding
This work was conducted with support from Research Incentive Fund (FIPE/HCPA), Postgraduate Program in Endocrinology Health Sciences at the Universidade Federal do Rio Grande do Sul, School of Medical Sciences at the Pontifícia Universidade Católica do Rio Grande do Sul and Hospital São Lucas da Pontifícia Universidade Católica do Rio Grande do Sul. This study was funded in part by the Coordination for the improvement of Higher Education Personnel – Brazil (CAPES) - Finance Code 001.
Author information
Authors and Affiliations
Contributions
GHT and J.A: Conceptualization, Methodology, Data curation, Writing- Original draft preparation. L.S.M: Methodology, Writing- Original draft preparation, Formal Analysis. L.F.F, J.B.T, I.N.E, V.G. M.A.B.B., G.D.O.A, J.S: Methodology, Writing- Original draft preparation. B.D.S: Supervision, Writing- Reviewing and Editing. G.H.T.1,3: Conceptualization, Supervision, Writing- Reviewing and Editing. All authors have reviewed the final version of the manuscript and agree with the publication of the results presented. GHT is the guarantor of this work and, as such, had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study was approved by the Research Ethics Committee (REC) of Hospital São Lucas da Pontifícia Universidade Católica do Rio Grande do Sul (No. 3.803.681), REC of Hospital de Clinicas de Porto Alegre (No. 2016-0286), and in the Basic Health Unit of IAPI and Family Health Strategy of IAPI (approved by the National Health Council in accordance with resolution 466/12 and by the Porto Alegre Municipal Health Office). All authors signed the confidentiality document for data usage.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Telo, G.H., Matzenbacher, L.S., Fontoura, L.F. et al. Hidden barriers: obesity bias in hypertension treatment. Int J Obes 48, 1506–1512 (2024). https://doi.org/10.1038/s41366-024-01613-4
Received:
Revised:
Accepted:
Published:
Version of record:
Issue date:
DOI: https://doi.org/10.1038/s41366-024-01613-4